Methodologies and Wearable Devices to Monitor Biophysical Parameters Related to Sleep Dysfunctions: An Overview
Abstract
:1. Introduction
- An in-depth discussion about sleep’s role in psychological, physiological, and behavioral mechanisms and the importance of sleep monitoring to detect and track symptoms related to sleep disturbances or disorders;
- A comprehensive overview of prototype and commercial wearable devices for sleep monitoring, reported in the scientific literature and on the market, enabling discreet and accurate monitoring of users’ vital signs during sleep;
- An overview of classical and representative-learning algorithms for sleep staging and sleep disorder detection by analyzing data related to single or multiple vital signs;
- A survey of the scientific works analyzing the effect of the COVID-19 pandemic on sleep functions, ascribable to both infection and changes in lifestyle.
2. Importance of Sleep Monitoring
3. Survey of Wearable Devices for Sleep Monitoring Presented in the Literature
- Brain activity using EEG with a high SNR, measuring also advanced sleep markers, such as sleep spindles and K-complexes;
- Eye movement using EOG;
- Physiological factors, with high accuracy for measuring heart rate (median error of 1.7 beats/min) and respiration (median error of 1 BrPM);
- Sleep stages, almost as well as polysomnography;
- Gross body movement and sleep posture.
4. Overview of Commercial Wearable Devices for Detecting Sleep Disorders
5. A Survey about Algorithms for Sleep Staging and Disorders Detection
5.1. Overview of Algorithms for Sleep Staging
5.2. Algorithms for Detecting Sleep Disorders
6. Effects of COVID-19 Pandemic on Sleep
- Insomnia;
- Sleep disruptions;
- Irregularity of the circadian rhythm;
- Nightmares;
- Reduction in sleep quality and duration;
- Excessive daytime sleepiness;
- Decreased focus;
- Bad mood.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Worley, S.L. The Extraordinary Importance of Sleep. Pharm. Ther. 2018, 43, 758–763. [Google Scholar]
- Okano, K.; Kaczmarzyk, J.R.; Dave, N.; Gabrieli, J.D.E.; Grossman, J.C. Sleep Quality, Duration, and Consistency Are Associated with Better Academic Performance in College Students. NPJ Sci. Learn. 2019, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Kapsi, S.; Katsantoni, S.; Drigas, A. The Role of Sleep and Impact on Brain and Learning. Int. J. Recent Contrib. Eng. Sci. IT (IJES) 2020, 8, 59–68. [Google Scholar] [CrossRef]
- Garbarino, S.; Lanteri, P.; Bragazzi, N.L.; Magnavita, N.; Scoditti, E. Role of Sleep Deprivation in Immune-Related Disease Risk and Outcomes. Commun. Biol. 2021, 4, 1304. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, D.J.; Ellenbogen, J.M.; Bianchi, M.T.; Czeisler, C.A. Sleep Deficiency and Motor Vehicle Crash Risk in the General Population: A Prospective Cohort Study. BMC Med. 2018, 16, 44. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Dai, C.; Ba, Y.; Zhang, L.; Shao, Y.; Tian, J. Effect of Sleep Deprivation on the Working Memory-Related N2-P3 Components of the Event-Related Potential Waveform. Front. Neurosci. 2020, 14, 469. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; The National Academies Collection: Reports Funded by National Institutes of Health; Colten, H.R., Altevogt, B.M., Eds.; National Academies Press: Washington, DC, USA, 2006; ISBN 978-0-309-10111-0. [Google Scholar]
- Kales, A.; Soldatos, C.R.; Kales, J.D. Sleep Disorders: Insomnia, Sleepwalking, Night Terrors, Nightmares, and Enuresis. Ann. Intern. Med. 1987, 106, 582–592. [Google Scholar] [CrossRef]
- Sack, R.L.; Auckley, D.; Auger, R.R.; Carskadon, M.A.; Wright, K.P., Jr.; Vitiello, M.V.; Zhdanova, I.V. Circadian Rhythm Sleep Disorders: Part I, Basic Principles, Shift Work and Jet Lag Disorders. Sleep 2007, 30, 1460–1483. [Google Scholar] [CrossRef]
- Gigli, G.L.; Adorati, M.; Dolso, P.; Piani, A.; Valente, M.; Brotini, S.; Budai, R. Restless Legs Syndrome in End-Stage Renal Disease. Sleep Med. 2004, 5, 309–315. [Google Scholar] [CrossRef]
- MedlinePlus. Sleep Disorders. Available online: https://medlineplus.gov/sleepdisorders.html (accessed on 15 July 2022).
