The New Kid on the Block: HLA-C, a Key Regulator of Natural Killer Cells in Viral Immunity
Abstract
1. Introduction
2. Structure, Expression, and Regulation of HLA-C
3. Regulation of NK Cells by HLA-C
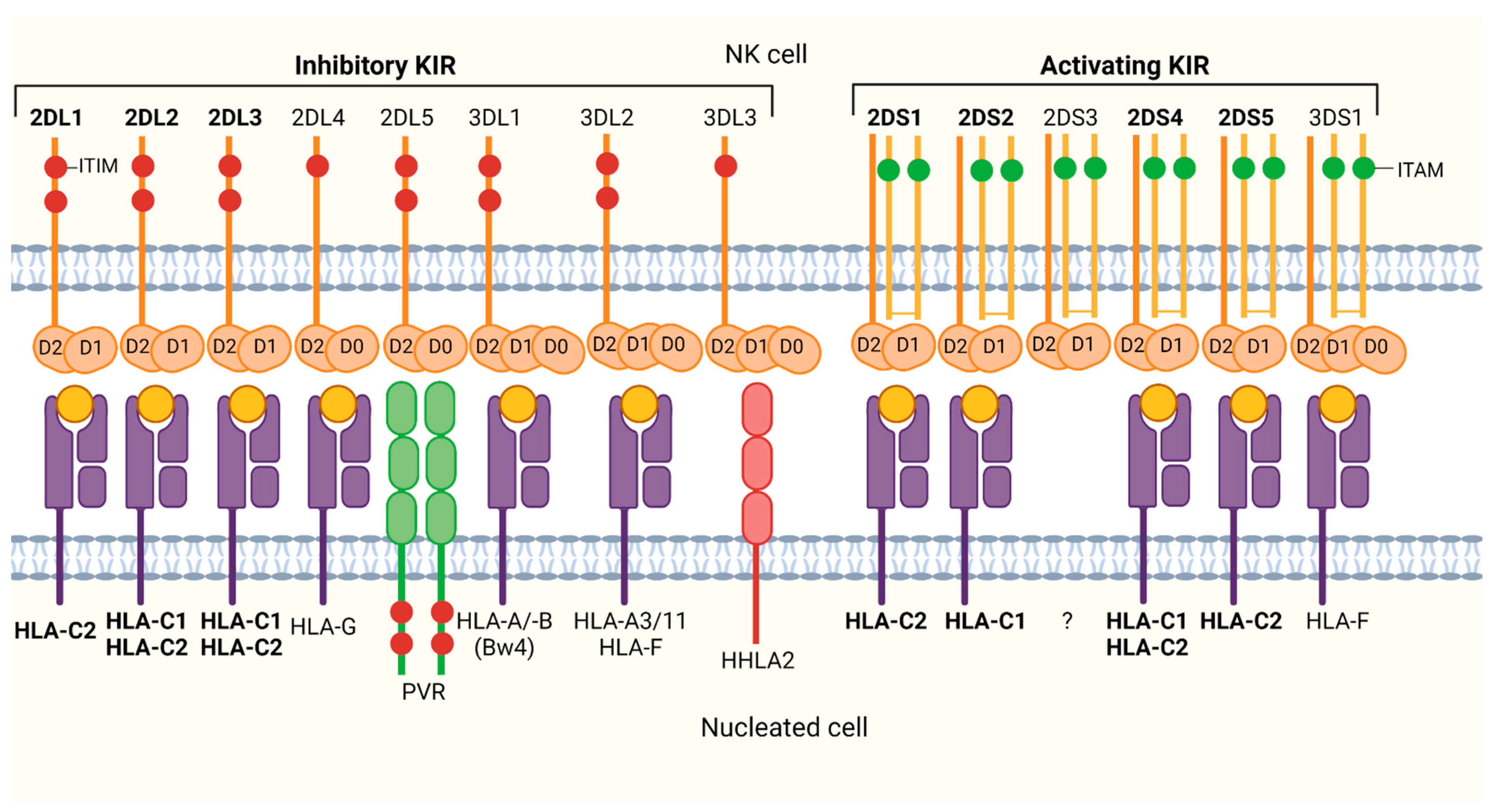
3.1. Killer-Cell Immunoglobulin-Like Receptors (KIRs) Recognize HLA-C
3.2. Appearance of HLA-C Triggered Rapid Co-Evolution of HLA-C Recognizing KIRs
3.3. HLA-C Regulates NK Cell Activity through Inhibitory KIRs
4. HLA-C-Mediated Impact of Viral Immune Response
4.1. Human Immunodeficiency Virus (HIV)
4.2. Hepatitis C Virus (HCV)
4.3. Human Cytomegaloviruses (CMV)
| Mechanism/Observation | Virus | Reference |
|---|---|---|
| KIR/HLA-C disease association | ||
| High HLA-C expression is associated with HIV-1 control | HIV-1 | [115,121,122,123] |
| KIR2DL3/HLA-C1 combination is associated with severe HIV-1 clinical outcome | HIV-1 | [131,132,133] |
| KIR2DL3/HLA-C1 combination is associated with HIV-1 protection | HIV-1 | [134,135] |
| Homozygous KIR2DL3/HLA-C1 combination is associated with spontaneous HCV resolution and better treatment response | HCV | [20,149,152,153] |
| Higher frequency of KIR2DL2/HLA-C1 in chronic HCV infection | HCV | [154] |
| Higher frequency of KIR2DL3 and low frequency of KIR2DL2 in persistent HCV infection | HCV | [3] |
| Increased frequency of C2/C2 in spontaneous HCV clearance | HCV/HIV-1 | [156] |
| Higher frequency of KIR2DS3/HLA-C2 in HCV resolution | HCV | [157] |
| Combination of KIR2DL2/HLA-C1 is a risk factor for chronic HCV infecton and associated with no treatment response | HCV | [159] |
| Homozygous KIR2DL3/HLA-C1 is associated with chronic HCV infection, higher frequency of KIR2DL2, KIR2DS2 and KIR2DL2/L3 in HCV clearance | HCV | [142] |
| Alterations of NK cell repertoire | ||
| Reactivation of CMV in patients with hemaotopoietic stem cell transplantation leads to expansion of NKG2C+ KIR+ NK cells | CMV | [165] |
| Healthy CMV-infected individuals have a stable imprint in the KIR repertoire with a bias for inhibitory KIRs specific for self HLA-C | CMV | [167] |
| Increased expression of KIR2DL1 in NKG2C+ NK cells in CMV infection | CMV | [168,170] |
| Mature CD56dimNKG2A-KIR+CD57+ NK cells of seropositive CMV donors highly express PD-1 | CMV | [166] |
| Antiviral activity of NK cells | ||
| KIR2DL1-3+ NK cells sense changes in HLA-C expression by increased antiviral activity | HIV-1 | [141] |
| Virus-mediated modulation of HLA-C | ||
| HIV-1 Vpu mediates HLA-C downmodulation | HIV-1 | [140,143] |
| HIV-2 Vif mediates HLA-C downmodulation | HIV-1 | [143] |
| Downmodulation of HLA-C by various CMV proteins | CMV | [176,177,180,181] |
| Selection of viral peptides | ||
| KIR2DL2-associated HIV-1 sequence polymorphisms modulate NK cell function | HIV-1 | [83] |
| HLA-C*0102-restricted HIV-1 p24 Gag epitopes modulates KIR2DL2 binding | HIV-1 | [145] |
| Sequence polymorphismus in HIV-1 p24 Gag modulates binding of KIR2DL2/3 to HLA-C*0304 | HIV-1 | [19,146] |
| Reduced expression of HIV-1-derived peptides and HLA-C*1403 and HLA-C*1202 | HIV-1 | [130] |
| HIV-1-derived peptides reduce binding of HLA-C*0304 to KIR2DL3 | HIV-1 | [147] |
| Presentation of HCV core protein by HLA-C*0304 results in inhibition of KIR2DL3+ NK cells | HCV | [163] |

4.4. Other Viruses
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Peakman, M.; Vergani, D. Basic and Clinical Immunology; Churchill Livingstone: London, UK, 2009. [Google Scholar]
- Turner, D. The human leucocyte antigen (HLA) system. Vox Sang. 2004, 87 (Suppl. 1), 87–90. [Google Scholar] [CrossRef]
- Martin, M.P.; Carrington, M. Immunogenetics of viral infections. Curr. Opin. Immunol. 2005, 17, 510–516. [Google Scholar] [CrossRef]
- Simmonds, M.; Gough, S. The HLA Region and Autoimmune Disease: Associations and Mechanisms of Action. Curr. Genomics 2009, 8, 453–465. [Google Scholar] [CrossRef]
- Shukla, S.A.; Rooney, M.S.; Rajasagi, M.; Tiao, G.; Dixon, P.M.; Lawrence, M.S.; Stevens, J.; Lane, W.J.; Dellagatta, J.L.; Steelman, S.; et al. Comprehensive analysis of cancer-associated somatic mutations in class I HLA genes. Nat. Biotechnol. 2015, 33, 1152–1158. [Google Scholar] [CrossRef]
- Claas, F.H.; Duquesnoy, R.J. The polymorphic alloimmune response in clinical transplantation. Curr. Opin. Immunol. 2008, 20, 566–567. [Google Scholar] [CrossRef]
- Jin, K.; Ho, H.N.; Speed, T.P.; Gill, T.J., 3rd. Reproductive failure and the major histocompatibility complex. Am. J. Hum. Genet. 1995, 56, 1456–1467. [Google Scholar]
- Ljunggren, H.G.; Kärre, K. In search of the “missing self”: MHC molecules and NK cell recognition. Immunol. Today 1990, 11, 237–244. [Google Scholar] [CrossRef]
- Kulski, J.K.; Gaudieri, S.; Bellgard, M.; Balmer, L.; Giles, K.; Inoko, H.; Dawkins, R.L. The Evolution of MHC Diversity by Segmental Duplication and Transposition of Retroelements. J. Mol. Evol. 1997, 45, 599–609. [Google Scholar] [CrossRef]
- Parham, P.; Abi-Rached, L.; Matevosyan, L.; Moesta, A.K.; Norman, P.J.; Older Aguilar, A.M.; Guethlein, L.A. Primate-specific regulation of natural killer cells. J. Med. Primatol. 2010, 39, 194–212. [Google Scholar] [CrossRef]
- Papúchová, H.; Meissner, T.B.; Li, Q.; Strominger, J.L.; Tilburgs, T. The Dual Role of HLA-C in Tolerance and Immunity at the Maternal-Fetal Interface. Front. Immunol. 2019, 10, 2730. [Google Scholar] [CrossRef]
- Apps, R.; Meng, Z.; Del Prete, G.Q.; Lifson, J.D.; Zhou, M.; Carrington, M. Relative Expression Levels of the HLA Class-I Proteins in Normal and HIV-Infected Cells. J. Immunol. 2015, 194, 3594–3600. [Google Scholar] [CrossRef]
- Falk, C.S.; Schendel, D.J. HLA-C revisited. Ten years of change. Immunol. Res. 1997, 16, 203–214. [Google Scholar] [CrossRef]
- Colonna, M.; Borsellino, G.; Falco, M.; Ferrara, G.B.; Strominger, J.L. HLA-C is the inhibitory ligand that determines dominant resistance to lysis by NK1- and NK2-specific natural killer cells. Proc. Natl. Acad. Sci. USA 1993, 90, 12000–12004. [Google Scholar] [CrossRef] [PubMed]
- Valiante, N.M.; Uhrberg, M.; Shilling, H.G.; Lienert-Weidenbach, K.; Arnett, K.L.; D’Andrea, A.; Phillips, J.H.; Lanier, L.L.; Parham, P. Functionally and structurally distinct NK cell receptor repertoires in the peripheral blood of two human donors. Immunity 1997, 7, 739–751. [Google Scholar] [CrossRef]
- Ferlazzo, G.; Thomas, D.; Lin, S.-L.; Goodman, K.; Morandi, B.; Muller, W.A.; Moretta, A.; Münz, C. The Abundant NK Cells in Human Secondary Lymphoid Tissues Require Activation to Express Killer Cell Ig-Like Receptors and Become Cytolytic. J. Immunol. 2004, 172, 1455–1462. [Google Scholar] [CrossRef]
- Uhrberg, M.; Valiante, N.M.; Shum, B.P.; Shilling, H.G.; Lienert-Weidenbach, K.; Corliss, B.; Tyan, D.; Lanier, L.L.; Parham, P. Human diversity in killer cell inhibitory receptor genes. Immunity 1997, 7, 753–763. [Google Scholar] [CrossRef]
