Abstract
Oral squamous cell carcinoma (OSCC) usually originates from the precancerous lesions of oral mucosa and accounts for approximately 90% of oral cancers. Current therapeutic approaches do not yet meet the needs of patients, and the 5-year survival rate of patients with OSCC is only 50%. Recent studies have revealed that the signal transducer and activator of transcription 3 (STAT3) plays a key role in the development and progression of OSCC. STAT3 is overexpressed and constitutively activated in OSCC cells, and promotes cancer cell proliferation and anti-apoptosis, migration and invasion, angiogenesis, radiotherapy resistance, and immune escape, as well as stem cell self-renewal and differentiation by regulating the transcription of its downstream target genes. Inhibitors of the STAT3 signaling pathway have shown the promising anticancer effects in vitro and in vivo, and STAT3 is expected to be a molecular target for the treatment of OSCC. In this review, we highlight the oncogenic significance of STAT3 in OSCC with an emphasis on the therapeutic approaches and effective small molecule inhibitors targeting STAT3. Finally, we also propose the potential research directions in the expectation of developing more specific STAT3 inhibitors for OSCC treatment.
1. Background
Oral squamous cell carcinoma (OSCC) represents the most frequent form of head and neck squamous cell carcinoma that is the sixth most common group of cancers worldwide [1,2]. OSCC originates from the tongue, palate, floor of mouth, alveolar ridge, buccal mucosa, and other areas of oral cavity, and accounts for about 90% of oral malignancies [3,4]. In 2020, about 377,713 new patients were diagnosed with lip and oral cavity cancers, and its number of deaths was around 177,757 worldwide. Most cases were discovered in Asia [5]. The risk factors for OSCC include smoking, excessive alcohol consumption, and betel nut chewing, exposure to carcinogens, immunodeficiency, irradiation, nutrition, and genetic susceptibility, as well as viral infections including human papillomavirus and herpes simplex virus [6]. The main biologic activity of OSCC is classified as highly, moderately, or poorly differentiated along with increased aggressiveness [7]. Histologically, OSCC exhibits grades ranging from well-differentiated keratinizing carcinoma to undifferentiated nonkeratinizing carcinoma, which is more apt to spread [8,9]. Patients with OSCC are asymptomatic in the early stages, and most patients are diagnosed when OSCC further progresses, resulting in the lower survival rate [10]. Tumor infiltration, lymph node metastasis, and high rates of local recurrence are the main factors leading to death in patients with OSCC [11]. Current treatment options for OSCC include surgery, chemotherapy, radiotherapy, or a combination of therapies, depending on factors such as the extent of the disease and the patient’s comorbidities [12]. However, the adverse effects of the treatment still exist. For example, salivary gland hypofunction is a common and permanent adverse effect of radiotherapy to the head and neck [13]. The common complications after selective neck dissection are spinal accessory nerve damage and shoulder dysfunction [14]. Systemic administration of chemotherapeutic drugs emphasizes the need to avoid the systemic undesired side effects. Targeted therapy for OSCC, which consists of immunotherapy, gene therapy, and bionic technology, has shown some promise in preliminary clinical studies, but further investigation is needed [15].
The signal transducer and activators of transcription (STAT) family are potential cytoplasmic transcription factors, including STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, and STAT6, which can be activated in response to cytokine and growth factor stimulation to mediate multiple intracellular signaling pathways [16]. STAT proteins are characterized by six functionally conserved domains. The N-terminal domain (NTD) mediates the formation of an anti-parallel dimer of un-phosphorylated STAT3; coiled-coil domain (CCD) is used to interact with regulatory proteins that positively or negatively regulate transcriptional activity; DNA-binding domain (DBD) can recognize specific DNA sequences of target genes; The linker domain (LD) is involved in nuclear export and DNA binding; the SH2 domain (SH2) is the most conserved STAT domain, involved in dimer formation, and plays a key role in signal transduction by binding to phosphorylated tyrosine residues of the receptor; the transcriptional activation domain (TAD) is a highly variable domain in length and sequence of STAT3, and regulates the transcriptional activation of target genes by interacting with other transcription factors [17]. The most widely studied one among the STAT family is STAT3, which consists of 770 amino acids and shares similar functional domains with other STAT family members. STAT3 can transmit signals from the cell membrane to the nucleus to activate target gene transcription and regulate a variety of cellular physiological activities, including cell proliferation, differentiation, apoptosis, angiogenesis, and immune system regulation [18]. Although STAT3 plays a crucial role in normal cells, constitutive activation of STAT3 in most human malignancies drives transcription of unscheduled genes and the transcription products subsequently promote tumor progression [19].
Recently, researchers have found that STAT3 is overexpressed and constitutively activated in OSCC and plays an important role in OSCC aggressiveness [20,21,22]. Growing evidence also suggests that STAT3 may be a potential molecular target and biomarker of OSCC, and STAT3 inhibitors have shown efficacy in inhibiting OSCC tumor growth and metastasis [23,24]. Thorough understanding of the roles of STAT3 in OSCC will facilitate the development of STAT3-targeted therapeutics. In this review, we focus on the protumor role of STAT3 in OSCC, and summarize the therapeutic strategies and representative small molecule inhibitors targeting STAT3. Finally, we outline more approaches to target STAT3 founded in other cancers, which may propose potential directions for further research to develop more specific STAT3 inhibitors for OSCC treatment.
2. The STAT3 Signaling Pathway
STAT3 is tightly regulated by negative modulators to maintain an inactive state in an unstimulated cell [25]. These negative modulators include members of the protein inhibitor of activated STAT (PIAS), suppressor of cytokine signaling (SOCS) family, cellular phosphatases (SHP1, SHP2, PTPN1, PTPN2, PTPRD, PTPRT, and DUSP22), as well as ubiquitin enzymes. The control of endogenous negative regulators can maintain the STAT3 signal as balanced and stable to perform physiological functions in normal cells [19]. The classical STAT3 signaling pathway is activated by the binding of cytokines or growth factors to their corresponding cell surface receptors. Extracellular ligands bind to cell surface receptors to form dimers, which then recruit and further activate Janus tyrosine kinase (JAK) [26,27]. Cytoplasmic tyrosine residues of the receptor are phosphorylated by activated JAKs to further recruit STAT3 to the phosphorylated tyrosine residues of the cytoplasmic receptor by interacting with the SH2 domain of STAT3. STAT3 is phosphorylated at tyrosine-705. Then, phosphorylated STAT3 (p-STAT3) monomers form homodimers via interactions between phosphorylated tyrosine-705 and the SH2 domain. STAT3 dimers further translocate to the nucleus and bind to DNA enhancer regions in a sequence-specific manner. This induces transcription of target genes critical for physiological and pathological functions [25,28]. Moreover, non-receptor tyrosine kinases such as Src and Abl can also lead to constitutive activation of STAT3 [29].
In the classical STAT3 signaling pathway, the p-STAT3 dimer is able to bind to the corresponding site on DNA and initiates nuclear transcription. Indeed, STAT3 is also localized in mitochondria as a monomer. Mitochondrial STAT3 (MitoSTAT3) can regulate complexes I and II to play a role of modulator for mitochondrial respiration [27,30]. MitoSTAT3 was shown to increase the activities of complex II, ATP synthase (complex V), and lactate dehydrogenase to maintain the glycolytic and oxidative phosphorylation, which contributed to the RAS-dependent oncogenic transformation of mouse embryonic fibroblasts, and inhibition of MitoSTAT3 stopped tumor growth [31,32]. MitoSTAT3’s improved bioenergetics may speed up early neoplastic lesions [33,34]. Unexpected STAT3 localization to the endoplasmic reticulum (ER) has also been discovered. STAT3-mediated IP3R3 downregulation in the ER was a major factor in anti-apoptotic effects of breast cancer cell lines [35]. These results suggest that a further non-canonical function played by constitutively phosphorylated STAT3 at its S727 residue promotes the growth of cancer and inhibits apoptosis, but the mechanism remains to be clarified [31,35,36]. The characteristics of activated STAT3 have been described above; however, it has also been discovered that inactivated STAT3 has bioactive properties. Unphosphorylated STAT3 monomers or dimers recognized specific DNA structures, which was significant for chromatin organization [37]. After IL-6 treatment, STAT3-mediated change of chromatin structure was significantly increased, which played a role in inflammation-mediated cancers [26]. However, the oncogenic role of unphosphorylated STAT3 needs further investigation.
3. The STAT3 Signaling Pathway in OSCC
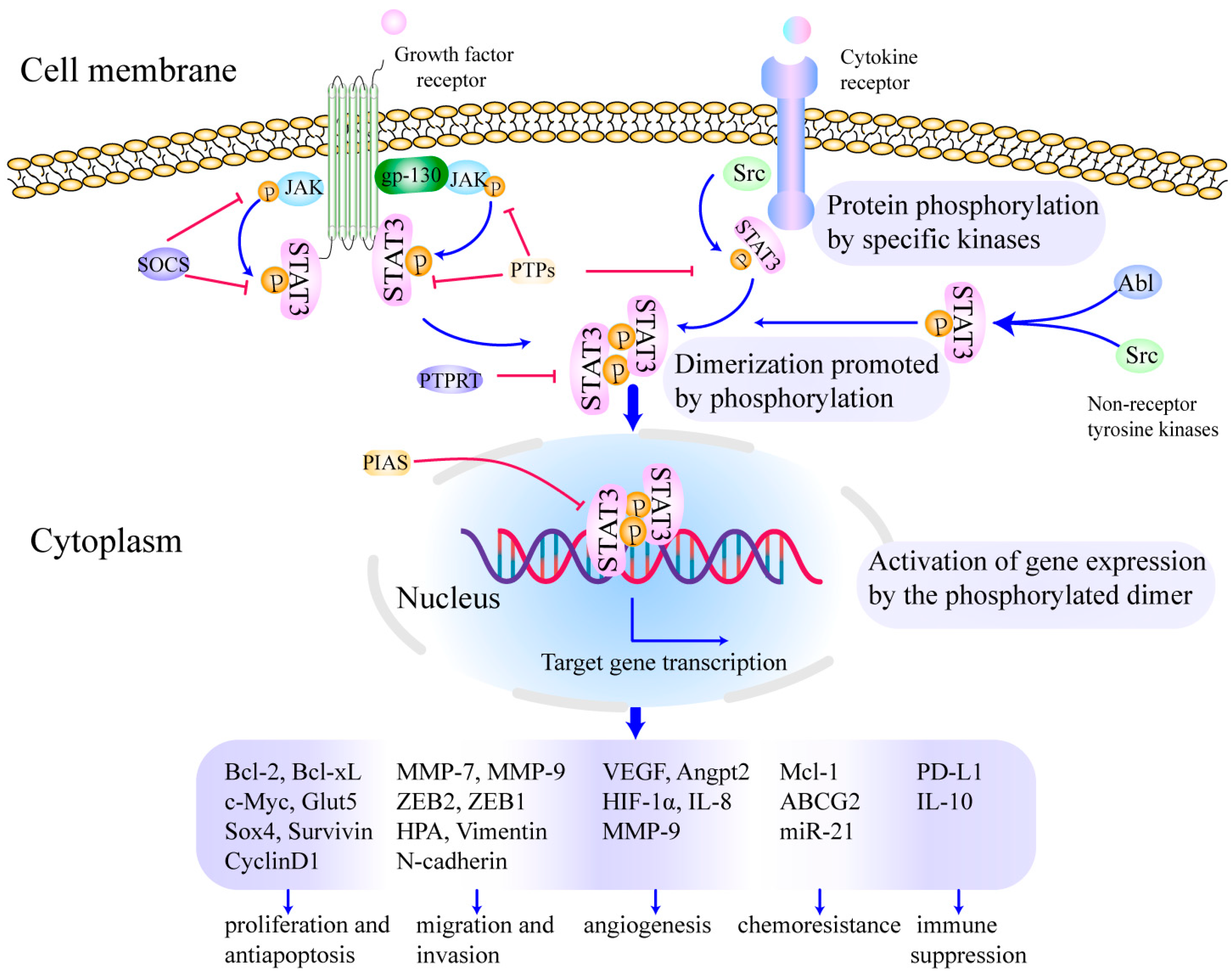
Studies have shown that overactivation of STAT3 in many types of tumors may depend on the following mechanisms: excessive stimulation caused by overexpressed cytokines and growth factors such as interleukin-6 (IL-6), interleukin-10 (IL-10), epidermal growth factor (EGF) as well as fibroblast growth factor (FGF); hyperactivation of receptors for cytokines or growth factors; elevated activity of cytoplasmic non-receptor tyrosine kinases, such as Src and Abl kinase; loss of negative regulation for STAT3 caused by inactivation or decreased expression of endogenous negative regulators, e.g., PIAS, SOCS, and PTPs. These mechanisms can induce uncontrolled cell growth, malignant cell transformation, angiogenesis, metastasis, invasion, and immune escape [38]. Importantly, STAT3 is overexpressed and constitutively activated in OSCC, which is highly related to OSCC initiation and progression (as shown in Figure 1). For example, a recent study verified that STAT3 was a direct target of mir-125b, and circPVT1 and LncRNA MALAT1 may promote OSCC cell growth by sponging mir-125b and increasing STAT3 expression [39,40]. In addition, endogenous negative regulators such as PTPN4, SOCS5 and SOCS6 were decreased in OSCC cells, which contributed to the upregulation of p-STAT3. The upregulated p-STAT3 promoted the OSCC progression [41,42]. Emerging research demonstrates the critical role of STAT3 in OSCC [20,24,43,44,45,46,47,48,49,50]; we herein present a comprehensive overview of its oncogenic functions in this section.