- Kelly, J.M.; Strecker, R.E.; Bianchi, M.T. Recent Developments in Home Sleep-Monitoring Devices. ISRN Neurol 2012, 2012, 768794. [Google Scholar] [CrossRef]
- Robbins, R.; Seixas, A.; Masters, L.W.; Chanko, N.; Diaby, F.; Vieira, D.; Jean-Louis, G. Sleep Tracking: A Systematic Review of the Research Using Commercially Available Technology. Curr. Sleep Med. Rep. 2019, 5, 156–163. [Google Scholar] [CrossRef]
- Hussain, Z.; Sheng, Q.Z.; Zhang, W.E.; Ortiz, J.; Pouriyeh, S. A Review of the Non-Invasive Techniques for Monitoring Different Aspects of Sleep. ACM Trans. Comput. Healthc. 2022, 3, 24. [Google Scholar] [CrossRef]
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed]
- De Fazio, R.; De Vittorio, M.; Visconti, P. A BLE-Connected Piezoresistive and Inertial Chest Band for Remote Monitoring of the Respiratory Activity by an Android Application: Hardware Design and Software Optimization. Future Internet 2022, 14, 183. [Google Scholar] [CrossRef]
- De Fazio, R.; Al-Hinnawi, A.-R.; De Vittorio, M.; Visconti, P. An Energy-Autonomous Smart Shirt Employing Wearable Sensors for Users’ Safety and Protection in Hazardous Workplaces. Appl. Sci. 2022, 12, 2926. [Google Scholar] [CrossRef]
- De Fazio, R.; Stabile, M.; De Vittorio, M.; Velázquez, R.; Visconti, P. An Overview of Wearable Piezoresistive and Inertial Sensors for Respiration Rate Monitoring. Electronics 2021, 10, 2178. [Google Scholar] [CrossRef]
- Imtiaz, S.A. A Systematic Review of Sensing Technologies for Wearable Sleep Staging. Sensors 2021, 21, 1562. [Google Scholar] [CrossRef]
- Schutte-Rodin, S.; Deak, M.C.; Khosla, S.; Goldstein, C.A.; Yurcheshen, M.; Chiang, A.; Gault, D.; Kern, J.; O’Hearn, D.; Ryals, S.; et al. Evaluating Consumer and Clinical Sleep Technologies: An American Academy of Sleep Medicine Update. J. Clin. Sleep Med. 2021, 17, 2275–2282. [Google Scholar] [CrossRef]
- Chinoy, E.D.; Cuellar, J.A.; Jameson, J.T.; Markwald, R.R. Performance of Four Commercial Wearable Sleep-Tracking Devices Tested under Unrestricted Conditions at Home in Healthy Young Adults. Nat. Sci. Sleep 2022, 14, 493–516. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Broström, A.; Tsang, H.W.H.; Griffiths, M.D.; Haghayegh, S.; Ohayon, M.M.; Lin, C.-Y.; Pakpour, A.H. Sleep Problems during COVID-19 Pandemic and Its’ Association to Psychological Distress: A Systematic Review and Meta-Analysis. eClinicalMedicine 2021, 36, 100916. [Google Scholar] [CrossRef]
- Lin, Y.N.; Liu, Z.R.; Li, S.Q.; Li, C.X.; Zhang, L.; Li, N.; Sun, X.W.; Li, H.P.; Zhou, J.P.; Li, Q.Y. Burden of Sleep Disturbance During COVID-19 Pandemic: A Systematic Review. Nat. Sci. Sleep 2021, 13, 933–966. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.K.; Molla, M.M.A.; Hasan, P.; Sharif, M.M.; Hossain, F.S.; Amin, M.R.; Rahman, M.R. Persistence of Sleep Disturbance among Post-COVID Patients: Findings from a 2-Month Follow-up Study in a Bangladeshi Cohort. J. Med. Virol. 2022, 94, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Tachiquin, R.; Velázquez, R.; Del-Valle-Soto, C.; Gutiérrez, C.A.; Carrasco, M.; De Fazio, R.; Trujillo-León, A.; Visconti, P.; Vidal-Verdú, F. Wearable Urban Mobility Assistive Device for Visually Impaired Pedestrians Using a Smartphone and a Tactile-Foot Interface. Sensors 2021, 21, 5274. [Google Scholar] [CrossRef] [PubMed]
- de Fazio, R.; Perrone, E.; Velázquez, R.; De Vittorio, M.; Visconti, P. Development of a Self-Powered Piezo-Resistive Smart Insole Equipped with Low-Power BLE Connectivity for Remote Gait Monitoring. Sensors 2021, 21, 4539. [Google Scholar] [CrossRef]
- Chokroverty, S. Overview of Sleep & Sleep Disorders. Indian J. Med. Res. 2010, 131, 126–140. [Google Scholar] [CrossRef]
- Thorpy, M.J. Classification of Sleep Disorders. Neurotherapeutics 2012, 9, 687–701. [Google Scholar] [CrossRef]
- Surantha, N.; Kusuma, G.P.; Isa, S.M. Internet of Things for Sleep Quality Monitoring System: A Survey. In Proceedings of the 2016 11th International Conference on Knowledge, Information and Creativity Support Systems (KICSS), Yogyakarta, Indonesia, 10–11 November 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 1–6. [Google Scholar]
- Wickboldt, A.T.; Bowen, A.F.; Kaye, A.J.; Kaye, A.M.; Bueno, F.R.; Kaye, A.D. Sleep Physiology, Abnormal States, and Therapeutic Interventions. Ochsner J. 2012, 12, 123–134. [Google Scholar]
- Chesson, A.L., Jr.; Ferber, R.A.; Fry, J.M.; Grigg-Damberger, M.; Hartse, K.M.; Hurwitz, T.D.; Johnson, S.; Kader, G.A.; Littner, M.; Rosen, G.; et al. The Indications for Polysomnography and Related Procedures. Sleep 1997, 20, 423–487. [Google Scholar] [CrossRef]
- Dijk, D.-J.; Neri, D.F.; Wyatt, J.K.; Ronda, J.M.; Riel, E.; Ritz-De Cecco, A.; Hughes, R.J.; Elliott, A.R.; Prisk, G.K.; West, J.B.; et al. Sleep, Performance, Circadian Rhythms, and Light-Dark Cycles during Two Space Shuttle Flights. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2001, 281, 1647–1664. [Google Scholar] [CrossRef]
- Oh, C.-M.; Kim, H.Y.; Na, H.K.; Cho, K.H.; Chu, M.K. The Effect of Anxiety and Depression on Sleep Quality of Individuals with High Risk for Insomnia: A Population-Based Study. Front. Neurol. 2019, 10, 849. [Google Scholar] [CrossRef]
- Silvani, A.; Dampney, R.A.L. Central Control of Cardiovascular Function during Sleep. Am. J. Physiol.-Heart Circ. Physiol. 2013, 305, H1683–H1692. [Google Scholar] [CrossRef] [PubMed]
- Somers, V.K.; Dyken, M.E.; Mark, A.L.; Abboud, F.M. Sympathetic-Nerve Activity during Sleep in Normal Subjects. N. Engl. J. Med. 1993, 328, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Murali, N.S.; Svatikova, A.; Somers, V.K. Cardiovascular Physiology and Sleep. Front. Biosci. 2003, 8, s636–s652. [Google Scholar] [CrossRef] [PubMed]
- Anusha, A.S.; Preejith, S.P.; Akl, T.J.; Sivaprakasam, M. Electrodermal Activity Based Autonomic Sleep Staging Using Wrist Wearable. Biomed. Signal Process. Control 2022, 75, 103562. [Google Scholar] [CrossRef]
- Mayo Clinic Polysomnography (Sleep Study). Available online: https://www.mayoclinic.org/tests-procedures/polysomnography/about/pac-20394877 (accessed on 15 July 2022).
