Chromosomal Heteromorphisms and Cancer Susceptibility Revisited
Abstract
1. Introduction
2. Large Heterochromatic CG-CNVs/Chromosomal Heteromorphisms
- There can be size variants of the centromeres of all 24 human chromosomes as diminished (=cen−) or enlarged by amplification or unequal crossing over (=cen+, cen++), or due to a duplication leading to a (pseudo) dicentric derivative. As enlarged centromeric regions can also include inversions, such events are also included here as common CHs. Centromeric insertions in other centromeres and/or euchromatic material can lead to altered banding patterns in cytogenetic analyses within healthy individuals. However, such derivative chromosomes can only be elucidated and characterized by FISH. Finally, centromeres of acrocentric chromosomes may provide unexpected FISH results when using alpha-satellite-specific probes; here, rare, unbalanced translocation events exclusively involving heterochromatic material may be the reason for CHs, again only resolvable by FISH.
- Similar to centromeres, subcentromeric heterochromatic blocks of chromosomes 1, 3, 9, and 16 (1q12, 3q11.2, 9q12, and 16q11.2) may by diminished or enlarged in size. However, here, amplification of material cannot be distinguished from duplication. Moreover, in chromosome 9, so-called hemi-heterochromatic bands adjacent to 9p11.1 (9p11.2~12) and to 9q12 (9q13) comprise copy-number-independent regions involved in euchromatic variants [26]. Thus, here, many subtypes of CHs consisting of hetero- and euchromatin are regularly observed in banding cytogenetics. Heteromorphic inversions and insertions of this region are also present in the human population.
- In males, the sub-band Yq12 and satellite DNAs are normally gender-specific. Sub-band Yq12 can also be reduced to minimal size or amplified to dramatically large sizes without obvious phenotypic effects. Amplifications and duplications, as well as inversions and insertions, can only be reliably characterized by FISH. However, Yq12 material can be transferred to other autosomes or even an X chromosome, and then also be observed throughout generations in males and females [27].
- There are 10 acrocentric chromosomes in the human genome, which carry nearly identical short (p-) arms. They comprise only one identified, substantially important genetic material, the nucleolus organizing region (NOR), each. As in many other vertebrate species, one NOR-bearing chromosome pair is sufficient for a species to function [28], and the tremendous variability observed for these 10 regions is no surprise. Figure 2 includes many of these variants, which can be picked up or at least suggested based on banding cytogenetics. FISH enables detection and substantially more insights as summarized elsewhere [8,23].
3. Chromosomal Heteromorphisms (CHs) and Cancer
3.1. Correlations Based on Pure Banding Cytogenetics
3.2. Possible Correlations
3.2.1. Amplification of CHs in Tumors
3.2.2. Epigenetic Changes in CHs in Tumors
3.2.3. CHs Expressed on RNA Level
3.2.4. Is the Two-Hit Model Also Applicable for Heterochromatic CNVs/CHs?
3.2.5. Necessary Future Research Directions
- Should other repeats/longer satellite sequences/HORs be studied, especially in cases of cancer?
- Additionally, might consideration being given to the individual sizes of heterochromatin make sense? If DNA stretches located in CHs matter for normal cell function, as shown in our favorite animal model—the mouse [80]—would it not to be expected that differences in the proportion of CHs compared to overall stable euchromatic genome size would result in some effects?
- What about studies checking on the cancerogenic effects of two types of cell lines: those with a high proportion of heterochromatin due to large CH regions and those with smaller, almost absent CHs?
- Why not combine banding cytogenetic data available for CHs in leukemia and lymphoma with data on lncRNA derived from HSATIII in the same cells as the basis for further studies?
