Clinical and Pathological Findings Associated with Aerosol Exposure of Macaques to Ricin Toxin
Abstract
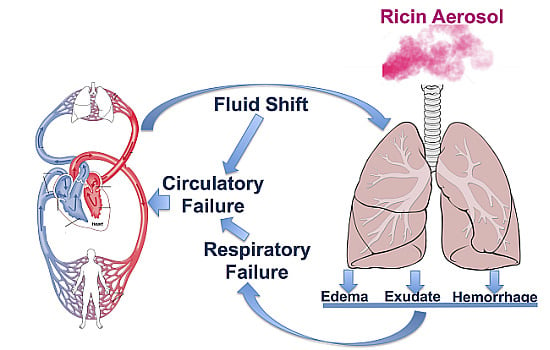
:1. Introduction
2. Results and Discussion
2.1. Lethal Aerosolized Ricin Exposure
| ID | Expt | Age (year) | Telemetry | Weight (kg) | Dose (µg/kg) | Survival (h) | % weight change | Lung % body weight |
|---|---|---|---|---|---|---|---|---|
| JE27 | 1 | 4.16 | N | 7.99 | 38.5 | 25 | −2.63 | 1.47 |
| JL68 | 1 | 3.71 | Y | 4.98 | 26.8 | 27 | −1.81 | 1.94 |
| KA65 | 1 | 2.16 | Y | 3.49 | 9.4 | 28 | 1.43 | 2.06 |
| JD11 | 2 | 4.34 | Y | 5.81 | 13.9 | 52 | −8.78 | 2.34 |
| JR16 | 2 | 3.24 | Y | 4.56 | 29.6 | 46 | −10.09 | 2.89 |
| KI03 | 2 | 2.1 | N | 3.81 | 22.6 | 48 | −4.46 | 2.77 |
2.2. Clinical Signs Following Lethal Ricin Exposure

2.3. Laboratory Findings
| Parameter | Units 1 | Δ Post Ricin | ||
|---|---|---|---|---|
| Mean | SEM | P 2 | ||
| Neutrophil | cell/mm3 | 24192.8 | 3301.4 | 0.0005 |
| Lymphocyte | cell/mm3 | −1904.2 | 1166.9 | 0.0031 |
| Monocyte | cell/mm3 | 452.2 | 161.9 | 0.0709 |
| Eosinophil | cell/mm3 | 106.3 | 139.0 | 0.6195 |
| Basophil | cell/mm3 | 37.1 | 15.5 | 0.0573 |
| Platelets | platelets/mm3 | −333.3 | 17742.0 | 0.9857 |
| RBC | cell × 106/mm3 | 1.51 | 0.32 | 0.0053 |
| Hgb | g/dL | 3.20 | 0.70 | 0.0060 |
| Hct | % by volume | 9.53 | 1.94 | 0.0044 |

| Parameter | Units | Δ Post Ricin | ||
|---|---|---|---|---|
| Mean | SEM | P | ||
| Na | mEq/L | 2.67 | 0.76 | 0.0171 |
| K | mEq/L | 0.55 | 0.32 | 0.1475 |
| Cl | mEq/L | 0.67 | 1.43 | 0.6606 |
| Glucose | mg/dL | 14.33 | 7.31 | 0.1070 |
| BUN | mg/dL | 10.50 | 3.45 | 0.0287 |
| Creatinine | mg/dL | 0.51 | 0.17 | 0.0300 |
| Total protein | g/dL | −0.85 | 0.27 | 0.0268 |
| Albumin | g/dL | −0.87 | 0.14 | 0.0014 |
| Globulin | g/dL | 0.02 | 0.15 | 0.9154 |
| AST | U/L | 25.33 | 12.07 | 0.0898 |
| ALT | U/L | 4.00 | 2.77 | 0.2082 |

