Induction of Cardiac Pathology: Endogenous versus Exogenous Nrf2 Upregulation
Abstract
1. Introduction
2. Nrf2 Composition
2.1. Nrf2 Activation Mechanism
2.1.1. Basal Expression/Repression of Nrf2: Keap1, ROS, and Autophagy
2.1.2. Nrf2 Action: Pre-Induction
2.1.3. Nrf2 Full Induction, Transcription, and Purpose of Target Genes
| Function | Gene | Description | Ref. |
|---|---|---|---|
| Detoxification Phase II | AHR | Aryl hydrocarbon receptor | [2] |
| CYP1B1 | Cytochrome P450 Family 1 Subfamily B Member 1 | [2] | |
| ALDH3A2 | Aldehyde Dehydrogenase 3 Family Member A2 | [2] | |
| NQO1 | NAD(P)H Quinone Dehydrogenase 1 | [2] | |
| AKR1C1 | Aldo-Keto Reductase Family 1 Member C1 | [40] | |
| GSTM3 | Glutathione S-Transferase Mu 3 | [40] | |
| Antioxidant Defense | GPX4 | Glutathione Peroxidase 4 | [2] |
| GSR1 | Glutathione reductase, mitochondrial | [2] | |
| TXN1 | Thioredoxin | [2] | |
| PRDX1 | Peroxiredoxin 1 | [2] | |
| SRXN1 | Sulfiredoxin 1 | [2] | |
| SOD1/2 | Superoxide dismutase 1 and 2 | [41] | |
| HO-1 | Heme Oxygenase 1 | [42] | |
| GSTM3 | Glutathione S-Transferase Mu 3 | [40] | |
| Pentose Phosphate Pathway | G6PD | Glucose-6-Phosphate Dehydrogenase | [40] |
| PGD | Phosphogluconate dehydrogenase | [3] | |
| TKT | Transketolase | [3] | |
| Serine/Glycine Biosynthesis | PHGDH | Phosphoglycerate Dehydrogenase | [31] |
| PSAT1 | Phosphoserine Aminotransferase 1 | [31] | |
| SHMT1/2 | Serine Hydroxymethyltransferase 1/2 | [31] | |
| Membrane Trafficking | RAB6B | Ras-related protein Rab-6B | [40] |
| Deubiquitination | UCH-L1 | Ubiquitin C-terminal hydrolase L1 | [40] |
| Zinc Finger Protein | TRIM16L | Tripartite motif-containing protein 16 | [40] |
| Glycolysis/ Glycogen Synthesis | HK1/2 | Hexokinase 1 and 2 | [3] |
| GP11 | Glucose phosphate isomerase 1 | [3] | |
| ALDA | Fructose-bisphosphate aldolase A | [3] | |
| ENO1 | Enolase 1 | [3] | |
| PKM2 | Pyruvate kinase muscle isoform 2 | [3] | |
| GLUT1 | Glucose transporter 1 | [3] |
2.1.4. Nrf2 Post-Induction: Proteasomal Degradation
3. Effects of Nrf2 in the Heart versus Other Systems
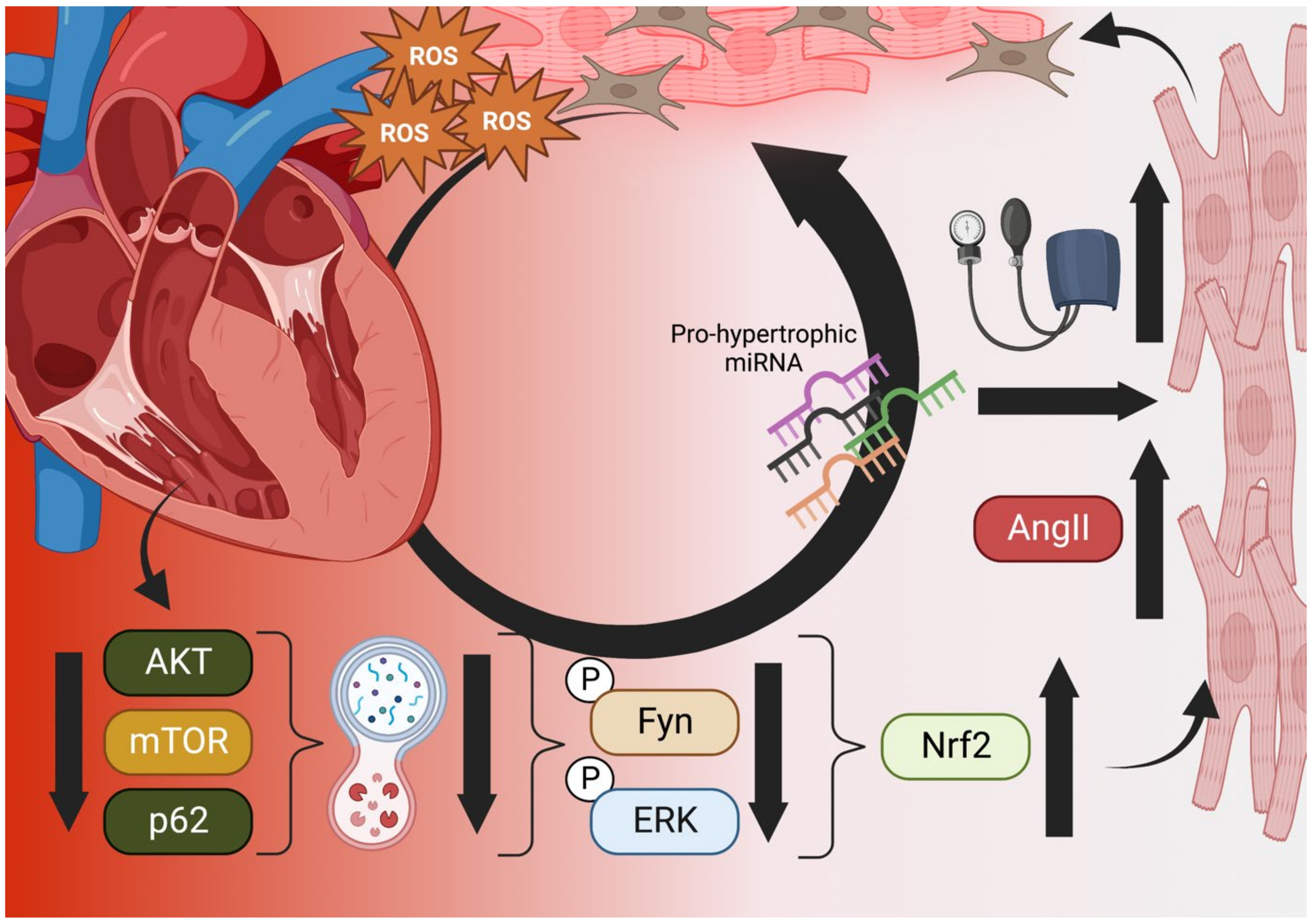
3.1. Nrf2 in the Myocardium: Not a Silver Bullet
3.2. Nrf2 in the Failing Heart: Autophagy as a Keystone Mechanism
3.3. Nrf2 in the Kidneys
4. Clinical Nrf2 Modulators
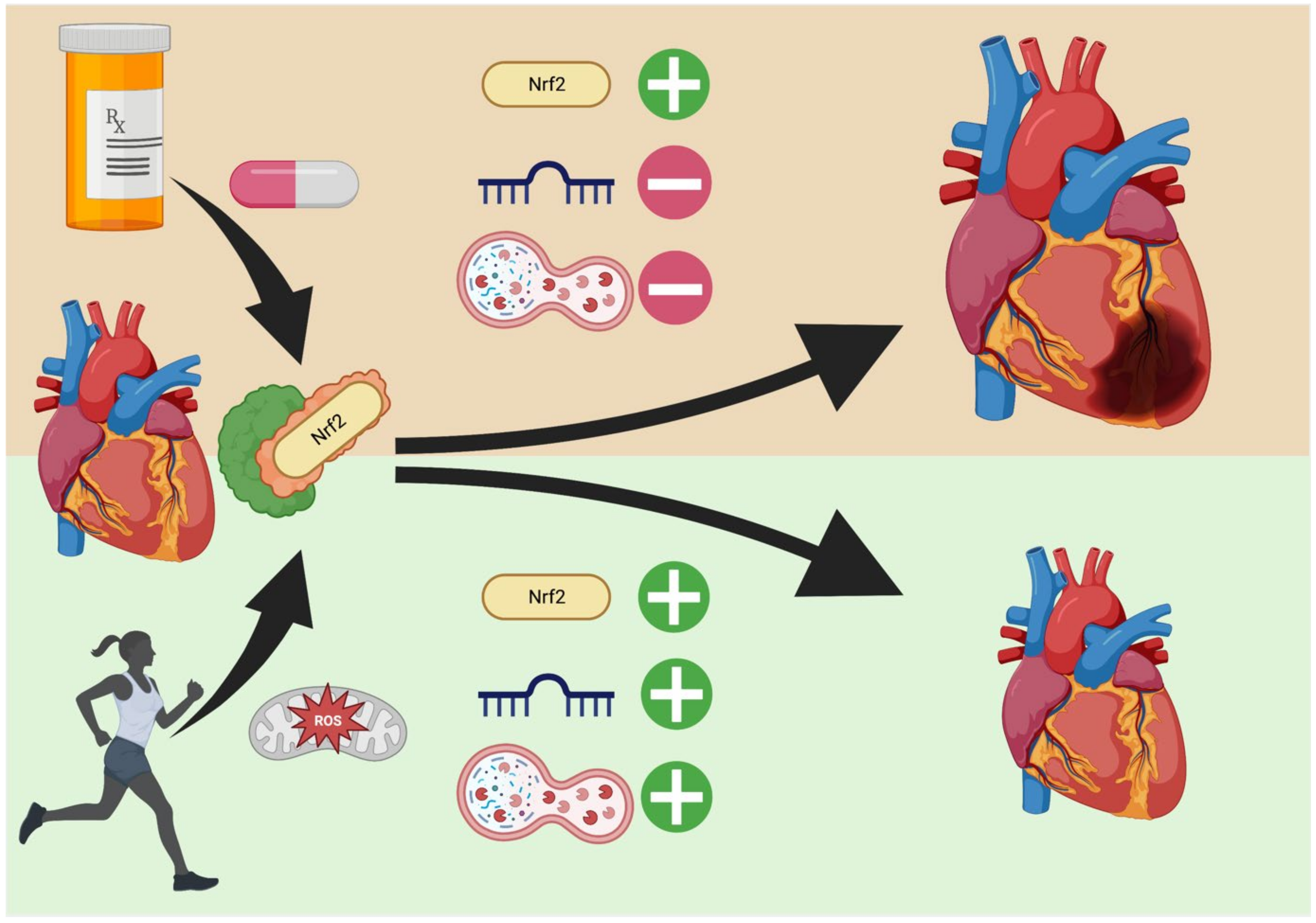
4.1. Exercise versus Exogenous Regulation
4.2. Clinical Trials with Exogenous Nrf2 Modulators
4.3. Clinical Trial Commentary: Reata Bardoloxone Trials
4.4. Clinical Perspective: Usefulness of Nrf2 Modulation in Heart Pathologies
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sykiotis, G.P.; Bohmann, D. Stress-Activated Cap’n’collar Transcription Factors in Aging and Human Disease. Sci. Signal. 2010, 3, re3. [Google Scholar] [CrossRef] [PubMed]
- Cuadrado, A.; Rojo, A.I.; Wells, G.; Hayes, J.D.; Cousin, S.P.; Rumsey, W.L.; Attucks, O.C.; Franklin, S.; Levonen, A.-L.; Kensler, T.W.; et al. Therapeutic targeting of the NRF2 and KEAP1 partnership in chronic diseases. Nat. Rev. Drug Discov. 2019, 18, 295–317. [Google Scholar] [CrossRef] [PubMed]
- He, F.; Ru, X.; Wen, T. NRF2, a Transcription Factor for Stress Response and Beyond. Int. J. Mol. Sci. 2020, 21, 4777. [Google Scholar] [CrossRef] [PubMed]
- Mathis, B.J.; Cui, T. The Role of Nrf2 in the Cardiovascular System and Atherosclerosis. In Nrf2 and its Modulation in Inflammation; Progress in Inflammation Research; Springer: Berlin/Heidelberg, Germany, 2020; pp. 97–127. [Google Scholar] [CrossRef]
- McMahon, M.; Thomas, N.; Itoh, K.; Yamamoto, M.; Hayes, J.D. Redox-regulated Turnover of Nrf2 Is Determined by at Least Two Separate Protein Domains, the Redox-sensitive Neh2 Degron and the Redox-insensitive Neh6 Degron. J. Biol. Chem. 2004, 279, 31556–31567. [Google Scholar] [CrossRef]
- Hushpulian, D.M.; Kaidery, N.A.; Ahuja, M.; Poloznikov, A.A.; Sharma, S.M.; Gazaryan, I.G.; Thomas, B. Challenges and Limitations of Targeting the Keap1-Nrf2 Pathway for Neurotherapeutics: Bach1 De-Repression to the Rescue. Front. Aging Neurosci. 2021, 13, 673205. [Google Scholar] [CrossRef]
- UniProt Consortium. UniProt: The universal protein knowledgebase in Nucleic acids research. Nucleic Acids Res. 2021, 49, D480–D489. [Google Scholar] [CrossRef]
- Mathis, B.J.; Cui, T. CDDO and Its Role in Chronic Diseases. In Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2016; Volume 929, pp. 291–314. Available online: http://www.ncbi.nlm.nih.gov/pubmed/27771930 (accessed on 2 November 2022).
- Poh, J.; Ponsford, A.H.; Boyd, J.; Woodsmith, J.; Stelzl, U.; Wanker, E.; Harper, N.; MacEwan, D.; Sanderson, C.M. A functionally defined high-density NRF2 interactome reveals new conditional regulators of ARE transactivation. Redox Biol. 2020, 37, 101686. [Google Scholar] [CrossRef]
- Tonelli, C.; Chio, I.I.C.; Tuveson, D.A. Transcriptional Regulation by Nrf2. Antioxid. Redox Signal. 2018, 29, 1727–1745. [Google Scholar] [CrossRef]
- Qin, J.-J.; Cheng, X.-D.; Zhang, J.; Zhang, W.-D. Dual roles and therapeutic potential of Keap1-Nrf2 pathway in pancreatic cancer: A systematic review. Cell Commun. Signal. 2019, 17, 121. [Google Scholar] [CrossRef]
- Nioi, P.; Nguyen, T.; Sherratt, P.J.; Pickett, C.B. The Carboxy-Terminal Neh3 Domain of Nrf2 Is Required for Transcriptional Activation. Mol. Cell. Biol. 2005, 25, 10895–10906. [Google Scholar] [CrossRef]
- Raghunath, A.; Sundarraj, K.; Nagarajan, R.; Arfuso, F.; Bian, J.; Kumar, A.P.; Sethi, G.; Perumal, E. Antioxidant response elements: Discovery, classes, regulation and potential applications. Redox Biol. 2018, 17, 297–314. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Kong, A.-N. Molecular mechanisms of Nrf2-mediated antioxidant response. Mol. Carcinog. 2008, 48, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Ortet, P.C.; Muellers, S.N.; Viarengo-Baker, L.A.; Streu, K.; Szymczyna, B.R.; Beeler, A.B.; Allen, K.N.; Whitty, A. Recapitulating the Binding Affinity of Nrf2 for KEAP1 in a Cyclic Heptapeptide, Guided by NMR, X-ray Crystallography, and Machine Learning. J. Am. Chem. Soc. 2021, 143, 3779–3793. [Google Scholar] [CrossRef] [PubMed]
- Dinkova-Kostova, A.T.; Kostov, R.V.; Canning, P. Keap1, the cysteine-based mammalian intracellular sensor for electrophiles and oxidants. Arch. Biochem. Biophys. 2017, 617, 84–93. [Google Scholar] [CrossRef]
