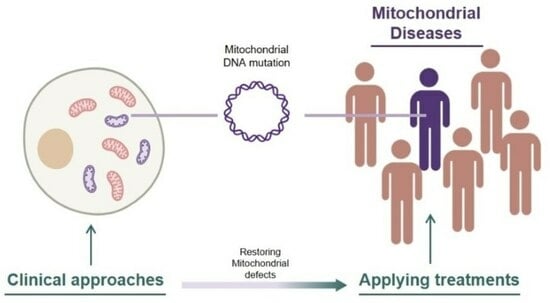
Clinical Approaches for Mitochondrial Diseases
Abstract
:1. Introduction
2. Features of Mitochondrial Disease
3. Types of Mitochondrial Disease
4. Clinical Approach with Treatments Involving Chemical Compounds
5. Clinical Approach Using Non-Chemical Treatments
6. Targeted Genome Editing
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Schapira, A.H. Mitochondrial disease. Lancet 2006, 368, 70–82. [Google Scholar] [CrossRef] [PubMed]
- Gorman, G.S.; Chinnery, P.F.; DiMauro, S.; Hirano, M.; Koga, Y.; McFarland, R.; Suomalainen, A.; Thorburn, D.R.; Zeviani, M.; Turnbull, D.M. Mitochondrial diseases. Nat. Rev. Dis. Primers 2016, 2, 16080. [Google Scholar] [CrossRef] [PubMed]
- Boengler, K.; Heusch, G.; Schulz, R. Nuclear-encoded mitochondrial proteins and their role in cardioprotection. Biochim. Biophys. Acta 2011, 1813, 1286–1294. [Google Scholar] [CrossRef]
- Monaghan, R.M.; Whitmarsh, A.J. Mitochondrial Proteins Moonlighting in the Nucleus. Trends Biochem. Sci. 2015, 40, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Lionaki, E.; Gkikas, I.; Tavernarakis, N. Differential Protein Distribution between the Nucleus and Mitochondria: Implications in Aging. Front. Genet. 2016, 7, 162. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.; Bankier, A.T.; Barrell, B.G.; de Bruijn, M.H.; Coulson, A.R.; Drouin, J.; Eperon, I.C.; Nierlich, D.P.; Roe, B.A.; Sanger, F.; et al. Sequence and organization of the human mitochondrial genome. Nature 1981, 290, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Khotina, V.A.; Vinokurov, A.Y.; Bagheri Ekta, M.; Sukhorukov, V.N.; Orekhov, A.N. Creation of Mitochondrial Disease Models Using Mitochondrial DNA Editing. Biomedicines 2023, 11, 532. [Google Scholar] [CrossRef]
- Taylor, R.W.; Turnbull, D.M. Mitochondrial DNA mutations in human disease. Nat. Rev. Genet. 2005, 6, 389–402. [Google Scholar] [CrossRef]
- Wong, L.-J.C. Diagnostic challenges of mitochondrial DNA disorders. Mitochondrion 2007, 7, 45–52. [Google Scholar] [CrossRef]
- Yang, M.; Xu, L.; Xu, C.; Cui, Y.; Jiang, S.; Dong, J.; Liao, L. The Mutations and Clinical Variability in Maternally Inherited Diabetes and Deafness: An Analysis of 161 Patients. Front. Endocrinol. 2021, 12, 728043. [Google Scholar] [CrossRef]
- Ying, Y.; Liang, Y.; Luo, X.; Wei, M. Case Report: Clinical and Genetic Characteristics of Pearson Syndrome in a Chinese Boy and 139 Patients. Front. Genet. 2022, 13, 802402. [Google Scholar] [CrossRef] [PubMed]
- Bi, C.; Wang, L.; Fan, Y.; Yuan, B.; Ramos-Mandujano, G.; Zhang, Y.; Alsolami, S.; Zhou, X.; Wang, J.; Shao, Y.; et al. Single-cell individual full-length mtDNA sequencing by iMiGseq uncovers unexpected heteroplasmy shifts in mtDNA editing. Nucleic Acids Res. 2023, 51, e48. [Google Scholar] [CrossRef]
- Thorburn, D.R. Mitochondrial disorders: Prevalence, myths and advances. J. Inherit. Metab. Dis. 2004, 27, 349–362. [Google Scholar] [CrossRef]
- Gorman, G.S.; Schaefer, A.M.; Ng, Y.; Gomez, N.; Blakely, E.L.; Alston, C.L.; Feeney, C.; Horvath, R.; Yu-Wai-Man, P.; Chinnery, P.F.; et al. Prevalence of nuclear and mitochondrial DNA mutations related to adult mitochondrial disease. Ann. Neurol. 2015, 77, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.S.; Belaramani, K.M.; Chan, C.K.; Chan, W.K.; Chan, W.L.; Chang, S.K.; Cheung, S.N.; Cheung, K.Y.; Cheung, Y.F.; Chong, S.J.; et al. Mitochondrial diseases in Hong Kong: Prevalence, clinical characteristics and genetic landscape. Orphanet J. Rare Dis. 2023, 18, 43. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liu, H.; Luo, S.; Lu, Z.; Chavez-Badiola, A.; Liu, Z.; Yang, M.; Merhi, Z.; Silber, S.J.; Munne, S.; et al. Live birth derived from oocyte spindle transfer to prevent mitochondrial disease. Reprod. Biomed. Online 2017, 34, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Mok, B.Y.; de Moraes, M.H.; Zeng, J.; Bosch, D.E.; Kotrys, A.V.; Raguram, A.; Hsu, F.; Radey, M.C.; Peterson, S.B.; Mootha, V.K.; et al. A bacterial cytidine deaminase toxin enables CRISPR-free mitochondrial base editing. Nature 2020, 583, 631–637. [Google Scholar] [CrossRef]
- Cho, S.I.; Lee, S.; Mok, Y.G.; Lim, K.; Lee, J.; Lee, J.M.; Chung, E.; Kim, J.S. Targeted A-to-G base editing in human mitochondrial DNA with programmable deaminases. Cell 2022, 185, 1764–1776.e12. [Google Scholar] [CrossRef]
- Yi, Z.; Zhang, X.; Tang, W.; Yu, Y.; Wei, X.; Zhang, X.; Wei, W. Strand-selective base editing of human mitochondrial DNA using mitoBEs. Nat. Biotechnol. 2023. [Google Scholar] [CrossRef]
- Giorgio, V.; Petronilli, V.; Ghelli, A.; Carelli, V.; Rugolo, M.; Lenaz, G.; Bernardi, P. The effects of idebenone on mitochondrial bioenergetics. Biochim. Biophys. Acta 2012, 1817, 363–369. [Google Scholar] [CrossRef]
- Jaber, S.M.; Ge, S.X.; Milstein, J.L.; VanRyzin, J.W.; Waddell, J.; Polster, B.M. Idebenone Has Distinct Effects on Mitochondrial Respiration in Cortical Astrocytes Compared to Cortical Neurons Due to Differential NQO1 Activity. J. Neurosci. 2020, 40, 4609–4619. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Shen, W.; Yu, G.; Jia, H.; Li, X.; Feng, Z.; Wang, Y.; Weber, P.; Wertz, K.; Sharman, E.; et al. Hydroxytyrosol promotes mitochondrial biogenesis and mitochondrial function in 3T3-L1 adipocytes. J. Nutr. Biochem. 2010, 21, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Sandoval-Acuna, C.; Ferreira, J.; Speisky, H. Polyphenols and mitochondria: An update on their increasingly emerging ROS-scavenging independent actions. Arch. Biochem. Biophys. 2014, 559, 75–90. [Google Scholar] [CrossRef]
- Duan, J.; Li, Y.; Gao, H.; Yang, D.; He, X.; Fang, Y.; Zhou, G. Phenolic compound ellagic acid inhibits mitochondrial respiration and tumor growth in lung cancer. Food Funct. 2020, 11, 6332–6339. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Yu, M.; Wu, Y.; Xia, T.; Wang, L.; Song, K.; Zhang, C.; Lu, K.; Rahimnejad, S. Hydroxytyrosol Promotes the Mitochondrial Function through Activating Mitophagy. Antioxidants 2022, 11, 893. [Google Scholar] [CrossRef]
- Herzig, S.; Shaw, R.J. AMPK: Guardian of metabolism and mitochondrial homeostasis. Nat. Rev. Mol. Cell Biol. 2018, 19, 121–135. [Google Scholar] [CrossRef]
- Wang, J.; Li, Z.; Gao, L.; Qi, Y.; Zhu, H.; Qin, X. The regulation effect of AMPK in immune related diseases. Sci. China Life Sci. 2018, 61, 523–533. [Google Scholar] [CrossRef]
- Pokhrel, R.H.; Acharya, S.; Ahn, J.-H.; Gu, Y.; Pandit, M.; Kim, J.-O.; Park, Y.-Y.; Kang, B.; Ko, H.-J.; Chang, J.-H. AMPK promotes antitumor immunity by downregulating PD-1 in regulatory T cells via the HMGCR/p38 signaling pathway. Mol. Cancer 2021, 20, 133. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, Z.; Hou, J.; Xiong, W.; Kim, H.; Chen, J.; Zheng, C.; Jiang, X.; Yoon, J.; Shen, J. Tumor Selective Metabolic Reprogramming as a Prospective PD-L1 Depression Strategy to Reactivate Immunotherapy. Adv. Mater. 2022, 34, e2206121. [Google Scholar] [CrossRef]
- Wang, S.; Zhou, Z.; Hu, R.; Dong, M.; Zhou, X.; Ren, S.; Zhang, Y.; Chen, C.; Huang, R.; Zhu, M.; et al. Metabolic Intervention Liposome Boosted Lung Cancer Radio-Immunotherapy via Hypoxia Amelioration and PD-L1 Restraint. Adv. Sci. 2023, 10, e2207608. [Google Scholar] [CrossRef]
- Zhao, B.; Qiang, L.; Joseph, J.; Kalyanaraman, B.; Viollet, B.; He, Y.-Y. Mitochondrial dysfunction activates the AMPK signaling and autophagy to promote cell survival. Genes Dis. 2016, 3, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Mikhail, A.I.; Ng, S.Y.; Mattina, S.R.; Ljubicic, V. AMPK is mitochondrial medicine for neuromuscular disorders. Trends Mol. Med. 2023, 29, 512–529. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Maraver, J.; Paz, M.V.; Cordero, M.D.; Bautista-Lorite, J.; Oropesa-Avila, M.; de la Mata, M.; Pavon, A.D.; de Lavera, I.; Alcocer-Gomez, E.; Galan, F.; et al. Critical role of AMP-activated protein kinase in the balance between mitophagy and mitochondrial biogenesis in MELAS disease. Biochim. Biophys. Acta 2015, 1852, 2535–2553. [Google Scholar] [CrossRef] [PubMed]
- Granatiero, V.; Giorgio, V.; Cali, T.; Patron, M.; Brini, M.; Bernardi, P.; Tiranti, V.; Zeviani, M.; Pallafacchina, G.; De Stefani, D.; et al. Reduced mitochondrial Ca(2+) transients stimulate autophagy in human fibroblasts carrying the 13514A>G mutation of the ND5 subunit of NADH dehydrogenase. Cell Death Differ. 2016, 23, 231–241. [Google Scholar] [CrossRef]
- Villanueva-Paz, M.; Povea-Cabello, S.; Villalon-Garcia, I.; Alvarez-Cordoba, M.; Suarez-Rivero, J.M.; Talaveron-Rey, M.; Jackson, S.; Falcon-Moya, R.; Rodriguez-Moreno, A.; Sanchez-Alcazar, J.A. Parkin-mediated mitophagy and autophagy flux disruption in cellular models of MERRF syndrome. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165726. [Google Scholar] [CrossRef]
- Shu, L.; Hu, C.; Xu, M.; Yu, J.; He, H.; Lin, J.; Sha, H.; Lu, B.; Engelender, S.; Guan, M.; et al. ATAD3B is a mitophagy receptor mediating clearance of oxidative stress-induced damaged mitochondrial DNA. EMBO J. 2021, 40, e106283. [Google Scholar] [CrossRef]