- Parham, P.; Moffett, A. Variable NK cell receptors and their MHC class I ligands in immunity, reproduction and human evolution. Nat. Rev. Immunol. 2013, 13, 133–144. [Google Scholar] [CrossRef]
- Hölzemer, A.; Thobakgale, C.F.; Jimenez Cruz, C.A.; Garcia-Beltran, W.F.; Carlson, J.M.; van Teijlingen, N.H.; Mann, J.K.; Jaggernath, M.; Kang, S.G.; Körner, C.; et al. Selection of an HLA-C*03:04-Restricted HIV-1 p24 Gag Sequence Variant Is Associated with Viral Escape from KIR2DL3+ Natural Killer Cells: Data from an Observational Cohort in South Africa. PLoS Med. 2015, 12, e1001900. [Google Scholar] [CrossRef]
- Khakoo, S.I.; Thio, C.L.; Martin, M.P.; Brooks, C.R.; Gao, X.; Astemborski, J.; Cheng, J.; Goedert, J.J.; Vlahov, D.; Hilgartner, M.; et al. HLA and NK cell inhibitory receptor genes in resolving hepatitis C virus infection. Science 2004, 305, 872–874. [Google Scholar] [CrossRef] [PubMed]
- Wauquier, N.; Petitdemange, C.; Tarantino, N.; Maucourant, C.; Coomber, M.; Lungay, V.; Bangura, J.; Debré, P.; Vieillard, V. HLA-C-restricted viral epitopes are associated with an escape mechanism from KIR2DL2 + NK cells in Lassa virus infection. EBioMedicine 2019, 40, 605–613. [Google Scholar] [CrossRef]
- Łuszczek, W.; Mańczak, M.; Cisło, M.; Nockowski, P.; Wiśniewski, A.; Jasek, M.; Kuśnierczyk, P. Gene for the activating natural killer cell receptor, KIR2DS1, is associated with susceptibility to psoriasis vulgaris. Hum. Immunol. 2004, 65, 758–766. [Google Scholar] [CrossRef]
- Snary, D.; Barnstable, C.J.; Bodmer, W.F.; Crumpton, M.J. Molecular structure of human histocompatibility antigens: The HLA-C series. Eur. J. Immunol. 1977, 7, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Van den Elsen, P.J.; Peijnenburg, A.; van Eggermond, M.C.; Gobin, S.J. Shared regulatory elements in the promoters of MHC class I and class II genes. Immunol. Today 1998, 19, 308–312. [Google Scholar] [CrossRef]
- Meissner, T.B.; Liu, Y.-J.; Lee, K.-H.; Li, A.; Biswas, A.; van Eggermond, M.C.J.A.; van den Elsen, P.J.; Kobayashi, K.S. NLRC5 Cooperates with the RFX Transcription Factor Complex to Induce MHC Class I Gene Expression. J. Immunol. 2012, 188, 4951–4958. [Google Scholar] [CrossRef]
- Gobin, S.J.; Peijnenburg, A.; Keijsers, V.; van den Elsen, P.J. Site α Is Crucial for Two Routes of IFNγ-Induced MHC Class I Transactivation: The ISRE-Mediated Route and a Novel Pathway Involving CIITA. Immunity 1997, 6, 601–611. [Google Scholar] [CrossRef]
- Schoneich, J.; Lee, J.L.; Mansky, P.; Sheffery, M.; Yang, S.Y. The pentanucleotide ATTGG, the “inverted CCAAT,” is an essential element for HLA class I gene transcription. J. Immunol. 1997, 158, 4788–4796. [Google Scholar]
- Meissner, T.B.; Li, A.; Biswas, A.; Lee, K.-H.; Liu, Y.-J.; Bayir, E.; Iliopoulos, D.; van den Elsen, P.J.; Kobayashi, K.S. NLR family member NLRC5 is a transcriptional regulator of MHC class I genes. Proc. Natl. Acad. Sci. USA 2010, 107, 13794–13799. [Google Scholar] [CrossRef]
- Ludigs, K.; Seguín-Estévez, Q.; Lemeille, S.; Ferrero, I.; Rota, G.; Chelbi, S.; Mattmann, C.; MacDonald, H.R.; Reith, W.; Guarda, G. NLRC5 exclusively transactivates MHC class I and related genes through a distinctive SXY module. PLoS Genet. 2015, 11, e1005088. [Google Scholar] [CrossRef]
- Gobin, S.J.; Keijsers, V.; van Zutphen, M.; van den Elsen, P.J. The role of enhancer A in the locus-specific transactivation of classical and nonclassical HLA class I genes by nuclear factor kappa B. J. Immunol. 1998, 161, 2276–2283. [Google Scholar]
- Carey, B.S.; Poulton, K.V.; Poles, A. Factors affecting HLA expression: A review. Int. J. Immunogenet. 2019, 46, 307–320. [Google Scholar] [CrossRef]
- Girdlestone, J.; Isamat, M.; Gewert, D.; Milstein, C. Transcriptional regulation of HLA-A and -B: Differential binding of members of the Rel and IRF families of transcription factors. Proc. Natl. Acad. Sci. USA 1993, 90, 11568–11572. [Google Scholar] [CrossRef]
- Johnson, D.R.; Pober, J.S. HLA class I heavy-chain gene promoter elements mediating synergy between tumor necrosis factor and interferons. Mol. Cell. Biol. 1994, 14, 1322–1332. [Google Scholar] [CrossRef]
- Davis, M.M.; Bjorkman, P.J. T-cell antigen receptor genes and T-cell recognition. Nature 1988, 334, 395–402. [Google Scholar] [CrossRef]
- Salter, R.D.; Benjamin, R.J.; Wesley, P.K.; Buxton, S.E.; Garrett, T.P.; Clayberger, C.; Krensky, A.M.; Norment, A.M.; Littman, D.R.; Parham, P. A binding site for the T-cell co-receptor CD8 on the alpha 3 domain of HLA-A2. Nature 1990, 345, 41–46. [Google Scholar] [CrossRef]
- Higgins, C.F. ABC Transporters: From Microorganisms to Man. Annu. Rev. Cell Biol. 1992, 8, 67–113. [Google Scholar] [CrossRef]
- Cresswell, P.; Bangia, N.; Dick, T.; Diedrich, G. The nature of the MHC class I peptide loading complex. Immunol. Rev. 1999, 172, 21–28. [Google Scholar] [CrossRef]
- Degen, E.; Williams, D.B. Participation of a novel 88-kD protein in the biogenesis of murine class I histocompatibility molecules. J. Cell Biol. 1991, 112, 1099–1115. [Google Scholar] [CrossRef]
- Hochstenbach, F.; David, V.; Watkins, S.; Brenner, M.B. Endoplasmic reticulum resident protein of 90 kilodaltons associates with the T- and B-cell antigen receptors and major histocompatibility complex antigens during their assembly. Proc. Natl. Acad. Sci. USA 1992, 89, 4734–4738. [Google Scholar] [CrossRef]
- Farmery, M.R.; Allen, S.; Allen, A.J.; Bulleid, N.J. The role of ERp57 in disulfide bond formation during the assembly of major histocompatibility complex class I in a synchronized semipermeabilized cell translation system. J. Biol. Chem. 2000, 275, 14933–14938. [Google Scholar] [CrossRef]
- Pamer, E.; Cresswell, P. Mechanisms of mhc class I–restricted antigen processing. Annu. Rev. Immunol. 1998, 16, 323–358. [Google Scholar] [CrossRef]
- Williams, A.; Peh, C.A.; Elliott, T. The cell biology of MHC class I antigen presentation. Tissue Antigens 2002, 59, 3–17. [Google Scholar] [CrossRef]
- Neefjes, J.J.; Ploegh, H.L. Allele and locus-specific differences in cell surface expression and the association of HLA class I heavy chain with β2-microglobulin: Differential effects of inhibition of glycosylation on class I subunit association. Eur. J. Immunol. 1988, 18, 801–810. [Google Scholar] [CrossRef]
- McCutcheon, J.A.; Gumperz, J.; Smith, K.D.; Lutz, C.T.; Parham, P. Low HLA-C expression at cell surfaces correlates with increased turnover of heavy chain mRNA. J. Exp. Med. 1995, 181, 2085–2095. [Google Scholar] [CrossRef]
- Johnson, D.R. Differential expression of human major histocompatibility class I loci: HLA-A, -B, and -C. Hum. Immunol. 2000, 61, 389–396. [Google Scholar] [CrossRef]
- Johnson, D.R. Locus-Specific Constitutive and Cytokine-Induced HLA Class I Gene Expression. J. Immunol. 2003, 170, 1894–1902. [Google Scholar] [CrossRef]
