Hyaluronic Acid Induction Promotes the Differentiation of Human Neural Crest-like Cells into Periodontal Ligament Stem-like Cells
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. PDLSC Induction
2.3. Osteoblastic Differentiation
2.4. Adipocytic Differentiation
2.5. Quantitative RT-PCR (qRT-PCR)
2.6. Gene Expression Microarray
2.7. Magnetic-Activated Cell Sorting (MACS) and Flow Cytometric Analysis
2.8. Small Interfering RNA (siRNA) Transfection
2.9. HA Stimulation
2.10. Fabrication of LMWHA-Containing Electrospun Nanofibrous Membranes
2.11. Scanning Electron Microscopy
2.12. Enzyme-Linked Immunosorbent Assay (ELISA)
2.13. Culturing SK-N-SH Cells with LMWHA-Containing Electrospun Nanofibrous Membranes
2.14. Statistical Analysis
3. Results
3.1. Differentiation of SK-N-SH Cells into PDLSCs
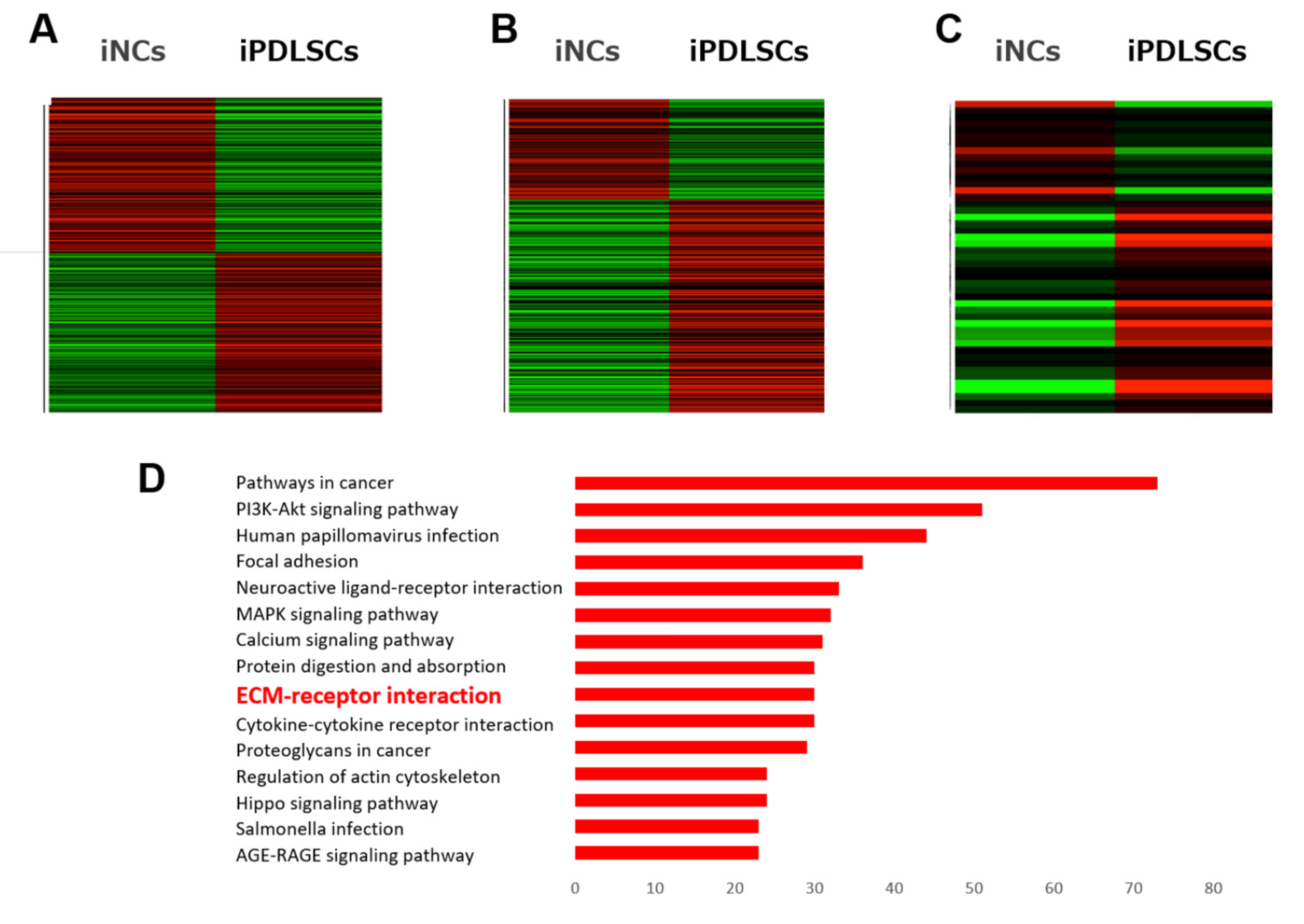
3.2. Genes Upregulated by Differentiation of NC Cells into PDLSCs
3.3. Differentiation of CD44+ SK-N-SH Cells into PDLSCs
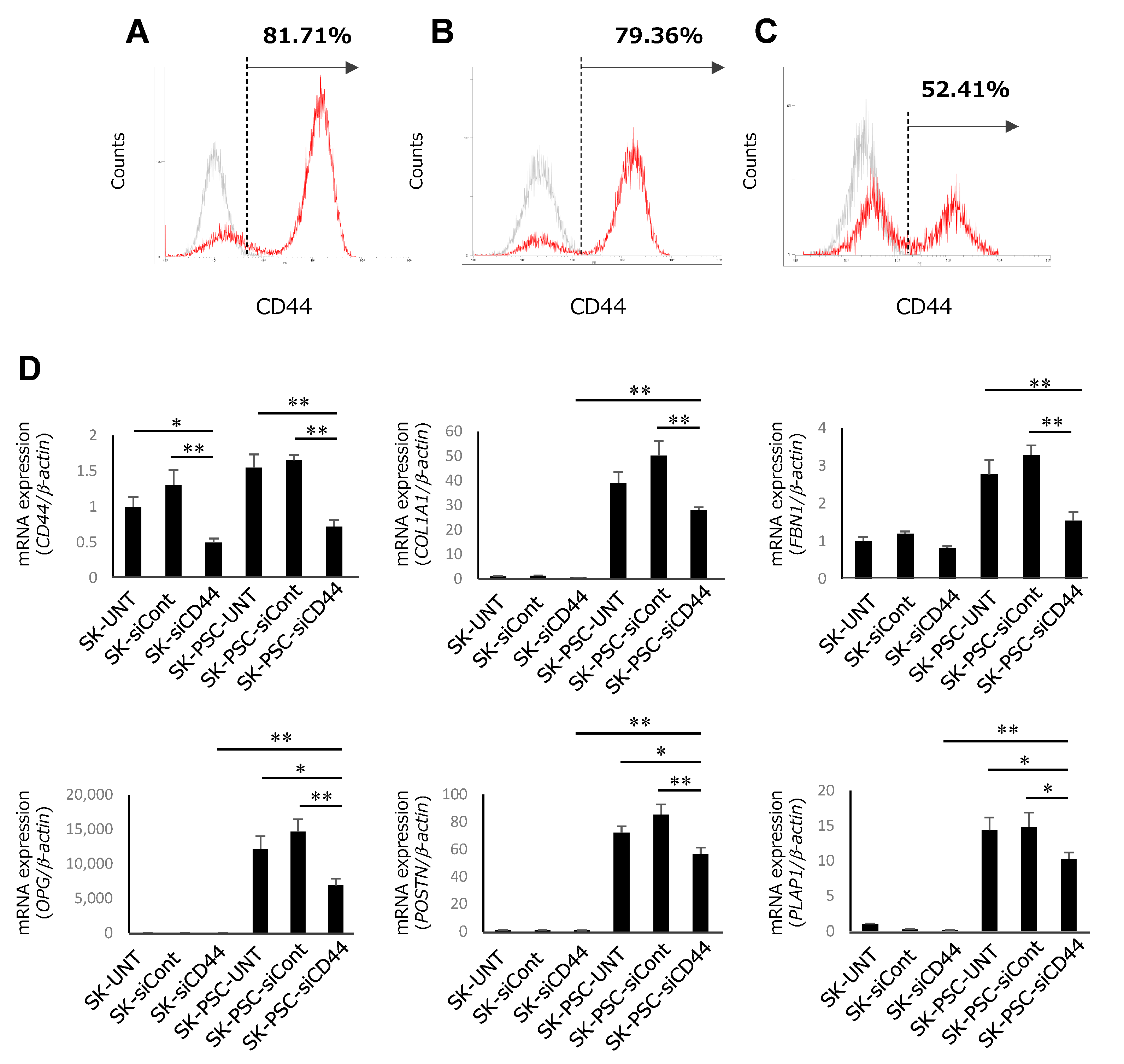
3.4. Differentiation of CD44-Suppressed SK-N-SH Cells into PDLSCs
