Abstract
Pancreatic ductal adenocarcinoma (PDAC) is a devastating malignant disease with a dismal prognosis. In the past decades, a plethora of genetically engineered mouse models (GEMMs) with autochthonous pancreatic tumor development have greatly facilitated studies of pancreatic cancer. Commonly used GEMMs of PDAC often harbor the oncogenic KRAS driver mutation (KrasG12D), in combination with either p53 mutation by knock-in strategy (Trp53R172H) or p53 loss by conditional knockout (Trp53cKO) strategy, in pancreatic cell lineages. However, the systematic comparison of the tumor microenvironment between KrasG12D; Trp53R172H (KPmut) mouse models and KrasG12D; Trp53cKO (KPloss) mouse models is still lacking. In this study, we conducted cross-dataset single-cell RNA-sequencing (scRNA-seq) analyses to compare the pancreatic tumor microenvironment from KPmut mouse models and KPloss mouse models, especially focusing on the cell compositions and transcriptomic phenotypes of major cell types including cancer cells, B cells, T cells, granulocytes, myeloid cells, cancer-associated fibroblasts, and endothelial cells. We identified the similarities and differences between KPmut and KPloss mouse models, revealing the effects of p53 mutation and p53 loss on oncogenic KRAS-driven pancreatic tumor progression.
1. Introduction
Pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest cancer types and is resistant to therapies [1]. Unfortunately, most patients already present with either locally advanced or metastatic PDAC upon diagnosis, thus preventing the surgical resection of the tumors [2]. PDAC is characterized by a desmoplastic microenvironment comprising various cell populations, including cancer cells, cancer-associated fibroblasts (CAFs), endothelial cells, and immune cells [3]. Recent observations utilizing a single-cell RNA-sequencing (scRNA-seq) technique have shed light on the landscape of these cell populations in the tumor microenvironment of PDAC [4,5,6,7,8,9,10,11,12]. Our recent studies using scRNA-seq and various transgenic mouse models of PDAC have identified the changes in specific cell populations associated with different tumor stages and genotypes [10,11,13]. The development of PDAC is frequently associated with genetic alterations of KRAS (KRAS gene) and p53 (TP53 gene). While oncogenic KRAS alteration is dominated by the G12* (especially G12D) mutation as the key driver of PDAC, p53 mutations can have either gain-of-function or loss-of-function effects [14]. One of the most studied p53 mutations in the context of PDAC mouse models is p53R172H, corresponding to the human p53R175H. The p53R172H mutation has been shown to be associated with p53 gain of function and overexpression in cancer cells, leading to oncogenic effects [15,16,17,18]. The other commonly observed p53 mutations in human cancers include R248Q, R248W, R273C, R273H, G245S, H179R, Y163C, Y220C, Y234C, G249, and R282, which are associated with p53 gain-of-function mutations [19,20,21]. Recent studies reported that p53R248W can promote the metastasis of human pancreatic cancer [22]. In this study, we focused on the p53R172H as a representative p53 gain-of-function mutation (hereafter referred to as “p53 mutation”), as compared to p53 deletion or loss-of-function mutations (hereafter referred to as “p53 loss”). Previous studies using various transgenic mouse models have shown that gain-of-function p53 mutations can have significantly different oncogenic and pro-metastatic effects as compared to the loss-of-function p53 mutations in the context of PDAC [15,16]. However, it remains unclear whether p53 mutation and p53 loss can differentially influence the various cell populations within the tumor ecosystem. Here, we performed cross-dataset analyses of scRNA-seq data from PDAC samples to systematically reveal the differences between p53 mutation and p53 loss in regulating the tumor microenvironment of oncogenic KRAS-driven PDAC.
2. Methods
2.1. Single-Cell RNA-Sequencing (scRNA-Seq) Analysis
The datasets used in this study were obtained by downloading our previously deposited files from the Gene Expression Omnibus (GEO) repository as described in our recent studies [10,11]. Specifically, the scRNA-seq data of early and late primary tumors from a KPmut (KrasG12D; Trp53R172H) mouse model with KRASG12D mutation and p53R172H mutation were from the GSE198815 dataset, and the scRNA-seq data of late primary tumors from a KPloss (KrasG12D; Trp53cKO) mouse model with KRASG12D mutation and p53 loss mice were from the GSE166298 dataset. As previously described, early-stage PDAC was defined by having less than 10% pancreatic adenocarcinoma areas, while late-stage PDAC was defined by having greater than 50% pancreatic adenocarcinoma areas. All the scRNA-seq datasets were derived from primary pancreatic tumors of background-matched mice. The KPmut-Early (early-stage primary tumor with KRAS and p53 mutations) group contained 6175 cells from 3 individual early-stage KPmut mice. The KPmut-Late (late-stage primary tumor with KRAS and p53 mutations) group contained 9479 cells from 3 individual late-stage KPmut mice. The KPloss-Late (late-stage primary tumor with KRAS mutation and p53 loss) group contained 4072 cells derived from 3 individual late-stage KPloss mice. All samples were processed using the same protocol by the Sequencing and Microarray Facility at MD Anderson Cancer Center (MDACC). To analyze the cells, we used the 10X Genomics Chromium controller and Single Cell 3’ Reagent Kits v2 (10X Genomics, Pleasanton, CA, USA). This generated cDNA, which was then amplified to create Illumina sequencing libraries. We used the Illumina NextSeq 500 to sequence the libraries, with a run format of 26 cycles for read 1, 8 cycles for index 1, and 124 cycles for read 2. For data analysis, we installed the R packages ‘Seurat’ version 4.4.0, ‘dplyr’, and ‘cowplot’ (version 4.3.1). We utilized these tools to filter low-quality cells based on a minimum of 200 and a maximum of 7000 genes per cell and removed cells with more than 10% of the mitochondrial genome. The “RunUMAP” function was used to cluster the cells, with the principal components determined by the “JackStrawPlot” and “ElbowPlot” functions. Cluster signature genes were identified using the “FindAllMarkers” function, and differentially expressed genes were identified for selected cell clusters between different groups using the “FindMarkers” function. The “DoHeatmap” function was used to display the top signature genes in each cluster, while “VlnPlot” and “DotPlot” functions were used to examine the expression profiles of selected genes across cell clusters. Relative cell type abundance was visualized with the R package ‘ggplot2’ (version 3.4.3).
2.2. Gene Signatures
Inflammation-signature-associated genes, including Ifng, Ifngr1, Ifngr2, Il10, Il12a, Il12b, Il12rb1, Il12rb2, Il13, Il17a, Il18, Il18r1, Il1a, Il1b, Il2, Il21, Il21r, Il22, Il23a, Il23r, Il2rg, Il4, Il5, Il6, Jun, Rela, Rora, Rorc, S100a8, S100a9, Stat1, Stat3, Stat4, Stat6, Tgfb1, Tgfb2, Tgfb3, and Tnf, were obtained from a previous publication [23].
Neutrophil-related functions, including immunosuppression (Havcr2, Fcgr2b, Il4ra, Cd274, Hif1a), ECM remodeling (Adamdec1, Ctsc, Ctsb, Rgcc, Ctss, Ctsz, Adam17, Adam10, Adam8), tumor proliferation (Tgfb1, Tnf, Il1a), myeloid cell recruitment (Ccl3, Mif, Cxcl14, Csf1, Vegfa, Ccl4, Cxcl3), angiogenesis (Vegfa, Snd1, Mtdh, Itga5, Tnf, Cxcl3, Anxa3, Hmgb1, Hif1a, Sema4d, Lrg1, Chil1), neutrophil degranulation (Abr, Anxa3, Cd177, Itgam, Itgb2, Itgb2l, Pikfyve, Pram1, Ptafr, Spi1, Stx11, Syk), neutrophil cytotoxicity (Ncf1, Myd88, Trem3, Trem1, Tusc2, Cybb, Cybc1, Ncf2, Ncf4, Rac1, Rac2), interferon signaling (Adar, Isg15, Isg20, Rsad2, Ifit1, Ifit3, Ifitm1, Ifitm3, Irak1, Oas3, Stat1, Stat2, Irf7, Cxcl10), were obtained from a previous publication [24]. All obtained calculation results are visualized through the “ggboxplot” function.
2.3. Gene Set Enrichment Analysis (GSEA)
We utilized the “Wilcoxauc” function to compute cell groups and obtained gene markers for each group. These markers were then compared using the HALLMARK category from the Molecular Signatures Database (MSigDB) gene sets. Following this, we conducted GSEA analysis using the package ‘fgsea’ (version 1.26.0), and the outcomes were presented using ‘ggplot2’ (version 3.4.3), pathway heatmaps, and correlations visualized using the ‘dittoSeq’ package (version 1.12.1).
2.4. The Cancer Genome Atlas (TCGA) Data
We obtained TCGA data of a pancreatic cancer cohort from the cBioPortal database and identified cases with TP53 truncating mutations as p53 loss (loss-of-function) in the context of KRAS G12* mutations. In comparison, we also identified cases with TP53 mutations including R175H, R248Q, R248W, R273C, R273H, G245S, H179R, Y163C, Y220C, Y234C, G249, and R282 as p53 gain-of-function mutations [19,20] in the context of the KRAS G12* mutations. We then compared the mRNA expression levels of selected genes between p53 loss and p53 mutation groups. The heatmaps was visualized using the ‘pheatmap’ package (version 1.0.12) after standardization and “ward.D2” clustering_method treatment. In addition, the above data together with patient survival data were analyzed using the log-rank (Mantel–Cox) test.
2.5. Statistical Analysis
Statistical analyses of mRNA expression between p53 loss and p53 mutation were performed with unpaired, one-tailed t-test using GraphPad Prism (GraphPad Software, Prism 10). The expression data of indicated genes among TCGA pancreatic adenocarcinoma patient samples were based on the RNA Seq V2 RSEM data. TCGA data were downloaded from the cBioPortal database [25,26]. A p value < 0.05 was considered statistically significant. Error bars represent standard error of the mean (S.E.M.).
