Real-Time Monitoring of the Effect of Tumour-Treating Fields on Cell Division Using Live-Cell Imaging
Abstract
:1. Introduction
2. Materials and Methods
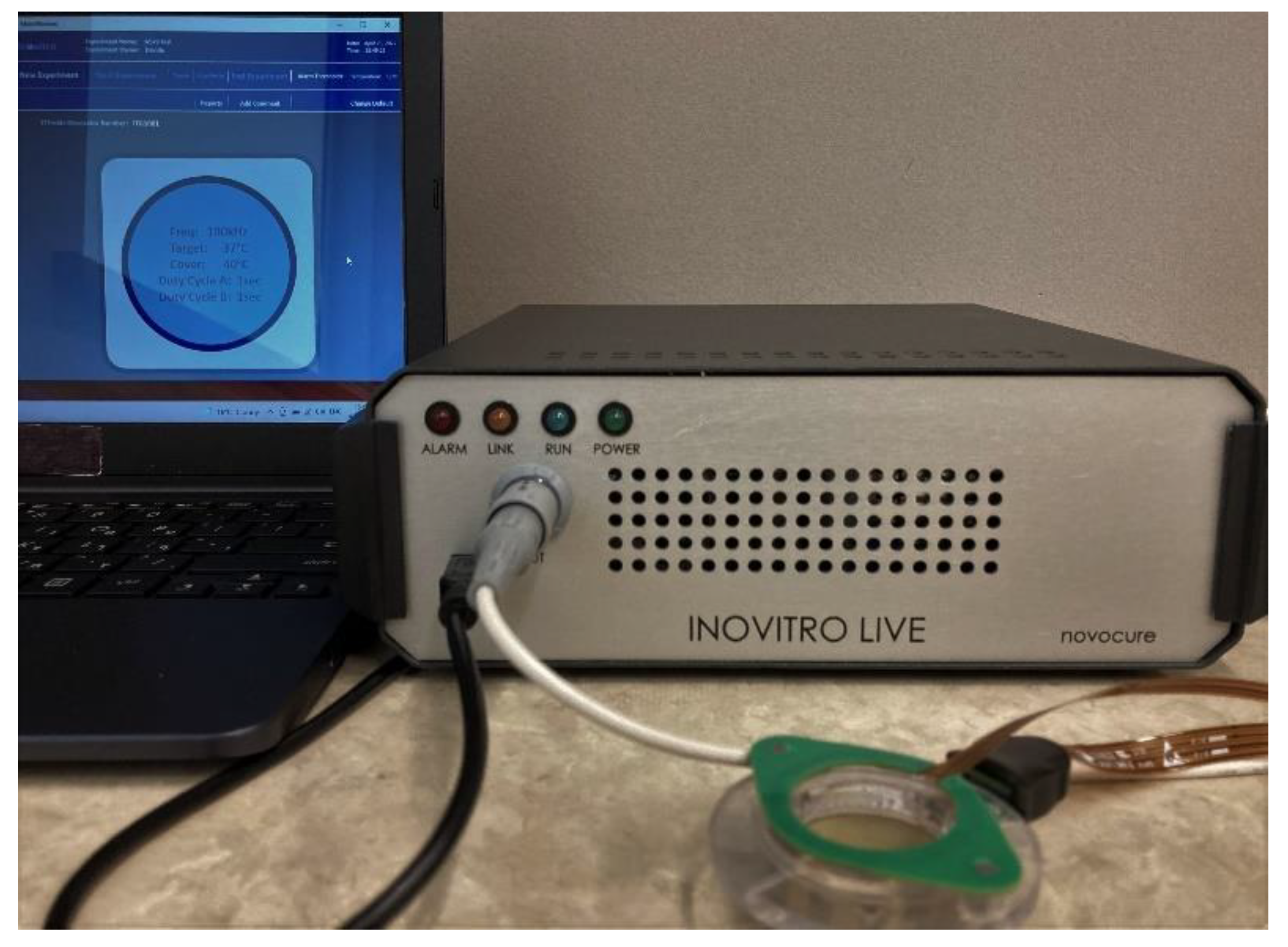
2.1. The Inovitro™ Live System
2.2. Cell Culture
2.3. TTFields Treatment
2.4. Live-Cell Imaging
2.5. Statistical Analysis
3. Results
3.1. TTFields Cause Mitotic and Cytokinetic Arrest in HeLa and MCF-10A Cells
3.2. Single and Two-Directional TTFields Exhibit Similar Inhibitory Effects on HeLa Cell Division
3.3. The Anti-Mitotic Effect of TTFields on HeLa Cells Is Stronger at 100 kHz vs. 200 kHz
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goodman, E.M.; Greenebaum, B.; Marron, M.T. Effects of Electromagnetic Fields on Molecules and Cells; Academic Press: Cambridge, MA, USA, 1995; Volume 158, pp. 279–338. [Google Scholar] [CrossRef]
- Taghian, T.; Narmoneva, D.A.; Kogan, A.B. Modulation of cell function by electric field: A high-resolution analysis. J. R. Soc. Interface 2015, 12, 20150153. [Google Scholar] [CrossRef] [PubMed]
- Markx, G.H. The use of electric fields in tissue engineering. Organogenesis 2008, 4, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Chu, K.F.; Dupuy, D.E. Thermal ablation of tumours: Biological mechanisms and advances in therapy. Nat. Rev. Cancer 2014, 14, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Malmivuo, J.; Plonsey, R. Bioelectromagnetism; Oxford University Press: New York, NY, USA, 1995. [Google Scholar]
- Davies, A.M.; Weinberg, U.; Palti, Y. Tumor treating fields: A new frontier in cancer therapy. Ann. N. Y. Acad. Sci. 2013, 1291, 86–95. [Google Scholar] [CrossRef]
- Kirson, E.D.; Gurvich, Z.; Schneiderman, R.; Dekel, E.; Itzhaki, A.; Wasserman, Y.; Schatzberger, R.; Palti, Y. Disruption of Cancer Cell Replication by Alternating Electric Fields. Cancer Res. 2004, 64, 3288–3295. [Google Scholar] [CrossRef]
- Kirson, E.D.; Dbaly, V.; Tovaryš, F.; Vymazal, J.; Soustiel, J.F.; Itzhaki, A.; Mordechovich, D.; Steinberg-Shapira, S.; Gurvich, Z.; Schneiderman, R.; et al. Alternating electric fields arrest cell proliferation in animal tumor models and human brain tumors. Proc. Natl. Acad. Sci. USA 2007, 104, 10152–10157. [Google Scholar] [CrossRef]
- Giladi, M.; Schneiderman, R.S.; Voloshin, T.; Porat, Y.; Munster, M.; Blat, R.; Sherbo, S.; Bomzon, Z.; Urman, N.; Itzhaki, A.; et al. Mitotic Spindle Disruption by Alternating Electric Fields Leads to Improper Chromosome Segregation and Mitotic Catastrophe in Cancer Cells. Sci. Rep. 2015, 5, 18046. [Google Scholar] [CrossRef]
- Gonzalez, C.F.; Remcho, V.T. Harnessing dielectric forces for separations of cells, fine particles and macromolecules. J. Chromatogr. A 2005, 1079, 59–68. [Google Scholar] [CrossRef]
