Cyclic Stretch of Either PNS or CNS Located Nerves Can Stimulate Neurite Outgrowth
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Sciatic Nerve and Central Nerves Connected to L4-L5 DRG Explants
2.3. Tensile Stretch Incubator
2.4. GalilTools Programming Code Used for Oscillatory Movement
2.5. DRG Cultures
2.6. Immunocytochemistry
2.7. Immunohistochemistry
2.8. Nerve Cryosectioning and Hematoxylin-Eosin (H&E) Staining
2.9. Imaging and Image Analysis
2.10. Statistical Analysis
3. Results
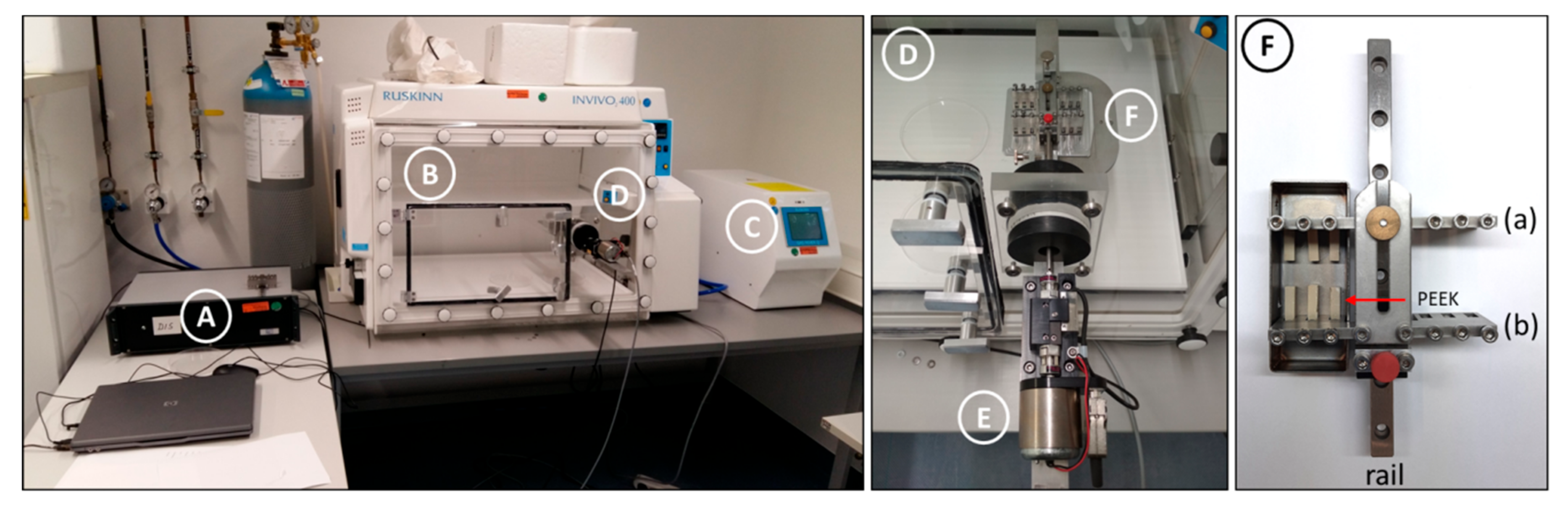
3.1. A Stretch Bioreactor was Built In-House to Apply Cyclic Mechanical Tension to DRG-Nerve Explants
3.2. Mechanical Tension Applied to DRG-Nerve Explants Can Enhance Axonal Outgrowth In vitro
3.3. Unlike 20% Stretch, 10% Stretch Does Not Drastically Change the Cytoarchitecture of the Subjected Nerves
3.4. 10%, but Not 20%, Stretch Enhances Neurite Outgrowth of Mechanoreceptors and/or Proprioceptors but Not Nociceptors
3.5. ATF3 Is Increased by 3 h 10% Mechanical Loading
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Mammoto, T.; Ingber, D.E. Mechanical control of tissue and organ development. Development 2010, 137, 1407–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franze, K. The mechanical control of nervous system development. Development 2013, 140, 3069–3077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LeGoff, L.; Lecuit, T. Mechanical forces and growth in animal tissues. Cold Spring Harb. Perspect. Biol. 2016, 8, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Geffeney, S.L.; Goodman, M.B. How We Feel: Ion Channel Partnerships that Detect Mechanical Inputs and Give Rise to Touch and Pain Perception. Neuron 2012, 74, 609–619. [Google Scholar] [CrossRef] [Green Version]
- Proske, U.; Gandevia, S.C. The proprioceptive senses: Their roles in signaling body shape, body position and movement, and muscle force. Physiol. Rev. 2012, 92, 1651–1697. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.H. Stretch growth of integrated axon tracts: Extremes and exploitations. Prog. Neurobiol. 2009, 89, 231–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suter, D.M.; Miller, K.E. The emerging role of forces in axonal elongation. Prog. Neurobiol. 2011, 94, 91–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lamoureux, P.; Ruthel, G.; Buxbaum, R.E.; Heidemann, S.R. Mechanical tension can specify axonal fate in hippocampal neurons. J. Cell Biol. 2002, 159, 499–508. [Google Scholar] [CrossRef]
- Loverde, J.R.; Pfister, B.J. Developmental axon stretch stimulates neuron growth while maintaining normal electrical activity, intracellular calcium flux, and somatic morphology. Front. Cell. Neurosci. 2015, 9, 308. [Google Scholar] [CrossRef] [Green Version]
- Loverde, J.R.; Ozoka, V.C.; Aquino, R.; Lin, L.; Pfister, B.J. Live imaging of axon stretch growth in embryonic and adult neurons. J. Neurotrauma 2011, 28, 2389–2403. [Google Scholar] [CrossRef]
