ERK: A Double-Edged Sword in Cancer. ERK-Dependent Apoptosis as a Potential Therapeutic Strategy for Cancer
Abstract
1. Introduction
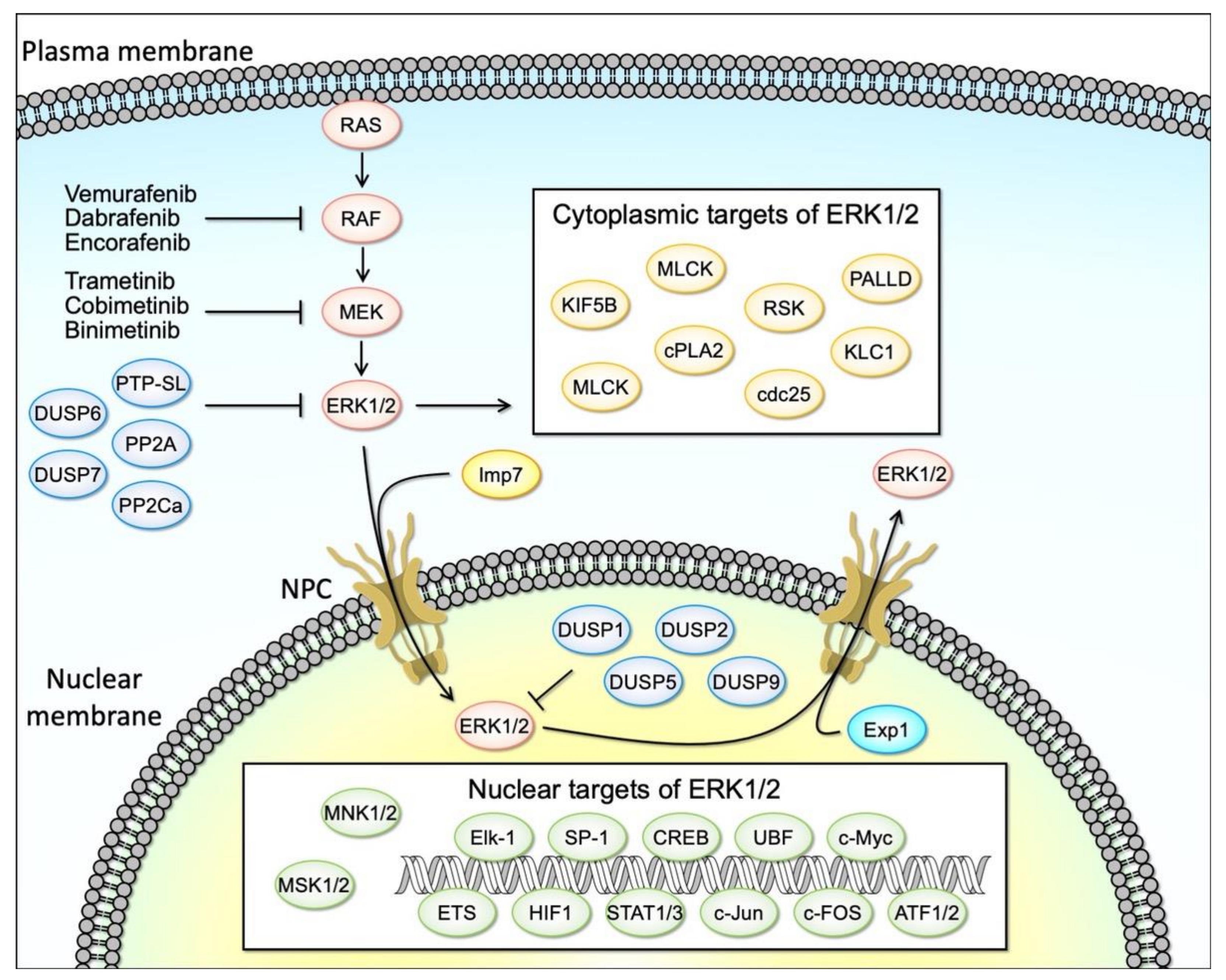
2. Overview of the RAS/RAF/MEK/ERK1/2 Signaling Pathway
3. Targeting the Oncogenic Activation of the RAS/RAF/MEK/ERK Signaling for Cancer Therapy
3.1. Roles of ERK Signaling in Proliferation and Survival
3.2. Roles of ERK Signaling in Tumor Development
3.3. Oncogenic Activation of ERK1/2 in Human Cancers
3.4. Anticancer Agents Targeting the ERK Cascade
4. Role for the ERK Cascade in Apoptosis
4.1. Compounds/Stimuli That Induce Apoptosis through ERK Activation
4.2. Mechanisms of ERK-Induced Apoptosis
4.3. DNA Damage and p53 in the ERK Activation-Induced Apoptosis
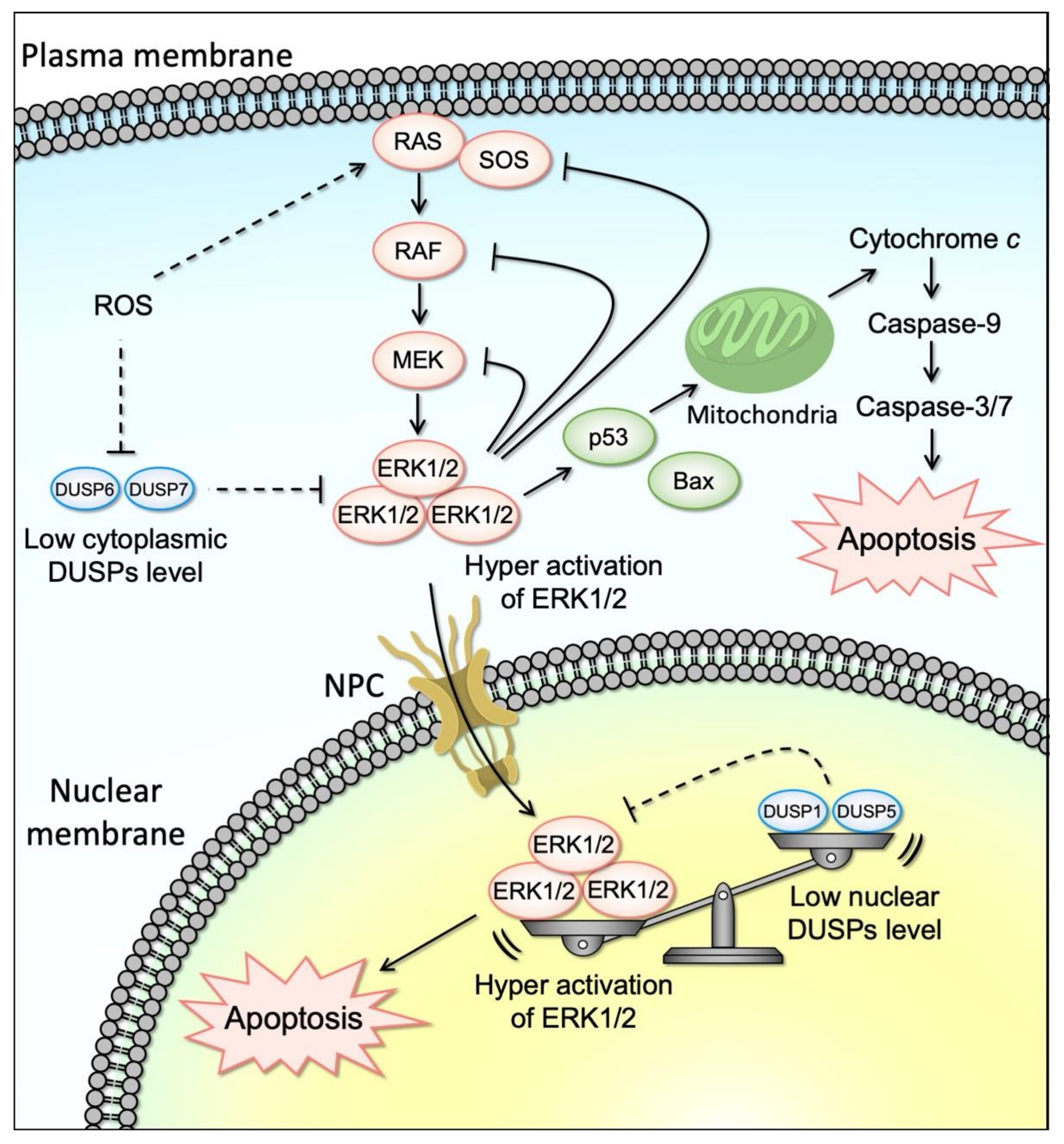
4.4. ROS and ERK Activation-Induced Cell Death
4.5. DUSP and Negative Regulators of the ERK Cascade in the ERK Activation-Induced Cell Death
4.6. Kinetics and Distribution of Phosphorylated ERK and Cell Death
4.7. The Cellular Threshold for ERK-Dependent Cell Death
4.8. ERK Activation and Other Types of Cell Death
5. Conclusions and Perspectives: Promises and Challenges for ERK-Induced Apoptosis in Cancer
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Santarpia, L.; Lippman, S.M.; El-Naggar, A.K. Targeting the MAPK–RAS–RAF Signaling Pathway in Cancer Therapy. Expert Opin. Ther. Target 2012, 16, 103–119. [Google Scholar] [CrossRef]
- Beeram, M.; Patnaik, A.; Rowinsky, E.K. Raf: A Strategic Target for Therapeutic Development Against Cancer. J. Clin. Oncol. 2005, 23, 6771–6790. [Google Scholar] [CrossRef] [PubMed]
- Braicu, C.; Buse, M.; Busuioc, C.; Drula, R.; Gulei, D.; Raduly, L.; Rusu, A.; Irimie, A.; Atanasov, A.G.; Slaby, O.; et al. A Comprehensive Review on MAPK: A Promising Therapeutic Target in Cancer. Cancers 2019, 11, 1618. [Google Scholar] [CrossRef]
- Stern, D.F. Keeping Tumors Out of the MAPK Fitness Zone. Cancer Discov. 2018, 8, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Yaeger, R.; Corcoran, R.B. Targeting Alterations in the RAF–MEK Pathway. Cancer Discov. 2019, 9, 329–341. [Google Scholar] [CrossRef] [PubMed]
- Kidger, A.M.; Sipthorp, J.; Cook, S.J. ERK1/2 Inhibitors: New Weapons to Inhibit the RAS-Regulated RAF-MEK1/2-ERK1/2 Pathway. Pharmacol. Therapeut. 2018, 187, 45–60. [Google Scholar] [CrossRef]
- Samatar, A.A.; Poulikakos, P.I. Targeting RAS–ERK Signalling in Cancer: Promises and Challenges. Nat. Rev. Drug Discov. 2014, 13, 928–942. [Google Scholar] [CrossRef]
- Wu, P.-K.; Park, J.-I. MEK1/2 Inhibitors: Molecular Activity and Resistance Mechanisms. Semin. Oncol. 2015, 42, 849–862. [Google Scholar] [CrossRef]
- Tate, J.G.; Bamford, S.; Jubb, H.C.; Sondka, Z.; Beare, D.M.; Bindal, N.; Boutselakis, H.; Cole, C.G.; Creatore, C.; Dawson, E.; et al. COSMIC: The Catalogue Of Somatic Mutations In Cancer. Nucleic Acids Res. 2018, 47, D941–D947. [Google Scholar] [CrossRef]
- Davies, H.; Bignell, G.R.; Cox, C.; Stephens, P.; Edkins, S.; Clegg, S.; Teague, J.; Woffendin, H.; Garnett, M.J.; Bottomley, W.; et al. Mutations of the BRAF Gene in Human Cancer. Nature 2002, 417, 949–954. [Google Scholar] [CrossRef]
- Burotto, M.; Chiou, V.L.; Lee, J.; Kohn, E.C. The MAPK Pathway across Different Malignancies: A New Perspective. Cancer 2014, 120, 3446–3456. [Google Scholar] [CrossRef]
- Zhuang, S.; Schnellmann, R.G. A Death-Promoting Role for Extracellular Signal-Regulated Kinase. J. Pharmacol. Exp. Ther. 2006, 319, 991–997. [Google Scholar] [CrossRef]
- Cagnol, S.; Chambard, J. ERK and Cell Death: Mechanisms of ERK-induced Cell Death—Apoptosis, Autophagy and Senescence. FEBS J. 2010, 277, 2–21. [Google Scholar] [CrossRef]
- Rieber, M.; Rieber, M.S. Signalling Responses Linked to Betulinic Acid-Induced Apoptosis Are Antagonized by MEK Inhibitor U0126 in Adherent or 3D Spheroid Melanoma Irrespective of P53 Status. Int. J. Cancer 2006, 118, 1135–1143. [Google Scholar] [CrossRef]
- Kim, Y.-H.; Lee, D.-H.; Jeong, J.-H.; Guo, Z.S.; Lee, Y.J. Quercetin Augments TRAIL-Induced Apoptotic Death: Involvement of the ERK Signal Transduction Pathway. Biochem. Pharmacol. 2008, 75, 1946–1958. [Google Scholar] [CrossRef]
- Randhawa, H.; Kibble, K.; Zeng, H.; Moyer, M.P.; Reindl, K.M. Activation of ERK Signaling and Induction of Colon Cancer Cell Death by Piperlongumine. Toxicol. In Vitro 2013, 27, 1626–1633. [Google Scholar] [CrossRef]
- Lee, E.-R.; Kang, Y.-J.; Kim, J.-H.; Lee, H.T.; Cho, S.-G. Modulation of Apoptosis in HaCaT Keratinocytes via Differential Regulation of ERK Signaling Pathway by Flavonoids. J. Biological. Chem. 2005, 280, 31498–31507. [Google Scholar] [CrossRef][Green Version]
- Radaszkiewicz, K.A.; Beckerová, D.; Woloszczuková, L.; Radaszkiewicz, T.W.; Lesáková, P.; Blanářová, O.V.; Kubala, L.; Humpolíček, P.; Pachernik, J. 12-O-Tetradecanoylphorbol-13-Acetate Increases Cardiomyogenesis through PKC/ERK Signaling. Sci. Rep.-UK 2020, 10, 15922. [Google Scholar] [CrossRef]
- Lee, K.-I.; Su, C.-C.; Yang, C.-Y.; Hung, D.-Z.; Lin, C.-T.; Lu, T.-H.; Liu, S.-H.; Huang, C.-F. Etoposide Induces Pancreatic β-Cells Cytotoxicity via the JNK/ERK/GSK-3 Signaling-Mediated Mitochondria-Dependent Apoptosis Pathway. Toxicol. In Vitro 2016, 36, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Kumari, R.; Chouhan, S.; Singh, S.; Chhipa, R.R.; Ajay, A.K.; Bhat, M.K. Constitutively Activated ERK Sensitizes Cancer Cells to Doxorubicin: Involvement of P53-EGFR-ERK Pathway. J. Biosci. 2017, 42, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Woessmann, W.; Chen, X.; Borkhardt, A. Ras-Mediated Activation of ERK by Cisplatin Induces Cell Death Independently of P53 in Osteosarcoma and Neuroblastoma Cell Lines. Cancer Chemoth. Pharm. 2002, 50, 397–404. [Google Scholar] [CrossRef]
- Martin, P.; Pognonec, P. ERK and Cell Death: Cadmium Toxicity, Sustained ERK Activation and Cell Death. FEBS J. 2010, 277, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.-S.; Zhang, Q.-H.; Huang, X.; Fu, X.-Q.; Qi, S.-T.; Wang, Y.-P.; Hou, Y.; Sheng, J.; Sun, Q.-Y. Icaritin Causes Sustained ERK1/2 Activation and Induces Apoptosis in Human Endometrial Cancer Cells. PLoS ONE 2011, 6, e16781. [Google Scholar] [CrossRef]
- Hong, S.-K.; Wu, P.-K.; Park, J.-I. A Cellular Threshold for Active ERK1/2 Levels Determines Raf/MEK/ERK-Mediated Growth Arrest versus Death Responses. Cell Signal. 2018, 42, 11–20. [Google Scholar] [CrossRef]
- Satoh, R.; Hamada, N.; Yamada, A.; Kanda, Y.; Ishikawa, F.; Takasaki, T.; Tanabe, G.; Sugiura, R. Discovery of New Benzhydrol Biscarbonate Esters as Potent and Selective Apoptosis Inducers of Human Melanomas Bearing the Activated ERK Pathway: SAR Studies on an ERK MAPK Signaling Modulator, ACA-28. Bioorg. Chem. 2020, 103, 104137. [Google Scholar] [CrossRef] [PubMed]
- Satoh, R.; Hagihara, K.; Matsuura, K.; Manse, Y.; Kita, A.; Kunoh, T.; Masuko, T.; Moriyama, M.; Moriyama, H.; Tanabe, G.; et al. Identification of ACA-28, a 1’-acetoxychavicol Acetate Analogue Compound, as a Novel Modulator of ERK MAPK Signaling, Which Preferentially Kills Human Melanoma Cells. Genes Cells 2017, 22, 608–618. [Google Scholar] [CrossRef]
- Kanda, Y.; Mizuno, A.; Takasaki, T.; Satoh, R.; Hagihara, K.; Masuko, T.; Endo, Y.; Tanabe, G.; Sugiura, R. Downregulation of DUSP6, a Negative Regulator of Oncogenic ERK Signaling, by ACA-28 Induces Apoptosis in NIH/3T3 Cells Overexpressing HER2/ErbB2. Genes Cells Devoted Mol. Cell Mech. 2020, 26, 109–116. [Google Scholar] [CrossRef]
- Lavoie, H.; Gagnon, J.; Therrien, M. ERK Signalling: A Master Regulator of Cell Behaviour, Life and Fate. Nat. Rev. Mol. Cell Biol. 2020, 21, 607–632. [Google Scholar] [CrossRef]
- Guo, Y.-J.; Pan, W.-W.; Liu, S.-B.; Shen, Z.-F.; Xu, Y.; Hu, L.-L. ERK/MAPK Signalling Pathway and Tumorigenesis. Exp. Ther. Med. 2020, 19, 1997–2007. [Google Scholar] [CrossRef]
- Roskoski, R. ERK1/2 MAP Kinases: Structure, Function, and Regulation. Pharmacol. Res. 2012, 66, 105–143. [Google Scholar] [CrossRef]
- Balmanno, K.; Cook, S.J. Tumour Cell Survival Signalling by the ERK1/2 Pathway. Cell Death Differ. 2009, 16, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Kohno, M.; Pouyssegur, J. Targeting the ERK Signaling Pathway in Cancer Therapy. Ann. Med. 2006, 38, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Degirmenci, U.; Wang, M.; Hu, J. Targeting Aberrant RAS/RAF/MEK/ERK Signaling for Cancer Therapy. Cells 2020, 9, 198. [Google Scholar] [CrossRef]
- Cargnello, M.; Roux, P.P. Activation and Function of the MAPKs and Their Substrates, the MAPK-Activated Protein Kinases. Microbiol. Mol. Biol. Rev. 2011, 75, 50–83. [Google Scholar] [CrossRef]
- Ng, D.C.H.; Bogoyevitch, M.A. The Mechanism of Heat Shock Activation of ERK Mitogen-Activated Protein Kinases in the Interleukin 3-Dependent ProB Cell Line BaF3. J. Biol. Chem. 2000, 275, 40856–40866. [Google Scholar] [CrossRef]
- Harris, D.; Bonfil, D.; CHuderland, D.; Kraus, S.; Seger, R.; Naor, Z. Activation of MAPK Cascades by GnRH: ERK and Jun N-Terminal Kinase Are Involved in Basal and GnRH-Stimulated Activity of the Glycoprotein Hormone LHβ-Subunit Promoter. Endocrinology 2002, 143, 1018–1025. [Google Scholar] [CrossRef]
- Tan, B.-J.; Chiu, G.N.C. Role of Oxidative Stress, Endoplasmic Reticulum Stress and ERK Activation in Triptolide-Induced Apoptosis. Int. J. Oncol. 2013, 42, 1605–1612. [Google Scholar] [CrossRef]
- Saud, K.; Herrera-Molina, R.; Bernhardi, R.V. Pro- and Anti-Inflammatory Cytokines Regulate the ERK Pathway: Implication of the Timing for the Activation of Microglial Cells. Neurotox. Res. 2005, 8, 277–287. [Google Scholar] [CrossRef]
- Rubinfeld, H.; Seger, R. The ERK Cascade: A Prototype of MAPK Signaling. Mol. Biotechnol. 2005, 31, 151–174. [Google Scholar] [CrossRef]
- Endo, T. Dominant-Negative Antagonists of the Ras–ERK Pathway: DA-Raf and Its Related Proteins Generated by Alternative Splicing of Raf. Exp. Cell Res. 2020, 387, 111775. [Google Scholar] [CrossRef]
- Wang, C.; Fung, G.; Deng, H.; Jagdeo, J.; Mohamud, Y.; Xue, Y.C.; Jan, E.; Hirota, J.A.; Luo, H. NLRP3 Deficiency Exacerbates Enterovirus Infection in Mice. FASEB J. 2019, 33, 942–952. [Google Scholar] [CrossRef] [PubMed]
- Wortzel, I.; Maik-Rachline, G.; Yadav, S.S.; Hanoch, T.; Seger, R. Mitotic HOOK3 Phosphorylation by ERK1c Drives Microtubule-Dependent Golgi Destabilization and Fragmentation. Iscience 2021, 24, 102670. [Google Scholar] [CrossRef]