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVID-19 Host Genetics Initiative. Mapping the human genetic architecture of COVID-19. Nature 2021, 600, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Huffman, J.E.; Butler-Laporte, G.; Khan, A.; Pairo-Castineira, E.; Drivas, T.G.; Peloso, G.M.; Nakanishi, T.; COVID-19 Host Genetics Initiative; Ganna, A.; Verma, A.; et al. Multi-ancestry fine mapping implicates OAS1 splicing in risk of severe COVID-19. Nat. Genet. 2022, 54, 125–127. [Google Scholar] [CrossRef]
- Liehr, T. Repetitive elements in humans. Int. J. Mol. Sci. 2021, 22, 2072. [Google Scholar] [CrossRef] [PubMed]
- Shastry, B.S. SNPs: Impact on gene function and phenotype. Methods Mol. Biol. 2009, 578, 3–22. [Google Scholar]
- Iafrate, A.J.; Feuk, L.; Rivera, M.N.; Listewnik, M.L.; Donahoe, P.K.; Qi, Y.; Scherer, S.W.; Lee, C. Detection of large-scale variation in the human genome. Nat. Genet. 2004, 36, 949–951. [Google Scholar] [CrossRef]
- Sebat, J.; Lakshmi, B.; Troge, J.; Alexander, J.; Young, J.; Lundin, P.; Månér, S.; Massa, H.; Walker, M.; Chi, M.; et al. Large-scale copy number polymorphism in the human genome. Science 2004, 305, 525–528. [Google Scholar] [CrossRef]
- Liehr, T. Copy number variations—Is there a biological difference between submicroscopic and microscopically visible ones? OA Genet. 2013, 1, 2. [Google Scholar]
- Liehr, T. Benign & Pathological Chromosomal Imbalances: Microscopic and Submicroscopic Copy Number Variations (CNVs) in Genetics and Counseling, 1st ed.; Academic Press: Berlin, Germany, 2014. [Google Scholar]
- Harel, T.; Lupski, J.R. Genomic disorders 20 years on-mechanisms for clinical manifestations. Clin. Genet. 2018, 93, 439–449. [Google Scholar] [CrossRef]
- Canales, C.P.; Walz, K. Copy number variation and susceptibility to complex traits. EMBO Mol. Med. 2011, 3, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Weise, A.; Mrasek, K.; Klein, E.; Mulatinho, M.; Llerena, J.C., Jr.; Hardekopf, D.; Pekova, S.; Bhatt, S.; Kosyakova, N.; Liehr, T.; et al. Microdeletion and microduplication syndromes. J. Histochem. Cytochem. 2012, 60, 346–358. [Google Scholar] [CrossRef]
- Girirajan, S.; Rosenfeld, J.A.; Cooper, G.M.; Antonacci, F.; Siswara, P.; Itsara, A.; Vives, L.; Walsh, T.; McCarthy, S.E.; Baker, C.; et al. A recurrent 16p12.1 microdeletion supports a two-hit model for severe developmental delay. Nat. Genet. 2010, 42, 203–209. [Google Scholar] [CrossRef]
- Albers, C.A.; Paul, D.S.; Schulze, H.; Freson, K.; Stephens, J.C.; Smethurst, P.A.; Jolley, J.D.; Cvejic, A.; Kostadima, M.; Bertone, P.; et al. Compound inheritance of a low-frequency regulatory SNP and a rare null mutation in exon-junction complex subunit RBM8A causes TAR syndrome. Nat. Genet. 2012, 44, 435–439, S1–S2. [Google Scholar] [CrossRef]
- Liehr, T. (Ed.) Cytogenomics; Academic Press: New York, NY, USA, 2021. [Google Scholar]
- Altemose, N.; Logsdon, G.A.; Bzikadze, A.V.; Sidhwani, P.; Langley, S.A.; Caldas, G.V.; Hoyt, S.J.; Uralsky, L.; Ryabov, F.D.; Shew, C.J.; et al. Complete genomic and epigenetic maps of human centromeres. Science 2022, 376, eabl4178. [Google Scholar] [CrossRef] [PubMed]
- Manvelyan, M.; Cremer, F.W.; Lancé, J.; Kläs, R.; Kelbova, C.; Ramel, C.; Reichenbach, H.; Schmidt, C.; Ewers, E.; Kreskowski, K.; et al. New cytogenetically visible copy number variant in region 8q21.2. Mol. Cytogenet. 2011, 4, 1. [Google Scholar] [CrossRef]
- UCSC-Browser; Build Dec. 2013 (GRCh38/hg38). Available online: http://genome.ucsc.edu/cgi-bin/hgGateway?hgsid=95241316&clade=vertebrate&org=Human&db=hg18&redirect=manual&source=genome.ucsc.edu (accessed on 9 September 2022).