- Pfister, B.J.; Iwata, A.; Meaney, D.F.; Smith, D.H. Extreme stretch growth of integrated axons. J. Neurosci. 2004, 24, 7978–7983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szikszay, T.; Hall, T.; Von Piekartz, H. In vivo effects of limb movement on nerve stretch, strain, and tension: A systematic review. J. Back Musculoskelet. Rehabil. 2017, 30, 1171–1186. [Google Scholar] [CrossRef] [PubMed]
- Collier, A.; Burge, P. Ulnar Nerve At the Elbow. Curr. Orthop. 2001, 15, 256d263. [Google Scholar] [CrossRef]
- Hicks, D.; Toby, E.B. Ulnar nerve strains at the elbow: The effect of in Situ decompression and medial epicondylectomy. J. Hand Surg. Am. 2002, 27, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Byl, C.; Puttlitz, C.; Byl, N.; Lotz, J.; Topp, K. Strain in the median and ulnar nerves during upper-extremity positioning. J. Hand Surg. Am. 2002, 27, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.; Ramot, R.; Green, A. Changes in mechanical tension in the median nerve: Possible implications for the upper limb tension test. Physiotherapy 1998, 84, 254–261. [Google Scholar] [CrossRef]
- Manvell, N.; Manvell, J.J.; Snodgrass, S.J.; Reid, S.A. Tension of the Ulnar, Median, and Radial Nerves During Ulnar Nerve Neurodynamic Testing: Observational Cadaveric Study. Phys. Ther. 2015, 95, 891–900. [Google Scholar] [CrossRef] [Green Version]
- Alshami, A.M.; Babri, A.S.; Souvlis, T.; Coppieters, M.W. Strain in the tibial and plantar nerves with foot and ankle movements and the influence of adjacent joint positions. J. Appl. Biomech. 2008, 24, 368–376. [Google Scholar] [CrossRef]
- Kleinrensink, G.J.; Stoeckart, R.; Vleeming, A.; Snijders, C.J.; Mulder, P.G.H. Mechanical tension in the median nerve. Clin. Biomech. 1995, 10, 240–244. [Google Scholar] [CrossRef] [Green Version]
- Sunderland, S.; Bradley, K.C. Stress-strain phenomena in human peripheral nerve trunks. Brain 1961, 84, 102–119. [Google Scholar] [CrossRef]
- Babbage, C.S.; Coppieters, M.W.; McGowan, C.M. Strain and excursion of the sciatic nerve in the dog: Biomechanical considerations in the development of a clinical test for increased neural mechanosensitivity. Vet. J. 2007, 174, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Coppieters, M.W.; Alshami, A.M.; Babri, A.S.; Souvlis, T.; Kippers, V.; Hodges, P.W. Strain and Excursion of the Sciatic, Tibial, and Plantar Nerves during a Modified Straight Leg Raising Test. J. Orthop. Res. Sept. 2007, 25, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Higgins, S.; Lee, J.S.; Ha, L.; Lim, J.Y. Inducing neurite outgrowth by mechanical cell stretch. Biores. Open Access 2013, 2, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Fontana, F. Trait sur le Venim de le Vipere sur les Poisons Americains sur le Laurier-Cerise; Tome 2; Nyon: Florence, Italy, 1781. [Google Scholar]
- Haninec, P. Undulating course of nerve fibres and bands of Fontana in peripheral nerves of the rat. Anat. Embryol. 1986, 174, 407–411. [Google Scholar] [CrossRef]