Figure 1.
Activation of STAT3 signaling promotes growth, metastasis, chemoresistance, immune suppression and angiogenesis in OSCC. The cytokines or growth factors bind to the corresponding receptors on the cell membrane, which further prompts STAT3 activation and subsequent regulates transcriptional activity. The whole process is divided into three steps as follows: (1) protein phosphorylation by specific kinases [19,26,27], (2) dimerization promoted by phosphorylation [51], (3) activation of gene expression by the phosphorylated dimer [52,53]. Finally, transcription and translation of the target gene regulate cell proliferation and anti-apoptosis, migration and invasion, chemoradiotherapy resistance and angiogenesis, as well as immune suppression in OSCC [22,54,55]. Reproduced/adopted in modified form from [56].
3.1. Role of STAT3 in OSCC Cell Proliferation and Anti-Apoptosis
Several studies have demonstrated that STAT3 promotes cell proliferation and inhibits apoptosis in OSCC by increasing the expression of target genes, including survivin, Mcl-1, c-Myc, Glut5, cyclin D1, B-cell lymphoma-2 (Bcl-2), and B-cell lymphoma extra -large (Bcl-xL) [22,57,58,59]. In OSCC, STAT3 directly bound to the c-Myc promoter and promoted its transcription [60,61]; this can be blocked by silencing upstream musashi RNA-binding protein 1 (MSI1) of STAT3 signaling [62]. LncRNA P4713 promoted OSCC cell proliferation via activating the JAK/STAT3/cyclinD1 pathway. After downregulation the expression level of P471, STAT3 was found to translocate from nucleus to cytoplasm accompanied by a decrease in phosphorylation levels, which attenuated tumor cell proliferation and migration capacity [63]. Porphyromonas gingivalis and Fusobacterium nucleatum were responsible for the upregulation of cyclin D1 via IL-6/STAT3 dependent-mechanism to drive the OSCC growth [64]. MiR-769-5p restrained the Bcl-2 protein level and increased the protein levels of Bcl-2 associated X protein (Bax) and cleaved-caspase 3 by inhibiting JAK1/STAT3 activity, suggesting the important role of STAT3 in promoting the OSCC growth [65]. Furthermore, STAT3 can promote the transcription of HNF1A-AS1 in OSCC cells, HNF1A-AS1 in turn activated the Notch signaling pathway to promote OSCC cell proliferation. Conversely, depletion of HNF1A-AS1 induced apoptosis and cell cycle arrest [66].
3.2. Role of STAT3 in OSCC Cell Migration and Invasion
Epithelial–mesenchymal transition (EMT) is an important biological mechanism underlying the metastasis of primary tumors [67]. During the EMT, the characteristic of epithelial cells will convert from epithelial cells highly expressing epithelial markers (E-cadherin) to mesenchymal cells acquiring the mesenchymal markers (N-cadherin and Vimentin). This transition can promote OSCC metastasis by enhancing migration and invasion [41,68]. A recent study unveiled that the enhanced JAK2/STAT3 pathway caused the EMT of OSCC cells, and EMT could be inhibited by the JAK2 inhibitor AG490 [69]. The activated JAK2/STAT3 signaling pathway decreased E-cadherin expression and increased N-cadherin and E-box binding zinc finger protein 2 (ZEB2) expression in OSCC cells, which induced OSCC growth and metastasis [70]. Furthermore, the role of STAT3 in promoting OSCC cell migration and invasion was also linked to the upregulated expression of matrix metalloproteinase 9 (MMP-9), MMP-7, E-box binding zinc finger protein 1 (ZEB1) [66,71,72]. For example, interleukin-22 (IL-22) and IL-6 were reported to promote the migration and invasion of OSCC cells by activating the JAK/STAT3/MMP-9 signaling pathway [66,72,73]. Moreover, the cytokine-inducible Src homology 2-containing protein (CISH) and SOCS1 increased metastasis of OSCC through promoting the activation of STAT3 [74,75].
Consistent with the above findings, the inhibition of the JAK2/STAT3 may significantly suppress p-STAT3-induced migration and invasion of OSCC cells. Terminal differentiation-induced non-coding RNA (TINCR) suppressed migration of OSCC by highly reducing the expression of JAK2, p-JAK2, STAT3, and p-STAT3 [76]. Aldehyde dehydrogenase 3A1 (ALDH3A1) and miR-144-3p acted as OSCC metastasis suppressors and inhibited EMT via downregulating the STAT3 signaling pathway in OSCC [77,78].
3.3. Role of STAT3 in Angiogenesis of OSCC
The pro-angiogenic role of STAT3 has been partially attributed to the upregulation of IL-8, MMP-9, vascular endothelial growth factor (VEGF), angiopoietin 2 (Angpt2), and hypoxia-inducible factor 1-alpha (HIF-1α) via p-STAT3 transactivation [79,80,81]. Recent studies demonstrated that CCL4 increased VEGF-C and Angpt2 production via activating the JAK2/STAT3 signaling pathways in OSCC cells, which was implicated in cell lymph angiogenesis and angiogenesis in OSCC [80,81]. In addition, PA28γ stimulated OSCC tumor angiogenesis in an IL-6/CCL2/STAT3 axis-dependent manner [82]. Conversely, humanized anti-Interleukin-6 receptor antibody Tocilizumab can bind to the IL-6-binding site of human IL-6R and competitively inhibits IL-6 signaling. A drastic reduction in STAT3 phosphorylation induced by Tocilizumab downregulated the expression of VEGF, IL-8, and MMP-9, which decreased microvessel density and vessel diameter in the OSCC xenograft model [79]. Diosmin also suppressed the abnormal expression of VEGF and HIF-1a to obstruct angiogenesis of buccal pouch carcinogenesis through preventing phosphorylation of JAK1/STAT3 [83].
3.4. Role of STAT3 in Chemoresistance of OSCC
It has been observed that blocking STAT3 signaling enhances the anticancer activity of chemotherapies in OSCC, thus endorsing a critical role of STAT3 in regulating the chemosensitivity of OSCC [84]. Overexpression and constitutive activation of the STAT3 signaling pathway have been shown to confer chemoresistance on OSCC cells. For example, cancer stem cell-derived extracellular vesicles (CSC-EVs) promoted chemoresistance, stemness, and the metastatic potential of oral cancer cells by enhancing PI3K/mTOR/STAT3 signaling [85]. To the best of our knowledge, several recent studies have revealed the mechanisms underlying STAT3-mediated chemoresistance in OSCC cell lines. Activation of STAT3 and AKT-mediated GSK3β inactivation upregulated Mcl-1 expression, which enhanced TPF resistance in OSCC [86]. Cisplatin treatment upregulated the programmed death ligand 2 (PD-L2) and drug efflux transporter ABCG2 expression in OSCC cell lines via STAT1/3 activation [87]. Indeed, the chemoresistance of cancer cells has been reported to depend on ABC transporter activity.
3.5. Role of STAT3 in Immune Suppression
Previous work suggested that STAT3 was a powerful regulator of tumor immunosuppression, and activation of the JAK2/STAT3/PD-L1 signaling axis played a crucial role in the immune escape of osteosarcoma and cervical cancer [88,89]. In OSCC cells, STAT3 also regulated the expression of PD-L1 [90]. Protein kinase D3 (PKD3) was a key kinase mediating the activation of STAT3. Elevated PKD3 expression promoted PD-L1 expression via activating STAT3 in OSCC [91]. STAT3-mediated PD-L1 upregulation affected the proliferation and functional characteristics of T cells [92]. STAT3 was also activated in tumor-associated immune cells to induce the expression of immune suppression related genes and contribute to immunosuppression in OSCC tumor microenvironment (TME) [93,94].
3.6. Role of STAT3 in OSCC Stem Cell Phenotypes
Recently, reports have shown that the JAK2/STAT3 signaling pathway also plays a critical role in the EMT and stemness of OSCC. For example, C-C chemokine receptor 7 (CCR7) and its ligand chemokine ligand 21 (CCL21) were reported to be abnormally abundant in OSCC tissues, and CCR7 expression was correlated with EMT and the stemness of OSCC. The treatment with JAK2 inhibitor AG490 could reduce the promotive effects of CCL21 on OSCC cells colony formation and sphere formation [21]. Moreover, blocking the activation of the Jak/Stat3 pathway significantly suppressed the colony forming, invasion, migration, microsphere forming, and xenograft forming abilities of OSCC cells [95]. Overall, these results demonstrated that the JAK/STAT3 signaling pathway may contribute to the stemness of OSCC cells.
3.7. Role of STAT3 in Autophagy of OSCC Cells
STAT3 phosphorylation status is capable of influencing autophagy in OSCC cells. Compound 59, an AMPK activator, inhibited JAK/STAT3 signaling, arrested cells in the G1 phase and promoted autophagy. These findings supported the potential of compound 59 for the treatment of OSCC patients through the suppression of STAT3 pathway [96]. Icaritin significantly inhibited the level of p-STAT3 in a dose- and time-dependent manners, and further suppressed proliferation, promoted apoptosis and autophagy [97]. However, more research is needed to understand the mechanism by which STAT3 affects OSCC autophagy.
3.8. Role of STAT3 in Radiosensitivity of OSCC Cells
Recently, increasingly more studies have shown STAT3 to contribute to radioresistance. Matsuoka et al. found that the IL-6/STAT3 pathway was relevant in resistance to radiation [98], and overexpression of STAT3 reduced the radiosensitivity of OSCC cells [99]. Yu et al. showed that the expression of Pre-B-cell leukaemia homeobox 1 (PBX1) was abnormally high in OSCC, and knockdown of PBX1 substantially enhanced sensitivity to radiation in OSCC cells by inhibiting STAT3 expression [100]. These studies suggested that STAT3 was not only involved in tumorigenesis and tumor development, but also lead to radioresistance. STAT3 is emerging as a promising target for radio-sensitization of cancer radiotherapy. The mechanism underlying STAT3-mediated radioresistance was related to the suppression of apoptosis and DNA damage induced by STAT3 signaling after radiotherapy [101]. STAT3 enhanced the transcription of apoptosis regulator Mcl-1 and cell cycle regulator cyclin D2 (CCND2) to decrease the sensitivity of cancer cells to radiation, according to more research on the glioma [102], as well as colorectal cancer [103].
3.9. Role of STAT3 in Immune Cells within the OSCC TME
TME is a highly complex and heterogenous ecosystem consisting of tumor infiltrating cancer cells, immune cells, and other cells. STAT3 is not only activated in cancer cells, but also becomes hyperactivated in immune cells within the OSCC TME. Some studies have suggested that activation of the JAK2/STAT signaling pathway impaired the antitumor activity of immune cells. For example, radiation treatment of head and neck cancer induced STAT3 signaling to enhance the abundance and function of regulatory T (Treg) cells and resistance to radiation therapy. STAT3 inhibition was beneficial in patients receiving radiation therapy [104]. IL-6-induced p-STAT3 increased PD-L1 and IL-10 expression in myeloid-derived suppressor cells (MDSCs), which impeded proliferation and activation of T cells and promoted Th17 cells differentiation in OSCC [94], and p-STAT3 inhibition (JSI-124) could alleviate immune suppression [42]. In addition, activation of STAT3 helped the immunosuppressive polarization of tumor-associated macrophages, which contributed to the tumor development [105]. On the contrary, overproduction of SOCS3 in dendritic cells can inhibit JAK2/STAT3 activation, as well as the differentiation and immune activity of dendritic cells, leading to their impaired antitumor effects [106]. The inconsistent role of STAT3 signaling in immune cells may be related to the difference in mechanism of action.