- Beach, C.; Karim, N.; Casson, A.J. A Graphene-Based Sleep Mask for Comfortable Wearable Eye Tracking. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 6693–6696. [Google Scholar]
- Greco, V.; Bergamo, D.; Cuoccio, P.; Konkoly, K.R.; Lombardo, K.M.; Lewis, P.A. Wearing an Eye Mask during Overnight Sleep Improves Episodic Learning and Alertness. bioRxiv-Neurosci. 2022, 1, 1–21. [Google Scholar] [CrossRef]
- Rostaminia, S.; Homayounfar, S.Z.; Kiaghadi, A.; Andrew, T.L.; Ganesan, D. PhyMask: Robust Sensing of Brain Activity and Physiological Signals during Sleep with an All-Textile Eye Mask. arXiv 2010, arXiv:2106.07645. [Google Scholar] [CrossRef]
- Hussain, I.; Park, S.J. HealthSOS: Real-Time Health Monitoring System for Stroke Prognostics. IEEE Access 2020, 8, 213574–213586. [Google Scholar] [CrossRef]
- Dang, B.; Dicarlo, J.; Lukashov, S.; Hinds, N.; Reinen, J.; Wen, B.; Hao, T.; Bilal, E.; Rogers, J. Development of a Smart Sleep Mask with Multiple Sensors. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC), Virtual, 1–5 November 2021; pp. 7058–7062. [Google Scholar]
- Homayounfar, S.Z.; Rostaminia, S.; Kiaghadi, A.; Chen, X.; Alexander, E.T.; Ganesan, D.; Andrew, T.L. Multimodal Smart Eyewear for Longitudinal Eye Movement Tracking. Matter 2020, 3, 1275–1293. [Google Scholar] [CrossRef]
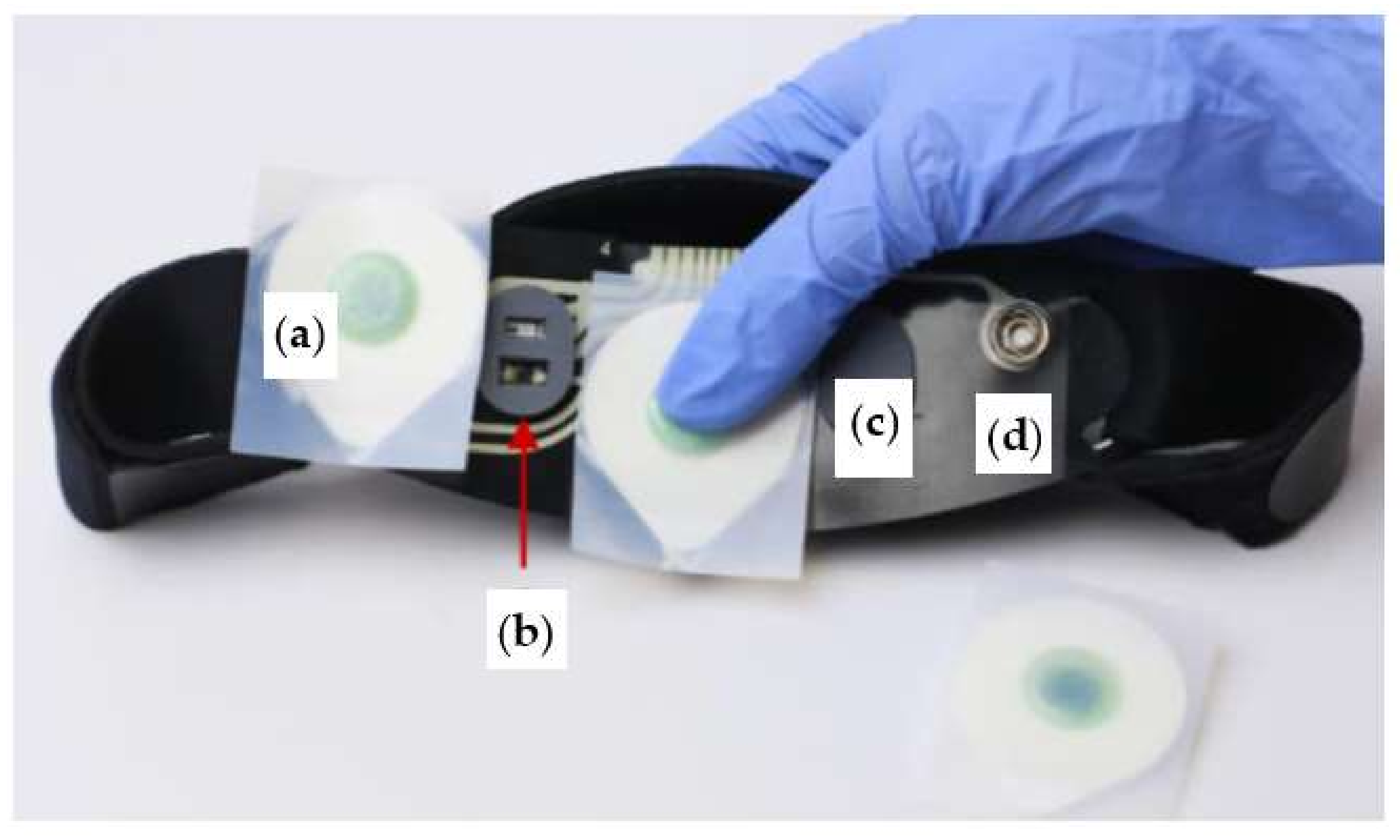
- Puri, R.S.; Athanassiadis, A.G.; Gill, N.; Sathya, S.S.; Rathod, G.; Wahi, A.; Satat, G.; Majmudar, M.; Shah, P. Design and Preliminary Evaluation of a Wearable Device for Mass-Screening of Sleep Apnea. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2016, 2016, 1870–1873. [Google Scholar] [CrossRef]
- Manoni, A.; Loreti, F.; Radicioni, V.; Pellegrino, D.; Della Torre, L.; Gumiero, A.; Halicki, D.; Palange, P.; Irrera, F. A New Wearable System for Home Sleep Apnea Testing, Screening, and Classification. Sensors 2020, 20, 7014. [Google Scholar] [CrossRef]
- Kuo, C.-E.; Liang, S.-F.; Li, Y.-C.; Cherng, F.-Y.; Lin, W.-C.; Chen, P.-Y.; Liu, Y.-C.; Shaw, F.-Z. An EOG-Based Sleep Monitoring System and Its Application on On-Line Sleep-Stage Sensitive Light Control. In Proceedings of the International Conference on Physiological Computing Systems (PhyCS), Lisbon, Portugal, 7–9 January 2014; pp. 20–30. [Google Scholar]
- Hei, Y.; Yuan, T.; Fan, Z.; Yang, B.; Hu, J. Sleep Staging Classification Based on a New Parallel Fusion Method of Multiple Sources Signals. Physiol. Meas. 2022, 43, 045003. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.; Sakharov, V.; Bulanov, S. Personal Apparatus for Conducting Electroencephalography. U.S. Patent WO2021183940A1, 13 March 2020. [Google Scholar]
- Brainbit. Brainbit Manual. Available online: http://brainbit.com/ (accessed on 3 March 2022).