- Altman, R.B. Direct-to-consumer genetic testing: Failure is not an option. Clin. Pharmacol. Ther. 2009, 86, 15–17. [Google Scholar] [CrossRef]
- Daban, J.R. Soft-matter properties of multilayer chromosomes. Phys. Biol. 2021, 18, 053001. [Google Scholar] [CrossRef]
- Liehr, T.; Mrasek, K.; Klein, E.; Weise, A. Modern high throughput approaches are not meant to replace ‘old fashioned’ but robust techniques. J. Genet. Genomes. 2017, 1, e101. [Google Scholar]
- Matylla-Kulinska, K.; Tafer, H.; Weiss, A.; Schroeder, R. Functional repeat-derived RNAs often originate from retrotransposon-propagated ncRNAs. Wiley Interdiscip. Rev. RNA 2014, 5, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Gemmell, N.J. Repetitive DNA: Genomic dark matter matters. Nat. Rev. Genet. 2021, 22, 342. [Google Scholar] [CrossRef] [PubMed]
- Liehr, T. Cases with Heteromorphisms. 2022. Available online: http://cs-tl.de/DB/CA/HCM/0-Start.html (accessed on 9 September 2022).
- Tyler-Smith, C.; Brown, W.R. Structure of the major block of alphoid satellite DNA on the human Y chromosome. J. Mol. Biol. 1987, 195, 457–470. [Google Scholar] [CrossRef]
- McGowan-Jordan, J.; Hastings, R.; Moore, S. (Eds.) ISCN 2020: An international System for Human Cytogenomic Nomenclature; Karger: Basel, Switzerland, 2020. [Google Scholar]
- Kosyakova, N.; Grigorian, A.; Liehr, T.; Manvelyan, M.; Simonyan, I.; Mkrtchyan, H.; Aroutiounian, R.; Polityko, A.D.; Kulpanovich, A.I.; Egorova, T.; et al. Heteromorphic variants of chromosome 9. Mol. Cytogenet. 2013, 6, 14. [Google Scholar] [CrossRef][Green Version]
- Genest, P. An eleven-generation satellited Y chromosome. Lancet 1972, 299, 1073. [Google Scholar] [CrossRef]
- Ditcharoen, S.; Khensuwan, S.; Seetapan, K.; Soonthornvipat, P.; Suwannapoom, C.; Pinthong, K.; Tongnunui, S.; Cioffi, M.d.B.; Liehr, T.; Tanomtong, A.; et al. First classical and molecular cytogenetic analyses of Sperata acicularis (Siluriformes, Bagridae). Taiwania 2021, 66, 203–213. [Google Scholar]
- Salgueiro, A.P.; Martelli, F.T.; D’Ávila, S.R.; Milnikel, T.R.; Koehler-Santos, P.; Maraschin, B.J.; da Silva, V.P.; Rados, P.V.; Visioli, F. Cytopathological tests for early detection of oral carcinogenesis. Eur. J. Cancer Prev. 2020, 29, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Janssen, A.; Colmenares, S.U.; Karpen, G.H. Heterochromatin: Guardian of the genome. Annu. Rev. Cell Dev. Biol. 2018, 34, 265–288. [Google Scholar] [CrossRef]
- Conte, R.A.; Mathews, T.; Kleyman, S.M.; Verma, R.S. Molecular characterization of 21p- variant chromosome. Clin. Genet. 1996, 50, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Starke, H.; Seidel, J.; Henn, W.; Reichardt, S.; Volleth, M.; Stumm, M.; Behrend, C.; Sandig, K.R.; Kelbova, C.; Senger, G.; et al. Homologous sequences at human chromosome 9 bands p12 and q13-21.1 are involved in different patterns of pericentric rearrangements. Eur. J. Hum. Genet. 2002, 10, 790–800. [Google Scholar] [CrossRef]