- Hauge, C.; Frödin, M. RSK and MSK in MAP Kinase Signalling. J. Cell Sci. 2006, 119, 3021–3023. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Liu, H.T. MAPK Signal Pathways in the Regulation of Cell Proliferation in Mammalian Cells. Cell Res. 2002, 12, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Chambard, J.-C.; Lefloch, R.; Pouysségur, J.; Lenormand, P. ERK Implication in Cell Cycle Regulation. Biochim. Et Biophys. Acta Bba-Mol. Cell Res. 2007, 1773, 1299–1310. [Google Scholar] [CrossRef]
- Yang, L.; Zheng, L.; Chng, W.J.; Ding, J.L. Comprehensive Analysis of ERK1/2 Substrates for Potential Combination Immunotherapies. Trends Pharmacol. Sci. 2019, 40, 897–910. [Google Scholar] [CrossRef]
- Casar, B.; Crespo, P. ERK Signals: Scaffolding Scaffolds? Front. Cell Dev. Biol. 2016, 4, 49. [Google Scholar] [CrossRef]
- Whitmarsh, A.J.; Davis, R.J. Signal Transduction by MAP Kinases: Regulation by Phosphorylation-Dependent Switches. Sci. Signal. 1999, 1999, pe1. [Google Scholar] [CrossRef]
- Mandl, M.; Slack, D.N.; Keyse, S.M. Specific Inactivation and Nuclear Anchoring of Extracellular Signal-Regulated Kinase 2 by the Inducible Dual-Specificity Protein Phosphatase DUSP5. Mol. Cell Biol. 2005, 25, 1830–1845. [Google Scholar] [CrossRef]
- Karlsson, M.; Mathers, J.; Dickinson, R.J.; Mandl, M.; Keyse, S.M. Both Nuclear-Cytoplasmic Shuttling of the Dual Specificity Phosphatase MKP-3 and Its Ability to Anchor MAP Kinase in the Cytoplasm Are Mediated by a Conserved Nuclear Export Signal. J. Biol. Chem. 2004, 279, 41882–41891. [Google Scholar] [CrossRef]
- Ekerot, M.; Stavridis, M.P.; Delavaine, L.; Mitchell, M.P.; Staples, C.; Owens, D.M.; Keenan, I.D.; Dickinson, R.J.; Storey, K.G.; Keyse, S.M. Negative-Feedback Regulation of FGF Signalling by DUSP6/MKP-3 Is Driven by ERK1/2 and Mediated by Ets Factor Binding to a Conserved Site within the DUSP6/MKP-3 Gene Promoter. Biochem. J. 2008, 412, 287–298. [Google Scholar] [CrossRef]
- Furukawa, T.; Tanji, E.; Xu, S.; Horii, A. Feedback Regulation of DUSP6 Transcription Responding to MAPK1 via ETS2 in Human Cells. Biochem. Biophys. Res. Commun. 2008, 377, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Brondello, J.-M.; Pouysségur, J.; McKenzie, F.R. Reduced MAP Kinase Phosphatase-1 Degradation After P42/P44MAPK-Dependent Phosphorylation. Science 1999, 286, 2514–2517. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-W.; Yang, J.-L. Cooperation of ERK and SCFSkp2 for MKP-1 Destruction Provides a Positive Feedback Regulation of Proliferating Signaling. J. Biol. Chem. 2006, 281, 915–926. [Google Scholar] [CrossRef] [PubMed]
- Lake, D.; Corrêa, S.A.L.; Müller, J. Negative Feedback Regulation of the ERK1/2 MAPK Pathway. Cell Mol. Life Sci. 2016, 73, 4397–4413. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. The Hallmarks of Cancer. Cell 2000, 100, 57–70. [Google Scholar] [CrossRef]
- Elmore, S. Apoptosis: A Review of Programmed Cell Death. Toxicol. Pathol. 2007, 35, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.C.; Cullen, S.P.; Martin, S.J. Apoptosis: Controlled Demolition at the Cellular Level. Nat. Rev. Mol. Cell Biol. 2008, 9, 231–241. [Google Scholar] [CrossRef]
- Sankari, S.L.; Babu, N.A.; Rajesh, E.; Kasthuri, M. Apoptosis in Immune-Mediated Diseases. J. Pharm. Bioallied Sci. 2015, 7, S200–S202. [Google Scholar] [CrossRef]
- Mattson, M.P. Apoptosis in Neurodegenerative Disorders. Nat. Rev. Mol. Cell Biol. 2000, 1, 120–130. [Google Scholar] [CrossRef]
- Reed, J.C. Dysregulation of Apoptosis in Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 1999, 17, 2941–2953. [Google Scholar] [CrossRef]
- Hongmei, Z.; Tobias, M. Extrinsic and Intrinsic Apoptosis Signal Pathway Review. In Apoptosis and Medicine; Tobias, M.N., Ed.; IntechOpen: London, UK, 2012; Available online: https://www.intechopen.com/chapters/38236 (accessed on 1 September 2021). [CrossRef]
- Bhartiya, D.; Singh, J. FSH–FSHR3–Stem Cells in Ovary Surface Epithelium: Basis for Adult Ovarian Biology, Failure, Aging, and Cancer. Reproduction 2015, 149, R35–R48. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Herr, D.R. G Protein-Coupled Receptor GPR19 Regulates E-Cadherin Expression and Invasion of Breast Cancer Cells. Biochim. Et Biophys. Acta Bba-Mol. Cell Res. 2017, 1864, 1318–1327. [Google Scholar] [CrossRef]
- Bang, Y.-J.; Kwon, J.H.; Kang, S.H.; Kim, J.W.; Yang, Y.C. Increased MAPK Activity and MKP-1 Overexpression in Human Gastric Adenocarcinoma. Biochem. Biophys. Res. Commun. 1998, 250, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Sebolt-Leopold, J.S.; Dudley, D.T.; Herrera, R.; Becelaere, K.V.; Wiland, A.; Gowan, R.C.; Tecle, H.; Barrett, S.D.; Bridges, A.; Przybranowski, S.; et al. Blockade of the MAP Kinase Pathway Suppresses Growth of Colon Tumors in Vivo. Nat. Med. 1999, 5, 810–816. [Google Scholar] [CrossRef]
- Pylayeva-Gupta, Y.; Grabocka, E.; Bar-Sagi, D. RAS Oncogenes: Weaving a Tumorigenic Web. Nat. Rev. Cancer 2011, 11, 761–774. [Google Scholar] [CrossRef]
- Baines, A.T.; Xu, D.; Der, C.J. Inhibition of Ras for Cancer Treatment: The Search Continues. Future Med. Chem. 2011, 3, 1787–1808. [Google Scholar] [CrossRef]
- Brenan, L.; Andreev, A.; Cohen, O.; Pantel, S.; Kamburov, A.; Cacchiarelli, D.; Persky, N.S.; Zhu, C.; Bagul, M.; Goetz, E.M.; et al. Phenotypic Characterization of a Comprehensive Set of MAPK1 /ERK2 Missense Mutants. Cell Rep. 2016, 17, 1171–1183. [Google Scholar] [CrossRef]
- Liu, F.; Yang, X.; Geng, M.; Huang, M. Targeting ERK, an Achilles’ Heel of the MAPK Pathway, in Cancer Therapy. Acta Pharm. Sin. B 2018, 8, 552–562. [Google Scholar] [CrossRef]
- Khan, I.; Rhett, J.M.; O’Bryan, J.P. Therapeutic Targeting of RAS: New Hope for Drugging the “Undruggable”. Biochim. Et Biophys. Acta Bba-Mol. Cell Res. 2020, 1867, 118570. [Google Scholar] [CrossRef]
- Nissan, M.H.; Rosen, N.; Solit, D.B. ERK Pathway Inhibitors: How Low Should We Go? Cancer Discov. 2013, 3, 719–721. [Google Scholar] [CrossRef] [PubMed]
- Smalley, I.; Smalley, K.S.M. ERK Inhibition: A New Front in the War against MAPK Pathway-Driven Cancers? Cancer Discov. 2018, 8, 140–142. [Google Scholar] [CrossRef] [PubMed]
- Cheung, E.C.C.; Slack, R.S. Emerging Role for ERK as a Key Regulator of Neuronal Apoptosis. Sci. Stke Signal. Transduct. Knowl. Environ. 2004, 2004, PE45. [Google Scholar] [CrossRef]
- Subramaniam, S.; Unsicker, K. ERK and Cell Death: ERK1/2 in Neuronal Death: ERK1/2 in Neuronal Death. FEBS J. 2009, 277, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.T.; Levinthal, D.J.; Kulich, S.M.; Chalovich, E.M.; DeFranco, D.B. Oxidative Neuronal Injury. The Dark Side of ERK1/2. Eur. J. Biochem. FEBS 2004, 271, 2060–2066. [Google Scholar] [CrossRef]
- Kulich, S.M.; Chu, C.T. Sustained Extracellular Signal-Regulated Kinase Activation by 6-Hydroxydopamine: Implications for Parkinson’s Disease: Sustained ERK Activation by 6-Hydroxydopamine. J. Neurochem. 2001, 77, 1058–1066. [Google Scholar] [CrossRef]
- Stanciu, M.; Wang, Y.; Kentor, R.; Burke, N.; Watkins, S.; Kress, G.; Reynolds, I.; Klann, E.; Angiolieri, M.R.; Johnson, J.W.; et al. Persistent Activation of ERK Contributes to Glutamate-Induced Oxidative Toxicity in a Neuronal Cell Line and Primary Cortical Neuron Cultures. J. Biol. Chem. 2000, 275, 12200–12206. [Google Scholar] [CrossRef]
- Chambon, J.-P.; Soule, J.; Pomies, P.; Fort, P.; Sahuquet, A.; Alexandre, D.; Mangeat, P.-H.; Baghdiguian, S. Tail Regression in Ciona Intestinalis (Prochordate) Involves a Caspase-Dependent Apoptosis Event Associated with ERK Activation. Dev. Camb. Engl. 2002, 129, 3105–3114. [Google Scholar]
- Kawakami, Y.; Rodríguez-León, J.; Koth, C.M.; Büscher, D.; Itoh, T.; Raya, Á.; Ng, J.K.; Esteban, C.R.; Takahashi, S.; Henrique, D.; et al. MKP3 Mediates the Cellular Response to FGF8 Signalling in the Vertebrate Limb. Nat. Cell Biol. 2003, 5, 513–519. [Google Scholar] [CrossRef]
- Deschênes-Simard, X.; Kottakis, F.; Meloche, S.; Ferbeyre, G. ERKs in Cancer: Friends or Foes? Cancer Res. 2014, 74, 412–419. [Google Scholar] [CrossRef]
- Szydlowska, K.; Gozdz, A.; Dabrowski, M.; Zawadzka, M.; Kaminska, B. Prolonged Activation of ERK Triggers Glutamate-Induced Apoptosis of Astrocytes: Neuroprotective Effect of FK506. J. Neurochem. 2010, 113, 904–918. [Google Scholar] [CrossRef] [PubMed]
- Cerioni, L.; Palomba, L.; Cantoni, O. The Raf/MEK Inhibitor PD98059 Enhances ERK1/2 Phosphorylation Mediated by Peroxynitrite via Enforced Mitochondrial Formation of Reactive Oxygen Species. FEBS Lett. 2003, 547, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Ong, Q.; Guo, S.; Zhang, K.; Cui, B. U0126 Protects Cells against Oxidative Stress Independent of Its Function as a MEK Inhibitor. ACS Chem. Neurosci. 2015, 6, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.-M.; Jung, J.H.; Jeong, S.-J.; Sohn, E.J.; Kim, B.; Kim, S.-H. Tanshinone IIA Induces Autophagic Cell Death via Activation of AMPK and ERK and Inhibition of MTOR and P70 S6K in KBM-5 Leukemia Cells. Phytother. Res. 2013, 28, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Ji, S.; Sun, R.; Xu, K.; Man, Z.; Ji, J.; Pu, Y.; Yin, L.; Zhang, J.; Pu, Y. Prodigiosin Induces Apoptosis and Inhibits Autophagy via the Extracellular Signal-Regulated Kinase Pathway in K562 Cells. Toxicol. In Vitro Int. J. Publ. Assoc. BiBRA 2019, 60, 107–115. [Google Scholar] [CrossRef]
- Thongnuanjan, P.; Soodvilai, S.; Fongsupa, S.; Chabang, N.; Vivithanaporn, P.; Tuchinda, P.; Soodvilai, S. Protective Effect of Panduratin A on Cisplatin-Induced Apoptosis of Human Renal Proximal Tubular Cells and Acute Kidney Injury in Mice. Biol. Pharm. Bull. 2021, 44, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.-C.; Lo, Y.-S.; Chuang, Y.-C.; Lin, C.-C.; Ho, H.-Y.; Hsieh, M.-J.; Lin, J.-T. Dehydrocrenatidine Extracted from Picrasma Quassioides Induces the Apoptosis of Nasopharyngeal Carcinoma Cells through the JNK and ERK Signaling Pathways. Oncol. Rep. 2021, 46, 166. [Google Scholar] [CrossRef]
- Deng, J.; Zhang, X.; Wu, H.; Gan, Y.; Ye, L.; Zheng, H.; Zhu, Z.; Liu, W.J.; Liu, H. ROS-ERK Pathway as Dual Mediators of Cellular Injury and Autophagy-Associated Adaptive Response in Urinary Protein-Irritated Renal Tubular Epithelial Cells. J. Diabetes Res. 2021, 2021, 1–8. [Google Scholar] [CrossRef]
- Wang, D.; Shi, S.; Ren, T.; Zhang, Y.; Guo, P.; Wang, J.; Wang, W. U0126 Pretreatment Inhibits Cisplatin-Induced Apoptosis and Autophagy in HEI-OC1 Cells and Cochlear Hair Cells. Toxicol. Appl. Pharm. 2021, 415, 115447. [Google Scholar] [CrossRef]
- An, J.; Li, L.; Zhang, X. Curcusone C Induces Apoptosis in Endometrial Cancer Cells via Mitochondria-Dependent Apoptotic and ERK Pathway. Biotechnol. Lett. 2021, 43, 329–338. [Google Scholar] [CrossRef]