- Lopez-Gordo, M.A.; Sanchez-Morillo, D.; Valle, F.P. Dry EEG Electrodes. Sensors 2014, 14, 12847–12870. [Google Scholar] [CrossRef] [PubMed]
- Diep, C.; Garcia-Molina, G.; Jasko, J.; Manousakis, J.; Ostrowski, L.; White, D.; Anderson, C. Acoustic Enhancement of Slow Wave Sleep on Consecutive Nights Improves Alertness and Attention in Chronically Short Sleepers. Sleep Med. 2021, 81, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Muse™. Headband Manual. Available online: https://choosemuse.com/ (accessed on 3 March 2022).
- Western University, Canada. Assessing the Effects of the Muse Sleep Intervention on Sleep; Western University: London, ON, Canada, 2021. Available online: https://clinicaltrials.gov (accessed on 10 February 2022).
- Dreem|Sleep Pioneers. Available online: https://dreem.com/en/ (accessed on 3 March 2022).
- da Costa, T.D.; Vara, M.D.F.F.; Cristino, C.S.; Zanella, T.Z.; Neto, G.N.N.; Nohama, P. Breathing Monitoring and Pattern Recognition with Wearable Sensors; IntechOpen: London, UK, 2019; ISBN 978-1-78984-497-9. [Google Scholar]
- Arnal, P.J.; Thorey, V.; Debellemaniere, E.; Ballard, M.E.; Bou Hernandez, A.; Guillot, A.; Jourde, H.; Harris, M.; Guillard, M.; Van Beers, P.; et al. The Dreem Headband Compared to Polysomnography for Electroencephalographic Signal Acquisition and Sleep Staging. Sleep 2020, 43, zsaa097. [Google Scholar] [CrossRef] [PubMed]
- IBand+ EEG Headband|Sleep Improvement & Lucid Dreaming Wearable Device. Available online: https://www.ibandplus.com/ (accessed on 4 March 2022).
- Neuroon Open: World’s Smartest Sleep Tracker. Available online: https://www.indiegogo.com/projects/2172509 (accessed on 4 March 2022).
- Somni Mask—The Easiest Way to Lucid Dreaming. Available online: https://somni.org/ (accessed on 14 March 2022).
- BrainLink by Macrotellect|Healthy Brainwaves for Everyone. Available online: http://www.macrotellect.com/ (accessed on 15 March 2022).
- Sleep Shepherd: Sleep Optimizer and Tracker. Available online: https://sleepshepherd.com/ (accessed on 14 March 2022).
- Kim, Y.; Moon, J.; Lee, H.-J.; Bae, C.-S.; Sohn, S. Integration of Electroencephalography Based Services into Consumer Electronics. In Proceedings of the 2012 IEEE 16th International Symposium on Consumer Electronics, Harrisburg, PA, USA, 4–6 June 2012; pp. 1–2. [Google Scholar]
- Sleep Profiler™ Specifications. Available online: https://www.advancedbrainmonitoring.com/products/sleep-profiler#section-specification (accessed on 14 March 2022).
- Levendowski, D.J.; Hamilton, G.S.; St. Louis, E.K.; Penzel, T.; Dawson, D.; Westbrook, P.R. A Comparison between Auto-Scored Apnea-Hypopnea Index and Oxygen Desaturation Index in the Characterization of Positional Obstructive Sleep Apnea. Nat. Sci. Sleep 2019, 11, 69–78. [Google Scholar] [CrossRef]
- Levendowski, D.J.; Ferini-Strambi, L.; Gamaldo, C.; Cetel, M.; Rosenberg, R.; Westbrook, P.R. The Accuracy, Night-to-Night Variability, and Stability of Frontopolar Sleep Electroencephalography Biomarkers. J. Clin. Sleep Med. 2017, 13, 791–803. [Google Scholar] [CrossRef]
- SmartSleep Deep Sleep Headband. Available online: https://www.usa.philips.com/c-e/smartsleep/deep-sleep-headband.html (accessed on 28 February 2022).
- Centers for Disease Control and Prevention (CDC). Unhealthy Sleep-Related Behaviors—12 States, 2009. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 233–238. [Google Scholar]
- American Sleep Association. Sleep Statistics: Data about Sleep Disorders. Available online: https://www.sleepassociation.org/about-sleep/sleep-statistics/ (accessed on 15 July 2022).