- Adhvaryu, S.G.; Rawal, U.M. C-band heterochromatin variants in individuals with neoplastic disorders: Carcinoma of breast and ovary. Neoplasma 1991, 38, 379–384. [Google Scholar]
- Aguilar, L.; Lisker, R.; Ruz, L.; Mutchinick, O. Constitutive heterochromatin polymorphisms in patients with malignant diseases. Cancer 1981, 47, 2437–2442. [Google Scholar] [CrossRef]
- Holden, J.J.; Reimer, D.L.; Higgins, M.J.; Roder, J.C.; White, B.N. Amplified sequences from chromosome 15, including centromeres, nucleolar organizer regions, and centromeric heterochromatin, in homogeneously staining regions in the human melanoma cell line MeWo. Cancer Genet. Cytogenet. 1985, 14, 131–146. [Google Scholar] [CrossRef]
- Savelyeva, L.; Schneider, B.; Finke, L.; Schlag, P.; Schwab, M. Amplification of satellite DNA at 16q11.2 in the germ-line of a patient with breast-cancer. Int. J. Oncol. 1994, 4, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Liehr, T.; Park, O.; Feuerstein, B.; Gebhart, E.; Rautenstrauss, B. The peripheral myelin protein 22 kDa (PMP22) gene is amplified in cell lines derived from glioma and osteogenic sarcoma. Int. J. Oncol. 1997, 10, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Gisselsson, D.; Höglund, M.; Mertens, F.; Mandahl, N. Variable stability of chromosomes containing amplified alpha-satellite sequences in human mesenchymal tumours. Chromosoma 1999, 108, 271–277. [Google Scholar] [CrossRef]
- Eichler, E.E.; Budarf, M.L.; Rocchi, M.; Deaven, L.L.; Doggett, N.A.; Baldini, A.; Nelson, D.L.; Mohrenweiser, H.W. Interchromosomal duplications of the adrenoleukodystrophy locus: A phenomenon of pericentromeric plasticity. Hum. Mol. Genet. 1997, 6, 991–1002. [Google Scholar] [CrossRef]
- Sirvent, N.; Forus, A.; Lescaut, W.; Burel, F.; Benzaken, S.; Chazal, M.; Bourgeon, A.; Vermeesch, J.R.; Myklebost, O.; Turc-Carel, C.; et al. Characterization of centromere alterations in liposarcomas. Genes Chromosomes Cancer 2000, 29, 117–129. [Google Scholar] [CrossRef]
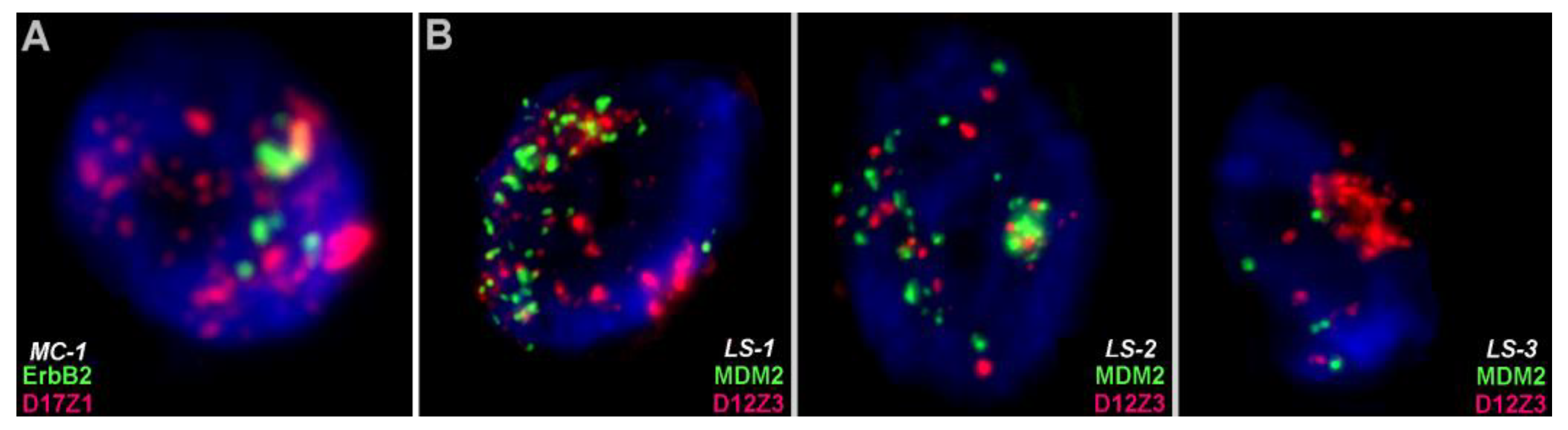
- Kashima, T.; Halai, D.; Ye, H.; Hing, S.N.; Delaney, D.; Pollock, R.; O'Donnell, P.; Tirabosco, R.; Flanagan, A.M. Sensitivity of MDM2 amplification and unexpected multiple faint alphoid 12 (alpha 12 satellite sequences) signals in atypical lipomatous tumor. Mod. Pathol. 2012, 25, 1384–1396. [Google Scholar] [CrossRef]
- Pathak, D.; Premi, S.; Srivastava, J.; Chandy, S.P.; Ali, S. Genomic instability of the DYZ1 repeat in patients with Y chromosome anomalies and males exposed to natural background radiation. DNA Res. 2006, 13, 103–109. [Google Scholar] [CrossRef]
- Sala, E.; Villa, N.; Crosti, F.; Miozzo, M.; Perego, P.; Cappellini, A.; Bonazzi, C.; Barisani, D.; Dalprà, L. Endometrioid-like yolk sac and Sertoli-Leydig cell tumors in a carrier of a Y heterochromatin insertion into 1qh region: A causal association? Cancer Genet. Cytogenet. 2007, 173, 164–169. [Google Scholar] [CrossRef]
