Ultrasensitive Electrochemical Immunosensors Using Nanobodies as Biocompatible Sniffer Tools of Agricultural Contaminants and Human Disease Biomarkers
Abstract
:1. Introduction

2. Generation of Nanobodies
3. Immobilization Strategies of Nanobodies
3.1. Direct Surface Functionalization
3.2. Indirect “In Tube” and “In Drop” Surface Functionalization
4. Nanobodies for the Electrochemical Detection of Food Contaminants
4.1. Allergens
4.2. Insecticides
4.3. Pesticides
4.4. Bacterial Toxins
4.5. Thermal Processing Product—Acrylamide

| Conductive Supports | Method | Redox Probe | Analyte | Nanobodies (Nbs) | Linear Range | Sensor Signal Stability | LOD | Ref |
|---|---|---|---|---|---|---|---|---|
| SPCE/ Chitosan/ AuNPs+ Fc-COOH | CV | 0.1 mM APP, 2 mM NADH | Ara h 1 1,3,5,10, 15,30,50,100 ng/mL | Nb152-HA (100 μg/mL)/ Nb152-B (100 μg/mL) | 4.5–55 ng/mL | 15 days at 4 °C | 0.86 ng/mL | [52] |
| SPCE/ nylon + CA | DPV | 1 mg/mL 1-NP | 3-PBA 8 × 10−4; 1 × 10−3, 5 × 10−3, 1 × 10−2, 5 × 10−2, 1 × 10−1, 5 × 10−1, 1 ng/mL & 3-PBA-BSACAT (10 μg/mL) | Nb-ALP (400 µg/mL) | 0.8–1000 pg/mL | 5 weeks at 4 °C | 0.64 pg/mL | [54] |
| SPCE | CV (cathodic peak) | 0.5 mM HQ/ 1.5 mM H2O2 | Parathion 10−2–102 ng/mL & parathion H1-OVACAT (5 µg/mL) | VHH9-HRP (9 µg/mL) | 10−2–102 ng/mL (8 conc.) | 63 days for selected 0.1 and 1 ng/mL parathion after regeneration cycles | 2.26 pg/mL | [55] |
| GCE | SWV | 2 mM K3[Fe(CN)6] | Cry1C -protein (1, 10, 102, 10−1, 10−2, 10−3 ng/mL) | Nb51 (100 µg/mL on electrode) & Nb54 (1 mg/mL added in GO-Th supernatant) | 1, 10, 102, 10−1, 10−2, 10−3 ng/mL | Nbs stable at 70 °C & Immuno-sensor stable for 15 days at 4 °C | 3.2 pg/mL | [57] |
| GCE/OMC + AuNPs | DPV | N2-saturated 100 mM PBS pH 7.4 | EPSPS - enzyme (1, 10, 102, 10−1, 10−2, 10−3 ng/mL) | Nb (10 µg/mL) & Th (100 µg/mL) | 1, 10, 102, 10−1, 10−2, 10−3 ng/mL | Nbs stable at 70 °C (~60% activity) & Immunosensor stable over 14 days at 4 °C (~80% from initial activity at 10 ng/mL Ag) | 0.72 pg/mL | [58] |
| Au-IDE | CV & EIS | 5 mM K3[Fe(CN)6]/ K4[Fe(CN)6] | Ricin chain-A 10−3, 1, 103, 106 pg/mL & 1 pg/mL | Ricin Nbs (5.2 mg/mL) | 10−3, 1, 103, 106 pg/mL | up to 40 °C with a shelf-life of 1 week | 1 fg/mL | [60] |
| SPCE/chitosan NPs | CV (cathodic peak) | 1 mM HQ/ 6% H2O2 | AA (0.39, 0.78, 1.56, 3.125, 12, 5, 25, 50 µg/mL) & XAA-OVACAT (10 µg/mL) | Nb-7E (7.45 µg/mL, used at 1:40 dilution ~ 18 µg/mL) | 0.39 to 50.0 μg/mL | bind to Ag at 95 °C due to four Cys involve in two disulfide bonds | 0.033 μg/mL | [61] |
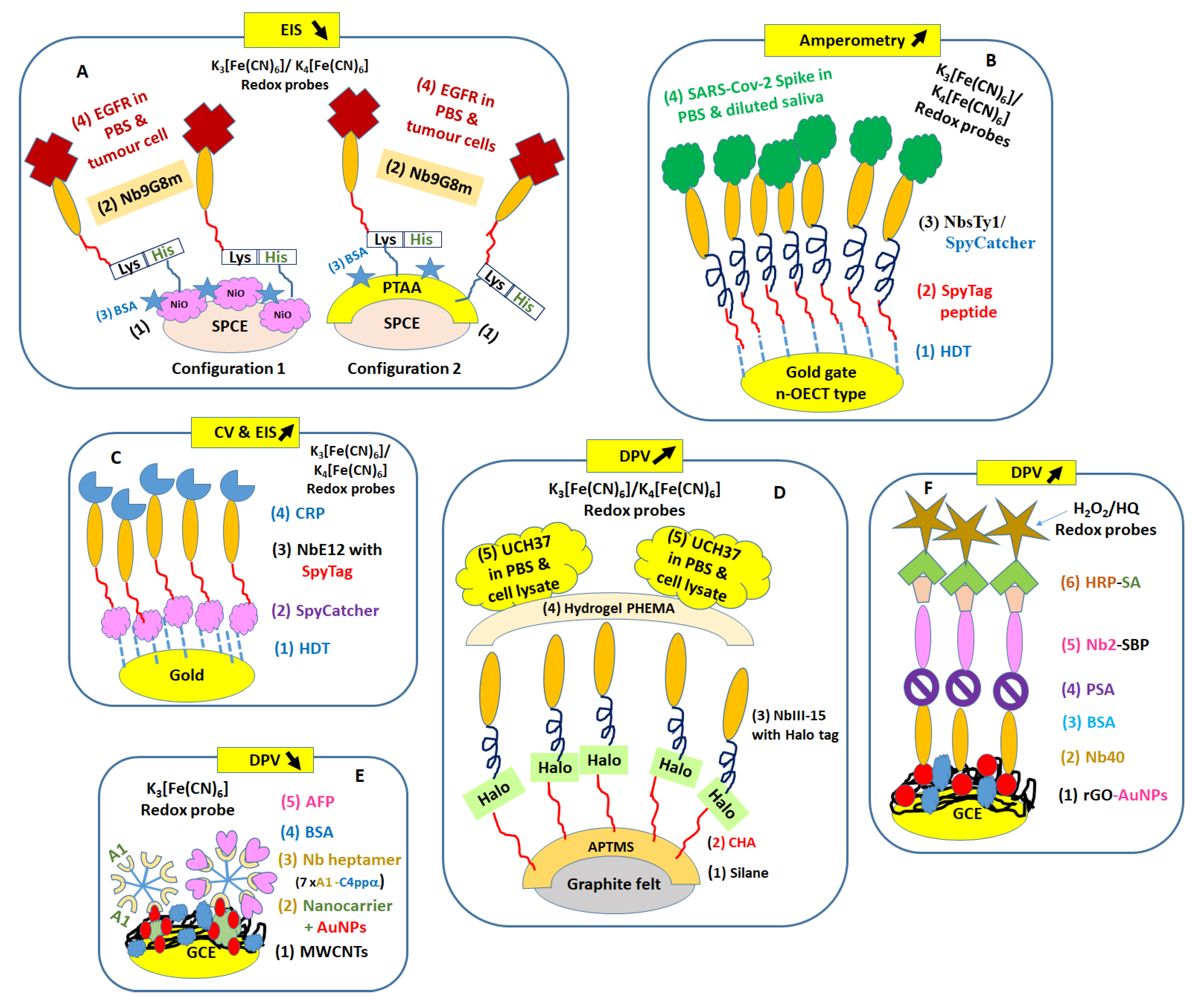
5. Nanobodies for the Electrochemical Detection of Human Biomarkers
5.1. Glycoproteins in Tumour Cells
5.2. Proteins in Complex Media—Saliva, Cell Lysate, Serum, Urine
| Conductive Supports | Method | Redox Probe | Analyte (Ag) | Nanobodies (Nbs) | Linear Range | Sensor Signal Stability | LOD | Ref |
|---|---|---|---|---|---|---|---|---|
| SPCE/ NiO NPs & SPCE/ PTAA film | EIS | 5 mM K3[Fe(CN)6]/ K4[Fe(CN)6] | EGFR 0.25, 1, 5, 10, 15, 25, 50 μg/mL−1 (on NiO NPs) & EGFR 0.5, 1, 5, 10, 15, 25, 50 μg/mL−1 (on PTAA) | Nb9G8m with Lys/His (50 μg/mL) | 0.25 to 50 μg/mL (on NiO NPs) & 0.5 to 50 μg/mL(on PTAA) | up to 40 °C with shelf-life of 1 week | 0.48 µg/mL (NiO NPs) & 1.14 µg/mL (PTAA) | [62] |