4. Targeting STAT3 for OSCC Prevention and Therapy
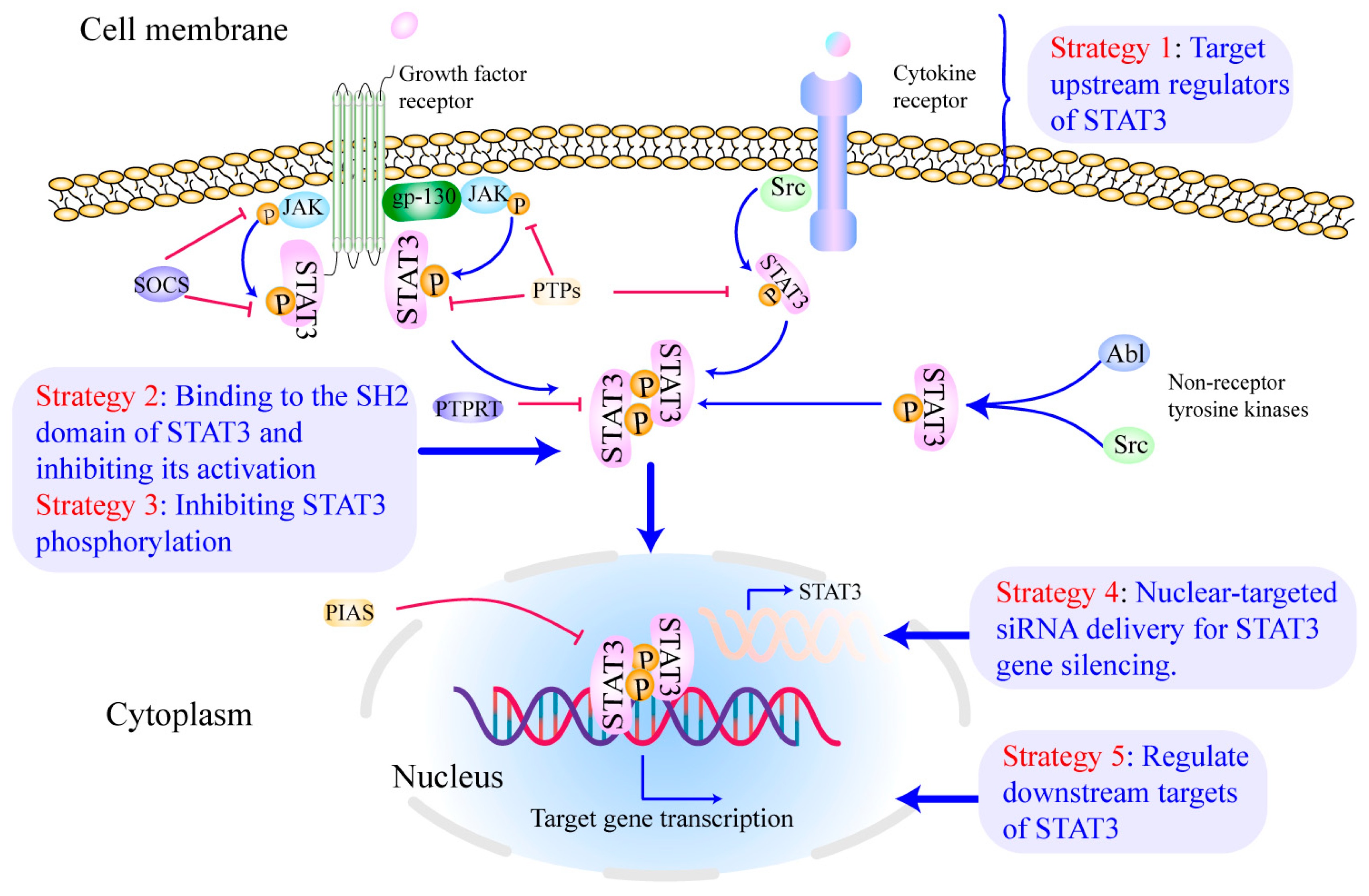
Abundant evidence has suggested that STAT3 may be a promising molecular target for OSCC treatment [107,108,109]. Targeting a druggable site on STAT3 or inhibiting the function of other proteins involved in the STAT3-dependent signaling cascade can directly or indirectly limit STAT3 signaling [28]. In this section, we discuss the current STAT3-targeting strategies (as shown in Figure 2) for treating and preventing OSCC, as well as the challenges in developing more specific and effective STAT3 inhibitors.
Figure 2.
Inhibiting STAT3 signaling at multiple levels for OSCC treatment. Currently, the majority of STAT3 inhibitors have been developed to target different sites in the STAT3 pathway: (1) targeting the upstream regulators of STAT3 [110,111], (2) binding to the SH2 domain of STAT3 and inhibiting its activation [112], (3) inhibiting STAT3 phosphorylation [113], (4) nuclear-targeted siRNA delivery for STAT3 gene silencing [114,115], (5) regulating downstream targets of STAT3 [116,117,118]. Reproduced/adopted in modified form from [56].
4.1. Target Upstream Regulators of STAT3
Various STAT3 inhibitors have been developed and shown some efficacy in OSCC in vitro and in vivo, which are showed in Table 1. A majority of STAT3 inhibitors have been identified to target the upstream regulators of STAT3 signaling. STAT3 is widely expressed and is transiently activated in response to EGF and IL-6. Therefore, small molecules and natural products that were able to inhibit IL-6 secretion and production, e.g., the highly pure neem leaf extract SCNE [119], magnolol [120], honokiol [107,108], and 2-O-Methylmagnolol [121], showed significant inhibitory effects on STAT3 signaling in OSCC. However, most of them also inhibited other signaling pathways in cancer cells and indicated a low level of specificity in targeting the STAT3 signaling pathway. As STAT3 is downstream to several cytokine and growth factor receptors and their associated JAKs, inhibiting JAKs by small molecular inhibitors represents a promising therapeutic option in OSCC. JAK2 inhibitors, including Licochalcone C [122] licochalcone D [123] and licochalcone H [124] were found to inhibit OSCC cell viability and induce apoptosis through tightly interacting with ATP-binding site of JAK2 and inhibiting the JAK2/STAT3 signaling pathway. In addition, all-trans retinoic acid (ATRA) showed great potential in cancer treatment through inhibition of p-STAT3 and p-JAK2 [125]. In recent years, Roxyl-ZR [126] and Alkannin [127] presented antitumor activities by hindering JAK1/STAT3 pathways in OSCC pathogenesis.

Table 1.
Summary of STAT3 inhibitors and their mechanisms of action for OSCC treatment.
Targeting the intrinsic STAT3 inhibitors, such as SOCS and PTPs, has been considered as a potential strategy for repressing STAT3 signaling pathway. For example, Bovine lactoferrin attenuated the growth of OSCC through increasing SOCS3 activation and then enhanced SOCS3-mediated STAT3 dephosphorylation and inactivation [132]. A microtubule inhibitor MPT0B098 suppressed the JAK2/STAT3 signaling pathway through modulation of SOCS3 stability in OSCC, which lead to sensitization of OSCC cells to MPT0B098 cytotoxicity [84]. Moreover, inactivated eIF5A2 induced by N1-guanyl-1,7-diaminoheptane (GC7) increased cisplatin chemosensitivity in OSCC cells via inhibition of the STAT3 signaling pathway [131]. Metformin also suppressed the invasion and migration of OSCC through the inhibition of PKM2/STAT3 [136,137]. Although many small molecule agents targeting the upstream regulators exhibited potential antitumor effects through the inhibition of STAT3, other off-target pathways were also activated. Therefore, more careful and thorough pre-clinical investigations must be implemented to prevent potential harmful effects.
4.2. Directly Bind to STAT3 and Inhibit Its Activation
STAT3 inhibitors have been developed to interact with the STAT3 domains, with a major focus on the SH2 domain and the DBD. For instance, N-4-hydroxyphenylretinamide (4-HPR) was highly bound at STAT3’s dimerization site and c-Abl and c-Src ATP-binding kinase sites to suppress cancer-promoting pathways including STAT3 phosphorylation, STAT3-DNA binding, and production of the trans-signaling enabling sIL-6R [138]. The STAT3 inhibitor compound (Stattic) was an SH2-domain inhibitor discovered by a high-throughput chemical library screen [109], and Stattic significantly attenuated EZH2 expression and local tumor invasion and outgrowth via targeting STAT3 [139]. However, STAT3 SH2-domain inhibitors moved slowly into clinical medicine due to high homology of the SH2 domain between STAT3 and other family members as well as high concentrations required for disruption of protein–protein interactions, which increased off-target toxicities [146].
4.3. Inhibit STAT3 Phosphorylation
Other STAT3 inhibitors were found to inhibit STAT3 phosphorylation, whereas they have not been investigated for the binding ability with STAT3 and ability to regulate upstream regulators of STAT3. For example, Niclosamide inhibited the migration and invasion in OSCC cells through the downregulation of p-STAT3 at Tyr705 [110]. Nitidine chloride acted as an apoptosis inducer in OSCC cells via inhibiting the phosphorylation of STAT3 and transcription of target genes [141,142]. Aspirin and anoctamin1 also suppressed the phosphorylation of STAT3 [140,145]. However, the mechanism of phosphorylation suppression needs to be further studied.
4.4. Nuclear-Targeted siRNA Delivery for STAT3 Gene Silencing
The STAT3 inhibitors we introduced above face many problems in their application. For example, how to target cancer cells or immune cells to improve the efficacy; the low cell permeability also prevents the inhibitors from being fully utilized; and the toxic side effects caused by off-target effects need to be addressed. Specificity and selectivity of these inhibitors of STAT3 have been questioned. Currently, a growing number of preclinical and clinical studies showed that antisense oligonucleotide (ASO)-induced STAT3 silence became a promising approach for lymphoma and lung cancer therapy. However, ASOs targeting STAT3 may cause thrombocytopenia, and toxicity limitations hindered the development of drugs [111,112]. In addition, STAT family members share a high degree of structural similarity with each other, which may induce the silence of other family members [147]. Moreover, transcription factors in different cell types usually regulate different gene networks and cellular functions, so how to target the specific cells is also crucial for the development of ideal therapeutic agents. The latest study suggested that ASO targeting STAT6 encapsulated in engineered exosome (exoASO-STAT6) was able to selectively silence STAT6 expression in macrophages [148]. This result may provide an inspiration to develop novel siRNA and antisense technology, which can specifically target STAT3 in tumor cells.
4.5. Regulate Downstream Targets of STAT3
As mentioned above, inhibitors targeting STAT3 or its upstream regulators may cause off-target effects, which are connected to the following factors: cell membranal or intracellular signals may deliver in a network, not in a single track; structural conservation of STAT family members; and diversity of STAT3 target genes. These underscore the need to develop inhibitors to regulate downstream targets of STAT3. Precise obstruction of STAT3 downstream signals could help prevent the unintended consequences of general STAT3 inhibition. For example, STAT3 has been reported to act as a transcription factor for Nicotinamide N-methyltransferase (NNMT), and upregulated NNMT in OSCC can contribute to proliferation and invasiveness [149,150]. Newly discovered NNMT inhibitors may be further proposed for OSCC treatment [113,114,115]. In addition, STAT3 was involved in the positive regulation of Sox4, Mcl-1, and so on. Genetic (siRNA) or pharmacological (Triptolide) inhibition of those targets suppressed OSCC growth in vivo [86,118]. Above all, the targeted molecules usually participate in complex signaling pathways. Although some STAT3 inhibitors have entered clinical trials in human OSCC or other malignancy (as shown in Table 2), future study should fully understand the role of STAT3 signaling in OSCC progression, which will aid in the discovery of more specific targeted therapeutics.

Table 2.
Summary of STAT3 inhibitors in clinical trials.
5. Conclusions
Although some progress has been made in the treatment of OSCC, its prognosis remains poor, with a 5-year survival rate of nearly 50% [10]. A comprehensive understanding of the genetic and molecular disorders of OSCC is critical for early diagnosis, appropriate treatment, and improved prognosis of patients with OSCC. The STAT3 oncogene has been reported to be overexpressed and constitutively activated in OSCC, and is associated with the poor survival outcomes [23,58]. STAT3 drives proliferation and anti-apoptosis, migration and invasion, chemoradiotherapy resistance and angiogenesis, as well as immune evasion of OSCC cells, which highlights the enormous therapeutic potential of STAT3 inhibitors.
Interestingly, contrary to its accepted tumor-promoting role, a fraction of research has shown an opposite role of STAT3 in cancer cells. It was observed that STAT3 knockdown promoted the growth of MDA-MB-231 cell-derived xenograft tumors [175]. Another finding also supported the role of STAT3 activation as a marker of favorable outcome in ER-positive/HER2-positive breast cancer patients [176]. These results imply that the oncogenic role of STAT3 in tumors might be context specific. STAT3 may be a negative regulator of certain cancer types, and therapies targeting STAT3 may therefore need to consider the origin of the tumor type.