3. Results
3.1. Single-Cell Analysis Reveals Unique Differences in the Composition and Genomic Profile of Cell Populations between the KPmut and KPloss Pancreatic Tumors
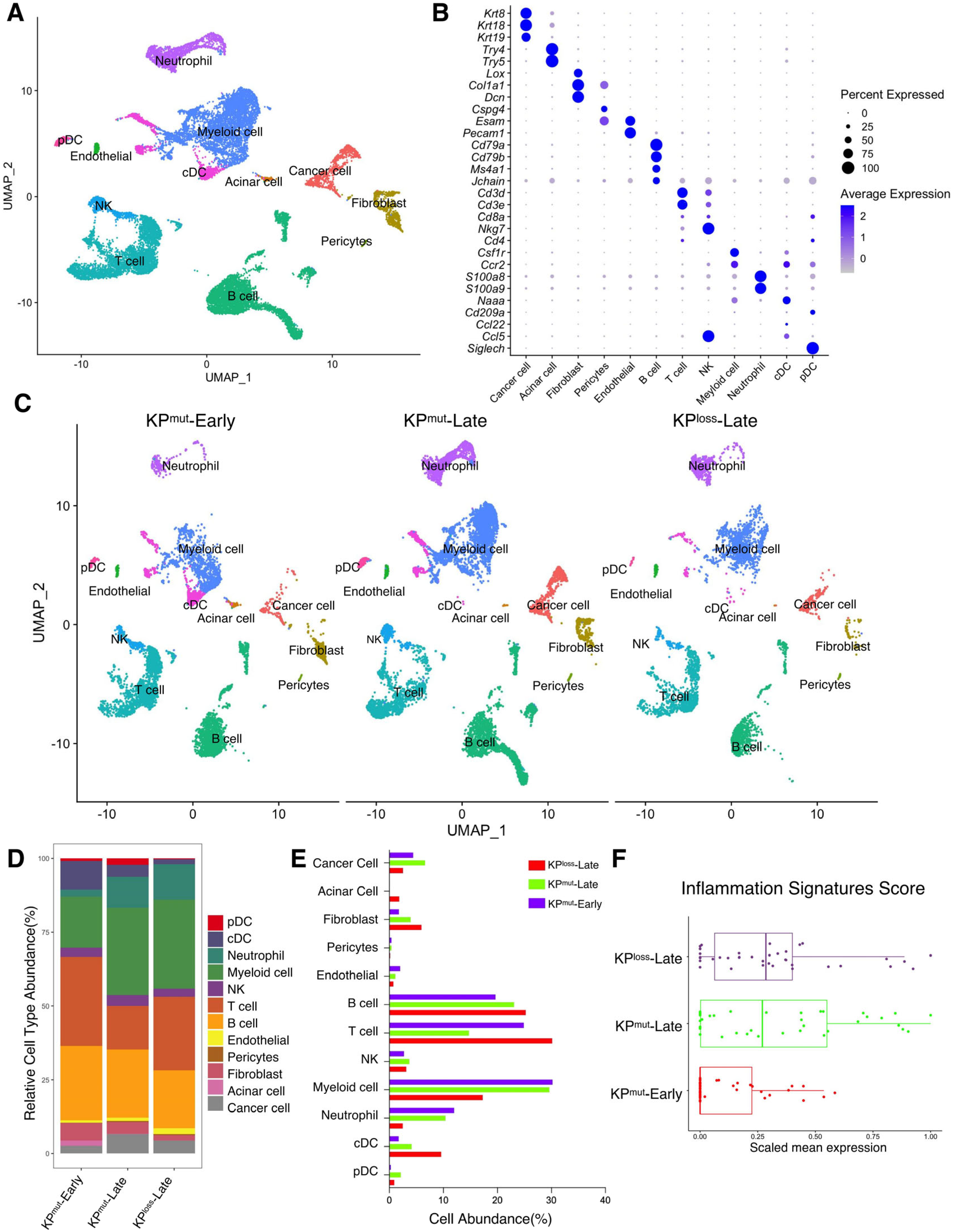
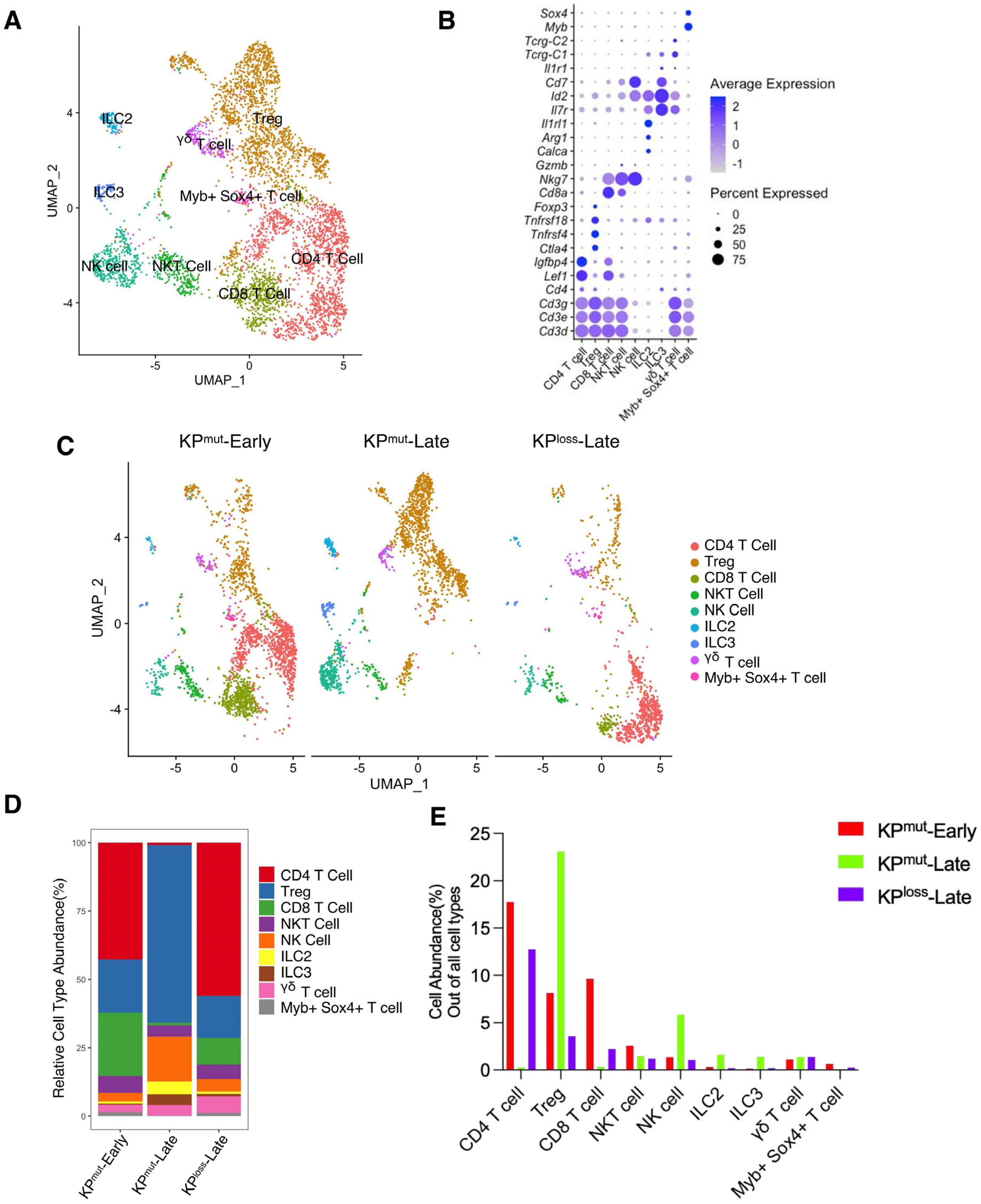
First, we included our recently published single-cell RNA-sequencing (scRNA-seq) datasets [10,11] to compare two mouse models with autochthonous pancreatic ductal adenocarcinoma (PDAC): the KPmut (KrasG12D; Trp53R172H) mouse model with KRASG12D mutation and p53R172H mutation, as compared to the KPloss (KrasG12D; Trp53cKO) mouse model with KRASG12D mutation and p53 loss (Figure 1A,B). We then compared the primary tumors across various cell types from early-stage KPC mice (KPmut-Early), late-stage KPC mice (KPmut-Late), and late-stage KPPF mice (KPloss-Late) (Figure 1C). Our analysis revealed significant differences in the composition of major cell populations between the KPmut-Early, KPmut-Late, and KPloss-Late (Figure 1D,E). As PDAC progressed in the contexts of different p53 alterations, the composition of cancer cell subpopulations significantly altered. Notably, a unique cancer cell subtype was present in the tumors of KPmut-Late mice but not KPloss-Late mice (Figure 1C). Cell number and phenotype alterations in neutrophils, fibroblasts, and other cell types were also observed (Figure 1C–E). T and B cell numbers were relatively high in KPmut-Early tumors and significantly decreased in KPmut-Late and KPloss-Late tumors (Figure 1D,E). Myeloid cell numbers in KPmut-Late and KPloss-Late were far beyond the KPmut-Early (Figure 1D,E). These results indicate that decreased lymphocyte number and increased myeloid cell number are associated with late-stage PDAC regardless of p53 alteration subtypes. Additionally, we utilized a recently reported methodology of analyzing the inflammation-related signals [23] and observed a significant increase in inflammation scores in KPmut-Late and KPloss-Late samples (Figure 1F), indicating the enrichment of inflammation-related signals in late-stage tumors but not in early-stage tumors.
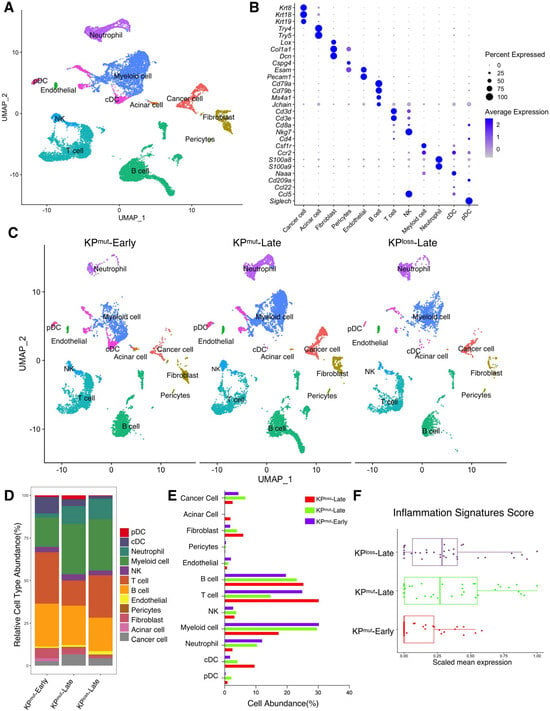
Figure 1.
Single-cell RNA-sequencing (scRNA-seq) analysis identifies distinct compositions of cell populations in oncogenic KRAS-driven pancreatic tumors with different p53 status. (A,B) scRNA-seq analysis of unfractionated live cell mixture from oncogenic KRASG12D-driven PDAC tumors with either p53 mutation (KPmut group) or p53 loss (KPloss group), as published in our previous datasets (GSE198815 and GSE166298). The major cell clusters are shown in a UMAP plot (A). (B) Dot plot showing the normalized expression of pre-defined marker genes for defined cell clusters. (C) UMAP plot that compares the cellular compositions of three groups of transgene mice (n = 3 per group): early-stage primary tumors (KPmut-Early), late-stage primary tumors (KPmut-Late), and late-stage p53 loss tumors (KPloss-Late). (D) Cell-type abundance of all captured cells across KPmut-Early, KPmut-Late, and KPloss-Late groups. (E) Abundance (%) of cell types across KPmut-Early, KPmut-Late, and KPloss-Late groups. (F) Scaled mean expression of inflammation signatures (n = 38) in cells from various groups. The median (horizontal line), second to third quartiles (box), and Tukey-style whiskers (beyond the box) are represented by the boxes. The dots denote the individual signatures. cDC, conventional dendritic cell; pDC, plasmacytoid dendritic cell; G-MDSC, granulocytic myeloid-derived suppressor cell; Gran-Mo progenitor, granulocyte-monocyte progenitor cell.
3.2. KPmut-Late Mice Harbor a Unique Cancer Cell Subcluster as Compared to KPloss-Late Mice (or KPmut-Early Mice)
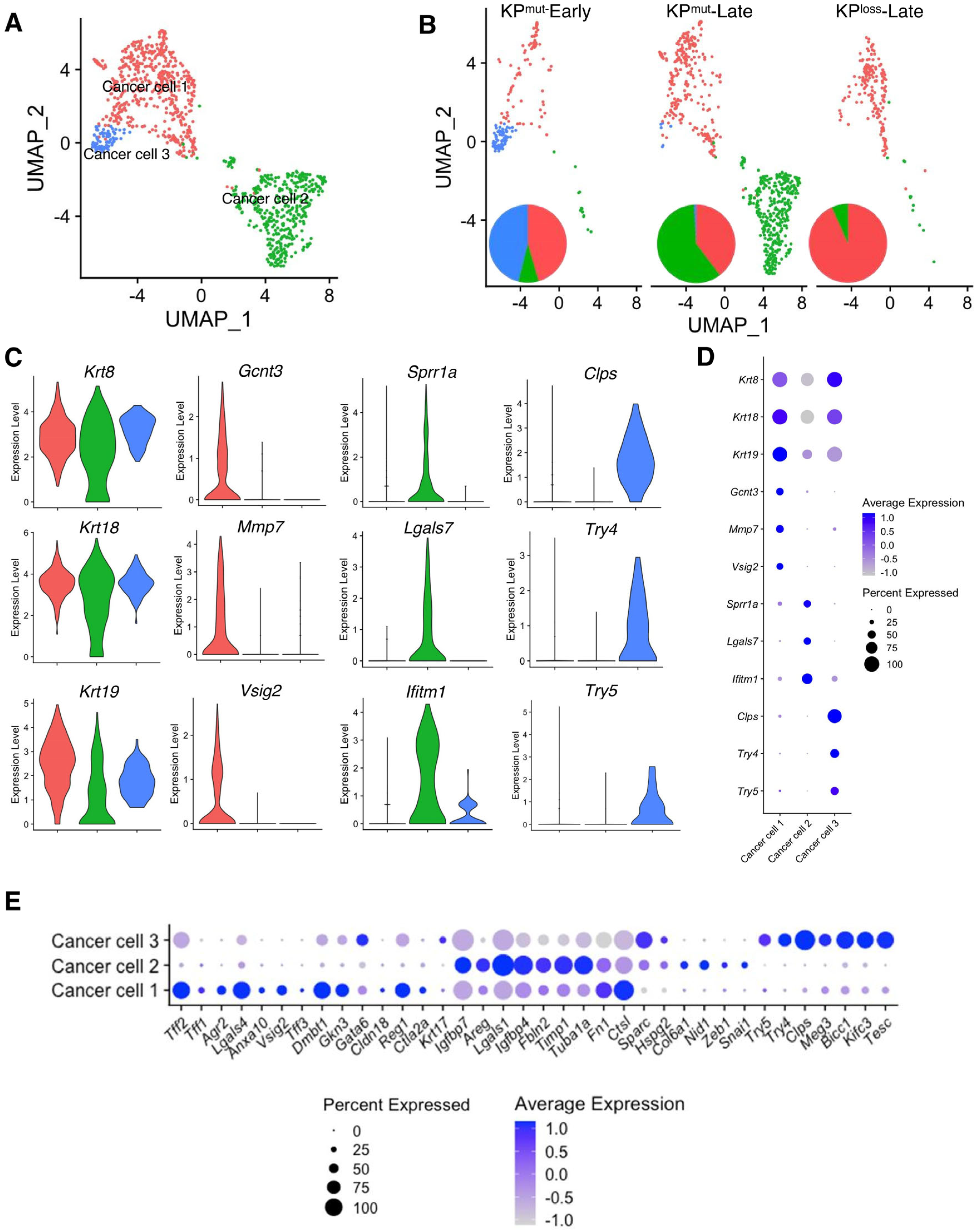
Based on our analysis, we have identified three distinct subclusters of cancer cells, namely ‘Cancer cell 1’, ‘Cancer cell 2’, and ‘Cancer cell 3’, as shown in Figure 2A. Specifically, Cancer cell 1 was present in all three groups, as the predominant cancer cell subtype in KPmut-Early and KPloss-Late tumors (Figure 2B). Cancer cell 2 was mainly enriched in KPmut-Late tumors, whereas Cancer cell 3 was mainly enriched in KPmut-Early tumors (Figure 2B). To further investigate the similarities and differences between these three subpopulations of cancer cells, we analyzed the marker genes of these cancer cell subtypes. As expected, all three subtypes of cancer cells expressed the generic pancreatic cancer cell marker genes, such as Krt8 and Krt18 (Figure 2C,D). Specifically, Cancer cell 1 expressed Gcnt3, Mmp7, and Vsig2, which are associated with the epithelial/classical subtype of pancreatic cancer cells [27,28,29] (Figure 2C,D). Cancer cell 2 expressed Sprr1a, Lgals7, and Ifitm1, which are associated with the mesenchymal/basal-like subtype and a poor prognosis in PDAC [30,31,32]. Cancer cell 3 represented the early-stage cancer-initiating cells with the expression of acinar cell genes such as Clps, Try4, and Try5 (Figure 2C,D), as well as epithelial marker genes such as Epcam and Cdh1 (Supplementary Figure S1A).