- Neglia, M.; Bertoni, L.; Zoli, W.; Giulotto, E. Amplification of the pericentromeric region of chromosome 1 in a newly established colon carcinoma cell line. Cancer Genet. Cytogenet. 2003, 142, 99–106. [Google Scholar] [CrossRef]
- Morerio, C.; Rapella, A.; Tassano, E.; Lanino, E.; Micalizzi, C.; Rosanda, C.; Panarello, C. Gain of 1q in pediatric myelodysplastic syndromes. Leuk. Res. 2006, 30, 1437–1441. [Google Scholar] [CrossRef]
- Millington, K.; Hudnall, S.D.; Northup, J.; Panova, N.; Velagaleti, G. Role of chromosome 1 pericentric heterochromatin (1q) in pathogenesis of myelodysplastic syndromes: Report of 2 new cases. Exp. Mol. Pathol. 2008, 84, 189–193. [Google Scholar] [CrossRef]
- Sawyer, J.R.; Tian, E.; Heuck, C.J.; Johann, D.J.; Epstein, J.; Swanson, C.M.; Lukacs, J.L.; Binz, R.L.; Johnson, M.; Sammartino, G.; et al. Evidence of an epigenetic origin for high-risk 1q21 copy number aberrations in multiple myeloma. Blood 2015, 125, 3756–3759. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.; Wu, S.Q.; DeVries, S.; Reznikoff, W.S.; Waldman, F.M.; Reznikoff, C.A. Carcinogen-induced amplification of SV40 DNA inserted at 9q12-21.1 associated with chromosome breakage, deletions, and translocations in human uroepithelial cell transformation in vitro. Genes Chromosomes Cancer 1993, 8, 155–166. [Google Scholar] [CrossRef]
- Fischer, U.; Wullich, B.; Sattler, H.P.; Göttert, E.; Zang, K.D.; Meese, E. Coamplification on chromosomes 7p12-13 and 9q12-13 identified by reverse chromosome painting in a glioblastoma multiforme. Hum. Genet. 1994, 93, 331–334. [Google Scholar] [CrossRef]
- Hough, M.R.; White, B.N.; Holden, J.J. Relative tumorigenicities of hybrid cells with and without HSR-bearing chromosomes from a human melanoma cell line. Int. J. Cancer 1989, 44, 360–366. [Google Scholar] [CrossRef]
- Ogunbiyi, O.A.; Scholefield, J.H.; Sharp, F.; Ginsberg, R.; Rogers, K. Nucleolar organiser regions (AgNORS) in anal intraepithelial neoplasia and invasive anal squamous cell carcinoma. J. Clin. Pathol. 1992, 45, 889–893. [Google Scholar] [CrossRef]
- Saint-Ruf, C.; Viegas-Péquignot, E.; Alfani, E.; Clementi, M.; Dutrillaux, B.; Carloni, G. Co-amplification of transcriptionally active epidermal growth factor receptor and ribosomal genes in the human hepatoma cell line Li7A. Oncogene 1992, 7, 1557–1565. [Google Scholar] [PubMed]
- Atkin, N.B.; Baker, M.C. Ectopic nucleolar organizer regions. A common anomaly revealed by Ag-NOR staining of metaphases from nine cancers. Cancer Genet. Cytogenet. 1995, 85, 129–132. [Google Scholar] [CrossRef]
- Plaat, B.E.; Molenaar, W.M.; Mastik, M.F.; Hoekstra, H.J.; te Meerman, G.J.; van den Berg, E. Computer-assisted cytogenetic analysis of 51 malignant peripheral-nerve-sheath tumors: Sporadic vs. neurofibromatosis-type-1-associated malignant schwannomas. Int. J. Cancer 1999, 83, 171–178. [Google Scholar] [CrossRef]
- Fonatsch, C.; Nowotny, H.; Pittermann-Höcker, E.; Streubel, B.; Jäger, U.; Valent, P.; Büchner, T.; Lechner, K. Amplification of ribosomal RNA genes in acute myeloid leukemia. Genes Chromosomes Cancer 2001, 32, 11–17. [Google Scholar] [CrossRef]