- Danese, A.; Patergnani, S.; Maresca, A.; Peron, C.; Raimondi, A.; Caporali, L.; Marchi, S.; La Morgia, C.; Del Dotto, V.; Zanna, C.; et al. Pathological mitophagy disrupts mitochondrial homeostasis in Leber’s hereditary optic neuropathy. Cell Rep. 2022, 40, 111124. [Google Scholar] [CrossRef]
- Zhang, J.; Merkle, H.; Hendrich, K.; Garwood, M.; From, A.H.; Ugurbil, K.; Bache, R.J. Bioenergetic abnormalities associated with severe left ventricular hypertrophy. J. Clin. Investig. 1993, 92, 993–1003. [Google Scholar] [CrossRef]
- Huss, J.M.; Kelly, D.P. Mitochondrial energy metabolism in heart failure: A question of balance. J. Clin. Investig. 2005, 115, 547–555. [Google Scholar] [CrossRef]
- Wu, F.; Zhang, J.; Beard, D.A. Experimentally observed phenomena on cardiac energetics in heart failure emerge from simulations of cardiac metabolism. Proc. Natl. Acad. Sci. USA 2009, 106, 7143–7148. [Google Scholar] [CrossRef]
- Wang, Z.; Ying, Z.; Bosy-Westphal, A.; Zhang, J.; Schautz, B.; Later, W.; Heymsfield, S.B.; Muller, M.J. Specific metabolic rates of major organs and tissues across adulthood: Evaluation by mechanistic model of resting energy expenditure. Am. J. Clin. Nutr. 2010, 92, 1369–1377. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.C.; Fan, W.; Procaccio, V. Mitochondrial energetics and therapeutics. Annu. Rev. Pathol. 2010, 5, 297–348. [Google Scholar] [CrossRef] [PubMed]
- Lotz, C.; Lin, A.J.; Black, C.M.; Zhang, J.; Lau, E.; Deng, N.; Wang, Y.; Zong, N.C.; Choi, J.H.; Xu, T.; et al. Characterization, design, and function of the mitochondrial proteome: From organs to organisms. J. Proteome Res. 2014, 13, 433–446. [Google Scholar] [CrossRef] [PubMed]
- Thome, T.; Coleman, M.D.; Ryan, T.E. Mitochondrial Bioenergetic and Proteomic Phenotyping Reveals Organ-Specific Consequences of Chronic Kidney Disease in Mice. Cells 2021, 10, 3282. [Google Scholar] [CrossRef]
- Faria-Pereira, A.; Morais, V.A. Synapses: The Brain’s Energy-Demanding Sites. Int. J. Mol. Sci. 2022, 23, 3627. [Google Scholar] [CrossRef]
- Trigo, D.; Avelar, C.; Fernandes, M.; Sa, J.; da Cruz, E.S.O. Mitochondria, energy, and metabolism in neuronal health and disease. FEBS Lett. 2022, 596, 1095–1110. [Google Scholar] [CrossRef]
- Jackson, M.J.; Schaefer, J.A.; Johnson, M.A.; Morris, A.A.; Turnbull, D.M.; Bindoff, L.A. Presentation and clinical investigation of mitochondrial respiratory chain disease. A study of 51 patients. Brain 1995, 118 Pt 2, 339–357. [Google Scholar] [CrossRef]
- Koenig, M.K. Presentation and diagnosis of mitochondrial disorders in children. Pediatr. Neurol. 2008, 38, 305–313. [Google Scholar] [CrossRef]
- Miao, J.; Qian, Q.; Zand, L. Long-Standing Hypokalemia and Lactic Acidosis as the Primary Presentation of Mitochondrial Myopathy. Kidney Int. Rep. 2020, 5, 742–745. [Google Scholar] [CrossRef]
- Chinnery, P.F.; Hudson, G. Mitochondrial genetics. Br. Med. Bull. 2013, 106, 135–159. [Google Scholar] [CrossRef]
- Stewart, J.B.; Chinnery, P.F. The dynamics of mitochondrial DNA heteroplasmy: Implications for human health and disease. Nat. Rev. Genet. 2015, 16, 530–542. [Google Scholar] [CrossRef] [PubMed]
- Bernardino Gomes, T.M.; Ng, Y.S.; Pickett, S.J.; Turnbull, D.M.; Vincent, A.E. Mitochondrial DNA disorders: From pathogenic variants to preventing transmission. Human Mol. Genet. 2021, 30, R245–R253. [Google Scholar] [CrossRef] [PubMed]
- Chuenkongkaew, W.L.; Chinkulkitnivat, B.; Lertrit, P.; Chirapapaisan, N.; Kaewsutthi, S.; Suktitipat, B.; Mitrpant, C. Clinical expression and mitochondrial deoxyribonucleic acid study in twins with 14484 Leber’s hereditary optic neuropathy: A case report. World J. Clin. Cases 2022, 10, 6944–6953. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Park, S.; Hwang, J.-M. Visual Prognosis of Leber’s Hereditary Optic Neuropathy with T14484C Mitochondrial DNA Mutation in Koreans. J. Korean Ophthalmol. Soc. 2012, 53, 151. [Google Scholar] [CrossRef]
- Iorga, R.E.; Mihailovici, R.; Ozturk, M.R.; Costin, D. Leber’s hereditary optic neuropathy—Case report. Rom. J. Ophthalmol. 2018, 62, 64–71. [Google Scholar] [CrossRef]
- Miao, Q.M.; Cheng, Y.F.; Zheng, H.M.; Yuan, J.J.; Chen, C.Z. Photoreceptor changes in Leber hereditary optic neuropathy with m.G11778A mutation. Int. J. Ophthalmol. 2023, 16, 928–932. [Google Scholar] [CrossRef]
- Chandra, S.R.; Issac, T.G.; Gayathri, N.; Gupta, N.; Abbas, M.M. A typical case of myoclonic epilepsy with ragged red fibers (MERRF) and the lessons learned. J. Postgrad. Med. 2015, 61, 200–202. [Google Scholar] [CrossRef]
- Xu, H.L.; Lian, Y.J.; Chen, X. Brain atrophy in a patient with mitochondrial DNA G8363A mutation. Chin. Med. J. 2019, 132, 2141–2142. [Google Scholar] [CrossRef]
- Liu, X.Q.; Shen, S.Q.; Yang, G.C.; Liu, Q. Mitochondrial A3243G mutation causes mitochondrial encephalomyopathy in a Chinese patient: Case report. Medicine 2019, 98, e15534. [Google Scholar] [CrossRef]
- Windpessl, M.; Muller, P.; Wallner, M. Truth is a daughter of time: A case of MELAS diagnosed 25 years after initial manifestation. Oxf. Med. Case Rep. 2014, 2014, 24–25. [Google Scholar] [CrossRef]
- Martens, E.; Demeestere, J.; Verhaaren, B. Microhemorrhages in MELAS Lesions: A Case Report. J. Belg. Soc. Radiol. 2022, 106, 88. [Google Scholar] [CrossRef] [PubMed]
- Diao, S.P.; Chen, S.F.; Liu, A.Q.; Zhou, Z.H.; Peng, Z.X.; Hong, M.F. Elderly onset of MELAS in a male: A case report. Front. Neurol. 2022, 13, 1018529. [Google Scholar] [CrossRef] [PubMed]
- Kanaumi, T.; Hirose, S.; Goto, Y.; Naitou, E.; Mitsudome, A. An infant with a mitochondrial A3243G mutation demonstrating the MELAS phenotype. Pediatr. Neurol. 2006, 34, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.; Dubey, S.; Bhuin, S.; Lahiri, D.; Ray, B.K.; Finsterer, J. MELAS with multiple stroke-like episodes due to the variant m.13513G>A in MT-ND5. Clin. Case Rep. 2022, 10, e05361. [Google Scholar] [CrossRef]
- Tanaka, K.; Ueno, T.; Yoshida, M.; Shimizu, Y.; Ogawa, T.; Nishisaka, T.; Kurashige, T.; Masaki, T. Chronic kidney disease caused by maternally inherited diabetes and deafness: A case report. CEN Case Rep. 2021, 10, 220–225. [Google Scholar] [CrossRef]
- Li, M.C.H.; Symmonds, M.; Pretorius, P.M.; Sheerin, F.; Nithi, K.; Hofer, M.; Poulton, J.; Sen, A. Very late-onset mitochondrial cytopathy featuring epilepsia partialis continua and bilateral deafness: A case report. Seizure 2020, 76, 153–155. [Google Scholar] [CrossRef]
- Shoeleh, C.; Donato, U.M.; Galligan, A.; Vitko, J. A Case Report on Pearson Syndrome With Emphasis on Genetic Screening in Patients Presenting With Sideroblastic Anemia and Lactic Acidosis. Cureus 2023, 15, e33963. [Google Scholar] [CrossRef]
- Zhu, Q.; Chen, C.; Yao, J. Kearns-Sayre syndrome with a novel large-scale deletion: A case report. BMC Ophthalmol. 2022, 22, 35. [Google Scholar] [CrossRef]
- Grigalioniene, K.; Burnyte, B.; Balkeliene, D.; Ambrozaityte, L.; Utkus, A. Kearns-Sayre syndrome case. Novel 5,9 kb mtDNA deletion. Mol. Genet. Genom. Med. 2023, 11, e2059. [Google Scholar] [CrossRef]
- Sano, M.; Shimada, T.; Sakurai, A.; Goto, Y.-i.; Tsunemi, T.; Hattori, N. A case of chronic progressive external ophthalmoplegia presenting with central neurogenic hyperventilation. Brain Disord. 2022, 8, 100057. [Google Scholar] [CrossRef]
- Sirbu, C.A.; Sîrbu, O.-M.; Sandu, A.-M. Chronic progressive external ophtalmoplegia (CPEO)—Case presentation. Rom. J. Neurol./Rev. Romana Neurol. 2014, 13, 150–152. [Google Scholar] [CrossRef]
- Eliyan, Y.; Rezania, K.; Gomez, C.M.; Seibert, K. Pontine stroke in a patient with Chronic Progressive External Ophthalmoplegia (CPEO): A case report. BMC Neurol. 2023, 23, 231. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Gomez, C.; Camara, Y.; Hirano, M.; Marti, R. 232nd ENMC international workshop: Recommendations for treatment of mitochondrial DNA maintenance disorders. 16–18 June 2017, Heemskerk, The Netherlands. Neuromuscul. Disord. 2022, 32, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.M.; Xin, C.J.; Wang, G.L.; Wu, X.M. Late-onset Leigh syndrome without delayed development in China: A case report. World J. Clin. Cases 2021, 9, 7133–7138. [Google Scholar] [CrossRef] [PubMed]
- Maruo, Y.; Ueda, Y.; Murayama, K.; Takeda, A. A case report of Leigh syndrome diagnosed by endomyocardial biopsy. Eur. Heart J. Case Rep. 2021, 5, ytaa582. [Google Scholar] [CrossRef]
- Legro, N.R.; Kumar, A.; Aliu, E. Case report of atypical Leigh syndrome in an adolescent male with novel biallelic variants in NDUFAF5 and review of the natural history of NDUFAF5-related disorders. Am. J. Med. Genet. A 2022, 188, 896–899. [Google Scholar] [CrossRef]
- Takeda, A.; Ueki, M.; Abe, J.; Maeta, K.; Horiguchi, T.; Yamazawa, H.; Izumi, G.; Chida-Nagai, A.; Sasaki, D.; Tsujioka, T.; et al. A case of infantile Barth syndrome with severe heart failure: Importance of splicing variants in the TAZ gene. Mol. Genet. Genom. Med. 2023, 11, e2190. [Google Scholar] [CrossRef]