- Gera, N.; Yang, A.; Holtzman, T.S.; Lee, S.X.; Wong, E.T.; Swanson, K.D. Tumor Treating Fields Perturb the Localization of Septins and Cause Aberrant Mitotic Exit. PLoS ONE 2015, 10, e0125269. [Google Scholar] [CrossRef] [Green Version]
- Giladi, M.; Weinberg, U.; Schneiderman, R.S.; Porat, Y.; Munster, M.; Voloshin, T.; Blatt, R.; Cahal, S.; Itzhaki, A.; Onn, A.; et al. Alternating Electric Fields (Tumor-Treating Fields Therapy) Can Improve Chemotherapy Treatment Efficacy in Non-Small Cell Lung Cancer Both In Vitro and In Vivo. Semin. Oncol. 2014, 41, S35–S41. [Google Scholar] [CrossRef]
- Voloshin, T.; Munster, M.; Blatt, R.; Shteingauz, A.; Roberts, P.C.; Schmelz, E.M.; Giladi, M.; Schneiderman, R.S.; Zeevi, E.; Porat, Y.; et al. Alternating electric fields (TTFields) in combination with paclitaxel are therapeutically effective against ovarian cancer cells in vitro and in vivo. Int. J. Cancer 2016, 139, 2850–2858. [Google Scholar] [CrossRef] [PubMed]
- Kanner, A.A.; Wong, E.T.; Villano, J.L.; Ram, Z. Post Hoc Analyses of Intention-to-Treat Population in Phase III Comparison of NovoTTF-100A™ System Versus Best Physician’s Choice Chemotherapy. Semin. Oncol. 2014, 41, S25–S34, Corrigendum in Semin. Oncol. 2015, 42, e56–e66. [Google Scholar] [CrossRef]
- Berger, T.R.; Wong, E.T. Tumor treating fields in neuro-oncology: Integration of alternating electric fields therapy into promising treatment strategies. Chin. Clin. Oncol. 2021, 10, 36. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.; Patel, C.B.; Pohling, C.; Young, C.; Song, J.; Flores, T.A.; Zeng, Y.; Joubert, L.M.; Arami, H.; Natarajan, A.; et al. Tumor treating fields increases membrane permeability in glioblastoma cells. Cell Death Discov. 2018, 4, 113. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, A.A.; Ho, M.C.; Chang, E.; Carlson, K.W.; Natarajan, A.; Marciano, T.; Bomzon, Z.; Patel, C.B. Permeabilizing Cell Membranes with Electric Fields. Cancers 2021, 13, 2283. [Google Scholar] [CrossRef] [PubMed]
- Karanam, N.K.; Srinivasan, K.; Ding, L.; Sishc, B.; Saha, D.; Story, M.D. Tumor-treating fields elicit a conditional vulnerability to ionizing radiation via the downregulation of BRCA1 signaling and reduced DNA double-strand break repair capacity in non-small cell lung cancer cell lines. Cell Death Dis. 2017, 8, e2711. [Google Scholar] [CrossRef]
- Karanam, N.K.; Ding, L.; Aroumougame, A.; Story, M.D. Tumor treating fields cause replication stress and interfere with DNA replication fork maintenance: Implications for cancer therapy. Transl. Res. 2020, 217, 33–46. [Google Scholar] [CrossRef]
- Voloshin, T.; Schneiderman, R.S.; Volodin, A.; Shamir, R.R.; Kaynan, N.; Zeevi, E.; Koren, L.; Klein-Goldberg, A.; Paz, R.; Giladi, M.; et al. Tumor Treating Fields (TTFields) Hinder Cancer Cell Motility through Regulation of Microtubule and Actin Dynamics. Cancers 2020, 12, 3016. [Google Scholar] [CrossRef]