- Chen, Y.-T.; Huang, Z.-Y.; Tang, H.-H.; Kuo, W.-T.; Wu, S.-Y.; Lan, S.-H.; Chang, K.-H.; Lin, P.-L.; Lee, M.-F.; Cheng, H.-C.; et al. Pterostilbene Sensitizes Cisplatin-Resistant Human Bladder Cancer Cells with Oncogenic HRAS. Cancers 2020, 12, 2869. [Google Scholar] [CrossRef]
- Wang, J.; Liu, X.; Zheng, H.; Liu, Q.; Zhang, H.; Wang, X.; Shen, T.; Wang, S.; Ren, D. Morusin Induces Apoptosis and Autophagy via JNK, ERK and PI3K/Akt Signaling in Human Lung Carcinoma Cells. Chem.-Biol. Interact. 2020, 331, 109279. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Wu, M.; Qin, L.; Song, Y.; Peng, A. DAXX Mediates High Phosphate-Induced Endothelial Cell Apoptosis in Vitro through Activating ERK Signaling. PEERJ 2020, 8, e9203. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.; Palau, V.E.; Mahboob, R.; Lightner, J.; Stone, W.; Krishnan, K. Upregulation of PERK and C-JUN by γ-Tocotrienol and Not α-Tocopherol Are Essential to the Differential Effect on Apoptosis in Prostate Cancer Cells. BMC Cancer 2020, 20, 428. [Google Scholar] [CrossRef]
- Liu, Y.; Fan, D. Ginsenoside Rg5 Induces G2/M Phase Arrest, Apoptosis and Autophagy via Regulating ROS-Mediated MAPK Pathways against Human Gastric Cancer. Biochem. Pharmacol. 2019, 168, 285–304. [Google Scholar] [CrossRef]
- Kang, M.-J.; Kim, S.-Y.; Kwon, E.-B.; Jo, Y.H.; Lee, M.K.; Lee, H.-S.; Moon, D.-O.; Kim, M.-O. Derrone Induces Autophagic Cell Death through Induction of ROS and ERK in A549 Cells. PLoS ONE 2019, 14, e0218659. [Google Scholar] [CrossRef]
- Yano, S.; Wu, S.; Sakao, K.; Hou, D.-X. Involvement of ERK1/2-Mediated ELK1/CHOP/DR5 Pathway in 6-(Methylsulfinyl)Hexyl Isothiocyanate-Induced Apoptosis of Colorectal Cancer Cells. Biosci. Biotechnol. Biochem. 2019, 83, 960–969. [Google Scholar] [CrossRef]
- Wang, T.; Yu, N.; Qian, M.; Feng, J.; Cao, S.; Yin, J.; Zhang, Q. ERK-Mediated Autophagy Promotes Inactivated Sendai Virus (HVJ-E)-Induced Apoptosis in HeLa Cells in an Atg3-Dependent Manner. Cancer Cell Int. 2018, 18, 200. [Google Scholar] [CrossRef]
- Zhou, D.; Zhai, W.; Zhang, M. Mesenchymal Stem Cell-Derived Extracellular Vesicles Promote Apoptosis in RSC96 Schwann Cells through the Activation of the ERK Pathway. Int. J. Clin. Exp. Pathol. 2018, 11, 5157–5170. [Google Scholar]
- Oliveira, M.D.; Barbosa, M.I.; de Souza, T.B.; Moreira, D.R.; Martins, F.T.; Villarreal, W.; Machado, R.P.; Doriguetto, A.C.; Soares, M.B.; Bezerra, D.P. A Novel Platinum Complex Containing a Piplartine Derivative Exhibits Enhanced Cytotoxicity, Causes Oxidative Stress and Triggers Apoptotic Cell Death by ERK/P38 Pathway in Human Acute Promyelocytic Leukemia HL-60 Cells. Redox Biol. 2019, 20, 182–194. [Google Scholar] [CrossRef]
- Jiao, Y.-N.; Wu, L.-N.; Xue, D.; Liu, X.-J.; Tian, Z.-H.; Jiang, S.-T.; Han, S.-Y.; Li, P.-P. Marsdenia Tenacissima Extract Induces Apoptosis and Suppresses Autophagy through ERK Activation in Lung Cancer Cells. Cancer Cell Int. 2018, 18, 149. [Google Scholar] [CrossRef]
- Sun, C.; Li, C.; Li, X.; Zhu, Y.; Su, Z.; Wang, X.; He, Q.; Zheng, G.; Feng, B. Scutellarin Induces Apoptosis and Autophagy in NSCLC Cells through ERK1/2 and AKT Signaling Pathways in Vitro and in Vivo. J. Cancer 2018, 9, 3247–3256. [Google Scholar] [CrossRef]
- Dubey, N.; Peng, B.-Y.; Lin, C.-M.; Wang, P.; Wang, J.; Chan, C.-H.; Wei, H.-J.; Deng, W.-P. NSC 95397 Suppresses Proliferation and Induces Apoptosis in Colon Cancer Cells through MKP-1 and the ERK1/2 Pathway. Int. J. Mol. Sci. 2018, 19, 1625. [Google Scholar] [CrossRef]
- Gao, H.; Zhang, Y.; Dong, L.; Qu, X.-Y.; Tao, L.-N.; Zhang, Y.-M.; Zhai, J.-H.; Song, Y.-Q. Triptolide Induces Autophagy and Apoptosis through ERK Activation in Human Breast Cancer MCF-7 Cells. Exp. Ther. Med. 2018, 15, 3413–3419. [Google Scholar] [CrossRef] [PubMed]
- Wan, B.; Zhu, J.; Chang, Q.; Zhou, H.; Shi, Z.; Min, L.; Cai, Y.; Guan, H. Alpha, 2′-Dihydroxy-4,4′-Dimethoxydihydrochalcone Inhibits Cell Proliferation, Invasion, and Migration in Gastric Cancer in Part via Autophagy. Biomed. Pharmacother. 2018, 98, 709–718. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-H.; Liu, J.-F.; Chiang, Y.-C.; Hu, S.C.-S.; Hsu, L.-F.; Lin, Y.-C.; Lin, Z.-C.; Lee, H.-C.; Chen, M.-C.; Huang, C.-L.; et al. Artocarpin, an Isoprenyl Flavonoid, Induces P53-Dependent or Independent Apoptosis via ROS-Mediated MAPKs and Akt Activation in Non-Small Cell Lung Cancer Cells. Oncotarget 2017, 8, 28342–28358. [Google Scholar] [CrossRef] [PubMed]
- Tavares, R.; Pathak, S.K. Helicobacter Pylori Secreted Protein HP1286 Triggers Apoptosis in Macrophages via TNF-Independent and ERK MAPK-Dependent Pathways. Front. Cell Infect. Microbiol. 2017, 7, 58. [Google Scholar] [CrossRef]
- Ogura, K.; Terasaki, Y.; Miyoshi-Akiyama, T.; Terasaki, M.; Moss, J.; Noda, M.; Yahiro, K. Vibrio Cholerae Cholix Toxin-Induced HepG2 Cell Death Is Enhanced by Tumor Necrosis Factor-Alpha through ROS and Intracellular Signal-Regulated Kinases. Toxicol. Sci. 2017, 156, 455–468. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-F.; Xu, Y.-L.; Tang, Z.-H.; Li, T.; Zhang, L.-L.; Chen, X.; Lu, J.-H.; Leung, C.-H.; Ma, D.-L.; Qiang, W.-A.; et al. Baicalein Induces Beclin 1- and Extracellular Signal-Regulated Kinase-Dependent Autophagy in Ovarian Cancer Cells. Am. J. Chin. Med. 2017, 45, 123–136. [Google Scholar] [CrossRef]
- Yang, Z.; Zhao, Y.; Yao, Y.; Li, J.; Wang, W.; Wu, X. Equol Induces Mitochondria-Dependent Apoptosis in Human Gastric Cancer Cells via the Sustained Activation of ERK1/2 Pathway. Mol. Cells 2016, 39, 742–749. [Google Scholar] [CrossRef]
- Kuo, H.-H.; Kakadiya, R.; Wu, Y.-C.; Su, T.-L.; Lee, T.-C.; Lin, Y.-W.; Yih, L.-H. Derivatives of 6-Cinnamamido-Quinoline-4-Carboxamide Impair Lysosome Function and Induce Apoptosis. Oncotarget 2015, 7, 38078–38090. [Google Scholar] [CrossRef]
- Chen, J.-C.; Hsieh, M.-J.; Chen, C.-J.; Lin, J.-T.; Lo, Y.-S.; Chuang, Y.-C.; Chien, S.-Y.; Chen, M.-K. Polyphyllin G Induce Apoptosis and Autophagy in Human Nasopharyngeal Cancer Cells by Modulation of AKT and Mitogen-Activated Protein Kinase Pathways in Vitro and in Vivo. Oncotarget 2016, 7, 70276–70289. [Google Scholar] [CrossRef] [PubMed]
- Park, B.H.; Lim, J.E.; Jeon, H.G.; Seo, S.I.; Lee, H.M.; Choi, H.Y.; Jeon, S.S.; Jeong, B.C. Curcumin Potentiates Antitumor Activity of Cisplatin in Bladder Cancer Cell Lines via ROS-Mediated Activation of ERK1/2. Oncotarget 2016, 7, 63870–63886. [Google Scholar] [CrossRef] [PubMed]
- Hasan, I.; Sugawara, S.; Fujii, Y.; Koide, Y.; Terada, D.; Iimura, N.; Fujiwara, T.; Takahashi, K.G.; Kojima, N.; Rajia, S.; et al. MytiLec, a Mussel R-Type Lectin, Interacts with Surface Glycan Gb3 on Burkitt’s Lymphoma Cells to Trigger Apoptosis through Multiple Pathways. Mar. Drugs 2015, 13, 7377–7389. [Google Scholar] [CrossRef] [PubMed]
- Liu, E.; Li, J.; Shi, S.; Wang, X.; Liang, T.; Wu, B.; Li, Q. Sustained ERK Activation-Mediated Proliferation Inhibition of Farrerol on Human Gastric Carcinoma Cell Line by G0/G1-Phase Cell-Cycle Arrest. Eur. J. Cancer Prev. 2016, 25, 490–499. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Liu, W.; Wang, Y.; Dai, N.; Gu, J.; Yuan, Y.; Liu, X.; Bian, J.; Liu, Z.-P. Cadmium Induces Apoptosis in Primary Rat Osteoblasts through Caspase and Mitogen-Activated Protein Kinase Pathways. J. Vet. Sci. 2015, 16, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Han, W.; Li, J.; Hu, L.; Zhou, Y. Physalin B Not Only Inhibits the Ubiquitin-Proteasome Pathway but Also Induces Incomplete Autophagic Response in Human Colon Cancer Cells in Vitro. Acta Pharmacol. Sin. 2015, 36, 517–527. [Google Scholar] [CrossRef]
- Seo, H.J.; Choi, S.J.; Lee, J.-H. Paraquat Induces Apoptosis through Cytochrome C Release and ERK Activation. Biomol. Ther. 2014, 22, 503–509. [Google Scholar] [CrossRef]
- Cheng, L.; Xia, T.-S.; Wang, Y.-F.; Zhou, W.; Liang, X.-Q.; Xue, J.-Q.; Shi, L.; Wang, Y.; Ding, Q. The Apoptotic Effect of D Rhamnose β-Hederin, a Novel Oleanane-Type Triterpenoid Saponin on Breast Cancer Cells. PLoS ONE 2014, 9, e90848. [Google Scholar] [CrossRef]
- Forbes, A.; Davey, A.K.; Perkins, A.V.; Grant, G.D.; McFarland, A.J.; McDermott, C.M.; Anoopkumar-Dukie, S. ERK1/2 Activation Modulates Pyocyanin-Induced Toxicity in A549 Respiratory Epithelial Cells. Chem.-Biol. Interact. 2014, 208, 58–63. [Google Scholar] [CrossRef]
- Choi, M.; Park, H.; Oh, J.; Lee, E.; Park, S.; Yoon, S. Nonylphenol-induced Apoptotic Cell Death in Mouse TM4 Sertoli Cells via the Generation of Reactive Oxygen Species and Activation of the ERK Signaling Pathway. J. Appl. Toxicol. 2014, 34, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Yiran, Z.; Chenyang, J.; Jiajing, W.; Yan, Y.; Jianhong, G.; Jianchun, B.; Xuezhong, L.; Zongping, L. Oxidative Stress and Mitogen-Activated Protein Kinase Pathways Involved in Cadmium-Induced BRL 3A Cell Apoptosis. Oxid. Med. Cell. Longev. 2013, 2013, 1–12. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, M.-Y.; Hao, K.; Chen, X.-Q.; Du, J.-Z. CRHR1 Mediates P53 Transcription Induced by High Altitude Hypoxia through ERK 1/2 Signaling in Rat Hepatic Cells. Peptides 2013, 44, 8–14. [Google Scholar] [CrossRef]
- Tsai, S.-C.; Huang, W.-W.; Huang, W.-C.; Lu, C.-C.; Chiang, J.-H.; Peng, S.-F.; Chung, J.-G.; Lin, Y.-H.; Hsu, Y.-M.; Amagaya, S.; et al. ERK-Modulated Intrinsic Signaling and G2/M Phase Arrest Contribute to the Induction of Apoptotic Death by Allyl Isothiocyanate in MDA-MB-468 Human Breast Adenocarcinoma Cells. Int. J. Oncol. 2012, 41, 2065–2072. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H.; Lee, S.-W.; Choi, S.-H.; Kim, S.-H.; Kim, W.-J.; Jung, J.-Y. P38 MAP Kinase and ERK Play an Important Role in Nitric Oxide-Induced Apoptosis of the Mouse Embryonic Stem Cells. Toxicol. In Vitro 2013, 27, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.-J.; Wang, H.-B.; Ma, X.-Q.; Chen, J.-H. β,β-Dimethylacrylshikonin Induces Mitochondria Dependent Apoptosis through ERK Pathway in Human Gastric Cancer SGC-7901 Cells. PLoS ONE 2012, 7, e41773. [Google Scholar] [CrossRef]
- Chi, J.; Zhu, Y.; Fu, Y.; Liu, Y.; Zhang, X.; Han, L.; Yin, X.; Zhao, D. Cyclosporin A Induces Apoptosis in H9c2 Cardiomyoblast Cells through Calcium-Sensing Receptor-Mediated Activation of the ERK MAPK and P38 MAPK Pathways. Mol. Cell. Biochem. 2012, 367, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Shimo, T.; Kurebayashi, J.; Kanomata, N.; Yamashita, T.; Kozuka, Y.; Moriya, T.; Sonoo, H. Antitumor and Anticancer Stem Cell Activity of a Poly ADP-Ribose Polymerase Inhibitor Olaparib in Breast Cancer Cells. Breast Cancer-Tokyo 2014, 21, 75–85. [Google Scholar] [CrossRef]