- Kang, D.Y.; DeYoung, P.N.; Malhotra, A.; Owens, R.L.; Coleman, T.P. A State Space and Density Estimation Framework for Sleep Staging in Obstructive Sleep Apnea. IEEE Trans. Biomed. Eng. 2018, 65, 1201–1212. [Google Scholar] [CrossRef]
- Malik, J.; Lo, Y.-L.; Wu, H. Sleep-Wake Classification via Quantifying Heart Rate Variability by Convolutional Neural Network. Physiol. Meas. 2018, 39, 085004. [Google Scholar] [CrossRef] [PubMed]
- Chouchou, F.; Desseilles, M. Heart Rate Variability: A Tool to Explore the Sleeping Brain? Front. Neurosci. 2014, 8, 402. [Google Scholar] [CrossRef]
- Gil, B.; Anastasova, S.; Yang, G.Z. A Smart Wireless Ear-Worn Device for Cardiovascular and Sweat Parameter Monitoring during Physical Exercise: Design and Performance Results. Sensors 2019, 19, 1616. [Google Scholar] [CrossRef] [PubMed]
- Radha, M.; Fonseca, P.; Moreau, A.; Ross, M.; Cerny, A.; Anderer, P.; Long, X.; Aarts, R.M. Sleep Stage Classification from Heart-Rate Variability Using Long Short-Term Memory Neural Networks. Sci. Rep. 2019, 9, 11644. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Lee, Y.J.; Jeong, D.U.; Park, K.S. Unconstrained Sleep Stage Estimation Based on Respiratory Dynamics and Body Movement. Methods Inf. Med. 2016, 55, 545–555. [Google Scholar] [CrossRef] [PubMed]
- Tataraidze, A.; Anishchenko, L.; Korostovtseva, L.; Bochkarev, M.; Sviryaev, Y.; Ivashov, S. Estimation of a Priori Probabilities of Sleep Stages: A Cycle-Based Approach. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2017, 2017, 3745–3748. [Google Scholar] [CrossRef]
- Beattie, Z.; Oyang, Y.; Statan, A.; Ghoreyshi, A.; Pantelopoulos, A.; Russell, A.; Heneghan, C. Estimation of Sleep Stages in a Healthy Adult Population from Optical Plethysmography and Accelerometer Signals. Physiol. Meas. 2017, 38, 1968–1979. [Google Scholar] [CrossRef]
- Yang, J.; Keller, J.M.; Popescu, M.; Skubic, M. Sleep Stage Recognition Using Respiration Signal. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2016, 2016, 2843–2846. [Google Scholar] [CrossRef]
- Aggarwal, K.; Khadanga, S.; Joty, S.; Kazaglis, L.; Srivastava, J. A Structured Learning Approach with Neural Conditional Random Fields for Sleep Staging. In Proceedings of the 2018 IEEE International Conference on Big Data (Big Data), Seattle, WA, USA, 10–13 December 2018; pp. 1318–1327. [Google Scholar]
- Purves, D.; Augustine, G.J.; Fitzpatrick, D.; Katz, L.C.; LaMantia, A.-S.; McNamara, J.O.; Williams, S.M. Stages of Sleep. In Neuroscience, 2nd ed.; Sinauer Associates: Sunderland, MA, USA, 2001. [Google Scholar]
- Malafeev, A.; Laptev, D.; Bauer, S.; Omlin, X.; Wierzbicka, A.; Wichniak, A.; Jernajczyk, W.; Riener, R.; Buhmann, J.; Achermann, P. Automatic Human Sleep Stage Scoring Using Deep Neural Networks. Front. Neurosci. 2018, 12, 781. [Google Scholar] [CrossRef]
- Wen, W. Sleep Quality Detection Based on EEG Signals Using Transfer Support Vector Machine Algorithm. Front. Neurosci. 2021, 15, 670745. [Google Scholar] [CrossRef]
- Shen, H.; Ran, F.; Xu, M.; Guez, A.; Li, A.; Guo, A. An Automatic Sleep Stage Classification Algorithm Using Improved Model Based Essence Features. Sensors 2020, 20, 4677. [Google Scholar] [CrossRef]
- Faust, O.; Razaghi, H.; Barika, R.; Ciaccio, E.J.; Acharya, U.R. A Review of Automated Sleep Stage Scoring Based on Physiological Signals for the New Millennia. Comput. Methods Programs Biomed. 2019, 176, 81–91. [Google Scholar] [CrossRef]
- Liang, S.-F.; Kuo, C.-E.; Hu, Y.-H.; Cheng, Y.-S. A Rule-Based Automatic Sleep Staging Method. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2011, 2011, 6067–6070. [Google Scholar] [CrossRef]
- Tagluk, M.E.; Sezgin, N.; Akin, M. Estimation of Sleep Stages by an Artificial Neural Network Employing EEG, EMG and EOG. J. Med. Syst. 2010, 34, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, R.; Gotman, J. Computer-Assisted Sleep Staging. IEEE Trans. Biomed. Eng. 2001, 48, 1412–1423. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, A.; Safari, A.; Mohebbi, M. Sleep Stage Classification Based on ECG-Derived Respiration and Heart Rate Variability of Single-Lead ECG Signal. In Proceedings of the 2019 26th National and 4th International Iranian Conference on Biomedical Engineering (ICBME), Tehran, Iran, 27–28 November 2019; pp. 158–163. [Google Scholar]
- McKight, P.E.; Najab, J. Kruskal-Wallis Test. In The Corsini Encyclopedia of Psychology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2010; p. 1. ISBN 978-0-470-47921-6. [Google Scholar]
- Ramírez-Gallego, S.; Lastra, I.; Martínez-Rego, D.; Bolón-Canedo, V.; Benítez, J.M.; Herrera, F.; Alonso-Betanzos, A. Fast-MRMR: Fast Minimum Redundancy Maximum Relevance Algorithm for High-Dimensional Big Data. Int. J. Intell. Syst. 2017, 32, 134–152. [Google Scholar] [CrossRef]
- Fonseca, P.; den Teuling, N.; Long, X.; Aarts, R.M. A Comparison of Probabilistic Classifiers for Sleep Stage Classification. Physiol. Meas. 2018, 39, 055001. [Google Scholar] [CrossRef]
- Li, Q.; Li, Q.; Liu, C.; Shashikumar, S.P.; Nemati, S.; Clifford, G.D. Deep Learning in the Cross-Time Frequency Domain for Sleep Staging from a Single-Lead Electrocardiogram. Physiol. Meas. 2018, 39, 124005. [Google Scholar] [CrossRef]
- Sateia, M.J. International Classification of Sleep Disorders-Third Edition. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef]