- Alvey, L.M.; Jones, J.F.X.; Tobin-O’Brien, C.; Pickering, M. Bands of Fontana are caused exclusively by the sinusoidal path of axons in peripheral nerves and predict axon path; evidence from rodent nerves and physical models. J. Anat. 2019, 234, 165–178. [Google Scholar] [CrossRef]
- Med, J.B. Spiral Nerve Bands Of Fontana. Br. Med. J. 1972, 2, 671. [Google Scholar] [CrossRef] [Green Version]
- Ruscheweyh, R.; Forsthuber, L.; Schoffnegger, D.; Sandkühler, J. Modification of classical neurochemical markers in identified primary afferent neurons with Aβ-, Aδ-, and C-fibers after chronic constriction injury in mice. J. Comp. Neurol. 2007, 502, 325–336. [Google Scholar] [CrossRef]
- Lawson, B.Y.S.N.; Waddell, P.J. Soma neurofillament immunoreactivity is related to cell size and fibre conduction velocity in rat primary sensory neurons. J. Physiol. 1991, 435, 41–63. [Google Scholar] [CrossRef]
- Lechner, S.G.; Frenzel, H.; Wang, R.; Lewin, G.R. Developmental waves of mechanosensitivity acquisition in sensory neuron subtypes during embryonic development. EMBO J. 2009, 28, 1479–1491. [Google Scholar] [CrossRef]
- Usoskin, D.; Furlan, A.; Islam, S.; Abdo, H.; Lönnerberg, P.; Lou, D.; Hjerling-Leffler, J.; Haeggström, J.; Kharchenko, O.; Kharchenko, P.V.; et al. Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing. Nat. Neurosci. 2015, 18, 145–153. [Google Scholar] [CrossRef]
- Ernfors, P.; Lee, K.F.; Kucera, J.; Jaenisch, R. Lack of neurotrophin-3 leads to deficiencies in the peripheral nervous system and loss of limb proprioceptive afferents. Cell 1994, 77, 503–512. [Google Scholar] [CrossRef]
- Keller, A.V.; Hainline, C.; Rees, K.; Krupp, S.; Prince, D.; Wood, B.D.; Shum-Siu, A.; Burke, D.A.; Petruska, J.C.; Magnuson, D.S.K. Nociceptor-dependent locomotor dysfunction after clinically-modeled hindlimb muscle stretching in adult rats with spinal cord injury. Exp. Neurol. 2019, 318, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Mahan, M.A.; Warner, W.S.; Yeoh, S.; Light, A. Rapid-stretch injury to peripheral nerves: Implications from an animal model. J. Neurosurg. 2019, 133, 1285–1633. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Chakraborty, G.; Ingoglia, N.A. Post-translational modification of proteins by arginine and lysine following crush injury and during regeneration of rat sciatic nerves. Restor. Neurol. Neurosci. 1990, 2, 53–61. [Google Scholar] [CrossRef]
- Shin, J.E.; Cho, Y. Epigenetic regulation of axon regeneration after neural injury. Mol. Cells 2017, 40, 10–16. [Google Scholar] [CrossRef]
- Patodia, S.; Raivich, G. Role of transcription factors in peripheral nerve regeneration. Front. Mol. Neurosci. 2012, 5, 1–15. [Google Scholar] [CrossRef] [Green Version]