- Vince, N.; Li, H.; Ramsuran, V.; Naranbhai, V.; Duh, F.M.; Fairfax, B.P.; Saleh, B.; Knight, J.C.; Anderson, S.K.; Carrington, M. HLA-C Level Is Regulated by a Polymorphic Oct1 Binding Site in the HLA-C Promoter Region. Am. J. Hum. Genet. 2016, 99, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.; Savan, R.; Qi, Y.; Gao, X.; Yuki, Y.; Bass, S.E.; Martin, M.P.; Hunt, P.; Deeks, S.G.; Telenti, A.; et al. Differential microRNA regulation of HLA-C expression and its association with HIV control. Nature 2011, 472, 495–498. [Google Scholar] [CrossRef]
- Neisig, A.; Melief, C.J.; Neefjes, J. Reduced cell surface expression of HLA-C molecules correlates with restricted peptide binding and stable TAP interaction. J. Immunol. 1998, 160, 171–179. [Google Scholar]
- Kaur, G.; Gras, S.; Mobbs, J.I.; Vivian, J.P.; Cortes, A.; Barber, T.; Kuttikkatte, S.B.; Jensen, L.T.; Attfield, K.E.; Dendrou, C.A.; et al. Structural and regulatory diversity shape HLA-C protein expression levels. Nat. Commun. 2017, 8, 15924. [Google Scholar] [CrossRef]
- Li, H.; Ivarsson, M.A.; Walker-Sperling, V.E.; Subleski, J.; Johnson, J.K.; Wright, P.W.; Carrington, M.; Björkström, N.K.; McVicar, D.W.; Anderson, S.K. Identification of an elaborate NK-specific system regulating HLA-C expression. PLoS Genet. 2018, 14, e1007163. [Google Scholar] [CrossRef]
- Zemmour, J.; Parham, P. Distinctive polymorphism at the HLA-C locus: Implications for the expression of HLA-C. J. Exp. Med. 1992, 176, 937–950. [Google Scholar] [CrossRef]
- Makadzange, A.T.; Gillespie, G.; Dong, T.; Kiama, P.; Bwayo, J.; Kimani, J.; Plummer, F.; Easterbrook, P.; Rowland-Jones, S.L. Characterization of an HLA-C-restricted CTL response in chronic HIV infection. Eur. J. Immunol. 2010, 40, 1036–1041. [Google Scholar] [CrossRef]
- Ameres, S.; Mautner, J.; Schlott, F.; Neuenhahn, M.; Busch, D.H.; Plachter, B.; Moosmann, A. Presentation of an Immunodominant Immediate-Early CD8+ T Cell Epitope Resists Human Cytomegalovirus Immunoevasion. PLoS Pathog. 2013, 9. [Google Scholar] [CrossRef]
- Vilches, C.; Parham, P. KIR: Diverse, rapidly evolving receptors of innate and adaptive immunity. Annu. Rev. Immunol. 2002, 20, 217–251. [Google Scholar] [CrossRef] [PubMed]
- Caligiuri, M.A. Human natural killer cells. Blood 2008, 112, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Pyo, C.-W.; Wang, R.; Vu, Q.; Cereb, N.; Yang, S.Y.; Duh, F.-M.; Wolinsky, S.; Martin, M.P.; Carrington, M.; Geraghty, D.E. Recombinant structures expand and contract inter and intragenic diversification at the KIR locus. BMC Genomics 2013, 14, 89. [Google Scholar] [CrossRef]
- Trowsdale, J. Genetic and functional relationships between MHC and NK receptor genes. Immunity 2001, 15, 363–374. [Google Scholar] [CrossRef]
- Marsh, S.G.E.; Parham, P.; Dupont, B.; Geraghty, D.E.; Trowsdale, J.; Middleton, D.; Vilches, C.; Carrington, M.; Witt, C.; Guethlein, L.A.; et al. Killer-cell immunoglobulin-like receptor (KIR) nomenclature report, 2002. Hum. Immunol. 2003, 64, 648–654. [Google Scholar] [CrossRef]
- Long, E.O. Regulation of immune responses through inhibitory receptors. Annu. Rev. Immunol. 1999, 17, 875–904. [Google Scholar] [CrossRef]
- Martin, A.M.; Freitas, E.M.; Witt, C.S.; Christiansen, F.T. The genomic organization and evolution of the natural killer immunoglobulin-like receptor (KIR) gene cluster. Immunogenetics 2000, 51, 268–280. [Google Scholar] [CrossRef]
- Hiby, S.E.; Apps, R.; Sharkey, A.M.; Farrell, L.E.; Gardner, L.; Mulder, A.; Claas, F.H.; Walker, J.J.; Redman, C.W.; Redman, C.C.; et al. Maternal activating KIRs protect against human reproductive failure mediated by fetal HLA-C2. J. Clin. Investig. 2010, 120, 4102–4110. [Google Scholar] [CrossRef] [PubMed]
- Lu, Z.; Zhang, B.; Chen, S.; Gai, Z.; Feng, Z.; Liu, X.; Liu, Y.; Wen, X.; Li, L.; Jiao, Y.; et al. Association of KIR genotypes and haplotypes with susceptibility to chronic hepatitis B virus infection in Chinese Han population. Cell. Mol. Immunol. 2008, 5, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Cheent, K.; Khakoo, S.I. Natural killer cells: Integrating diversity with function. Immunology 2009, 126, 449–457. [Google Scholar] [CrossRef]
- Hiby, S.E.; Walker, J.J.; O’shaughnessy, K.M.; Redman, C.W.G.; Carrington, M.; Trowsdale, J.; Moffett, A. Combinations of maternal KIR and fetal HLA-C genes influence the risk of preeclampsia and reproductive success. J. Exp. Med. 2004, 200, 957–965. [Google Scholar] [CrossRef]
- Hiby, S.E.; Ashrafian-Bonab, M.; Farrell, L.; Single, R.M.; Balloux, F.; Carrington, M.; Moffett, A.; Ebrahimi, Z. Distribution of killer cell immunoglobulin-like receptors (KIR) and their HLA-C ligands in two Iranian populations. Immunogenetics 2010, 62, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Gourraud, P.-A.; Meenagh, A.; Cambon-Thomsen, A.; Middleton, D. Linkage disequilibrium organization of the human KIR superlocus: Implications for KIR data analyses. Immunogenetics 2010, 62, 729–740. [Google Scholar] [CrossRef]
- Older Aguilar, A.M.; Guethlein, L.A.; Adams, E.J.; Abi-Rached, L.; Moesta, A.K.; Parham, P. Coevolution of killer cell Ig-like receptors with HLA-C to become the major variable regulators of human NK cells. J. Immunol. 2010, 185, 4238–4251. [Google Scholar] [CrossRef]
- Mandelboim, O.; Reyburn, H.T.; Valés-Gómez, M.; Pazmany, L.; Colonna, M.; Borsellino, G.; Strominger, J.L. Protection from lysis by natural killer cells of group 1 and 2 specificity is mediated by residue 80 in human histocompatibility leukocyte antigen C alleles and also occurs with empty major histocompatibility complex molecules. J. Exp. Med. 1996, 184, 913–922. [Google Scholar] [CrossRef]
- Biassoni, R.; Pessino, A.; Malaspina, A.; Cantoni, C.; Bottino, C.; Sivori, S.; Moretta, L.; Moretta, A. Role of amino acid position 70 in the binding affinity of p50.1 and p58.1 receptors for HLA-Cw4 molecules. Eur. J. Immunol. 1997, 27, 3095–3099. [Google Scholar] [CrossRef]
- Hilton, H.G.; Guethlein, L.A.; Goyos, A.; Nemat-Gorgani, N.; Bushnell, D.A.; Norman, P.J.; Parham, P. Polymorphic HLA-C Receptors Balance the Functional Characteristics of KIR Haplotypes. J. Immunol. 2015, 195, 3160–3170. [Google Scholar] [CrossRef] [PubMed]
- Blokhuis, J.H.; Hilton, H.G.; Guethlein, L.A.; Norman, P.J.; Nemat-Gorgani, N.; Nakimuli, A.; Chazara, O.; Moffett, A.; Parham, P. KIR2DS5 allotypes that recognize the C2 epitope of HLA-C are common among Africans and absent from Europeans. Immun. Inflamm. Dis. 2017, 5, 461–468. [Google Scholar] [CrossRef]
- Moesta, A.K.; Norman, P.J.; Yawata, M.; Yawata, N.; Gleimer, M.; Parham, P. Synergistic Polymorphism at Two Positions Distal to the Ligand-Binding Site Makes KIR2DL2 a Stronger Receptor for HLA-C Than KIR2DL3. J. Immunol. 2008, 180, 3969–3979. [Google Scholar] [CrossRef] [PubMed]
- Graef, T.; Moesta, A.K.; Norman, P.J.; Abi-Rached, L.; Vago, L.; Older Aguilar, A.M.; Gleimer, M.; Hammond, J.A.; Guethlein, L.A.; Bushnell, D.A.; et al. KIR2DS4 is a product of gene conversion with KIR3DL2 that introduced specificity for HLA-A*11 while diminishing avidity for HLA-C. J. Exp. Med. 2009, 206, 2557–2572. [Google Scholar] [CrossRef]