- Naidu, S.D.; Muramatsu, A.; Saito, R.; Asami, S.; Honda, T.; Hosoya, T.; Itoh, K.; Yamamoto, M.; Suzuki, T.; Dinkova-Kostova, A.T. C151 in KEAP1 is the main cysteine sensor for the cyanoenone class of NRF2 activators, irrespective of molecular size or shape. Sci. Rep. 2018, 23, 8037. [Google Scholar] [CrossRef]
- Taguchi, K.; Fujikawa, N.; Komatsu, M.; Ishii, T.; Unno, M.; Akaike, T.; Motohashi, H.; Yamamoto, M. Keap1 degradation by autophagy for the maintenance of redox homeostasis. Proc. Natl. Acad. Sci. USA 2012, 109, 13561–13566. [Google Scholar] [CrossRef]
- Tebay, L.E.; Robertson, H.; Durant, S.T.; Vitale, S.R.; Penning, T.M.; Dinkova-Kostova, A.T.; Hayes, J.D. Mechanisms of activation of the transcription factor Nrf2 by redox stressors, nutrient cues, and energy status and the pathways through which it attenuates degenerative disease. Free Radic. Biol. Med. 2015, 88, 108–146. [Google Scholar] [CrossRef]
- Park, J.-Y.; Kim, S.; Sohn, H.Y.; Koh, Y.H.; Jo, C. TFEB activates Nrf2 by repressing its E3 ubiquitin ligase DCAF11 and promoting phosphorylation of p62. Sci. Rep. 2019, 9, 14354. [Google Scholar] [CrossRef]
- Chowdhry, S.; Zhang, Y.; McMahon, M.; Sutherland, C.; Cuadrado, A.; Hayes, J.D. Nrf2 is controlled by two distinct β-TrCP recognition motifs in its Neh6 domain, one of which can be modulated by GSK-3 activity. Oncogene 2013, 32, 3765–3781. [Google Scholar] [CrossRef]
- Brewer, A.C.; Murray, T.V.; Arno, M.; Zhang, M.; Anilkumar, N.P.; Mann, G.E.; Shah, A.M. Nox4 regulates Nrf2 and glutathione redox in cardiomyocytes in vivo. Free Radic. Biol. Med. 2011, 51, 205–215. [Google Scholar] [CrossRef]
- Theodore, M.; Kawai, Y.; Yang, J.; Kleshchenko, Y.; Reddy, S.P.; Villalta, F.; Arinze, I.J. Multiple Nuclear Localization Signals Function in the Nuclear Import of the Transcription Factor Nrf2. J. Biol. Chem. 2008, 283, 8984–8994. [Google Scholar] [CrossRef] [PubMed]
- Joo, M.S.; Kim, W.D.; Lee, K.Y.; Kim, J.H.; Koo, J.H.; Kim, S.G. AMPK Facilitates Nuclear Accumulation of Nrf2 by Phosphorylating at Serine 550. Mol. Cell. Biol. 2016, 36, 1931–1942. [Google Scholar] [CrossRef] [PubMed]
- De la Vega, M.R.; Chapman, E.; Zhang, D.D. NRF2 and the Hallmarks of Cancer. Cancer Cell 2018, 34, 21–43. [Google Scholar]
- Zang, H.; Mathew, R.O.; Cui, T. The Dark Side of Nrf2 in the Heart. Front. Physiol. 2020, 11, 722. [Google Scholar] [CrossRef]
- Jaganjac, M.; Milkovic, L.; Sunjic, S.B.; Zarkovic, N. The NRF2, Thioredoxin, and Glutathione System in Tumorigenesis and Anti-cancer Therapies. Antioxidants 2020, 9, 1151. [Google Scholar] [CrossRef]
- Sun, J.; Hoshino, H.; Takaku, K.; Nakajima, O.; Muto, A.; Suzuki, H.; Tashiro, S.; Takahashi, S.; Shibahara, S.; Alam, J.; et al. Hemoprotein Bach1 regulates enhancer availability of heme oxygenase-1 gene. EMBO J. 2002, 21, 5216–5224. [Google Scholar] [CrossRef]
- Zhang, X.; Guo, J.; Wei, X.; Niu, C.; Jia, M.; Li, Q.; Meng, D. Bach1: Function, Regulation, and Involvement in Disease. Oxidative Med. Cell. Longev. 2018, 2018, 1347969. [Google Scholar] [CrossRef]
- Nishizawa, H.; Matsumoto, M.; Shindo, T.; Saigusa, D.; Kato, H.; Suzuki, K.; Sato, M.; Ishii, Y.; Shimokawa, H.; Igarashi, K. Ferroptosis is controlled by the coordinated transcriptional regulation of glutathione and labile iron metabolism by the transcription factor BACH1. J. Biol. Chem. 2020, 295, 69–82. [Google Scholar] [CrossRef]
- DeNicola, G.M.; Chen, P.-H.; Mullarky, E.; Sudderth, J.A.; Hu, Z.; Wu, D.; Tang, H.; Xie, Y.; Asara, J.M.; Huffman, K.E.; et al. NRF2 regulates serine biosynthesis in non-small cell lung cancer. Nat. Genet. 2015, 47, 1475–1481. [Google Scholar] [CrossRef]
- Wang, W.; Li, S.; Wang, H.; Li, B.; Shao, L.; Lai, Y.; Horvath, G.; Wang, Q.; Yamamoto, M.; Janicki, J.S.; et al. Nrf2 enhances myocardial clearance of toxic ubiquitinated proteins. J. Mol. Cell. Cardiol. 2014, 72, 305–315. [Google Scholar] [CrossRef]
- Chio, I.I.C.; Jafarnejad, S.M.; Ponz-Sarvise, M.; Park, Y.; Rivera, K.; Palm, W.; Wilson, J.; Sangar, V.; Hao, Y.; Öhlund, D.; et al. NRF2 Promotes Tumor Maintenance by Modulating mRNA Translation in Pancreatic Cancer. Cell 2016, 166, 963–976. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Thimmulappa, R.K.; Kumar, V.; Cui, W.; Kumar, S.; Kombairaju, P.; Zhang, H.; Margolick, J.; Matsui, W.; Macvittie, T.; et al. NRF2-mediated Notch pathway activation en-hances hematopoietic reconstitution following myelosuppressive radiation. J. Clin. Investig. 2014, 124, 730–741. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, N.; Chartoumpekis, D.V.; Kensler, T.W. Crosstalk between Nrf2 and Notch signaling. Free Radic. Biol. Med. 2015, 88, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Chai, D.; Zhang, L.; Xi, S.; Cheng, Y.; Jiang, H.; Hu, R. Nrf2 Activation Induced by Sirt1 Ameliorates Acute Lung Injury After Intestinal Ischemia/Reperfusion Through NOX4-Mediated Gene Regulation. Cell. Physiol. Biochem. 2018, 46, 781–792. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, K.; Papagiannakopoulos, T.; Motohashi, H. Metabolic features of cancer cells in NRF2 addiction status. Biophys. Rev. 2020, 12, 435–441. [Google Scholar] [CrossRef]
- Dodson, M.; Anandhan, A.; Zhang, D.D.; Madhavan, L. An NRF2 Perspective on Stem Cells and Ageing. Front. Aging 2021, 2, 690686. [Google Scholar] [CrossRef]
- Safran, M.; Rosen, N.; Twik, M.; BarShir, R.; Stein, T.I.; Dahary, D.; Fishilevich, S.; Lancet, D. The GeneCards Suite; Springer: Berlin/Heidelberg, Germany, 2021; pp. 27–56. [Google Scholar] [CrossRef]
- Namani, A.; Rahaman, M.; Chen, M.; Tang, X. Gene-expression signature regulated by the KEAP1-NRF2-CUL3 axis is associated with a poor prognosis in head and neck squamous cell cancer. BMC Cancer 2018, 18, 46. [Google Scholar] [CrossRef]
- De Freitas Alves, A.; de Moura, A.C.; Andreolla, H.F.; Gorini da Veiga, A.B.; Fiegenbaum, M.; Giovenardi, M.; Almeida, A. Gene expression evaluation of antioxidant enzymes in patients with hepatocellular carcinoma: RT-qPCR and bioinformatic analyses. Genet. Mol. Biol. 2021, 44, e20190373. [Google Scholar] [CrossRef]
- Loboda, A.; Damulewicz, M.; Pyza, E.; Jozkowicz, A.; Dulak, J. Role of Nrf2/HO-1 system in development, oxidative stress response and diseases: An evolutionarily conserved mechanism. Cell. Mol. Life Sci. 2016, 73, 3221–3247. [Google Scholar] [CrossRef]