- van Kesteren, R.E.; Mason, M.R.J.; MacGillavry, H.D.; Smit, A.B.; Verhaagen, J. A Gene Network Perspective on Axonal Regeneration. Front. Mol. Neurosci. 2011, 4, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Gey, M.; Wanner, R.; Schilling, C.; Pedro, M.T.; Sinske, D.; Knöll, B. Atf3 mutant mice show reduced axon regeneration and impaired regeneration-associated gene induction after peripheral nerve injury. Open Biol. 2016, 6, 160091. [Google Scholar] [CrossRef] [Green Version]
- Tsujino, H.; Kondo, E.; Fukuoka, T.; Dai, Y.; Tokunaga, A.; Miki, K.; Yonenobu, K.; Ochi, T.; Noguchi, K. Activating transcription factor 3 (ATF3) induction by axotomy in sensory and motoneurons: A novel neuronal marker of nerve injury. Mol. Cell. Neurosci. 2000, 15, 170–182. [Google Scholar] [CrossRef]
- Seijffers, R.; Mills, C.D.; Woolf, C.J. ATF3 increases the intrinsic growth state of DRG neurons to enhance peripheral nerve regeneration. J. Neurosci. 2007, 27, 7911–7920. [Google Scholar] [CrossRef] [Green Version]
- Koivisto, E.; Jurado Acosta, A.; Moilanen, A.M.; Tokola, H.; Aro, J.; Pennanen, H.; Säkkinen, H.; Kaikkonen, L.; Ruskoaho, H.; Rysä, J. Characterization of the regulatory mechanisms of activating transcription factor 3 by hypertrophic stimuli in rat cardiomyocytes. PLoS ONE 2014, 9, e105168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puttagunta, R.; Tedeschi, A.; Sória, M.G.; Hervera, A.; Lindner, R.; Rathore, K.I.; Gaub, P.; Joshi, Y.; Nguyen, T.; Schmandke, A.; et al. PCAF-dependent epigenetic changes promote axonal regeneration in the central nervous system. Nat. Commun. 2014, 5, 3527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmisano, I.; Danzi, M.C.; Hutson, T.H.; Zhou, L.; McLachlan, E.; Serger, E.; Shkura, K.; Srivastava, P.K.; Hervera, A.; Neill, N.O.; et al. Epigenomic signatures underpin the axonal regenerative ability of dorsal root ganglia sensory neurons. Nat. Neurosci. 2019, 22, 1913–1924. [Google Scholar] [CrossRef] [PubMed]
- Gaub, P.; Tedeschi, A.; Puttagunta, R.; Nguyen, T.; Schmandke, A.; Di Giovanni, S. HDAC inhibition promotes neuronal outgrowth and counteracts growth cone collapse through CBP/p300 and P/CAF-dependent p53 acetylation. Cell Death Differ. 2010. [Google Scholar] [CrossRef] [Green Version]
- Hutson, T.H.; Kathe, C.; Palmisano, I.; Bartholdi, K.; Hervera, A.; De Virgiliis, F.; McLachlan, E.; Zhou, L.; Kong, G.; Barraud, Q.; et al. Cbp-dependent histone acetylation mediates axon regeneration induced by environmental enrichment in rodent spinal cord injury models. Sci. Transl. Med. 2019, 11, eaaw2064. [Google Scholar] [CrossRef] [Green Version]
- Gilmour, D.; Knaut, H.; Maischein, H.M.; Nüsslein-Volhard, C. Towing of sensory axons by their migrating target cells in vivo. Nat. Neurosci. 2004, 7, 491–492. [Google Scholar] [CrossRef]
- Franze, K. Atomic force microscopy and its contribution to understanding the development of the nervous system. Curr. Opin. Genet. Dev. 2011, 21, 530–537. [Google Scholar] [CrossRef]
- Paulus, J.D.; Willer, G.B.; Willer, J.R.; Gregg, R.G.; Halloran, M.C. Muscle contractions guide Rohon-Beard peripheral sensory axons. J. Neurosci. 2009, 29, 13190–13201. [Google Scholar] [CrossRef] [Green Version]