- Abi-Rached, L.; Parham, P. Natural selection drives recurrent formation of activating killer cell immunoglobulin-like receptor and Ly49 from inhibitory homologues. J. Exp. Med. 2005, 201, 1319–1332. [Google Scholar] [CrossRef]
- Stewart, C.A.; Laugier-Anfossi, F.; Vely, F.; Saulquin, X.; Riedmuller, J.; Tisserant, A.; Gauthier, L.; Romagne, F.; Ferracci, G.; Arosa, F.A.; et al. Recognition of peptide-MHC class I complexes by activating killer immunoglobulin-like receptors. Proc. Natl. Acad. Sci. USA 2005, 102, 13224–13229. [Google Scholar] [CrossRef] [PubMed]
- Winter, C.C.; Long, E.O. A single amino acid in the p58 killer cell inhibitory receptor controls the ability of natural killer cells to discriminate between the two groups of HLA-C allotypes. J. Immunol. 1997, 158, 4026–4028. [Google Scholar] [PubMed]
- Hilton, H.G.; Norman, P.J.; Nemat-Gorgani, N.; Goyos, A.; Hollenbach, J.A.; Henn, B.M.; Gignoux, C.R.; Guethlein, L.A.; Parham, P. Loss and Gain of Natural Killer Cell Receptor Function in an African Hunter-Gatherer Population. PLoS Genet. 2015, 11, e1005439. [Google Scholar] [CrossRef] [PubMed]
- Ivarsson, M.A.; Michaëlsson, J.; Fauriat, C. Activating killer cell Ig-like receptors in health and disease. Front. Immunol. 2014, 5, 184. [Google Scholar] [CrossRef]
- Hilton, H.G.; Moesta, A.K.; Guethlein, L.A.; Blokhuis, J.; Parham, P.; Norman, P.J. The production of KIR-Fc fusion proteins and their use in a multiplex HLA class I binding assay. J. Immunol. Methods 2015, 425, 79–87. [Google Scholar] [CrossRef]
- Fadda, L.; Borhis, G.; Ahmed, P.; Cheent, K.; Pageon, S.V.; Cazaly, A.; Stathopoulos, S.; Middleton, D.; Mulder, A.; Claas, F.H.J.; et al. Peptide antagonism as a mechanism for NK cell activation. Proc. Natl. Acad. Sci. USA 2010, 107, 10160–10165. [Google Scholar] [CrossRef]
- Long, E.O.; Rajagopalan, S. HLA class I recognition by killer cell Ig-like receptors. Semin. Immunol. 2000, 12, 101–108. [Google Scholar] [CrossRef]
- Alter, G.; Heckerman, D.; Schneidewind, A.; Fadda, L.; Kadie, C.M.; Carlson, J.M.; Oniangue-Ndza, C.; Martin, M.; Li, B.; Khakoo, S.I.; et al. HIV-1 adaptation to NK-cell-mediated immune pressure. Nature 2011, 476, 96–101. [Google Scholar] [CrossRef]
- Cassidy, S.; Mukherjee, S.; Myint, T.M.; Mbiribindi, B.; North, H.; Traherne, J.; Mulder, A.; Claas, F.H.J.; Purbhoo, M.A.; Das, J.; et al. Peptide selectivity discriminates NK cells from KIR2DL2- and KIR2DL3-positive individuals. Eur. J. Immunol. 2015, 45, 492–500. [Google Scholar] [CrossRef]
- Nanbakhsh, A.; Malarkannan, S. The Role of microRNAs in NK Cell Development and Function. Cells 2021, 10, 2020. [Google Scholar] [CrossRef] [PubMed]
- Pesce, S.; Squillario, M.; Greppi, M.; Loiacono, F.; Moretta, L.; Moretta, A.; Sivori, S.; Castagnola, P.; Barla, A.; Candiani, S.; et al. New miRNA Signature Heralds Human NK Cell Subsets at Different Maturation Steps: Involvement of miR-146a-5p in the Regulation of KIR Expression. Front. Immunol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- The HLA FactsBook; Elsevier: Amsterdam, The Netherlands, 2000.
- Hollenbach, J.A.; Nocedal, I.; Ladner, M.B.; Single, R.M.; Trachtenberg, E.A. Killer cell immunoglobulin-like receptor (KIR) gene content variation in the HGDP-CEPH populations. Immunogenetics 2012, 64, 719–737. [Google Scholar] [CrossRef]
- Parham, P. MHC class I molecules and KIRs in human history, health and survival. Nat. Rev. Immunol. 2005, 5, 201–214. [Google Scholar] [CrossRef]
- Carrington, M.; Martin, M.P. The Impact of Variation at the KIR Gene Cluster on Human Disease. In Current Topics in Microbiology and Immunology; Springer: Berlin/Heidelberg, Germany, 2006; Volume 298, pp. 225–257. [Google Scholar]
- Adams, E.J.; Parham, P. Species-specific evolution of MHC class I genes in the higher primates. Immunol. Rev. 2001, 183, 41–64. [Google Scholar] [CrossRef]
- Bimber, B.N.; Moreland, A.J.; Wiseman, R.W.; Hughes, A.L.; O’Connor, D.H. Complete Characterization of Killer Ig-Like Receptor (KIR) Haplotypes in Mauritian Cynomolgus Macaques: Novel Insights into Nonhuman Primate KIR Gene Content and Organization. J. Immunol. 2008, 181, 6301–6308. [Google Scholar] [CrossRef] [PubMed]
- Blokhuis, J.H.; van der Wiel, M.K.; Doxiadis, G.G.M.; Bontrop, R.E. The mosaic of KIR haplotypes in rhesus macaques. Immunogenetics 2010, 62, 295–306. [Google Scholar] [CrossRef]
- Kruse, P.H.; Rosner, C.; Walter, L. Characterization of rhesus macaque KIR genotypes and haplotypes. Immunogenetics 2010, 62, 281–293. [Google Scholar] [CrossRef]
- Abi-Rached, L.; Moesta, A.K.; Rajalingam, R.; Guethlein, L.A.; Parham, P. Human-specific evolution and adaptation led to major qualitative differences in the variable receptors of human and chimpanzee natural killer cells. PLoS Genet. 2010, 6, e1001192. [Google Scholar] [CrossRef]
- King, A.; Burrows, T.D.; Hiby, S.E.; Bowen, J.M.; Joseph, S.; Verma, S.; Lim, P.B.; Gardner, L.; Le Bouteiller, P.; Ziegler, A.; et al. Surface expression of HLA-C antigen by human extravillous trophoblast. Placenta 2000, 21, 376–387. [Google Scholar] [CrossRef] [PubMed]
- Yawata, M.; Yawata, N.; Draghi, M.; Little, A.-M.; Partheniou, F.; Parham, P. Roles for HLA and KIR polymorphisms in natural killer cell repertoire selection and modulation of effector function. J. Exp. Med. 2006, 203, 633–645. [Google Scholar] [CrossRef]
- Parham, P. The genetic and evolutionary balances in human NK cell receptor diversity. Semin. Immunol. 2008, 20, 311–316. [Google Scholar] [CrossRef]
- Lanier, L.L.; Corliss, B.C.; Wu, J.; Leong, C.; Phillips, J.H. Immunoreceptor DAP12 bearing a tyrosine-based activation motif is involved in activating NK cells. Nature 1998, 391, 703–707. [Google Scholar] [CrossRef]
- Yokoyama, W.M.; Plougastel, B.F.M. Immune functions encoded by the natural killer gene complex. Nat. Rev. Immunol. 2003, 3, 304–316. [Google Scholar] [CrossRef] [PubMed]
- Burshtyn, D.N.; Scharenberg, A.M.; Wagtmann, N.; Rajagopalan, S.; Berrada, K.; Yi, T.; Kinet, J.-P.; Long, E.O. Recruitment of Tyrosine Phosphatase HCP by the Killer Cell Inhibitory Receptor. Immunity 1996, 4, 77–85. [Google Scholar] [CrossRef]
- Boudreau, J.E.; Hsu, K.C. Natural Killer Cell Education and the Response to Infection and Cancer Therapy: Stay Tuned. Trends Immunol. 2018, 39, 222–239. [Google Scholar] [CrossRef]
- Pearce, E.L.; Pearce, E.J. Metabolic pathways in immune cell activation and quiescence. Immunity 2013, 38, 633–643. [Google Scholar] [CrossRef]
- Pfeifer, C.; Highton, A.J.; Peine, S.; Sauter, J.; Schmidt, A.H.; Bunders, M.J.; Altfeld, M.; Körner, C. Natural Killer Cell Education Is Associated With a Distinct Glycolytic Profile. Front. Immunol. 2018, 9, 3020. [Google Scholar] [CrossRef]