- Amini, O.; Lakziyan, R.; Abavisani, M.; Sarchahi, Z. The cardiomyopathy of Friedreich’s ataxia common in a family: A case report. Ann. Med. Surg. 2021, 66, 102408. [Google Scholar] [CrossRef] [PubMed]
- Damasio, J.; Sardoeira, A.; Araujo, M.; Carvalho, I.; Sequeiros, J.; Barros, J. Rare occurrence of severe blindness and deafness in Friedreich ataxia: A case report. Cerebellum Ataxias 2021, 8, 17. [Google Scholar] [CrossRef]
- Yu-Wai-Man, P.; Chinnery, P.F. Leber Hereditary Optic Neuropathy; Adam, M.P., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; GeneReviews®: Seattle, WA, USA, 1993. [Google Scholar]
- Finsterer, J.; Zarrouk-Mahjoub, S. Leber’s hereditary optic neuropathy is multiorgan not mono-organ. Clin. Ophthalmol. 2016, 10, 2187–2190. [Google Scholar] [CrossRef]
- Esmaeil, A.; Ali, A.; Behbehani, R. Leber’s hereditary optic neuropathy: Update on current diagnosis and treatment. Front. Ophthalmol. 2023, 2, 1077395. [Google Scholar] [CrossRef]
- Shemesh, A.; Sood, G.; Margolin, E. Leber Hereditary Optic Neuropathy (LHON); StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Wong, A.; Cortopassi, G. 14—Mitochondrial Genetic Diseases. In Neurobiology of Disease; Gilman, S., Ed.; Academic Press: Burlington, MA, USA, 2007; pp. 157–161. [Google Scholar]
- Jacobi, F.K.; Leo-Kottler, B.; Mittelviefhaus, K.; Zrenner, E.; Meyer, J.; Pusch, C.M.; Wissinger, B. Segregation patterns and heteroplasmy prevalence in Leber’s hereditary optic neuropathy. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1208–1214. [Google Scholar]
- Dai, Y.; Wang, C.; Nie, Z.; Han, J.; Chen, T.; Zhao, X.; Ai, C.; Ji, Y.; Gao, T.; Jiang, P. Mutation analysis of Leber’s hereditary optic neuropathy using a multi-gene panel. Biomed. Rep. 2018, 8, 51–58. [Google Scholar] [CrossRef]
- Bianco, A.; Valletti, A.; Longo, G.; Bisceglia, L.; Montoya, J.; Emperador, S.; Guerriero, S.; Petruzzella, V. Mitochondrial DNA copy number in affected and unaffected LHON mutation carriers. BMC Res. Notes 2018, 11, 911. [Google Scholar] [CrossRef] [PubMed]
- Piotrowska-Nowak, A.; Krawczynski, M.R.; Kosior-Jarecka, E.; Ambroziak, A.M.; Korwin, M.; Oldak, M.; Tonska, K.; Bartnik, E. Mitochondrial genome variation in male LHON patients with the m.11778G > A mutation. Metab. Brain Dis. 2020, 35, 1317–1327. [Google Scholar] [CrossRef] [PubMed]
- Giordano, C.; Iommarini, L.; Giordano, L.; Maresca, A.; Pisano, A.; Valentino, M.L.; Caporali, L.; Liguori, R.; Deceglie, S.; Roberti, M.; et al. Efficient mitochondrial biogenesis drives incomplete penetrance in Leber’s hereditary optic neuropathy. Brain 2014, 137, 335–353. [Google Scholar] [CrossRef]
- Giordano, L.; Deceglie, S.; d’Adamo, P.; Valentino, M.L.; La Morgia, C.; Fracasso, F.; Roberti, M.; Cappellari, M.; Petrosillo, G.; Ciaravolo, S.; et al. Cigarette toxicity triggers Leber’s hereditary optic neuropathy by affecting mtDNA copy number, oxidative phosphorylation and ROS detoxification pathways. Cell Death Dis. 2015, 6, e2021. [Google Scholar] [CrossRef]
- Dombi, E.; Diot, A.; Morten, K.; Carver, J.; Lodge, T.; Fratter, C.; Ng, Y.S.; Liao, C.; Muir, R.; Blakely, E.L.; et al. The m.13051G>A mitochondrial DNA mutation results in variable neurology and activated mitophagy. Neurology 2016, 86, 1921–1923. [Google Scholar] [CrossRef]
- Moura-Coelho, N.; Pinto Proenca, R.; Tavares Ferreira, J.; Cunha, J.P. Late-onset Leber’s hereditary optic neuropathy: The role of environmental factors in hereditary diseases. BMJ Case Rep. 2019, 12, e227977. [Google Scholar] [CrossRef]
- Finsterer, J. More likely than through head trauma: Is LHON triggered by mitochondrion-toxic drugs or oxidative stress. Doc. Ophthalmol. 2021, 142, 395–396. [Google Scholar] [CrossRef]
- Vela-Sebastian, A.; Lopez-Gallardo, E.; Emperador, S.; Hernandez-Ainsa, C.; Pacheu-Grau, D.; Blanco, I.; Ros, A.; Pascual-Benito, E.; Rabaneda-Lombarte, N.; Presas-Rodriguez, S.; et al. Toxic and nutritional factors trigger Leber hereditary optic neuropathy due to a mitochondrial tRNA mutation. Clin. Genet. 2022, 102, 339–344. [Google Scholar] [CrossRef]
- Riordan-Eva, P.; Harding, A.E. Leber’s hereditary optic neuropathy: The clinical relevance of different mitochondrial DNA mutations. J. Med. Genet. 1995, 32, 81–87. [Google Scholar] [CrossRef]
- Hameed, S.; Tadi, P. Myoclonic Epilepsy and Ragged Red Fibers; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Shoffner, J.M.; Lott, M.T.; Lezza, A.M.; Seibel, P.; Ballinger, S.W.; Wallace, D.C. Myoclonic epilepsy and ragged-red fiber disease (MERRF) is associated with a mitochondrial DNA tRNA(Lys) mutation. Cell 1990, 61, 931–937. [Google Scholar] [CrossRef] [PubMed]
- Hammans, S.R.; Sweeney, M.G.; Brockington, M.; Lennox, G.G.; Lawton, N.F.; Kennedy, C.R.; Morgan-Hughes, J.A.; Harding, A.E. The mitochondrial DNA transfer RNA(Lys)A-->G(8344) mutation and the syndrome of myoclonic epilepsy with ragged red fibres (MERRF). Relationship of clinical phenotype to proportion of mutant mitochondrial DNA. Brain 1993, 116 Pt 3, 617–632. [Google Scholar] [CrossRef] [PubMed]
- Velez-Bartolomei, F.; Lee, C.; Enns, G. Merrf; Adam, M.P., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; GeneReviews®: Seattle, WA, USA, 1993. [Google Scholar]
- Ripolone, M.; Zanotti, S.; Napoli, L.; Ronchi, D.; Ciscato, P.; Comi, G.P.; Moggio, M.; Sciacco, M. MERRF Mutation A8344G in a Four-Generation Family without Central Nervous System Involvement: Clinical and Molecular Characterization. J. Pers. Med. 2023, 13, 147. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-T.; Tay, H.-Y.; Yang, J.-T.; Liao, H.-H.; Ma, Y.-S.; Wei, Y.-H. Mitochondrial impairment and synaptic dysfunction are associated with neurological defects in iPSCs-derived cortical neurons of MERRF patients. J. Biomed. Sci. 2023, 30, 70. [Google Scholar] [CrossRef]
- Goto, Y.; Tsugane, K.; Tanabe, Y.; Nonaka, I.; Horai, S. A new point mutation at nucleotide pair 3291 of the mitochondrial tRNA(Leu(UUR)) gene in a patient with mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes (MELAS). Biochem. Biophys. Res. Commun. 1994, 202, 1624–1630. [Google Scholar] [CrossRef]
- Nishigaki, Y.; Tadesse, S.; Bonilla, E.; Shungu, D.; Hersh, S.; Keats, B.J.; Berlin, C.I.; Goldberg, M.F.; Vockley, J.; DiMauro, S.; et al. A novel mitochondrial tRNA(Leu(UUR)) mutation in a patient with features of MERRF and Kearns-Sayre syndrome. Neuromuscul. Disord. 2003, 13, 334–340. [Google Scholar] [CrossRef]
- Chomyn, A.; Meola, G.; Bresolin, N.; Lai, S.T.; Scarlato, G.; Attardi, G. In vitro genetic transfer of protein synthesis and respiration defects to mitochondrial DNA-less cells with myopathy-patient mitochondria. Mol. Cell. Biol. 1991, 11, 2236–2244. [Google Scholar] [CrossRef]
- Chomyn, A.; Lai, S.T.; Shakeley, R.; Bresolin, N.; Scarlato, G.; Attardi, G. Platelet-mediated transformation of mtDNA-less human cells: Analysis of phenotypic variability among clones from normal individuals—And complementation behavior of the tRNALys mutation causing myoclonic epilepsy and ragged red fibers. Am. J. Hum. Genet. 1994, 54, 966–974. [Google Scholar]
- Yoneda, M.; Chomyn, A.; Martinuzzi, A.; Hurko, O.; Attardi, G. Marked replicative advantage of human mtDNA carrying a point mutation that causes the MELAS encephalomyopathy. Proc. Natl. Acad. Sci. USA 1992, 89, 11164–11168. [Google Scholar] [CrossRef] [PubMed]
- Chomyn, A.; Enriquez, J.A.; Micol, V.; Fernandez-Silva, P.; Attardi, G. The mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episode syndrome-associated human mitochondrial tRNALeu(UUR) mutation causes aminoacylation deficiency and concomitant reduced association of mRNA with ribosomes. J. Biol. Chem. 2000, 275, 19198–19209. [Google Scholar] [CrossRef] [PubMed]
- Janssen, G.M.; Hensbergen, P.J.; van Bussel, F.J.; Balog, C.I.; Maassen, J.A.; Deelder, A.M.; Raap, A.K. The A3243G tRNALeu(UUR) mutation induces mitochondrial dysfunction and variable disease expression without dominant negative acting translational defects in complex IV subunits at UUR codons. Hum. Mol. Genet. 2007, 16, 2472–2481. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Guan, M.X. Human mitochondrial leucyl-tRNA synthetase corrects mitochondrial dysfunctions due to the tRNALeu(UUR) A3243G mutation, associated with mitochondrial encephalomyopathy, lactic acidosis, and stroke-like symptoms and diabetes. Mol. Cell. Biol. 2010, 30, 2147–2154. [Google Scholar] [CrossRef]
- Goldstein, A.; Servidei, S. Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-Like Episodes (MELAS). In Diagnosis and Management of Mitochondrial Disorders; Mancuso, M., Klopstock, T., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 81–100. [Google Scholar]
- Hirano, M.; Ricci, E.; Koenigsberger, M.R.; Defendini, R.; Pavlakis, S.G.; DeVivo, D.C.; DiMauro, S.; Rowland, L.P. Melas: An original case and clinical criteria for diagnosis. Neuromuscul. Disord. 1992, 2, 125–135. [Google Scholar] [CrossRef]