- Svojgr, K.; Kalina, T.; Kanderova, V.; Skopcova, T.; Brdicka, T.; Zuna, J. The Adaptor Protein NTAL Enhances Proximal Signaling and Potentiates Corticosteroid-Induced Apoptosis in T-ALL. Exp. Hematol. 2012, 40, 379–385. [Google Scholar] [CrossRef]
- Lin, H.-P.; Chang, J.-Y.; Lin, S.-R.; Lee, M.-H.; Huang, S.-S.; Hsu, L.-J.; Chang, N.-S. Identification of an In Vivo MEK/WOX1 Complex as a Master Switch for Apoptosis in T Cell Leukemia. Genes Cancer 2011, 2, 550–562. [Google Scholar] [CrossRef][Green Version]
- Banerjee, C.; Goswami, R.; Datta, S.; Rajagopal, R.; Mazumder, S. Arsenic-Induced Alteration in Intracellular Calcium Homeostasis Induces Head Kidney Macrophage Apoptosis Involving the Activation of Calpain-2 and ERK in Clarias Batrachus. Toxicol. Appl. Pharm. 2011, 256, 44–51. [Google Scholar] [CrossRef]
- Yang, H.; Dou, Y.; Zheng, X.; Tan, Y.; Cheng, J.; Li, L.; Du, Y.; Zhu, D.; Lou, Y. Cysteinyl Leukotrienes Synthesis Is Involved in Aristolochic Acid I-Induced Apoptosis in Renal Proximal Tubular Epithelial Cells. Toxicology 2011, 287, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Govind, S.; Sajankila, S.P.; Mi, L.; Roy, R.; Chung, F. Phenethyl Isothiocyanate Sensitizes Human Cervical Cancer Cells to Apoptosis Induced by Cisplatin. Mol. Nutr. Food Res. 2011, 55, 1572–1581. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.-Y.; Chang, G.-C.; Chen, K.-C.; Hung, H.-W.; Hsu, K.-H.; Sheu, G.-T.; Hsu, S.-L. Sustained Activation of ERK and Cdk2/Cyclin-A Signaling Pathway by Pemetrexed Leading to S-Phase Arrest and Apoptosis in Human Non-Small Cell Lung Cancer A549 Cells. Eur. J. Pharmacol. 2011, 663, 17–26. [Google Scholar] [CrossRef]
- Guo, Y.; Zhang, X.; Meng, J.; Wang, Z.-Y. An Anticancer Agent Icaritin Induces Sustained Activation of the Extracellular Signal-Regulated Kinase (ERK) Pathway and Inhibits Growth of Breast Cancer Cells. Eur. J. Pharmacol. 2011, 658, 114–122. [Google Scholar] [CrossRef]
- Snyder, A.; Alsauskas, Z.C.; Leventhal, J.S.; Rosenstiel, P.E.; Gong, P.; Chan, J.J.; Barley, K.; He, J.C.; Klotman, M.E.; Ross, M.J.; et al. HIV-1 Viral Protein r Induces ERK and Caspase-8-Dependent Apoptosis in Renal Tubular Epithelial Cells. Aids 2010, 24, 1107–1119. [Google Scholar] [CrossRef]
- Lu, K.; Liang, C.; Liliang, P.; Yang, C.; Cho, C.; Weng, H.; Tsai, Y.; Wang, K.; Chen, H. Inhibition of Extracellular Signal-regulated Kinases 1/2 Provides Neuroprotection in Spinal Cord Ischemia/Reperfusion Injury in Rats: Relationship with the Nuclear Factor-κB-regulated Anti-apoptotic Mechanisms. J. Neurochem. 2010, 114, 237–246. [Google Scholar] [CrossRef]
- Negrín, G.; Eiroa, J.L.; Morales, M.; Triana, J.; Quintana, J.; Estévez, F. Naturally Occurring Asteriscunolide A Induces Apoptosis and Activation of Mitogen-activated Protein Kinase Pathway in Human Tumor Cell Lines. Mol. Carcinog. 2010, 49, 488–499. [Google Scholar] [CrossRef]
- Huang, C.-F.; Liu, S.-H.; Su, C.-C.; Fang, K.-M.; Yen, C.-C.; Yang, C.-Y.; Tang, F.-C.; Liu, J.-M.; Wu, C.-C.; Lee, K.-I.; et al. Roles of ERK/Akt Signals in Mitochondria-Dependent and Endoplasmic Reticulum Stress-Triggered Neuronal Cell Apoptosis Induced by 4-Methyl-2,4-Bis(4-Hydroxyphenyl)Pent-1-Ene, a Major Active Metabolite of Bisphenol A. Toxicology 2021, 455, 152764. [Google Scholar] [CrossRef]
- Paul, M.; Manikanta, K.; Hemshekhar, M.; Sundaram, M.S.; Naveen, S.; Ramesh, T.N.; Kemparaju, K.; Girish, K.S. Bisdemethoxycurcumin Promotes Apoptosis in Human Platelets via Activation of ERK Signaling Pathway. Toxicol. In Vitro 2020, 63, 104743. [Google Scholar] [CrossRef]
- Sreenivasulu, R.; Reddy, K.T.; Sujitha, P.; Kumar, C.G.; Raju, R.R. Synthesis, Antiproliferative and Apoptosis Induction Potential Activities of Novel Bis(Indolyl)Hydrazide-Hydrazone Derivatives. Bioorgan. Med. Chem. 2019, 27, 1043–1055. [Google Scholar] [CrossRef]
- Lee, J.S.; Lee, M.S.; Cha, E.Y.; Thuong, P.T.; Sul, J.Y.; Park, J.B.; Ko, Y.B. A Natural Ent-Kaurane Diterpenoid Induces Antiproliferation in Ovarian Cancer Cells via ERK1/2 Regulation and Inhibition of Cellular Migration and Invasion. Mol. Med. Rep. 2018, 18, 3898–3906. [Google Scholar] [CrossRef] [PubMed]
- Zong, D.; Li, J.; Cai, S.; He, S.; Liu, Q.; Jiang, J.; Chen, S.; Long, Y.; Chen, Y.; Chen, P.; et al. Notch1 Regulates Endothelial Apoptosis via the ERK Pathway in Chronic Obstructive Pulmonary Disease. Am. J. Physiol.-Cell Physiol. 2018, 315, C330–C340. [Google Scholar] [CrossRef] [PubMed]
- Han, M.; Gao, H.; Ju, P.; Gao, M.; Yuan, Y.; Chen, X.; Liu, K.; Han, Y.; Han, Z. Hispidulin Inhibits Hepatocellular Carcinoma Growth and Metastasis through AMPK and ERK Signaling Mediated Activation of PPARγ. Biomed. Pharmacother. 2018, 103, 272–283. [Google Scholar] [CrossRef]
- Huang, K.; Chen, Y.; Zhang, R.; Wu, Y.; Ma, Y.; Fang, X.; Shen, S. Honokiol Induces Apoptosis and Autophagy via the ROS/ERK1/2 Signaling Pathway in Human Osteosarcoma Cells in Vitro and in Vivo. Cell Death Dis. 2018, 9, 157. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.K.; Kim, S.-J. Desipramine Induces Apoptosis in Hepatocellular Carcinoma Cells. Oncol. Rep. 2017, 38, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Bastola, T.; An, R.; Kim, Y.-C.; Kim, J.; Seo, J. Cearoin Induces Autophagy, ERK Activation and Apoptosis via ROS Generation in SH-SY5Y Neuroblastoma Cells. Molecules 2017, 22, 242. [Google Scholar] [CrossRef]
- Zhang, C.; Liu, S.; Yuan, X.; Hu, Z.; Li, H.; Wu, M.; Yuan, J.; Zhao, Z.; Su, J.; Wang, X.; et al. Valproic Acid Promotes Human Glioma U87 Cells Apoptosis and Inhibits Glycogen Synthase Kinase-3β Through ERK/Akt Signaling. Cell. Physiol. Biochem. 2016, 39, 2173–2185. [Google Scholar] [CrossRef]
- Teng, H.; Huang, Q.; Chen, L. Inhibition of Cell Proliferation and Triggering of Apoptosis by Agrimonolide through MAP Kinase (ERK and P38) Pathways in Human Gastric Cancer AGS Cells. Food Funct. 2016, 7, 4605–4613. [Google Scholar] [CrossRef]
- Jang, H.J.; Hong, E.M.; Park, S.W.; Byun, H.W.; Koh, D.H.; Choi, M.H.; Kae, S.H.; Lee, J. Statin Induces Apoptosis of Human Colon Cancer Cells and Downregulation of Insulin-like Growth Factor 1 Receptor via Proapoptotic ERK Activation. Oncol. Lett. 2016, 12, 250–256. [Google Scholar] [CrossRef]
- Zhang, D.-X.; Ma, D.-Y.; Yao, Z.-Q.; Fu, C.-Y.; Shi, Y.-X.; Wang, Q.-L.; Tang, Q.-Q. ERK1/2/P53 and NF-ΚB Dependent-PUMA Activation Involves in Doxorubicin-Induced Cardiomyocyte Apoptosis. Eur. Rev. Med. Pharmacol. 2016, 20, 2435–2442. [Google Scholar]
- Huang, F.; Liu, Q.; Xie, S.; Xu, J.; Huang, B.; Wu, Y.; Xia, D. Cypermethrin Induces Macrophages Death through Cell Cycle Arrest and Oxidative Stress-Mediated JNK/ERK Signaling Regulated Apoptosis. Int. J. Mol. Sci. 2016, 17, 885. [Google Scholar] [CrossRef]
- Feng, D.; Wang, B.; Ma, Y.; Shi, W.; Tao, K.; Zeng, W.; Cai, Q.; Zhang, Z.; Qin, H. The Ras/Raf/Erk Pathway Mediates the Subarachnoid Hemorrhage-Induced Apoptosis of Hippocampal Neurons Through Phosphorylation of P53. Mol. Neurobiol. 2015, 53, 5737–5748. [Google Scholar] [CrossRef]
- Yeh, P.-S.; Wang, W.; Chang, Y.-A.; Lin, C.-J.; Wang, J.-J.; Chen, R.-M. Honokiol Induces Autophagy of Neuroblastoma Cells through Activating the PI3K/Akt/MTOR and Endoplasmic Reticular Stress/ERK1/2 Signaling Pathways and Suppressing Cell Migration. Cancer Lett. 2016, 370, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Ruan, H.; Gu, P.; Ding, W.; Luo, X.; Huang, R.; Zhao, W.; Gao, L. The Roles of P38 MAPK and ERK1/2 in Coplanar Polychlorinated Biphenyls-Induced Apoptosis of Human Extravillous Cytotrophoblast-Derived Transformed Cells. Cell. Physiol. Biochem. 2015, 36, 2418–2432. [Google Scholar] [CrossRef]
- Baek, S.H.; Kim, C.; Lee, J.H.; Nam, D.; Lee, J.; Lee, S.-G.; Chung, W.-S.; Jang, H.-J.; Kim, S.-H.; Ahn, K.S. Cinobufagin Exerts Anti-Proliferative and pro-Apoptotic Effects through the Modulation ROS-Mediated MAPKs Signaling Pathway. Immunopharm. Immunot. 2015, 37, 265–273. [Google Scholar] [CrossRef]
- Meng, G.; Wang, W.; Chai, K.; Yang, S.; Li, F.; Jiang, K. Combination Treatment with Triptolide and Hydroxycamptothecin Synergistically Enhances Apoptosis in A549 Lung Adenocarcinoma Cells through PP2A-Regulated ERK, P38 MAPKs and Akt Signaling Pathways. Int. J. Oncol. 2015, 46, 1007–1017. [Google Scholar] [CrossRef]
- Pathania, A.S.; Kumar, S.; Guru, S.K.; Bhushan, S.; Sharma, P.R.; Aithagani, S.K.; Singh, P.P.; Vishwakarma, R.A.; Kumar, A.; Malik, F. The Synthetic Tryptanthrin Analogue Suppresses STAT3 Signaling and Induces Caspase Dependent Apoptosis via ERK Up Regulation in Human Leukemia HL-60 Cells. PLoS ONE 2014, 9, e110411. [Google Scholar] [CrossRef]
- Zerin, T.; Song, H.-Y.; Kim, Y.-S. Extracellular Signal-Regulated Kinase Pathway Play Distinct Role in Acetochlor-Mediated Toxicity and Intrinsic Apoptosis in A549 Cells. Toxicol. In Vitro 2015, 29, 85–92. [Google Scholar] [CrossRef]
- Lee, Y.J.; Choi, S.-Y.; Yang, J.H. NMDA Receptor-Mediated ERK 1/2 Pathway Is Involved in PFHxS-Induced Apoptosis of PC12 Cells. Sci. Total Environ. 2014, 491–492, 227–234. [Google Scholar] [CrossRef]
- Lee, S.H.; Kang, Y.J.; Sung, B.; Kim, D.H.; Lim, H.S.; Kim, H.R.; Kim, S.J.; Yoon, J.-H.; Moon, H.R.; Chung, H.Y.; et al. MHY-449, a Novel Dihydrobenzofuro[4,5-b][1,8] Naphthyridin-6-One Derivative, Induces Apoptotic Cell Death through Modulation of Akt/FoxO1 and ERK Signaling in PC3 Human Prostate Cancer Cells. Int. J. Oncol. 2014, 44, 905–911. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lu, T.-H.; Tseng, T.-J.; Su, C.-C.; Tang, F.-C.; Yen, C.-C.; Liu, Y.-Y.; Yang, C.-Y.; Wu, C.-C.; Chen, K.-L.; Hung, D.-Z.; et al. Arsenic Induces Reactive Oxygen Species-Caused Neuronal Cell Apoptosis through JNK/ERK-Mediated Mitochondria-Dependent and GRP 78/CHOP-Regulated Pathways. Toxicol. Lett. 2014, 224, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Xu, L.; Fan, Y.; Li, C.; Zhang, Y.; Zheng, H.; Hou, K.; Qu, X.; Liu, Y. Interferon-α Enhances 5′-Deoxy-5-Fluorouridine-Induced Apoptosis by ERK-Dependant Upregulation of Thymidine Phosphorylase. Biomed Res. Int. 2013, 2013, 1–8. [Google Scholar] [CrossRef][Green Version]
- Chien, C.-S.; Ma, K.-H.; Lee, H.-S.; Liu, P.-S.; Li, Y.-H.; Huang, Y.-S.; Chueh, S.-H. Dual Effect of Capsaicin on Cell Death in Human Osteosarcoma G292 Cells. Eur. J. Pharmacol. 2013, 718, 350–360. [Google Scholar] [CrossRef] [PubMed]