- Li, W.; Jain, M.R.; Chen, C.; Yue, X.; Hebbar, V.; Zhou, R.; Kong, A.-N.T. Nrf2 Possesses a Redox-insensitive Nuclear Export Signal Overlapping with the Leucine Zipper Motif. J. Biol. Chem. 2005, 280, 28430–28438. [Google Scholar] [CrossRef]
- Burroughs, A.F.; Eluhu, S.; Whalen, D.; Goodwin, J.S.; Sakwe, A.M.; Arinze, I.J. PML-Nuclear Bodies Regulate the Stability of the Fusion Protein Dendra2-Nrf2 in the Nucleus. Cell. Physiol. Biochem. 2018, 47, 800–816. [Google Scholar] [CrossRef] [PubMed]
- Walters, T.S.; McIntosh, D.J.; Ingram, S.M.; Tillery, L.; Motley, E.D.; Arinze, I.J.; Misra, S. SUMO-Modification of Human Nrf2 at K110 and K533 Regulates Its Nucleocytoplasmic Localization, Stability and Transcriptional Activity. Cell. Physiol. Biochem. 2021, 55, 141–159. [Google Scholar] [PubMed]
- Qin, Q.; Qu, C.; Niu, T.; Zang, H.; Qi, L.; Lyu, L.; Wang, X.; Nagarkatti, M.; Nagarkatti, P.; Janicki, J.S.; et al. Nrf2-Mediated Cardiac Maladaptive Remodeling and Dysfunction in a Setting of Autophagy Insufficiency. Hypertension 2016, 67, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Lu, H.; Bai, Y. Nrf2 in cancers: A double-edged sword. Cancer Med. 2019, 8, 2252–2267. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.I.E.; Buckberg, G.D. The Myocardial Oxygen Supply:Demand Index Revisited. J. Am. Heart Assoc. 2014, 3, e000285. [Google Scholar] [CrossRef] [PubMed]
- Moris, D.; Spartalis, M.; Tzatzaki, E.; Spartalis, E.; Karachaliou, G.-S.; Triantafyllis, A.S.; Karaolanis, G.I.; Tsilimigras, D.I.; Theocharis, S. The role of reactive oxygen species in myocardial redox signaling and regulation. Ann. Transl. Med. 2017, 5, 324. [Google Scholar] [CrossRef] [PubMed]
- Noseda, M.; Abreu-Paiva, M.; Schneider, M.D. The Quest for the Adult Cardiac Stem Cell. Circ. J. 2015, 79, 1422–1430. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Li, Z.; Bao, P.; Chen, M.; Zhang, M.; Yan, F.; Xu, Y.; Ji, C.; Hu, X.; Sanchis, D. Nrf2 deficiency aggravates Angiotensin II-induced cardiac injury by in-creasing hypertrophy and enhancing IL-6/STAT3-dependent inflammation. Biochim. Biophys. Acta 2019, 1865, 1253–1264. [Google Scholar] [CrossRef]
- Syed, A.M.; Kundu, S.; Ram, C.; Kulhari, U.; Kumar, A.; Mugale, M.N.; Mohapatra, P.; Murty, U.S.; Sahu, B.D. Up-regulation of Nrf2/HO-1 and inhibition of TGF-β1/Smad2/3 signaling axis by daphnetin alleviates transverse aortic constriction-induced cardiac remodeling in mice. Free Radic. Biol. Med. 2022, 186, 17–30. [Google Scholar] [CrossRef]
- Gutiérrez-Cuevas, J.; Galicia-Moreno, M.; Monroy-Ramírez, H.C.; Sandoval-Rodriguez, A.; García-Bañuelos, J.; Santos, A.; Armendariz-Borunda, J. The Role of NRF2 in Obesity-Associated Cardiovascular Risk Factors. Antioxidants 2022, 11, 235. [Google Scholar] [CrossRef]
- Zhou, S.; Sun, W.; Zhang, Z.; Zheng, Y. The Role of Nrf2-Mediated Pathway in Cardiac Remodeling and Heart Failure. Oxidative Med. Cell. Longev. 2014, 2014, 260429. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; An, L.; Taylor, M.R.G.; Chen, Q.M. Nrf2 signaling in heart failure: Expression of Nrf2, Keap1, antioxidant, and detoxification genes in dilated or ischemic cardiomyopathy. Physiol. Genom. 2022, 54, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Leopold, J.A. Antioxidants and coronary artery disease: From pathophysiology to preventive therapy. Coron. Artery Dis. 2015, 26, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, A.D.J.; Kitts, D.; Giovannucci, E.L.; Sahye-Pudaruth, S.; Paquette, M.; Mejia, S.B.; Patel, D.; Kavanagh, M.; Tsirakis, T.; Kendall, C.W.C.; et al. Selenium, antioxidants, cardiovascular disease, and all-cause mortality: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2020, 112, 1642–1652. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Weinstein, S.J.; Yu, K.; Männistö, S.; Albanes, D. Serum Beta Carotene and Overall and Cause-Specific Mortality. Circ. Res. 2018, 123, 1339–1349. [Google Scholar] [CrossRef] [PubMed]
- Henkel, R.; Sandhu, I.S.; Agarwal, A. The excessive use of antioxidant therapy: A possible cause of male infertility? Andrologia 2019, 51, e13162. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.P.; Butler, J.; Rossignol, P.; Pitt, B.; Anker, S.D.; Kosiborod, M.; Lund, L.H.; Bakris, G.L.; Weir, M.R.; Zannad, F. Abnormalities of Potassium in Heart Failure: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 2836–2850. [Google Scholar] [CrossRef]
- Abdellatif, M.; Sedej, S.; Carmona-Gutierrez, D.; Madeo, F.; Kroemer, G. Autophagy in Cardiovascular Aging. Circ. Res. 2018, 123, 803–824. [Google Scholar] [CrossRef]
- Marks, A.R. Calcium cycling proteins and heart failure: Mechanisms and therapeutics. J. Clin. Investig. 2013, 123, 46–52. [Google Scholar] [CrossRef]
- Bitto, A.; Lerner, C.; Torres, C.; Roell, M.; Malaguti, M.; Perez, V.; Lorenzini, A.; Hrelia, S.; Ikeno, Y.; Matzko, M.E.; et al. Long-Term IGF-I Exposure Decreases Autophagy and Cell Viability. PLoS ONE 2010, 5, e12592. [Google Scholar] [CrossRef]
- Yang, M.; Wen, T.; Chen, H.; Deng, J.; Yang, C.; Zhang, Z. Knockdown of insulin-like growth factor 1 exerts a protective effect on hypoxic injury of aged BM-MSCs: Role of autophagy. Stem Cell Res. Ther. 2018, 9, 284. [Google Scholar] [CrossRef] [PubMed]
- Ben Wang, B.; Shi, Y.; Chen, J.; Shao, Z.; Ni, L.; Lin, Y.; Wu, Y.; Tian, N.; Zhou, Y.; Sun, L.; et al. High glucose suppresses autophagy through the AMPK pathway while it induces autophagy via oxidative stress in chondrocytes. Cell Death Dis. 2021, 12, 506. [Google Scholar] [CrossRef] [PubMed]
- Bagherniya, M.; Butler, A.E.; Barreto, G.E.; Sahebkar, A. The effect of fasting or calorie restriction on autophagy induction: A review of the literature. Ageing Res. Rev. 2018, 47, 183–197. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Long, J.; Liu, J. Autophagy: Cancer, Other Pathologies, Inflammation, Immunity, Infection, and Aging; Elsevier: Amsterdam, The Netherlands, 2014; pp. 105–115. [Google Scholar]
- Salin, K.; Villasevil, E.M.; Anderson, G.J.; Auer, S.K.; Selman, C.; Hartley, R.C.; Mullen, W.; Chinopoulos, C.; Metcalfe, N.B. Decreased mitochondrial metabolic requirements in fasting animals carry an oxidative cost. Funct. Ecol. 2018, 32, 2149–2157. [Google Scholar] [CrossRef] [PubMed]