| Glass/Au/ HDT | Amperometric | 10 mM K3[Fe(CN)6]/ K4[Fe(CN)6] | SARS-CoV-2 spike 10−9, 10−10, 10−11, 10−12, 10−13 10−14, 10−15, 10−16, 10−17, 10−18 M (in PBS) & SARS-CoV-2 spike 3 × 10−7, 3 × 10−9, 3 × 10−12, 3 × 10−15, 3 × 10−17 M (in 4 × dil. saliva) | on n-OECT gate sensor:Nbs Ty1with SpyCatcher linker 20 × 10−6 M on n-OECT gate sensor & Nbs GFP1 × 10−9 M (as control) | NA | Current stability over 1 h | 10−16 M | [64] |
| Gold | CV & EIS | 5 mM K3[Fe(CN)6]/ K4[Fe(CN)6] | CRP 0.25; 0.35; 0.5; 1; 1.50 µg/mL (for CV/EIS) | NbE12 with SpyTag linker 2.5 µg/mL | 0.25; 0.35; 0.5; 1µg/mL (for CV/EIS) | NA | 0.21 µg/mL | [67] |
| Graphite felt | DPV | 5 mM K3[Fe(CN)6]/ K4[Fe(CN)6] | UCH37 3 × 101, 1 × 102, 2.5 × 102, 5 × 102, 1 × 103, pmoL (in PBS) & ~ 50 pmol UCH37/mL PBS in 1 mg cell lysate | NbIII.15 with HaloTag protein tail (5 × 106 M) | NA | NA | 25–30 pmol in PBS & cell lysate | [70] |
| GCE/ nanocarrier | DPV | 5 mM K3[Fe(CN)6] | AFP 1, 10, 102, 10−1, 10−2, 10−3, 10−4 ng/mL(in PBS) & 6.289, 12.564, 37.320, 72.693 ng/mL (in 4 human sera 10× dil. with PBS) | NbA1-C4bp α with Cys tail assembled intoheptamer structure (10 μg/mL) | 1, 10, 102, 10−1, 10−2, 10−3, 10−4 ng/mL | 14 days at 4 °C | 0.033 pg/mL in PBS | [72] |
| GCE/rGO +AuNPs | DPV | 1 mM HQ, 10 mM H2O2 in deaerated PBS | PSA 10−1, 5 × 10−1, 1, 2.5, 5, 7.5, 15, 2 × 10, 3 × 10, 5 × 10, 102 ng/mL | Nb40 on sensor (80 µg/mL) & Nb2-SBP for sandwich (90 µg/mL) | 10−1 to 102 ng/mL | over 4 weeks at 4 °C | 0.08 ng/mL | [76] |
6. Conclusions and Perspectives
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hamers-Casterman, C.; Atarhouch, T.; Muyldermans, S.; Robinson, G.; Hammers, C.; Bajyana Songa, E.; Bendahman, N.; Hammers, R. Naturally occurring antibodies devoid of light chains. Nature 1993, 363, 446–448. [Google Scholar] [CrossRef] [PubMed]
- Asaadi, Y.; Jouneghani, F.F.; Janani, S.; Rahbarizadeh, F. A comprehensive comparison between camelid nanobodies and single chain variable fragments. Biomark. Res. 2021, 9, 87. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Guo, X.; Liu, T.; Li, L.; Zhou, N.; Ma, X.; Meng, X.; Liu, J.; Zhu, H.; Jia, B.; et al. High in-vivo stability in preclinical and first-in-human experiments with [18F]AlF-RESCA-MIRC213: A 18F-labeled nanobody as PET radiotracer for diagnosis of HER2-positive cancers. Eur. J. Nucl. Med. Mol. Imaging 2023, 50, 302–313. [Google Scholar] [CrossRef]
- Rashidian, M.; Ploegh, H. Nanobodies as non-invasive imaging tools. Immuno-Oncol. Technol. 2020, 7, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Bao, G.; Tang, M.; Zhao, J.; Zhu, X. Nanobody: A promising toolkit for molecular imaging and disease therapy. EJNMMI Res. 2021, 11, 6. [Google Scholar] [CrossRef]
- Berland, L.; Kim, L.; Abousaway, O.; Mines, A.; Mishra, S.; Clark, L.; Hofman, P.; Rashidian, M. Nanobodies for medical imaging: About ready for prime time? Biomolecules 2021, 11, 637. [Google Scholar] [CrossRef]
- Nachit, M.; Montemagno, C.; Clerc, R.; Ahmadi, M.; Briand, F.; Bacot, S.; Devoogdt, N.; Serdjebi, C.; Ghezzi, C.; Sulpice, T.; et al. Molecular imaging of liver inflammation using an anti-VCAM-1 nanobody. Nat. Commun. 2023, 14, 1062. [Google Scholar] [CrossRef]
- Yong Joon Kim, J.; Sang, Z.; Xiang, Y.; Shen, Z.; Shi, Y. Nanobodies: Robust miniprotein binders in biomedicine. Adv. Drug Deliv. Rev. 2023, 195, 114726. [Google Scholar] [CrossRef]