- Kong, D.; Zheng, T.; Zhang, M.; Wang, D.; Du, S.; Li, X.; Fang, J.; Cao, X. Static Mechanical Stress Induces Apoptosis in Rat Endplate Chondrocytes through MAPK and Mitochondria-Dependent Caspase Activation Signaling Pathways. PLoS ONE 2013, 8, e69403. [Google Scholar] [CrossRef]
- Pan, T.-L.; Wang, P.-W. Explore the Molecular Mechanism of Apoptosis Induced by Tanshinone IIA on Activated Rat Hepatic Stellate Cells. Evid.-Based Complement. Altern Med. Ecam. 2012, 2012, 734987. [Google Scholar] [CrossRef]
- Lee, Y.J.; Lee, H.-G.; Yang, J.-H. Perfluorooctane Sulfonate-Induced Apoptosis of Cerebellar Granule Cells Is Mediated by ERK 1/2 Pathway. Chemosphere 2013, 90, 1597–1602. [Google Scholar] [CrossRef]
- Bhattarai, G.; Lee, Y.-H.; Lee, N.-H.; Lee, I.-K.; Yun, B.-S.; Hwang, P.-H.; Yi, H.-K. Fomitoside-K from Fomitopsis Nigra Induces Apoptosis of Human Oral Squamous Cell Carcinomas (YD-10B) via Mitochondrial Signaling Pathway. Biol. Pharm. Bull. 2012, 35, 1711–1719. [Google Scholar] [CrossRef][Green Version]
- Lee, C.-C.; Lin, Y.-H.; Chang, W.-H.; Wu, Y.-C.; Chang, J.-G. The Small Molecule Calactin Induces DNA Damage and Apoptosis in Human Leukemia Cells. Eur. J. Cancer Prev. 2012, 21, 467–473. [Google Scholar] [CrossRef]
- Lin, M.-W.; Lin, A.-S.; Wu, D.-C.; Wang, S.S.W.; Chang, F.-R.; Wu, Y.-C.; Huang, Y.-B. Euphol from Euphorbia Tirucalli Selectively Inhibits Human Gastric Cancer Cell Growth through the Induction of ERK1/2-Mediated Apoptosis. Food Chem. Toxicol. 2012, 50, 4333–4339. [Google Scholar] [CrossRef]
- Jo, J.-R.; Park, J.S.; Park, Y.-K.; Chae, Y.Z.; Lee, G.-H.; Park, G.-Y.; Jang, B.-C. Pinus Densiflora Leaf Essential Oil Induces Apoptosis via ROS Generation and Activation of Caspases in YD-8 Human Oral Cancer Cells. Int. J. Oncol. 2011, 40, 1238–1245. [Google Scholar] [CrossRef]
- Arbon, K.S.; Christensen, C.M.; Harvey, W.A.; Heggland, S.J. Cadmium Exposure Activates the ERK Signaling Pathway Leading to Altered Osteoblast Gene Expression and Apoptotic Death in Saos-2 Cells. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2011, 50, 198–205. [Google Scholar] [CrossRef]
- Yang, L.; Ling, Y.; Zhang, Z.; Zhao, Q.; Tang, J.; Ji, H.; Zhang, Y. ZL11n Is a Novel Nitric Oxide-Releasing Derivative of Farnesylthiosalicylic Acid That Induces Apoptosis in Human Hepatoma HepG2 Cells via MAPK/Mitochondrial Pathways. Biochem. Biophys. Res. Commun. 2011, 409, 752–757. [Google Scholar] [CrossRef]
- Liu, H.; Li, H.; Xu, A.; Kan, Q.; Liu, B. Role of Phosphorylated ERK in Amygdala Neuronal Apoptosis in Single-Prolonged Stress Rats. Mol. Med. Rep. 2010, 3, 1059–1063. [Google Scholar] [CrossRef] [PubMed]
- Pal, P.; Kanaujiya, J.K.; Lochab, S.; Tripathi, S.B.; Bhatt, M.L.B.; Singh, P.K.; Sanyal, S.; Trivedi, A.K. 2-D Gel Electrophoresis-Based Proteomic Analysis Reveals That Ormeloxifen Induces G0-G1 Growth Arrest and ERK-Mediated Apoptosis in Chronic Myeloid Leukemia Cells K562. Proteomics 2011, 11, 1517–1529. [Google Scholar] [CrossRef]
- Iwayama, H.; Sakamoto, T.; Nawa, A.; Ueda, N. Crosstalk between Smad and Mitogen-Activated Protein Kinases for the Regulation of Apoptosis in Cyclosporine A-Induced Renal Tubular Injury. Nephron Extra 2011, 1, 178–189. [Google Scholar] [CrossRef] [PubMed]
- An, H.-X.; Jin, Z.-F.; Ge, X.-F.; Wu, J.; Chen, C.; Zhang, F.-M.; Qu, W.; Liu, X.-G.; Liu, S.-Y. Parathyroid Hormone(1-34)-Induced Apoptosis in Neuronal Rat PC12 Cells: Implications for Neurotoxicity. Pathol.-Res. Pract. 2010, 206, 821–827. [Google Scholar] [CrossRef]
- Guo, D.; Guo, C.; Fang, L.; Sang, T.; Wang, Y.; Wu, K.; Guo, C.; Wang, Y.; Pan, H.; Chen, R.; et al. Qizhen Capsule Inhibits Colorectal Cancer by Inducing NAG-1/GDF15 Expression That Mediated via MAPK/ERK Activation. J. Ethnopharmacol. 2021, 273, 113964. [Google Scholar] [CrossRef]
- Lee, J.H.; Han, S.H.; Kim, Y.M.; Kim, S.H.; Yoo, E.S.; Woo, J.S.; Jung, G.H.; Jung, S.H.; Kim, B.S.; Jung, J.Y. Shikonin Inhibits Proliferation of Melanoma Cells by MAPK Pathway-Mediated Induction of Apoptosis. Biosci. Rep. 2021, 41. [Google Scholar] [CrossRef]
- Ghosh, J.; Das, J.; Manna, P.; Sil, P.C. Hepatotoxicity of Di-(2-Ethylhexyl)Phthalate Is Attributed to Calcium Aggravation, ROS-Mediated Mitochondrial Depolarization, and ERK/NF-ΚB Pathway Activation. Free Radic Biol. Med. 2010, 49, 1779–1791. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Kim, H.J.; Kwon, C.H.; Kim, J.H.; Woo, J.S.; Jung, J.S.; Kim, J.M. Role of ERK Activation in Cisplatin-Induced Apoptosis in OK Renal Epithelial Cells. J. Appl. Toxicol. 2005, 25, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Park, S.A.; Park, H.J.; Lee, B.I.; Ahn, Y.H.; Kim, S.U.; Choi, K.S. Bcl-2 Blocks Cisplatin-Induced Apoptosis by Suppression of ERK-Mediated P53 Accumulation in B104 Cells. Mol. Brain Res. 2001, 93, 18–26. [Google Scholar] [CrossRef]
- Park, B.G.; Yoo, C.I.; Kim, H.T.; Kwon, C.H.; Kim, Y.K. Role of Mitogen-Activated Protein Kinases in Hydrogen Peroxide-Induced Cell Death in Osteoblastic Cells. Toxicology 2005, 215, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Boutahar, N.; Reynaud, E.; Lassabliere, F.; Borg, J. Timing Differences of Signaling Response in Neuron Cultures Activated by Glutamate Analogue or Free Radicals. Brain Res. 2008, 1191, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Jo, S.-K.; Cho, W.Y.; Sung, S.A.; Kim, H.K.; Won, N.H. MEK Inhibitor, U0126, Attenuates Cisplatin-Induced Renal Injury by Decreasing Inflammation and Apoptosis. Kidney Int. 2005, 67, 458–466. [Google Scholar] [CrossRef]
- Wang, Z.-Q.; Wu, D.-C.; Huang, F.-P.; Yang, G.-Y. Inhibition of MEK/ERK 1/2 Pathway Reduces pro-Inflammatory Cytokine Interleukin-1 Expression in Focal Cerebral Ischemia. Brain Res. 2004, 996, 55–66. [Google Scholar] [CrossRef]
- Sinha, D.; Bannergee, S.; Schwartz, J.H.; Lieberthal, W.; Levine, J.S. Inhibition of Ligand-Independent ERK1/2 Activity in Kidney Proximal Tubular Cells Deprived of Soluble Survival Factors Up-Regulates Akt and Prevents Apoptosis. J. Biol. Chem. 2004, 279, 10962–10972. [Google Scholar] [CrossRef]
- Rai, S.N.; Dilnashin, H.; Birla, H.; Singh, S.S.; Zahra, W.; Rathore, A.S.; Singh, B.K.; Singh, S.P. The Role of PI3K/Akt and ERK in Neurodegenerative Disorders. Neurotox. Res. 2019, 35, 775–795. [Google Scholar] [CrossRef]
- Grant, S. Cotargeting Survival Signaling Pathways in Cancer. J. Clin. Investig. 2008, 118, 3003–3006. [Google Scholar] [CrossRef]
- Tang, D.; Wu, D.; Hirao, A.; Lahti, J.M.; Liu, L.; Mazza, B.; Kidd, V.J.; Mak, T.W.; Ingram, A.J. ERK Activation Mediates Cell Cycle Arrest and Apoptosis after DNA Damage Independently of P53. J. Biol. Chem. 2002, 277, 12710–12717. [Google Scholar] [CrossRef]
- Billecke, C.; Finniss, S.; Tahash, L.; Miller, C.; Mikkelsen, T.; Farrell, N.P.; Bögler, O. Polynuclear Platinum Anticancer Drugs Are More Potent than Cisplatin and Induce Cell Cycle Arrest in Glioma. Neuro-Oncology 2006, 8, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.J. P53, the Cellular Gatekeeper for Growth and Division. Cell 1997, 88, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Haupt, S.; Berger, M.; Goldberg, Z.; Haupt, Y. Apoptosis—the P53 Network. J. Cell Sci. 2003, 116, 4077–4085. [Google Scholar] [CrossRef] [PubMed]
- Mihara, M.; Erster, S.; Zaika, A.; Petrenko, O.; Chittenden, T.; Pancoska, P.; Moll, U.M. P53 Has a Direct Apoptogenic Role at the Mitochondria. Mol. Cell 2003, 11, 577–590. [Google Scholar] [CrossRef] [PubMed]
- Mirza, A.; McGuirk, M.; Hockenberry, T.N.; Wu, Q.; Ashar, H.; Black, S.; Wen, S.F.; Wang, L.; Kirschmeier, P.; Bishop, W.R.; et al. Human Survivin Is Negatively Regulated by Wild-Type P53 and Participates in P53-Dependent Apoptotic Pathway. Oncogene 2002, 21, 2613–2622. [Google Scholar] [CrossRef]
- Wang, S.; Shi, X. Mechanisms of Cr(VI)-Induced P53 Activation: The Role of Phosphorylation, Mdm2 and ERK. Carcinogenesis 2001, 22, 757–762. [Google Scholar] [CrossRef]
- Yeh, P.Y.; Chuang, S.-E.; Yeh, K.-H.; Song, Y.C.; Chang, L.L.-Y.; Cheng, A.-L. Phosphorylation of P53 on Thr55 by ERK2 Is Necessary for Doxorubicin-Induced P53 Activation and Cell Death. Oncogene 2004, 23, 3580–3588. [Google Scholar] [CrossRef]
- Liu, J.; Mao, W.; Ding, B.; Liang, C. ERKs/P53 Signal Transduction Pathway Is Involved in Doxorubicin-Induced Apoptosis in H9c2 Cells and Cardiomyocytes. Am. J. Physiol.-Heart C 2008, 295, H1956–H1965. [Google Scholar] [CrossRef]
- Singh, S.; Upadhyay, A.K.; Ajay, A.K.; Bhat, M.K. P53 Regulates ERK Activation in Carboplatin Induced Apoptosis in Cervical Carcinoma: A Novel Target of P53 in Apoptosis. FEBS Lett. 2006, 581, 289–295. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Shin, S.J.; Kim, H.-S. ERK1/2 Activation Mediated by the Nutlin-3-Induced Mitochondrial Translocation of P53. Int. J. Oncol. 2013, 42, 1027–1035. [Google Scholar] [CrossRef]
- Heo, J.-I.; Oh, S.-J.; Kho, Y.-J.; Kim, J.-H.; Kang, H.-J.; Park, S.-H.; Kim, H.-S.; Shin, J.-Y.; Kim, M.-J.; Kim, M.; et al. ATM Mediates Interdependent Activation of P53 and ERK through Formation of a Ternary Complex with P-P53 and p-ERK in Response to DNA Damage. Mol. Biol. Rep. 2012, 39, 8007–8014. [Google Scholar] [CrossRef]
- Ozben, T. Oxidative Stress and Apoptosis: Impact on Cancer Therapy. J. Pharm. Sci. 2007, 96, 2181–2196. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, Y.; Kawai, Y.; Kohda, Y.; Gemba, M. Involvement of Activation of NADPH Oxidase and Extracellular Signal-Regulated Kinase (ERK) in Renal Cell Injury Induced by Zinc. J. Toxicol. Sci. 2005, 30, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Ramachandiran, S.; Huang, Q.; Dong, J.; Lau, S.S.; Monks, T.J. Mitogen-Activated Protein Kinases Contribute to Reactive Oxygen Species-Induced Cell Death in Renal Proximal Tubule Epithelial Cells. Chem. Res. Toxicol. 2002, 15, 1635–1642. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Shan, P.; Sasidhar, M.; Chupp, G.L.; Flavell, R.A.; Choi, A.M.K.; Lee, P.J. Reactive Oxygen Species and Extracellular Signal-Regulated Kinase 1/2 Mitogen-Activated Protein Kinase Mediate Hyperoxia-Induced Cell Death in Lung Epithelium. Am. J. Resp. Cell Mol. 2003, 28, 305–315. [Google Scholar] [CrossRef]
- Zhang, P.; Wang, Y.-Z.; Kagan, E.; Bonner, J.C. Peroxynitrite Targets the Epidermal Growth Factor Receptor, Raf-1, and MEK Independently to Activate MAPK*. J. Biol. Chem. 2000, 275, 22479–22486. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-J.; Cho, H.-N.; Soh, J.-W.; Jhon, G.J.; Cho, C.-K.; Chung, H.-Y.; Bae, S.; Lee, S.-J.; Lee, Y.-S. Oxidative Stress-Induced Apoptosis Is Mediated by ERK1/2 Phosphorylation. Exp. Cell Res. 2003, 291, 251–266. [Google Scholar] [CrossRef] [PubMed]