- El-Hattab, A.W.; Adesina, A.M.; Jones, J.; Scaglia, F. MELAS syndrome: Clinical manifestations, pathogenesis, and treatment options. Mol. Genet. Metab. 2015, 116, 4–12. [Google Scholar] [CrossRef]
- Aurangzeb, S.; Vale, T.; Tofaris, G.; Poulton, J.; Turner, M.R. Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS) in the older adult. Pract. Neurol. 2014, 14, 432–436. [Google Scholar] [CrossRef]
- Sunde, K.; Blackburn, P.R.; Cheema, A.; Gass, J.; Jackson, J.; Macklin, S.; Atwal, P.S. Case report: 5 year follow-up of adult late-onset mitochondrial encephalomyopathy with lactic acid and stroke-like episodes (MELAS). Mol. Genet. Metab. Rep. 2016, 9, 94–97. [Google Scholar] [CrossRef]
- Mukai, M.; Nagata, E.; Mizuma, A.; Yamano, M.; Sugaya, K.; Nishino, I.; Goto, Y.I.; Takizawa, S. Adult-onset Mitochondrial Myopathy, Encephalopathy, Lactic Acidosis, and Stroke (MELAS)-like Encephalopathy Diagnosed Based on the Complete Sequencing of Mitochondrial DNA Extracted from Biopsied Muscle without any Myopathic Changes. Intern. Med. 2017, 56, 95–99. [Google Scholar] [CrossRef]
- Yang, F.; Peng, S.; Peng, Q. Diagnosis of adult-onset MELAS with suspected recurrent strokes: A case report. Exp. Ther. Med. 2022, 24, 466. [Google Scholar] [CrossRef]
- Gebhart, S.S.; Shoffner, J.M.; Koontz, D.; Kaufman, A.; Wallace, D. Insulin resistance associated with maternally inherited diabetes and deafness. Metabolism 1996, 45, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Guillausseau, P.J.; Massin, P.; Dubois-LaForgue, D.; Timsit, J.; Virally, M.; Gin, H.; Bertin, E.; Blickle, J.F.; Bouhanick, B.; Cahen, J.; et al. Maternally inherited diabetes and deafness: A multicenter study. Ann. Intern. Med. 2001, 134, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S.; Oka, Y.; Kadowaki, T.; Kanatsuka, A.; Kuzuya, T.; Kobayashi, M.; Sanke, T.; Seino, Y.; Nanjo, K. Clinical features of diabetes mellitus with the mitochondrial DNA 3243 (A-G) mutation in Japanese: Maternal inheritance and mitochondria-related complications. Diabetes Res. Clin. Pract. 2003, 59, 207–217. [Google Scholar] [CrossRef] [PubMed]
- de Wit, H.M.; Westeneng, H.J.; van Engelen, B.G.; Mudde, A.H. MIDD or MELAS: That’s not the question MIDD evolving into MELAS: A severe phenotype of the m.3243A>G mutation due to paternal co-inheritance of type 2 diabetes and a high heteroplasmy level. Neth. J. Med. 2012, 70, 460–462. [Google Scholar] [PubMed]
- Goel, H.; Szczepanczyk, K.; Mirza, F.S. Late-Onset Melas with Midd: An Uncommon Age of Presentation. AACE Clin. Case Rep. 2018, 4, 228–231. [Google Scholar] [CrossRef]
- Bukhari, K.; Pennant, M. Mitochondrial Diabetes: The Clinical Spectrum of MIDD and MELAS in Association With the A3243G Mutation. J. Endocr. Soc. 2021, 5, A392–A393. [Google Scholar] [CrossRef]
- Rahman, S.; Blok, R.B.; Dahl, H.H.; Danks, D.M.; Kirby, D.M.; Chow, C.W.; Christodoulou, J.; Thorburn, D.R. Leigh syndrome: Clinical features and biochemical and DNA abnormalities. Ann. Neurol. 1996, 39, 343–351. [Google Scholar] [CrossRef]
- Iwata, R.; Casimir, P.; Vanderhaeghen, P. Mitochondrial dynamics in postmitotic cells regulate neurogenesis. Science 2020, 369, 858–862. [Google Scholar] [CrossRef]
- Inak, G.; Rybak-Wolf, A.; Lisowski, P.; Pentimalli, T.M.; Juttner, R.; Glazar, P.; Uppal, K.; Bottani, E.; Brunetti, D.; Secker, C.; et al. Defective metabolic programming impairs early neuronal morphogenesis in neural cultures and an organoid model of Leigh syndrome. Nat. Commun. 2021, 12, 1929. [Google Scholar] [CrossRef]
- Lake, N.J.; Compton, A.G.; Rahman, S.; Thorburn, D.R. Leigh syndrome: One disorder, more than 75 monogenic causes. Ann. Neurol. 2016, 79, 190–203. [Google Scholar] [CrossRef]
- Lee, J.S.; Yoo, T.; Lee, M.; Lee, Y.; Jeon, E.; Kim, S.Y.; Lim, B.C.; Kim, K.J.; Choi, M.; Chae, J.H. Genetic heterogeneity in Leigh syndrome: Highlighting treatable and novel genetic causes. Clin. Genet. 2020, 97, 586–594. [Google Scholar] [CrossRef] [PubMed]
- Sofou, K.; de Coo, I.F.M.; Ostergaard, E.; Isohanni, P.; Naess, K.; De Meirleir, L.; Tzoulis, C.; Uusimaa, J.; Lonnqvist, T.; Bindoff, L.A.; et al. Phenotype-genotype correlations in Leigh syndrome: New insights from a multicentre study of 96 patients. J. Med. Genet. 2018, 55, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Ganetzky, R.D.; Stendel, C.; McCormick, E.M.; Zolkipli-Cunningham, Z.; Goldstein, A.C.; Klopstock, T.; Falk, M.J. MT-ATP6 mitochondrial disease variants: Phenotypic and biochemical features analysis in 218 published cases and cohort of 14 new cases. Hum. Mutat. 2019, 40, 499–515. [Google Scholar] [CrossRef]
- Baertling, F.; Rodenburg, R.J.; Schaper, J.; Smeitink, J.A.; Koopman, W.J.; Mayatepek, E.; Morava, E.; Distelmaier, F. A guide to diagnosis and treatment of Leigh syndrome. J. Neurol. Neurosurg. Psychiatry 2014, 85, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Sakushima, K.; Tsuji-Akimoto, S.; Niino, M.; Saitoh, S.; Yabe, I.; Sasaki, H. Adult Leigh disease without failure to thrive. Neurologist 2011, 17, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Jabeen, S.A.; Sandeep, G.; Mridula, K.R.; Meena, A.K.; Borgohain, R.; Sundaram, C. Adult-onset Leigh’s disease: A rare entity. Ann. Indian Acad. Neurol. 2016, 19, 140–142. [Google Scholar] [CrossRef]
- Holt, I.J.; Harding, A.E.; Morgan-Hughes, J.A. Deletions of muscle mitochondrial DNA in patients with mitochondrial myopathies. Nature 1988, 331, 717–719. [Google Scholar] [CrossRef]
- Chinnery, P.F.; DiMauro, S.; Shanske, S.; Schon, E.A.; Zeviani, M.; Mariotti, C.; Carrara, F.; Lombes, A.; Laforet, P.; Ogier, H.; et al. Risk of developing a mitochondrial DNA deletion disorder. Lancet 2004, 364, 592–596. [Google Scholar] [CrossRef]
- Wei, W.; Chinnery, P.F. Inheritance of mitochondrial DNA in humans: Implications for rare and common diseases. J. Intern. Med. 2020, 287, 634–644. [Google Scholar] [CrossRef]
- Krishnan, K.J.; Reeve, A.K.; Samuels, D.C.; Chinnery, P.F.; Blackwood, J.K.; Taylor, R.W.; Wanrooij, S.; Spelbrink, J.N.; Lightowlers, R.N.; Turnbull, D.M. What causes mitochondrial DNA deletions in human cells? Nat. Genet. 2008, 40, 275–279. [Google Scholar] [CrossRef]
- Nissanka, N.; Minczuk, M.; Moraes, C.T. Mechanisms of Mitochondrial DNA Deletion Formation. Trends Genet. 2019, 35, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Shoffner, J.M.; Lott, M.T.; Voljavec, A.S.; Soueidan, S.A.; Costigan, D.A.; Wallace, D.C. Spontaneous Kearns-Sayre/chronic external ophthalmoplegia plus syndrome associated with a mitochondrial DNA deletion: A slip-replication model and metabolic therapy. Proc. Natl. Acad. Sci. USA 1989, 86, 7952–7956. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; He, J.; Huang, Y.; Zhao, W. The generation of mitochondrial DNA large-scale deletions in human cells. J. Human Genet. 2011, 56, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.F.; Lee, H.J.; Chi, C.S.; Tsai, C.R.; Chang, T.K.; Wang, C.J. The neurological evolution of Pearson syndrome: Case report and literature review. Eur. J. Paediatr. Neurol. 2007, 11, 208–214. [Google Scholar] [CrossRef]
- Wild, K.T.; Goldstein, A.C.; Muraresku, C.; Ganetzky, R.D. Broadening the phenotypic spectrum of Pearson syndrome: Five new cases and a review of the literature. Am. J. Med. Genet. A 2020, 182, 365–373. [Google Scholar] [CrossRef]
- Horga, A.; Pitceathly, R.D.; Blake, J.C.; Woodward, C.E.; Zapater, P.; Fratter, C.; Mudanohwo, E.E.; Plant, G.T.; Houlden, H.; Sweeney, M.G.; et al. Peripheral neuropathy predicts nuclear gene defect in patients with mitochondrial ophthalmoplegia. Brain 2014, 137, 3200–3212. [Google Scholar] [CrossRef]
- Karpati, G.; Hilton-Jones, D.; Griggs, R.C. Disorders of Voluntary Muscle; Cambridge University Press: Cambridge, UK, 2001. [Google Scholar]
- van Everdingen, J.A.M.; de Faber, J.-T. Chapter 109—Chronic Progressive External Ophthalmoplegia (CPEO) 359.1 (Abiotrophic Ophthalmoplegia, CPEO with Ragged Red Fibres, Oculocraniosomatic Neuromuscular Disease, Ocular Myopathy, Olson’s Disease, Kearns–Sayre–Daroff Syndrome, Kearns–Sayre Syndrome, Progressive External Ophthalmoplegia Plus). In Roy and Fraunfelder’s Current Ocular Therapy, 6th ed.; Roy, F.H., Fraunfelder, F.W., Fraunfelder, F.T., Tindall, R., Jensvold, B., Eds.; W.B. Saunders: Edinburgh, Scotland, 2008; pp. 207–210. [Google Scholar]
- Lenaz, G.; Fato, R.; Formiggini, G.; Genova, M.L. The role of Coenzyme Q in mitochondrial electron transport. Mitochondrion 2007, 7, S8–S33. [Google Scholar] [CrossRef]
- Ernster, L.; Dallner, G. Biochemical, physiological and medical aspects of ubiquinone function. Biochim. Biophys. Acta 1995, 1271, 195–204. [Google Scholar] [CrossRef]
- Bentinger, M.; Brismar, K.; Dallner, G. The antioxidant role of coenzyme Q. Mitochondrion 2007, 7, S41–S50. [Google Scholar] [CrossRef]
- Mordente, A.; Martorana, G.E.; Minotti, G.; Giardina, B. Antioxidant properties of 2,3-dimethoxy-5-methyl-6-(10-hydroxydecyl)-1,4-benzoquinone (idebenone). Chem. Res. Toxicol. 1998, 11, 54–63. [Google Scholar] [CrossRef]