- Jiang, Y.; Lin, Y.; Krishnaswamy, S.; Pan, R.; Wu, Q.; Sandusky-Beltran, L.A.; Liu, M.; Ku, M.-H.; Kong, X.-P.; Congdon, E.E.; et al. Single-domain antibody-based noninvasive in vivo imaging of α-synuclein or tau pathology. Sci. Adv. 2023, 9, eadf3775. [Google Scholar] [CrossRef]
- Al-Baradie, R.S. Nanobodies as versatile tools: A focus on targeted tumor therapy, tumor imaging and diagnostics. Hum. Antibodies 2020, 28, 259–272. [Google Scholar] [CrossRef]
- Su, J.; Liu, X.; Guo, S.; Zhang, J.; Wei, X.; Li, X. Nanobodies: A new potential for prostate cancer treatment. J. Cancer Res. Clin. Oncol. 2023, 149, 6703–6710. [Google Scholar] [CrossRef]
- Jovčevska, I.; Muyldermans, S. The Therapeutic Potential of Nanobodies. BioDrugs 2020, 34, 11–26. [Google Scholar] [CrossRef] [Green Version]
- Deffar, K.; Shi, H.; Li, A.; Wang, X.; Zhu, X. Nanobodies—The new concept in antibody engineering. Afr. J. Biotechnol. 2009, 8, 2645–2652. [Google Scholar]
- Soler, M.A.; Fortuna, S.; De Marco, A.; Laio, A. Binding affinity prediction of nanobody-protein complexes by scoring of molecular dynamics trajectories. Phys. Chem. Chem. Phys. 2018, 20, 3438–3444. [Google Scholar] [CrossRef] [PubMed]
- Bannas, P.; Hambach, J.; Koch-Nolte, F. Nanobodies and nanobody-based human heavy chain antibodies as antitumor therapeutics. Front. Immunol. 2017, 8, 1603. [Google Scholar] [CrossRef]
- Hosseindokht, M.; Bakherad, H.; Zare, H. Nanobodies: A tool to open new horizons in diagnosis and treatment of prostate cancer. Cancer Cell Int. 2021, 21, 580. [Google Scholar] [CrossRef] [PubMed]
- Moliner-Morro, A.; McInerney, G.M.; Hanke, L. Nanobodies in the limelight: Multifunctional tools in the fight against viruses. J. Gen. Virol. 2022, 103, 001731. [Google Scholar] [CrossRef]
- Sroga, P.; Safronetz, D.; Stein, D.R. Nanobodies: A new approach for the diagnosis and treatment of viral infectious diseases. Future Virol. 2020, 15, 195–205. [Google Scholar] [CrossRef]
- Delfin-Riela, T.; Rossotti, M.A.; Mattiuzzo, G.; Echaides, C.; González-Sapienza, G. Nanobody-Based Blocking of Binding ELISA for the Detection of Anti-NS1 Zika-Virus-Specific Antibodies in Convalescent Patients. Trop. Med. Infect. Dis. 2023, 8, 55. [Google Scholar] [CrossRef]
- Hong, J.; Kwon, H.J.; Cachau, R.; Chen, C.Z.; Butay, K.J.; Duan, Z.; Li, D.; Ren, H.; Liang, T.; Zhu, J.; et al. Dromedary camel nanobodies broadly neutralize SARS-CoV-2 variants. Proc. Natl. Acad. Sci. USA 2022, 119, e2201433119. [Google Scholar] [CrossRef]
- Sanaei, M.; Setayesh, N.; Sepehrizadeh, Z.; Mahdavi, M.; Yazdi, M.H. Nanobodies in Human Infections: Prevention, Detection, and Treatment. Immunol. Investig. 2020, 49, 875–896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mei, Y.; Chen, Y.; Sivaccumar, J.P.; An, Z.; Xia, N.; Luo, W. Research progress and applications of nanobody in human infectious diseases. Front. Pharmacol. 2022, 13, 963978. [Google Scholar] [CrossRef] [PubMed]
- Zettl, I.; Ivanova, T.; Strobl, M.R.; Weichwald, C.; Goryainova, O.; Khan, E.; Rutovskaya, M.V.; Focke-Tejkl, M.; Drescher, A.; Bohle, B.; et al. Isolation of nanobodies with potential to reduce patients’ IgE binding to Bet v 1. Allergy Eur. J. Allergy Clin. Immunol. 2022, 77, 1751–1760. [Google Scholar] [CrossRef]