- Siechen, S.; Yang, S.; Chiba, A.; Saif, T. Mechanical tension contributes to clustering of neurotransmitter vesicles at presynaptic terminals. Proc. Natl. Acad. Sci. USA 2009, 106, 12611–12616. [Google Scholar] [CrossRef] [Green Version]
- Sandrow-Feinberg, H.R.; Houlé, J.D. Exercise after spinal cord injury as an agent for neuroprotection, regeneration and rehabilitation. Brain Res. 2015, 1619, 12–21. [Google Scholar] [CrossRef] [Green Version]
- Armada-da-silva, P.A.S.; Pereira, C.; Amado, S. Role of Physical Exercise for Improving Posttraumatic Nerve Regeneration. Int. Rev. Neurobiol. 2013, 109, 125–149. [Google Scholar] [CrossRef]
- Molteni, R.; Zheng, J.Q.; Ying, Z.; Gómez-Pinilla, F.; Twiss, J.L. Voluntary exercise increases axonal regeneration from sensory neurons. Proc. Natl. Acad. Sci. USA 2004, 101, 8473–8478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Udina, E.; Puigdemasa, A.; Navarro, X. Passive and active exercise improve regeneration and muscle reinnervation after peripheral nerve injury in the rat. Muscle Nerve 2011, 43, 500–509. [Google Scholar] [CrossRef] [PubMed]
- Pachter, B.R.; Eberstein, A. Passive exercise and reinnervation of the rat denervated extensor digitorum longus muscle after nerve crush. Am. J. Phys. Med. Rehabil. 1989, 68, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Bendella, H.; Pavlov, S.P.; Grosheva, M.; Irintchev, A.; Angelova, S.K.; Merkel, D.; Sinis, N.; Kaidoglou, K.; Skouras, E.; Dunlop, S.A.; et al. Non-invasive stimulation of the vibrissal pad improves recovery of whisking function after simultaneous lesion of the facial and infraorbital nerves in rats. Exp. Brain Res. 2011, 212, 65–79. [Google Scholar] [CrossRef]
- English, A.W.; Wilhelm, J.C.; Sabatier, M.J. Enhancing recovery from peripheral nerve injury using treadmill training. Ann. Anat. 2011, 193, 354–361. [Google Scholar] [CrossRef] [Green Version]
- Chang, Y.J.; Tsai, C.J.; Tseng, F.G.; Chen, T.J.; Wang, T.W. Micropatterned stretching system for the investigation of mechanical tension on neural stem cells behavior. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 345–355. [Google Scholar] [CrossRef]
- Hutchinson, K.J.; Gómez-Pinilla, F.; Crowe, M.J.; Ying, Z.; Basso, D.M. Three exercise paradigms differentially improve sensory recovery after spinal cord contusion in rats. Brain 2004, 127, 1403–1414. [Google Scholar] [CrossRef] [Green Version]
- Goldshmit, Y.; Lythgo, N.; Galea, M.P.; Turnley, A.M. Treadmill training after spinal cord hemisection in mice promotes axonal sprouting and synapse formation and improves motor recovery. J. Neurotrauma 2008, 25, 449–465. [Google Scholar] [CrossRef]
- Gómez-Pinilla, F.; Ying, Z.; Roy, R.R.; Molteni, R.; Reggie Edgerton, V. Voluntary exercise induces a BDNF-mediated mechanism that promotes neuroplasticity. J. Neurophysiol. 2002, 88, 2187–2195. [Google Scholar] [CrossRef] [Green Version]
