Cancers 2019, 11(9), 1358; https://doi.org/10.3390/cancers11091358 - 12 Sep 2019
Cited by 103 | Viewed by 9253
Abstract
The interleukin-3 receptor alpha chain (IL-3R), more commonly referred to as CD123, is widely overexpressed in various hematological malignancies, including acute myeloid leukemia (AML), B-cell acute lymphoblastic leukemia, hairy cell leukemia, Hodgkin lymphoma and particularly, blastic plasmacytoid dendritic neoplasm (BPDCN). Importantly, CD123 is
[...] Read more.
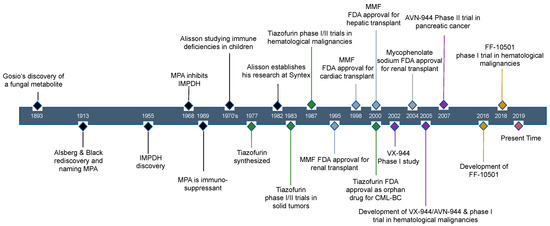
The interleukin-3 receptor alpha chain (IL-3R), more commonly referred to as CD123, is widely overexpressed in various hematological malignancies, including acute myeloid leukemia (AML), B-cell acute lymphoblastic leukemia, hairy cell leukemia, Hodgkin lymphoma and particularly, blastic plasmacytoid dendritic neoplasm (BPDCN). Importantly, CD123 is expressed at both the level of leukemic stem cells (LSCs) and more differentiated leukemic blasts, which makes CD123 an attractive therapeutic target. Various agents have been developed as drugs able to target CD123 on malignant leukemic cells and on the normal counterpart. Tagraxofusp (SL401, Stemline Therapeutics), a recombinant protein composed of a truncated diphtheria toxin payload fused to IL-3, was approved for use in patients with BPDCN in December of 2018 and showed some clinical activity in AML. Different monoclonal antibodies directed against CD123 are under evaluation as antileukemic drugs, showing promising results either for the treatment of AML minimal residual disease or of relapsing/refractory AML or BPDCN. Finally, recent studies are exploring T cell expressing CD123 chimeric antigen receptor-modified T-cells (CAR T) as a new immunotherapy for the treatment of refractory/relapsing AML and BPDCN. In December of 2018, MB-102 CD123 CAR T developed by Mustang Bio Inc. received the Orphan Drug Designation for the treatment of BPDCN. In conclusion, these recent studies strongly support CD123 as an important therapeutic target for the treatment of BPDCN, while a possible in the treatment of AML and other hematological malignancies will have to be evaluated by in the ongoing clinical studies.
Full article