- Nabeyrat, E.; Jones, G.E.; Fenwick, P.S.; Barnes, P.J.; Donnelly, L.E. Mitogen-Activated Protein Kinases Mediate Peroxynitrite-Induced Cell Death in Human Bronchial Epithelial Cells. Am. J. Physiol.-Lung C 2003, 284, L1112–L1120. [Google Scholar] [CrossRef]
- Kohda, Y.; Hiramatsu, J.; Gemba, M. Involvement of MEK/ERK Pathway in Cephaloridine-Induced Injury in Rat Renal Cortical Slices. Toxicol. Lett. 2003, 143, 185–194. [Google Scholar] [CrossRef]
- Shin, H.-J.; Kwon, H.-K.; Lee, J.-H.; Anwar, M.A.; Choi, S. Etoposide Induced Cytotoxicity Mediated by ROS and ERK in Human Kidney Proximal Tubule Cells. Sci. Rep.-UK 2016, 6, 34064. [Google Scholar] [CrossRef]
- McCubrey, J.A.; LaHair, M.M.; Franklin, R.A. Reactive Oxygen Species-Induced Activation of the MAP Kinase Signaling Pathways. Antioxid Redox Sign 2006, 8, 1775–1789. [Google Scholar] [CrossRef]
- Torres, M.; Forman, H.J. Redox Signaling and the MAP Kinase Pathways. Biofactors 2003, 17, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.I.; Griendling, K.K. Nox Proteins in Signal Transduction. Free Radic. Biol. Med. 2009, 47, 1239–1253. [Google Scholar] [CrossRef] [PubMed]
- Verbon, E.H.; Post, J.A.; Boonstra, J. The Influence of Reactive Oxygen Species on Cell Cycle Progression in Mammalian Cells. Gene 2012, 511, 1–6. [Google Scholar] [CrossRef] [PubMed]
- León-Buitimea, A.; Rodríguez-Fragoso, L.; Lauer, F.T.; Bowles, H.; Thompson, T.A.; Burchiel, S.W. Ethanol-Induced Oxidative Stress Is Associated with EGF Receptor Phosphorylation in MCF-10A Cells Overexpressing CYP2E1. Toxicol. Lett. 2012, 209, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Lander, H.M.; Milbank, A.J.; Tauras, J.M.; Hajjar, D.P.; Hempstead, B.L.; Schwartz, G.D.; Kraemer, R.T.; Mirza, U.A.; Chait, B.T.; Burk, S.C.; et al. Redox Regulation of Cell Signalling. Nature 1996, 381, 380–381. [Google Scholar] [CrossRef]
- Deora, A.A.; Hajjar, D.P.; Lander, H.M. Recruitment and Activation of Raf-1 Kinase by Nitric Oxide-Activated Ras †. Biochem.-US 2000, 39, 9901–9908. [Google Scholar] [CrossRef]
- Hoyos, B.; Imam, A.; Korichneva, I.; Levi, E.; Chua, R.; Hammerling, U. Activation of C-Raf Kinase by Ultraviolet Light. J. Biol. Chem. 2002, 277, 23949–23957. [Google Scholar] [CrossRef]
- Nowak, G. Protein Kinase C-α and ERK1/2 Mediate Mitochondrial Dysfunction, Decreases in Active Na+ Transport, and Cisplatin-Induced Apoptosis in Renal Cells. J. Biol. Chem. 2002, 277, 43377–43388. [Google Scholar] [CrossRef]
- Basu, A.; Tu, H. Activation of ERK during DNA Damage-Induced Apoptosis Involves Protein Kinase Cδ. Biochem. Biophys. Res. Commun. 2005, 334, 1068–1073. [Google Scholar] [CrossRef]
- Zhou, J.-Y.; Liu, Y.; Wu, G.S. The Role of Mitogen-Activated Protein Kinase Phosphatase-1 in Oxidative Damage–Induced Cell Death. Cancer Res. 2006, 66, 4888–4894. [Google Scholar] [CrossRef]
- Moosavi, S.M.; Prabhala, P.; Ammit, A.J. Role and Regulation of MKP-1 in Airway Inflammation. Respir. Res. 2017, 18, 154. [Google Scholar] [CrossRef]
- Chiarugi, P.; Fiaschi, T.; Taddei, M.L.; Talini, D.; Giannoni, E.; Raugei, G.; Ramponi, G. Two Vicinal Cysteines Confer a Peculiar Redox Regulation to Low Molecular Weight Protein Tyrosine Phosphatase in Response to Platelet-Derived Growth Factor Receptor Stimulation. J. Biol. Chem. 2001, 276, 33478–33487. [Google Scholar] [CrossRef]
- Sugiura, R.; Toda, T.; Shuntoh, H.; Yanagida, M.; Kuno, T. Pmp1+, a Suppressor of Calcineurin Deficiency, Encodes a Novel MAP Kinase Phosphatase in Fission Yeast. EMBO J. 1998, 17, 140–148. [Google Scholar] [CrossRef]
- Unni, A.M.; Lockwood, W.W.; Zejnullahu, K.; Lee-Lin, S.-Q.; Varmus, H. Evidence That Synthetic Lethality Underlies the Mutual Exclusivity of Oncogenic KRAS and EGFR Mutations in Lung Adenocarcinoma. Elife 2015, 4, e06907. [Google Scholar] [CrossRef]
- Unni, A.M.; Harbourne, B.; Oh, M.H.; Wild, S.; Ferrarone, J.R.; Lockwood, W.W.; Varmus, H. Hyperactivation of ERK by Multiple Mechanisms Is Toxic to RTK-RAS Mutation-Driven Lung Adenocarcinoma Cells. Elife 2018, 7, e33718. [Google Scholar] [CrossRef]
- Park, J.-W.; Wollmann, G.; Urbiola, C.; Fogli, B.; Florio, T.; Geley, S.; Klimaschewski, L. Sprouty2 Enhances the Tumorigenic Potential of Glioblastoma Cells. Neuro-Oncology 2018, 20, 1044–1054. [Google Scholar] [CrossRef] [PubMed]
- Arkun, Y.; Yasemi, M. Dynamics and Control of the ERK Signaling Pathway: Sensitivity, Bistability, and Oscillations. PLoS ONE 2018, 13, e0195513. [Google Scholar] [CrossRef]
- Chen, J.-R.; Plotkin, L.I.; Aguirre, J.I.; Han, L.; Jilka, R.L.; Kousteni, S.; Bellido, T.; Manolagas, S.C. Transient Versus Sustained Phosphorylation and Nuclear Accumulation of ERKs Underlie Anti-Versus Pro-Apoptotic Effects of Estrogens. J. Biol. Chem. 2005, 280, 4632–4638. [Google Scholar] [CrossRef]
- Fehrenbacher, N.; Bastholm, L.; Kirkegaard-Sørensen, T.; Rafn, B.; Bøttzauw, T.; Nielsen, C.; Weber, E.; Shirasawa, S.; Kallunki, T.; Jäättelä, M. Sensitization to the Lysosomal Cell Death Pathway by Oncogene-Induced Down-Regulation of Lysosome-Associated Membrane Proteins 1 and 2. Cancer Res. 2008, 68, 6623–6633. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, S.; Yan, Y.; Daubert, R.A.; Han, J.; Schnellmann, R.G. ERK Promotes Hydrogen Peroxide-Induced Apoptosis through Caspase-3 Activation and Inhibition of Akt in Renal Epithelial Cells. Am. J. Physiol.-Ren. 2007, 292, F440–F447. [Google Scholar] [CrossRef]
- Zhuang, S.; Kinsey, G.R.; Yan, Y.; Han, J.; Schnellmann, R.G. Extracellular Signal-Regulated Kinase Activation Mediates Mitochondrial Dysfunction and Necrosis Induced by Hydrogen Peroxide in Renal Proximal Tubular Cells. J. Pharmacol. Exp. Ther. 2008, 325, 732–740. [Google Scholar] [CrossRef] [PubMed]
- An, H.-J.; Maeng, O.; Kang, K.-H.; Lee, J.-O.; Kim, Y.-S.; Paik, S.-G.; Lee, H. Activation of Ras Up-Regulates Pro-Apoptotic BNIP3 in Nitric Oxide-Induced Cell Death*. J. Biol. Chem. 2006, 281, 33939–33948. [Google Scholar] [CrossRef]
- Yang, R.; Piperdi, S.; Gorlick, R. Activation of the RAF/Mitogen-Activated Protein/Extracellular Signal-Regulated Kinase Kinase/Extracellular Signal-Regulated Kinase Pathway Mediates Apoptosis Induced by Chelerythrine in Osteosarcoma. Clin. Cancer Res. 2008, 14, 6396–6404. [Google Scholar] [CrossRef] [PubMed]
- Kauffmann-Zeh, A.; Rodriguez-Viciana, P.; Ulrich, E.; Gilbert, C.; Coffer, P.; Downward, J.; Evan, G. Suppression of C-Myc-Induced Apoptosis by Ras Signalling through PI(3)K and PKB. Nature 1997, 385, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.; Benchimol, S. The Involvement of MAPK Signaling Pathways in Determining the Cellular Response to P53 Activation. J. Biol. Chem. 2006, 281, 3832–3840. [Google Scholar] [CrossRef]
- Chen, C.-H.; Wang, W.-J.; Kuo, J.-C.; Tsai, H.-C.; Lin, J.-R.; Chang, Z.-F.; Chen, R.-H. Bidirectional Signals Transduced by DAPK?ERK Interaction Promote the Apoptotic Effect of DAPK. EMBO J. 2004, 24, 294–304. [Google Scholar] [CrossRef]
- Zheng, A.; Kallio, A.; Härkönen, P. Tamoxifen-Induced Rapid Death of MCF-7 Breast Cancer Cells Is Mediated via Extracellularly Signal-Regulated Kinase Signaling and Can Be Abrogated by Estrogen. Endocrinology 2007, 148, 2764–2777. [Google Scholar] [CrossRef]
- Choi, J.; Yip-Schneider, M.; Albertin, F.; Wiesenauer, C.; Wang, Y.; Schmidt, C.M. The Effect of Doxorubicin on MEK-ERK Signaling Predicts Its Efficacy in HCC. J. Surg. Res. 2008, 150, 219–226. [Google Scholar] [CrossRef]
- Bermudez, O.; Pagès, G.; Gimond, C. The Dual-Specificity MAP Kinase Phosphatases: Critical Roles in Development and Cancer. Am. J. Physiol. Cell Physiol. 2010, 299, C189–C202. [Google Scholar] [CrossRef]
- Lee, M.; Kim, S.Y.; Kim, J.; Kim, H.-S.; Kim, S.-M.; Kim, E.J. Mitogen-Activated Protein Kinase Phosphatase-1 Inhibition and Sustained Extracellular Signal-Regulated Kinase 1/2 Activation in Camptothecin-Induced Human Colon Cancer Cell Death. Cancer Biol. Ther. 2013, 14, 1007–1015. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kidger, A.M.; Rushworth, L.K.; Stellzig, J.; Davidson, J.; Bryant, C.J.; Bayley, C.; Caddye, E.; Rogers, T.; Keyse, S.M.; Caunt, C.J. Dual-Specificity Phosphatase 5 Controls the Localized Inhibition, Propagation, and Transforming Potential of ERK Signaling. Proc. Natl. Acad Sci USA 2017, 114, E317–E326. [Google Scholar] [CrossRef] [PubMed]
- Torii, S.; Nakayama, K.; Yamamoto, T.; Nishida, E. Regulatory Mechanisms and Function of ERK MAP Kinases. J. Biochem. 2004, 136, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Luttrell, L. “Location, Location, Location”: Activation and Targeting of MAP Kinases by G Protein-Coupled Receptors. J. Mol. Endocrinol. 2003, 30, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Formstecher, E.; Ramos, J.W.; Fauquet, M.; Calderwood, D.A.; Hsieh, J.C.; Canton, B.; Nguyen, X.T.; Barnier, J.V.; Camonis, J.; Ginsberg, M.H.; et al. PEA-15 Mediates Cytoplasmic Sequestration of ERK MAP Kinase. Dev. Cell 2001, 1, 239–250. [Google Scholar] [CrossRef]
- Mebratu, Y.A.; Dickey, B.F.; Evans, C.; Tesfaigzi, Y. The BH3-Only Protein Bik/Blk/Nbk Inhibits Nuclear Translocation of Activated ERK1/2 to Mediate IFNgamma-Induced Cell Death. J. Cell Biol. 2008, 183, 429–439. [Google Scholar] [CrossRef]
- Mizrak, S.C.; Renault-Mihara, F.; Párraga, M.; Bogerd, J.; van de Kant, H.J.G.; López-Casas, P.P.; Paz, M.; del Mazo, J.; de Rooij, D.G. Phosphoprotein Enriched in Astrocytes-15 Is Expressed in Mouse Testis and Protects Spermatocytes from Apoptosis. Reproduction 2007, 133, 743–751. [Google Scholar] [CrossRef]
- Hartman, M.L. Non-Apoptotic Cell Death Signaling Pathways in Melanoma. Int. J. Mol. Sci. 2020, 21, 2980. [Google Scholar] [CrossRef]
- Collado, M.; Blasco, M.A.; Serrano, M. Cellular Senescence in Cancer and Aging. Cell 2007, 130, 223–233. [Google Scholar] [CrossRef]
- Ogier-Denis, E.; Pattingre, S.; Benna, J.E.; Codogno, P. Erk1/2-Dependent Phosphorylation of Gα-Interacting Protein Stimulates Its GTPase Accelerating Activity and Autophagy in Human Colon Cancer Cells. J. Biol. Chem. 2000, 275, 39090–39095. [Google Scholar] [CrossRef]
- Pattingre, S.; Bauvy, C.; Codogno, P. Amino Acids Interfere with the ERK1/2-Dependent Control of Macroautophagy by Controlling the Activation of Raf-1 in Human Colon Cancer HT-29 Cells. J. Biol. Chem. 2003, 278, 16667–16674. [Google Scholar] [CrossRef] [PubMed]