- Wang, W.; Hu, Y.; Li, B.; Wang, H.; Shen, J. Applications of nanobodies in the prevention, detection, and treatment of the evolving SARS-CoV-2. Biochem. Pharmacol. 2023, 208, 115401. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Zhu, J.; Nie, Y.; Hu, R.; Wang, T.; Li, P.; Zhang, Q.; Yang, Y. Nanobody technology for mycotoxin detection in the field of food safety: Current status and prospects. Toxins 2016, 10, 180. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Wang, Y.; Vasylieva, N.; Wan, D.; Yin, Z.; Dong, J.; Hammock, B.D. An Ultrasensitive Bioluminescent Enzyme Immunoassay Based on Nanobody/Nanoluciferase Heptamer Fusion for the Detection of Tetrabromobisphenol A in Sediment. Anal. Chem. 2020, 92, 10083–10090. [Google Scholar] [CrossRef]
- Zhang, J.; Sun, H.; Pei, W.; Jiang, H.; Chen, J. Nanobody-based immunosensing methods for safeguarding public health. J. Biomed. Res. 2021, 35, 318–326. [Google Scholar] [CrossRef]
- Gettemans, J.; de Dobbelaer, B. Tranforming nanobodies into high-precision tools for protein function analysis. Am. J. Physiol. Cell Physiol. 2021, 320, C195–C215. [Google Scholar] [CrossRef]
- Van Audenhove, I.; Gettemans, J. Nanobodies as Versatile Tools to Understand, Diagnose, Visualize and Treat Cancer. EBioMedicine 2016, 8, 40–48. [Google Scholar] [CrossRef] [Green Version]
- Freitas, M.; Nouws, H.P.A.; Delerue-Matos, C. Voltammetric immunosensor to track a major peanut allergen (Ara h 1) in food products employing quantum dot labels. Biosensors 2021, 11, 426. [Google Scholar] [CrossRef]
- Li, H.; Xie, T.; Shi, D.; Jin, J.; Xie, C. Enhanced electrochemiluminescence of luminol at the gold nanoparticle/carbon nanotube/electropolymerised molecular imprinting composite membrane interface for selective recognition of triazophos. Int. J. Environ. Anal. Chem. 2016, 96, 1300–1311. [Google Scholar] [CrossRef]
- White, S.P.; Sreevatsan, S.; Frisbie, C.D.; Dorfman, K.D. Rapid, Selective, Label-Free Aptameric Capture and Detection of Ricin in Potable Liquids Using a Printed Floating Gate Transistor. ACS Sens. 2016, 1, 1213–1216. [Google Scholar] [CrossRef]
- Wu, M.-F.; Wang, Y.; Li, S.; Dong, X.-X.; Yang, J.-Y.; Shen, Y.-D.; Wang, H.; Sun, Y.-M.; Lei, H.-T.; Xu, Z.-L. Ultrasensitive immunosensor for acrylamide based on chitosan/SnO2—SiC hollow sphere nanochains/gold nanomaterial as signal amplification. Anal. Chim. Acta 2019, 1049, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Vásquez, V.; Navas, M.-C.; Jaimes, J.A.; Orozco, J. SARS-CoV-2 electrochemical immunosensor based on the spike-ACE2 complex. Anal. Chim. Acta 2022, 1205, 339718. [Google Scholar] [CrossRef]
- Ding, C.; Zhao, F.; Ren, R.; Lin, J.-M. An electrochemical biosensor for α-fetoprotein based on carbon paste electrode constructed of room temperature ionic liquid and gold nanoparticles. Talanta 2009, 78, 1148–1154. [Google Scholar] [CrossRef]
- Akbari Jonous, Z.; Shayeh, J.S.; Yazdian, F.; Yadegari, A.; Hashemi, M.; Omidi, M. An electrochemical biosensor for prostate cancer biomarker detection using graphene oxide–gold nanostructures. Eng. Life Sci. 2019, 19, 206–216. [Google Scholar] [CrossRef] [Green Version]
- Muyldermans, S. A guide to: Generation and design of nanobodies. FEBS J. 2021, 288, 2084–2102. [Google Scholar] [CrossRef]
- Yan, J.; Li, G.; Hu, Y.; Ou, W.; Wan, Y. Construction of a synthetic phage-displayed nanobody library with CDR3 regions randomized by trinucleotide cassettes for diagnostic applications. J. Transl. Med. 2014, 12, 343. [Google Scholar] [CrossRef]