- Kirson, E.D.; Giladi, M.; Gurvich, Z.; Itzhaki, A.; Mordechovich, D.; Schneiderman, R.S.; Wasserman, Y.; Ryffel, B.; Goldsher, D.; Palti, Y. Alternating electric fields (TTFields) inhibit metastatic spread of solid tumors to the lungs. Clin. Exp. Metastasis 2009, 26, 633–640. [Google Scholar] [CrossRef] [Green Version]
- Silginer, M.; Weller, M.; Stupp, R.; Roth, P. Biological activity of tumor-treating fields in preclinical glioma models. Cell Death Dis. 2017, 8, e2753. [Google Scholar] [CrossRef]
- Ho Kim, E.; Sook Song, H.; Hoon Yoo, S.; Yoon, M. Tumor treating fields inhibit glioblastoma cell migration, invasion and angiogenesis. Oncotarget 2016, 7, 65125–65136. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.M.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Ostrom, Q.T.; Gittleman, H.; Xu, J.; Kromer, C.; Wolinsky, Y.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2009–2013. Neuro Oncol. 2016, 18, v1–v75. [Google Scholar] [CrossRef] [PubMed]
- Fonkem, E.; Wong, E.T. NovoTTF-100A: A new treatment modality for recurrent glioblastoma. Expert Rev. Neurother. 2012, 12, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Wong, E.T.; Kanner, A.A.; Steinberg, D.; Engelhard, H.; Heidecke, V.; Kirson, E.D.; Taillibert, S.; Liebermann, F.; Dbalý, V.; et al. NovoTTF-100A versus physician’s choice chemotherapy in recurrent glioblastoma: A randomised phase III trial of a novel treatment modality. Eur. J. Cancer 2012, 48, 2192–2202. [Google Scholar] [CrossRef]
- Farber, O.; Weinberg, U.; Palti, Y. Phase III trial of tumor treating fields (TTFields) together with temozolomide (TMZ) com- pared to temozolomide alone in patients with newly diagnosed glioblastoma (GBM). Neuro Oncol. 2013, 15, iii75–iii84. [Google Scholar] [CrossRef]
- Stupp, R.; Taillibert, S.; Kanner, A.A.; Kesari, S.; Steinberg, D.M.; Toms, S.A.; Taylor, L.P.; Lieberman, F.; Silvani, A.; Fink, K.L.; et al. Maintenance Therapy With Tumor-Treating Fields Plus Temozolomide vs Temozolomide Alone for Glioblastoma: A Randomized Clinical Trial. J. Am. Med. Assoc. 2015, 314, 2535–2543. [Google Scholar] [CrossRef]
- Ceresoli, G.; Aerts, J.; Madrzak, J.; Dziadziuszko, R.; Ramlau, R.; Cedres, S.; Hiddinga, B.; Van Meerbeeck, J.; Mencoboni, M.; Planchard, D.; et al. STELLAR-Final Results of a Phase 2 Trial of TTFields with Chemotherapy for First-Line Treatment of Malignant Pleural Mesothelioma. J. Thorac. Oncol. 2018, 13, S397–S398. [Google Scholar] [CrossRef]