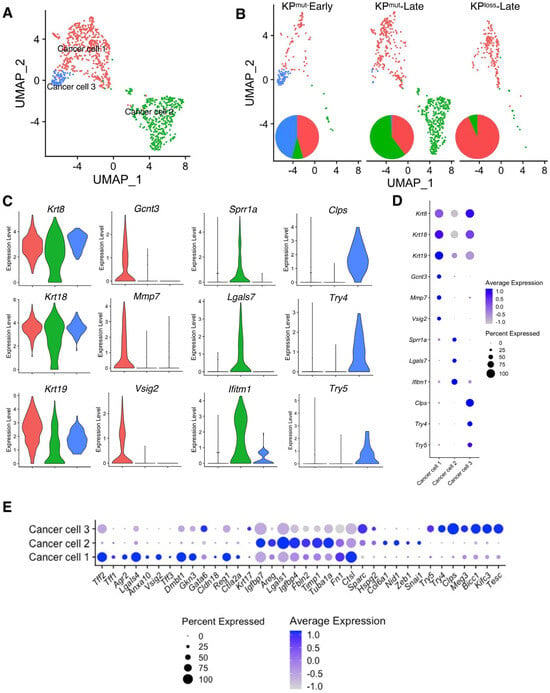
Figure 2.
Cancer cell subpopulations are different between KPmut and KPloss pancreatic tumors. (A,B) Cancer cells from KPmut-Early, KPmut-Late, and KPloss-Late groups are stratified into three distinct subclusters in the UMAP plot (A) and compared across three groups (B). The pie charts also show the changes in cancer cell subcluster composition among the three groups. (C,D) Expression profiles of signature genes for the cancer cell subpopulations, shown as violin plots (C) and dot plots (D). (E) The cancer cell subpopulations were examined for expression profiles of genes associated with the definition of classical and basal-like cancer cell subtypes, as shown in dot plots. Acinar-like signature genes are also shown in comparison with classical and basal-like signature genes.
To establish a correlation between cancer cell subclusters and PDAC subtypes [32], we analyzed the expression profiles of signature genes associated with the classical and basal-like subtypes (Figure 2E, Supplementary Figure S1B,C). In particular, Cancer cell 1 (enriched in KPloss-Late tumors) exhibited high expression levels of classical subtype genes such as Lgals4, Dmbt1, Agr2, Tff2, and Vsig2. Cancer cell 2 expressed high levels of mesenchymal/basal-like subtype genes including Lgals1, Fbln2, Timp1, and Areg. Furthermore, GSEA revealed differentially enriched pathways of the three cancer cell subtypes. Specifically, Cancer cell 1 subcluster highly expressed the signature genes of Interferon α, Interferon γ, KRAS, and p53 pathways, while the MYC pathway was downregulated. Cancer cell 2 subcluster highly expressed the signature genes of MYC target v1, MYC target v2, and oxidative phosphorylation pathways. Cancer cell 3 subcluster highly expressed the signature genes of Interferon α, Interferon γ, and KRAS pathways, which were also observed in Cancer cell 1 (Supplementary Figure S2). In summary, these results revealed that the cancer cells of KPloss-Late tumors exhibit an enriched epithelial/classical phenotype, which was similar to that of KPmut-Early tumors. In contrast, the cancer cells of KPmut-Late tumor exhibit enriched subcluster with mesenchymal/basal-like phenotype.
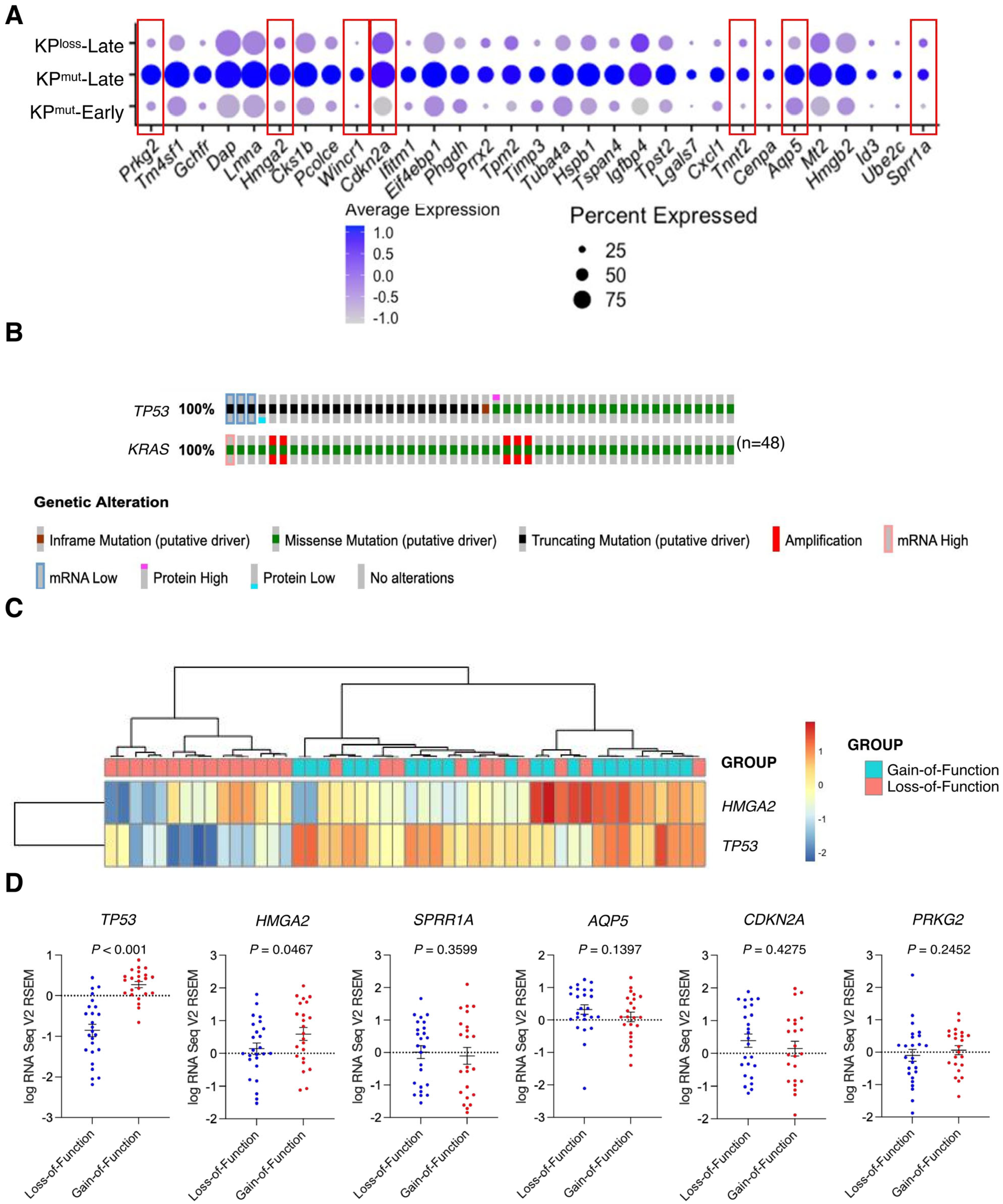
3.3. Tumors with p53 Mutation Reveal Elevated Expression of HMGA2 in Cancer Cells as Compared to Tumors with p53 Loss
Further analysis on cancer cell-specific genes revealed that KPmut-Late tumors exhibit elevated expression levels of several genes, including Prkg2, Hmga2, Wincr1, Cdkn2a, Tnnt2, Aqp5, and Sprr1 (Figure 3A). Notably, these genes were upregulated specifically in cancer cells (Supplementary Figure S3A). Next, we utilized the TCGA database to compare the gene profiles of human PDAC with p53 mutation or p53 loss. We selected those patient samples with KRAS G12 mutations and then stratified them into two groups (with either p53 mutation or p53 loss). Based on the genetic alterations of TP53, the gain-of-function mutations were categorized as p53 mutation (n = 23), while the loss-of-function and truncating mutations were classified as p53 loss (n = 25) (Figure 3B). Further analysis of the TCGA pancreatic cancer dataset revealed that p53 gain-of-function mutations were associated with moderately worse survival of patients, as compared with p53 loss-of-function mutations (Supplementary Figure S3B). The expression of HMGA2 in the TCGA database and the expression of Hmga2 in our single-cell RNA-sequencing data were consistently upregulated in p53 mutant tumors, as compared to p53 loss tumors (Figure 3C,D). As expected, we also observed a significant decrease of TP53 expression in the p53 loss cases as compared to p53 mutation cases (Figure 3D). These findings suggested the distinct genetic variances of p53 mutation and p53 loss might impact the phenotypes of both the cancer cells and their microenvironment.
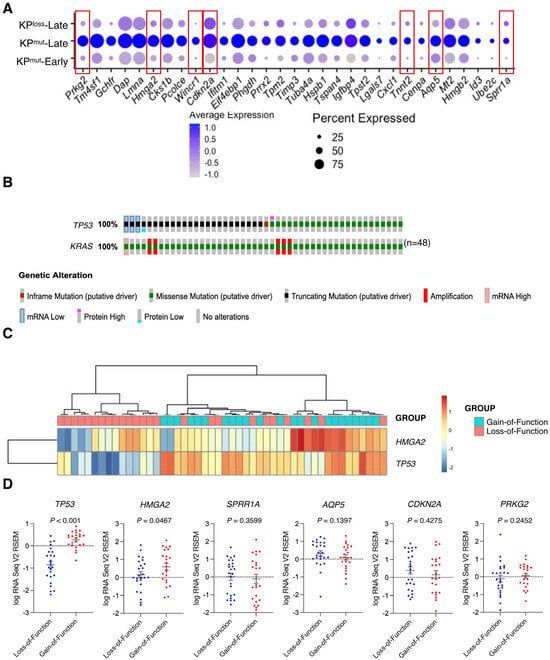
Figure 3.