- Sachdeva, R.; Theisen, C.C.; Ninan, V.; Twiss, J.L.; Houlé, J.D. Exercise dependent increase in axon regeneration into peripheral nerve grafts by propriospinal but not sensory neurons after spinal cord injury is associated with modulation of regeneration-associated genes. Exp. Neurol. 2016, 276, 72–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanslik, K.L.; Allen, S.R.; Harkenrider, T.L.; Fogerson, S.M.; Guadarrama, E.; Morgan, J.R. Regenerative capacity in the lamprey spinal cord is not altered after a repeated transection. PLoS ONE 2019, 14, e0204193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doyle, L.M.F.; Roberts, B.L. Exercise enhances axonal growth and functional recovery in the regenerating spinal cord. Neuroscience 2006, 141, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Luna, C.; Detrick, L.; Shah, S.B.; Cohen, A.H.; Aranda-espinoza, H. Mechanical properties of the lamprey spinal cord: Uniaxial loading and physiological strain. J. Biomech. 2013, 46, 2194–2200. [Google Scholar] [CrossRef]
- Zhang, G.; Rodemer, W.; Sinitsa, I.; Hu, J.; Selzer, M.E. Source of Early Regenerating Axons in Lamprey Spinal Cord Revealed by Wholemount Optical Clearing with BABB. Cells 2020, 9, 2427. [Google Scholar] [CrossRef]
- Assas, B.M.; Pennock, J.I.; Miyan, J.A. Calcitonin gene-related peptide is a key neurotransmitter in the neuro-immune axis. Front. Neurosci. 2014, 8, 23. [Google Scholar] [CrossRef] [Green Version]
- Gladman, S.J.; Ward, R.E.; Michael-titus, A.T. The effect of mechanical strain or hypoxia on cell death in subpopulations of rat dorsal root ganglion neurons in vitro. Neuroscience 2010, 171, 577–587. [Google Scholar] [CrossRef]
- Berkelaar, M.; Clarke, D.B.; Wang, Y.C.; Bray, G.M.; Aguayo, A.J. Axotomy results in delayed death and apoptosis of retinal ganglion cells in adult rats. J. Neurosci. 1994, 14, 4368–4374. [Google Scholar] [CrossRef] [Green Version]
- Steketee, M.B.; Oboudiyat, C.; Daneman, R.; Trakhtenberg, E.; Lamoureux, P.; Weinstein, J.E.; Heidemann, S.; Barres, B.A.; Goldberg, J.L. Regulation of intrinsic axon growth ability at retinal ganglion cell growth cones. Investig. Ophthalmol. Vis. Sci. 2014, 55, 4369–4377. [Google Scholar] [CrossRef] [Green Version]
- Xia, J.; Lim, J.C.; Lu, W.; Beckel, J.M.; Macarak, E.J.; Laties, A.M.; Mitchell, C.H. Neurons respond directly to mechanical deformation with pannexin-mediated ATP release and autostimulation of P2X7 receptors. J. Physiol. 2012, 590, 2285–2304. [Google Scholar] [CrossRef] [Green Version]
- Lim, J.C.; Lu, W.; Beckel, J.M.; Mitchell, C.H.; Fornai, F.; Ceruti, S. Neuronal Release of Cytokine IL-3 Triggered by Mechanosensitive Autostimulation of the P2X7 Receptor Is Neuroprotective. Front. Cell. Neurosci. 2016. [Google Scholar] [CrossRef] [PubMed]
- Kerns, J.; Piponov, H.; Helder, C.; Amirouche, F.; Solitro, G.; Gonzalez, M. Mechanical Properties of the Human Tibial and Peroneal Nerves Following Stretch with Histological Correlations. Anat. Rec. 2019, 302, 2030–2039. [Google Scholar] [CrossRef] [PubMed]