- Ceresoli, G.L.; Aerts, J.G.; Dziadziuszko, R.; Ramlau, R.; Cedres, S.; van Meerbeeck, J.P.; Mencoboni, M.; Planchard, D.; Chella, A.; Crino, L.; et al. Tumour Treating Fields in combination with pemetrexed and cisplatin or carboplatin as first-line treatment for unresectable malignant pleural mesothelioma (STELLAR): A multicentre, single-arm phase 2 trial. Lancet Oncol. 2019, 20, 1702–1709, Erratum in Lancet Oncol. 2020, 21, e70. [Google Scholar] [CrossRef]
- Davis, A.; Ke, H.; Kao, S.; Pavlakis, N. An Update on Emerging Therapeutic Options for Malignant Pleural Mesothelioma. Lung Cancer 2022, 13, 1–12. [Google Scholar] [CrossRef]
- Rominiyi, O.; Vanderlinden, A.; Clenton, S.J.; Bridgewater, C.; Al-Tamimi, Y.; Collis, S.J. Tumour treating fields therapy for glioblastoma: Current advances and future directions. Br. J. Cancer 2021, 124, 697–709. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, U.; Farber, O.; Giladi, M.; Bomzon, Z.; Kirson, E.D. 194TiP: LUNAR: Phase III study of front-line chemotherapy with TTFields for advanced squamous NSCLC. J. Thorac. Oncol. 2016, 11, S141. [Google Scholar] [CrossRef]
- Mehta, M.P.; Gondi, V.; Brown, P.D. METIS: A phase 3 study of radiosurgery with TTFields for 1-10 brain metastases from NSCLC. J. Clin. Oncol. 2017, 35, TPS9106. [Google Scholar] [CrossRef]
- Mehta, M.P.; Gondi, V.; Ahluwalia, M.; Brown, P.D. Phase III METIS study: Tumor treating fields (150 kHz) and radiosurgery for supra- and/or infratentorial brain metastases (1-10) from non-small cell lung cancer (NSCLC). Ann. Oncol. 2019, 30, ii70–ii71. [Google Scholar] [CrossRef]
- Kirson, E.D.; Giladi, M.; Bomzon, Z.; Weinberg, U.; Farber, O. INNOVATE-3: Phase 3 randomized, international study of tumor treating fields (200 kHz) concomitant with weekly paclitaxel for the treatment of platinum-resistant ovarian cancer. J. Clin. Oncol. 2018, 36, TPS5614. [Google Scholar] [CrossRef]
- Vergote, I.B.; Sehouli, J.; Fossati, R.; Coleman, R.; Monk, B.; Copeland, L.; O’malley, D. 403 Phase 3 trial of tumor treating fields concomitant with weekly paclitaxel for platinum-resistant ovarian cancer: ENGOT-OV50/GOG-329/INNOVATE-3. Int. J. Gynecol. Cancer 2020, 30, A113. [Google Scholar] [CrossRef]
- Picozzi, V.J.; Macarulla, T.; Philip, P.A.; Becerra, C.R.; Dragovich, T. PANOVA-3: A phase III study of tumor treating fields with nab-paclitaxel and gemcitabine for front-line treatment of locally advanced pancreatic adenocarcinoma (LAPC). J. Clin. Oncol. 2020, 38, TPS792. [Google Scholar] [CrossRef]
- Shteingauz, A.; Porat, Y.; Voloshin, T.; Schneiderman, R.S.; Munster, M.; Zeevi, E.; Kaynan, N.; Gotlib, K.; Giladi, M.; Kirson, E.D.; et al. AMPK-dependent autophagy upregulation serves as a survival mechanism in response to Tumor Treating Fields (TTFields). Cell Death Dis. 2018, 9, 1074. [Google Scholar] [CrossRef]
- Shi, P.; Tian, J.; Ulm, B.S.; Mallinger, J.C.; Khoshbouei, H.; Deleyrolle, L.P.; Sarkisian, M.R. Tumor Treating Fields Suppression of Ciliogenesis Enhances Temozolomide Toxicity. Front. Oncol. 2022, 12, 837589. [Google Scholar] [CrossRef]