- Ellington, A.A.; Berhow, M.A.; Singletary, K.W. Inhibition of Akt Signaling and Enhanced ERK1/2 Activity Are Involved in Induction of Macroautophagy by Triterpenoid B-Group Soyasaponins in Colon Cancer Cells. Carcinogenesis 2005, 27, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Levine, B.; Kroemer, G. Autophagy in the Pathogenesis of Disease. Cell 2008, 132, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Salazar, M.; Hernández-Tiedra, S.; Torres, S.; Lorente, M.; Guzmán, M.; Velasco, G. Detecting Autophagy in Response to ER Stress Signals in Cancer. Methods Enzym. 2011, 489, 297–317. [Google Scholar] [CrossRef]
- Li, X.; Feng, K.; Li, J.; Yu, D.; Fan, Q.; Tang, T.; Yao, X.; Wang, X. Curcumin Inhibits Apoptosis of Chondrocytes through Activation ERK1/2 Signaling Pathways Induced Autophagy. Nutrients 2017, 9, 414. [Google Scholar] [CrossRef]
- Bartholomeusz, C.; Rosen, D.; Wei, C.; Kazansky, A.; Yamasaki, F.; Takahashi, T.; Itamochi, H.; Kondo, S.; Liu, J.; Ueno, N.T. PEA-15 Induces Autophagy in Human Ovarian Cancer Cells and Is Associated with Prolonged Overall Survival. Cancer Res. 2008, 68, 9302–9310. [Google Scholar] [CrossRef]
- Kim, B.-W.; Lee, E.-R.; Min, H.-M.; Jeong, H.-S.; Ahn, J.-Y.; Kim, J.-H.; Choi, H.-Y.; Choi, H.; Kim, E.Y.; Park, S.P.; et al. Sustained ERK Activation Is Involved in the Kaempferol-Induced Apoptosis of Breast Cancer Cells and Is More Evident under 3-D Culture Condition. Cancer Biol. Ther. 2008, 7, 1080–1089. [Google Scholar] [CrossRef]
- Nguyen, T.T.T.; Tran, E.; Nguyen, T.H.; Do, P.T.; Huynh, T.H.; Huynh, H. The Role of Activated MEK-ERK Pathway in Quercetin-Induced Growth Inhibition and Apoptosis in A549 Lung Cancer Cells. Carcinogenesis 2004, 25, 647–659. [Google Scholar] [CrossRef]
- Ota, Y.; Itoh, Y.; Kaise, A.; Ohta, K.; Endo, Y.; Masuda, M.; Sowa, Y.; Sakai, T.; Suzuki, T. Targeting Cancer with PCPA-Drug Conjugates: LSD1 Inhibition-Triggered Release of 4-Hydroxytamoxifen. Angew. Chem. Int. Ed. 2016, 55, 16115–16118. [Google Scholar] [CrossRef]
| In Vivo/Cellular Model | Stimuli Inducing Cell Death | Detected Time Points of Activated ERK | Timing of Evaluating Cell Death | Characteristics of Cell Death | Evidence Implicating MEK–ERK in Cell Death | p53- Dependent | p53 Activation | ROS Induction | Reference |
|---|---|---|---|---|---|---|---|---|---|
| RPTEC/TERT1 cells, Mouse renal proximal tubular cells | Cisplatin | 72 h | 48, 72 h | Caspase-3, Bcl-2, Anneexin V, Propidium iodide (PI) | Panduratin A | no information | no information | YES | [87] |
| Nasopharyngeal carcinoma (NPC) cell line (NPC-039 and NPC-BM) | Dehydrocrenatidine | 24 h | 24 h | Caspase-3, -8, -9, Bak, Bax, Bcl-xL, Bcl-2, PARP | U0126 | no information | no information | NO | [88] |
| Human proximal tubular cell (HK-2) | Urinary proteins | 2, 8 h | 48 h | Annexin V | U0126 | no information | no information | YES | [89] |
| Mouse auditory cell line (HEI-OC1) | Cisplatin | 24 h | 24 h | Caspase-3, TUNEL, LC3-II | U0126 | no information | no information | YES | [90] |
| Human endometrial cancer (EC) cell (Ishikawa, HEC-1A) | Curcusone C | 24 h | 24 h | Caspase-3, -9 | U0126 | no information | no information | no information | [91] |
| T24 | Pterostilbene, Cisplatin, Gemcitabine | 48 h | 48 h | LC3-II, β-galactosidase (senescence) | U0126 | NO | no information | no information | [92] |
| Human non-small cell lung cancer (NSCLC) cell (A549, NCI-H292) | Morusin | 1, 2, 4, 8, 12, 24 h | 48 h | Caspase-3, PARP, LC3-II, | U0126 | no information | no information | YES | [93] |
| Human umbilical vein endothelial cells (HUVECs) | Death-domain associated protein (DAXX) and inorganic phosphate (Pi) | 1 h | 24 h | Caspase-3 | U0126 | no information | no information | no information | [94] |
| LNCaP and PC-3 cells | γ-tocotrienol (GT3) | 6 h | 12 h | Caspase-3, -9 | U0126 | no information | no information | no information | [95] |
| Human gastric cancer cell lines (SGC-7901, BGC-823) | Ginsenoside Rg5 | 24 h | 24 h | Caspase-3, -8, -9, PARP, LC3-II | U0126 | no information | no information | YES | [96] |
| A549 | Derrone (DR) | 3, 6, 12, 24 h | 24 h | Caspase-3, -8, PARP, LC3-II | U0126 | YES | no information | YES | [97] |
| Human colorectal cancer cells (HCT116 p53+/+ and p53−/−) | 6-(Methylsulfinyl)hexyl isothiocyanate (6-MSITC) | 6, 12, 18, 24, 36, 48 h | 48 h | Caspase-3, PARP | U0126 | NO | no information | no information | [98] |
| HeLa | HVJ-E infection | 24 h | 24 h | Caspase-3, -9, LC3-II | U0126 | no information | no information | no information | [99] |
| RSC96 | Mesenchymal stem cells (MSC)-derived extracellular vesicles (EVs) | 24 h | 24 h | Annexin V, Bcl-2, Bax | U0126 | no information | no information | no information | [100] |
| HL-60 | Platinum complex containing a piplartine derivative cis-[PtCl(PIP-OH)(PPh3)2]PF6 (where, PIP-OH = piplartine demethylated derivative; and PPh3 = triphenylphosphine) | no infromation | 24, 48 h | Annexin V, Caspase-3 | U0126 | no information | no information | YES | [101] |
| Non-small cell lung cancer (NSCLC) cells (H1975, A549) | M. tenacissima extract (MTE) | 24 h | 24 h | Caspase-3, PARP, LC3-II | U0126 | no information | no information | no information | [102] |
| Non-small cell lung cancer (NSCLC) cells (PC9, H1975) | Scutellarin | 48 h | 24, 48 h | Annexin V, LC3-II | U0126 | no information | no information | no information | [103] |
| Colon cancer cell lines (SW480, SW620, DLD-1) | NSC95397 | 6 h | 24 h | Caspase-3, -7, -9, PARP | U0126 | NO | no information | no information | [104] |
| Human breast cancer cell line (MDA-MB-231) | Triptolide | 2, 4, 8, 24, 48 h | 48, 72 h | Caspase-3, PARP | U0126 | no information | no information | YES | [37] |
| Human breast cancer cell (MCF-7) | Triptolide (TPI) | 24 h | 24 h | Caspase-3, LC3-II | U0126 | no information | no information | no information | [105] |
| MKN45 | Alpha, 2′-dihydroxy-4,4′-dimethoxydihydrochalcone | 48 h | 48 h | Annexin V, LC3-II | U0126 | no information | no information | YES | [106] |
| Non-small cell lung carcinoma (NSCLC) (A549, H226, H1299) | Artocarpin | 0.5, 1, 2, 3, 4 h | 6, 24 h | Caspase-3 | U0126, SB202190 | dependent and independent | YES | YES | [107] |
| Murine macrophage cell line RAW264.7 | H. pylori secreted protein HP1286 | 15, 30, 60, 90, 120 m | 24 h | Caspase-3 | U0126 | no information | no information | no information | [108] |
| HepG2 | Cholix toxin (Cholix) | 4, 8, 12 h | 12 h | Caspase-3, -9 | U0126, SB20852, SP600125 | no information | no information | YES | [109] |
| Human ovarian cancer cell lines (HEY, A2780) | Baicalein (BA) | 24 h | 24 h | LC3-II, PARP | U0126, ERK siRNA | no information | no information | no information | [110] |
| MGC-803 | Equol | 12, 24, 48 h | 24 h | Caspase-3, PARP, cIAP1 | U0126 | no information | no information | no information | [111] |
| A549 | Derivatives of 6-cinnamamido-quinoline-4-carboxamide (CiQ) | 8 h | 48 h | Caspase-9, PARP, LC3-II | U0126, dominant-negative MEK1 | NO | no information | no information | [112] |
| Human nasopharyngeal carcinoma (NPC) cell lines (HONE-1, NPC-039) | Polyphyllin G (polyphyllin VII) | 3, 6, 12 h | 24 h | Caspase-8, -3, -9, Bax, Bcl-xL, Bcl-2, LC3-II | U0126 | no information | no information | no information | [113] |
| 253J-Bv, T24 | Co-treatment of curcumin and cisplatin | 3, 6, 24 h | 24 h | Caspase-3, Anneexin V | U0126 | dependent and independent | YES | YES | [114] |
| Burkitt’s lymphoma Ramos cells | MytiLec | 12, 24 h | 24 h | Caspase-3, -9, Annexin V | U0126 | no information | no information | no information | [115] |
| Human umbilical vein endothelial cells (HUVECs) (SGC7901) | farrerol | 24 h | 24 h | G0/G1 cell cycle arrest | U0126 | no information | no information | no information | [116] |
| Osteoblasts (OBs) | Cadmium (Cd) | 2, 3, 4, 5, 6 h | 24 h | Bax, Bcl-2, Caspase-3, -9, PARP | U0126 | no information | no information | Decrease in ROS generation | [117] |
| HCT116 | Physalin B | 12, 24, 36 h | 24 h | Caspase-3, PARP, LC3-II | U0126 | no information | no information | YES | [118] |
| NIH/3T3 | Paraquat | 0.5, 1, 6, 12, 24 h | 24 h | Cytochrome c | U0126 | no information | no information | YES | [119] |
| Breast cancer cell lines (MCF-7, BT474, MDA-MB-231, SUM1315) | D Rhamnose β-hederin (DRβ-H) | 5, 30 m, 2, 6, 48 h | 48 h | Annexin V, caspase-3, -8, -9 | U0126 | no information | no information | no information | [120] |
| A549 | Pyocyanin (PCN) | 5 m, 1, 3, 6, 12, 24 h | 24 h | Caspase-3 | U0126 | no information | no information | YES | [121] |
| Mouse TM4 Sertoli cells | Nonylphenol (NP) | 15, 30, 60, 180 m | 24 h | Sub G1, Caspase-3, PARP, Bcl-2, Bax | U0126 | no information | no information | YES | [122] |
| HT-29 | Piperlongumine (PPLGM) | 5, 10, 15, 30, 60 m | 24 h | Caspase-3 | U0126 | no information | no information | no information | [16] |
| BRL 3A | Cadmium (Cd) | 12 h | 12 h | Annexin V, Bax, Bcl-2 | U0126 | no information | no information | YES | [123] |
| Rat liver cells | Corticotrophin-releasing hormone (CRH) | 8 h | 8, 24 h | Bax, Bcl-2 | U0126 | no information | YES | no information | [124] |
| MDA-MB-468 | Allyl isothiocyanate (AITC) | 2 h | 12 h | Caspase-3, -9, Bcl-2, Cytochrome c | U0126 | NO | NO | YES | [125] |
| Mouse embryonic stem (mES) cells | Sodium nitroprusside (SNP) | 4, 8, 12, 24 h | 24 h | Caspase-3, -8, -9, Annexin V | U0126 | no information | no information | YES | [126] |
| SGC-7901 | β,β-Dimethylacrylshikonin | 2, 4, 8, 12, 24 h | 48 h | Caspase-3, -8, -9, Bax, Bcl-xL, Bcl-2, PARP, Cytochrome c | U0126 | no information | no information | no information | [127] |
| H9c2 | Cyclosporine A (CsA) | 0.25, 0.5, 1, 4, 8, 12, 24 h | 4 h | Caspase-3, Bax, Bcl-2, Annexin V, TUNEL | U0126 | no information | no information | no information | [128] |
| Breast cancer cell lines (MDA-MB-231, KPL-3C) | Olaparib | 1, 12 h | 12, 24 h | Annexin V | U0126 | no information | no information | no information | [129] |
| Jurkat/NTAL(+) | Methylprednisolone | 5, 30 m | 24 h | Annexin V, Propidium iodide (PI) | U0126 | no information | no information | no information | [130] |
| Jurkat | Phorbol myristate acetate (PMA) | 24 h | 16, 24 h | DNA fragmentation | U0126, PD98059 | no information | no information | no information | [131] |
| Head kidney macrophage (HKM) | Arsenic | 24 h | 24 h | Caspase-3 | U0126 | no information | no information | YES | [132] |
| LLC-PK1 | Cysteinyl leukotrienes (cysLTs) synthesis | 0.5, 1, 3, 6, 12, 24 h | 24 h | Caspase-3, Bax, Bcl-2, Cytochrome C | U0126 | no information | no information | no information | [133] |