- Shifrin, N.; Raulet, D.H.; Ardolino, M. NK cell self tolerance, responsiveness and missing self recognition. Semin. Immunol. 2014, 26, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Poursine-Laurent, J.; Truscott, S.M.; Lybarger, L.; Song, Y.-J.; Yang, L.; French, A.R.; Sunwoo, J.B.; Lemieux, S.; Hansen, T.H.; et al. Licensing of natural killer cells by host major histocompatibility complex class I molecules. Nature 2005, 436, 709–713. [Google Scholar] [CrossRef]
- Cronk, J.M.; Fafoutis, E.; Brown, M.G. Licensing Natural Killers for Antiviral Immunity. Pathogens 2021, 10, 908. [Google Scholar] [CrossRef]
- Anfossi, N.; André, P.; Guia, S.; Falk, C.S.; Roetynck, S.; Stewart, C.A.; Breso, V.; Frassati, C.; Reviron, D.; Middleton, D.; et al. Human NK cell education by inhibitory receptors for MHC class I. Immunity 2006, 25, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Berg, M.G.; Olivo, A.; Harris, B.J.; Rodgers, M.A.; James, L.; Mampunza, S.; Niles, J.; Baer, F.; Yamaguchi, J.; Kaptue, L.; et al. A high prevalence of potential HIV elite controllers identified over 30 years in Democratic Republic of Congo. EBioMedicine 2021, 65, 103258. [Google Scholar] [CrossRef]
- Deeks, S.G.; Walker, B.D. Human Immunodeficiency Virus Controllers: Mechanisms of Durable Virus Control in the Absence of Antiretroviral Therapy. Immunity 2007, 27, 406–416. [Google Scholar] [CrossRef]
- Woldemeskel, B.A.; Kwaa, A.K.; Garliss, C.C.; Laeyendecker, O.; Ray, S.C.; Blankson, J.N. Healthy donor T cell responses to common cold coronaviruses and SARS-CoV-2. J. Clin. Investig. 2020, 130, 6631–6638. [Google Scholar] [CrossRef] [PubMed]
- Emu, B.; Sinclair, E.; Hatano, H.; Ferre, A.; Shacklett, B.; Martin, J.N.; McCune, J.M.; Deeks, S.G. HLA Class I-Restricted T-Cell Responses May Contribute to the Control of Human Immunodeficiency Virus Infection, but Such Responses Are Not Always Necessary for Long-Term Virus Control. J. Virol. 2008, 82, 5398–5407. [Google Scholar] [CrossRef] [PubMed]
- Walker-Sperling, V.E.; Pohlmeyer, C.W.; Veenhuis, R.T.; May, M.; Luna, K.A.; Kirkpatrick, A.R.; Laeyendecker, O.; Cox, A.L.; Carrington, M.; Bailey, J.R.; et al. Factors Associated with the Control of Viral Replication and Virologic Breakthrough in a Recently Infected HIV-1 Controller. EBioMedicine 2017, 16, 141–149. [Google Scholar] [CrossRef]
- Naranbhai, V.; Altfeld, M.; Karim, S.S.A.; Ndung’u, T.; Karim, Q.A.; Carr, W.H. Changes in Natural Killer Cell Activation and Function during Primary HIV-1 Infection. PLoS ONE 2013, 8, e53251. [Google Scholar] [CrossRef]
- Fellay, J.; Shianna, K.V.; Ge, D.; Colombo, S.; Ledergerber, B.; Weale, M.; Zhang, K.; Gumbs, C.; Castagna, A.; Cossarizza, A.; et al. A whole-genome association study of major determinants for host control of HIV-1. Science 2007, 317, 944–947. [Google Scholar] [CrossRef] [PubMed]
- International HIV Controllers Study; Pereyra, F.; Jia, X.; McLaren, P.J.; Telenti, A.; de Bakker, P.I.W.; Walker, B.D.; Ripke, S.; Brumme, C.J.; Pulit, S.L.; et al. The Major Genetic Determinants of HIV-1 Control Affect HLA Class I Peptide Presentation. Science 2010, 330, 1551–1557. [Google Scholar] [CrossRef]
- Migueles, S.A.; Sabbaghian, M.S.; Shupert, W.L.; Bettinotti, M.P.; Marincola, F.M.; Martino, L.; Hallahan, C.W.; Selig, S.M.; Schwartz, D.; Sullivan, J.; et al. HLA B*5701 is highly associated with restriction of virus replication in a subgroup of HIV-infected long term nonprogressors. Proc. Natl. Acad. Sci. USA 2000, 97, 2709–2714. [Google Scholar] [CrossRef]
- Altfeld, M.; Addo, M.M.; Rosenberg, E.S.; Hecht, F.M.; Lee, P.K.; Vogel, M.; Yu, X.G.; Draenert, R.; Johnston, M.N.; Strick, D.; et al. Influence of HLA-B57 on clinical presentation and viral control during acute HIV-1 infection. AIDS 2003, 17, 2581–2591. [Google Scholar] [CrossRef] [PubMed]
- Stranger, B.E.; Forrest, M.S.; Clark, A.G.; Minichiello, M.J.; Deutsch, S.; Lyle, R.; Hunt, S.; Kahl, B.; Antonarakis, S.E.; Tavaré, S.; et al. Genome-Wide Associations of Gene Expression Variation in Humans. PLoS Genet. 2005, 1, e78. [Google Scholar] [CrossRef] [PubMed]
- Stranger, B.E.; Nica, A.C.; Forrest, M.S.; Dimas, A.; Bird, C.P.; Beazley, C.; Ingle, C.E.; Dunning, M.; Flicek, P.; Koller, D.; et al. Population genomics of human gene expression. Nat. Genet. 2007, 39, 1217–1224. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Apps, R.; Qi, Y.; Gao, X.; Male, V.; O’hUigin, C.; O’Connor, G.; Ge, D.; Fellay, J.; Martin, J.N.; et al. HLA-C cell surface expression and control of HIV/AIDS correlate with a variant upstream of HLA-C. Nat. Genet. 2009, 41, 1290–1294. [Google Scholar] [CrossRef] [PubMed]
- Fellay, J.; Ge, D.; Shianna, K.V.; Colombo, S.; Ledergerber, B.; Cirulli, E.T.; Urban, T.J.; Zhang, K.; Gumbs, C.E.; Smith, J.P.; et al. Common Genetic Variation and the Control of HIV-1 in Humans. PLoS Genet. 2009, 5, e1000791. [Google Scholar] [CrossRef]
- Apps, R.; Qi, Y.; Carlson, J.M.; Chen, H.; Gao, X.; Thomas, R.; Yuki, Y.; Del Prete, G.Q.; Goulder, P.; Brumme, Z.L.; et al. Influence of HLA-C expression level on HIV control. Science 2013, 340, 87–91. [Google Scholar] [CrossRef]
- Blais, M.-E.; Zhang, Y.; Rostron, T.; Griffin, H.; Taylor, S.; Xu, K.; Yan, H.; Wu, H.; James, I.; John, M.; et al. High frequency of HIV mutations associated with HLA-C suggests enhanced HLA-C-restricted CTL selective pressure associated with an AIDS-protective polymorphism. J. Immunol. 2012, 188, 4663–4670. [Google Scholar] [CrossRef]
- Kulkarni, S.; Qi, Y.; O’hUigin, C.; Pereyra, F.; Ramsuran, V.; McLaren, P.; Fellay, J.; Nelson, G.; Chen, H.; Liao, W.; et al. Genetic interplay between HLA-C and MIR148A in HIV control and Crohn disease. Proc. Natl. Acad. Sci. USA 2013, 110, 20705–20710. [Google Scholar] [CrossRef]
- Martin, M.P.; Gao, X.; Lee, J.H.; Nelson, G.W.; Detels, R.; Goedert, J.J.; Buchbinder, S.; Hoots, K.; Vlahov, D.; Trowsdale, J.; et al. Epistatic interaction between KIR3DS1 and HLA-B delays the progression to AIDS. Nat. Genet. 2002, 31, 429–434. [Google Scholar] [CrossRef]
- Bashirova, A.A.; Thomas, R.; Carrington, M. HLA/KIR restraint of HIV: Surviving the fittest. Annu. Rev. Immunol. 2011, 29, 295–317. [Google Scholar] [CrossRef]
- Jamil, K.M.; Khakoo, S.I. KIR/HLA interactions and pathogen immunity. J. Biomed. Biotechnol. 2011, 2011, 298348. [Google Scholar] [CrossRef]
- Körner, C.; Granoff, M.E.; Amero, M.A.; Sirignano, M.N.; Vaidya, S.A.; Jost, S.; Allen, T.M.; Rosenberg, E.S.; Altfeld, M. Increased frequency and function of KIR2DL1-3+ NK cells in primary HIV-1 infection are determined by HLA-C group haplotypes. Eur. J. Immunol. 2014, 44, 2938–2948. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Kuroki, K.; Kuse, N.; Sun, X.; Akahoshi, T.; Qi, Y.; Chikata, T.; Naruto, T.; Koyanagi, M.; Murakoshi, H.; et al. HIV-1 Control by NK Cells via Reduced Interaction between KIR2DL2 and HLA-C∗12:02/C∗14:03. Cell Rep. 2016, 17, 2210–2220. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Leitman, E.; Walker, B.; Ndung’u, T.; Carrington, M.; Goulder, P. Impact of HLA Allele-KIR Pairs on HIV Clinical Outcome in South Africa. J. Infect. Dis. 2019, 219, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Wichukchinda, N.; Miyahara, R.; Rojanawiwat, A.; Pathipvanich, P.; Tsuchiya, N.; Miura, T.; Yasunami, M.; Ariyoshi, K.; Sawanpanyalert, P. The effect of KIR2D-HLA-C receptor-ligand interactions on clinical outcome in a HIV-1 CRF01_AE-infected Thai population. AIDS 2015, 29, 1607–1615. [Google Scholar] [CrossRef]