- Slangen, P.L.; Porat, Y.; Mertz, M.; van den Broek, B.; Jalink, K.; de Gooijer, M.C.; van Tellingen, O.; Borst, G.R. Protocol for live-cell imaging during Tumor Treating Fields treatment with Inovitro Live. STAR Protoc. 2022, 3, 101246. [Google Scholar] [CrossRef]
- Porat, Y.; Giladi, M.; Schneiderman, R.S.; Blat, R.; Shteingauz, A.; Zeevi, E.; Munster, M.; Voloshin, T.; Kaynan, N.; Tal, O.; et al. Determining the Optimal Inhibitory Frequency for Cancerous Cells Using Tumor Treating Fields (TTFields). J. Vis. Exp. 2017, 123, e55820. [Google Scholar] [CrossRef] [PubMed]
- Rasband, W.S. ImageJ. Available online: https://imagej.nih.gov/ij/ (accessed on 11 August 2022).
- Schneider, C.A.; Rasband, W.S.; Eliceiri, K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 2012, 9, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Whitfield, M.L.; Sherlock, G.; Saldanha, A.J.; Murray, J.I.; Ball, C.A.; Alexander, K.E.; Matese, J.C.; Perou, C.M.; Hurt, M.M.; Brown, P.O.; et al. Identification of Genes Periodically Expressed in the Human Cell Cycle and Their Expression in Tumors. Mol. Biol. Cell 2002, 13, 1977–2000. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.Y.; Ma, W.L.; Liang, S.; Zeng, Y.; Shi, R.; Yu, H.L.; Xiao, W.W.; Zheng, W.L. Analysis of microRNA expression profiles during the cell cycle in synchronized HeLa cells. BMB Rep. 2009, 42, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Vitale, I.; Galluzzi, L.; Castedo, M.; Kroemer, G. Mitotic catastrophe: A mechanism for avoiding genomic instability. Nat. Rev. Mol. Cell Biol. 2011, 12, 385–392. [Google Scholar] [CrossRef]
- Kessler, A.F.; Frombling, G.E.; Gross, F.; Hahn, M.; Ernestus, R.I.; Lohr, M.; Hagemann, C. Effects of tumor treating fields (TTFields) on glioblastoma cells are augmented by mitotic checkpoint inhibition. Cell Death Discov. 2018, 4, 12. [Google Scholar] [CrossRef]
- Munster, M.; Gotlib, K.; Schneiderman, R.S.; Porat, Y.; Voloshin, T.; Davidi, S.; Shteingauz, A.; Kaynan, N.; Zeevi, E.; Giladi, M.; et al. Efficacy of Tumor Treating Fields (TTFields) in Combination with Cisplatin or Pemetrexed for the Treatment ofMesothelioma in Vitro and in Vivo. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, E679. [Google Scholar] [CrossRef]
- Mujib, S.; Alamsyah, F.; Taruno, W. Cell Death and Induced p53 Expression in Oral Cancer, HeLa, and Bone Marrow Mesenchyme Cells under the Exposure to Noncontact Electric Fields. Integr. Med. Int. 2017, 4, 161–170. [Google Scholar] [CrossRef]
- Mahgoub, E.O.; Hussain, A.; Sharifi, M.; Falahati, M.; Marei, H.E.; Hasan, A. The therapeutic effects of tumor treating fields on cancer and noncancerous cells. Arab. J. Chem. 2021, 14, 103386. [Google Scholar] [CrossRef]