- Young, T.; Palta, M.; Dempsey, J.; Skatrud, J.; Weber, S.; Badr, S. The Occurrence of Sleep-Disordered Breathing among Middle-Aged Adults. N. Engl. J. Med. 1993, 328, 1230–1235. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, Q.; Wang, Y.; Qiu, C. A Real-Time Auto-Adjustable Smart Pillow System for Sleep Apnea Detection and Treatment. In Proceedings of the 2013 ACM/IEEE International Conference on Information Processing in Sensor Networks (IPSN), Philadelphia, PA, USA, 8–11 April 2013; pp. 179–190. [Google Scholar]
- Lyons, M.M.; Bhatt, N.Y.; Pack, A.I.; Magalang, U.J. Global Burden of Sleep-Disordered Breathing and Its Implications. Respirology 2020, 25, 690–702. [Google Scholar] [CrossRef]
- Acquavella, J.; Mehra, R.; Bron, M.; Suomi, J.M.-H.; Hess, G.P. Prevalence of Narcolepsy and Other Sleep Disorders and Frequency of Diagnostic Tests from 2013–2016 in Insured Patients Actively Seeking Care. J. Clin. Sleep Med. 2020, 16, 1255–1263. [Google Scholar] [CrossRef]
- Neikrug, A.B.; Ancoli-Israel, S. Sleep Disorders in the Older Adult—A Mini-Review. Gerontology 2010, 56, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, M.; Forouzanfar, M. Sleep Apnea Detection from Single-Lead ECG: A Comprehensive Analysis of Machine Learning and Deep Learning Algorithms. IEEE Trans. Instrum. Meas. 2022, 71, 4003011. [Google Scholar] [CrossRef]
- Sharma, M.; Tiwari, J.; Patel, V.; Acharya, U.R. Automated Identification of Sleep Disorder Types Using Triplet Half-Band Filter and Ensemble Machine Learning Techniques with EEG Signals. Electronics 2021, 10, 1531. [Google Scholar] [CrossRef]
- Mostafa, S.S.; Mendonça, F.; Ravelo-Garcia, A.G.; Gabriel Juliá-Serdá, G.; Morgado-Dias, F. Multi-Objective Hyperparameter Optimization of Convolutional Neural Network for Obstructive Sleep Apnea Detection. IEEE Access 2020, 8, 129586–129599. [Google Scholar] [CrossRef]
- Lado, M.J.; Vila, X.A.; Rodríguez-Liñares, L.; Méndez, A.J.; Olivieri, D.N.; Félix, P. Detecting Sleep Apnea by Heart Rate Variability Analysis: Assessing the Validity of Databases and Algorithms. J. Med. Syst. 2011, 35, 473–481. [Google Scholar] [CrossRef]
- Vila, X.A.; Lado, M.J.; Mendez, A.J.; Olivieri, D.N.; Linares, L.R. An R Package for Heart Rate Variability Analysis. In Proceedings of the 2009 IEEE International Symposium on Intelligent Signal Processing, Budapest, Hungary, 26–28 August 2009; pp. 217–222. [Google Scholar]
- Bahrami, M.; Forouzanfar, M. Detection of Sleep Apnea from Single-Lead ECG: Comparison of Deep Learning Algorithms. In Proceedings of the 2021 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lausanne, Switzerland, 23–25 June 2021; pp. 1–5. [Google Scholar]
- Alqaraawi, A.; Alwosheel, A.; Alasaad, A. Heart Rate Variability Estimation in Photoplethysmography Signals Using Bayesian Learning Approach. Healthc. Technol. Lett. 2016, 3, 136–142. [Google Scholar] [CrossRef]
- Bhat, S.; Chokroverty, S. Sleep Disorders and COVID-19. Sleep Med. 2021, 91, 253–261. [Google Scholar] [CrossRef]
- Coronasomnia: Definition, Symptoms, and Solutions. Available online: https://www.sleepfoundation.org/covid-19-and-sleep/coronasomnia (accessed on 10 April 2022).
- Jahrami, H.; BaHammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep Problems during the COVID-19 Pandemic by Population: A Systematic Review and Meta-Analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef]
- Pedder, H.; Sarri, G.; Keeney, E.; Nunes, V.; Dias, S. Data Extraction for Complex Meta-Analysis (DECiMAL) Guide. Syst. Rev. 2016, 5, 212. [Google Scholar] [CrossRef]
- Metlaine, A.; Sauvet, F.; Chennaoui, M.; Leger, D.; Elbaz, M. Sleep and COVID-19. A Case Report of a Mild COVID-19 Patient Monitored by Consumer-Targeted Sleep Wearables. Sensors 2021, 21, 7944. [Google Scholar] [CrossRef]
- Salfi, F.; Amicucci, G.; Corigliano, D.; D’Atri, A.; Viselli, L.; Tempesta, D.; Ferrara, M. Changes of Evening Exposure to Electronic Devices during the COVID-19 Lockdown Affect the Time Course of Sleep Disturbances. Sleep 2021, 44, zsab080. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.T.C.; Ramamurthy, M.B.; Aishworiya, R.; Rajgor, D.D.; Tran, A.P.; Hiriyur, P.; Kunaseelan, S.; Jabri, M.; Goh, D.Y.T. School Closure during the Coronavirus Disease 2019 (COVID-19) Pandemic—Impact on Children’s Sleep. Sleep Med. 2021, 78, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The Enemy Who Sealed the World: Effects Quarantine Due to the COVID-19 on Sleep Quality, Anxiety, and Psychological Distress in the Italian Population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef]
- Sun, W.; Ling, J.; Zhu, X.; Lee, T.M.-C.; Li, S.X. Associations of Weekday-to-Weekend Sleep Differences with Academic Performance and Health-Related Outcomes in School-Age Children and Youths. Sleep Med. Rev. 2019, 46, 27–53. [Google Scholar] [CrossRef] [PubMed]