Many STAT3-targeted therapies have been successfully developed and have shown efficacy in preclinical models of OSCC in vitro and in vivo. However, cancers including OSCC are multifaceted heterogeneous diseases [177]. OSCC has been reported to harbor multiple genetic alterations, which contribute to its initiation and progression. Therefore, STAT3 inhibition combined with other targeted therapies may be more effective for OSCC. Furthermore, many small molecule agents with potential therapeutic effects for OSCC should be further studied with a view to achieving precise drug delivery, avoiding drug side effects, and translating research findings into clinical applications. In summary, it is essential to have a comprehensive understanding of STAT3 and develop the effective approaches to inhibit the STAT3 signaling pathway with high selectivity and specificity for the treatment of OSCC.
Author Contributions
Funding
This work was supported by the Natural Science Foundation Project from Jilin Provincial Department of Science and Technology (20200201329JC), Outstanding Young and Middle-aged Backbone Talents Project from Jilin Province Department of Finance (JCSZ2019378-14), Natural Science Foundation Project from Department of Science and Technology of Liaoning Province (2021-MS-175), and Bethune Planned Research project from Jilin University (2018B27).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Leemans, C.R.; Snijders, P.J.F.; Brakenhoff, R.H. The molecular landscape of head and neck cancer. Nat. Rev. Cancer 2018, 18, 269–282. [Google Scholar] [CrossRef] [PubMed]
- Cancer Genome Atlas Network. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015, 517, 576–582.
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Kalogirou, E.M.; Tosios, K.I.; Christopoulos, P.F. The Role of Macrophages in Oral Squamous Cell Carcinoma. Front. Oncol. 2021, 11, 611115. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.Q.M. Head and Neck Cancer. N. Engl. J. Med. 2020, 382, 60–72. [Google Scholar] [CrossRef]
- Woolgar, J.A. Histopathological prognosticators in oral and oropharyngeal squamous cell carcinoma. Oral Oncol. 2006, 42, 229–239. [Google Scholar] [CrossRef]
- Hashibe, M.; Brennan, P.; Chuang, S.C.; Boccia, S.; Castellsague, X.; Chen, C.; Curado, M.P.; Dal Maso, L.; Daudt, A.W.; Fabianova, E.; et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: Pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol. Biomark. Prev. 2009, 18, 541–550. [Google Scholar] [CrossRef]
- Argiris, A.; Karamouzis, M.V.; Raben, D.; Ferris, R.L. Head and neck cancer. Lancet 2008, 371, 1695–1709. [Google Scholar] [CrossRef]
- Chi, A.C.; Day, T.A.; Neville, B.W. Oral cavity and oropharyngeal squamous cell carcinoma--an update. CA A Cancer J. Clin. 2015, 65, 401–421. [Google Scholar] [CrossRef] [PubMed]
- Hingsammer, L.; Seier, T.; Ikenberg, J.; Schumann, P.; Zweifel, D.; Rücker, M.; Bredell, M.; Lanzer, M. The influence of lymph node ratio on survival and disease recurrence in squamous cell carcinoma of the tongue. Int. J. Oral Maxillofac. Surg. 2019, 48, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Colevas, A.D.; Yom, S.S.; Pfister, D.G.; Spencer, S.; Adelstein, D.; Adkins, D.; Brizel, D.M.; Burtness, B.; Busse, P.M.; Caudell, J.J.; et al. NCCN Guidelines Insights: Head and Neck Cancers, Version 1.2018. J. Natl. Compr. Cancer Netw. 2018, 16, 479–490. [Google Scholar] [CrossRef] [PubMed]
- Mercadante, V.; Al Hamad, A.; Lodi, G.; Porter, S.; Fedele, S. Interventions for the management of radiotherapy-induced xerostomia and hyposalivation: A systematic review and meta-analysis. Oral Oncol. 2017, 66, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Garreau, B.; Dubreuil, P.A.; Bondaz, M.; Majoufre, C.; Etchebarne, M. The necessity of level IIb dissection for clinically negative neck oral squamous cell carcinoma. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 658–660. [Google Scholar] [CrossRef]
- Li, H.; Zhang, Y.; Xu, M.; Yang, D. Current trends of targeted therapy for oral squamous cell carcinoma. J. Cancer Res. Clin. Oncol. 2022, 148, 2169–2186. [Google Scholar] [CrossRef]
- Darnell, J.E., Jr.; Kerr, I.M.; Stark, G.R. Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science 1994, 264, 1415–1421. [Google Scholar] [CrossRef]
- Xiong, A.; Yang, Z.; Shen, Y.; Zhou, J.; Shen, Q. Transcription Factor STAT3 as a Novel Molecular Target for Cancer Prevention. Cancers 2014, 6, 926–957. [Google Scholar] [CrossRef]
- Bowman, T.; Garcia, R.; Turkson, J.; Jove, R. STATs in oncogenesis. Oncogene 2000, 19, 2474–2488. [Google Scholar] [CrossRef]
- Johnson, D.E.; O’Keefe, R.A.; Grandis, J.R. Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat. Rev. Clin. Oncol. 2018, 15, 234–248. [Google Scholar] [CrossRef]
- Gkouveris, I.; Nikitakis, N.; Avgoustidis, D.; Karanikou, M.; Rassidakis, G.; Sklavounou, A. ERK1/2, JNK and STAT3 activation and correlation with tumor differentiation in oral SCC. Histol. Histopathol. 2017, 32, 1065–1076. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Shao, Z.; Jiang, E.; Zhou, X.; Wang, L.; Wang, H.; Luo, X.; Chen, Q.; Liu, K.; Shang, Z. CCL21/CCR7 interaction promotes EMT and enhances the stemness of OSCC via a JAK2/STAT3 signaling pathway. J. Cell. Physiol. 2020, 235, 5995–6009. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Fang, J.; Lai, W.; Hu, Y.; Li, L.; Zhong, Y.; Yang, S.; He, D.; Liu, R.; Tang, Q. IL-6/STAT3 Axis Activates Glut5 to Regulate Fructose Metabolism and Tumorigenesis. Int. J. Biol. Sci. 2022, 18, 3668–3675. [Google Scholar] [CrossRef] [PubMed]
- Macha, M.A.; Matta, A.; Kaur, J.; Chauhan, S.S.; Thakar, A.; Shukla, N.K.; Gupta, S.D.; Ralhan, R. Prognostic significance of nuclear pSTAT3 in oral cancer. Head Neck 2011, 33, 482–489. [Google Scholar] [CrossRef]
- Pindiprolu, S.H.; Pindiprolu, S. CD133 receptor mediated delivery of STAT3 inhibitor for simultaneous elimination of cancer cells and cancer stem cells in oral squamous cell carcinoma. Med. Hypotheses 2019, 129, 109241. [Google Scholar] [CrossRef]
- Zou, S.; Tong, Q.; Liu, B.; Huang, W.; Tian, Y.; Fu, X. Targeting STAT3 in Cancer Immunotherapy. Mol. Cancer 2020, 19, 145. [Google Scholar] [CrossRef]
- Yu, H.; Lee, H.; Herrmann, A.; Buettner, R.; Jove, R. Revisiting STAT3 signalling in cancer: New and unexpected biological functions. Nat. Rev. Cancer 2014, 14, 736–746. [Google Scholar] [CrossRef]
- Garbers, C.; Aparicio-Siegmund, S.; Rose-John, S. The IL-6/gp130/STAT3 signaling axis: Recent advances towards specific inhibition. Curr. Opin. Immunol. 2015, 34, 75–82. [Google Scholar] [CrossRef]
- Thilakasiri, P.S.; Dmello, R.S.; Nero, T.L.; Parker, M.W.; Ernst, M.; Chand, A.L. Repurposing of drugs as STAT3 inhibitors for cancer therapy. Semin. Cancer Biol. 2021, 68, 31–46. [Google Scholar] [CrossRef]
- Karras, J.G.; Wang, Z.; Huo, L.; Howard, R.G.; Frank, D.A.; Rothstein, T.L. Signal transducer and activator of transcription-3 (STAT3) is constitutively activated in normal, self-renewing B-1 cells but only inducibly expressed in conventional B lymphocytes. J. Exp. Med. 1997, 185, 1035–1042. [Google Scholar] [CrossRef]
- Wegrzyn, J.; Potla, R.; Chwae, Y.J.; Sepuri, N.B.; Zhang, Q.; Koeck, T.; Derecka, M.; Szczepanek, K.; Szelag, M.; Gornicka, A.; et al. Function of mitochondrial Stat3 in cellular respiration. Science 2009, 323, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Gough, D.J.; Corlett, A.; Schlessinger, K.; Wegrzyn, J.; Larner, A.C.; Levy, D.E. Mitochondrial STAT3 supports Ras-dependent oncogenic transformation. Science 2009, 324, 1713–1716. [Google Scholar] [CrossRef] [PubMed]
- An, H.; Heo, J.S.; Kim, P.; Lian, Z.; Lee, S.; Park, J.; Hong, E.; Pang, K.; Park, Y.; Ooshima, A.; et al. Tetraarsenic hexoxide enhances generation of mitochondrial ROS to promote pyroptosis by inducing the activation of caspase-3/GSDME in triple-negative breast cancer cells. Cell Death Dis. 2021, 12, 159. [Google Scholar] [CrossRef] [PubMed]
- Kang, R.; Loux, T.; Tang, D.; Schapiro, N.E.; Vernon, P.; Livesey, K.M.; Krasinskas, A.; Lotze, M.T.; Zeh, H.J., III. The expression of the receptor for advanced glycation endproducts (RAGE) is permissive for early pancreatic neoplasia. Proc. Natl. Acad. Sci. USA 2012, 109, 7031–7036. [Google Scholar] [CrossRef]
- Kang, R.; Tang, D.; Lotze, M.T.; Zeh, H.J., III. AGER/RAGE-mediated autophagy promotes pancreatic tumorigenesis and bioenergetics through the IL6-pSTAT3 pathway. Autophagy 2012, 8, 989–991. [Google Scholar] [CrossRef]
- Avalle, L.; Camporeale, A.; Morciano, G.; Caroccia, N.; Ghetti, E.; Orecchia, V.; Viavattene, D.; Giorgi, C.; Pinton, P.; Poli, V. STAT3 localizes to the ER, acting as a gatekeeper for ER-mitochondrion Ca(2+) fluxes and apoptotic responses. Cell Death Differ. 2019, 26, 932–942. [Google Scholar] [CrossRef]
- Gough, D.J.; Marié, I.J.; Lobry, C.; Aifantis, I.; Levy, D.E. STAT3 supports experimental K-RasG12D-induced murine myeloproliferative neoplasms dependent on serine phosphorylation. Blood 2014, 124, 2252–2261. [Google Scholar] [CrossRef]
- Timofeeva, O.A.; Chasovskikh, S.; Lonskaya, I.; Tarasova, N.I.; Khavrutskii, L.; Tarasov, S.G.; Zhang, X.; Korostyshevskiy, V.R.; Cheema, A.; Zhang, L.; et al. Mechanisms of unphosphorylated STAT3 transcription factor binding to DNA. J. Biol. Chem. 2012, 287, 14192–14200. [Google Scholar] [CrossRef]
- Tolomeo, M.; Cascio, A. The Multifaced Role of STAT3 in Cancer and Its Implication for Anticancer Therapy. Int. J. Mol. Sci. 2021, 22, 603. [Google Scholar] [CrossRef]
- He, T.; Li, X.; Xie, D.; Tian, L. Overexpressed circPVT1 in oral squamous cell carcinoma promotes proliferation by serving as a miRNA sponge. Mol. Med. Rep. 2019, 20, 3509–3518. [Google Scholar] [CrossRef]