- Jennes, W.; Verheyden, S.; Demanet, C.; Adjé-Touré, C.A.; Vuylsteke, B.; Nkengasong, J.N.; Kestens, L. Cutting Edge: Resistance to HIV-1 Infection among African Female Sex Workers Is Associated with Inhibitory KIR in the Absence of Their HLA Ligands. J. Immunol. 2006, 177, 6588–6592. [Google Scholar] [CrossRef]
- Paximadis, M.; Minevich, G.; Winchester, R.; Schramm, D.B.; Gray, G.E.; Sherman, G.G.; Coovadia, A.H.; Kuhn, L.; Tiemessen, C.T. KIR-HLA and maternal-infant HIV-1 transmission in sub-Saharan Africa. PLoS ONE 2011, 6, e16541. [Google Scholar] [CrossRef]
- Ravet, S.; Scott-Algara, D.; Bonnet, E.; Tran, H.K.; Tran, T.; Nguyen, N.; Truong, L.X.; Theodorou, I.; Barré-Sinoussi, F.; Pancino, G.; et al. Distinctive NK-cell receptor repertoires sustain high-level constitutive NK-cell activation in HIV-exposed uninfected individuals. Blood 2007, 109, 4296–4305. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, O.; Maréchal, V.; Le Gall, S.; Lemonnier, F.; Heard, J.-M. Endocytosis of major histocompatibility complex class I molecules is induced by the HIV–1 Nef protein. Nat. Med. 1996, 2, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Collins, K.L.; Chen, B.K.; Kalams, S.A.; Walker, B.D.; Baltimore, D. HIV-1 Nef protein protects infected primary cells against killing by cytotoxic T lymphocytes. Nature 1998, 391, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Le Gall, S.; Erdtmann, L.; Benichou, S.; Berlioz-Torrent, C.; Liu, L.; Benarous, R.; Heard, J.M.; Schwartz, O. Nef interacts with the mu subunit of clathrin adaptor complexes and reveals a cryptic sorting signal in MHC I molecules. Immunity 1998, 8, 483–495. [Google Scholar] [CrossRef]
- Cohen, G.B.; Gandhi, R.T.; Davis, D.M.; Mandelboim, O.; Chen, B.K.; Strominger, J.L.; Baltimore, D. The selective downregulation of class I major histocompatibility complex proteins by HIV-1 protects HIV-infected cells from NK cells. Immunity 1999, 10, 661–671. [Google Scholar] [CrossRef]
- Apps, R.; Del Prete, G.Q.; Chatterjee, P.; Lara, A.; Brumme, Z.L.; Brockman, M.A.; Neil, S.; Pickering, S.; Schneider, D.K.; Piechocka-Trocha, A.; et al. HIV-1 Vpu Mediates HLA-C Downregulation. Cell Host Microbe 2016, 19, 686–695. [Google Scholar] [CrossRef]
- Körner, C.; Simoneau, C.R.; Schommers, P.; Granoff, M.; Ziegler, M.; Hölzemer, A.; Lunemann, S.; Chukwukelu, J.; Corleis, B.; Naranbhai, V.; et al. HIV-1-Mediated Downmodulation of HLA-C Impacts Target Cell Recognition and Antiviral Activity of NK Cells. Cell Host Microbe 2017, 22, 111–119.e4. [Google Scholar] [CrossRef]
- Bachtel, N.D.; Umviligihozo, G.; Pickering, S.; Mota, T.M.; Liang, H.; Del Prete, G.Q.; Chatterjee, P.; Lee, G.Q.; Thomas, R.; Brockman, M.A.; et al. HLA-C downregulation by HIV-1 adapts to host HLA genotype. PLoS Pathog. 2018, 14, e1007257. [Google Scholar] [CrossRef]
- Hopfensperger, K.; Richard, J.; Stürzel, C.M.; Bibollet-Ruche, F.; Apps, R.; Leoz, M.; Plantier, J.-C.; Hahn, B.H.; Finzi, A.; Kirchhoff, F.; et al. Convergent Evolution of HLA-C Downmodulation in HIV-1 and HIV-2. MBio 2020, 11, e00782-20. [Google Scholar] [CrossRef]
- Sauter, D.; Hotter, D.; Van Driessche, B.; Stürzel, C.M.; Kluge, S.F.; Wildum, S.; Yu, H.; Baumann, B.; Wirth, T.; Plantier, J.C.; et al. Differential Regulation of NF-κB-Mediated Proviral and Antiviral Host Gene Expression by Primate Lentiviral Nef and Vpu Proteins. Cell Rep. 2015, 10, 586–599. [Google Scholar] [CrossRef] [PubMed]
- Fadda, L.; Körner, C.; Kumar, S.; van Teijlingen, N.H.; Piechocka-Trocha, A.; Carrington, M.; Altfeld, M. HLA-Cw*0102-restricted HIV-1 p24 epitope variants can modulate the binding of the inhibitory KIR2DL2 receptor and primary NK cell function. PLoS Pathog. 2012, 8, e1002805. [Google Scholar] [CrossRef] [PubMed]
- Van Teijlingen, N.H.; Hölzemer, A.; Körner, C.; García-Beltrán, W.F.; Schafer, J.L.; Fadda, L.; Suscovich, T.J.; Brander, C.; Carrington, M.; Evans, D.T.; et al. Sequence variations in HIV-1 p24 Gag-derived epitopes can alter binding of KIR2DL2 to HLA-C*03. AIDS 2014, 28, 1399–1408. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, M.C.; Nelde, A.; Weber, J.K.; Schreitmüller, C.M.; Martrus, G.; Huynh, T.; Bunders, M.J.; Lunemann, S.; Stevanovic, S.; Zhou, R.; et al. HIV-1 induced changes in HLA-C*03: 04-presented peptide repertoires lead to reduced engagement of inhibitory natural killer cell receptors. AIDS 2020, 34, 1713–1723. [Google Scholar] [CrossRef]
- Yoon, J.C.; Yang, C.M.; Song, Y.; Lee, J.M. Natural killer cells in hepatitis C: Current progress. World J. Gastroenterol. 2016, 22, 1449–1460. [Google Scholar] [CrossRef]
- Knapp, S.; Warshow, U.; Hegazy, D.; Brackenbury, L.; Guha, I.N.; Fowell, A.; Little, A.; Alexander, G.J.; Rosenberg, W.M.C.; Cramp, M.E.; et al. Consistent beneficial effects of killer cell immunoglobulin-like receptor 2DL3 and group 1 human leukocyte antigen-C following exposure to hepatitis C virus. Hepatology 2010, 51, 1168–1175. [Google Scholar] [CrossRef] [PubMed]
- Kuśnierczyk, P.; Mozer-Lisewska, I.; Zwolińska, K.; Kowala-Piaskowska, A.E.; Bura, M.; Bereszyńska, I.; Pauli, A.; Żeromski, J. Contribution of genes for killer cell immunoglobulin-like receptors (KIR) to the susceptibility to chronic hepatitis C virus infection and to viremia. Hum. Immunol. 2015, 76, 102–108. [Google Scholar] [CrossRef]
- Hoofnagle, J.H. Course and outcome of hepatitis C. Hepatology 2002, 36, s21–s29. [Google Scholar] [CrossRef]
- Suppiah, V.; Gaudieri, S.; Armstrong, N.J.; O’Connor, K.S.; Berg, T.; Weltman, M.; Abate, M.L.; Spengler, U.; Bassendine, M.; Dore, G.J.; et al. IL28B, HLA-C, and KIR variants additively predict response to therapy in chronic hepatitis C virus infection in a European cohort: A cross-sectional study. PLoS Med. 2011, 8. [Google Scholar] [CrossRef]
- Vidal-Castiñeira, J.R.; López-Vázquez, A.; Díaz-Peña, R.; Alonso-Arias, R.; Martínez-Borra, J.; Pérez, R.; Fernández-Suárez, J.; Melón, S.; Prieto, J.; Rodrigo, L.; et al. Effect of Killer Immunoglobulin-Like Receptors in the Response to Combined Treatment in Patients with Chronic Hepatitis C Virus Infection. J. Virol. 2010, 84, 475–481. [Google Scholar] [CrossRef]
- De Vasconcelos, J.M.; de Móia, L.J.M.P.; do Amaral, I.S.A.; Miranda, E.C.B.M.; CicaliseTakeshita, L.Y.; de Oliveira, L.F.; de Mendes, L.A.M.; Sastre, D.; Tamegão-Lopes, B.P.; de Pedroza, L.S.R.A.; et al. Association of killer cell immunoglobulin-like receptor polymorphisms with chronic hepatitis C and responses to therapy in Brazil. Genet. Mol. Biol. 2013, 36, 022–027. [Google Scholar] [CrossRef]