- Cachón-Zagalaz, J.; Zagalaz-Sánchez, M.L.; Arufe-Giráldez, V.; Sanmiguel-Rodríguez, A.; González-Valero, G. Physical Activity and Daily Routine among Children Aged 0–12 during the COVID-19 Pandemic in Spain. Int. J. Environ. Res. Public Health 2021, 18, 703. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Guo, Y.; Xiao, Y.; Zhu, R.; Sun, W.; Huang, W.; Liang, D.; Tang, L.; Zhang, F.; Zhu, D.; et al. The Effects of Online Homeschooling on Children, Parents, and Teachers of Grades 1–9 during the COVID-19 Pandemic. Med. Sci. Monit. 2020, 26, e925591. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Farias, N.; Toledo-Vargas, M.; Miranda-Marquez, S.; Cortinez-O’Ryan, A.; Cristi-Montero, C.; Rodriguez-Rodriguez, F.; Martino-Fuentealba, P.; Okely, A.D.; del Pozo Cruz, B. Sociodemographic Predictors of Changes in Physical Activity, Screen Time, and Sleep among Toddlers and Preschoolers in Chile during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 176. [Google Scholar] [CrossRef]
- Dutta, K.; Mukherjee, R.; Sen, D.; Sahu, S. Effect of COVID-19 Lockdown on Sleep Behavior and Screen Exposure Time: An Observational Study among Indian School Children. Biol. Rhythm. Res. 2022, 53, 628–639. [Google Scholar] [CrossRef]
- Abid, R.; Ammar, A.; Maaloul, R.; Souissi, N.; Hammouda, O. Effect of COVID-19-Related Home Confinement on Sleep Quality, Screen Time and Physical Activity in Tunisian Boys and Girls: A Survey. Int. J. Environ. Res. Public Health 2021, 18, 3065. [Google Scholar] [CrossRef]
- Partinen, M.; Holzinger, B.; Morin, C.M.; Espie, C.; Chung, F.; Penzel, T.; Benedict, C.; Bolstad, C.J.; Cedernaes, J.; Chan, R.N.Y.; et al. Sleep and Daytime Problems during the COVID-19 Pandemic and Effects of Coronavirus Infection, Confinement and Financial Suffering: A Multinational Survey Using a Harmonised Questionnaire. BMJ Open 2021, 11, e050672. [Google Scholar] [CrossRef]
- Hale, L.; Guan, S. Screen Time and Sleep among School-Aged Children and Adolescents: A Systematic Literature Review. Sleep Med. Rev. 2015, 21, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Adıbelli, D.; Sümen, A. The Effect of the Coronavirus (COVID-19) Pandemic on Health-Related Quality of Life in Children. Child. Youth Serv. Rev. 2020, 119, 105595. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Tang, H.; Jin, Q.; Wang, G.; Yang, Z.; Chen, H.; Yan, H.; Rao, W.; Owens, J. Sleep of Preschoolers during the Coronavirus Disease 2019 (COVID-19) Outbreak. J. Sleep Res. 2021, 30, e13142. [Google Scholar] [CrossRef] [PubMed]
- Mishra, T.; Wang, M.; Metwally, A.A.; Bogu, G.K.; Brooks, A.W.; Bahmani, A.; Alavi, A.; Celli, A.; Higgs, E.; Dagan-Rosenfeld, O.; et al. Pre-symptomatic detection of COVID-19 from smartwatch data. Nat. Biomed. Eng. 2020, 4, 1208–1220. [Google Scholar] [CrossRef]
- Quer, G.; Radin, J.M.; Gadaleta, M.; Baca-Motes, K.; Ariniello, L.; Ramos, E.; Kheterpal, V.; Topol, E.J.; Steinhubl, S.R. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nat. Med. 2020, 27, 73–77. [Google Scholar] [CrossRef]
- Chi, J.; Cao, W.; Gu, Y. Recent Progress in Sleep Quality Monitoring and Non-Drug Sleep Improvement. Front. Hum. Neurosci. 2020, 14, 21. [Google Scholar] [CrossRef]
- Roomkham, S.; Lovell, D.; Cheung, J.; Perrin, D. Promises and Challenges in the Use of Consumer-Grade Devices for Sleep Monitoring. IEEE Rev. Biomed. Eng. 2018, 11, 53–67. [Google Scholar] [CrossRef]
- Kwon, S.; Kim, H.; Yeo, W.-H. Recent Advances in Wearable Sensors and Portable Electronics for Sleep Monitoring. iScience 2021, 24, 102461. [Google Scholar] [CrossRef]





| Work | Number of Detected Parameters | Type of Detected Parameters | Availability of Wireless Module to Transfer Data | Tested Individuals | Accuracy | Sensitivity | Invasiveness |
|---|---|---|---|---|---|---|---|
| Mask B [39] | 1 | Eye movement | No | 4 | N.A. 1 | N.A. 1 | Low |
| Phymask [41] | 5 | Brain activity, eye movement, heart, and respiration rate, sleep stages, body movement | Yes | 10 | >0.8 2 | >0.8 2 | Low |
| HealthSOS [42] | 1 | Brain activity | Yes | 37 | 92% | 98% | Low |
| Smart Sleep Mask [43] | 4 | Eye movement, head position, temperature, and breathing sounds | Yes | 1 | N.A. 1 | N.A. 1 | Low |
| Chesma [44] | 2 | Eye movement, heart rate | Yes | 1 | N.A. 1 | N.A. 1 | Low |
| ARAM [45] | 2 | Respiration activity, body movement | No | 6 | N.A. 1 | N.A. 1 | Medium |
| Morfea [46] | 3 | Apnea and hypopnea events, chest movements, head position | Yes | 1 | 93% | 89% | Medium |
| Device | Number of Parameters Detected | Integrated Sensors | Gathered Parameters | Feedbacks/ Interventions | Cost |
|---|---|---|---|---|---|
| BrainBit [50] | 4 | EEG, PPG, EMG, EOG | Brain activity, heart rate, body movement, eye movement | Psychology and cognitive remediation | USD $499 |
| SmartSleep [67] | 1 | EEG | Brain activity | Audio tones to boost the slow wave | USD $399 |
| Muse S [53] | 4 | EEG, PPG, gyroscope, accelerometer | Brain activity, heart rate, breath rate, body movements | Digital sleeping pills (sleep stories and meditation, ambient soundscape, nature and music biofeedbacks) | USD $399 |
| Dreem 2 [55] | 4 | EEG, PPG, gyroscope, accelerometer | Brain activity, heart rate, breath rate, body movement | CBT-I exercises | N.A. 1 |
| iBand+ [58] | 2 | EEG, accelerometer, gyroscope | Brain activity, head movement | Audio tones to induce sleep | USD $449 |
| Neuroon Open [59] | 4 | EEG, EOG, PPG, thermometer, | Brain activity, eye movement, body temperature, blood oxygenation | Audio tones to induce sleep | N.A. 1 |
| Somni [60] | 2 | EOG, accelerometer | Eye movement, head movement | Audiovisual feedback to induce sleep | N.A. 1 |