- Fan, R.; Du, J.; Park, K.-W.; Chang, L.H.; Strieter, E.R.; Strieter, E.R. Immobilization of Nanobodies with Vapor-Deposited Polymer Encapsulation for Robust Biosensors. ACS Appl. Polym. Mater. 2021, 3, 2561–2567. [Google Scholar] [CrossRef]
- Oloketuyi, S.; Mazzega, E.; Zavašnik, J.; Pungjunun, K.; Kalcher, K.; de Marco, A.; Mehmeti, E. Electrochemical immunosensor functionalized with nanobodies for the detection of the toxic microalgae Alexandrium minutum using glassy carbon electrode modified with gold nanoparticles. Biosens. Bioelectron. 2020, 154, 112052. [Google Scholar] [CrossRef]
- Simões, B.; Guedens, W.J.; Keene, C.; Kubiak-Ossowska, K.; Mulheran, P.; Kotowska, A.M.; Scurr, D.J.; Alexander, M.R.; Brroisat, A.; Johnson, S.; et al. Direct immobilization of engineered nanobodies on gold sensors. ACS Appl. Mater. Interfaces 2021, 13, 17353–17360. [Google Scholar] [CrossRef] [PubMed]
- England, C.G.; Luo, H.; Cai, W. HaloTag Technology: A Versatile Platform for Biomedical Applications. Bioconjug. Chem. 2015, 26, 975–986. [Google Scholar] [CrossRef] [Green Version]
- Anderson, G.P.; Liu, J.L.; Shriver-Lake, L.C.; Zabetakis, D.; Sugiharto, V.A.; Chen, H.-W.; Lee, C.-R.; Defang, G.N.; Wu, S.-J.L.; Venkateswaran, N.; et al. Oriented Immobilization of Single-Domain Antibodies Using SpyTag /SpyCatcher Yields Improved Limits of Detection. Anal. Chem. 2019, 91, 9424–9429. [Google Scholar] [CrossRef]
- Guo, K.; Wustoni, S.; Koklu, A.; Diaz-Galicia, E.; Moser, M.; Hama, A.; Alqahtani, A.A.; Ahmed, A.N.; Alhamlan, F.S.; Shuaib, M.; et al. Rapid single-molecule detection of COVID-19 and MERS antigens via nanobody-functionalized organic electrochemical transistors. Nat. Biomed. Eng. 2021, 5, 666–677. [Google Scholar] [CrossRef] [PubMed]
- Patris, S.; De Pauw, P.; Vandeput, M.; Huet, J.; van Antwerpen, P.; Muyldermans, S.; Kauffmann, J.-M. Nanoimmunoassay onto a screen printed electrode for HER2 breast cancer biomarker determination. Talanta 2014, 130, 164–170. [Google Scholar] [CrossRef]
- Wisdom, G.B. Conjugation of antibodies to horseradish peroxidase. Methods Mol Biol. 2005, 295, 127–130. [Google Scholar] [PubMed]
- Cheloha, R.W.; Harmand, T.J.; Wijne, C.; Schwartz, T.U.; Ploegh, H.L. Exploring cellular biochemistry with nanobodies. J. Biol. Chem. 2020, 95, 15307–15327. [Google Scholar] [CrossRef]
- Omidfar, K.; Darzianiazizi, M.; Ahmadi, A.; Daneshpour, M.; Shirazi, H. A high sensitive electrochemical nanoimmunosensor based on Fe3O4/TMC/Au nanocomposite and PT-modified electrode for the detection of cancer biomarker epidermal growth factor receptor. Sens. Actuators B Chem. 2015, 220, 1311–1319. [Google Scholar] [CrossRef]
- Gefen, T.; Vaya, J.; Khatib, S.; Rapoport, I.; Lupo, M.; Barnea, E.; Admon, A.; Heller, E.D.; Aizenshtein, E.; Pitcovski, J. The effect of haptens on protein-carrier immunogenicity. Immunology 2014, 144, 116–126. [Google Scholar] [CrossRef]
- Yan, T.; Zhu, J.; Li, Y.; He, T.; Yang, Y.; Liu, M. Development of a biotinylated nanobody for sensitive detection of aflatoxin B1 in cereal via ELISA. Talanta 2022, 239, 123125. [Google Scholar] [CrossRef]