- Chang, S.M.; Hu, W.W. Long non-coding RNA MALAT1 promotes oral squamous cell carcinoma development via microRNA-125b/STAT3 axis. J. Cell. Physiol. 2018, 233, 3384–3396. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Dong, Y.; Song, D. Inhibition of microRNA-15b-5p Attenuates the Progression of Oral Squamous Cell Carcinoma via Modulating the PTPN4/STAT3 Axis. Cancer Manag. Res. 2020, 12, 10559–10572. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Xiang, L.; Xu, G. LncRNA MEG3 suppresses migration and promotes apoptosis by sponging miR-548d-3p to modulate JAK-STAT pathway in oral squamous cell carcinoma. IUBMB Life 2019, 71, 882–890. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Du, F.; Gong, X.; Xu, P. Circ_0005320 promotes oral squamous cell carcinoma tumorigenesis by sponging microRNA-486-3p and microRNA-637. Bioengineered 2022, 13, 440–454. [Google Scholar] [CrossRef] [PubMed]
- Cao, M.; Tian, K.; Sun, W.; Xu, J.; Tang, Y.; Wu, S. MicroRNA-141-3p inhibits the progression of oral squamous cell carcinoma via targeting PBX1 through the JAK2/STAT3 pathway. Exp. Ther. Med. 2022, 23, 97. [Google Scholar] [CrossRef] [PubMed]
- Crawford, M.; Liu, X.; Cheng, Y.L.; Tsai, R.Y. Nucleostemin upregulation and STAT3 activation as early events in oral epithelial dysplasia progression to squamous cell carcinoma. Neoplasia 2021, 23, 1289–1299. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, K.; Oikawa, M.; Miki, Y.; Takahashi, T.; Kumamoto, H. Immunohistochemical assessment of growth factor signaling molecules: MAPK, Akt, and STAT3 pathways in oral epithelial precursor lesions and squamous cell carcinoma. Odontology 2020, 108, 91–101. [Google Scholar] [CrossRef]
- Yakin, M.; Seo, B.; Rich, A. Tunicamycin-induced endoplasmic reticulum stress up-regulates tumour-promoting cytokines in oral squamous cell carcinoma. Cytokine 2019, 120, 130–143. [Google Scholar] [CrossRef]
- Meram, A.T.; Chen, J.; Patel, S.; Kim, D.D.; Shirley, B.; Covello, P.; Coppola, D.; Wei, E.X.; Ghali, G.; Kevil, C.G.; et al. Hydrogen Sulfide Is Increased in Oral Squamous Cell Carcinoma Compared to Adjacent Benign Oral Mucosae. Anticancer. Res. 2018, 38, 3843–3852. [Google Scholar] [CrossRef]
- Liu, S.; Ye, D.; Wang, T.; Guo, W.; Song, H.; Liao, Y.; Xu, D.; Zhu, H.; Zhang, Z.; Deng, J. Repression of GPRC5A is associated with activated STAT3, which contributes to tumor progression of head and neck squamous cell carcinoma. Cancer Cell Int. 2017, 17, 34. [Google Scholar] [CrossRef]
- Zhang, E.; Li, Z.; Xu, Z.; Duan, W.; Sun, C.; Lu, L. Frizzled2 mediates the migration and invasion of human oral squamous cell carcinoma cells through the regulation of the signal transducer and activator of transcription-3 signaling pathway. Oncol. Rep. 2015, 34, 3061–3067. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Shen, Y.; Wang, S.; Shen, Q.; Zhou, X. The role of STAT3 in leading the crosstalk between human cancers and the immune system. Cancer Lett. 2018, 415, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Sgrignani, J.; Garofalo, M.; Matkovic, M.; Merulla, J.; Catapano, C.V.; Cavalli, A. Structural Biology of STAT3 and Its Implications for Anticancer Therapies Development. Int. J. Mol. Sci. 2018, 19, 1591. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Kortylewski, M.; Pardoll, D. Crosstalk between cancer and immune cells: Role of STAT3 in the tumour microenvironment. Nat. Rev. Immunol. 2007, 7, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Xiang, F.; Feng, Y.; Gao, F.; Ge, S.; Wang, C.; Zhang, X.; Wang, N. Neutrophils Promote Tumor Progression in Oral Squamous Cell Carcinoma by Regulating EMT and JAK2/STAT3 Signaling Through Chemerin. Front. Oncol. 2022, 12, 812044. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Li, J.; Shen, X.; Lyu, J.; Yan, C.; Tang, B.; Ma, W.; Xie, H.; Zhao, L.; Cheng, L.; et al. Oral Microbiota from Periodontitis Promote Oral Squamous Cell Carcinoma Development via γδ T Cell Activation. mSystems 2022, e0046922. [Google Scholar] [CrossRef]
- Qin, J.J.; Yan, L.; Zhang, J.; Zhang, W.D. STAT3 as a potential therapeutic target in triple negative breast cancer: A systematic review. J. Exp. Clin. Cancer Res. 2019, 38, 195. [Google Scholar] [CrossRef]
- Alam, M.; Mishra, R. Bcl-xL expression and regulation in the progression, recurrence, and cisplatin resistance of oral cancer. Life Sci. 2021, 280, 119705. [Google Scholar] [CrossRef]
- Wei, L.Y.; Lin, H.C.; Tsai, F.C.; Ko, J.Y.; Kok, S.H.; Cheng, S.J.; Lee, J.J.; Chia, J.S. Effects of Interleukin-6 on STAT3-regulated signaling in oral cancer and as a prognosticator of patient survival. Oral Oncol. 2022, 124, 105665. [Google Scholar] [CrossRef]
- Deepak Roshan, V.G.; Sinto, M.S.; Thomas, S.; Kannan, S. Cyclin D1 overexpression associated with activation of STAT3 in oral carcinoma patients from South India. J. Cancer Res. Ther. 2018, 14, 403–408. [Google Scholar] [CrossRef]
- Chuerduangphui, J.; Ekalaksananan, T.; Chaiyarit, P.; Patarapadungkit, N.; Chotiyano, A.; Kongyingyoes, B.; Promthet, S.; Pientong, C. Effects of arecoline on proliferation of oral squamous cell carcinoma cells by dysregulating c-Myc and miR-22, directly targeting oncostatin M. PLoS ONE 2018, 13, e0192009. [Google Scholar] [CrossRef] [PubMed]
- Chuerduangphui, J.; Pientong, C.; Chaiyarit, P.; Patarapadungkit, N.; Chotiyano, A.; Kongyingyoes, B.; Promthet, S.; Swangphon, P.; Wongjampa, W.; Ekalaksananan, T. Effect of human papillomavirus 16 oncoproteins on oncostatin M upregulation in oral squamous cell carcinoma. Med. Oncol. 2016, 33, 83. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.F.; Zhang, H.C.; Feng, X.M.; Song, X.M.; Wu, Y.N. Knockdown of MSI1 inhibits the proliferation of human oral squamous cell carcinoma by inactivating STAT3 signaling. Int. J. Mol. Med. 2019, 44, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, Y.; Li, X.; Ren, X.; Xia, J.; Wang, Z.; Cheng, B.; Wang, Y. Long non-coding RNA P4713 contributes to the malignant phenotypes of oral squamous cell carcinoma by activating the JAK/STAT3 pathway. Int. J. Clin. Exp. Pathol. 2017, 10, 10947–10958. [Google Scholar] [PubMed]
- Binder Gallimidi, A.; Fischman, S.; Revach, B.; Bulvik, R.; Maliutina, A.; Rubinstein, A.M.; Nussbaum, G.; Elkin, M. Periodontal pathogens Porphyromonas gingivalis and Fusobacterium nucleatum promote tumor progression in an oral-specific chemical carcinogenesis model. Oncotarget 2015, 6, 22613–22623. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Xu, X.M.; Feng, Y. MiR-769-5p inhibits cancer progression in oral squamous cell carcinoma by directly targeting JAK1/STAT3 pathway. Neoplasma 2020, 67, 528–536. [Google Scholar] [CrossRef]
- Liu, Z.; Li, H.; Fan, S.; Lin, H.; Lian, W. STAT3-induced upregulation of long noncoding RNA HNF1A-AS1 promotes the progression of oral squamous cell carcinoma via activating Notch signaling pathway. Cancer Biol. Ther. 2019, 20, 444–453. [Google Scholar] [CrossRef]
- Vaidya, A.M.; Sun, Z.; Ayat, N.; Schilb, A.; Liu, X.; Jiang, H.; Sun, D.; Scheidt, J.; Qian, V.; He, S.; et al. Systemic Delivery of Tumor-Targeting siRNA Nanoparticles against an Oncogenic LncRNA Facilitates Effective Triple-Negative Breast Cancer Therapy. Bioconjugate Chem. 2019, 30, 907–919. [Google Scholar] [CrossRef]
- Wu, Q.; Zheng, Z.; Zhang, J.; Piao, Z.; Xin, M.; Xiang, X.; Wu, A.; Zhao, T.; Huang, S.; Qiao, Y.; et al. Chordin-Like 1 Regulates Epithelial-to-Mesenchymal Transition and Metastasis via the MAPK Signaling Pathway in Oral Squamous Cell Carcinoma. Front. Oncol. 2022, 12, 862751. [Google Scholar] [CrossRef]
- Wang, Y.; Jing, Y.; Ding, L.; Zhang, X.; Song, Y.; Chen, S.; Zhao, X.; Huang, X.; Pu, Y.; Wang, Z.; et al. Epiregulin reprograms cancer-associated fibroblasts and facilitates oral squamous cell carcinoma invasion via JAK2-STAT3 pathway. J. Exp. Clin. Cancer Res. 2019, 38, 274. [Google Scholar] [CrossRef]
- Jiang, X.; Huang, Z.; Sun, X.; Zheng, X.; Liu, J.; Shen, J.; Jia, B.; Luo, H.; Mai, Z.; Chen, G.; et al. CCL18-NIR1 promotes oral cancer cell growth and metastasis by activating the JAK2/STAT3 signaling pathway. BMC Cancer 2020, 20, 632. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.P.; Chen, K.C.; Chen, M.Y.; Huang, L.Y.; Su, A.Y.; Chiang, W.F.; Huang, W.T.; Huang, T.T. Epigenetic Deregulation of Protein Tyrosine Kinase 6 Promotes Carcinogenesis of Oral Squamous Cell Carcinoma. Int. J. Mol. Sci. 2022, 23, 4495. [Google Scholar] [CrossRef] [PubMed]
- Komine-Aizawa, S.; Aizawa, S.; Takano, C.; Hayakawa, S. Interleukin-22 promotes the migration and invasion of oral squamous cell carcinoma cells. Immunol. Med. 2020, 43, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Alves, A.; Diel, L.; Ramos, G.; Pinto, A.; Bernardi, L.; Yates, J., III; Lamers, M. Tumor microenvironment and Oral Squamous Cell Carcinoma: A crosstalk between the inflammatory state and tumor cell migration. Oral Oncol. 2021, 112, 105038. [Google Scholar] [CrossRef]
- Peng, H.Y.; Hsiao, J.R.; Chou, S.T.; Hsu, Y.M.; Wu, G.H.; Shieh, Y.S.; Shiah, S.G. MiR-944/CISH mediated inflammation via STAT3 is involved in oral cancer malignance by cigarette smoking. Neoplasia 2020, 22, 554–565. [Google Scholar] [CrossRef]
- Baba, O.; Hasegawa, S.; Nagai, H.; Uchida, F.; Yamatoji, M.; Kanno, N.I.; Yamagata, K.; Sakai, S.; Yanagawa, T.; Bukawa, H. MicroRNA-155-5p is associated with oral squamous cell carcinoma metastasis and poor prognosis. J. Oral Pathol. Med. 2016, 45, 248–255. [Google Scholar] [CrossRef]
- Zhuang, Z.; Huang, J.; Wang, W.; Wang, C.; Yu, P.; Hu, J.; Liu, H.; Yin, H.; Hou, J.; Liu, X. Down-Regulation of Long Non-Coding RNA TINCR Induces Cell Dedifferentiation and Predicts Progression in Oral Squamous Cell Carcinoma. Front. Oncol. 2020, 10, 624752. [Google Scholar] [CrossRef]