Differentially expressed genes (DEGs) are identified by comparing cancer cells from KPmut-Late with cancer cells from KPmut-Early and KPloss-Late groups. (A) Expression profiles of indicated marker genes in cancer cells from various groups are shown in a dot plot. Cancer cell-specific genes with elevated expression levels in KPmut-Late group were indicated by red boxes. (B) Samples from TCGA pancreatic cancer cohort with indicated (either loss-of-function or gain-of-function) TP53 mutations together with KRAS G12* mutations. (C) Heatmap showing the expression of selected marker genes in PDAC samples with loss-of-function or gain-of-function p53 mutations from the TCGA pancreatic cancer cohort. (D) Expression profiles of selected marker genes in PDAC samples with loss-of-function or gain-of-function p53 mutations. Statistical differences between groups in panel (D) were assessed by t-test.
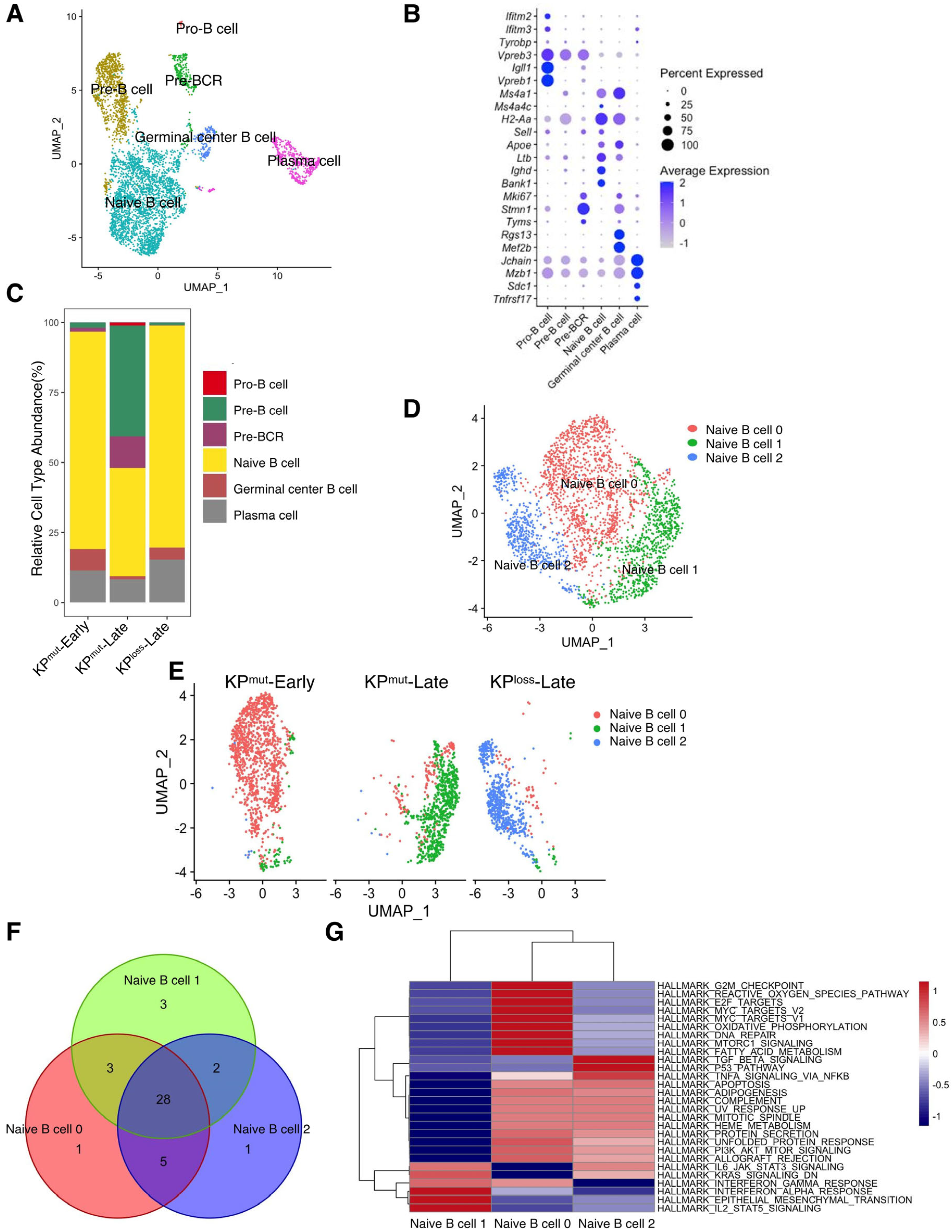
3.4. Compositions of B Cells and T Cells Vary among KPmut-Early, KPmut-Late, and KPloss-Late Tumors
According to our previous results, p53 mutation and loss may differentially regulate the phenotypes of cancer cells and the tumor microenvironment. Therefore, we further compared the alterations in immune cell profiles between KPmut tumors and KPloss tumors. We observed that the B cells in KPmut tumors exhibited different phenotypes from those in KPloss tumors (Figure 4A). We divided B cells into Pro-B cell, Pre-B cell, Pre-BCR, Naive B cell, Germinal center B cell, and Plasma cell based on the reported signature genes (Figure 4A,B) [33,34,35,36,37,38]. Subsequently, the B cell compositions of the KPmut-Early, KPmut-Late, and KPloss-Late groups were analyzed (Figure 4C). We observed that KPmut-Late tumors had higher numbers of Pro-B cells, Pre-B cells, and Pre-BCR than KPloss-Late tumors (or KPmut-Early tumors). Pro-B cells, Pre-B cells, and Pre-BCR were hardly detectable in KPloss-Late tumors or KPmut-Early tumors. Notably, all three groups of mice contained a considerable amount of naïve B cells (Figure 4C). Upon further analysis, we discovered distinct states of naïve B cells in three types of mice: naïve B cell 0, naïve B cell 1, and naïve B cell 2, present in the KPmut-Early, KPmut-Late, and KPloss-Late groups, respectively (Figure 4D,E). Through extensive GSEA analysis, we identified 28 overlapping pathways among these naïve B cell subtypes. Subsequent differential analysis revealed the similarities between naïve B cell 0 and naïve B cell 2 (Figure 4F,G). These results indicated that the expression profile of B cells in KPloss-Late tumors is more analogous to that in KPmut-Early tumors, which is distinct from that in KPloss-Late tumors.
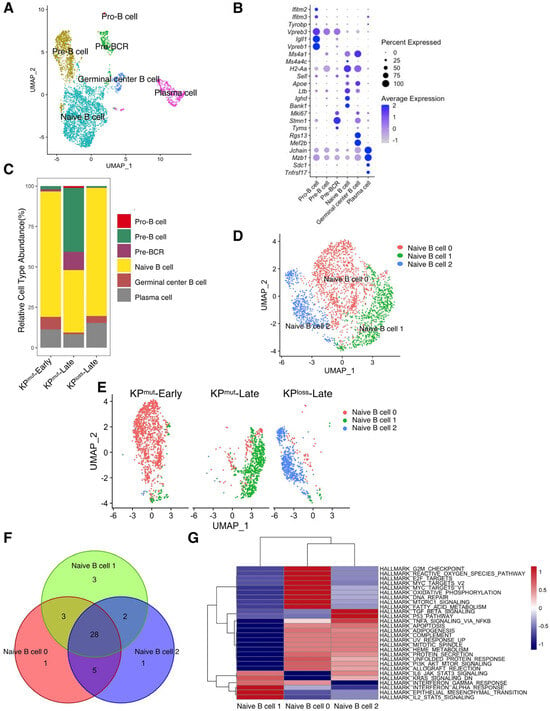
Figure 4.
Comparing B cell subtype compositions in KPmut-Early, KPmut-Late, and KPloss-Late tumors. (A,B) B cells from KPmut-Early, KPmut-Late, and KPloss-Late tumors are segregated into distinct subclusters in the UMAP plot (A) based on the diverse expression profiles of signature genes depicted in the dot plot (B). (C) B cell-subtype abundance across KPmut-Early, KPmut-Late, and KPloss-Late groups. (D) Naïve B cells from KPmut-Early, KPmut-Late, and KPloss-Late are segregated into distinct subclusters in the UMAP plot. (E) UMAP plot comparing the Naïve B cell compositions of three groups. (F) Venn diagram of the GSEA across naive B cell subtypes. (G) Heatmap of the GSEA across three Naïve B cell subtypes.
We also analyzed the cell composition of T cell subclusters (Figure 5A,B). In general, the T cell population of KPmut-Late tumors was predominantly composed of regulatory T cells (Tregs; FOXP3+CD4+), with a small proportion of NK cells. In contrast, the T cell population in KPloss-Late tumors was primarily composed of CD4+FOXP3 T cells, followed by Tregs and CD8+ T cells. Interestingly, the numbers of innate lymphoid cell subclusters, ILC2 and ILC3, increased in KPmut-Late tumors, which merits further investigation to determine the underlying mechanism. To summarize, T cells revealed distinct subtype composition patterns between KPmut-Late and KPloss-Late tumors.
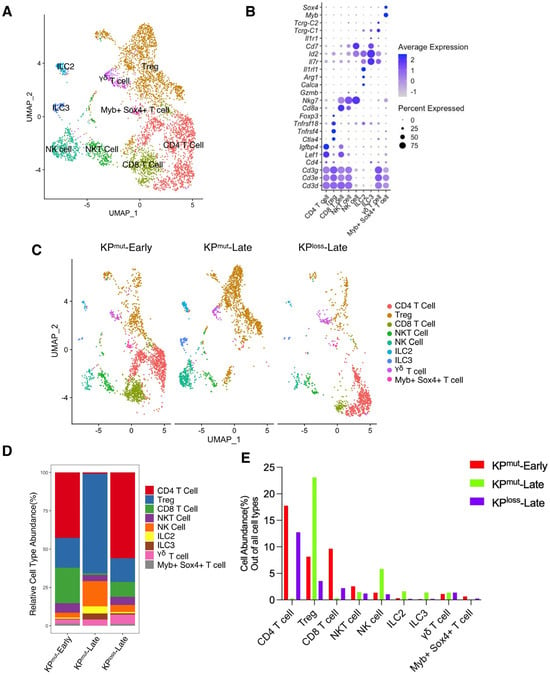
Figure 5.
Subpopulation compositions of T cells and NK cells in KPmut-Early, KPmut-Late, and KPloss-Late tumors. (A,B) T cells and NK cells from KPmut-Early, KPmut-Late, and KPloss-Late tumors are classified into distinct subclusters in the UMAP plot (A) based on the diverse expression profiles of signature genes depicted in the dot plot (B). (C) UMAP plot comparing the T cells and NK cells compositions across three groups. (D) T and NK cell subtype abundance across KPmut-Early, KPmut-Late, and KPloss-Late groups. (E) abundance (%) of T and NK cells across KPmut-Early, KPmut-Late, and KPloss-Late groups.