- Vogl, A.W.; Lillie, M.A.; Piscitelli, M.A.; Goldbogen, J.A.; Pyenson, N.D.; Shadwick, R.E. Stretchy nerves are an essential component of the extreme feeding mechanism of rorqual whales. Curr. Biol. 2015, 25, R360–R361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry, M.J.; Lawson, S.N.; Robertson, J. Neurofilament immunoreactivity in populations of rat primary afferent neurons: A quantitative study of phosphorylated and non-phosphorylated subunits. J. Neurocytol. 1991, 20, 746–758. [Google Scholar] [CrossRef]
- Kim, J.E.; Cho, Y.H.; Seo, T.B. Treadmill exercise activates ATF3 and ERK1/2 downstream molecules to facilitate axonal regrowth after sciatic nerve injury. J. Exerc. Rehabil. 2020, 16, 141–147. [Google Scholar] [CrossRef]
- Birukov, K.G. Cyclic stretch, reactive oxygen species, and vascular remodeling. Antioxid. Redox Signal. 2009, 11, 1651–1667. [Google Scholar] [CrossRef] [Green Version]
- Nichols, E.L.; Smith, C.J. Synaptic-like Vesicles Facilitate Pioneer Axon Invasion. Curr. Biol. 2019, 29, 2652–2664. [Google Scholar] [CrossRef]
- Nichols, E.L.; Smith, C.J. Functional Regeneration of the Sensory Root via Axonal Invasion. Cell Rep. 2020, 30, 9–17. [Google Scholar] [CrossRef] [Green Version]
- Hamzeh, M.T.; Sridhara, R.; Alexander, L.D. Cyclic stretch-induced TGF-β1 and fibronectin expression is mediated by β1-integrin through c-Src- and STAT3-dependent pathways in renal epithelial cells. Am. J. Physiol. Physiol. 2015, 308, F425–F436. [Google Scholar] [CrossRef] [Green Version]
- Lodyga, M.; Bai, X.-H.; Mourgeon, E.; Han, B.; Keshavjee, S.; Liu, M. Molecular cloning of actin filament-associated protein: A putative adaptor in stretch-induced Src activation. Am. J. Physiol. Cell. Mol. Physiol. 2002, 283, L265–L274. [Google Scholar] [CrossRef] [Green Version]
- Pizzi, M.A.; Crowe, M.J. Matrix metalloproteinases and proteoglycans in axonal regeneration. Exp. Neurol. 2007, 204, 496–511. [Google Scholar] [CrossRef] [PubMed]
- Zuo, J.; Neubauer, D.; Dyess, K.; Ferguson, T.A.; Muir, D. Degradation of chondroitin sulfate proteoglycan enhances the neurite- promoting potential of spinal cord tissue. Exp. Neurol. 1998, 154, 654–662. [Google Scholar] [CrossRef] [PubMed]
- Pastrana, E.; Moreno-Flores, M.T.; Gurzov, E.N.; Avila, J.; Wandosell, F.; Diaz-Nido, J. Genes associated with adult axon regeneration promoted by olfactory ensheathing cells: A new role for matrix metalloproteinase 2. J. Neurosci. 2006, 26, 5347–5359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, Z.; Dent, R.G.; Leadbeater, W.E.; Smith, C.; Berry, M.; Logan, A. Matrix metalloproteases: Degradation of the inhibitory environment of the transected optic nerve and the scar by regenerating axons. Mol. Cell. Neurosci. 2005, 28, 64–78. [Google Scholar] [CrossRef]