- Li, X.; Yang, F.; Rubinsky, B. A Correlation Between Electric Fields That Target the Cell Membrane Potential and Dividing HeLa Cancer Cell Growth Inhibition. IEEE Trans. Biomed. Eng. 2021, 68, 1951–1956. [Google Scholar] [CrossRef]
- Blatt, R.; Davidi, S.; Munster, M.; Shteingauz, A.; Cahal, S.; Zeidan, A.; Marciano, T.; Bomzon, Z.; Haber, A.; Giladi, M.; et al. In Vivo Safety of Tumor Treating Fields (TTFields) Applied to the Torso. Front. Oncol. 2021, 11, 2459. [Google Scholar] [CrossRef] [PubMed]
- Wenger, C.; Miranda, P.C.; Salvador, R.; Thielscher, A.; Bomzon, Z.; Giladi, M.; Mrugala, M.M.; Korshoej, A.R. A Review on Tumor-Treating Fields (TTFields): Clinical Implications Inferred From Computational Modeling. IEEE Rev. Biomed. Eng. 2018, 11, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Jamous, S.; Comba, A.; Lowenstein, P.R.; Motsch, S. Self-organization in brain tumors: How cell morphology and cell density influence glioma pattern formation. PLoS Comput. Biol. 2020, 16, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Baker, G.J.; Yadav, V.N.; Motsch, S.; Koschmann, C.; Calinescu, A.A.; Mineharu, Y.; Camelo-Piragua, S.I.; Orringer, D.; Bannykh, S.; Nichols, W.S.; et al. Mechanisms of Glioma Formation: Iterative Perivascular Glioma Growth and Invasion Leads to Tumor Progression, VEGF-Independent Vascularization, and Resistance to Antiangiogenic Therapy. Neoplasia 2014, 16, 543–561. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Clelland, C.; Rahman, N. Pleural space. In Encyclopedia of Respiratory Medicine; Laurent, G.J., Shapiro, S.D., Eds.; Academic Press: Oxford, UK, 2006; pp. 397–402. [Google Scholar] [CrossRef]
- Vona, G.; Sabile, A.; Louha, M.; Sitruk, V.; Romana, S.; Schutze, K.; Capron, F.; Franco, D.; Pazzagli, M.; Vekemans, M.; et al. Isolation by Size of Epithelial Tumor Cells: A New Method for the Immunomorphological and Molecular Characterization of Circulating Tumor Cells. Am. J. Pathol. 2000, 156, 57–63. [Google Scholar] [CrossRef]
- Puck, T.T.; Marcus, P.I.; Cieciura, S.J. Clonal Growth of Mammalian Cells In Vitro: Growth Characteristics of Colonies from Single HeLa Cells with and without a “Feeder” Layer. J. Exp. Med. 1956, 103, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Milo, R.; Phillips, R. Cell Biology by the Numbers; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar] [CrossRef]
- Borle, A.B. Kinetic Analyses of Calcium Movements in HeLa Cell Cultures: I. Calcium influx. J. Gen. Physiol. 1969, 53, 43–56. [Google Scholar] [CrossRef] [Green Version]
- Jo, Y.; Sung, J.; Jeong, H.; Hong, S.; Jeong, Y.K.; Kim, E.H.; Yoon, M. Effectiveness of a Fractionated Therapy Scheme in Tumor Treating Fields Therapy. Technol. Cancer Res. Treat. 2019, 18, 1533033819845008. [Google Scholar] [CrossRef]