- Quan, W.; Lim, Y.-M.; Lee, M.-S. Role of autophagy in diabetes and endoplasmic reticulum stress of pancreatic β-cells. Exp. Mol. Med. 2012, 44, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Kanamori, H.; Takemura, G.; Goto, K.; Tsujimoto, A.; Mikami, A.; Ogino, A.; Watanabe, T.; Morishita, K.; Okada, H.; Kawasaki, M.; et al. Autophagic adaptations in diabetic cardiomyopathy differ between type 1 and type 2 diabetes. Autophagy 2015, 11, 1146–1160. [Google Scholar] [CrossRef]
- Wu, W.; Qin, Q.; Ding, Y.; Zang, H.; Li, D.-S.; Nagarkatti, M.; Nagarkatti, P.; Wang, W.; Wang, X.; Cui, T. Autophagy Controls Nrf2-Mediated Dichotomy in Pressure Over-loaded Hearts. Front. Physiol. 2021, 13, 12. [Google Scholar]
- Jiang, T.; Harder, B.; Rojo de la Vega, M.; Wong, P.K.; Chapman, E.; Zhang, D.D. p62 links autophagy and Nrf2 signaling. Free Radic. Biol. Med. 2015, 88 Pt B, 199–204. [Google Scholar] [CrossRef]
- Nezu, M.; Suzuki, N. Roles of Nrf2 in Protecting the Kidney from Oxidative Damage. Int. J. Mol. Sci. 2020, 21, 2951. [Google Scholar] [CrossRef]
- Kriz, W. Adenosine and ATP: Traffic regulators in the kidney. J. Clin. Investig. 2004, 114, 611–613. [Google Scholar] [CrossRef]
- Guerrero-Hue, M.; Rayego-Mateos, S.; Vázquez-Carballo, C.; Palomino-Antolín, A.; García-Caballero, C.; Opazo-Rios, L.; Morgado-Pascual, J.L.; Herencia, C.; Mas, S.; Ortiz, A. Protective Role of Nrf2 in Renal Disease. Antioxidants 2020, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Nezu, M.; Suzuki, N. Nrf2 activation for kidney disease treatment—A mixed blessing? Kidney Int. 2021, 99, 20–22. [Google Scholar] [CrossRef] [PubMed]
- Rush, B.M.; Bondi, C.D.; Stocker, S.D.; Barry, K.M.; Small, S.A.; Ong, J.; Jobbagy, S.; Stolz, D.B.; Bastacky, S.I.; Chartoumpekis, D.V. Genetic or pharmacologic Nrf2 activation increases proteinuria in chronic kidney disease in mice. Kidney Int. 2021, 99, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.; Livingston, M.J.; Liu, Z.; Dong, Z. Autophagy in kidney homeostasis and disease. Nat. Rev. Nephrol. 2020, 16, 489–508. [Google Scholar] [CrossRef]
- Robledinos-Antón, N.; Fernández-Ginés, R.; Manda, G.; Cuadrado, A. Activators and Inhibitors of NRF2: A Review of Their Potential for Clinical Development. Oxidative Med. Cell. Longev. 2019, 2019, 9372182. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Quan, J.I.; Li, L.; Kinghorn, K.J.; Ivanov, D.K.; Tain, L.S.; Slack, C.; Kerr, F.; Nespital, T.; Thornton, J.; Hardy, J.; et al. Lithium Promotes Longevity through GSK3/NRF2-Dependent Hormesis. Cell Rep. 2016, 15, 638–650. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Gu, X.; Gao, J.; Wang, Z.; Liu, G.; Barkema, H.W.; Han, B. Chlorogenic acid promotes the Nrf2/HO-1 anti-oxidative pathway by activating p21Waf1/Cip1 to resist dexamethasone-induced apoptosis in osteoblastic cells. Free Radic. Biol. Med. 2019, 137, 1–12. [Google Scholar] [CrossRef]
- Ahuja, M.; Kaidery, N.A.; Yang, L.; Calingasan, N.; Smirnova, N.; Gaisin, A.; Gaisina, I.N.; Gazaryan, I.; Hushpulian, D.M.; Kaddour-Djebbar, I.; et al. Distinct Nrf2 Signaling Mechanisms of Fumaric Acid Esters and Their Role in Neuroprotection against 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Induced Experimental Parkinson’s-Like Disease. J. Neurosci. 2016, 36, 6332–6351. [Google Scholar] [CrossRef]
- Unoki, T.; Akiyama, M.; Kumagai, Y. Nrf2 Activation and Its Coordination with the Protective Defense Systems in Response to Electrophilic Stress. Int. J. Mol. Sci. 2020, 21, 545. [Google Scholar] [CrossRef]
- Egbujor, M.C.; Petrosino, M.; Zuhra, K.; Saso, L. The Role of Organosulfur Compounds as Nrf2 Activators and Their Antioxidant Effects. Antioxidants 2022, 11, 1255. [Google Scholar] [CrossRef]
- Shin, J.W.; Chun, K.-S.; Kim, D.-H.; Kim, S.-J.; Kim, S.H.; Cho, N.-C.; Na, H.-K.; Surh, Y.-J. Curcumin induces stabilization of Nrf2 protein through Keap1 cysteine modification. Biochem. Pharmacol. 2020, 173, 113820. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Eggler, A.L.; Liu, D.; Liu, G.; Mesecar, A.D.; van Breemen, R.B. Sites of alkylation of human Keap1 by natural chemoprevention agents. J. Am. Soc. Mass Spectrom. 2007, 18, 2226–2232. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Weng, X.; Bao, X.; Bai, X.; Lv, Y.; Zhang, S.; Chen, Y.; Zhao, C.; Zeng, M.; Huang, J.; et al. A novel anti-atherosclerotic mechanism of quercetin: Competitive binding to KEAP1 via Arg483 to inhibit macrophage pyroptosis. Redox Biol. 2022, 57, 102511. [Google Scholar] [CrossRef] [PubMed]
- Egea, J.; Buendia, I.; Parada, E.; Navarro, E.; Rada, P.; Cuadrado, A.; López, M.G.; García, A.G.; León, R. Melatonin-sulforaphane hybrid ITH12674 induces neuro-protection in oxidative stress conditions by a “drug-prodrug” mechanism of action. Br. J. Pharmacol. 2015, 172, 1807–1821. [Google Scholar] [CrossRef]
- Liang, N.; Dupuis, J.H.; Yada, R.Y.; Kitts, D.D. Chlorogenic acid isomers directly interact with Keap 1-Nrf2 signaling in Caco-2 cells. Mol. Cell. Biochem. 2019, 457, 105–118. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, S.; Fu, X.; Zhou, W.; Hong, W.; Zou, D.; Li, X.; Liu, J.; Ran, P.; Li, B. tert-Butylhydroquinone mobilizes intracellular-bound zinc to stabilize Nrf2 through inhibiting phosphatase activity. Am. J. Physiol. Physiol. 2015, 309, C148–C158. [Google Scholar] [CrossRef]
- Mostafavi-Pour, Z.; Ramezani, F.; Keshavarzi, F.; Samadi, N. The role of quercetin and vitamin C in Nrf2-dependent oxidative stress production in breast cancer cells. Oncol. Lett. 2017, 13, 1965–1973. [Google Scholar] [CrossRef]
- Gao, L.; Wang, J.; Sekhar, K.R.; Yin, H.; Yared, N.F.; Schneider, S.N.; Sasi, S.; Dalton, T.P.; Anderson, M.E.; Chan, J.Y.; et al. Novel n-3 Fatty Acid Oxidation Products Activate Nrf2 by Destabilizing the Association between Keap1 and Cullin3. J. Biol. Chem. 2007, 282, 2529–2537. [Google Scholar] [CrossRef]
- Ahmadi, Z.; Ashrafizadeh, M. Melatonin as a potential modulator of Nrf2. Fundam. Clin. Pharmacol. 2019, 34, 11–19. [Google Scholar] [CrossRef]
- Fuda, H.; Miyanaga, S.; Furukawa, T.; Umetsu, S.; Joko, S.; Roan, Y.; Suzuki, H.; Hui, S.-P.; Watanabe, M.; Chiba, H. Flazin as a Promising Nrf2 Pathway Activator. J. Agric. Food Chem. 2019, 67, 12844–12853. [Google Scholar] [CrossRef]