- Qu, Y.; He, Y.; Yang, Y.; Li, S.; An, W.; Li, Z.; Wang, X.; Han, Z.; Qin, L. ALDH3A1 acts as a prognostic biomarker and inhibits the epithelial mesenchymal transition of oral squamous cell carcinoma through IL-6/STAT3 signaling pathway. J. Cancer 2020, 11, 2621–2631. [Google Scholar] [CrossRef]
- Li, X.; Li, Y.; Jiang, C.; Chen, L.; Gan, N. MicroRNA-144-3p Inhibits Tumorigenesis of Oral Squamous Cell Carcinoma by downregulating ERO1L. J. Cancer 2020, 11, 759–768. [Google Scholar] [CrossRef]
- Shinriki, S.; Jono, H.; Ota, K.; Ueda, M.; Kudo, M.; Ota, T.; Oike, Y.; Endo, M.; Ibusuki, M.; Hiraki, A.; et al. Humanized anti-interleukin-6 receptor antibody suppresses tumor angiogenesis and in vivo growth of human oral squamous cell carcinoma. Clin. Cancer Res. 2009, 15, 5426–5434. [Google Scholar] [CrossRef]
- Lu, C.C.; Tsai, H.C.; Yang, D.Y.; Wang, S.W.; Tsai, M.H.; Hua, C.H.; Chen, K.J.; Chen, M.Y.; Lien, M.Y.; Tang, C.H. The Chemokine CCL4 Stimulates Angiopoietin-2 Expression and Angiogenesis via the MEK/ERK/STAT3 Pathway in Oral Squamous Cell Carcinoma. Biomedicines 2022, 10, 1612. [Google Scholar] [CrossRef] [PubMed]
- Lien, M.Y.; Tsai, H.C.; Chang, A.C.; Tsai, M.H.; Hua, C.H.; Wang, S.W.; Tang, C.H. Chemokine CCL4 Induces Vascular Endothelial Growth Factor C Expression and Lymphangiogenesis by miR-195-3p in Oral Squamous Cell Carcinoma. Front. Immunol. 2018, 9, 412. [Google Scholar] [CrossRef]
- Liu, S.; Liu, D.; Zeng, X.; Wang, J.; Liu, J.; Cheng, J.; Lei, K.; Bai, H.; Ji, N.; Zhou, M.; et al. PA28γ acts as a dual regulator of IL-6 and CCL2 and contributes to tumor angiogenesis in oral squamous cell carcinoma. Cancer Lett. 2018, 428, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Rajasekar, M.; Suresh, K.; Sivakumar, K. Diosmin induce apoptosis through modulation of STAT-3 signaling in 7,12 dimethylbenz(a)anthracene induced harmster buccal pouch carcinogenesis. Biomed. Pharmacother. 2016, 83, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.Y.; Cheng, Y.C.; Hsu, Y.M.; Wu, G.H.; Kuo, C.C.; Liou, J.P.; Chang, J.Y.; Jin, S.L.; Shiah, S.G. MPT0B098, a Microtubule Inhibitor, Suppresses JAK2/STAT3 Signaling Pathway through Modulation of SOCS3 Stability in Oral Squamous Cell Carcinoma. PLoS ONE 2016, 11, e0158440. [Google Scholar] [CrossRef]
- Chen, J.H.; Wu, A.T.H.; Bamodu, O.A.; Yadav, V.K.; Chao, T.Y.; Tzeng, Y.M.; Mukhopadhyay, D.; Hsiao, M.; Lee, J.C. Ovatodiolide Suppresses Oral Cancer Malignancy by Down-Regulating Exosomal Mir-21/STAT3/β-Catenin Cargo and Preventing Oncogenic Transformation of Normal Gingival Fibroblasts. Cancers 2019, 12, 56. [Google Scholar] [CrossRef]
- Maji, S.; Shriwas, O.; Samal, S.K.; Priyadarshini, M.; Rath, R.; Panda, S.; Das Majumdar, S.K.; Muduly, D.K.; Dash, R. STAT3- and GSK3β-mediated Mcl-1 regulation modulates TPF resistance in oral squamous cell carcinoma. Carcinogenesis 2019, 40, 173–183. [Google Scholar] [CrossRef]
- Sudo, S.; Kajiya, H.; Okano, S.; Sasaki, M.; Katsumata, Y.; Ohno, J.; Ikebe, T.; Hiraki, A.; Okabe, K. Cisplatin-induced programmed cell death ligand-2 expression is associated with metastasis ability in oral squamous cell carcinoma. Cancer Sci. 2020, 111, 1113–1123. [Google Scholar] [CrossRef]
- Jing, D.; Wu, W.; Chen, X.; Xiao, H.; Zhang, Z.; Chen, F.; Zhang, Z.; Liu, J.; Shao, Z.; Pu, F. Quercetin encapsulated in folic acid-modified liposomes is therapeutic against osteosarcoma by non-covalent binding to the JH2 domain of JAK2 Via the JAK2-STAT3-PDL1. Pharmacol. Res. 2022, 182, 106287. [Google Scholar] [CrossRef]
- Zhou, C.; Wei, W.; Ma, J.; Yang, Y.; Liang, L.; Zhang, Y.; Wang, Z.; Chen, X.; Huang, L.; Wang, W.; et al. Cancer-secreted exosomal miR-1468-5p promotes tumor immune escape via the immunosuppressive reprogramming of lymphatic vessels. Mol. Ther. 2021, 29, 1512–1528. [Google Scholar] [CrossRef]
- Wu, L.; Deng, W.W.; Huang, C.F.; Bu, L.L.; Yu, G.T.; Mao, L.; Zhang, W.F.; Liu, B.; Sun, Z.J. Expression of VISTA correlated with immunosuppression and synergized with CD8 to predict survival in human oral squamous cell carcinoma. Cancer Immunol. Immunother. 2017, 66, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Cui, B.; Chen, J.; Luo, M.; Wang, L.; Chen, H.; Kang, Y.; Wang, J.; Zhou, X.; Feng, Y.; Zhang, P. Protein kinase D3 regulates the expression of the immunosuppressive protein, PD-L1, through STAT1/STAT3 signaling. Int. J. Oncol. 2020, 56, 909–920. [Google Scholar] [CrossRef] [PubMed]
- Maruse, Y.; Kawano, S.; Jinno, T.; Matsubara, R.; Goto, Y.; Kaneko, N.; Sakamoto, T.; Hashiguchi, Y.; Moriyama, M.; Toyoshima, T.; et al. Significant association of increased PD-L1 and PD-1 expression with nodal metastasis and a poor prognosis in oral squamous cell carcinoma. Int. J. Oral Maxillofac. Surg. 2018, 47, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liu, S.; Qu, D.; Wang, K.; Zhang, L.; Jing, X.; Li, C.; Wei, F.; Qu, X. Kif4A mediate the accumulation and reeducation of THP-1 derived macrophages via regulation of CCL2-CCR2 expression in crosstalking with OSCC. Sci. Rep. 2017, 7, 2226. [Google Scholar] [CrossRef]
- Dar, A.A.; Patil, R.S.; Pradhan, T.N.; Chaukar, D.A.; D’Cruz, A.K.; Chiplunkar, S.V. Myeloid-derived suppressor cells impede T cell functionality and promote Th17 differentiation in oral squamous cell carcinoma. Cancer Immunol. Immunother. 2020, 69, 1071–1086. [Google Scholar] [CrossRef]
- You, Y.; Tian, Z.; Du, Z.; Wu, K.; Xu, G.; Dai, M.; Wang, Y.; Xiao, M. M1-like tumor-associated macrophages cascade a mesenchymal/stem-like phenotype of oral squamous cell carcinoma via the IL6/Stat3/THBS1 feedback loop. J. Exp. Clin. Cancer Res. 2022, 41, 10. [Google Scholar] [CrossRef]
- Weng, J.R.; Dokla, E.M.E.; Bai, L.Y.; Chen, C.S.; Chiu, S.J.; Shieh, T.M. A 5’ AMP-Activated Protein Kinase Enzyme Activator, Compound 59, Induces Autophagy and Apoptosis in Human Oral Squamous Cell Carcinoma. Basic Clin. Pharmacol. Toxicol. 2018, 123, 21–29. [Google Scholar] [CrossRef]
- Yang, J.G.; Lu, R.; Ye, X.J.; Zhang, J.; Tan, Y.Q.; Zhou, G. Icaritin Reduces Oral Squamous Cell Carcinoma Progression via the Inhibition of STAT3 Signaling. Int. J. Mol. Sci. 2017, 18, 132. [Google Scholar] [CrossRef]
- Matsuoka, Y.; Nakayama, H.; Yoshida, R.; Hirosue, A.; Nagata, M.; Tanaka, T.; Kawahara, K.; Sakata, J.; Arita, H.; Nakashima, H.; et al. IL-6 controls resistance to radiation by suppressing oxidative stress via the Nrf2-antioxidant pathway in oral squamous cell carcinoma. Br. J. Cancer 2016, 115, 1234–1244. [Google Scholar] [CrossRef]
- Jia, L.; Huang, P.; Lin, T.; Lin, C.; Ding, X.; Lin, L.; Zhu, L.; Zhou, Z. CircPUM1 Knockdown Confers Radiosensitivity in Oral Squamous Cell Carcinoma by Regulating the miR-580/STAT3 Pathway. Front. Genet. 2022, 13, 907219. [Google Scholar] [CrossRef]
- Yu, D.; Ma, Y.; Feng, C.; Ma, Z.; Guo, J.; Chen, H.; He, T.; Guo, J.; Sun, X.; Qin, Q.; et al. PBX1 Increases the Radiosensitivity of Oesophageal Squamous Cancer by Targeting of STAT3. Pathol. Oncol. Res. 2020, 26, 2161–2168. [Google Scholar] [CrossRef] [PubMed]
- Sugase, T.; Takahashi, T.; Serada, S.; Fujimoto, M.; Hiramatsu, K.; Ohkawara, T.; Tanaka, K.; Miyazaki, Y.; Makino, T.; Kurokawa, Y.; et al. SOCS1 Gene Therapy Improves Radiosensitivity and Enhances Irradiation-Induced DNA Damage in Esophageal Squamous Cell Carcinoma. Cancer Res. 2017, 77, 6975–6986. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Ran, H.; Song, S.; Liu, W.; Zou, W.; Jiang, B.; Zhao, H.; Shao, B. Overexpression of RPN2 suppresses radiosensitivity of glioma cells by activating STAT3 signal transduction. Mol. Med. 2020, 26, 43. [Google Scholar] [CrossRef]
- Park, S.Y.; Lee, C.J.; Choi, J.H.; Kim, J.H.; Kim, J.W.; Kim, J.Y.; Nam, J.S. The JAK2/STAT3/CCND2 Axis promotes colorectal Cancer stem cell persistence and radioresistance. J. Exp. Clin. Cancer Res. 2019, 38, 399. [Google Scholar] [CrossRef] [PubMed]
- Oweida, A.J.; Darragh, L.; Phan, A.; Binder, D.; Bhatia, S.; Mueller, A.; Court, B.V.; Milner, D.; Raben, D.; Woessner, R.; et al. STAT3 Modulation of Regulatory T Cells in Response to Radiation Therapy in Head and Neck Cancer. J. Natl. Cancer Inst. 2019, 111, 1339–1349. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; He, Y.; Wang, B.; Li, J.; Qin, L. ALDH3A1 overexpression in OSCC inhibits inflammation via phospho-Ser727 at STAT3 in tumor-associated macrophages. Oral Dis. 2022. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.X.; Tan, X.Y.; Huang, H.S.; Li, Y.T.; Liu, B.L.; Liu, K.S.; Chen, X.; Chen, Z.; Guan, X.Y.; Zou, C.; et al. Targeting cancer-associated fibroblast-secreted WNT2 restores dendritic cell-mediated antitumour immunity. Gut 2022, 71, 333–344. [Google Scholar] [CrossRef]
- Chi, J.; Liu, Y.; Yang, L.; Yang, J. Silencing of B7H4 Represses the Development of Oral Squamous Cell Carcinoma Through Promotion of M1 Macrophage Polarization. J. Oral Maxillofac. Surg. 2022, 80, 1408–1423. [Google Scholar] [CrossRef]
- Li, Z.; Wang, X.; Jia, R. Poly(rC) binding protein 1 represses the translation of STAT3 through 5’ UTR. Curr. Gene Ther. 2022, 22, 397–405. [Google Scholar] [CrossRef]
- Xiao, L.; Li, X.; Cao, P.; Fei, W.; Zhou, H.; Tang, N.; Liu, Y. Interleukin-6 mediated inflammasome activation promotes oral squamous cell carcinoma progression via JAK2/STAT3/Sox4/NLRP3 signaling pathway. J. Exp. Clin. Cancer Res. 2022, 41, 166. [Google Scholar] [CrossRef]
- Chang, M.T.; Lee, S.P.; Fang, C.Y.; Hsieh, P.L.; Liao, Y.W.; Lu, M.Y.; Tsai, L.L.; Yu, C.C.; Liu, C.M. Chemosensitizing effect of honokiol in oral carcinoma stem cells via regulation of IL-6/Stat3 signaling. Environ. Toxicol. 2018, 33, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.S.; Yao, C.J.; Chuang, S.E.; Yeh, C.T.; Lee, L.M.; Chen, R.M.; Chao, W.J.; Whang-Peng, J.; Lai, G.M. Honokiol inhibits sphere formation and xenograft growth of oral cancer side population cells accompanied with JAK/STAT signaling pathway suppression and apoptosis induction. BMC Cancer 2016, 16, 245. [Google Scholar] [CrossRef] [PubMed]