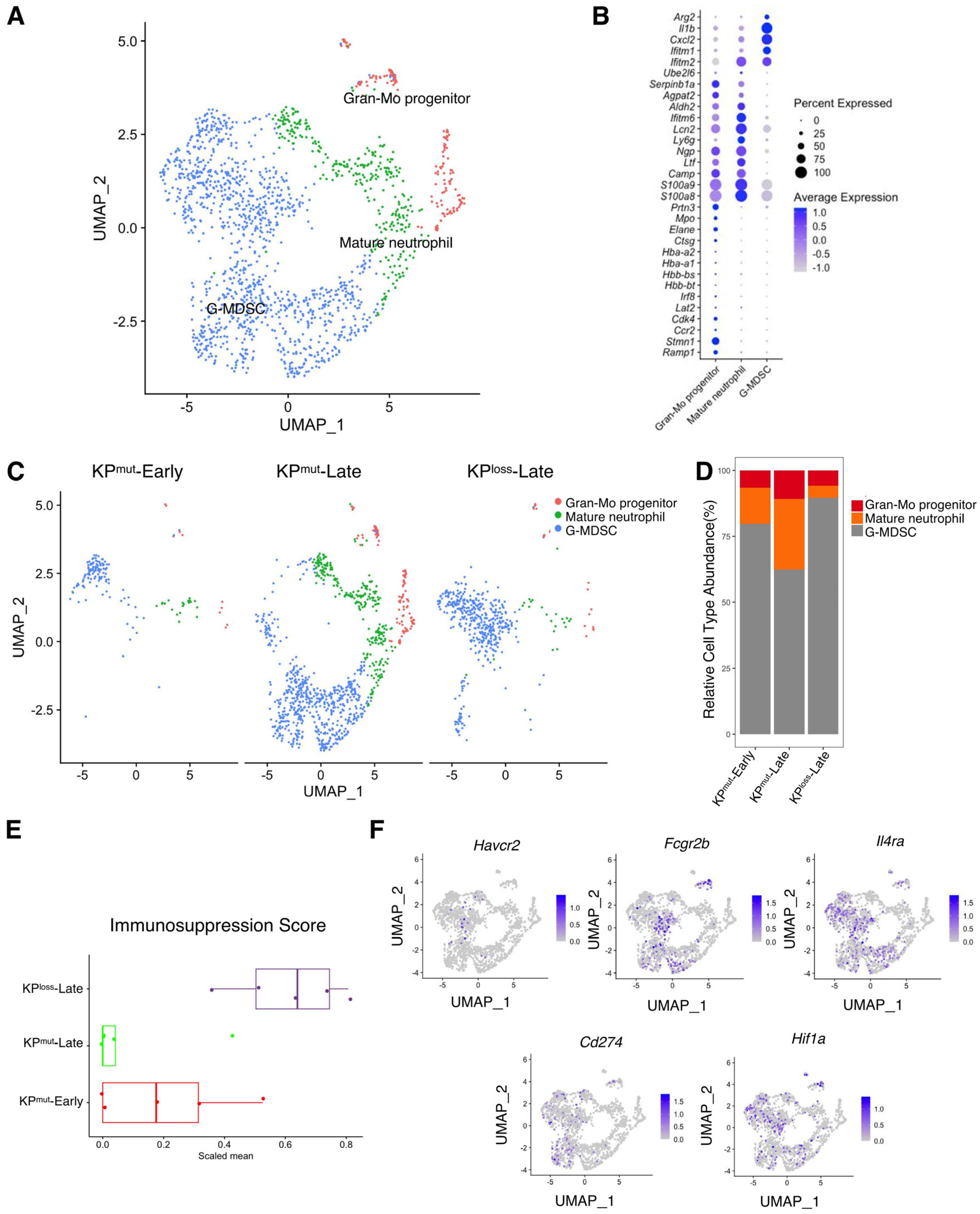
3.5. Neutrophil Subpopulations Differ among KPmut-Early, KPmut-Late, and KPloss-Late Tumors
We next analyzed the differences in neutrophils across KPmut-Early, KPmut-Late, and KPloss-Late tumors. We stratified the total granulocyte/neutrophil population into three subclusters: Gran-Mo progenitor, G-MDSC, and Mature neutrophil (Figure 6A,B). We observed that KPmut-Late tumors exhibited the presence of Gran-Mo progenitor, G-MDSC, and Mature neutrophil. In contrast, KPloss-Late tumors and KPmut-Early tumors exhibited a predominant presence of G-MDSC (Figure 6C,D). These findings provide valuable insights into the cellular components of the samples and can aid in further research endeavors. Based on a recently published methodology [24], we analyzed the signature scores of neutrophils in tumors. We observed that the immunosuppression signature of tumor-associated neutrophils was significantly upregulated in KPloss-Late tumors but was downregulated in KPmut-Late tumors (Figure 6E,F). Notably, KPloss-Late tumors exhibited similar profiles to KPmut-Early tumors in terms of pathways including angiogenesis, ECM remodeling, myeloid cell recruitment, proliferation, and neutrophil cytotoxicity, while KPmut-Late tumors revealed downregulation of several of the aforementioned pathways (Supplementary Figure S4).
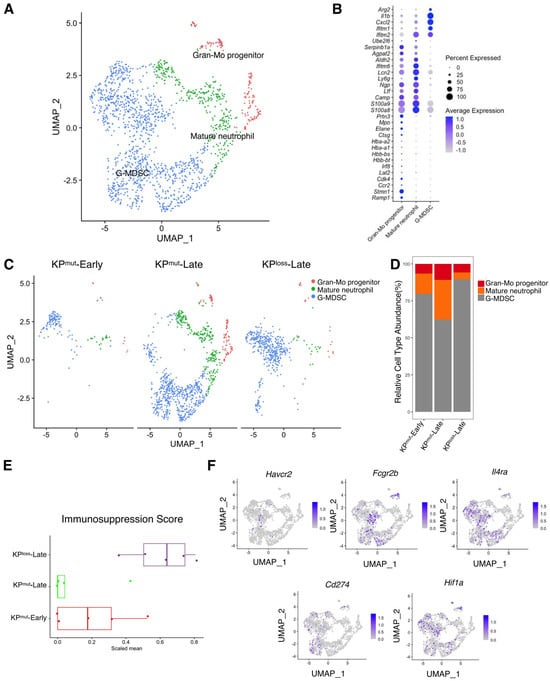
Figure 6.
Similarities and differences of neutrophil subclusters across KPmut-Early, KPmut-Late, and KPloss-Late tumors. (A,B) Neutrophils from KPmut-Early, KPmut-Late, and KPloss-Late tumors are segregated into distinct subclusters in the UMAP plot (A) based on the diverse expression profiles of signature genes depicted in the dot plot (B). (C) The UMAP plot compares the neutrophil compositions across KPmut-Early, KPmut-Late, and KPloss-Late groups. (D) Neutrophil subtype abundance across KPmut-Early, KPmut-Late, and KPloss-Late groups. (E) Scaled mean expression of immunosuppression signatures (n = 5) in cells from various groups. The median (horizontal line), second to third quartiles (box), and Tukey-style whiskers (beyond the box) are represented by the boxes. The dots denote the individual signatures. (F) Immunosuppression-related genes (Havcr2, Fcgr2b, Il4ra, Cd274, Hif1a) are characterized in a UMAP plot.
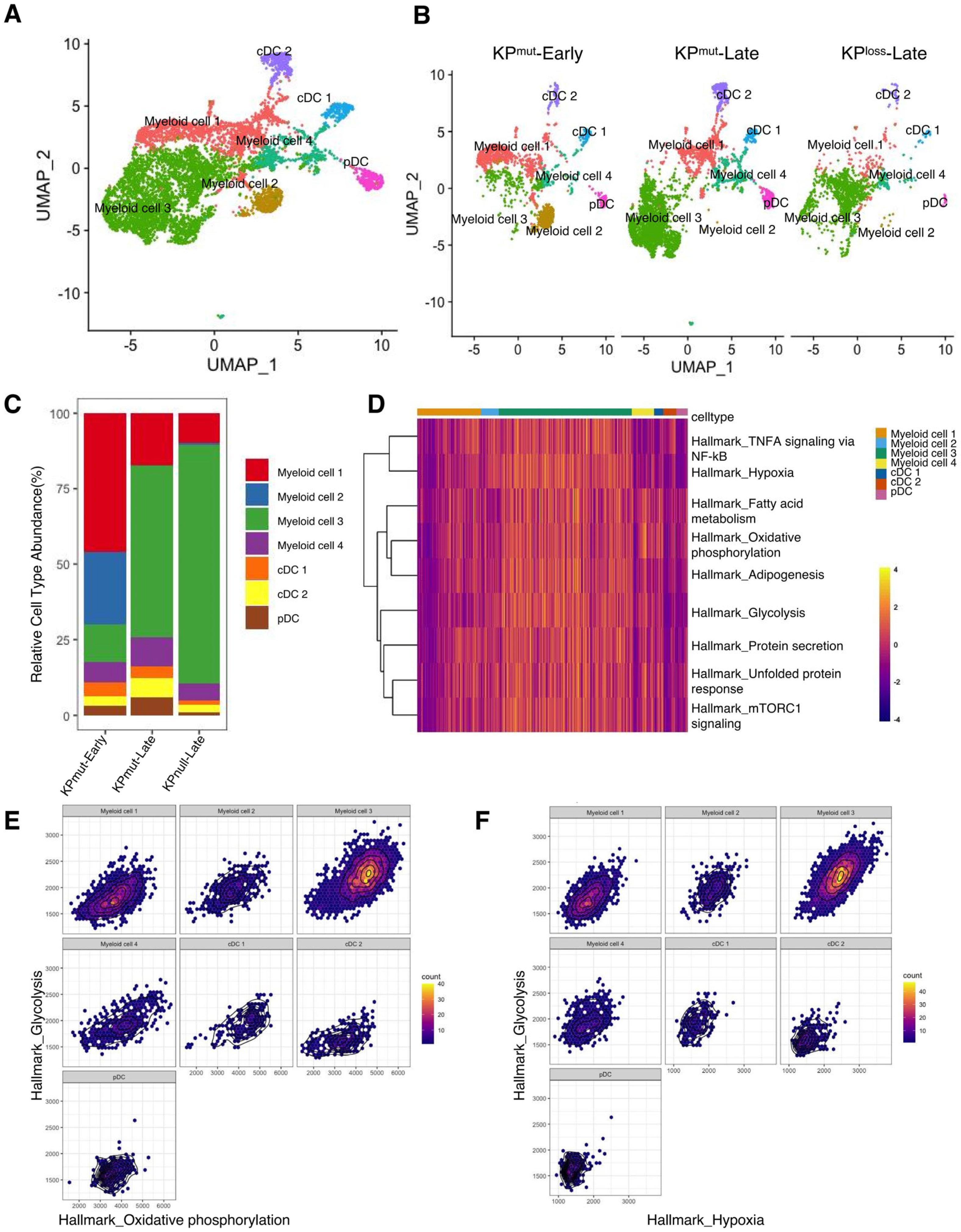
3.6. KPmut-Early, KPmut-Late, and KPloss-Late Tumors Reveal Different Compositions of Myeloid Cell and Dendritic Cell (DC) Subclusters
Next, we plotted the signature genes of myeloid cells and DCs (Figure 7A,B). Myeloid cells could be categorized into four subclusters: myeloid cell 1, myeloid cell 2, myeloid cell 3, and myeloid cell 4. Meanwhile, DCs were divided into cDC1, cDC2, and pDC. Notably, myeloid cell 1 exhibited higher levels of H2-Aa, H2-Ab1, and Cd74, while myeloid cell 2 displayed elevated expression of Retnla and Fcrls. Myeloid cell 3 presented higher levels of Arg1, Hilpda, Serpine1, Rnase2a, Chil3, while myeloid cell 4 had lower levels of Csf1r, Mrc1, C1qa, C1qb, and C1qc, but highly expressed Hp, Ifitm6, Gpr141, and Ms4a4c. Moreover, both myeloid cell 3 and myeloid cell 4 expressed Mmp8 and Vcan. Lastly, cDCs were primarily divided into cDC1 with high expression of Naaa and cDC2 with high expression of Ccl22/Ccl5 (Supplementary Figure S5A). We observed a higher proportion of Myeloid cell 3 in both KPmut-Late and KPloss-Late (Figure 7C). GSEA identified that myeloid cell 3 subcluster has upregulated pathways including Oxidative_phosphorylation, Glycolysis, Fatty acid metabolism, mTORC1 signaling, Unfolded protein response, Protein secretion, Adipogenesis, TNFA signaling via NF-kB (Figure 7D and Supplementary Figure S5B). Further analysis showed that glycolysis in myeloid cell 3 has a strong positive correlation with both oxidative phosphorylation and hypoxia (Figure 7E,F and Supplementary Figure S5C,D). Recent studies reported that monocytes can simultaneously increase the efficiency of glycolysis and oxidative phosphorylation under the stimulation of low concentrations of LPS [39]. However, the exact role of these cellular functions in tumors warrants further exploration.
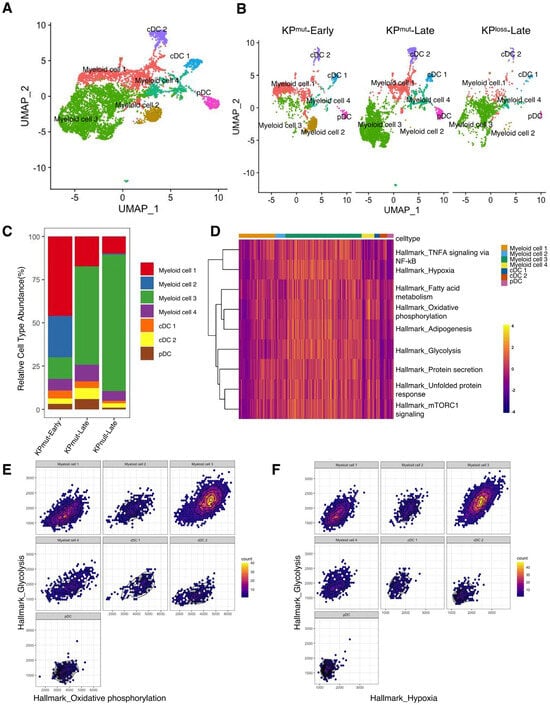
Figure 7.