- Kwon, S.J.; Yang, H.; Jo, K.; Kwak, J. An electrochemical immunosensor using p-aminophenol redox cycling by NADH on a self-assembled monolayer and ferrocene-modified Au electrodes. Analyst 2008, 133, 1599–1604. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Lin, J.; Peng, L.; Wang, Y.; Wu, S.; Ji, X.; Lv, H.; Wu, J.; Zhang, Y.; Wang, S. Nanobody-Based Electrochemical Immunoassay for Sensitive Detection of Peanut Allergen Ara h 1. J. Agric. Food Chem. 2023, 71, 7535–7545. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Liu, Z.; Ding, G.; Li, J.; Vasylieva, N.; Li, Q.X.; Li, D.; Gee, S.J.; Hammock, B.D.; Xu, T. Development of a one-step immunoassay for triazophos using camel single-domain antibody–alkaline phosphatase fusion protein. Anal. Bioanal. Chem. 2019, 411, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- El-Moghazy, A.Y.; Huo, J.; Amaly, N.; Vasylieva, N.; Hammock, B.D.; Sun, G. An innovative nanobody-based electrochemical immunosensor using decorated nylon nanofibers for point-of-care monitoring of human exposure to phrethroid insecticides. ACS Appl. Mater. Interfaces 2020, 12, 6159–6168. [Google Scholar] [CrossRef]
- Yin, W.-J.; Zhang, J.-X.; Wang, H.; Hammock, B.D.; Wen, P. A highly sensitive electrochemical immunosensor based on electrospun nanocomposite for the detection of parathion. Food Chem. 2023, 404, 134371. [Google Scholar] [CrossRef]
- Palma, L.; Muñoz, D.; Berry, C.; Murillo, J.; Caballero, P. Bacillus thuringiensis toxins: An overview of their biocidal activity. Toxins 2014, 6, 3296–3325. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Q.; Li, G.; Zhang, Y.; Zhu, M.; Wan, Y.; Shen, Y. Highly Selective and Sensitive Electrochemical Immunoassay of Cry1C Using Nanobody and π-π Stacked Graphene Oxide/Thionine Assembly. Anal. Chem. 2016, 88, 9830–9836. [Google Scholar] [CrossRef]
- Zhang, M.; Li, G.; Zhou, Q.; Pan, D.; Zhu, M.; Xiao, R.; Zhang, Y.; Wu, G.; Wan, Y.; Shen, Y. Boosted Electrochemical Immunosensing of Genetically Modified Crop Markers Using Nanobody and Mesoporous Carbon. ACS Sens. 2018, 3, 684–691. [Google Scholar] [CrossRef]
- Gaylord, S.T.; Dinh, T.L.; Goldman, E.R.; Anderson, G.P.; Ngan, K.C.; Walt, D.R. Ultrasensitive detection of ricin toxin in multiple sample matrixes using single-domain antibodies. Anal. Chem. 2015, 87, 6570–6577. [Google Scholar] [CrossRef]
- Singh, A.; Pasha, S.K.; Manickam, P.; Bhansali, S. Single-domain antibody thermally stable electrochemical immunosensor. Biosens. Bioelectron. 2016, 83, 162–168. [Google Scholar] [CrossRef] [Green Version]
- Liang, Y.; Zeng, Y.; Luo, L.; Xu, Z.; Shen, Y.; Wang, H.; Hammock, B.D. Detection of Acrylamide in Foodstuffs by Nanobody-Based Immunoassays. J. Agric. Food Chem. 2022, 70, 9179–9186. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Pacheco, A.F.; Monsalve, Y.; Serrano-Rivero, Y.; Salaraz-Uribe, J.; Moreno, E.; Orozco, J. Engineered synthetic nanobody-based biosensors for electrochemical detection of epidermal growth factor receptor. Chem. Eng. J. 2023, 465, 142941. [Google Scholar] [CrossRef]
- Kaczor-Urbanowicz, K.E.; Martin Carreras-Presas, C.; Aro, K.; Tu, M.; Garcia-Godoy, F.; Wong, D.T.W. Saliva diagnostics—Current views and directions. Exp. Biol. Med. 2017, 242, 4596472. [Google Scholar] [CrossRef] [Green Version]
- Koklu, A.; Wustoni, S.; Guo, K.; Silva, R.; Salvigni, L.; Hama, A.; Diaz-Galicia, E.; Moser, M.; Marks, A.; McCulloch, I.; et al. Convection Driven Ultrarapid Protein Detection via Nanobody-Functionalized Organic Electrochemical Transistors. Adv. Mater. 2022, 34, 2202972. [Google Scholar] [CrossRef]