- Sato, S.; Rancourt, A.; Sato, Y.; Satoh, M.S. Single-cell lineage tracking analysis reveals that an established cell line comprises putative cancer stem cells and their heterogeneous progeny. Sci. Rep. 2016, 6, 23328. [Google Scholar] [CrossRef]
- Machado, C.M.; Schenka, A.; Vassallo, J.; Tamashiro, W.M.; Goncalves, E.M.; Genari, S.C.; Verinaud, L. Morphological characterization of a human glioma cell line. Cancer Cell Int. 2005, 5, 13. [Google Scholar] [CrossRef]
- Mullins, C.S.; Schneider, B.; Stockhammer, F.; Krohn, M.; Classen, C.F.; Linnebacher, M. Establishment and Characterization of Primary Glioblastoma Cell Lines from Fresh and Frozen Material: A Detailed Comparison. PLoS ONE 2013, 8, e71070. [Google Scholar] [CrossRef]
- Oraiopoulou, M.E.; Tzamali, E.; Tzedakis, G.; Vakis, A.; Papamatheakis, J. In Vitro/In Silico Study on the Role of Doubling Time Heterogeneity among Primary Glioblastoma Cell Lines. BioMed Res. Int. 2017, 2017, 8569328. [Google Scholar] [CrossRef] [PubMed]
- Relan, V.; Morrison, L.; Parsonson, K.; Clarke, B.E.; Duhig, E.E.; Windsor, M.N.; Matar, K.S.; Naidoo, R.; Passmore, L.; McCaul, E.; et al. Phenotypes and Karyotypes of Human Malignant Mesothelioma Cell Lines. PLoS ONE 2013, 8, e58132. [Google Scholar] [CrossRef]
- Ye, E.; Lee, J.E.; Lim, Y.S.; Yang, S.H.; Park, S.M. Effect of duty cycles of tumor-treating fields on glioblastoma cells and normal brain organoids. Int. J. Oncol. 2022, 60, 8, Erratum in Int. J. Oncol. 2022, 61, 107. [Google Scholar] [CrossRef] [PubMed]
- Havelka, D.; Cifra, M.; Kučera, O.; Pokorny, J.; Vrba, J. High-frequency electric field and radiation characteristics of cellular microtubule network. J. Theor. Biol. 2011, 286, 31–40. [Google Scholar] [CrossRef]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le, H.T.; Staelens, M.; Lazzari, D.; Chan, G.; Tuszyński, J.A. Real-Time Monitoring of the Effect of Tumour-Treating Fields on Cell Division Using Live-Cell Imaging. Cells 2022, 11, 2712. https://doi.org/10.3390/cells11172712
Le HT, Staelens M, Lazzari D, Chan G, Tuszyński JA. Real-Time Monitoring of the Effect of Tumour-Treating Fields on Cell Division Using Live-Cell Imaging. Cells. 2022; 11(17):2712. https://doi.org/10.3390/cells11172712
Chicago/Turabian StyleLe, Hoa T., Michael Staelens, Davide Lazzari, Gordon Chan, and Jack A. Tuszyński. 2022. "Real-Time Monitoring of the Effect of Tumour-Treating Fields on Cell Division Using Live-Cell Imaging" Cells 11, no. 17: 2712. https://doi.org/10.3390/cells11172712
APA StyleLe, H. T., Staelens, M., Lazzari, D., Chan, G., & Tuszyński, J. A. (2022). Real-Time Monitoring of the Effect of Tumour-Treating Fields on Cell Division Using Live-Cell Imaging. Cells, 11(17), 2712. https://doi.org/10.3390/cells11172712