Compositions of myeloid cells and dendritic cells (DCs) in KPmut-Early, KPmut-Late, and KPloss-Late tumors. (A,B) Myeloid cells and DCs from KPmut-Early, KPmut-Late, and KPloss-Late tumors are segregated into distinct subclusters in the UMAP plot(A) and compared across the groups (B). (C) Myeloid cell and DC subtype abundance across KPmut-Early, KPmut-Late, and KPloss-Late groups. (D) Heatmap showing the expression profile of ‘Myeloid cell 3’-associated GSEA pathways in myeloid cell and DC subpopulations. (E) Relationship between Hallmark_glycolysis and Hallmark_oxidative_phosphorylation examined in myeloid cell and DC subtypes. (F) Correlation between Hallmark_glycolysis and Hallmark_hypoxia in myeloid cell and DC subtypes.
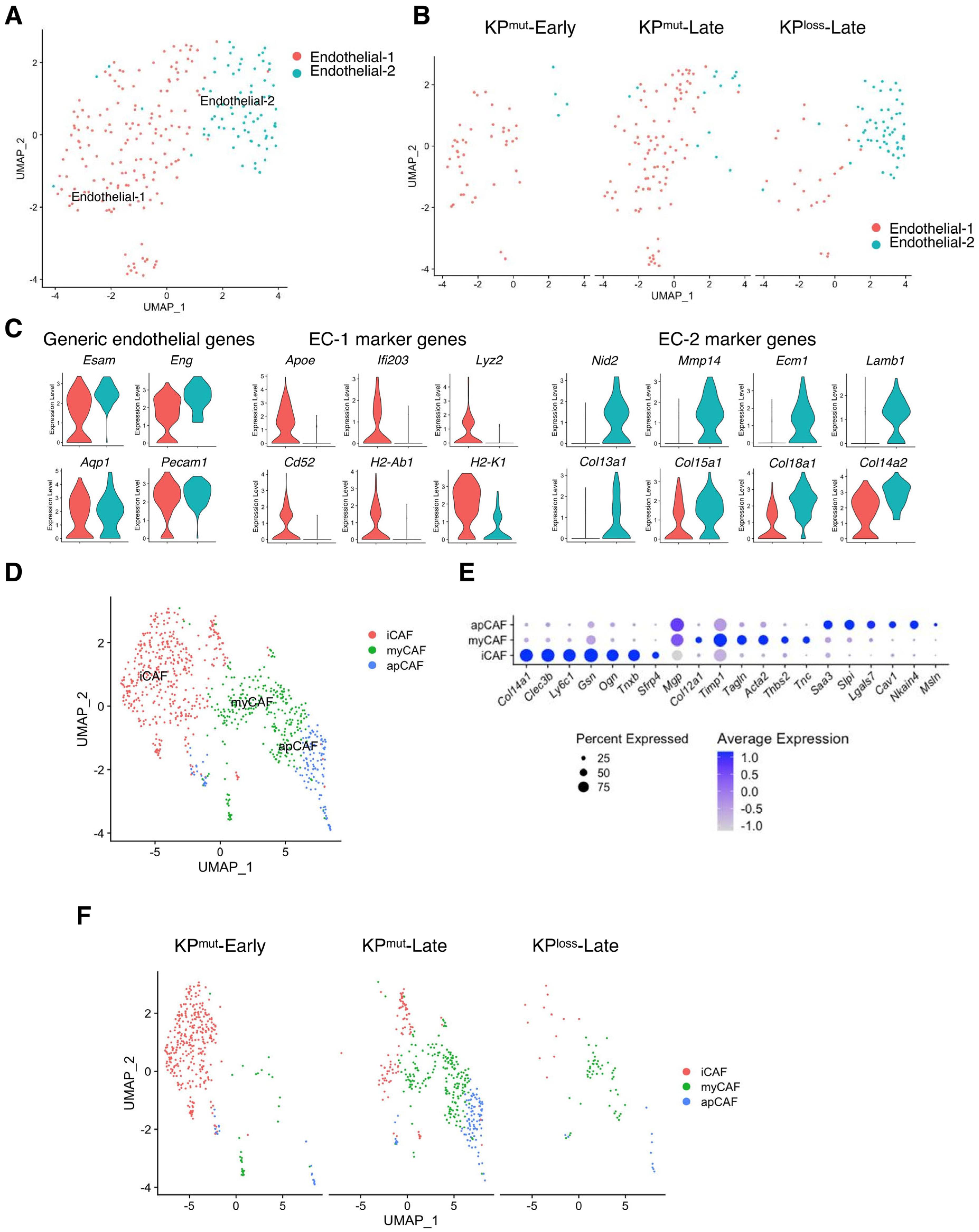
3.7. Compositions of Endothelial Cells and Fibroblasts Vary among KPmut-Early, KPmut-Late and KPloss-Late
We observed two distinct subpopulations of endothelial cells that result from p53 mutation and p53 loss, known as endothelial-1 (EC-1) and endothelial-2 (EC-2) (Figure 8A). EC-1 was primarily found in KPmut-Early and KPmut-Late with the expression of Apoe, Lyz2, and Cd52, while EC-2 was mainly found in KPloss-Late with the expression of Mmp14, Ecm1, Col13a, and Lamb (Figure 8B,C).
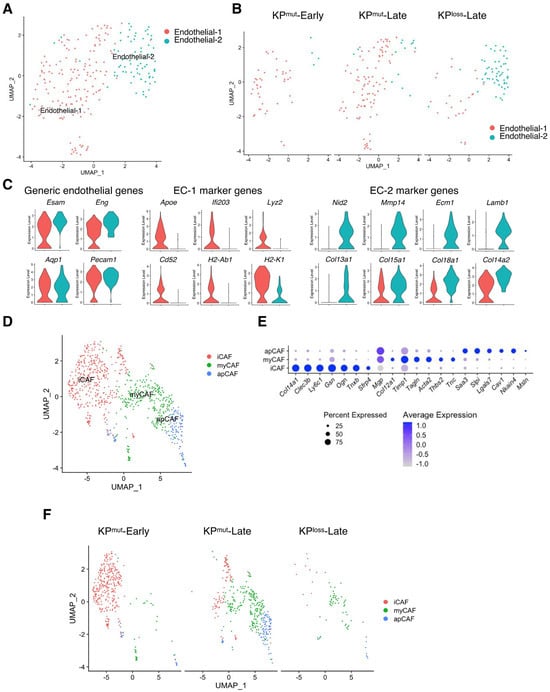
Figure 8.
Subclusters of endothelial cells and cancer-associated fibroblasts (CAFs) in KPmut-Early, KPmut-Late, and KPloss-Late tumors. (A,B) Endothelial cells from KPmut-Early, KPmut-Late, and KPloss-Late tumors are segregated into distinct subclusters in the UMAP plot (A) and compared across the groups (B). (C) Signature genes of endothelial cells from KPmut-Early, KPmut-Late, and KPloss-Late tumors shown in a violin plot. (D,E) Inflammatory CAFs (iCAF), myofibroblastic CAFs (myCAF), and antigen-presenting CAF (apCAF) subclusters are denoted. CAFs obtained from KPmut-Early, KPmut-Late, and KPloss-Late tumors are segregated into aforementioned subclusters in the UMAP plot (D) based on the diverse expression profiles of signature genes depicted in the dot plot (E). (F) UMAP plot comparing the CAF subtype compositions across three groups.
Next, we analyzed the compositions and related characteristics of cancer-associated fibroblasts (CAFs) KPmut-Early, KPmut-Late, and KPloss-Late tumors. CAFs were categorized based on specific marker genes [5] into three subtypes: inflammatory CAF (iCAF), myofibroblast (myCAF), and antigen-presenting CAF (apCAF) (Figure 8D,E). We observed that iCAF was predominantly present in KPmut-Early tumors, while myCAF and apCAF subtypes were enriched in KPmut-Late tumors (Figure 8F). The CAF subcluster composition between KPloss-Late tumors and KPmut-Late tumors was similar, although the total number of CAFs in KPloss-Late tumors was significantly lower than that in KPmut-Late tumors (Figure 8F). Taken together, our findings indicated that p53 loss and p53 mutation in pancreatic cancer cells differentially affect the subclusters of various cell populations such as endothelial cell, CAFs, and immune cells.
4. Discussion
Pancreatic cancer is one of the deadliest cancers worldwide and is refractory to most therapies, due to the complex nature of its tumor microenvironment [1]. As a result, extensive investigations are still required to elucidate the biology of the tumor microenvironment of pancreatic cancer. There are several oncogenic drivers that contribute to the development of pancreatic ductal adenocarcinoma (PDAC), including KRAS and p53 mutations. While oncogenic KRAS mutation is dominated by the KRAS G12* format in PDAC, p53 mutations can have either gain-of-function or loss-of-function alterations. Previous studies have shown that both gain-of-function or loss-of-function types of p53 mutations can occur in human pancreatic cancer and have distinct impacts on tumor progression [15,16]. Oncogenic effects are often observed in the gain-of-function p53 mutations, which are commonly found in R175H, R248Q, R248W, R273C, R273H, G245S, H179R, Y163C, Y220C, Y234C, G249, and R282 [19,20]. On the other hand, loss-of-function p53 mutations are associated with increased tumor penetrance and decreased life expectancy, as seen in the context of the p53 E224D mutant [40]. A recent study suggested that p53 loss induces ordered and deterministic cancer genome evolution [41]. Another study previously reported that the genotype plays a crucial role in modulating the tumor microenvironment of PDAC, leading to the induction of matricellular fibrosis and the progression of the tumor [42]. It is crucial to investigate the distinct effects induced by these oncogenic mutations on both cancer cells and the surrounding microenvironment, which may reveal potential vulnerabilities of PDAC that are associated with specific cancer genotypes.
Previous studies also demonstrated that gain-of-function p53 mutations can have significantly different oncogenic effects as compared to the loss-of-function p53 mutations [15,16]. Utilizing a single-cell technique and various transgenic mouse models, we can conduct an in-depth comparison of the tumor microenvironment components between p53-mutated and p53-loss pancreatic tumors, both in the context of oncogenic KRASG12D-driven PDAC. Our study focuses on identifying the transcriptomic alterations in various cell populations across early-stage p53-mutated (KPmut-Early) tumors, late-stage p53-mutated (KPmut-Late) tumors, and late-stage p53-loss (KPloss-Late) tumors.
The utilization of transgenic mouse models has dramatically facilitated the in-depth investigation on the complex biology of PDAC in the past decades. Transgenic mouse models of oncogenic KRAS-driven PDAC with either p53 mutation [43] or p53 loss [44,45,46] have been widely used by numerous studies. Both the p53-mutated KrasG12D; Trp53R172H (KPmut) mouse model and p53-loss KrasG12D; Trp53cKO (KPloss) mouse model are clinically relevant and can faithfully recapitulate human PDAC with distinct genotypes. The KPmut mouse model can recapitulate the human PDAC cases with KRASG12D mutation and p53R172H mutation (or other similar gain-of-function mutations), with 23 cases within the TCGA PDAC cohort as shown in this present study. In comparison, The KPloss mouse model can recapitulate the human PDAC cases with KRASG12D mutation and p53 loss-of-function mutations/truncations, with 25 cases within the TCGA PDAC cohort. The p53 loss-of-function mutations and truncations have been widely observed in various cancer types [47,48,49]. The previous findings are consistent with our results showing that patients with p53 gain-of-function mutations exhibit worse prognosis than patients with p53 loss-of-function mutations, based on the analysis of TCGA pancreatic cancer cohort data.
By integrating our recently published single-cell datasets [9,10,11,13], we compared the similarities and differences between p53-mutated (KPmut) and p53-loss (KPloss) tumors. Our analysis identified the enrichment of a mesenchymal/basal-like cancer cell subcluster in late-stage KPmut tumors, but not in late-stage KPloss tumors or early-stage KPmut tumors. Furthermore, our study has revealed that HMGA2 is upregulated in both mouse PDAC tumors of KPmut-Late mice and human PDAC samples with p53 mutations in TCGA dataset (p53 mutation group, n = 23; as compared to p53 loss group, n = 25). It has been reported that HMGA2 exhibits a strong association with tumor metastasis and growth [50]. Besides the Cancer cell 2 subpopulation uniquely enriched in KPloss tumors, we also identified a shared Cancer cell 1 subpopulation that is abundantly present in both KPloss tumors and KPmut tumors. These results indicate that this epithelial/classical Cancer cell 1 subpopulation is presumably the common cancer-initiating cell lineage during PDAC development.