- Haefeli, R.H.; Erb, M.; Gemperli, A.C.; Robay, D.; Courdier Fruh, I.; Anklin, C.; Dallmann, R.; Gueven, N. NQO1-dependent redox cycling of idebenone: Effects on cellular redox potential and energy levels. PLoS ONE 2011, 6, e17963. [Google Scholar] [CrossRef] [PubMed]
- Erb, M.; Hoffmann-Enger, B.; Deppe, H.; Soeberdt, M.; Haefeli, R.H.; Rummey, C.; Feurer, A.; Gueven, N. Features of idebenone and related short-chain quinones that rescue ATP levels under conditions of impaired mitochondrial complex I. PLoS ONE 2012, 7, e36153. [Google Scholar] [CrossRef]
- Lyseng-Williamson, K.A. Idebenone: A Review in Leber’s Hereditary Optic Neuropathy. Drugs 2016, 76, 805–813. [Google Scholar] [CrossRef]
- Riederer, P.; Sofic, E.; Rausch, W.D.; Schmidt, B.; Reynolds, G.P.; Jellinger, K.; Youdim, M.B. Transition metals, ferritin, glutathione, and ascorbic acid in parkinsonian brains. J. Neurochem. 1989, 52, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Blankenberg, F.G.; Kinsman, S.L.; Cohen, B.H.; Goris, M.L.; Spicer, K.M.; Perlman, S.L.; Krane, E.J.; Kheifets, V.; Thoolen, M.; Miller, G.; et al. Brain uptake of Tc99m-HMPAO correlates with clinical response to the novel redox modulating agent EPI-743 in patients with mitochondrial disease. Mol. Genet. Metab. 2012, 107, 690–699. [Google Scholar] [CrossRef] [PubMed]
- Pastore, A.; Petrillo, S.; Tozzi, G.; Carrozzo, R.; Martinelli, D.; Dionisi-Vici, C.; Di Giovamberardino, G.; Ceravolo, F.; Klein, M.B.; Miller, G.; et al. Glutathione: A redox signature in monitoring EPI-743 therapy in children with mitochondrial encephalomyopathies. Mol. Genet. Metab. 2013, 109, 208–214. [Google Scholar] [CrossRef]
- Canto, C.; Houtkooper, R.H.; Pirinen, E.; Youn, D.Y.; Oosterveer, M.H.; Cen, Y.; Fernandez-Marcos, P.J.; Yamamoto, H.; Andreux, P.A.; Cettour-Rose, P.; et al. The NAD(+) precursor nicotinamide riboside enhances oxidative metabolism and protects against high-fat diet-induced obesity. Cell Metab. 2012, 15, 838–847. [Google Scholar] [CrossRef]
- Canto, C.; Menzies, K.J.; Auwerx, J. NAD(+) Metabolism and the Control of Energy Homeostasis: A Balancing Act between Mitochondria and the Nucleus. Cell Metab. 2015, 22, 31–53. [Google Scholar] [CrossRef]
- Zhang, H.; Ryu, D.; Wu, Y.; Gariani, K.; Wang, X.; Luan, P.; D’Amico, D.; Ropelle, E.R.; Lutolf, M.P.; Aebersold, R.; et al. NAD(+) repletion improves mitochondrial and stem cell function and enhances life span in mice. Science 2016, 352, 1436–1443. [Google Scholar] [CrossRef]
- Trammell, S.A.; Weidemann, B.J.; Chadda, A.; Yorek, M.S.; Holmes, A.; Coppey, L.J.; Obrosov, A.; Kardon, R.H.; Yorek, M.A.; Brenner, C. Nicotinamide Riboside Opposes Type 2 Diabetes and Neuropathy in Mice. Sci. Rep. 2016, 6, 26933. [Google Scholar] [CrossRef]
- Seo, K.S.; Kim, J.H.; Min, K.N.; Moon, J.A.; Roh, T.C.; Lee, M.J.; Lee, K.W.; Min, J.E.; Lee, Y.M. KL1333, a Novel NAD(+) Modulator, Improves Energy Metabolism and Mitochondrial Dysfunction in MELAS Fibroblasts. Front. Neurol. 2018, 9, 552. [Google Scholar] [CrossRef] [PubMed]
- Beyrath, J.; Pellegrini, M.; Renkema, H.; Houben, L.; Pecheritsyna, S.; van Zandvoort, P.; van den Broek, P.; Bekel, A.; Eftekhari, P.; Smeitink, J.A.M. KH176 Safeguards Mitochondrial Diseased Cells from Redox Stress-Induced Cell Death by Interacting with the Thioredoxin System/Peroxiredoxin Enzyme Machinery. Sci. Rep. 2018, 8, 6577. [Google Scholar] [CrossRef] [PubMed]
- Barish, G.D.; Narkar, V.A.; Evans, R.M. PPAR delta: A dagger in the heart of the metabolic syndrome. J. Clin. Investig. 2006, 116, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.Z.; Nikolic, N.; Bakke, S.S.; Boekschoten, M.V.; Kersten, S.; Kase, E.T.; Rustan, A.C.; Thoresen, G.H. PPARdelta activation in human myotubes increases mitochondrial fatty acid oxidative capacity and reduces glucose utilization by a switch in substrate preference. Arch. Physiol. Biochem. 2014, 120, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Bell, E.L.; Shine, R.W.; Dwyer, P.; Olson, L.; Truong, J.; Fredenburg, R.; Goddeeris, M.; Stickens, D.; Tozzo, E. PPARdelta modulation rescues mitochondrial fatty acid oxidation defects in the mdx model of muscular dystrophy. Mitochondrion 2019, 46, 51–58. [Google Scholar] [CrossRef]
- Fedorova, L.V.; Sodhi, K.; Gatto-Weis, C.; Puri, N.; Hinds, T.D., Jr.; Shapiro, J.I.; Malhotra, D. Peroxisome proliferator-activated receptor delta agonist, HPP593, prevents renal necrosis under chronic ischemia. PLoS ONE 2013, 8, e64436. [Google Scholar] [CrossRef]
- Szeto, H.H. First-in-class cardiolipin-protective compound as a therapeutic agent to restore mitochondrial bioenergetics. Br. J. Pharmacol. 2014, 171, 2029–2050. [Google Scholar] [CrossRef]
- Paradies, G.; Paradies, V.; Ruggiero, F.M.; Petrosillo, G. Role of Cardiolipin in Mitochondrial Function and Dynamics in Health and Disease: Molecular and Pharmacological Aspects. Cells 2019, 8, 728. [Google Scholar] [CrossRef]
- Probst, B.L.; Trevino, I.; McCauley, L.; Bumeister, R.; Dulubova, I.; Wigley, W.C.; Ferguson, D.A. RTA 408, A Novel Synthetic Triterpenoid with Broad Anticancer and Anti-Inflammatory Activity. PLoS ONE 2015, 10, e0122942. [Google Scholar] [CrossRef]
- Zighan, M.; Arkadir, D.; Douiev, L.; Keller, G.; Miller, C.; Saada, A. Variable effects of omaveloxolone (RTA408) on primary fibroblasts with mitochondrial defects. Front. Mol. Biosci. 2022, 9, 890653. [Google Scholar] [CrossRef]
- Lopez-Gomez, C.; Levy, R.J.; Sanchez-Quintero, M.J.; Juanola-Falgarona, M.; Barca, E.; Garcia-Diaz, B.; Tadesse, S.; Garone, C.; Hirano, M. Deoxycytidine and Deoxythymidine Treatment for Thymidine Kinase 2 Deficiency. Ann. Neurol. 2017, 81, 641–652. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, C.; Augustin, S.; Ellouze, S.; Benit, P.; Bouaita, A.; Rustin, P.; Sahel, J.A.; Corral-Debrinski, M. The optimized allotopic expression of ND1 or ND4 genes restores respiratory chain complex I activity in fibroblasts harboring mutations in these genes. Biochim. Biophys. Acta 2008, 1783, 1707–1717. [Google Scholar] [CrossRef]
- Yu, H.; Koilkonda, R.D.; Chou, T.H.; Porciatti, V.; Ozdemir, S.S.; Chiodo, V.; Boye, S.L.; Boye, S.E.; Hauswirth, W.W.; Lewin, A.S.; et al. Gene delivery to mitochondria by targeting modified adenoassociated virus suppresses Leber’s hereditary optic neuropathy in a mouse model. Proc. Natl. Acad. Sci. USA 2012, 109, E1238–E1247. [Google Scholar] [CrossRef]
- Cwerman-Thibault, H.; Augustin, S.; Lechauve, C.; Ayache, J.; Ellouze, S.; Sahel, J.A.; Corral-Debrinski, M. Nuclear expression of mitochondrial ND4 leads to the protein assembling in complex I and prevents optic atrophy and visual loss. Mol. Ther. Methods Clin. Dev. 2015, 2, 15003. [Google Scholar] [CrossRef] [PubMed]
- Koilkonda, R.; Yu, H.; Talla, V.; Porciatti, V.; Feuer, W.J.; Hauswirth, W.W.; Chiodo, V.; Erger, K.E.; Boye, S.L.; Lewin, A.S.; et al. LHON gene therapy vector prevents visual loss and optic neuropathy induced by G11778A mutant mitochondrial DNA: Biodistribution and toxicology profile. Investig. Ophthalmol. Vis. Sci. 2014, 55, 7739–7753. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, E.; Ben Yakir-Blumkin, M.; Blumenfeld-Kan, S.; Brody, Y.; Meir, A.; Melamed-Book, N.; Napso, T.; Pozner, G.; Saadi, E.; Shabtay-Orbach, A.; et al. Mitochondrial augmentation of CD34(+) cells from healthy donors and patients with mitochondrial DNA disorders confers functional benefit. NPJ Regen. Med. 2021, 6, 58. [Google Scholar] [CrossRef]
- Spendiff, S.; Reza, M.; Murphy, J.L.; Gorman, G.; Blakely, E.L.; Taylor, R.W.; Horvath, R.; Campbell, G.; Newman, J.; Lochmuller, H.; et al. Mitochondrial DNA deletions in muscle satellite cells: Implications for therapies. Hum. Mol. Genet. 2013, 22, 4739–4747. [Google Scholar] [CrossRef] [PubMed]
- van Tienen, F.; Zelissen, R.; Timmer, E.; van Gisbergen, M.; Lindsey, P.; Quattrocelli, M.; Sampaolesi, M.; Mulder-den Hartog, E.; de Coo, I.; Smeets, H. Healthy, mtDNA-mutation free mesoangioblasts from mtDNA patients qualify for autologous therapy. Stem Cell Res. Ther. 2019, 10, 405. [Google Scholar] [CrossRef]
- Arenas-Jal, M.; Sune-Negre, J.M.; Garcia-Montoya, E. Coenzyme Q10 supplementation: Efficacy, safety, and formulation challenges. Compr. Rev. Food Sci. Food Saf. 2020, 19, 574–594. [Google Scholar] [CrossRef]
- Sood, B.; Keenaghan, M. Coenzyme Q10; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Quinzii, C.M.; Hirano, M. Coenzyme Q and mitochondrial disease. Dev. Disabil. Res. Rev. 2010, 16, 183–188. [Google Scholar] [CrossRef]
- Hargreaves, I.P. Coenzyme Q10 as a therapy for mitochondrial disease. Int. J. Biochem. Cell Biol. 2014, 49, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Parkinson Study Group QE3 Investigators; Beal, M.F.; Oakes, D.; Shoulson, I.; Henchcliffe, C.; Galpern, W.R.; Haas, R.; Juncos, J.L.; Nutt, J.G.; Voss, T.S.; et al. A randomized clinical trial of high-dosage coenzyme Q10 in early Parkinson disease: No evidence of benefit. JAMA Neurol. 2014, 71, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Tarnopolsky, M.A. The mitochondrial cocktail: Rationale for combined nutraceutical therapy in mitochondrial cytopathies. Adv. Drug Deliv. Rev. 2008, 60, 1561–1567. [Google Scholar] [CrossRef] [PubMed]