| HeLa | Phenethyl isothiocyanate (PEITC) | 8, 24 h | 24 h | Caspase-3, PARP | U0126 | no information | no information | no information | [134] |
| Human lung adenocarcinoma A549 | Pemetrexed | 4, 8, 12, 24, 48 h | 72 h | Caspase-3, TUNEL | U0126, PD98059, ERK siRNA | no information | no information | no information | [135] |
| Human endometrial cancer Hec1A | Icaritin | 3, 6, 12, 24 h | 24 h | Caspase-3, -9, PARP, Cytochrome c, TUNEL, Annexin V | U0126 | no information | no information | no information | [23] |
| Breast cancer MDA-MB-453 and MCF7 | Icaritin | 5, 15, 30 m, 1, 2, 4, 8, 12, 24 h | 48 h | Bcl-2, PARP, Annexin V | U0126 | no information | no information | no information | [136] |
| Renal tubular epithelial cell (RTEC) | HIV-1 viral protein r (Vpr) | 5 d | 5 d | Caspase-3, -8, -9, PARP | U0126 | no information | no information | no information | [137] |
| Spinal cord | Spinal cord ischemia/Reperfusion (I/R) injury | 3 h | 24 h | Caspase-3, TUNEL, c-IAP2 | U0126 | no information | no information | no information | [138] |
| HL-60, U397, SK-MEL-1 | Asteriscunolide A (AS) | 0.5, 1, 2, 3 h | 24 h | Caspase-3, -7, -9, PARP | U0126, PD98059 | no information | no information | YES | [139] |
| Astrocytes | Glutamate | 3, 6, 9 h | 24 h | Caspase-3, TUNEL | U0126, DUSP5, 6 over-expression | no information | no information | no information | [82] |
| Neuro-2a | 4-Methyl-2,4-bis(4-hydroxyphenyl)pent-1-ene (MBP) | 0.5, 1, 2, 4, 6, 8 h | 24 h | Sub-G1, Caspase-3, -7, -9, -12, Bax, Bcl-2, PARP, Cytochrome c | PD98059 | no information | no information | no information | [140] |
| Human platelets | Bisdemethoxycurcumin (BDMC) | 1, 2 h | 1 h | Caspase-3, -8, -9, Bax, BID, Bcl-2, Bcl-xL, Cytochrome c | PD98059 | no information | no information | YES | [141] |
| HeLa, MCF-7 | N-Methyl and N,N-dimethyl bis(indolyl)hydrazide-hydrazone analog derivatives | no information | 24 h | Bak | PD98059 | YES | YES | YES | [142] |
| Human ovary adenocarcinoma (SKOV3) | CRT1 (Ent-18-acetoxy-7β-hydroxy kaur-15-oxo-16-ene) | 24 h | 24 h | Caspase-3, -7, -9, PARP, Cytochrome c, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [143] |
| Human pulmonary microvascular endothelial cells (HPMECs) | Cigarette smoke extract (CSE) | 12 h | 12 h | Caspase-3, TUNEL, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [144] |
| Hepatocellular carcinoma (HCC) (SMMC7721, Bel7402) | Hispidulin | 48 h | 48 h | Caspase-3, Bax, Bcl-2, Annexin V, Propidium iodide (PI), TUNEL | PD98059 | no information | no information | no information | [145] |
| Human osteosarcoma cells (HOS) | Honokiol (HNK) | 24 h | 24 h | Caspase-3, -9, Bcl-2, Bcl-xL, survivin, PARP, Annexin V, Propidium iodide (PI), TUNEL | PD98059 | no information | no information | YES | [146] |
| Human hepatoma (Hep3B) | Desipramine | 1, 2, 4, 8 h | 24 h | LDH | PD98059 | no information | no information | YES | [147] |
| Human neuroblastoma (SH-SY5Y) | Cearoin | 12 h | 12 h | Caspase-3, Bax, Bcl-2, PARP | PD98059 | no information | no information | YES | [148] |
| Human Glioma (U87) | Valproic acid (VPA) | 72 h | 72 h | Hoechst 33342, Caspase-3, -9, Bax, Bcl-2, Cytochrome c, TUNEL, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [149] |
| Human gastric cancer cells (AGS) | Agrimonolide (AM) | 24 h | 24 h | Caspase-3, -8, -9, Bax, Bcl-2, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | YES | [150] |
| β-cell-derived cells (RIN-m5F) | Etoposide | 15, 30, 60 m | 24 h | SubG1, Caspase-3, -6, -7, -9, Cytochrome c, Bax, Bcl-2, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [19] |
| HT-29 | Simvastatin | 24 h | 48 h | Caspase-3, Bax, Bcl-2 | PD98059 | no information | no information | no information | [151] |
| Ardiac myocytes (H9c2) | Doxorubicin (DOX) | 2, 6, 12, 24, 48 h | 24 h, 48 h | TUNEL, Annexin V, Propidium iodide (PI) | PD98059, ERK siRNA | YES | YES | no information | [152] |
| RAW 264.7 cells | Cypermethrin | 15, 30 m | 48 h | Annexin V, Propidium iodide (PI) | PD98059 | no information | YES | YES | [153] |
| Male Sprague–Dawley rats, Primary hippocampal neuron cells | Early brain injury (EBI) following subarachnoid hemorrhage (SAH), oxyhemoglobin (OxyHb) | 6, 12, 24, 48 h | 24 h | Caspase-3, -8, -9, PARP, TUNEL | PD98059 | YES | YES | YES | [154] |
| Neuroblastoma cells (neuro-2a) | Honokiol (HNK) | 48, 72 h | 72 h | BrdU | PD98059 | no information | no information | YES | [155] |
| Human extravillous cytotrophoblast (EVCT)-derived cells (HTR-8/SVneo, HPT-8) | Coplanar polychlorinated biphenyls (Co-PCBs) | 24 h | 24 h | Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [156] |
| Human multiple myeloma (MM) cells (U266) | Cinobufagin (CBG) | 3 h | 24 h | Caspase-3, Bcl-xL, Bcl-2, PARP, Survivin, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | YES | [157] |
| Lung adenocarcinoma cells (A549) | Triptolide (TP)/Hydroxycamptothecin (HCPT) | 24 h | 24 h | Caspase-3, -9, Cytochrome c, Bax, Bcl-2, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [158] |
| Human leukemia cells (HL-60) | Bromo analogue (TBr) | 6, 12, 24 h | 24 h | Caspase-3, -8, -9, PARP, Bax, BID, Bcl-2, Sub-G1, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [159] |
| Human alveolar cells (A549) | Acetochlor (ACETO) | 6, 12, 24, 48 h | 72 h | Caspase-3, -9, PARP, Bak, Bax, BID, Bad, MCL-1, Bcl-xL, Bcl-2, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | YES | [160] |
| PC12 | Perfluorohexanesulfonate (PFHxS) | 0.5, 1, 3, 6, 9, 16, 24 h | 24 h | Caspase-3, Propidium iodide (PI), TUNEL | PD98059 | no information | no information | YES | [161] |
| Prostate cancer cells (PC3) | MHY-449 | 24 h | 24 h | Caspase-3, -8, Bax, Bcl-2, PARP, Annexin V, Propidium iodide (PI) | PD98059 | NO | no information | no information | [162] |
| Neuro-2a | As2O3 | 15, 30, 60 m | 24 h | Caspase-3, -6, -7, -9, -12, PARP, Bax, Bcl-2, | PD98059 | no information | no information | YES | [163] |
| Gastric cancer cells (SGC7901, MGC803) | Interferon-α (IFN-α)/5’-Deoxy-5-fluorouracil (5’-DFUR) | 24, 48 h | 24 h, 48 h | Caspase-3, -9, PARP | PD98059, ERK siRNA | no information | no information | no information | [164] |
| Osteosarcoma cells (G292) | Capsaicin | 2, 6 h | 24 h | Caspase-9, Annexin-V | PD98059 | no information | no information | no information | [165] |
| Rat chondrocyte | Mechanical stress (0.5 MPa) | 24 h | 24 h | Caspase-3, -9, Bax, Bcl-2, Annexin V, Propidium iodide (PI), TUNEL | PD98059 | no information | no information | no information | [166] |
| Leukemia cells (KBM-5) | Tanshinone IIA (Tan IIA) | 6, 12, 18, 24 h | 24 h | Sub-G1, PARP | PD184352 | no information | no information | no information | [85] |
| Rat hepatic stellate cell (HSC-T6) | Tanshinone IIA (Tan IIA) | 6 h | 24 h | Sub-G1, Caspase-3, -9, PARP, Bax, Bcl-2 | PD98059 | no information | no information | YES | [167] |
| Cerebellar granule cells (CGCs) | Perfluorooctane sulfonate (PFOS) | 5, 10, 15, 30 m, 1, 3, 6 h | 24 h | Hoechst 33342, Caspase-3 | PD98059 | no information | no information | no information | [168] |
| Human oral squamous cell carcinomas (YD-10B) | Fomitoside-K | 4, 8, 12, 24 h | 24 h | Caspase-3, -9, PARP, Bax, Bcl-2, Survivin, Propidium iodide (PI) | PD98059 | no information | no information | YES | [169] |
| Human myeloid leukemia cells (K562) | Calactin | 6, 12, 24 h | 12 h, 24 h | Caspase-3, -8, Caspase-9, Bax, Bcl-2, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [170] |
| Human gastric cancer cells (CS12) | Euphol | 4, 24, 48, 72 h | 48 h, 72 h | Caspase-3, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [171] |
| Human oral squamous cell carcinoma (OSCC) cells (YD-8) | P. densiflora leaf essential oil (PLEO) | 4, 8 h | 8 h | Caspase-9, PARP, Bax, Bcl-2 | PD98059 | no information | no information | YES | [172] |
| Osteoblasts (Saos-2) | CdCl2 | 3, 4, 18 h | 48 h, 72 h | APO Percentage dye | PD98059 | no information | no information | no information | [173] |
| Human hepatoma (HepG2) | ZL11n | 24 h | 24 h | Caspase-3, Bax, Bcl-2, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [174] |
| Amygdala region in SPS rats | Single-prolonged stress (SPS) | 1 h | 1 h, 7 d | Bax, Bcl-2, TUNEL | PD98059 | no information | no information | no information | [175] |
| Human myeloid leukemia cells (K562) | Ormeloxifen (ORM) | 1, 3, 6, 24 h | 48 h | Caspase-3, -9, Bax, Bcl-2, Annexin V, Propidium iodide (PI), TUNEL | PD98059 | no information | no information | no information | [176] |
| HK-2 | Cyclosporine A (CyA) | 1, 3, 6, 24 h | 24 h | Hoechst 33258 | PD98059 | no information | no information | no information | [177] |
| PC12 | Parathyroid hormone (PTH) | 24, 48, 72 h | 24, 48, 72, 96 h | Caspase-3, Propidium iodide (PI), DNA ladder | PD98059 | no information | no information | no information | [178] |
| HCT116 | Qizhen capsule (QZC) | 15, 30, 60 m | 24 h, 48 h | Caspase-3, -9, Bax, Bcl-2, PARP, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | no information | [179] |
| Human melanoma cells (A375SM), mouse xenograft model | Shikonin | 24 h | 24 h | Bax, Bcl-2, PARP, Annexin V, propidium iodide (PI), TUNEL | no information | no information | no information | no information | [180] |
| Rat hepatocytes | Di-(2-ethylhexyl)phthalate (DEHP) | 24 h | 24 h | Caspase-3, PARP, Bad, Bax, Bcl-2, Bcl-xL, Annexin V, Propidium iodide (PI) | PD98059 | no information | no information | YES (ROS independent) | [181] |
| Human leukemia cell line (K562) | Prodigiosin | 48 h | 24, 48 h | Caspase-3, -8, -9, Annexin V, LC-3 | PD184352 | no information | no information | YES | [86] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sugiura, R.; Satoh, R.; Takasaki, T. ERK: A Double-Edged Sword in Cancer. ERK-Dependent Apoptosis as a Potential Therapeutic Strategy for Cancer. Cells 2021, 10, 2509. https://doi.org/10.3390/cells10102509
Sugiura R, Satoh R, Takasaki T. ERK: A Double-Edged Sword in Cancer. ERK-Dependent Apoptosis as a Potential Therapeutic Strategy for Cancer. Cells. 2021; 10(10):2509. https://doi.org/10.3390/cells10102509
Chicago/Turabian StyleSugiura, Reiko, Ryosuke Satoh, and Teruaki Takasaki. 2021. "ERK: A Double-Edged Sword in Cancer. ERK-Dependent Apoptosis as a Potential Therapeutic Strategy for Cancer" Cells 10, no. 10: 2509. https://doi.org/10.3390/cells10102509
APA StyleSugiura, R., Satoh, R., & Takasaki, T. (2021). ERK: A Double-Edged Sword in Cancer. ERK-Dependent Apoptosis as a Potential Therapeutic Strategy for Cancer. Cells, 10(10), 2509. https://doi.org/10.3390/cells10102509