- Montes-Cano, M.A.; Caro-Oleas, J.L.; Romero-Gómez, M.; Diago, M.; Andrade, R.; Carmona, I.; Aguilar Reina, J.; Núñez-Roldán, A.; González-Escribano, M.F. HLA-C and KIR genes in hepatitis C virus infection. Hum. Immunol. 2005, 66, 1106–1109. [Google Scholar] [CrossRef]
- Legrand, N.; David, G.; Rodallec, A.; Gaultier, A.; Salmon, D.; Cesbron, A.; Wittkop, L.; Raffi, F.; Gendzekhadze, K.; Retière, C.; et al. Influence of HLA-C environment on the spontaneous clearance of hepatitis C in European HIV–HCV co-infected individuals. Clin. Exp. Immunol. 2021, 204, 107–124. [Google Scholar] [CrossRef]
- Dring, M.M.; Morrison, M.H.; McSharry, B.P.; Guinan, K.J.; Hagan, R.; O’Farrelly, C.; Gardiner, C.M.; Courtney, G.; Crosbie, O.; Crowe, J.; et al. Innate immune genes synergize to predict increased risk of chronic disease in hepatitis C virus infection. Proc. Natl. Acad. Sci. USA 2011, 108, 5736–5741. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Umemura, T.; Joshita, S.; Yamazaki, T.; Fujimori, N.; Kimura, T.; Komatsu, M.; Matsumoto, A.; Tanaka, E.; Ota, M. KIR2DL2 combined with HLA-C1 confers risk of hepatitis C virus-related hepatocellular carcinoma in younger patients. Oncotarget 2018, 9, 19650–19661. [Google Scholar] [CrossRef]
- Hu, S.; Yuan, F.; Feng, L.; Zheng, F.; Gong, F.; Huang, H.; Sun, B. KIR2DL2/C1 is a Risk Factor for Chronic Infection and Associated with Non-response to PEG-IFN and RBV Combination Therapy in Hepatitis C Virus Genotype 1b Patients in China. Virol. Sin. 2018, 33, 369–372. [Google Scholar] [CrossRef] [PubMed]
- Shan, Z.; Huang, J.; Liao, Q.; Huang, K.; Wang, M.; Xu, R.; Tang, X.; Zhang, W.; Nelson, K.; Fu, Y.; et al. Association of killer cell immunoglobulin-like receptors with spontaneous clearance of hepatitis C virus in the Chinese population. Transfusion 2018, 58, 1028–1035. [Google Scholar] [CrossRef]
- Shen, C.; Ge, Z.; Dong, C.; Wang, C.; Shao, J.; Cai, W.; Huang, P.; Fan, H.; Li, J.; Zhang, Y.; et al. Genetic Variants in KIR/HLA-C Genes Are Associated With the Susceptibility to HCV Infection in a High-Risk Chinese Population. Front. Immunol. 2021, 12, 632353. [Google Scholar] [CrossRef]
- Ursu, L.; Calenic, B.; Diculescu, M.; Dima, A.; Constantinescu, I. HLA Alleles and KIR Genes in Romanian Patients with Chronic Hepatitis C. J. Gastrointest. Liver Dis. 2020, 29, 595–601. [Google Scholar] [CrossRef]
- Lunemann, S.; Martrus, G.; Hölzemer, A.; Chapel, A.; Ziegler, M.; Körner, C.; Garcia Beltran, W.; Carrington, M.; Wedemeyer, H.; Altfeld, M. Sequence variations in HCV core-derived epitopes alter binding of KIR2DL3 to HLA-C∗03:04 and modulate NK cell function. J. Hepatol. 2016, 65, 252–258. [Google Scholar] [CrossRef]
- Gumá, M.; Angulo, A.; Vilches, C.; Gómez-Lozano, N.; Malats, N.; López-Botet, M. Imprint of human cytomegalovirus infection on the NK cell receptor repertoire. Blood 2004, 104, 3664–3671. [Google Scholar] [CrossRef]
- Foley, B.; Cooley, S.; Verneris, M.R.; Pitt, M.; Curtsinger, J.; Luo, X.; Lopez-Vergès, S.; Lanier, L.L.; Weisdorf, D.; Miller, J.S. Cytomegalovirus reactivation after allogeneic transplantation promotes a lasting increase in educated NKG2C+ natural killer cells with potent function. Blood 2012, 119, 2665–2674. [Google Scholar] [CrossRef]
- Pesce, S.; Greppi, M.; Tabellini, G.; Rampinelli, F.; Parolini, S.; Olive, D.; Moretta, L.; Moretta, A.; Marcenaro, E. Identification of a subset of human natural killer cells expressing high levels of programmed death 1: A phenotypic and functional characterization. J. Allergy Clin. Immunol. 2017, 139, 335–346.e3. [Google Scholar] [CrossRef] [PubMed]
- Béziat, V.; Liu, L.L.; Malmberg, J.-A.; Ivarsson, M.A.; Sohlberg, E.; Björklund, A.T.; Retière, C.; Sverremark-Ekström, E.; Traherne, J.; Ljungman, P.; et al. NK cell responses to cytomegalovirus infection lead to stable imprints in the human KIR repertoire and involve activating KIRs. Blood 2013, 121, 2678–2688. [Google Scholar] [CrossRef]
- Charoudeh, H.N.; Terszowski, G.; Czaja, K.; Gonzalez, A.; Schmitter, K.; Stern, M. Modulation of the natural killer cell KIR repertoire by cytomegalovirus infection. Eur. J. Immunol. 2013, 43, 480–487. [Google Scholar] [CrossRef]
- Lopez-Verges, S.; Milush, J.M.; Schwartz, B.S.; Pando, M.J.; Jarjoura, J.; York, V.A.; Houchins, J.P.; Miller, S.; Kang, S.-M.; Norris, P.J.; et al. Expansion of a unique CD57+NKG2Chi natural killer cell subset during acute human cytomegalovirus infection. Proc. Natl. Acad. Sci. USA 2011, 108, 14725–14732. [Google Scholar] [CrossRef]
- Manser, A.R.; Scherenschlich, N.; Thöns, C.; Hengel, H.; Timm, J.; Uhrberg, M. KIR Polymorphism Modulates the Size of the Adaptive NK Cell Pool in Human Cytomegalovirus–Infected Individuals. J. Immunol. 2019, 203, 2301–2309. [Google Scholar] [CrossRef]
- Della Chiesa, M.; Falco, M.; Bertaina, A.; Muccio, L.; Alicata, C.; Frassoni, F.; Locatelli, F.; Moretta, L.; Moretta, A. Human Cytomegalovirus Infection Promotes Rapid Maturation of NK Cells Expressing Activating Killer Ig–like Receptor in Patients Transplanted with NKG2C −/− Umbilical Cord Blood. J. Immunol. 2014, 192, 1471–1479. [Google Scholar] [CrossRef] [PubMed]
- Crespo, Â.C.; Strominger, J.L.; Tilburgs, T. Expression of KIR2DS1 by decidual natural killer cells increases their ability to control placental HCMV infection. Proc. Natl. Acad. Sci. USA 2016, 113, 15072–15077. [Google Scholar] [CrossRef] [PubMed]
- Van der Ploeg, K.; Chang, C.; Ivarsson, M.A.; Moffett, A.; Wills, M.R.; Trowsdale, J. Modulation of human leukocyte antigen-C by human cytomegalovirus stimulates KIR2DS1 recognition by natural killer cells. Front. Immunol. 2017, 8. [Google Scholar] [CrossRef]
- Prod’homme, V.; Griffin, C.; Aicheler, R.J.; Wang, E.C.Y.; McSharry, B.P.; Rickards, C.R.; Stanton, R.J.; Borysiewicz, L.K.; López-Botet, M.; Wilkinson, G.W.G.; et al. The Human Cytomegalovirus MHC Class I Homolog UL18 Inhibits LIR-1 + but Activates LIR-1 − NK Cells. J. Immunol. 2007, 178, 4473–4481. [Google Scholar] [CrossRef]
- Smith, W.; Tomasec, P.; Aicheler, R.; Loewendorf, A.; Nemčovičová, I.; Wang, E.C.Y.; Stanton, R.J.; MacAuley, M.; Norris, P.; Willen, L.; et al. Human cytomegalovirus glycoprotein UL141 targets the TRAIL death receptors to thwart host innate antiviral defenses. Cell Host Microbe 2013, 13, 324–335. [Google Scholar] [CrossRef]
- Barel, M.T.; Ressing, M.; Pizzato, N.; van Leeuwen, D.; Le Bouteiller, P.; Lenfant, F.; Wiertz, E.J.H.J. Human cytomegalovirus-encoded US2 differentially affects surface expression of MHC class I locus products and targets membrane-bound, but not soluble HLA-G1 for degradation. J. Immunol. 2003, 171, 6757–6765. [Google Scholar] [CrossRef]