- Tragni, V.; Primiano, G.; Tummolo, A.; Cafferati Beltrame, L.; La Piana, G.; Sgobba, M.N.; Cavalluzzi, M.M.; Paterno, G.; Gorgoglione, R.; Volpicella, M.; et al. Personalized Medicine in Mitochondrial Health and Disease: Molecular Basis of Therapeutic Approaches Based on Nutritional Supplements and Their Analogs. Molecules 2022, 27, 3494. [Google Scholar] [CrossRef]
- Geromel, V.; Darin, N.; Chretien, D.; Benit, P.; DeLonlay, P.; Rotig, A.; Munnich, A.; Rustin, P. Coenzyme Q(10) and idebenone in the therapy of respiratory chain diseases: Rationale and comparative benefits. Mol. Genet. Metab. 2002, 77, 21–30. [Google Scholar] [CrossRef]
- Singh, A.; Faccenda, D.; Campanella, M. Pharmacological advances in mitochondrial therapy. EBioMedicine 2021, 65, 103244. [Google Scholar] [CrossRef]
- Shrader, W.D.; Amagata, A.; Barnes, A.; Enns, G.M.; Hinman, A.; Jankowski, O.; Kheifets, V.; Komatsuzaki, R.; Lee, E.; Mollard, P.; et al. alpha-Tocotrienol quinone modulates oxidative stress response and the biochemistry of aging. Bioorg. Med. Chem. Lett. 2011, 21, 3693–3698. [Google Scholar] [CrossRef]
- Baudouin-Cornu, P.; Lagniel, G.; Kumar, C.; Huang, M.E.; Labarre, J. Glutathione degradation is a key determinant of glutathione homeostasis. J. Biol. Chem. 2012, 287, 4552–4561. [Google Scholar] [CrossRef]
- Enns, G.M.; Kinsman, S.L.; Perlman, S.L.; Spicer, K.M.; Abdenur, J.E.; Cohen, B.H.; Amagata, A.; Barnes, A.; Kheifets, V.; Shrader, W.D.; et al. Initial experience in the treatment of inherited mitochondrial disease with EPI-743. Mol. Genet. Metab. 2012, 105, 91–102. [Google Scholar] [CrossRef]
- Kouga, T.; Takagi, M.; Miyauchi, A.; Shimbo, H.; Iai, M.; Yamashita, S.; Murayama, K.; Klein, M.B.; Miller, G.; Goto, T.; et al. Japanese Leigh syndrome case treated with EPI-743. Brain Dev. 2018, 40, 145–149. [Google Scholar] [CrossRef]
- Srivastava, S. Emerging therapeutic roles for NAD(+) metabolism in mitochondrial and age-related disorders. Clin. Transl. Med. 2016, 5, 25. [Google Scholar] [CrossRef] [PubMed]
- Dolopikou, C.F.; Kourtzidis, I.A.; Margaritelis, N.V.; Vrabas, I.S.; Koidou, I.; Kyparos, A.; Theodorou, A.A.; Paschalis, V.; Nikolaidis, M.G. Acute nicotinamide riboside supplementation improves redox homeostasis and exercise performance in old individuals: A double-blind cross-over study. Eur. J. Nutr. 2020, 59, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Remie, C.M.E.; Roumans, K.H.M.; Moonen, M.P.B.; Connell, N.J.; Havekes, B.; Mevenkamp, J.; Lindeboom, L.; de Wit, V.H.W.; van de Weijer, T.; Aarts, S.; et al. Nicotinamide riboside supplementation alters body composition and skeletal muscle acetylcarnitine concentrations in healthy obese humans. Am. J. Clin. Nutr. 2020, 112, 413–426. [Google Scholar] [CrossRef] [PubMed]
- Lapatto, H.A.K.; Kuusela, M.; Heikkinen, A.; Muniandy, M.; van der Kolk, B.W.; Gopalakrishnan, S.; Pollanen, N.; Sandvik, M.; Schmidt, M.S.; Heinonen, S.; et al. Nicotinamide riboside improves muscle mitochondrial biogenesis, satellite cell differentiation, and gut microbiota in a twin study. Sci. Adv. 2023, 9, eadd5163. [Google Scholar] [CrossRef]
- Feng, L.; Luo, H.; Xu, Z.; Yang, Z.; Du, G.; Zhang, Y.; Yu, L.; Hu, K.; Zhu, W.; Tong, Q.; et al. Bavachinin, as a novel natural pan-PPAR agonist, exhibits unique synergistic effects with synthetic PPAR-gamma and PPAR-alpha agonists on carbohydrate and lipid metabolism in db/db and diet-induced obese mice. Diabetologia 2016, 59, 1276–1286. [Google Scholar] [CrossRef]
- de Boer, E.M.J.; Orie, V.K.; Williams, T.; Baker, M.R.; De Oliveira, H.M.; Polvikoski, T.; Silsby, M.; Menon, P.; van den Bos, M.; Halliday, G.M.; et al. TDP-43 proteinopathies: A new wave of neurodegenerative diseases. J. Neurol. Neurosurg. Psychiatry 2020, 92, 86–95. [Google Scholar] [CrossRef]
- Falabella, M.; Vernon, H.J.; Hanna, M.G.; Claypool, S.M.; Pitceathly, R.D.S. Cardiolipin, Mitochondria, and Neurological Disease. Trends Endocrinol. Metab. 2021, 32, 224–237. [Google Scholar] [CrossRef]
- Gautam, M.; Genc, B.; Helmold, B.; Ahrens, A.; Kuka, J.; Makrecka-Kuka, M.; Gunay, A.; Kocak, N.; Aguilar-Wickings, I.R.; Keefe, D.; et al. SBT-272 improves TDP-43 pathology in ALS upper motor neurons by modulating mitochondrial integrity, motility, and function. Neurobiol. Dis. 2023, 178, 106022. [Google Scholar] [CrossRef]
- Birk, A.V.; Liu, S.; Soong, Y.; Mills, W.; Singh, P.; Warren, J.D.; Seshan, S.V.; Pardee, J.D.; Szeto, H.H. The mitochondrial-targeted compound SS-31 re-energizes ischemic mitochondria by interacting with cardiolipin. J. Am. Soc. Nephrol. 2013, 24, 1250–1261. [Google Scholar] [CrossRef]
- Dai, D.F.; Hsieh, E.J.; Chen, T.; Menendez, L.G.; Basisty, N.B.; Tsai, L.; Beyer, R.P.; Crispin, D.A.; Shulman, N.J.; Szeto, H.H.; et al. Global proteomics and pathway analysis of pressure-overload-induced heart failure and its attenuation by mitochondrial-targeted peptides. Circ. Heart Fail. 2013, 6, 1067–1076. [Google Scholar] [CrossRef]
- Machiraju, P.; Wang, X.; Sabouny, R.; Huang, J.; Zhao, T.; Iqbal, F.; King, M.; Prasher, D.; Lodha, A.; Jimenez-Tellez, N.; et al. SS-31 Peptide Reverses the Mitochondrial Fragmentation Present in Fibroblasts From Patients With DCMA, a Mitochondrial Cardiomyopathy. Front. Cardiovasc. Med. 2019, 6, 167. [Google Scholar] [CrossRef] [PubMed]
- Reid Thompson, W.; Hornby, B.; Manuel, R.; Bradley, E.; Laux, J.; Carr, J.; Vernon, H.J. A phase 2/3 randomized clinical trial followed by an open-label extension to evaluate the effectiveness of elamipretide in Barth syndrome, a genetic disorder of mitochondrial cardiolipin metabolism. Genet. Med. 2021, 23, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.E.; Pennington, E.R.; Perry, J.B.; Dadoo, S.; Makrecka-Kuka, M.; Dambrova, M.; Moukdar, F.; Patel, H.D.; Han, X.; Kidd, G.K.; et al. The cardiolipin-binding peptide elamipretide mitigates fragmentation of cristae networks following cardiac ischemia reperfusion in rats. Commun. Biol. 2020, 3, 389. [Google Scholar] [CrossRef] [PubMed]
- Distelmaier, F.; Visch, H.J.; Smeitink, J.A.; Mayatepek, E.; Koopman, W.J.; Willems, P.H. The antioxidant Trolox restores mitochondrial membrane potential and Ca2+ -stimulated ATP production in human complex I deficiency. J. Mol. Med. 2009, 87, 515–522. [Google Scholar] [CrossRef]
- Blanchet, L.; Smeitink, J.A.; van Emst-de Vries, S.E.; Vogels, C.; Pellegrini, M.; Jonckheere, A.I.; Rodenburg, R.J.; Buydens, L.M.; Beyrath, J.; Willems, P.H.; et al. Quantifying small molecule phenotypic effects using mitochondrial morpho-functional fingerprinting and machine learning. Sci. Rep. 2015, 5, 8035. [Google Scholar] [CrossRef] [PubMed]
- Klein Gunnewiek, T.M.; Verboven, A.H.A.; Pelgrim, I.; Hogeweg, M.; Schoenmaker, C.; Renkema, H.; Beyrath, J.; Smeitink, J.; de Vries, B.B.A.; Hoen, P.A.C.; et al. Sonlicromanol improves neuronal network dysfunction and transcriptome changes linked to m.3243A>G heteroplasmy in iPSC-derived neurons. Stem Cell Rep. 2021, 16, 2197–2212. [Google Scholar] [CrossRef]
- Abeti, R.; Uzun, E.; Renganathan, I.; Honda, T.; Pook, M.A.; Giunti, P. Targeting lipid peroxidation and mitochondrial imbalance in Friedreich’s ataxia. Pharmacol. Res. 2015, 99, 344–350. [Google Scholar] [CrossRef]
- Abeti, R.; Baccaro, A.; Esteras, N.; Giunti, P. Novel Nrf2-Inducer Prevents Mitochondrial Defects and Oxidative Stress in Friedreich’s Ataxia Models. Front. Cell. Neurosci. 2018, 12, 188. [Google Scholar] [CrossRef]
- Tiberi, J.; Segatto, M.; Fiorenza, M.T.; La Rosa, P. Apparent Opportunities and Hidden Pitfalls: The Conflicting Results of Restoring NRF2-Regulated Redox Metabolism in Friedreich’s Ataxia Pre-Clinical Models and Clinical Trials. Biomedicines 2023, 11, 1293. [Google Scholar] [CrossRef]
- Naso, M.F.; Tomkowicz, B.; Perry, W.L., 3rd; Strohl, W.R. Adeno-Associated Virus (AAV) as a Vector for Gene Therapy. BioDrugs 2017, 31, 317–334. [Google Scholar] [CrossRef]
- Wang, D.; Tai, P.W.L.; Gao, G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat. Rev. Drug Discov. 2019, 18, 358–378. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Samulski, R.J. Engineering adeno-associated virus vectors for gene therapy. Nat. Rev. Genet. 2020, 21, 255–272. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Ozdemir, S.S.; Koilkonda, R.D.; Chou, T.H.; Porciatti, V.; Chiodo, V.; Boye, S.L.; Hauswirth, W.W.; Lewin, A.S.; Guy, J. Mutant NADH dehydrogenase subunit 4 gene delivery to mitochondria by targeting sequence-modified adeno-associated virus induces visual loss and optic atrophy in mice. Mol. Vis. 2012, 18, 1668–1683. [Google Scholar] [PubMed]
- Newman, N.J.; Yu-Wai-Man, P.; Subramanian, P.S.; Moster, M.L.; Wang, A.G.; Donahue, S.P.; Leroy, B.P.; Carelli, V.; Biousse, V.; Vignal-Clermont, C.; et al. Randomized trial of bilateral gene therapy injection for m.11778G>A MT-ND4 Leber optic neuropathy. Brain 2023, 146, 1328–1341. [Google Scholar] [CrossRef]