3.5. Effect of Continuous HA Stimulation on Differentiation of SK-N-SH Cells into SK-PDLSCs
3.6. Effect of Initial LMWHA Stimulation on Differentiation of SK-N-SH Cells into SK-PDLSCs
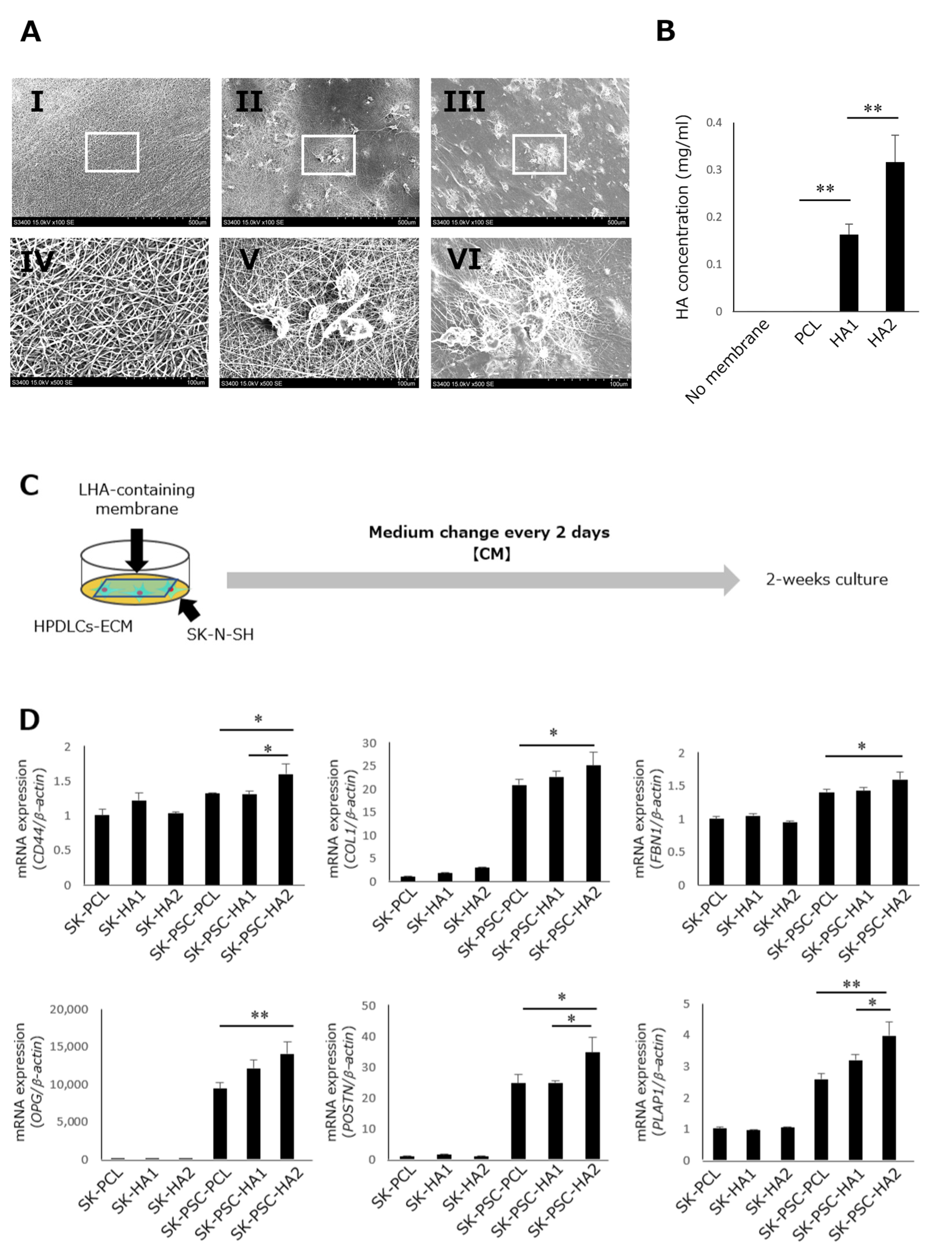
3.7. Effect of LMWHA-Containing Electrospun Nanofibrous Membranes on Differentiation of SK-N-SH Cells into SK-PDLSCs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, M.G.; Park, C.H. Tooth-Supporting Hard Tissue Regeneration Using Biopolymeric Material Fabrication Strategies. Molecules 2020, 25, 4802. [Google Scholar] [CrossRef] [PubMed]
- Bartold, P.M.; Xiao, Y.; Lyngstaadas, S.P.; Paine, M.L.; Snead, M.L. Principles and applications of cell delivery systems for periodontal regeneration. Periodontology 2000 2006, 41, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Bosshardt, D.D.; Sculean, N. Does periodontal tissue regeneration really work? Periodontolgy 2000 2009, 51, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Tomokiyo, A.; Yoshida, S.; Hamano, S.; Hasegawa, D.; Sugii, H.; Maeda, H. Detection, Characterization, and Clinical Application of Mesenchymal Stem Cells in Periodontal Ligament Tissue. Stem Cells Int. 2018, 2018, 5450768. [Google Scholar] [CrossRef]