- Kraskouskaya, D.; Duodu, E.; Arpin, C.C.; Gunning, P.T. Progress towards the development of SH2 domain inhibitors. Chem. Soc. Rev. 2013, 42, 3337–3370. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ding, R.; Han, Z.; Ma, Z.; Wang, Y. Targeting of cell cycle and let-7a/STAT3 pathway by niclosamide inhibits proliferation, migration and invasion in oral squamous cell carcinoma cells. Biomed. Pharmacother. 2017, 96, 434–442. [Google Scholar] [CrossRef]
- Hong, D.; Kurzrock, R.; Kim, Y.; Woessner, R.; Younes, A.; Nemunaitis, J.; Fowler, N.; Zhou, T.; Schmidt, J.; Jo, M.; et al. AZD9150, a next-generation antisense oligonucleotide inhibitor of STAT3 with early evidence of clinical activity in lymphoma and lung cancer. Sci. Transl. Med. 2015, 7, 314ra185. [Google Scholar] [CrossRef]
- Reilley, M.J.; McCoon, P.; Cook, C.; Lyne, P.; Kurzrock, R.; Kim, Y.; Woessner, R.; Younes, A.; Nemunaitis, J.; Fowler, N.; et al. STAT3 antisense oligonucleotide AZD9150 in a subset of patients with heavily pretreated lymphoma: Results of a phase 1b trial. J. Immunother. Cancer 2018, 6, 119. [Google Scholar] [CrossRef]
- van Haren, M.J.; Zhang, Y.; Thijssen, V.; Buijs, N.; Gao, Y.; Mateuszuk, L.; Fedak, F.A.; Kij, A.; Campagna, R.; Sartini, D.; et al. Macrocyclic peptides as allosteric inhibitors of nicotinamide N-methyltransferase (NNMT). RSC Chem. Biol. 2021, 2, 1546–1555. [Google Scholar] [CrossRef]
- Gao, Y.; van Haren, M.J.; Buijs, N.; Innocenti, P.; Zhang, Y.; Sartini, D.; Campagna, R.; Emanuelli, M.; Parsons, R.B.; Jespers, W.; et al. Potent Inhibition of Nicotinamide N-Methyltransferase by Alkene-Linked Bisubstrate Mimics Bearing Electron Deficient Aromatics. J. Med. Chem. 2021, 64, 12938–12963. [Google Scholar] [CrossRef]
- van Haren, M.J.; Gao, Y.; Buijs, N.; Campagna, R.; Sartini, D.; Emanuelli, M.; Mateuszuk, L.; Kij, A.; Chlopicki, S.; Escudé Martinez de Castilla, P.; et al. Esterase-Sensitive Prodrugs of a Potent Bisubstrate Inhibitor of Nicotinamide N-Methyltransferase (NNMT) Display Cellular Activity. Biomolecules 2021, 11, 1357. [Google Scholar] [CrossRef]
- Morris, J.; Gonzales, C.B.; De La Chapa, J.J.; Cabang, A.B.; Fountzilas, C.; Patel, M.; Orozco, S.; Wargovich, M.J. The Highly Pure Neem Leaf Extract, SCNE, Inhibits Tumorigenesis in Oral Squamous Cell Carcinoma via Disruption of Pro-tumor Inflammatory Cytokines and Cell Signaling. Front. Oncol. 2019, 9, 890. [Google Scholar] [CrossRef]
- Peng, C.Y.; Yu, C.C.; Huang, C.C.; Liao, Y.W.; Hsieh, P.L.; Chu, P.M.; Yu, C.H.; Lin, S.S. Magnolol inhibits cancer stemness and IL-6/Stat3 signaling in oral carcinomas. J. Formos. Med. Assoc. 2021, 121, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.H.; Fang, J.Y.; Wu, S.J.; Liu, Y.W.; Chan, C.W.; Chuang, S.Y.; Chen, C.Y. 2-O-Methylmagnolol Induces Apoptosis and Inhibits IL-6/STAT3 Signaling in Oral Squamous Cell Carcinoma. Cell. Physiol. Biochem. 2018, 50, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.N.; Seo, J.H.; Lee, M.H.; Kim, C.; Kim, E.; Yoon, G.; Cho, S.S.; Cho, Y.S.; Choi, H.W.; Shim, J.H.; et al. Licochalcone C induced apoptosis in human oral squamous cell carcinoma cells by regulation of the JAK2/STAT3 signaling pathway. J. Cell. Biochem. 2018, 119, 10118–10130. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.H.; Choi, H.W.; Oh, H.N.; Lee, M.H.; Kim, E.; Yoon, G.; Cho, S.S.; Park, S.M.; Cho, Y.S.; Chae, J.I.; et al. Licochalcone D directly targets JAK2 to induced apoptosis in human oral squamous cell carcinoma. J. Cell. Physiol. 2019, 234, 1780–1793. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.N.; Oh, K.B.; Lee, M.H.; Seo, J.H.; Kim, E.; Yoon, G.; Cho, S.S.; Cho, Y.S.; Choi, H.W.; Chae, J.I.; et al. JAK2 regulation by licochalcone H inhibits the cell growth and induces apoptosis in oral squamous cell carcinoma. Phytomedicine 2019, 52, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.J.; He, M.J.; Zhou, G. All-trans retinoic acid induces anti-tumor effects via STAT3 signaling inhibition in oral squamous cell carcinoma and oral dysplasia. J. Oral Pathol. Med. 2019, 48, 832–839. [Google Scholar] [CrossRef]
- Zhao, B.; Huang, Z.; Qin, Z.; Li, Y.; Wang, T.; Wang, L.; Zhou, W.; Yu, C.; Wang, X.; Yang, S.; et al. Enhancement of Histone Deacetylase Inhibitor Sensitivity in Combination with Cyclin-Dependent Kinase Inhibition for the Treatment of Oral Squamous Cell Carcinoma. Cell. Physiol. Biochem. 2019, 53, 141–156. [Google Scholar] [CrossRef]
- Mao, Y.; Zhang, W.; Zhang, R.; Zuo, J. Alkannin restrains oral squamous carcinoma cell growth, migration and invasion by regulating microRNA-9/RECK axis. Artif. Cells Nanomed. Biotechnol. 2019, 47, 3153–3162. [Google Scholar] [CrossRef]
- Zhen, L.; Fan, D.; Yi, X.; Cao, X.; Chen, D.; Wang, L. Curcumin inhibits oral squamous cell carcinoma proliferation and invasion via EGFR signaling pathways. Int. J. Clin. Exp. Pathol. 2014, 7, 6438–6446. [Google Scholar]
- Wang, H.; Ma, Y. β-Elemene alleviates cisplatin resistance in oral squamous cell carcinoma cell via inhibiting JAK2/STAT3 pathway in vitro and in vivo. Cancer Cell Int. 2022, 22, 244. [Google Scholar] [CrossRef]
- Chen, H.L.; Lo, Y.H.; Lin, C.L.; Lee, T.H.; Leung, W.; Wang, S.W.; Lin, I.P.; Lin, M.Y.; Lee, C.H. Trichodermin inhibits the growth of oral cancer through apoptosis-induced mitochondrial dysfunction and HDAC-2-mediated signaling. Biomed. Pharmacother. 2022, 153, 113351. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Gao, L.; Xie, L.; Xiao, G. GC7 enhances cisplatin sensitivity via STAT3 signaling pathway inhibition and eIF5A2 inactivation in mesenchymal phenotype oral cancer cells. Oncol. Rep. 2018, 39, 1283–1291. [Google Scholar] [CrossRef] [PubMed]
- Chea, C.; Miyauchi, M.; Inubushi, T.; Febriyanti Ayuningtyas, N.; Subarnbhesaj, A.; Nguyen, P.T.; Shrestha, M.; Haing, S.; Ohta, K.; Takata, T. Molecular mechanism of inhibitory effects of bovine lactoferrin on the growth of oral squamous cell carcinoma. PLoS ONE 2018, 13, e0191683. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Liu, L.; Yang, Y.; Xun, W.; Wei, K.; Zeng, G. Betulinic Acid Inhibits Cell Proliferation in Human Oral Squamous Cell Carcinoma via Modulating ROS-Regulated p53 Signaling. Oncol. Res. 2017, 25, 1141–1152. [Google Scholar] [CrossRef]
- Aswathy, M.; Banik, K.; Parama, D.; Sasikumar, P.; Harsha, C.; Joseph, A.G.; Sherin, D.R.; Thanathu, M.K.; Kunnumakkara, A.B.; Vasu, R.K. Exploring the Cytotoxic Effects of the Extracts and Bioactive Triterpenoids from Dillenia indica against Oral Squamous Cell Carcinoma: A Scientific Interpretation and Validation of Indigenous Knowledge. ACS Pharmacol. Transl. Sci. 2021, 4, 834–847. [Google Scholar] [CrossRef]
- Liu, S.C.; Huang, C.S.; Huang, C.M.; Hsieh, M.S.; Huang, M.S.; Fong, I.H.; Yeh, C.T.; Lin, C.C. Isoorientin inhibits epithelial-to-mesenchymal properties and cancer stem-cell-like features in oral squamous cell carcinoma by blocking Wnt/β-catenin/STAT3 axis. Toxicol. Appl. Pharmacol. 2021, 424, 115581. [Google Scholar] [CrossRef]
- Yin, W.; Liu, Y.; Liu, X.; Ma, X.; Sun, B.; Yu, Z. Metformin inhibits epithelial-mesenchymal transition of oral squamous cell carcinoma via the mTOR/HIF-1α/PKM2/STAT3 pathway. Oncol. Lett. 2021, 21, 31. [Google Scholar] [CrossRef]
- He, Y.; Fan, Z.; He, L.; Zhang, C.; Ping, F.; Deng, M.; Liu, S.; Wang, Y.; Cheng, B.; Xia, J. Metformin Combined with 4SC-202 Inhibited the Migration and Invasion of OSCC via STAT3/TWIST1. OncoTargets Ther. 2020, 13, 11019–11029. [Google Scholar] [CrossRef]
- Mallery, S.R.; Wang, D.; Santiago, B.; Pei, P.; Schwendeman, S.P.; Nieto, K.; Spinney, R.; Tong, M.; Koutras, G.; Han, B.; et al. Benefits of Multifaceted Chemopreventives in the Suppression of the Oral Squamous Cell Carcinoma (OSCC) Tumorigenic Phenotype. Cancer Prev. Res. 2017, 10, 76–88. [Google Scholar] [CrossRef]
- Wang, Y.; Guo, W.; Li, Z.; Wu, Y.; Jing, C.; Ren, Y.; Zhao, M.; Kong, L.; Zhang, C.; Dong, J.; et al. Role of the EZH2/miR-200 axis in STAT3-mediated OSCC invasion. Int. J. Oncol. 2018, 52, 1149–1164. [Google Scholar] [CrossRef]
- Zhang, X.; Feng, H.; Li, Z.; Guo, J.; Li, M. Aspirin is Involved in the Cell Cycle Arrest, Apoptosis, Cell Migration, and Invasion of Oral Squamous Cell Carcinoma. Int. J. Mol. Sci. 2018, 19. [Google Scholar] [CrossRef] [PubMed]
- Yang, I.H.; Jung, W.; Kim, L.H.; Shin, J.A.; Cho, N.P.; Hong, S.D.; Hong, K.O.; Cho, S.D. Nitidine chloride represses Mcl-1 protein via lysosomal degradation in oral squamous cell carcinoma. J. Oral Pathol. Med. 2018, 47, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Kim, L.H.; Khadka, S.; Shin, J.A.; Jung, J.Y.; Ryu, M.H.; Yu, H.J.; Lee, H.N.; Jang, B.; Yang, I.H.; Won, D.H.; et al. Nitidine chloride acts as an apoptosis inducer in human oral cancer cells and a nude mouse xenograft model via inhibition of STAT3. Oncotarget 2017, 8, 91306–91315. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhang, J.; Wen, Y.; Wang, P.; Fan, L. Bupivacaine inhibits the malignant biological behavior of oral squamous cell carcinoma cells by inhibiting the activation of ERK1/2 and STAT3. Ann. Transl. Med. 2021, 9, 839. [Google Scholar] [CrossRef]
- Zhou, X.; Ren, Y.; Liu, A.; Han, L.; Zhang, K.; Li, S.; Li, P.; Li, P.; Kang, C.; Wang, X.; et al. STAT3 inhibitor WP1066 attenuates miRNA-21 to suppress human oral squamous cell carcinoma growth in vitro and in vivo. Oncol. Rep. 2014, 31, 2173–2180. [Google Scholar] [CrossRef]