- Wang, J.; Wang, H.; Sun, K.; Wang, X.; Pan, H.; Zhu, J.; Ji, X.; Li, X. Chrysin suppresses proliferation, migration, and invasion in glioblastoma cell lines via mediating the ERK/Nrf2 signaling pathway. Drug Des. Dev. Ther. 2018, 12, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Arlt, A.; Sebens, S.; Krebs, S.; Geismann, C.; Grossmann, M.; Kruse, M.-L.; Schreiber, S.; Schäfer, H. Inhibition of the Nrf2 transcription factor by the alkaloid trigonelline renders pancreatic cancer cells more susceptible to apoptosis through decreased proteasomal gene expression and proteasome activity. Oncogene 2012, 32, 4825–4835. [Google Scholar] [CrossRef] [PubMed]
- Gęgotek, A.; Skrzydlewska, E. Antioxidative and Anti-Inflammatory Activity of Ascorbic Acid. Antioxidants 2022, 11, 1993. [Google Scholar] [CrossRef] [PubMed]
- Ren, D.; Villeneuve, N.F.; Jiang, T.; Wu, T.; Lau, A.; Toppin, H.A.; Zhang, D.D. Brusatol enhances the efficacy of chemotherapy by inhibiting the Nrf2-mediated defense mechanism. Proc. Natl. Acad. Sci. USA 2011, 108, 1433–1438. [Google Scholar] [CrossRef]
- Chian, S.; Thapa, R.; Chi, Z.; Wang, X.J.; Tang, X. Luteolin inhibits the Nrf2 signaling pathway and tumor growth in vivo. Biochem. Biophys. Res. Commun. 2014, 447, 602–608. [Google Scholar] [CrossRef]
- Shanmugam, G.; Challa, A.K.; Devarajan, A.; Athmanathan, B.; Litovsky, S.H.; Krishnamurthy, P.; Davidson, C.J.; Rajasekaran, N.S. Exercise Mediated Nrf2 Signaling Protects the Myocardium from Isoproterenol-Induced Pathological Remodeling. Front. Cardiovasc. Med. 2019, 6, 68. [Google Scholar] [CrossRef]
- Kitaoka, Y. The Role of Nrf2 in Skeletal Muscle on Exercise Capacity. Antioxidants 2021, 10, 1712. [Google Scholar] [CrossRef]
- Wang, L.; Wang, J.; Cretoiu, D.; Li, G.; Xiao, J. Exercise-mediated regulation of autophagy in the cardiovascular system. J. Sport Health Sci. 2019, 9, 203–210. [Google Scholar] [CrossRef]
- Sorriento, D.; Di Vaia, E.; Iaccarino, G. Physical Exercise: A Novel Tool to Protect Mitochondrial Health. Front. Physiol. 2021, 12, 660068. [Google Scholar] [CrossRef]
- Wen, D.-T.; Zheng, L.; Li, J.-X.; Lu, K.; Hou, W.-Q. The activation of cardiac dSir2-related pathways mediates physical exercise resistance to heart aging in old Drosophila. Aging 2019, 11, 7274–7293. [Google Scholar] [CrossRef]
- Fernandes, T.; Baraúna, V.G.; Negrão, C.E.; Phillips, M.I.; Oliveira, E.M. Aerobic exercise training promotes physiological cardiac remodeling involving a set of microRNAs. Am. J. Physiol. Circ. Physiol. 2015, 309, H543–H552. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Dong, X.; Wang, Z.; Wu, J. MicroRNA-1 in Cardiac Diseases and Cancers. Korean J. Physiol. Pharmacol. 2014, 18, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Carè, A.; Catalucci, D.; Felicetti, F.; Bonci, D.; Addario, A.; Gallo, P.; Bang, M.-L.; Segnalini, P.; Gu, Y.; Dalton, N.D.; et al. MicroRNA-133 controls cardiac hypertrophy. Nat. Med. 2007, 13, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhao, S.-P.; Zhao, Y.-H. MicroRNA-143/-145 in Cardiovascular Diseases. BioMed Res. Int. 2015, 2015, 531740. [Google Scholar] [CrossRef]
- Nishi, H.; Ono, K.; Horie, T.; Nagao, K.; Kinoshita, M.; Kuwabara, Y.; Watanabe, S.; Takaya, T.; Tamaki, Y.; Takanabe-Mori, R.; et al. MicroRNA-27a Regulates Beta Cardiac Myosin Heavy Chain Gene Expression by Targeting Thyroid Hormone Receptor β1 in Neonatal Rat Ventricular Myocytes. Mol. Cell. Biol. 2011, 31, 744–755. [Google Scholar] [CrossRef]
- Livingstone, M.C.; Johnson, N.M.; Roebuck, B.D.; Kensler, T.W.; Groopman, J.D. Profound changes in miRNA expression during cancer initiation by aflatoxin B1 and their abrogation by the chemopreventive triterpenoid CDDO-Im. Mol. Carcinog. 2017, 56, 2382–2390. [Google Scholar] [CrossRef]
- Brown, G.R.; Hem, V.; Katz, K.S.; Ovetsky, M.; Wallin, C.; Ermolaeva, O.; Tolstoy, I.; Tatusova, T.; Pruitt, K.; Maglott, D.R.; et al. Gene: A gene-centered information resource at NCBI. Nucleic Acids Res. 2014, 43, D36–D42. [Google Scholar] [CrossRef]
- Chen, J.-F.; Mandel, E.M.; Thomson, J.M.; Wu, Q.; Callis, E.T.; Hammond, S.M.; Conlon, F.L.; Wang, D.-Z. The Role of MicroRNA-1 and MicroRNA-133 in Skeletal Muscle Proliferation and Differentiation. Nat. Genet. 2005, 38, 228–233. [Google Scholar] [CrossRef]
- Jeyabal, P.; Thandavarayan, R.A.; Joladarashi, D.; Babu, S.S.; Krishnamurthy, S.; Bhimaraj, A.; Youker, K.A.; Kishore, R.; Krishnamurthy, P. MicroRNA-9 inhibits hyperglycemia-induced pyroptosis in human ventricular cardiomyocytes by targeting ELAVL1. Biochem. Biophys. Res. Commun. 2016, 471, 423–429. [Google Scholar] [CrossRef]
- Wu, M.; Liu, X.; Li, Z.; Huang, X.; Guo, H.; Guo, X.; Yang, X.; Li, B.; Xuan, K.; Jin, Y. SHED aggregate exosomes shuttled miR-26a promote angiogenesis in pulp regeneration via TGF-β/SMAD2/3 signalling. Cell Prolif. 2021, 54, e13074. [Google Scholar] [CrossRef]
- Castaigne, A.D.; Duval, A.M.; Dubois-Rande, J.L.; Herve, C.; Jan, F.; Louvard, Y. Prehospital Administration of Anisoylated Plasminogen Streptokinase Activator Complex in Acute Myocardial Infarction. Drugs 1987, 33, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Liu, H.; Guo, J.; Yu, Y.; Yang, D.; He, F.; Du, Z. MicroRNA-98 negatively regulates myocardial infarction-induced apoptosis by down-regulating Fas and caspase-3. Sci. Rep. 2017, 7, 7460. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Lu, Y.; Li, Z.; Wang, Q. microRNA-133: Expression, Function and Therapeutic Potential in Muscle Diseases and Cancer. Curr. Drug Targets 2014, 15, 817–828. [Google Scholar] [CrossRef] [PubMed]
- Ye, D.; Shen, Z.; Zhou, S. Function of microRNA-145 and mechanisms underlying its role in malignant tumor diagnosis and treatment. Cancer Manag. Res. 2019, 11, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, J.; Ramanujam, D.P.; Sassi, Y.; Ahles, A.; Jentzsch, C.; Werfel, S.; Leierseder, S.; Loyer, X.; Giacca, M.; Zentilin, L.; et al. MiR-378 Controls Cardiac Hypertrophy by Combined Repression of Mitogen-Activated Protein Kinase Pathway Factors. Circulation 2013, 127, 2097–2106. [Google Scholar] [CrossRef]
- Hullinger, T.G.; Montgomery, R.L.; Seto, A.G.; Dickinson, B.A.; Semus, H.M.; Lynch, J.M.; Dalby, C.M.; Robinson, K.; Stack, C.; Latimer, P.A.; et al. Inhibition of miR-15 Protects Against Cardiac Ischemic Injury. Circ. Res. 2012, 110, 71–81. [Google Scholar] [CrossRef]
- Zheng, M.; Wang, M. A narrative review of the roles of the miR-15/107 family in heart disease: Lessons and prospects for heart disease. Ann. Transl. Med. 2021, 9, 66. [Google Scholar] [CrossRef]