- Bánkfalvi, A.; Giuffrè, G.; Ofner, D.; Diallo, R.; Poremba, C.; Buchwalow, I.B.; Barresi, V.; Böcker, W.; Tuccari, G. Relationship between HER2 status and proliferation rate in breast cancer assessed by immunohistochemistry, fluorescence in situ hybridisation and standardised AgNOR analysis. Int. J. Oncol. 2003, 23, 1285–1292. [Google Scholar] [CrossRef]
- Roberts, C.G.; Tattersall, M.H. Analysis of inferred cytogenetic clonal evolution in a metastatic human ovarian carcinoma. Cancer Genet. Cytogenet. 1990, 48, 53–60. [Google Scholar] [CrossRef]
- Kallioniemi, A.; Kallioniemi, O.P.; Sudar, D.; Rutovitz, D.; Gray, J.W.; Waldman, F.; Pinkel, D. Comparative genomic hybridization for molecular cytogenetic analysis of solid tumors. Science 1992, 258, 818–821. [Google Scholar] [CrossRef]
- Slee, R.B.; Steiner, C.M.; Herbert, B.S.; Vance, G.H.; Hickey, R.J.; Schwarz, T.; Christan, S.; Radovich, M.; Schneider, B.P.; Schindelhauer, D.; et al. Cancer-associated alteration of pericentromeric heterochromatin may contribute to chromosome instability. Oncogene 2012, 31, 3244–3253. [Google Scholar] [CrossRef]
- Santos, S.; Chaves, R.; Adega, F.; Bastos, E.; Guedes-Pinto, H. Amplification of the major satellite DNA family (FA-SAT) in a cat fibrosarcoma might be related to chromosomal instability. J. Hered. 2006, 97, 114–118. [Google Scholar] [CrossRef]
- Tantravahi, U.; Erlanger, B.F.; Miller, O.J. The rat XC sarcoma cell line: Ribosomal RNA gene amplification and banded karyotype. Cancer Genet. Cytogenet. 1982, 5, 63–73. [Google Scholar] [CrossRef]
- Bostock, C.J.; Clark, E.M. Satellite DNA in large marker chromosomes of methotrexate-resistant mouse cells. Cell 1980, 19, 709–715. [Google Scholar] [CrossRef]
- Riva, P.; Orlando, S.; Labella, T.; Larizza, L. Satellite DNA sequences flank amplified DHFR domains in marker chromosomes of mouse fibrosarcoma cells. Genetica 1994, 94, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Flavahan, W.A.; Gaskell, E.; Bernstein, B.E. Epigenetic plasticity and the hallmarks of cancer. Science 2017, 357, eaal2380. [Google Scholar] [CrossRef]
- Hernández-Saavedra, D.; Strakovsky, R.S.; Ostrosky-Wegman, P.; Pan, Y.X. Epigenetic regulation of centromere chromatin stability by dietary and environmental factors. Adv. Nutr. 2017, 8, 889–904. [Google Scholar] [CrossRef]
- Enukashvily, N.I.; Donev, R.; Waisertreiger, I.S.; Podgornaya, O.I. Human chromosome 1 satellite 3 DNA is decondensed, demethylated and transcribed in senescent cells and in A431 epithelial carcinoma cells. Cytogenet. Genome Res. 2007, 118, 42–54. [Google Scholar] [CrossRef]
- Wong, N.; Lam, W.C.; Lai, P.B.; Pang, E.; Lau, W.Y.; Johnson, P.J. Hypomethylation of chromosome 1 heterochromatin DNA correlates with q-arm copy gain in human hepatocellular carcinoma. Am. J. Pathol. 2001, 159, 465–471. [Google Scholar] [CrossRef]