- McGrady, N.R.; Boal, A.M.; Risner, M.L.; Taiel, M.; Sahel, J.A.; Calkins, D.J. Ocular stress enhances contralateral transfer of lenadogene nolparvovec gene therapy through astrocyte networks. Mol. Ther. 2023, 31, 2005–2013. [Google Scholar] [CrossRef]
- Spees, J.L.; Olson, S.D.; Whitney, M.J.; Prockop, D.J. Mitochondrial transfer between cells can rescue aerobic respiration. Proc. Natl. Acad. Sci. USA 2006, 103, 1283–1288. [Google Scholar] [CrossRef]
- Islam, M.N.; Das, S.R.; Emin, M.T.; Wei, M.; Sun, L.; Westphalen, K.; Rowlands, D.J.; Quadri, S.K.; Bhattacharya, S.; Bhattacharya, J. Mitochondrial transfer from bone-marrow-derived stromal cells to pulmonary alveoli protects against acute lung injury. Nat. Med. 2012, 18, 759–765. [Google Scholar] [CrossRef]
- Hayakawa, K.; Esposito, E.; Wang, X.; Terasaki, Y.; Liu, Y.; Xing, C.; Ji, X.; Lo, E.H. Transfer of mitochondria from astrocytes to neurons after stroke. Nature 2016, 535, 551–555. [Google Scholar] [CrossRef]
- Dong, L.F.; Rohlena, J.; Zobalova, R.; Nahacka, Z.; Rodriguez, A.M.; Berridge, M.V.; Neuzil, J. Mitochondria on the move: Horizontal mitochondrial transfer in disease and health. J. Cell Biol. 2023, 222, e202211044. [Google Scholar] [CrossRef]
- Jacoby, E.; Bar-Yosef, O.; Gruber, N.; Lahav, E.; Varda-Bloom, N.; Bolkier, Y.; Bar, D.; Blumkin, M.B.; Barak, S.; Eisenstein, E.; et al. Mitochondrial augmentation of hematopoietic stem cells in children with single large-scale mitochondrial DNA deletion syndromes. Sci. Transl. Med. 2022, 14, eabo3724. [Google Scholar] [CrossRef]
- Sampaolesi, M.; Torrente, Y.; Innocenzi, A.; Tonlorenzi, R.; D’Antona, G.; Pellegrino, M.A.; Barresi, R.; Bresolin, N.; De Angelis, M.G.; Campbell, K.P.; et al. Cell therapy of alpha-sarcoglycan null dystrophic mice through intra-arterial delivery of mesoangioblasts. Science 2003, 301, 487–492. [Google Scholar] [CrossRef]
- Roobrouck, V.D.; Clavel, C.; Jacobs, S.A.; Ulloa-Montoya, F.; Crippa, S.; Sohni, A.; Roberts, S.J.; Luyten, F.P.; Van Gool, S.W.; Sampaolesi, M.; et al. Differentiation potential of human postnatal mesenchymal stem cells, mesoangioblasts, and multipotent adult progenitor cells reflected in their transcriptome and partially influenced by the culture conditions. Stem Cells 2011, 29, 871–882. [Google Scholar] [CrossRef] [PubMed]
- Dellavalle, A.; Sampaolesi, M.; Tonlorenzi, R.; Tagliafico, E.; Sacchetti, B.; Perani, L.; Innocenzi, A.; Galvez, B.G.; Messina, G.; Morosetti, R.; et al. Pericytes of human skeletal muscle are myogenic precursors distinct from satellite cells. Nat. Cell Biol. 2007, 9, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Dellavalle, A.; Maroli, G.; Covarello, D.; Azzoni, E.; Innocenzi, A.; Perani, L.; Antonini, S.; Sambasivan, R.; Brunelli, S.; Tajbakhsh, S.; et al. Pericytes resident in postnatal skeletal muscle differentiate into muscle fibres and generate satellite cells. Nat. Commun. 2011, 2, 499. [Google Scholar] [CrossRef]
- Cree, L.; Loi, P. Mitochondrial replacement: From basic research to assisted reproductive technology portfolio tool-technicalities and possible risks. Mol. Hum. Reprod. 2015, 21, 3–10. [Google Scholar] [CrossRef]
- Sharma, H.; Singh, D.; Mahant, A.; Sohal, S.K.; Kesavan, A.K.; Samiksha. Development of mitochondrial replacement therapy: A review. Heliyon 2020, 6, e04643. [Google Scholar] [CrossRef] [PubMed]
- Connor, S. When replacement becomes reversion. Nat. Biotechnol. 2017, 35, 1012–1015. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Sato, S.; Ooka, R.; Akashi, K.; Nakamura, A.; Miyado, K.; Akutsu, H.; Tanaka, M. Mitochondrial replacement by genome transfer in human oocytes: Efficacy, concerns, and legality. Reprod. Med. Biol. 2021, 20, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Pompei, M.; Pompei, F. Overcoming bioethical, legal, and hereditary barriers to mitochondrial replacement therapy in the USA. J. Assist. Reprod. Genet. 2019, 36, 383–393. [Google Scholar] [CrossRef]
- Anzalone, A.V.; Koblan, L.W.; Liu, D.R. Genome editing with CRISPR-Cas nucleases, base editors, transposases and prime editors. Nat. Biotechnol. 2020, 38, 824–844. [Google Scholar] [CrossRef]
- Gammage, P.A.; Moraes, C.T.; Minczuk, M. Mitochondrial Genome Engineering: The Revolution May Not Be CRISPR-Ized. Trends Genet. 2018, 34, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Moscou, M.J.; Bogdanove, A.J. A Simple Cipher Governs DNA Recognition by TAL Effectors. Science 2009, 326, 1501. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.C.; Tan, S.; Qiao, G.; Barlow, K.A.; Wang, J.; Xia, D.F.; Meng, X.; Paschon, D.E.; Leung, E.; Hinkley, S.J.; et al. A TALE nuclease architecture for efficient genome editing. Nat. Biotechnol. 2011, 29, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Boch, J.; Scholze, H.; Schornack, S.; Landgraf, A.; Hahn, S.; Kay, S.; Lahaye, T.; Nickstadt, A.; Bonas, U. Breaking the Code of DNA Binding Specificity of TAL-Type III Effectors. Science 2009, 326, 1509–1512. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lee, S.; Baek, G.; Kim, A.; Kang, B.C.; Seo, H.; Kim, J.S. Mitochondrial DNA editing in mice with DddA-TALE fusion deaminases. Nat. Commun. 2021, 12, 1190. [Google Scholar] [CrossRef]
- Mok, B.Y.; Kotrys, A.V.; Raguram, A.; Huang, T.P.; Mootha, V.K.; Liu, D.R. CRISPR-free base editors with enhanced activity and expanded targeting scope in mitochondrial and nuclear DNA. Nat. Biotechnol. 2022, 40, 1378–1387. [Google Scholar] [CrossRef]
- Lee, S.; Lee, H.; Baek, G.; Namgung, E.; Park, J.M.; Kim, S.; Hong, S.; Kim, J.S. Enhanced mitochondrial DNA editing in mice using nuclear-exported TALE-linked deaminases and nucleases. Genome Biol. 2022, 23, 211. [Google Scholar] [CrossRef]
- Guo, J.; Chen, X.; Liu, Z.; Sun, H.; Zhou, Y.; Dai, Y.; Ma, Y.E.; He, L.; Qian, X.; Wang, J.; et al. DdCBE mediates efficient and inheritable modifications in mouse mitochondrial genome. Mol. Ther.—Nucleic Acids 2022, 27, 73–80. [Google Scholar] [CrossRef]
- Tan, L.; Qi, X.; Kong, W.; Jin, J.; Lu, D.; Zhang, X.; Wang, Y.; Wang, S.; Dong, W.; Shi, X.; et al. A conditional knockout rat resource of mitochondrial protein-coding genes via a DdCBE-induced premature stop codon. Sci. Adv. 2023, 9, eadf2695. [Google Scholar] [CrossRef]
- Silva-Pinheiro, P.; Mutti, C.D.; Van Haute, L.; Powell, C.A.; Nash, P.A.; Turner, K.; Minczuk, M. A library of base editors for the precise ablation of all protein-coding genes in the mouse mitochondrial genome. Nat. Biomed. Eng. 2023, 7, 692–703. [Google Scholar] [CrossRef]
- Gaudelli, N.M.; Komor, A.C.; Rees, H.A.; Packer, M.S.; Badran, A.H.; Bryson, D.I.; Liu, D.R. Programmable base editing of A•T to G•C in genomic DNA without DNA cleavage. Nature 2017, 551, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.F.; Zhao, K.T.; Eton, E.; Lapinaite, A.; Newby, G.A.; Thuronyi, B.W.; Wilson, C.; Koblan, L.W.; Zeng, J.; Bauer, D.E.; et al. Phage-assisted evolution of an adenine base editor with improved Cas domain compatibility and activity. Nat. Biotechnol. 2020, 38, 883–891. [Google Scholar] [CrossRef] [PubMed]
- Thuronyi, B.W.; Koblan, L.W.; Levy, J.M.; Yeh, W.-H.; Zheng, C.; Newby, G.A.; Wilson, C.; Bhaumik, M.; Shubina-Oleinik, O.; Holt, J.R.; et al. Continuous evolution of base editors with expanded target compatibility and improved activity. Nat. Biotechnol. 2019, 37, 1070–1079. [Google Scholar] [CrossRef]
- Zhao, D.; Li, J.; Li, S.; Xin, X.; Hu, M.; Price, M.A.; Rosser, S.J.; Bi, C.; Zhang, X. Glycosylase base editors enable C-to-A and C-to-G base changes. Nat. Biotechnol. 2021, 39, 35–40. [Google Scholar] [CrossRef]
- Kurt, I.C.; Zhou, R.; Iyer, S.; Garcia, S.P.; Miller, B.R.; Langner, L.M.; Grünewald, J.; Joung, J.K. CRISPR C-to-G base editors for inducing targeted DNA transversions in human cells. Nat. Biotechnol. 2021, 39, 41–46. [Google Scholar] [CrossRef]
- Chen, L.; Hong, M.; Luan, C.; Gao, H.; Ru, G.; Guo, X.; Zhang, D.; Zhang, S.; Li, C.; Wu, J.; et al. Adenine transversion editors enable precise, efficient A•T-to-C•G base editing in mammalian cells and embryos. Nat. Biotechnol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Lei, Z.; Meng, H.; Liu, L.; Zhao, H.; Rao, X.; Yan, Y.; Wu, H.; Liu, M.; He, A.; Yi, C. Mitochondrial base editor induces substantial nuclear off-target mutations. Nature 2022, 606, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Li, Z.; Xu, K.; Feng, H.; Xie, L.; Li, D.; Zuo, Z.; Zhang, M.; Xu, C.; Yang, H.; et al. Mitochondrial base editor DdCBE causes substantial DNA off-target editing in nuclear genome of embryos. Cell Discov. 2022, 8, 27. [Google Scholar] [CrossRef]
- Jeppesen, T.D.; Schwartz, M.; Olsen, D.B.; Wibrand, F.; Krag, T.; Duno, M.; Hauerslev, S.; Vissing, J. Aerobic training is safe and improves exercise capacity in patients with mitochondrial myopathy. Brain 2006, 129, 3402–3412. [Google Scholar] [CrossRef]