- Jo, S.; Yang, E.; Lee, Y.; Jeon, D.; Namkung, W. Cinobufagin Exerts Anticancer Activity in Oral Squamous Cell Carcinoma Cells through Downregulation of ANO1. Int. J. Mol. Sci. 2021, 22, 12037. [Google Scholar] [CrossRef]
- Furtek, S.L.; Backos, D.S.; Matheson, C.J.; Reigan, P. Strategies and Approaches of Targeting STAT3 for Cancer Treatment. ACS Chem. Biol. 2016, 11, 308–318. [Google Scholar] [CrossRef]
- Loh, C.Y.; Arya, A.; Naema, A.F.; Wong, W.F.; Sethi, G.; Looi, C.Y. Signal Transducer and Activator of Transcription (STATs) Proteins in Cancer and Inflammation: Functions and Therapeutic Implication. Front. Oncol. 2019, 9, 48. [Google Scholar] [CrossRef]
- Kamerkar, S.; Leng, C.; Burenkova, O.; Jang, S.C.; McCoy, C.; Zhang, K.; Dooley, K.; Kasera, S.; Zi, T.; Sisó, S.; et al. Exosome-mediated genetic reprogramming of tumor-associated macrophages by exoASO-STAT6 leads to potent monotherapy antitumor activity. Sci. Adv. 2022, 8, eabj7002. [Google Scholar] [CrossRef]
- Tomida, M.; Ohtake, H.; Yokota, T.; Kobayashi, Y.; Kurosumi, M. Stat3 up-regulates expression of nicotinamide N-methyltransferase in human cancer cells. J. Cancer Res. Clin. Oncol. 2008, 134, 551–559. [Google Scholar] [CrossRef]
- Seta, R.; Mascitti, M.; Campagna, R.; Sartini, D.; Fumarola, S.; Santarelli, A.; Giuliani, M.; Cecati, M.; Muzio, L.L.; Emanuelli, M. Overexpression of nicotinamide N-methyltransferase in HSC-2 OSCC cell line: Effect on apoptosis and cell proliferation. Clin. Oral Investig. 2019, 23, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Sen, M.; Thomas, S.M.; Kim, S.; Yeh, J.I.; Ferris, R.L.; Johnson, J.T.; Duvvuri, U.; Lee, J.; Sahu, N.; Joyce, S.; et al. First-in-human trial of a STAT3 decoy oligonucleotide in head and neck tumors: Implications for cancer therapy. Cancer Discov. 2012, 2, 694–705. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.R.; Walker, S.R.; Heppler, L.N.; Tyekucheva, S.; Nelson, E.A.; Klitgaard, J.; Nicolais, M.; Kroll, Y.; Xiang, M.; Yeh, J.E.; et al. Targeting constitutively active STAT3 in chronic lymphocytic leukemia: A clinical trial of the STAT3 inhibitor pyrimethamine with pharmacodynamic analyses. Am. J. Hematol. 2021, 96, E95–E98. [Google Scholar] [CrossRef] [PubMed]
- Sparano, J.A.; Moulder, S.; Kazi, A.; Coppola, D.; Negassa, A.; Vahdat, L.; Li, T.; Pellegrino, C.; Fineberg, S.; Munster, P.; et al. Phase II trial of tipifarnib plus neoadjuvant doxorubicin-cyclophosphamide in patients with clinical stage IIB-IIIC breast cancer. Clin. Cancer Res. 2009, 15, 2942–2948. [Google Scholar] [CrossRef]
- Oh, D.Y.; Lee, S.H.; Han, S.W.; Kim, M.J.; Kim, T.M.; Kim, T.Y.; Heo, D.S.; Yuasa, M.; Yanagihara, Y.; Bang, Y.J. Phase I Study of OPB-31121, an Oral STAT3 Inhibitor, in Patients with Advanced Solid Tumors. Cancer Res. Treat. 2015, 47, 607–615. [Google Scholar] [CrossRef]
- Bendell, J.C.; Hong, D.S.; Burris, H.A., III; Naing, A.; Jones, S.F.; Falchook, G.; Bricmont, P.; Elekes, A.; Rock, E.P.; Kurzrock, R. Phase 1, open-label, dose-escalation, and pharmacokinetic study of STAT3 inhibitor OPB-31121 in subjects with advanced solid tumors. Cancer Chemother. Pharmacol. 2014, 74, 125–130. [Google Scholar] [CrossRef]
- Ribrag, V.; Lee, S.T.; Rizzieri, D.; Dyer, M.J.S.; Fayad, L.; Kurzrock, R.; Andritsos, L.; Bouabdallah, R.; Hayat, A.; Bacon, L.; et al. A Phase 1b Study to Evaluate the Safety and Efficacy of Durvalumab in Combination With Tremelimumab or Danvatirsen in Patients With Relapsed or Refractory Diffuse Large B-Cell Lymphoma. Clin. Lymphoma Myeloma Leuk. 2021, 21, 309–317. [Google Scholar] [CrossRef]
- Borazanci, E.; Schram, A.M.; Garralda, E.; Brana, I.; Vieito Villar, M.; Spreafico, A.; Oliva, M.; Lakhani, N.J.; Hoffman, K.; Hallett, R.M.; et al. Phase I, first-in-human study of MSC-1 (AZD0171), a humanized anti-leukemia inhibitory factor monoclonal antibody, for advanced solid tumors. ESMO Open 2022, 7, 100530. [Google Scholar] [CrossRef]
- Wong, A.L.; Soo, R.A.; Tan, D.S.; Lee, S.C.; Lim, J.S.; Marban, P.C.; Kong, L.R.; Lee, Y.J.; Wang, L.Z.; Thuya, W.L.; et al. Phase I and biomarker study of OPB-51602, a novel signal transducer and activator of transcription (STAT) 3 inhibitor, in patients with refractory solid malignancies. Ann. Oncol. 2015, 26, 998–1005. [Google Scholar] [CrossRef]
- Groot, J.; Ott, M.; Wei, J.; Kassab, C.; Fang, D.; Najem, H.; O’Brien, B.; Weathers, S.P.; Matsouka, C.K.; Majd, N.K.; et al. A first-in-human Phase I trial of the oral p-STAT3 inhibitor WP1066 in patients with recurrent malignant glioma. CNS Oncol. 2022, 11, Cns87. [Google Scholar] [CrossRef]
- Bauman, J.E.; Duvvuri, U.; Gooding, W.E.; Rath, T.J.; Gross, N.D.; Song, J.; Jimeno, A.; Yarbrough, W.G.; Johnson, F.M.; Wang, L.; et al. Randomized, placebo-controlled window trial of EGFR, Src, or combined blockade in head and neck cancer. JCI Insight 2017, 2, e90449. [Google Scholar] [CrossRef] [PubMed]
- Jonker, D.J.; Nott, L.; Yoshino, T.; Gill, S.; Shapiro, J.; Ohtsu, A.; Zalcberg, J.; Vickers, M.M.; Wei, A.C.; Gao, Y.; et al. Napabucasin versus placebo in refractory advanced colorectal cancer: A randomised phase 3 trial. Lancet Gastroenterol. Hepatol. 2018, 3, 263–270. [Google Scholar] [CrossRef]
- Taniguchi, H.; Masuishi, T.; Kawazoe, A.; Muro, K.; Kadowaki, S.; Bando, H.; Iino, S.; Kageyama, R.; Yoshino, T. Phase I study of napabucasin in combination with FOLFIRI + bevacizumab in Japanese patients with metastatic colorectal cancer. Int. J. Clin. Oncol. 2021, 26, 2017–2024. [Google Scholar] [CrossRef] [PubMed]
- Yoo, C.; Kang, J.; Lim, H.Y.; Kim, J.H.; Lee, M.A.; Lee, K.H.; Kim, T.Y.; Ryoo, B.Y. Phase I Dose-Finding Study of OPB-111077, a Novel STAT3 Inhibitor, in Patients with Advanced Hepatocellular Carcinoma. Cancer Res. Treat. 2019, 51, 510–518. [Google Scholar] [CrossRef]
- Tolcher, A.; Flaherty, K.; Shapiro, G.I.; Berlin, J.; Witzig, T.; Habermann, T.; Bullock, A.; Rock, E.; Elekes, A.; Lin, C.; et al. A First-in-Human Phase I Study of OPB-111077, a Small-Molecule STAT3 and Oxidative Phosphorylation Inhibitor, in Patients with Advanced Cancers. Oncologist 2018, 23, 658-e672. [Google Scholar] [CrossRef]
- Lynce, F.; Williams, J.T.; Regan, M.M.; Bunnell, C.A.; Freedman, R.A.; Tolaney, S.M.; Chen, W.Y.; Mayer, E.L.; Partridge, A.H.; Winer, E.P.; et al. Phase I study of JAK1/2 inhibitor ruxolitinib with weekly paclitaxel for the treatment of HER2-negative metastatic breast cancer. Cancer Chemother. Pharmacol. 2021, 87, 673–679. [Google Scholar] [CrossRef]
- Park, J.S.; Hong, M.H.; Chun, Y.J.; Kim, H.R.; Cho, B.C. A phase Ib study of the combination of afatinib and ruxolitinib in EGFR mutant NSCLC with progression on EGFR-TKIs. Lung Cancer 2019, 134, 46–51. [Google Scholar] [CrossRef]
- Spaner, D.E.; Wang, G.; McCaw, L.; Li, Y.; Disperati, P.; Cussen, M.A.; Shi, Y. Activity of the Janus kinase inhibitor ruxolitinib in chronic lymphocytic leukemia: Results of a phase II trial. Haematologica 2016, 101, e192–e195. [Google Scholar] [CrossRef]
- Kearney, M.; Franks, L.; Lee, S.; Tiersten, A.; Makower, D.F.; Cigler, T.; Mundi, P.; Chi, D.C.; Goel, A.; Klein, P.; et al. Phase I/II trial of ruxolitinib in combination with trastuzumab in metastatic HER2 positive breast cancer. Breast Cancer Res. Treat. 2021, 189, 177–185. [Google Scholar] [CrossRef]
- Eghtedar, A.; Verstovsek, S.; Estrov, Z.; Burger, J.; Cortes, J.; Bivins, C.; Faderl, S.; Ferrajoli, A.; Borthakur, G.; George, S.; et al. Phase 2 study of the JAK kinase inhibitor ruxolitinib in patients with refractory leukemias, including postmyeloproliferative neoplasm acute myeloid leukemia. Blood 2012, 119, 4614–4618. [Google Scholar] [CrossRef]
- Sweet, K.; Hazlehurst, L.; Sahakian, E.; Powers, J.; Nodzon, L.; Kayali, F.; Hyland, K.; Nelson, A.; Pinilla-Ibarz, J. A phase I clinical trial of ruxolitinib in combination with nilotinib in chronic myeloid leukemia patients with molecular evidence of disease. Leuk. Res. 2018, 74, 89–96. [Google Scholar] [CrossRef]
- Plimack, E.R.; Lorusso, P.M.; McCoon, P.; Tang, W.; Krebs, A.D.; Curt, G.; Eckhardt, S.G. AZD1480: A phase I study of a novel JAK2 inhibitor in solid tumors. Oncologist 2013, 18, 819–820. [Google Scholar] [CrossRef]
- Santos, F.P.; Kantarjian, H.M.; Jain, N.; Manshouri, T.; Thomas, D.A.; Garcia-Manero, G.; Kennedy, D.; Estrov, Z.; Cortes, J.; Verstovsek, S. Phase 2 study of CEP-701, an orally available JAK2 inhibitor, in patients with primary or post-polycythemia vera/essential thrombocythemia myelofibrosis. Blood 2010, 115, 1131–1136. [Google Scholar] [CrossRef]
- Delyon, J.; Chevret, S.; Jouary, T.; Dalac, S.; Dalle, S.; Guillot, B.; Arnault, J.P.; Avril, M.F.; Bedane, C.; Bens, G.; et al. STAT3 Mediates Nilotinib Response in KIT-Altered Melanoma: A Phase II Multicenter Trial of the French Skin Cancer Network. J. Investig. Dermatol. 2018, 138, 58–67. [Google Scholar] [CrossRef]
- Gullaksen, S.E.; Skavland, J.; Gavasso, S.; Tosevski, V.; Warzocha, K.; Dumrese, C.; Ferrant, A.; Gedde-Dahl, T.; Hellmann, A.; Janssen, J.; et al. Single cell immune profiling by mass cytometry of newly diagnosed chronic phase chronic myeloid leukemia treated with nilotinib. Haematologica 2017, 102, 1361–1367. [Google Scholar] [CrossRef][Green Version]
- Banerjee, K.; Pru, C.; Pru, J.K.; Resat, H. STAT3 Knockdown Induces Tumor Formation by MDA-MB-231 Cells. Clin. Oncol. Res. 2018, 1. [Google Scholar] [CrossRef]
- Sonnenblick, A.; Agbor-Tarh, D.; de Azambuja, E.; Hultsch, S.; Izquierdo, M.; Liu, M.; Pruneri, G.; Harbeck, N.; Piccart, M.; Moreno-Aspita, A.; et al. STAT3 activation in HER2-positive breast cancers: Analysis of data from a large prospective trial. Int. J. Cancer 2021, 148, 1529–1535. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).