Also, we observed similarities of many immune cell populations between KPmut and KPloss tumors. In fact, the overall cell population compositions and phenotypes were surprisingly similar between KPmut and KPloss mouse models, as revealed by scRNA-seq (Figure 1). These findings support the notion that both KPmut and KPloss mouse models are useful for studying the tumor microenvironment of PDAC, consistent with previous studies using both model systems [17,43,44,45,46]. Specifically, both KPmut-Late and KPloss-Late tumors exhibit significantly enriched immunosuppressive myeloid cells with high expression levels of Arg1 and Chil3, which resembles the phenotype of tumor-associated macrophage. These results indicate that the enrichment of immunosuppressive myeloid cells is likely a common feature associated with late-stage PDAC, despite the presence of p53 mutation or p53 loss. Despite the similar enrichment of myeloid cells in KPmut-Late and KPloss-Late tumors, the phenotype and composition of tumor-associated neutrophils in KPloss-Late tumors are significantly different from those in KPmut-Late tumors. Future studies are required to determine whether leveraging these myeloid cells and neutrophils can provide insights into new therapeutic strategies for PDAC.
5. Conclusions
To summarize, we conducted a thorough analysis across multiple datasets of scRNA-seq data to compare the tumor microenvironment of oncogenic KRAS-driven PDAC harboring p53 mutation or p53 loss. Our analyses uncovered distinctive phenotypic and transcriptional profiles of various cell populations in the context of p53 mutation as compared to p53 loss. We also identified the similarities in overall cell type compositions between KPmut and KPloss mouse models. While this study provides valuable insights, further investigations are necessary to fully comprehend the mechanisms that govern the distinct roles of p53 mutation and p53 loss in regulating the tumor microenvironment and PDAC progression.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cells12222614/s1, Figure S1. Expression levels of signature genes in cancer cells reveal distinct differences between KPmut and KPloss pancreatic tumors. Continued from Figure 2. (A–C) The signature genes associated with classical and basal-like subtypes in cancer cell subpopulations (‘Cancer cell 1’, ‘Cancer cell 2’, and ‘Cancer cell 3’) in the combined dataset of KPmut-Early, KPmut-Late, and KPloss-Late tumors, shown in a violin plot (A,B) and a heatmap plot (C). Figure S2. GSEA enrichment of cancer cells in KPmut and KPloss pancreatic tumors. Continued from Figure 2. Gene Set Enrichment Analysis (GSEA) demonstrated enrichment in the three distinct subtypes of cancer cells, which were classified based on their specific markers. The GSEA results, with a statistical significance of p < 0.05, are visually depicted in DotPlot. Figure S3. Expression levels of cancer-associated signature genes across all cell types. Continued from Figure 3. (A) The signature genes associated with ‘Cancer cell 2’ subtype, particularly in the KPmut-Late tumors, are examined across various major cell types including cancer cells, endothelial cells, cancer-associated fibroblasts, and immune cells. The dot plot shows the expression levels of these genes in the combined dataset of KPmut-Early, KPmut-Late, and KPloss-Late tumors. (B) Cases of TCGA pancreatic cancer cohort harboring KRAS G12* mutations were stratified into two groups based on either loss-of-function or gain-of-function TP53 mutations. The survival between the two groups was compared by the log-rank (Mantel–Cox) test. Figure S4. Comparison of different functions of neutrophils in KPmut-Early, KPmut-Late, and KPloss-Late tumors. Continued from Figure 6. (A–G) Scaled mean expression scores for multiple pathway signatures, namely angiogenesis, ECM remodeling, interferon signaling, myeloid cell recruitment, neutrophil cytotoxicity, neutrophil degranulation, and tumor proliferation. The median (horizontal line), second to third quartiles (box), and Tukey-style whiskers (beyond the box) are represented by the boxes. The dots denote the individual signatures. Figure S5. Marker gene expression profiles in myeloid cells and DCs. Continued from Figure 7. (A) Dot plot showing the normalized expression of pre-defined marker genes for myeloid cells and DCs. (B) GSEA pathway enrichment in the ‘Myeloid cell 3’ subcluster. The GSEA results are visually depicted in the bubble plot. (C) The correlation between Hallmark_glycolysis and Hallmark_oxidative_phosphorylation in myeloid cells and DCs. (D) Relationship between Hallmark_glycolysis and Hallmark_hypoxia in myeloid cell and DC subtypes.
Author Contributions
Conceptualization: Y.C. Data curation: Y.C., X.S. and D.Y. Formal analysis: Y.C. and X.S. Methodology: Y.C. and X.S. Investigation: X.S. and D.Y. Resources: Y.C. Supervision: Y.C. Validation: Y.C. and X.S. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by The MDACC Start-Up Funding, The University of Texas System Rising STARs Award, and The MDACC SPORE in Gastrointestinal Cancer Grant P50 CA221707 Career Enhancement Program Award.
Institutional Review Board Statement
The animal study protocol was approved by the MD Anderson Cancer Center Institutional Animal Care and Use Committee (protocol code 00002328-RN00, approved on 15 November 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All datasets of transgenic mouse models analyzed in this study were previously deposited at the National Center for Biotechnology Information’s Gene Expression Omnibus (GEO) database repository with the following accession numbers: GSE198815 and GSE166298. The survival and gene expression data of TCGA pancreatic adenocarcinoma cohort were based on the GDAC Firehose PAAD dataset.
Acknowledgments
The authors thank Ignacio I. Wistuba, Anirban Maitra, and Huamin Wang for their guidance and support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kuehn, B.M. Looking to Long-term Survivors for Improved Pancreatic Cancer Treatment. JAMA 2020, 324, 2242–2244. [Google Scholar] [CrossRef] [PubMed]
- Li, O.; Li, L.; Sheng, Y.; Ke, K.; Wu, J.; Mou, Y.; Liu, M.; Jin, W. Biological characteristics of pancreatic ductal adenocarcinoma: Initiation to malignancy, intracellular to extracellular. Cancer Lett. 2023, 574, 216391. [Google Scholar] [CrossRef] [PubMed]
- Perez-Diez, I.; Andreu, Z.; Hidalgo, M.R.; Perpina-Clerigues, C.; Fantin, L.; Fernandez-Serra, A.; de la Iglesia-Vaya, M.; Lopez-Guerrero, J.A.; Garcia-Garcia, F. A Comprehensive Transcriptional Signature in Pancreatic Ductal Adenocarcinoma Reveals New Insights into the Immune and Desmoplastic Microenvironments. Cancers 2023, 15, 2887. [Google Scholar] [CrossRef] [PubMed]
- Bernard, V.; Semaan, A.; Huang, J.; San Lucas, F.A.; Mulu, F.C.; Stephens, B.M.; Guerrero, P.A.; Huang, Y.; Zhao, J.; Kamyabi, N.; et al. Single-Cell Transcriptomics of Pancreatic Cancer Precursors Demonstrates Epithelial and Microenvironmental Heterogeneity as an Early Event in Neoplastic Progression. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2019, 25, 2194–2205. [Google Scholar] [CrossRef]
- Elyada, E.; Bolisetty, M.; Laise, P.; Flynn, W.F.; Courtois, E.T.; Burkhart, R.A.; Teinor, J.A.; Belleau, P.; Biffi, G.; Lucito, M.S.; et al. Cross-Species Single-Cell Analysis of Pancreatic Ductal Adenocarcinoma Reveals Antigen-Presenting Cancer-Associated Fibroblasts. Cancer Discov. 2019, 9, 1102–1123. [Google Scholar] [CrossRef]
- Hosein, A.N.; Huang, H.; Wang, Z.; Parmar, K.; Du, W.; Huang, J.; Maitra, A.; Olson, E.; Verma, U.; Brekken, R.A. Cellular heterogeneity during mouse pancreatic ductal adenocarcinoma progression at single-cell resolution. JCI Insight 2019, 5, e129212. [Google Scholar] [CrossRef]
- Peng, J.; Sun, B.F.; Chen, C.Y.; Zhou, J.Y.; Chen, Y.S.; Chen, H.; Liu, L.; Huang, D.; Jiang, J.; Cui, G.S.; et al. Single-cell RNA-seq highlights intra-tumoral heterogeneity and malignant progression in pancreatic ductal adenocarcinoma. Cell Res. 2019, 29, 725–738. [Google Scholar] [CrossRef]
- Steele, N.G.; Carpenter, E.S.; Kemp, S.B.; Sirihorachai, V.R.; The, S.; Delrosario, L.; Lazarus, J.; Amir, E.D.; Gunchick, V.; Espinoza, C.; et al. Multimodal Mapping of the Tumor and Peripheral Blood Immune Landscape in Human Pancreatic Cancer. Nat. Cancer 2020, 1, 1097–1112. [Google Scholar] [CrossRef]
- Carstens, J.L.; Yang, S.; Correa de Sampaio, P.; Zheng, X.; Barua, S.; McAndrews, K.M.; Rao, A.; Burks, J.K.; Rhim, A.D.; Kalluri, R. Stabilized epithelial phenotype of cancer cells in primary tumors leads to increased colonization of liver metastasis in pancreatic cancer. Cell Rep. 2021, 35, 108990. [Google Scholar] [CrossRef]
- McAndrews, K.M.; Chen, Y.; Darpolor, J.K.; Zheng, X.; Yang, S.; Carstens, J.L.; Li, B.; Wang, H.; Miyake, T.; Correa de Sampaio, P.; et al. Identification of Functional Heterogeneity of Carcinoma-Associated Fibroblasts with Distinct IL6-Mediated Therapy Resistance in Pancreatic Cancer. Cancer Discov. 2022, 12, 1580–1597. [Google Scholar] [CrossRef]
- Chen, Y.; Kim, J.; Yang, S.; Wang, H.; Wu, C.J.; Sugimoto, H.; LeBleu, V.S.; Kalluri, R. Type I collagen deletion in alphaSMA(+) myofibroblasts augments immune suppression and accelerates progression of pancreatic cancer. Cancer Cell 2021, 39, 548–565.e546. [Google Scholar] [CrossRef]
- Hwang, W.L.; Jagadeesh, K.A.; Guo, J.A.; Hoffman, H.I.; Yadollahpour, P.; Reeves, J.W.; Mohan, R.; Drokhlyansky, E.; Van Wittenberghe, N.; Ashenberg, O.; et al. Single-nucleus and spatial transcriptome profiling of pancreatic cancer identifies multicellular dynamics associated with neoadjuvant treatment. Nat. Genet. 2022, 54, 1178–1191. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Moniruzzaman, R.; Wang, H.; Wang, H.; Chen, Y. Cross-Dataset Single-Cell Analysis Identifies Temporal Alterations in Cell Populations of Primary Pancreatic Tumor and Liver Metastasis. Cancers 2023, 15, 2396. [Google Scholar] [CrossRef] [PubMed]