- Murphy, J.L.; Blakely, E.L.; Schaefer, A.M.; He, L.; Wyrick, P.; Haller, R.G.; Taylor, R.W.; Turnbull, D.M.; Taivassalo, T. Resistance training in patients with single, large-scale deletions of mitochondrial DNA. Brain 2008, 131, 2832–2840. [Google Scholar] [CrossRef]
- Lopez-Gomez, C.; Sanchez-Quintero, M.J.; Lee, E.J.; Kleiner, G.; Tadesse, S.; Xie, J.; Akman, H.O.; Gao, G.; Hirano, M. Synergistic Deoxynucleoside and Gene Therapies for Thymidine Kinase 2 Deficiency. Ann. Neurol. 2021, 90, 640–652. [Google Scholar] [CrossRef] [PubMed]



| Disease | Main Symptoms | Case Reports References | Cause |
|---|---|---|---|
| LHON (Leber hereditary optic neuropathy) | Vision loss (retinal ganglion cells and axon loss) | Significant decrease in visual acuity, dyschromatopsia [54,55,56] | m.T14484C (Complex1 ND6) |
| m.G3460A (Complex1 ND1) | |||
| m.G11778A (Complex1 ND4) | |||
| MERRF (Myoclonic epilepsy with ragged red fiber) | Myoclonus, generalized epilepsy, ataxia, myopathy, exercise intolerance | Bilateral primary optic atrophy, sensorineural hearing loss, gait unsteadiness [57] | m.A8344G (tRNA lysine) |
| Slurred speech, fatigue, hearing loss, limb weakness [58] | m.G8363A (tRNA lysine) | ||
| Dysphonia, memory loss, stroke-like episode [59] | m.A3243G (tRNA leucine) | ||
| MELAS (Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes) | Muscle weakness in whole body, dementia, aphasia, myoclonus, ataxia | Developing diabetes, hearing loss, progressively deteriorating functional status [60] | m.A3243G (tRNA leucine) |
| Aphasia, subtle loss of muscle strength in right arm [61] | |||
| Migraine-like headaches, muscle damage [62] | |||
| disturbances of consciousness, ventilatory failure [63] | |||
| Aeizures, transient sensory disturbances, weakness, visual impairment, cognitive impairment [64] | m.G13513A (Complex1 ND5) | ||
| Maternally inherited diabetes and deafness (MIDD) | Chronic kidney disease, deafness, loss of oral sensation, neuropathy, hearing loss, myopathy | Proteinuria, glomerular abnormality progressive renal failuare [65] | m.A3243G (tRNA leucine) |
| Hearing loss, loss of oral sensation, dysarthria, drolling [66] | |||
| Hearing loss, central nervous system diseases, myopathy, cardiac disease, nephropathy, underweight [10] | |||
| Pearson syndrome | Failure to thrive, malabsorption | Refractory anemia, digestive system failuare, bone marrow failure, metabolic disorders, gastrointestinal symptoms, renal disorders, pancreatic exocrine insufficiency [11] | Large deletion of mtDNA |
| Malabsorption, lactic acidemia, sideroblasts on bone marrow evaluation, microcephaly [67] | |||
| Kearns–Sayre syndrome (KSS) | Heart block, growth retardation, external ophthalmoplegia, vestibular dysfunction | Vision loss, progressive external ophthalmoplegia, retinitis pigmentosa, heart block, vestibular dysfunction, growth retardation [68] | Large deletion of mtDNA |
| Photophobia, nystagmus, sensorineural hearing loss, tremor, progressive cerebellar ataxia [69] | |||
| Chronic progressive external ophthalmoplegia (CPEO) | Loosing control of eyelids and eye movements, ptosis | Central neurogenic hyperventilation, restriction of eye movement and ptosis [70] | Multiple deletion of mtDNA |
| Low birth weight and congenital deafness [71] | |||
| Hemifacial weakness, dysarthria, mental retardation, sensorineural hearing loss [72] | mtDNA mutation with mitochondrial protein-encoding nuclear DNA mutations [73] | ||
| Ophthalmoplegia, strabismus, loosing control of extraocular muscles [71] | |||
| Leigh syndrome | Neurological symptoms, cardiac dysfunction, dyspraxia | Blepharoptosis, ptosis, inability to walk, sensory deficits, fever [74] | m.T9176C (MT-ATP6) |
| Delay of psychomotor development, cardiomyopathy [75] | m.A14453G (Complex1 ND6) | ||
| Bilateral exotropia, nystagmus bilateral, childhood-onset neuromuscular regression [76] | Nuclear NDUFAF5 gene mutation, (Complex 1 NDUFAF5) | ||
| Barth syndrome | Heart failure | Left ventricular hypertrophy, heart failure with metabolic crisis [77] | Nuclear TAZ gene C640T (mitochondrial acyl chain composition remodeling enzyme) |
| Friedreich’s ataxia | Ataxia, gait unsteadiness, cardiomyopathy | Chest pain, dyspnea, palpitation, left ventricular hypertrophy [78] | Nuclear FAZ gene (mitochondrial iron metabolism related enzyme) |
| Blindness, sensorineural deafness [79], |
| Treatment | Mechanisms | Target Disease | Clinical Trial /NCT Number |
|---|---|---|---|
| Coenzyme Q10 | Diffusible electron carrier of the mitochondrial respiratory chain [145], lipid peroxidation interfering antioxidants [146,147] | Mitochondrial diseases | Phase 3 (Completed) /NCT00432744 |
| RAXONE (Idebenone) | Transfer electrons directly to complex III by bypassing malfunctional complex I [148,149,150,151] | LHON (Leber hereditary optic neuropathy) | Phase 4 (Completed) /NCT02774005 |
| Vatiquinone (EPI-743, PTC-743) | Inhibiting 15-lipoxygenase (15-LO) [152] leads to increased GSH levels and decreased oxidized GSH [153,154] | Friedreich ataxia | Phase 3 (Active) /NCT05515536 |
| Mitochondrial disease with refractory epilepsy | Phase 2/3 (Active) /NCT04378075 | ||
| Mitochondrial respiratory chain diseases | Phase 2 (Active) /NCT01370447 | ||
| Nicotinamide Riboside (NR) | Precursor of Nicotinamide adenine dinucleotide (NAD+); increasing intracellular NAD+ level increases mitochondrial function and mitochondrial number [155,156,157,158] | Mitochondrial myopathy disorder | Phase 2 (Active) /NCT05590468 |
| KL1333 | Interacts with NQO1 and acts as precursor of NAD+, recovers deficiency of mitochondrial respiratory chain [159] | Mitochondrial disease | Phase 2 (Active) /NCT05650229 |
| Sonlicromanol (KH176) | ROS-redox modulator through interaction with the Thioredoxin System, which is a major antioxidant and redox signaling cellular system [160] | m.A3243G causing mitochondrial diseases | Phase 2 (Completed) /NCT04165239 |
| Bocidelpar (ASP0367) | Agonist of PPARδ, enhances fatty acid oxidation, mitochondrial respiration and oxidative metabolism, which further leads to increment of skeletal muscle genes expression [161,162,163] | Primary mitochondrial myopathy | Phase 2/3 (Active) /NCT04641962 |
| Mavodelpar (REN001, HPP593) | Agonist of PPARδ upregulates oxidative stress defense genes, contributes to attenuating oxidative stress [164] | Primary mitochondrial myopathy | Phase 2 (Active) /NCT04535609 |
| Elamipretide (SBT-272) | Binding mitochondrial inner membrane cardiolipin; rescues dysmorphology of mitochondria [165,166] | Primary mitochondrial myopathy | Phase 3 (Active) /NCT05162768 |
| Barth syndrome | Phase 3 (Completed) /NCT03098797 | ||
| Mitochondrial dysfunction in age-related macular degeneration | Phase 2 (Completed) /NCT03891875 | ||
| Friedreich Ataxia | Phase 1/2 (Active) /NCT05168774 | ||
| Skyclarys (Omaveloxolone) | Nrf2 degradation inhibitor; upregulates the expression of antioxidant gene, downregulates the expression of pro-inflammatory genes, and enhances mitochondrial biogenesis [167,168] | Friedreich’s ataxia | FDA approved |
| Deoxynucleosides Pyrimidines (Deoxycytidine dC and Deoxythymidine dT) | Enhances mtDNA maintenance by bypassing malfunctional mitochondrial pyrimidine salvage pathway [169] | Mitochondrial depletion syndromes with neurological phenotypes dysfunction | Phase 2 (Active) /NCT04802707 |
| Treatment | Mechanisms | Target disease | Clinical trials |
|---|---|---|---|
| LUMEVOQ (GS010, rAAV2/2-ND4), | MT-ND4 deficiency rescue via allotopic expression of normal MT-ND4 using recombinant AAV [170,171,172] | LHON (Leber hereditary optic neuropathy) | Phase 3 (Active) /NCT03293524 |
| NR082 (rAAV2-ND4), | Phase 2/3 (Active) /NCT03153293 | ||
| ScAAV2-P1ND4v2 | MT-ND4 deficiency rescue via allotopic expression of normal MT-ND4 using self-complementary AAV [173] | Phase 1 (Active) /NCT02161380 | |
| Mitochondrial augmentation | Replacement of dysfunctional mitochondria with healthy-exogenous donor mitochondria using in vitro uptake [174] | mtDNA depletion disease (Pearson syndrome) | Phase 1/2 (Active) /NCT03384420 |
| Mesoangioblasts (MABs) | Intra-arterial injection of in vitro cultured patient-autologous mesoangioblasts, which harbor far fewer mtDNA mutations despite a much higher mutation load in patient [175,176] | Mitochondrial myopathy with m.A3243G mutation | Phase 2 (Active) /NCT05962333 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, S.; Kim, S.; Kim, K.; Lee, H. Clinical Approaches for Mitochondrial Diseases. Cells 2023, 12, 2494. https://doi.org/10.3390/cells12202494
Hong S, Kim S, Kim K, Lee H. Clinical Approaches for Mitochondrial Diseases. Cells. 2023; 12(20):2494. https://doi.org/10.3390/cells12202494
Chicago/Turabian StyleHong, Seongho, Sanghun Kim, Kyoungmi Kim, and Hyunji Lee. 2023. "Clinical Approaches for Mitochondrial Diseases" Cells 12, no. 20: 2494. https://doi.org/10.3390/cells12202494
APA StyleHong, S., Kim, S., Kim, K., & Lee, H. (2023). Clinical Approaches for Mitochondrial Diseases. Cells, 12(20), 2494. https://doi.org/10.3390/cells12202494