- Jenike, A.E.; Halushka, M.K. miR-21: A non-specific biomarker of all maladies. Biomark. Res. 2021, 9, 18. [Google Scholar] [CrossRef]
- Li, S.; Ren, J.; Sun, Q. The expression of microRNA-23a regulates acute myocardial infarction in patients and in vitro through targeting PTEN. Mol. Med. Rep. 2018, 17, 6866–6872. [Google Scholar] [CrossRef]
- Li, D.; Shen, M.; Deng, X.; Bai, Y. MicroRNA miR-27a-3p accelerates cardiac hypertrophy by targeting neuro-oncological ventral antigen 1. Bioengineered 2022, 13, 8982–8993. [Google Scholar] [CrossRef]
- Boon, R.A.; Iekushi, K.; Lechner, S.; Seeger, T.; Fischer, A.; Heydt, S.; Kaluza, D.; Tréguer, K.; Carmona, G.; Bonauer, A.; et al. MicroRNA-34a regulates cardiac ageing and function. Nature 2013, 495, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Rech, M.; Kuhn, A.R.; Lumens, J.; Carai, P.; van Leeuwen, R.; Verhesen, W.; Verjans, R.; Lecomte, J.; Liu, Y.; Luiken, J.J.; et al. AntagomiR-103 and -107 Treatment Affects Cardiac Function and Metabolism. Mol. Ther. Nucleic Acids 2018, 14, 424–437. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.; Tao, T.; Chen, S.; Liang, C.; Qiu, Y.; Zhou, Y.; Zhang, R. MicroRNA-143 promotes cardiac ischemia-mediated mitochondrial impairment by the inhibition of protein kinase Cepsilon. Basic Res. Cardiol. 2017, 112, 60. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Li, C.; Zhang, H.; Qiu, S.; Fu, T.; Xu, Y. Downregulation of miR-146a Contributes to Cardiac Dysfunction Induced by the Tyrosine Kinase Inhibitor Sunitinib. Front. Pharmacol. 2019, 10, 914. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Ji, R.; Liao, X.; Castillero, E.; Kennel, P.J.; Brunjes, D.L.; Franz, M.; Möbius-Winkler, S.; Drosatos, K.; George, I.; et al. MicroRNA-195 Regulates Metabolism in Failing Myocardium Via Alterations in Sirtuin 3 Expression and Mitochondrial Protein Acetylation. Circulation 2018, 137, 2052–2067. [Google Scholar] [CrossRef] [PubMed]
- Gabisonia, K.; Prosdocimo, G.; Aquaro, G.D.; Carlucci, L.; Zentilin, L.; Secco, I.; Ali, H.; Braga, L.; Gorgodze, N.; Bernini, F.; et al. MicroRNA therapy stimulates uncontrolled cardiac repair after myocardial infarction in pigs. Nature 2019, 569, 418–422. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wang, Y.; Sun, X. The functions of microRNA-208 in the heart. Diabetes Res. Clin. Pract. 2020, 160, 108004. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Huang, M.; Li, Z.; Jia, F.; Ghosh, Z.; Lijkwan, M.A.; Fasanaro, P.; Sun, N.; Wang, X.; Martelli, F.; et al. MicroRNA-210 as a Novel Therapy for Treatment of Ischemic Heart Disease. Circulation 2010, 122, S124–S131. [Google Scholar] [CrossRef]
- Verjans, R.; Peters, T.; Beaumont, F.J.; van Leeuwen, R.; van Herwaarden, T.; van Verhesen, W.; Munts, C.; Bijnen, M.; Henkens, M.; Diez, J.; et al. MicroRNA-221/222 Family Coun-teracts Myocardial Fibrosis in Pressure Overload–Induced Heart Failure. Hypertension 2018, 71, 280–288. [Google Scholar] [CrossRef]
- Zhang, L.; Chen, X.; Su, T.; Li, H.; Huang, Q.; Wu, D.; Yang, C.; Han, Z. Circulating miR-499 are novel and sensitive biomarker of acute myocardial infarction. J. Thorac. Dis. 2015, 7, 303–308. [Google Scholar] [CrossRef]
- Wan, Q.; Xu, T.; Ding, W.; Zhang, X.; Ji, X.; Yu, T.; Yu, W.; Lin, Z.; Wang, J. miR-499-5p Attenuates Mitochondrial Fission and Cell Apoptosis via p21 in Doxorubicin Cardiotoxicity. Front. Genet. 2019, 9, 734. [Google Scholar] [CrossRef] [PubMed]
- Zang, H.; Wu, W.; Qi, L.; Tan, W.; Nagarkatti, P.; Nagarkatti, M.; Wang, X.; Cui, T. Autophagy Inhibition Enables Nrf2 to Exaggerate the Progression of Diabetic Cardiomyopathy in Mice. Diabetes 2020, 69, 2720–2734. [Google Scholar] [CrossRef] [PubMed]
- Wafi, A.M.; Hong, J.; Rudebush, T.L.; Yu, L.; Hackfort, B.; Wang, H.; Schultz, H.D.; Zucker, I.H.; Gao, L. Curcumin improves exercise performance of mice with coronary artery ligation-induced HFrEF: Nrf2 and antioxidant mechanisms in skeletal muscle. J. Appl. Physiol. 2019, 126, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.; Gao, L.; Zucker, I.H. Regulation of Nrf2 signaling pathway in heart failure: Role of extracellular vesicles and non-coding RNAs. Free Radic. Biol. Med. 2021, 167, 218–231. [Google Scholar] [CrossRef]
- Tian, C.; Gao, L.; Zhang, A.; Hackfort, B.T.; Zucker, I.H. Therapeutic Effects of Nrf2 Activation by Bardoxolone Methyl in Chronic Heart Failure. J. Pharmacol. Exp. Ther. 2019, 371, 642–651. [Google Scholar] [CrossRef]
- Victor, P.; Sarada, D.; Ramkumar, K.M. Pharmacological activation of Nrf2 promotes wound healing. Eur. J. Pharmacol. 2020, 886, 173395. [Google Scholar] [CrossRef]
- Schieffer, L.; Manzl, C.; Schatz, C.; Haybaeck, J.; Crismani, A. Nrf2 in the Field of Dentistry with Special Attention to NLRP3. Antioxidants 2022, 11, 149. [Google Scholar] [CrossRef]
| Function | Region | AA | Features |
|---|---|---|---|
| C-Terminus | |||
| Keap1 Binding | Neh2 | 16-89 | Nrf2 Ubiquitin degradation domain; DLG and ETGE elements |
| Functional | Neh4 | 111-134 | p300, Creb binding |
| Functional | Neh5 | 182-209 | p300, Creb binding |
| RXRa Binding | Neh7 | 209-316 | RXRa ARE repressor domain |
| Nrf2 Stabilizer | Neh6 | 337-394 | β-TrCP-mediated degradation; DSGIS/DSAPGS and Ubiquitin elements |
| DNA Binding | Neh1 | 435-569 | bZIP region for sMAF and ARE interaction; Cap N′ Collar region; nuclear localization |
| Functional | Neh3 | 569-605 | CHD6, Creb binding |
| Carboxy Terminus |
| Variant ID/ Position | Translocation | Disease/Effect |
|---|---|---|
| VAR_080492/31 | G > R | Immunodeficiency/developmental disorders, hypohomocysteinemia |
| VAR_080493/79 | E > K | Immunodeficiency/developmental disorders, hypohomocysteinemia |
| VAR_080494/80 | T > K | Immunodeficiency/developmental disorders, hypohomocysteinemia |
| VAR_080495/81 | G > S | Immunodeficiency/developmental disorders, hypohomocysteinemia |
| Disease Variants | ||
| CA16602902 | E > D | Squamous and uterine cancer |
| CA16602899 | E > Q | Lung, squamous, uterine cancers |
| CA16602901 | E > V | Lung, squamous, uterine cancers |
| CA349380460 | T > K | Disruption of redox homeostasis |
| CA349366919 | E > K | Immunodeficiency/developmental disorders, hypohomocysteinemia |
| Mutagenic Variants | Location | Effects |
| Putative | 79–82 | Reduced Keap1 interaction |