2.4. Results of Post-Mortem Examinations

2.5. Sublethal Aerosolized Ricin Exposure

3. Experimental Details
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Griffiths, G.D. Understanding ricin from a defensive viewpoint. Toxins 2011, 3, 1373–1392. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.D. Bioterrorism: Toxins as weapons. J. Pharm. Pract. 2012, 25, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Reisler, R.B.; Smith, L.A. The need for continued development of ricin countermeasures. Adv. Prev. Med. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Bradberry, S.M.; Dickers, K.J.; Rice, P.; Griffiths, G.D.; Vale, J.A. Ricin poisoning. Toxicol. Rev. 2003, 22, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Holtermann, K. Response to a Ricin Incident: Guidelines for Federal, State, and Local Public Health and Medical Officials. 2006; pp. 1–88. Available online: http://www.bt.cdc.gov/agent/ricin/hp.asp (accessed on 4 June 2015). [Google Scholar]
- Schep, L.J.; Temple, W.A.; Butt, G.A.; Beasley, M.D. Ricin as a weapon of mass terror—Separating fact from fiction. Environ. Int. 2009, 35, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Audi, J.; Belson, M.; Patel, M.; Schier, J.; Osterloh, J. Ricin poisoning: A comprehensive review. JAMA J. Am. Med. Assoc. 2005, 294, 2342–2351. [Google Scholar] [CrossRef] [PubMed]
- Franz, D.R.; Jaax, N.K. Chapter 32: Ricin Toxin. In Medical Aspects of Chemical and Biological Warfare; Sidell, F.R., Takafuji, E.T., Franz, D.R., Eds.; Office of the Surgeon General of the Army: Washington, DC, USA, 1997; Volume 3, pp. 631–642. [Google Scholar]
- Roy, C.J.; Song, K.; Sivasubramani, S.K.; Gardner, D.J.; Pincus, S.H. Animal models of ricin toxicosis. Curr. Top. Microbiol. Immunol. 2012, 357, 243–257. [Google Scholar] [PubMed]
- Pincus, S.H.; Smallshaw, J.E.; Song, K.; Berry, J.; Vitetta, E.S. Passive and active vaccination strategies to prevent ricin poisoning. Toxins 2011, 3, 1163–1184. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, M.; Didier, P.J.; Sivasubramani, S.K.; Doyle, L.A.; Holley, J.; Roy, C.J. Pathology of Lethal and Sublethal Doses of Aerosolized Ricin in Rhesus Macaques. Toxicol. Pathol. 2014, 42, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.J.; Hale, M.; Hartings, J.M.; Pitt, L.; Duniho, S. Impact of inhalation exposure modality and particle size on the respiratory deposition of ricin in BALB/c mice. Inhal. Toxicol. 2003, 15, 619–638. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, G.D.; Phillips, G.J.; Holley, J. Inhalation toxicology of ricin preparations: Animal models, prophylactic and therapeutic approaches to protection. Inhal. Toxicol. 2007, 19, 873–887. [Google Scholar] [CrossRef] [PubMed]
- Sandvig, K.; van Deurs, B. Endocytosis and intracellular transport of ricin: Recent discoveries. FEBS Lett. 1999, 452, 67–70. [Google Scholar] [CrossRef]
- Lord, M.J.; Jolliffe, N.A.; Marsden, C.J.; Pateman, C.S.; Smith, D.C.; Spooner, R.A.; Watson, P.D.; Roberts, L.M. Ricin. Mechanisms of cytotoxicity. Toxicol. Rev. 2003, 22, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Benson, J.M.; Gomez, A.P.; Wolf, M.L.; Tibbetts, B.M.; March, T.H. The acute toxicity, tissue distribution, and histopathology of inhaled ricin in Sprague Dawley rats and BALB/c mice. Inhal. Toxicol. 2011, 23, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.; Korcheva, V.; Jacoby, D.B.; Magun, B. Intrapulmonary delivery of ricin at high dosage triggers a systemic inflammatory response and glomerular damage. Am. J. Pathol. 2007, 170, 1497–1510. [Google Scholar] [CrossRef] [PubMed]
- David, J.; Wilkinson, L.J.; Griffiths, G.D. Inflammatory gene expression in response to sub-lethal ricin exposure in Balb/c mice. Toxicology 2009, 264, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Lindauer, M.L.; Wong, J.; Iwakura, Y.; Magun, B.E. Pulmonary inflammation triggered by ricin toxin requires macrophages and IL-1 signaling. J. Immunol. 2009, 183, 1419–1426. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmsen, C.L.; Pitt, M.L. Lesions of acute inhaled lethal ricin intoxication in rhesus monkeys. Vet. Pathol. 1996, 33, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.J.; Brey, R.N.; Mantis, N.J.; Mapes, K.; Pop, I.V.; Pop, L.M.; Ruback, S.; Killeen, S.Z.; Doyle-Meyers, L.; Vinet-Oliphant, H.S.; et al. Thermostable ricin vaccine protects rhesus macaques against aerosolized ricin: Epitope-specific neutralizing antibodies correlate with protection. Proc. Natl. Acad. Sci. USA 2015, 112, 3782–3787. [Google Scholar] [PubMed]