- Hall, L.L.; Byron, M.; Carone, D.M.; Whitfield, T.W.; Pouliot, G.P.; Fischer, A.; Jones, P.; Lawrence, J.B. Demethylated HSATII DNA and HSATII RNA foci sequester PRC1 and MeCP2 into cancer-specific nuclear bodies. Cell Rep. 2017, 18, 2943–2956. [Google Scholar] [CrossRef]
- Brückmann, N.H.; Pedersen, C.B.; Ditzel, H.J.; Gjerstorff, M.F. Epigenetic reprogramming of pericentromeric satellite DNA in premalignant and malignant lesions. Mol. Cancer Res. 2018, 16, 417–427. [Google Scholar] [CrossRef]
- Traynor, S.; Møllegaard, N.E.; Jørgensen, M.G.; Brückmann, N.H.; Pedersen, C.B.; Terp, M.G.; Johansen, S.; Dejardin, J.; Ditzel, H.J.; Gjerstorff, M.F. Remodeling and destabilization of chromosome 1 pericentromeric heterochromatin by SSX proteins. Nucleic Acids Res. 2019, 47, 6668–6684. [Google Scholar] [CrossRef] [PubMed]
- Kimura, F.; Florl, A.R.; Seifert, H.H.; Louhelainen, J.; Maas, S.; Knowles, M.A.; Schulz, W.A. Destabilization of chromosome 9 in transitional cell carcinoma of the urinary bladder. Br. J. Cancer 2001, 85, 1887–1893. [Google Scholar] [CrossRef]
- Eymery, A.; Souchier, C.; Vourch, C.; Jolly, C. Heat shock factor 1 binds to and transcribes satellite II and III sequences at several pericentromeric regions in heat-shocked cells. Exp. Cell Res. 2010, 316, 1845–1855. [Google Scholar] [CrossRef]
- McNulty, S.M.; Sullivan, B.A. Alpha satellite DNA biology: Finding function in the recesses of the genome. Chromosome Res. 2018, 26, 115–138. [Google Scholar] [CrossRef]
- Jolly, C.; Metz, A.; Govin, J.; Vigneron, M.; Turner, B.M.; Khochbin, S.; Vourch, C. Stress-induced transcription of satellite III repeats. J. Cell Biol. 2004, 164, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Hall, L.E.; Mitchell, S.E.; O'Neill, R.J. Pericentric and centromeric transcription: A perfect balance required. Chromosome Res. 2012, 20, 535–546. [Google Scholar] [CrossRef]
- Crosetto, N.; Mitra, A.; Silva, M.J.; Bienko, M.; Dojer, N.; Wang, Q.; Karaca, E.; Chiarle, R.; Skrzypczak, M.; Ginalski, K.; et al. Nucleotide-resolution DNA double-strand break mapping by next-generation sequencing. Nat. Methods 2013, 10, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Ting, D.T.; Lipson, D.; Paul, S.; Brannigan, B.W.; Akhavanfard, S.; Coffman, E.J.; Contino, G.; Deshpande, V.; Iafrate, A.J.; Letovsky, S.; et al. Aberrant overexpression of satellite repeats in pancreatic and other epithelial cancers. Science 2011, 331, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, K.; Iwakiri, J.; Aly, M.K.; Sakaguchi, Y.; Adachi, S.; Natsume, T.; Terai, G.; Asai, K.; Suzuki, T.; Hirose, T. m6 A modification of HSATIII lncRNAs regulates temperature-dependent splicing. EMBO J. 2021, 40, e107976. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, M.; Sengupta, S. Human satellite III long noncoding RNA imparts survival benefits to cancer cells. Cell Biol. Int. 2022, 46, 611–627. [Google Scholar] [CrossRef]