- Luan, Y.-Y.; Yao, Y.-M. The clinical significance and potential role of C-reactive protein in chronic inflammatory and neurodegenerative diseases. Front. Immunol. 2018, 9, 1302. [Google Scholar] [CrossRef] [Green Version]
- Eckschlager, C.; Schwenoha, K.; Roth, C.; Bogner, B.; Oostingh, G.J. Comparative analysis of high CRP-levels in human blood using point-of-care and laboratory-based methods. Pract. Lab. Med. 2019, 17, e00137. [Google Scholar] [CrossRef]
- Oloketuyi, S.; Bernedo, R.; Christmann, A.; Borkowska, J.; Cazzaniga, G.; Schuchmann, H.W.; Niedziolka-Jonsson, J.; Szot-Karpinska, K.; Kolmar, H.; de Marco, A. Native llama nanobody library panning performed by phage and yeast display provides binders suitable for C-reactive protein detection. Biosensors 2021, 11, 496. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Fu, D.; Tang, W.; Cai, Y.; Mctivita, D.; Wang, H.; Xue, R.; Liu, T.; Huang, X.; Dong, L.; et al. Ubiquitin C-terminal Hydrolase 37, a novel predictor for hepatocellular carcinoma recurrence, promotes cell migration and invasion via interacting and deubiquitinating PRP19. Biochim. Biophys. Acta Mol. Cell Res. 2013, 1833, 559–572. [Google Scholar] [CrossRef] [Green Version]
- Fu, J.; Li, J.; Wang, W.; Wu, H.; Zhou, P.; Li, Y.; He, Q.; Tu, Z. One-step oriented immobilization of nanobodies and its application for immunoglobulin purification. J.Chromatogr. A 2019, 1603, 15–22. [Google Scholar] [CrossRef]
- Fan, R.; Li, Y.; Park, K.-P.; Du, J.; Chang, L.H.; Strieter, E.R.; Andrew, T.L. A strategy for accesing nanobody-based electrochemical sensors for analyte detection in complex media. ECS Sens. Plus 2022, 1, 010601. [Google Scholar] [CrossRef]
- Galle, P.R.; Foerster, F.; Kudo, M.; Chan, S.L.; Llovet, J.M.; Qin, S.; Schelman, W.R.; Chintharlapalli, S.; Sherman, M.; Zhu, A.X. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma. Liver Int. 2019, 39, 2214–2229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.; Liu, X.; Su, B.; Zhang, H.; Li, R.; Liu, Z.; Huang, T.; Cao, H. An innovative electrochemical immunosensor based on nanobody heptamer and AuNPs@ZIF-8 nanocomposites as support for the detection of alpha fetoprotein in serum. Microchem. J. 2022, 179, 107463. [Google Scholar] [CrossRef]
- Ahyai, S.A.; Graefen, M.; Steuber, T.; Haese, A.; Schlomm, T.; Walz, J.; Kollermann, J.; Briganti, A.; Zacharias, M.; Friedrich, M.G.; et al. Contemporary Prostate Cancer Prevalence among T1c Biopsy-Referred Men with a Prostate-Specific Antigen Level ≤ 4.0 ng per Milliliter. Eur. Urol. 2008, 53, 750–757. [Google Scholar] [CrossRef]
- Jeun, M.; Park, S.; Kim, Y.; Choi, J.; Song, S.H.; Jeong, I.G.; Kim, C.-S.; Lee, K.H. Self-Normalized Detection of ANXA3 from Untreated Urine of Prostate Cancer Patients without Digital Rectal Examination. Adv. Healthc. Mater. 2017, 6, 1700449. [Google Scholar] [CrossRef] [PubMed]
- Rebelo, T.S.C.R.; Pereira, C.M.; Sales, M.G.F.; Noronha, J.P.; Silva, F. Protein Imprinted Material electrochemical sensor for determination of Annexin A3 in biological samples. Electrochim. Acta 2016, 190, 887–893. [Google Scholar] [CrossRef]
- Liu, X.; Wang, D.; Chu, J.; Xu, Y.; Wang, W. Sandwich pair nanobodies, a potential tool for electrochemical immunosensing serum prostate-specific antigen with preferable specificity. J. Pharm. Biomed. Anal. 2018, 158, 361–369. [Google Scholar] [CrossRef]