- Jun, Y.; Kim, E.; Jin, M.; Sung, H.C.; Han, H.; Geraghty, D.E.; Ahn, K. Human Cytomegalovirus Gene Products US3 and US6 Down-Regulate Trophoblast Class I MHC Molecules. J. Immunol. 2000, 164, 805–811. [Google Scholar] [CrossRef] [PubMed]
- Schust, D.J.; Tortorella, D.; Seebach, J.; Phan, C.; Ploegh, H.L. Trophoblast class I major histocompatibility complex (MHC) products are resistant to rapid degradation imposed by the human cytomegalovirus (HCMV) gene products US2 and US11. J. Exp. Med. 1998, 188, 497–503. [Google Scholar] [CrossRef]
- Gewurz, B.E.; Wang, E.W.; Tortorella, D.; Schust, D.J.; Ploegh, H.L. Human Cytomegalovirus US2 Endoplasmic Reticulum-Lumenal Domain Dictates Association with Major Histocompatibility Complex Class I in a Locus-Specific Manner. J. Virol. 2001, 75, 5197–5204. [Google Scholar] [CrossRef]
- Huard, B.; Früh, K. A role for MHC class I down-regulation in NK cell lysis of herpes virus-infected cells. Eur. J. Immunol. 2000, 30, 509–515. [Google Scholar] [CrossRef]
- Llano, M.; Gumá, M.; Ortega, M.; Angulo, A.; López-Botet, M. Differential effects of US2, US6, and US11 human cytomegalovirus proteins of HLA class Ia and HLA-E expression: Impact on target susceptibility to NK cell subsets. Eur. J. Immunol. 2003, 33, 2744–2754. [Google Scholar] [CrossRef]
- Hosie, L.; Pachnio, A.; Zuo, J.; Pearce, H.; Riddell, S.; Moss, P. Cytomegalovirus-Specific T Cells Restricted by HLA-Cw*0702 Increase Markedly with Age and Dominate the CD8+ T-Cell Repertoire in Older People. Front. Immunol. 2017, 8, 1776. [Google Scholar] [CrossRef] [PubMed]
- Elboim, M.; Grodzovski, I.; Djian, E.; Wolf, D.G.; Mandelboim, O. HSV-2 Specifically Down Regulates HLA-C Expression to Render HSV-2-Infected DCs Susceptible to NK Cell Killing. PLoS Pathog. 2013, 9, e1003226. [Google Scholar] [CrossRef]
- Ahlenstiel, G.; Martin, M.P.; Gao, X.; Carrington, M.; Rehermann, B. Distinct KIR/HLA compound genotypes affect the kinetics of human antiviral natural killer cell responses. J. Clin. Investig. 2008, 118, 1017–1026. [Google Scholar] [CrossRef]
- La, D.; Czarnecki, C.; El-Gabalawy, H.; Kumar, A.; Meyers, A.F.A.; Bastien, N.; Simonsen, J.N.; Plummer, F.A.; Luo, M. Enrichment of Variations in KIR3DL1/S1 and KIR2DL2/L3 among H1N1/09 ICU Patients: An Exploratory Study. PLoS ONE 2011, 6, e29200. [Google Scholar] [CrossRef]
- Koutsakos, M.; McWilliam, H.E.G.; Aktepe, T.E.; Fritzlar, S.; Illing, P.T.; Mifsud, N.A.; Purcell, A.W.; Rockman, S.; Reading, P.C.; Vivian, J.P.; et al. Downregulation of MHC class I expression by influenza A and B viruses. Front. Immunol. 2019, 10. [Google Scholar] [CrossRef]
- Björkström, N.K.; Lindgren, T.; Stoltz, M.; Fauriat, C.; Braun, M.; Evander, M.; Michaëlsson, J.; Malmberg, K.-J.; Klingström, J.; Ahlm, C.; et al. Rapid expansion and long-term persistence of elevated NK cell numbers in humans infected with hantavirus. J. Exp. Med. 2011, 208, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Petitdemange, C.; Becquart, P.; Wauquier, N.; Béziat, V.; Debré, P.; Leroy, E.M.; Vieillard, V. Unconventional repertoire profile is imprinted during acute chikungunya infection for natural killer cells polarization toward cytotoxicity. PLoS Pathog. 2011, 7, e1002268. [Google Scholar] [CrossRef] [PubMed]
- Petitdemange, C.; Wauquier, N.; Jacquet, J.-M.; Theodorou, I.; Leroy, E.; Vieillard, V. Association of HLA class-I and inhibitory KIR genotypes in Gabonese patients infected by Chikungunya or Dengue type-2 viruses. PLoS ONE 2014, 9, e108798. [Google Scholar] [CrossRef]
- Wauquier, N.; Padilla, C.; Becquart, P.; Leroy, E.; Vieillard, V. Association of KIR2DS1 and KIR2DS3 with fatal outcome in Ebola virus infection. Immunogenetics 2010, 62, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Wawina-Bokalanga, T.; Vanmechelen, B.; Lhermitte, V.; Martí-Carreras, J.; Vergote, V.; Koundouno, F.R.; Akoi-Boré, J.; Thom, R.; Tipton, T.; Steeds, K.; et al. Human Diversity of Killer Cell Immunoglobulin-Like Receptors and Human Leukocyte Antigen Class I Alleles and Ebola Virus Disease Outcomes - Volume 27, Number 1—January 2021—Emerging Infectious Diseases journal - CDC. Emerg. Infect. Dis. 2021, 27, 76–84. [Google Scholar] [CrossRef]
- Cimini, E.; Viola, D.; Cabeza-Cabrerizo, M.; Romanelli, A.; Tumino, N.; Sacchi, A.; Bordoni, V.; Casetti, R.; Turchi, F.; Martini, F.; et al. Different features of Vδ2 T and NK cells in fatal and non-fatal human Ebola infections. PLoS Negl. Trop. Dis. 2017, 11, e0005645. [Google Scholar] [CrossRef] [PubMed]
- Maucourant, C.; Filipovic, I.; Ponzetta, A.; Aleman, S.; Cornillet, M.; Hertwig, L.; Strunz, B.; Lentini, A.; Reinius, B.; Brownlie, D.; et al. Natural killer cell immunotypes related to COVID-19 disease severity. Sci. Immunol. 2020, 5, eabd6832. [Google Scholar] [CrossRef]
- Sim, M.J.W.; Rajagopalan, S.; Altmann, D.M.; Boyton, R.J.; Sun, P.D.; Long, E.O. Human NK cell receptor KIR2DS4 detects a conserved bacterial epitope presented by HLA-C. Proc. Natl. Acad. Sci. USA 2019, 116, 12964–12973. [Google Scholar] [CrossRef] [PubMed]
- Littera, R.; Chessa, L.; Deidda, S.; Angioni, G.; Campagna, M.; Lai, S.; Melis, M.; Cipri, S.; Firinu, D.; Santus, S.; et al. Natural killer-cell immunoglobulin-like receptors trigger differences in immune response to SARS-CoV-2 infection. PLoS ONE 2021, 16, e0255608. [Google Scholar] [CrossRef] [PubMed]


| HLA-C1 (80N) | HLA-C2 (80K) |
|---|---|
| 01:02, 01:03, 01:04, 01:05 | 02:02, 02:03, 02:04, 02:05 |
| 03:02, 03:03, 03:04, 03:05, 03:06,03:08, 03:09 03:10, 03:11, 03:12, 03:13, 03:14 | 03:07 |
| 04:01, 04:03, 04:04, 04:05, 04:06, 04:07, 04:08 | |
| 05:01, 05:02, 05:03, 05:04 | |
| 06:02, 06:03, 06:04, 06:05, 06:06, 06:07 | |
| 07:01, 07:02, 07:03, 07:04, 07:05, 07:06, 07:08, 07:10, 07:11, 07:12, 07:13, 07:14, 07:15 | 07:07, 07:09 |
| 08:01, 08:02, 08:03, 08:04, 08:05, 08:06, 08:07, 08:08, 08:09 | |
| 12:02, 12:03, 12:06, 12:08 | 12:04, 12:05, 12:07 |
| 13:01 | |
| 14:02, 14:03, 14:05 | 14:04 |
| 15:07 | 15:02, 15:03, 15:04, 15:05, 15:06, 15:08, 15:09, 15:10, 15:11 |
| 16:01, 16:04 | 16:02 |
| 17:01, 17:02, 17:03 | |
| 18:01, 18:02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vollmers, S.; Lobermeyer, A.; Körner, C. The New Kid on the Block: HLA-C, a Key Regulator of Natural Killer Cells in Viral Immunity. Cells 2021, 10, 3108. https://doi.org/10.3390/cells10113108
Vollmers S, Lobermeyer A, Körner C. The New Kid on the Block: HLA-C, a Key Regulator of Natural Killer Cells in Viral Immunity. Cells. 2021; 10(11):3108. https://doi.org/10.3390/cells10113108
Chicago/Turabian StyleVollmers, Sarah, Annabelle Lobermeyer, and Christian Körner. 2021. "The New Kid on the Block: HLA-C, a Key Regulator of Natural Killer Cells in Viral Immunity" Cells 10, no. 11: 3108. https://doi.org/10.3390/cells10113108
APA StyleVollmers, S., Lobermeyer, A., & Körner, C. (2021). The New Kid on the Block: HLA-C, a Key Regulator of Natural Killer Cells in Viral Immunity. Cells, 10(11), 3108. https://doi.org/10.3390/cells10113108