- Pincus, S.H.; Eng, L.; Cooke, C.L.; Maddaloni, M. Identification of hypoglycemia in mice as a surrogate marker of ricin toxicosis. Comp. Med. 2002, 52, 530–533. [Google Scholar] [PubMed]
- Tang, X. Tumor-associated macrophages as potential diagnostic and prognostic biomarkers in breast cancer. Cancer Lett. 2013, 332, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Soulas, C.; Conerly, C.; Kim, W.-K.; Burdo, T.H.; Alvarez, X.; Lackner, A.A.; Williams, K.C. Recently infiltrating MAC387+ monocytes/macrophages a third macrophage population involved in SIV and HIV encephalitic lesion formation. Am. J. Pathol. 2011, 178, 2121–2135. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Biswas, S.K.; Galdiero, M.R.; Sica, A.; Locati, M. Macrophage plasticity and polarization in tissue repair and remodelling. J. Pathol. 2013, 229, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Smallshaw, J.; Firan, A.; Fulmer, J.; Ruback, S.L.; Ghetie, V.; Vitetta, E. A novel recombinant vaccine which protects mice against ricin intoxication. Vaccine 2002, 20, 3422–3427. [Google Scholar] [CrossRef]
- Vitetta, E.S.; Smallshaw, J.E.; Coleman, E.; Jafri, H.; Foster, C.; Munford, R.; Schindler, J. A pilot clinical trial of a recombinant ricin vaccine in normal humans. Proc. Natl. Acad. Sci. USA 2006, 103, 2268–2273. [Google Scholar] [CrossRef] [PubMed]
- Maddaloni, M.; Cooke, C.; Wilkinson, R.; Stout, A.V.; Eng, L.; Pincus, S.H. Immunological characteristics associated with protective efficacy of antibodies to ricin. J. Immunol. 2004, 172, 6221–6228. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.; Plüddemann, A.; Martinez Estrada, F. Macrophage heterogeneity in tissues: Phenotypic diversity and functions. Immunol. Rev. 2014, 262, 36–55. [Google Scholar] [CrossRef] [PubMed]
- Sica, A.; Mantovani, A. Macrophage plasticity and polarization: In vivo veritas. J. Clin. Investig. 2012, 122, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Pincus, S.H.; Johnson, C.; Maresh, G.; Song, K. Improving Anti-Ricin Antibodies: Chimerization and Selection of Ricin-Resistant Hybridoma Cell Lines. In Ricin Toxin, 1st ed.; Cherwonogrodzky, J.W., Ed.; Bentham Science Publishers, 2014; Volume 1, pp. 130–144. [Google Scholar]
- Wu, F.; Fan, S.; Martiniuk, F.; Pincus, S.; Müller, S.; Kohler, H.; Tchou-Wong, K.-M. Protective effects of anti-ricin A-chain antibodies delivered intracellularly against ricin-induced cytotoxicity. WJBC 2010, 1, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Roche, J.; Stone, M.; Gross, L.; Lindner, M.; Seaner, R.; Pincus, S.; Obrig, T. Post-exposure targeting of specific epitopes on ricin toxin abrogates toxin-induced hypoglycemia, hepatic injury, and lethality in a mouse model. Lab. Investig. 2008, 88, 1178–1191. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pincus, S.H.; Bhaskaran, M.; Brey, R.N., III; Didier, P.J.; Doyle-Meyers, L.A.; Roy, C.J. Clinical and Pathological Findings Associated with Aerosol Exposure of Macaques to Ricin Toxin. Toxins 2015, 7, 2121-2133. https://doi.org/10.3390/toxins7062121
Pincus SH, Bhaskaran M, Brey RN III, Didier PJ, Doyle-Meyers LA, Roy CJ. Clinical and Pathological Findings Associated with Aerosol Exposure of Macaques to Ricin Toxin. Toxins. 2015; 7(6):2121-2133. https://doi.org/10.3390/toxins7062121
Chicago/Turabian StylePincus, Seth H., Manoj Bhaskaran, Robert N. Brey, III, Peter J. Didier, Lara A. Doyle-Meyers, and Chad J. Roy. 2015. "Clinical and Pathological Findings Associated with Aerosol Exposure of Macaques to Ricin Toxin" Toxins 7, no. 6: 2121-2133. https://doi.org/10.3390/toxins7062121
APA StylePincus, S. H., Bhaskaran, M., Brey, R. N., III, Didier, P. J., Doyle-Meyers, L. A., & Roy, C. J. (2015). Clinical and Pathological Findings Associated with Aerosol Exposure of Macaques to Ricin Toxin. Toxins, 7(6), 2121-2133. https://doi.org/10.3390/toxins7062121