- Xu, J.; Xu, K.; Jung, S.; Conte, A.; Lieberman, J.; Muecksch, F.; Cetrulo Lorenci, J.C.; Park, S.; Schmidt, F.; Wang, Z.; et al. Nanobodies from camelid mice and llamas neutralize SARS-CoV-2 variants. Nature 2021, 595, 278–282. [Google Scholar] [CrossRef]
- Sharma, A.; Balda, S.; Apreja, M.; Kataria, K.; Capalash, N.; Sharma, P. COVID-19 diagnosis: Current and future techniques. Int. J. Biol. Macromol. 2021, 193, 1835–1844. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, G.; Lu, H.; Li, H.; Tang, M.; Tong, A. Development of therapeutic antibodies for the treatment of diseases. Molec. Biomed. 2022, 3, 35. [Google Scholar] [CrossRef]
- Mokhtarzadeh, A.; Eivazzadeh-Keihan, R.; Pashazadeh, P.; Hejazi, M.; Gharaatifar, N.; Hasanzadeh, M.; Baradaran, B.; de la Guardia, M. Nanomaterial-based biosensors for detection of pathogenic virus. Trends Analyt Chem. 2017, 97, 445–457. [Google Scholar] [CrossRef]
- Ionescu, R.E.; Marks, R.S.; Gheber, L.A. Manufacturing of nanochannels with controlled dimensions using protease nanolithography. Nano Lett. 2005, 5, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Valdés-Tresanco, M.S.; Valdés-Tresanco, M.E.; Jiménez-Gutiérrez, D.E.; Moreno, E. Structural modelling of nanobodies: A benchmark of state-of-the-art artificial intelligence programs. Molecules 2023, 28, 3991. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Davidsen, K.; Gomez-Castillo, L.; Jiang, H.; Fu, X.; Li, Z.; Liang, Y.; Jahn, M.; Moussa, M.; Dimaio, F.; et al. COMBINES-CID: An efficient method for de novo engineering of highly specific chemically induced protein dimerization systems. Int. J. Biol. Macromol. 2021, 193, 1835–1844. [Google Scholar] [CrossRef] [PubMed]
- Kao, K.S.; Gupta, A.; Zong, G.; Li, C.; Kerschbaumer, I.; Achkar, J.M.; Bournazos, S.; Wang, L.-X.; Ravetch, J.V. Synthetic nanobodies as tools to distinguish IgG Fc glycoforms. Proc. Natl. Acad. Sci. USA 2022, 119, e2212658119. [Google Scholar] [CrossRef]
- Goode, J.; Dillon, G.; Millner, P.A. The development and optimisation of nanobody based electrochemical immunosensors for IgG. Sens. Actuators B Chem. 2016, 234, 478–484. [Google Scholar] [CrossRef] [Green Version]
- Muyldermans, S. Applications of nanobodies. Annu. Rev. Anim. Biosci. 2021, 9, 401–421. [Google Scholar] [CrossRef]
- Steeland, S.; Vandenbroucke, R.E.; Libert, C. Nanobodies as therapeutics: Big opportunities for small antibodies. Drug Discov. Today 2016, 21, 1076–1113. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ionescu, R.E. Ultrasensitive Electrochemical Immunosensors Using Nanobodies as Biocompatible Sniffer Tools of Agricultural Contaminants and Human Disease Biomarkers. Micromachines 2023, 14, 1486. https://doi.org/10.3390/mi14081486
Ionescu RE. Ultrasensitive Electrochemical Immunosensors Using Nanobodies as Biocompatible Sniffer Tools of Agricultural Contaminants and Human Disease Biomarkers. Micromachines. 2023; 14(8):1486. https://doi.org/10.3390/mi14081486
Chicago/Turabian StyleIonescu, Rodica Elena. 2023. "Ultrasensitive Electrochemical Immunosensors Using Nanobodies as Biocompatible Sniffer Tools of Agricultural Contaminants and Human Disease Biomarkers" Micromachines 14, no. 8: 1486. https://doi.org/10.3390/mi14081486
APA StyleIonescu, R. E. (2023). Ultrasensitive Electrochemical Immunosensors Using Nanobodies as Biocompatible Sniffer Tools of Agricultural Contaminants and Human Disease Biomarkers. Micromachines, 14(8), 1486. https://doi.org/10.3390/mi14081486