| T > A | 80 | Reduced Keap1 interaction |
| E > G | 82 | Reduced Keap1 interaction |
| K > A | 462 | Loss of function * |
| K > A | 472 | * |
| K > A | 487 | * |
| R > A | 499 | * |
| R.> A | 569 | * |
| Activate/Suppress | Action | Compound | Type/Origin | Ref. |
|---|---|---|---|---|
| Activate | Keap1 Cys151 alkylation | CDDO-Me | Triterpinoid | [79] |
| RTA-408 (omaveloxolone) | Triterpinoid | [79] | ||
| Oltipraz | Organosulfur | [79] | ||
| Sulforaphane | Organosulfur | [79] | ||
| Sulforadex | Organosulfur | [79] | ||
| Alpha lipoic acid | Organosulfur | [79] | ||
| ALKS-8700 | Fumaric acid | [79] | ||
| BG-12/Tecfidera | Fumaric acid | [79] | ||
| Dimethyl fumarate | Fumaric acid | [79] | ||
| Curcumin | Stilbene | [79,85] | ||
| Resveratrol | Stilbene | [79] | ||
| Ursodiol | Bile acid | [79] | ||
| Xanthohumol | Chalcone | [86] | ||
| Hydrogen sulfide | Inorganic | [87] | ||
| ITH12674 | Melatonin-sulforaphane | [79,88] | ||
| Keap1 Cys 273 and 278 targeting | CXA-10 | Fatty acid | [79] | |
| Keap1 Cys 368 and 513 targeting | CGA | Chlorogenic Acid | [89] | |
| Keap1 Cys 368 and 513 targeting | NMP | Chlorogenic Acid | [8] | |
| Inhibits phosphatase action on Nrf2 | tBHQ | Quinone | [8,90] | |
| Activate or Suppress | Binds to Arg415/483 or Nrf2 translocation blocker | Quercetin | Polyphenol | [8,87,91] |
| Cullin3 destabilization | DHA | Lipid | [8,92] | |
| GSK-3 inhibition | Lithium Chloride | Inorganic | [80] | |
| NF-kB regulation | Melatonin | Hormone | [93] | |
| NR | Flazin | B-carboline alkaloid | [94] | |
| Competitive binding to Keap1 | Apigenin | Quassinoid | [95] | |
| Suppress | Nrf2 translocation blocker | Trigollenine | Alkaloid | [96] |
| Nrf2 translocation blocker | Ascorbic acid | Vitamin | [97] | |
| Nrf2 Ub/Prot Turnover | Brusatol | Quassinoid | [98] | |
| Nrf2 translocation blocker | Chrysin | Quassinoid | [95] | |
| Nrf2 Transcriptional repressor | Luteolin | Quassinoid | [99] |
| Role | Gene/miRNA Type | Function | Ref. |
|---|---|---|---|
| Anti- Hypertrophic | miRNA-1 | HDAC4 targeting | [105,112] |
| miRNA-9 | Downregulation of ELAVL1-mediated inflammation | [105,113] | |
| miRNA-26a-1 | Promotes angiogenesis; MGFβ-SMAD2/3 signaling | [105,114] | |
| miRNA-98 | Downregulates FAS and caspase-3 | [105,115,116] | |
| miRNA-133 | Cardiac muscle development; SFR, HDAC4, cyclin D2 targeting | [105,117] | |
| miRNA-145 | Targets C-MYC, OCT4, SOX2, KLF4, and STAT1; inhibits SMC proliferation | [105,118] | |
| miRNA-378 | Autophagy promotion via FOXO, PDK1, and ULK1 targeting | [105,119] | |
| Pro- Hypertrophic | miRNA-15b/107 | Decreases hypoxia response; targets BCL2, ARL2, PDK4, and SGK1 | [105,120,121] |
| miRNA-21 | Pancellular expression; Interacts with PTEN, TPM1, PDCD4 | [105,122] | |
| miRNA-23a | Suppresses p53, BAX/BCL2, and PTEN | [105,123] | |
| miRNA-27a-3p | Targets NOVA1 to induce hypertrophy | [105,124] | |
| miRNA-34 | Targets PNUTS; enhances telomere shortening in cardiomyocytes | [105,125] | |
| miRNA-103 | Reduces mitochondrial oxidation | [105,126] | |
| miRNA-143 | Protein kinase C epsilon targeting | [105,127] | |
| miRNA-146a | Targets PLN and ANK2; reduces contractile ability | [105,128] | |
| miRNA-195 | Targets SIRT3 | [105,129] | |
| miRNA-199a -3p/5p | Controls cardiac repair via TAOK1, β-TrCP, Cofilin2 | [105,130] | |
| miRNA-208a/b | Downregulates SOX6 and NLK | [105,131] | |
| miRNA-210 | HIF-1alpha dependent; angiogenesis factor | [105,132] | |
| miRNA-221 | Downregulates TGF-β and SMAD2, JNK1, ETS1 | [105,133] | |
| miRNA-222 | Downregulates TGF-β and SMAD2, JNK1, ETS1 | [105,133] | |
| miRNA-499 | Targets p21 | [105,134,135] |
| Compound | Number of Studies | RCT ID | Year | Recruit Status | Cardiac Issues? | Notes |
|---|---|---|---|---|---|---|
| ALKS-8700 | 2 | NCT02634307 | 2022 | Complete | 2/239 | |
| NCT03093324 | 2020 | Complete | 1/253 | |||
| Apigenin | 12 | NCT01286324 | 2017 | Complete | 0/17 | |
| Ascorbic Acid | 1000+ | NCT03422159 | 2021 | Complete | 0/68 | |
| NCT03389555 | 2021 | Complete | 0/101 | |||
| NCT03338569 | 2021 | Complete | 4/61 | 3/64 in placebo | ||
| NCT00532844 | 2021 | Complete | 1/50 | Combination Sapropterin DiHCl | ||
| NCT01167569 | 2020 | Complete | 0/28 | |||
| NCT03148236 | 2019 | Complete | 1/10 | |||
| NCT02106975 | 2019 | Complete | 0/84 | |||
| NCT01723696 | 2019 | Complete | 3/120 | Infants | ||
| NCT01413360 | 2016 | Complete | 0/10 | |||
| NCT00621023 | 2013 | Complete | 1/6 | |||
| BG-12 | 6 | NCT00273364 | 2020 | Complete | 0/55 | |
| NCT01568112 | 2016 | Complete | 0/42 | |||
| CDDO-Me | 34 | NCT04494646 | 2022 | Complete | 0/21 | |
| NCT03366337 | 2022 | Complete | 1/18 | CDDO-Me in glomerulosclerosis | ||
| NCT00529113 | 2022 | Terminated | NR | Reata | ||
| NCT02036970 | 2021 | Complete | 4/12 | CDDO-me 5 mg vs. 0/4 in 20 mg | ||
| NCT01549769 | 2014 | Terminated | NR | Reata: Safety Concerns | ||
| NCT01351675 | 2014 | Terminated | NR | Reata | ||
| NCT01500798 | 2014 | Terminated | NR | Reata | ||
| NCT01551446 | 2012 | Withdrawn | NR | Reata | ||
| NCT01655186 | 2012 | Withdrawn | NR | Reata | ||
| NCT01576887 | 2012 | Withdrawn | NR | Reata | ||
| NCT00550849 | 2007 | Terminated | NR | Reata | ||
| Curcumin | 294 | NCT03085680 | 2022 | Complete | 0/8 | |
| NCT02494141 | 2022 | Complete | 0/34 | |||
| NCT03584724 | 2022 | Complete | 0/20 | |||
| NCT02978339 | 2020 | Complete | 0/15 | |||
| NCT01383161 | 2020 | Complete | 0/25 | |||
| NCT00094445 | 2020 | Complete | 5/44 | |||
| NCT02104752 | 2019 | Complete | 0/17 | |||
| NCT02300727 | 2019 | Terminated | 0/3 | Not enough volunteers | ||
| NCT01514370 | 2019 | Complete | 0/38 | Plus IFNB | ||
| NCT01740323 | 2019 | Complete | 3/15 | |||
| NCT00641147 | 2017 | Complete | 0/21 | |||
| NCT02556632 | 2017 | Complete | 0/64 | |||
| NCT01246973 | 2016 | Complete | 0/344 | |||
| NCT00365209 | 2015 | Complete | 0/22 | |||
| NCT00525421 | 2013 | Complete | 0/10 | |||
| NCT01042938 | 2012 | Complete | 0/14 | |||
| CXA-10 | 1 | NCT04125745 | 2022 | Terminated | 0/1 | Early termination. No safety problems |
| DHA | 94 | NCT01732874 | 2021 | Complete | 0/11 | |
| NCT01903525 | 2021 | Complete | 0/20 | |||
| NCT02514070 | 2021 | Complete | 0/33 | |||
| NCT02947100 | 2020 | Complete | 0/3 | |||
| NCT02487771 | 2018 | Complete | 0/0 | |||
| NCT01976806 | 2017 | Complete | 1/27 | Palpitations | ||