- Rivlin, N.; Brosh, R.; Oren, M.; Rotter, V. Mutations in the p53 Tumor Suppressor Gene: Important Milestones at the Various Steps of Tumorigenesis. Genes Cancer 2011, 2, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Morton, J.P.; Timpson, P.; Karim, S.A.; Ridgway, R.A.; Athineos, D.; Doyle, B.; Jamieson, N.B.; Oien, K.A.; Lowy, A.M.; Brunton, V.G.; et al. Mutant p53 drives metastasis and overcomes growth arrest/senescence in pancreatic cancer. Proc. Natl. Acad. Sci. USA 2010, 107, 246–251. [Google Scholar] [CrossRef]
- Gencel-Augusto, J.; Su, X.; Qi, Y.; Whitley, E.M.; Pant, V.; Xiong, S.; Shah, V.; Lin, J.; Perez, E.; Fiorotto, M.L.; et al. Dimeric p53 Mutant Elicits Unique Tumor-Suppressive Activities through an Altered Metabolic Program. Cancer Discov. 2023, 13, 1230–1249. [Google Scholar] [CrossRef]
- Olive, K.P.; Tuveson, D.A.; Ruhe, Z.C.; Yin, B.; Willis, N.A.; Bronson, R.T.; Crowley, D.; Jacks, T. Mutant p53 gain of function in two mouse models of Li-Fraumeni syndrome. Cell 2004, 119, 847–860. [Google Scholar] [CrossRef]
- Muller, P.A.; Vousden, K.H. Mutant p53 in cancer: New functions and therapeutic opportunities. Cancer Cell 2014, 25, 304–317. [Google Scholar] [CrossRef]
- Pal, A.; Gonzalez-Malerva, L.; Eaton, S.; Xu, C.; Zhang, Y.; Grief, D.; Sakala, L.; Nwekwo, L.; Zeng, J.; Christensen, G.; et al. Multidimensional quantitative phenotypic and molecular analysis reveals neomorphic behaviors of p53 missense mutants. NPJ Breast Cancer 2023, 9, 78. [Google Scholar] [CrossRef]
- Ding, D.; Blee, A.M.; Zhang, J.; Pan, Y.; Becker, N.A.; Maher, L.J., 3rd; Jimenez, R.; Wang, L.; Huang, H. Gain-of-function mutant p53 together with ERG proto-oncogene drive prostate cancer by beta-catenin activation and pyrimidine synthesis. Nat. Commun. 2023, 14, 4671. [Google Scholar] [CrossRef]
- Pan, M.; Jiang, C.; Zhang, Z.; Achacoso, N.; Alexeeff, S.; Solorzano, A.V.; Tse, P.; Chung, E.; Sundaresan, T.; Suga, J.M.; et al. TP53 Gain-of-Function and Non-Gain-of-Function Mutations Are Associated with Differential Prognosis in Advanced Pancreatic Ductal Adenocarcinoma. JCO Precis. Oncol. 2023, 7, e2200570. [Google Scholar] [CrossRef] [PubMed]
- Klemke, L.; Fehlau, C.F.; Winkler, N.; Toboll, F.; Singh, S.K.; Moll, U.M.; Schulz-Heddergott, R. The Gain-of-Function p53 R248W Mutant Promotes Migration by STAT3 Deregulation in Human Pancreatic Cancer Cells. Front. Oncol. 2021, 11, 642603. [Google Scholar] [CrossRef] [PubMed]
- Smillie, C.S.; Biton, M.; Ordovas-Montanes, J.; Sullivan, K.M.; Burgin, G.; Graham, D.B.; Herbst, R.H.; Rogel, N.; Slyper, M.; Waldman, J.; et al. Intra- and Inter-cellular Rewiring of the Human Colon during Ulcerative Colitis. Cell 2019, 178, 714–730.e722. [Google Scholar] [CrossRef] [PubMed]
- Gungabeesoon, J.; Gort-Freitas, N.A.; Kiss, M.; Bolli, E.; Messemaker, M.; Siwicki, M.; Hicham, M.; Bill, R.; Koch, P.; Cianciaruso, C.; et al. A neutrophil response linked to tumor control in immunotherapy. Cell 2023, 186, 1448–1464.e1420. [Google Scholar] [CrossRef]
- Cerami, E.; Gao, J.; Dogrusoz, U.; Gross, B.E.; Sumer, S.O.; Aksoy, B.A.; Jacobsen, A.; Byrne, C.J.; Heuer, M.L.; Larsson, E.; et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012, 2, 401–404. [Google Scholar] [CrossRef]
- Gao, J.; Aksoy, B.A.; Dogrusoz, U.; Dresdner, G.; Gross, B.; Sumer, S.O.; Sun, Y.; Jacobsen, A.; Sinha, R.; Larsson, E.; et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal 2013, 6, pl1. [Google Scholar] [CrossRef]
- Rao, C.V.; Janakiram, N.B.; Madka, V.; Kumar, G.; Scott, E.J.; Pathuri, G.; Bryant, T.; Kutche, H.; Zhang, Y.; Biddick, L.; et al. Small-Molecule Inhibition of GCNT3 Disrupts Mucin Biosynthesis and Malignant Cellular Behaviors in Pancreatic Cancer. Cancer Res. 2016, 76, 1965–1974. [Google Scholar] [CrossRef]
- Van Doren, S.R. MMP-7 marks severe pancreatic cancer and alters tumor cell signaling by proteolytic release of ectodomains. Biochem. Soc. Trans. 2022, 50, 839–851. [Google Scholar] [CrossRef]
- Xu, J.; Quan, G.; Huang, W.; Jiang, J. VSIG2 promotes malignant progression of pancreatic ductal adenocarcinoma by enhancing LAMTOR2-mediated mTOR activation. Cell Commun. Signal 2023, 21, 223. [Google Scholar] [CrossRef]
- Yamakawa, K.; Koyanagi-Aoi, M.; Uehara, K.; Masuda, A.; Yanagimoto, H.; Toyama, H.; Fukumoto, T.; Kodama, Y.; Aoi, T. Increased expression of SPRR1A is associated with a poor prognosis in pancreatic ductal adenocarcinoma. PLoS ONE 2022, 17, e0266620. [Google Scholar] [CrossRef]
- Wu, L.; Zhu, X.; Yan, D.; Tang, M.; Ma, C.; Yan, S. Identification of IFN-Induced Transmembrane Protein 1 With Prognostic Value in Pancreatic Cancer Using Network Module-Based Analysis. Front. Oncol. 2021, 11, 626883. [Google Scholar] [CrossRef] [PubMed]
- Moffitt, R.A.; Marayati, R.; Flate, E.L.; Volmar, K.E.; Loeza, S.G.; Hoadley, K.A.; Rashid, N.U.; Williams, L.A.; Eaton, S.C.; Chung, A.H.; et al. Virtual microdissection identifies distinct tumor- and stroma-specific subtypes of pancreatic ductal adenocarcinoma. Nat. Genet. 2015, 47, 1168–1178. [Google Scholar] [CrossRef] [PubMed]
- Hao, D.; Han, G.; Sinjab, A.; Gomez-Bolanos, L.I.; Lazcano, R.; Serrano, A.; Hernandez, S.D.; Dai, E.; Cao, X.; Hu, J.; et al. The Single-Cell Immunogenomic Landscape of B and Plasma Cells in Early-Stage Lung Adenocarcinoma. Cancer Discov. 2022, 12, 2626–2645. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, J.; Akatsu, C.; Zhang, R.; Zhang, H.; Zhu, H.; Liu, K.; Zhu, H.Y.; Min, Q.; Meng, X.; et al. LAPTM5 mediates immature B cell apoptosis and B cell tolerance by regulating the WWP2-PTEN-AKT pathway. Proc. Natl. Acad. Sci. USA 2022, 119, e2205629119. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.D.; Munro, S.A.; Knutson, T.P.; LaRue, R.S.; Heltemes-Harris, L.M.; Farrar, M.A. Single-cell analysis identifies dynamic gene expression networks that govern B cell development and transformation. Nat. Commun. 2021, 12, 6843. [Google Scholar] [CrossRef] [PubMed]
- Felizola, S.J.; Katsu, K.; Ise, K.; Nakamura, Y.; Arai, Y.; Satoh, F.; Sasano, H. Pre-B Lymphocyte Protein 3 (VPREB3) Expression in the Adrenal Cortex: Precedent for non-Immunological Roles in Normal and Neoplastic Human Tissues. Endocr. Pathol. 2015, 26, 119–128. [Google Scholar] [CrossRef]
- Chen, D.; Zheng, J.; Gerasimcik, N.; Lagerstedt, K.; Sjögren, H.; Abrahamsson, J.; Fogelstrand, L.; Mårtensson, I.L. The Expression Pattern of the Pre-B Cell Receptor Components Correlates with Cellular Stage and Clinical Outcome in Acute Lymphoblastic Leukemia. PLoS ONE 2016, 11, e0162638. [Google Scholar] [CrossRef]
- Ly, A.; Liao, Y.; Pietrzak, H.; Ioannidis, L.J.; Sidwell, T.; Gloury, R.; Doerflinger, M.; Triglia, T.; Qin, R.Z.; Groom, J.R.; et al. Transcription Factor T-bet in B Cells Modulates Germinal Center Polarization and Antibody Affinity Maturation in Response to Malaria. Cell Rep. 2019, 29, 2257–2269.e2556. [Google Scholar] [CrossRef]
- Lachmandas, E.; Boutens, L.; Ratter, J.M.; Hijmans, A.; Hooiveld, G.J.; Joosten, L.A.; Rodenburg, R.J.; Fransen, J.A.; Houtkooper, R.H.; van Crevel, R.; et al. Microbial stimulation of different Toll-like receptor signalling pathways induces diverse metabolic programmes in human monocytes. Nat. Microbiol. 2016, 2, 16246. [Google Scholar] [CrossRef]
- Lock, I.C.; Leisenring, N.H.; Floyd, W.; Xu, E.S.; Luo, L.; Ma, Y.; Mansell, E.C.; Cardona, D.M.; Lee, C.L.; Kirsch, D.G. Mis-splicing Drives Loss of Function of p53 (E224D) Point Mutation. bioRxiv 2023. [Google Scholar] [CrossRef]
- Baslan, T.; Morris, J.P.t.; Zhao, Z.; Reyes, J.; Ho, Y.J.; Tsanov, K.M.; Bermeo, J.; Tian, S.; Zhang, S.; Askan, G.; et al. Ordered and deterministic cancer genome evolution after p53 loss. Nature 2022, 608, 795–802. [Google Scholar] [CrossRef]
- Laklai, H.; Miroshnikova, Y.A.; Pickup, M.W.; Collisson, E.A.; Kim, G.E.; Barrett, A.S.; Hill, R.C.; Lakins, J.N.; Schlaepfer, D.D.; Mouw, J.K.; et al. Genotype tunes pancreatic ductal adenocarcinoma tissue tension to induce matricellular fibrosis and tumor progression. Nat. Med. 2016, 22, 497–505. [Google Scholar] [CrossRef]
- Hingorani, S.R.; Wang, L.; Multani, A.S.; Combs, C.; Deramaudt, T.B.; Hruban, R.H.; Rustgi, A.K.; Chang, S.; Tuveson, D.A. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell 2005, 7, 469–483. [Google Scholar] [CrossRef]
- Rhim, A.D.; Mirek, E.T.; Aiello, N.M.; Maitra, A.; Bailey, J.M.; McAllister, F.; Reichert, M.; Beatty, G.L.; Rustgi, A.K.; Vonderheide, R.H.; et al. EMT and dissemination precede pancreatic tumor formation. Cell 2012, 148, 349–361. [Google Scholar] [CrossRef]
- Ying, H.; Kimmelman, A.C.; Lyssiotis, C.A.; Hua, S.; Chu, G.C.; Fletcher-Sananikone, E.; Locasale, J.W.; Son, J.; Zhang, H.; Coloff, J.L.; et al. Oncogenic Kras maintains pancreatic tumors through regulation of anabolic glucose metabolism. Cell 2012, 149, 656–670. [Google Scholar] [CrossRef]
- Schonhuber, N.; Seidler, B.; Schuck, K.; Veltkamp, C.; Schachtler, C.; Zukowska, M.; Eser, S.; Feyerabend, T.B.; Paul, M.C.; Eser, P.; et al. A next-generation dual-recombinase system for time- and host-specific targeting of pancreatic cancer. Nat. Med. 2014, 20, 1340–1347. [Google Scholar] [CrossRef]
- Poeta, M.L.; Manola, J.; Goldwasser, M.A.; Forastiere, A.; Benoit, N.; Califano, J.A.; Ridge, J.A.; Goodwin, J.; Kenady, D.; Saunders, J.; et al. TP53 mutations and survival in squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 2007, 357, 2552–2561. [Google Scholar] [CrossRef]
- Holstege, H.; Joosse, S.A.; van Oostrom, C.T.; Nederlof, P.M.; de Vries, A.; Jonkers, J. High incidence of protein-truncating TP53 mutations in BRCA1-related breast cancer. Cancer Res. 2009, 69, 3625–3633. [Google Scholar] [CrossRef]
- Cavagna, R.O.; Pinto, I.A.; Escremim de Paula, F.; Berardinelli, G.N.; Sant’Anna, D.; Santana, I.; da Silva, V.D.; Da Silva, E.C.A.; Miziara, J.E.; Mourao Dias, J.; et al. Disruptive and Truncating TP53 Mutations Are Associated with African-Ancestry and Worse Prognosis in Brazilian Patients with Lung Adenocarcinoma. Pathobiology 2023, 90, 344–355. [Google Scholar] [CrossRef]
- Chen, X.; Zeng, K.; Xu, M.; Liu, X.; Hu, X.; Xu, T.; He, B.; Pan, Y.; Sun, H.; Wang, S. P53-induced miR-1249 inhibits tumor growth, metastasis, and angiogenesis by targeting VEGFA and HMGA2. Cell Death Dis. 2019, 10, 131. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).