| BrainLink Pro [61] | 4 | EEG, PPG, gyroscope thermometer, accelerometer, | Brain activity, heart rate, body temperature, head movement | No | USD $259 |
| Sleep Shepherd [62] | 2 | EEG, gyroscope, movement sensor | Brain activity head movement | Binaural tones to induce sleep | N.A. 1 |
| Sleep Profiler [64] | 5 | EEG, EOG, EMG, accelerometer, ECG (optional), PPG (optional), nasal transducer (model SP29), pulse rate sensor (model SP29), oximeter (model SP29) | Brain activity, eye movement, head position, heart rate, quantitative snoring | No | N.A. 1 |
| CGMH-Training | CGMH-Validation | DRAMS Subjects | UCDSADB | |
|---|---|---|---|---|
| TP | 4.464 | 1.800 | 1.777 | 1.838 |
| FP | 2.143 | 1.763 | 2.151 | 2.853 |
| TN | 31.550 | 14.906 | 14.532 | 12.883 |
| FN | 3.315 | 1.633 | 1.572 | 2.400 |
| SE (%) | 57.4 | 52.4 | 53.1 | 43.4 |
| SP (%) | 93.6 | 89.4 | 87.1 | 81.9 |
| ACC (%) | 86.8 | 83.1 | 81.4 | 73.7 |
| PR (%) | 67.6 | 50.5 | 45.2 | 39.2 |
| F1 | 0.62 | 0.51 | 0.49 | 0.41 |
| AUC | 0.90 | 0.83 | 0.81 | 0.72 |
| Kappa | 0.54 | 0.41 | 0.38 | 0.24 |
| Stage | Precision | Accuracy | Cohen’s Kappa |
|---|---|---|---|
| Wake | 0.73 ± 0.20 | 0.90 ± 0.07 | 0.63 ± 0.19 |
| REM | 0.71 ± 0.22 | 0.92 ± 0.04 | 0.68 ± 0.22 |
| N1/N2 | 0.80 ± 0.11 | 0.79 ± 0.08 | 0.56 ± 0.15 |
| N3 | 0.62 ± 0.33 | 0.92 ± 0.04 | 0.53 ± 0.27 |
| Authors | Number of Detected Parameters | Detected Parameters | Number of Sleep Stage | Accuracy [%] | Used Algorithms | Participants |
|---|---|---|---|---|---|---|
| J. Malik et al. [71] | 2 | ECG and PPG (deriving HRV and IHR 1) | 2 | 86.8 | CNN | 56 patients and 90 healthy subjects |
| M. Radha et al. [74] | 4 | ECG, EEG, EOG, EMG (deriving HRV) | 4 | N.A. 2 | LSTM | 97 patients and 195 healthy subjects |
| H. Hwang et al. [75] | 2 | Breathing activity and body movements from the PVDF sensor | 2 | 70.9 | Decision rules algorithm | 13 patients and 12 healthy subjects |
| A. Tataraidze et al. [76] | 1 | Effort signals using RIP | 4 | N.A. 2 | XGB, a decision tree-based algorithm | 685 healthy subjects |
| Z. Beattie et al. [77] | 2 | Breathing activity and body movements from a 3D accelerometer and optical PPG (deriving HRV) | 4 | 69.0 | LDA | 60 healthy subjects |
| K. Aggarwal et al. [79] | 1 | Breathing activity from CPAP | 4 | 74.1 | CRF | 400 patients |
| A. Malafeev et al. [81] | 4 | EEG, EMG, ECG, and EOG | 5 | N.A. 2 | RF, LSTM, CNN-LSTM | 23 patients and 18 healthy subjects |
| W. Wen [82] | 1 | EEG | 5 | N.A. 2 | SVM | 6641 healthy subjects |
| H. Shen et al. [83] | 1 | EEG | 4 | 92.0 | Begged trees | Patients and healthy subjects from three databases |
| R. Agarwal et al. [87] | 3 | EEG, EOG, and EMG | 6 | N.A. 2 | CASS | 12 subjects, some of them suffering from sleep disorders |
| A. Rahimi et al. [88] | 1 | ECG (deriving HRV and EDR) | 2 | 81.8 | SVM | Not specified |
| P. Fonseca et al. [91] | 2 | ECG and RIP | 5 | 61.1% | LD, HMM, CRF | 231 subjects, some of them suffering from sleep disorders |
| Q. Li et al. [92] | 1 | ECG (deriving HRV, EDR, and RSA) | 3 | 85.1% | CPC, CNN, SVM | 7451 subjects |
| Work | Number of Detected Parameters | Detected Parameters | Type of Used Algorithm | Detected Sleep Disorder | Features Extracted |
|---|---|---|---|---|---|
| M. Bahrami et al. [99] | 1 | ECG | LDA, QDA, LR, Gaussian naïve Bayes classifiers, Gaussian process, SVMs, KNN, DT, ET, RF, AdaBoost, GB, MLP, MV, convolutional networks, and DRNNs | Sleep apnea | From R–R intervals: minimum, range, median, mean, standard deviation, skewness, kurtosis, the standard deviation of successive differences between adjacent R–R intervals, root mean square of successive differences between normal heartbeats, VLF, LF, HF, cardiovagal index, cardio sympathetic index |
| S. S. Mostafa et al. [101] | 1 | EEG | EBT; EBooT, SVMs, and KNN | OSA | Activity, mobility, and complexity |
| M. Sharma et al. [100] | 2 | ECG and SpO2 | CNN and NSGA-II | Insomnia, NFLE, RBD, PLM disorder, and SDB | N.A. 1 |
| M. J. Lado et al. [102] | 1 | ECG (deriving HR and HRV) | RHRV | OSA | LF/HF quotient |
| M. Bahrami et al. [104] | 1 | ECG | DRNNs and CNN | Sleep apnea | R-peak amplitude and R–R intervals |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Fazio, R.; Mattei, V.; Al-Naami, B.; De Vittorio, M.; Visconti, P. Methodologies and Wearable Devices to Monitor Biophysical Parameters Related to Sleep Dysfunctions: An Overview. Micromachines 2022, 13, 1335. https://doi.org/10.3390/mi13081335
De Fazio R, Mattei V, Al-Naami B, De Vittorio M, Visconti P. Methodologies and Wearable Devices to Monitor Biophysical Parameters Related to Sleep Dysfunctions: An Overview. Micromachines. 2022; 13(8):1335. https://doi.org/10.3390/mi13081335
Chicago/Turabian StyleDe Fazio, Roberto, Veronica Mattei, Bassam Al-Naami, Massimo De Vittorio, and Paolo Visconti. 2022. "Methodologies and Wearable Devices to Monitor Biophysical Parameters Related to Sleep Dysfunctions: An Overview" Micromachines 13, no. 8: 1335. https://doi.org/10.3390/mi13081335
APA StyleDe Fazio, R., Mattei, V., Al-Naami, B., De Vittorio, M., & Visconti, P. (2022). Methodologies and Wearable Devices to Monitor Biophysical Parameters Related to Sleep Dysfunctions: An Overview. Micromachines, 13(8), 1335. https://doi.org/10.3390/mi13081335