| NCT00266825 | 2016 | Complete | 0/154 | |||
| NCT00100230 | 2015 | Complete | 0/27 | |||
| NCT01007110 | 2014 | Complete | 0/35 | |||
| NCT00440050 | 2014 | Complete | 8/214 | Pulmonary embolus | ||
| Dimethyl Fumarate | 131 | NCT02981082 | 2022 | Terminated | 0/4 | Low recruitment |
| NCT04570670 | 2022 | Complete | 1/50 | |||
| NCT02739542 | 2022 | Complete | 0/44 | |||
| NCT02634307 | 2022 | Complete | 1/225 | ALKS-8700 2/239 | ||
| NCT02907177 | 2021 | Terminated | 1/68 | Low recruitment | ||
| NCT02975349 | 2021 | Active no recruit | 0/54 | |||
| NCT00835770 | 2020 | Complete | 9/868 | 3x/day 11/868 2x/day | ||
| NCT03093324 | 2020 | Complete | 0/251 | ALKS-8700 1/253 | ||
| NCT02428231 | 2020 | Terminated | 0/32 | |||
| NCT02410278 | 2020 | Complete | 0/98 | |||
| NCT02951533 | 2020 | Complete | 0/84 | |||
| NCT03331835 | 2020 | Complete | 0/102 | |||
| NCT00273364 | 2020 | Complete | 0/55 | |||
| NCT02784834 | 2019 | Terminated | 0/2 | No funding | ||
| NCT02525874 | 2019 | Complete | 1/218 | |||
| NCT02555215 | 2019 | Complete | 1/20 | |||
| NCT03255382 | 2019 | Complete | 0/57 | Fumaderm | ||
| NCT02634801 | 2019 | Complete | 0/19 | |||
| NCT02438137 | 2017 | Complete | 1/21 | MI | ||
| NCT02125604 | 2017 | Complete | 0/211 | |||
| NCT01156311 | 2017 | Complete | 3/57 | With IFNB, 1/47 with Glatiramer acetate | ||
| NCT02430532 | 2017 | Terminated | 0/28 | Sponsor terminated | ||
| NCT02410200 | 2017 | Complete | 0/22 | |||
| NCT01873417 | 2017 | Complete | 1/233 | |||
| NCT02343159 | 2017 | Terminated | 1/27 | Angina; Sponsor Decision | ||
| NCT02097849 | 2017 | Complete | 0/38 | |||
| NCT02117050 | 2017 | Terminated | 0/0 | Low recruitment | ||
| NCT02217982 | 2017 | Terminated | 0/4 | Low recruitment | ||
| NCT02474082 | 2017 | Complete | 0/95 | |||
| NCT02241785 | 2017 | Terminated | 0/47 | Business Reasons | ||
| NCT02090413 | 2016 | Complete | 0/80 | |||
| NCT01568112 | 2016 | Complete | 0/43 | |||
| NCT00420212 | 2015 | Complete | 3/826 | |||
| NCT00451451 | 2015 | Complete | 1/703 | |||
| Melatonin | 49 | NCT02654314 | 2022 | Terminated | 0/136 | |
| NCT02386319 | 2021 | Complete | 0/16 | |||
| NCT03597529 | 2021 | Complete | 0/40 | |||
| NCT02344316 | 2021 | Complete | 0/13 | |||
| NCT02631148 | 2021 | Terminated | 0/12 | |||
| NCT04137627 | 2019 | Complete | 0/13 | |||
| NCT01700959 | 2018 | Complete | 9/66 | delayed sleep onset | ||
| NCT00925899 | 2017 | Complete | 0/34 | |||
| NCT01805089 | 2015 | Complete | 0/48 | |||
| NCT01355523 | 2014 | Terminated | 1/27 | Inclusion/finances | ||
| Quercetin | 109 | NCT02195232 | 2021 | Complete | 0/57 | |
| NCT02463357 | 2021 | Complete | 0/20 | |||
| NCT01722669 | 2020 | Complete | 0/30 | |||
| NCT01708278 | 2016 | Complete | 0/6 | |||
| NCT00913081 | 2015 | Complete | 0/17 | |||
| Resveratrol | 192 | NCT01354977 | 2022 | Complete | 0/12 | |
| NCT02523274 | 2022 | Complete | 0/20 | |||
| NCT04668274 | 2022 | Complete | 0/24 | |||
| NCT01321151 | 2021 | Complete | 0/6 | |||
| NCT02767869 | 2021 | Complete | 0/12 | |||
| NCT02114892 | 2020 | Complete | 0/12 | |||
| NCT03384329 | 2020 | Complete | 0/11 | |||
| NCT00920556 | 2019 | Terminated | 2/24 | At study directors discretion | ||
| NCT02095873 | 2017 | Complete | 0/32 | |||
| NCT02475564 | 2016 | Complete | 0/22 | |||
| NCT01504854 | 2016 | Complete | 1/64 | |||
| NCT01640197 | 2012 | Complete | 0/30 | |||
| RTA-408 | 2 | NCT02259231 | 2021 | Complete | 5/41 | |
| NCT02255422 | 2021 | Complete | 3/40 | |||
| Sulforaphane | 92 | NCT03126539 | 2022 | Terminated | 0/9 | Adminstrative |
| NCT03402230 | 2022 | Complete | 1/49 | |||
| NCT02810964 | 2021 | Complete | 1/32 | Placebo 3/32 | ||
| NCT02561481 | 2020 | Complete | 0/32 | |||
| NCT02909959 | 2020 | Complete | 0/24 | |||
| NCT02885025 | 2020 | Complete | 0/30 | |||
| NCT00621309 | 2019 | Complete | 0/29 | |||
| NCT02656420 | 2019 | Complete | 0/115 | |||
| NCT01474993 | 2018 | Complete | 0/26 | |||
| NCT00982319 | 2018 | Complete | 0/15 | |||
| NCT01437501 | 2018 | Complete | 0/148 | |||
| NCT01228084 | 2017 | Complete | 0/20 | |||
| NCT01335971 | 2017 | Complete | 1/29 | COPD exacerbation | ||
| NCT00843167 | 2017 | Complete | 0/27 | |||
| NCT01845220 | 2017 | Complete | 0/30 | |||
| NCT00946309 | 2016 | Complete | 0/21 | |||
| Ursodiol | 182 | NCT02748616 | 2022 | Complete | 0/2 | |
| NCT03226067 | 2022 | Complete | 0/74 | |||
| NCT03602560 | 2022 | Complete | 0/188 | |||
| NCT02955602 | 2022 | Complete | 2/108 | |||
| NCT01865812 | 2022 | Complete | 0/26 | |||
| NCT03633227 | 2022 | Terminated | 2/10 | Sponsor decision | ||
| NCT00059202 | 2021 | Terminated | 0/76 | Futility | ||
| NCT03394924 | 2021 | Complete | 0/59 | |||
| NCT02078882 | 2020 | Complete | 1/16 | |||
| NCT00706381 | 2020 | Complete | 0/29 | |||
| NCT03742973 | 2020 | Terminated | 0/0 | Low recruitment | ||
| NCT04053023 | 2020 | Complete | 0/19 | |||
| NCT02033876 | 2019 | Complete | 0/12 | |||
| NCT01904058 | 2019 | Complete | 1/20 | |||
| NCT03124108 | 2019 | Complete | 0/30 | |||
| NCT02244944 | 2018 | Terminated | 0/2 | Low recruitment | ||
| NCT00575042 | 2018 | Complete | 0/20 | |||
| NCT01097304 | 2017 | Complete | 6/36 | |||
| NCT01389973 | 2016 | Complete | 0/20 | |||
| NCT02111603 | 2016 | Complete | 0/12 | |||
| NCT00877604 | 2014 | Complete | 0/15 | |||
| NCT01249092 | 2013 | Complete | 0/20 | |||
| NCT00200343 | 2012 | Complete | 0/596 | |||
| NCT00550862 | 2012 | Complete | 1/41 | |||
| NCT00909753 | 2009 | Complete | NR | |||
| NCT00909610 | 2009 | Complete | NR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mathis, B.J.; Kato, H.; Hiramatsu, Y. Induction of Cardiac Pathology: Endogenous versus Exogenous Nrf2 Upregulation. Cells 2022, 11, 3855. https://doi.org/10.3390/cells11233855
Mathis BJ, Kato H, Hiramatsu Y. Induction of Cardiac Pathology: Endogenous versus Exogenous Nrf2 Upregulation. Cells. 2022; 11(23):3855. https://doi.org/10.3390/cells11233855
Chicago/Turabian StyleMathis, Bryan J., Hideyuki Kato, and Yuji Hiramatsu. 2022. "Induction of Cardiac Pathology: Endogenous versus Exogenous Nrf2 Upregulation" Cells 11, no. 23: 3855. https://doi.org/10.3390/cells11233855
APA StyleMathis, B. J., Kato, H., & Hiramatsu, Y. (2022). Induction of Cardiac Pathology: Endogenous versus Exogenous Nrf2 Upregulation. Cells, 11(23), 3855. https://doi.org/10.3390/cells11233855