- Haseneen, N.A.; Vaday, G.G.; Zucker, S.; Foda, H.D. Mechanical stretch induces MMP-2 release and activation in lung endothelium: Role of EMMPRIN. Am. J. Physiol. Lung Cell. Mol. Physiol. 2003, 284, 541–547. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Xu, G.; Fan, J.; Zhang, M. Mechanical stretching induces matrix metalloproteinase-2 expression in rat retinal glial (Müller) cells. Neuroreport 2013, 24, 224–228. [Google Scholar] [CrossRef]
- Udina, E.; Cobianchi, S.; Allodi, I.; Navarro, X. Effects of activity-dependent strategies on regeneration and plasticity after peripheral nerve injuries. Ann. Anat. 2011, 193, 347–353. [Google Scholar] [CrossRef]
- English, A.W.; Meador, W.; Carrasco, D.I. Neurotrophin-4/5 is required for the early growth of regenerating axons in peripheral nerves. Eur. J. Neurosci. 2005, 21, 2624–2634. [Google Scholar] [CrossRef]
- Martino, F.; Perestrelo, A.R.; Vinarský, V.; Pagliari, S.; Forte, G. Cellular mechanotransduction: From tension to function. Front. Physiol. 2018, 9, 1–21. [Google Scholar] [CrossRef]
- Nieuwenhuis, B.; Haenzi, B.; Andrews, M.R.; Verhaagen, J.; Fawcett, J.W. Integrins promote axonal regeneration after injury of the nervous system. Biol. Rev. 2018, 93, 1339–1362. [Google Scholar] [CrossRef]
- Kerstein, P.C.; Jacques-Fricke, B.T.; Rengifo, J.; Mogen, B.J.; Williams, J.C.; Gottlieb, P.A.; Sachs, F.; Gomez, T.M. Mechanosensitive TRPC1 channels promote calpain proteolysis of talin to regulate spinal axon outgrowth. J. Neurosci. 2013, 33, 273–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shibasaki, K.; Murayama, N.; Ono, K.; Ishizaki, Y.; Tominaga, M. TRPV2 enhances axon outgrowth through its activation by membrane stretch in developing sensory and motor neurons. J. Neurosci. 2010, 30, 4601–4612. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| % Stretch, Frequency (Hz) | Time of Stretch (h) | Recovery Time (h) |
|---|---|---|
| 2.5%, 0.5 Hz | 3 h | 0 h |
| 5%, 0.5 Hz | 6 h | 0 h |
| 5%, 0.5 Hz | 3 h | 3 h |
| 5%, 0.5 Hz | 3 h | 0 h |
| 10%, 0.25 Hz | 3 h | 0 h |
| 10%, 0.5 Hz | 3 h | 0 h |
| 20%, 0.25 Hz | 3 h | 0 h |
| 20%, 0.5 Hz | 3 h | 0 h |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kampanis, V.; Tolou-Dabbaghian, B.; Zhou, L.; Roth, W.; Puttagunta, R. Cyclic Stretch of Either PNS or CNS Located Nerves Can Stimulate Neurite Outgrowth. Cells 2021, 10, 32. https://doi.org/10.3390/cells10010032
Kampanis V, Tolou-Dabbaghian B, Zhou L, Roth W, Puttagunta R. Cyclic Stretch of Either PNS or CNS Located Nerves Can Stimulate Neurite Outgrowth. Cells. 2021; 10(1):32. https://doi.org/10.3390/cells10010032
Chicago/Turabian StyleKampanis, Vasileios, Bahardokht Tolou-Dabbaghian, Luming Zhou, Wolfgang Roth, and Radhika Puttagunta. 2021. "Cyclic Stretch of Either PNS or CNS Located Nerves Can Stimulate Neurite Outgrowth" Cells 10, no. 1: 32. https://doi.org/10.3390/cells10010032
APA StyleKampanis, V., Tolou-Dabbaghian, B., Zhou, L., Roth, W., & Puttagunta, R. (2021). Cyclic Stretch of Either PNS or CNS Located Nerves Can Stimulate Neurite Outgrowth. Cells, 10(1), 32. https://doi.org/10.3390/cells10010032