- Maison, C.; Bailly, D.; Peters, A.H.; Quivy, J.P.; Roche, D.; Taddei, A.; Lachner, M.; Jenuwein, T.; Almouzni, G. Higher-order structure in pericentric heterochromatin involves a distinct pattern of histone modification and an RNA component. Nat. Genet. 2002, 30, 329–334. [Google Scholar] [CrossRef]
- Liehr, T. False-positives and false-negatives in non-invasive prenatal testing (NIPT): What can we learn from a meta-analyses on > 750,000 tests? Mol. Cytogenet. 2022, 15, 36. [Google Scholar] [CrossRef]


| Can Access Heterochromatic CNV | |||||
|---|---|---|---|---|---|
| Cytogenomic Approach | SNPs | MicS/MinS | SSREs | SSIIDDs | CHs |
| banding cytogenetics | - | - | - | (+) | + |
| molecular cytogenetics | - | + | + | + | + |
| (Southern) blotting | + | + | (+) | + | (+) |
| Pulsed-field gel electrophoresis | - | + | (+) | + | (+) |
| microsatellite analyses | (+) | + | - | - | - |
| CMA | - | - | (+) | (+) | - |
| Sanger sequencing | + | (+) | + | (+) 1 | - |
| NGS | + | (+) | + | (+) 2 | - |
| optical genomic mapping | - | - | - | (+) | (+) |
| Cytoband | Position [GRCh38/hg38] |
|---|---|
| 1p11.1–q11 | 121,700,001–125,100,000 |
| 1q12 | 125,100,001–143,200,000 |
| 2p11.1–q11.1 | 91,800,001–96,000,000 |
| 3p11.1–q11.1 | 87,800,001–94,000,000 |
| 3q11.2 | 94,000,001–98,600,000 |
| 4p11–q11 | 48,200,001–51,800,000 |
| 5p11–q11.1 | 46,100,001–51,400,000 |
| 6p11.1–q11.1 | 58,500,001–62,600,000 |
| 7p11.1–q11.1 | 58,100,001–62,100,000 |
| 8p11.1–q11.1 | 43,200,001–47,200,000 |
| 9p11.1–q11 | 42,200,001–45,500,000 |
| 9q12 | 45,500,001–61,500,000 |
| 10p11.1–q11.1 | 38,000,001–41,600,000 |
| 11p11.1–q11.1 | 51,000,001–55,800,000 |
| 12p11.1–q11.1 | 33,200,001–37,800,000 |
| 13p13–p11.2 | 1–16,500,000 |
| 13p11.1–q11 | 16,500,001–18,900,000 |
| 14p13–p11.2 | 1–16,100,000 |
| 14p11.1–q11.1 | 16,100,001–18,200,000 |
| 15p13–p11.2 | 1–17,500,000 |
| 15p11.1–q11.1 | 17,500,001–20,500,000 |
| 16p11.1–q11.1 | 35,300,001–38,400,000 |
| 17p11.1–q11.1 | 22,700,001–27,400,000 |
| 18p11.1–q11.1 | 15,400,001–21,500,000 |
| 19p11–q11 | 24,200,001–28,100,000 |
| 20p11.1–q11.1 | 25,700,001–30,400,000 |
| 21p13–p11.2 | 1–10,900,000 |
| 21p11.1–q11 | 10,900,001–13,00,000 |
| 22p13–p11.2 | 1–13,700,000 |
| 22p11.1–q11.1 | 13,700,001–17,400,000 |
| Xp11.1–q11.1 | 58,100,001–63,800,000 |
| Yp11.1–q11.1 | 10,300,001–10,600,000 |
| Yq12 | 26,600,001–57,227,415 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liehr, T. Chromosomal Heteromorphisms and Cancer Susceptibility Revisited. Cells 2022, 11, 3239. https://doi.org/10.3390/cells11203239
Liehr T. Chromosomal Heteromorphisms and Cancer Susceptibility Revisited. Cells. 2022; 11(20):3239. https://doi.org/10.3390/cells11203239
Chicago/Turabian StyleLiehr, Thomas. 2022. "Chromosomal Heteromorphisms and Cancer Susceptibility Revisited" Cells 11, no. 20: 3239. https://doi.org/10.3390/cells11203239
APA StyleLiehr, T. (2022). Chromosomal Heteromorphisms and Cancer Susceptibility Revisited. Cells, 11(20), 3239. https://doi.org/10.3390/cells11203239