- Seo, B.-M.; Miura, M.; Gronthos, S.; Bartold, P.M.; Batouli, S.; Brahim, J.; Young, M.; Robey, P.G.; Wang, C.Y.; Shi, S. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet 2004, 364, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Bassir, S.H.; Wisitrasameewong, W.; Raanan, J.; Ghaffarigarakani, S.; Chung, J.; Freire, M.; Andrada, L.C.; Intini, G. Potential for Stem Cell-Based Periodontal Therapy. J. Cell. Physiol. 2016, 231, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Vandana, K.L.; Shalini, H.S. Direct application of autologous periodontal ligament stem cell niche in treatment of periodontal osseous defects: A randomized controlled trial. J. Indian Soc. Periodontol. 2018, 22, 503–512. [Google Scholar] [CrossRef] [PubMed]
- An, S.; Huang, X.; Gao, Y.; Ling, J.; Huang, Y.; Xiao, Y. FGF-2 induces the proliferation of human periodontal ligament cells and modulates their osteoblastic phenotype by affecting Runx2 expression in the presence and absence of osteogenic inducers. Int. J. Mol. Med. 2015, 36, 705–711. [Google Scholar] [CrossRef]
- Selleck, M.A.; Scherson, T.Y.; Bronner-Fraser, M. Origins of Neural Crest Cell Diversity. Dev. Biol. 1993, 159, 1–11. [Google Scholar] [CrossRef]
- Delfino-Machín, M.; Chipperfield, T.R.; Rodrigues, F.S.; Kelsh, R.N. The proliferating field of neural crest stem cells. Dev. Dyn. 2007, 236, 3242–3254. [Google Scholar] [CrossRef]
- Chai, Y.; Jiang, X.; Ito, Y.; Bringas, P., Jr.; Han, J.; Rowitch, D.H.; Soriano, P.; McMahon, A.P.; Sucov, H.M. Fate of the mammalian cranical neural crest durng tooth and mandibular morphogenesis. Development 2000, 127, 1671–1679. [Google Scholar] [CrossRef]
- Tomokiyo, A.; Maeda, H.; Fujii, S.; Monnouchi, S.; Wada, N.; Kono, K.; Yamamoto, N.; Koori, K.; Teramatsu, Y.; Akamine, A. A multipotent clonal human periodontal ligament cell line with neural crest cell phenotypes promotes neurocytic differentiation, migration, and survival. J. Cell. Physiol. 2012, 227, 2040–2050. [Google Scholar] [CrossRef]
- Mehrotra, P.; Tseropoulos, G.; Bronner, M.E.; Andreadis, S.T. Adult tissue–derived neural crest-like stem cells: Sources, regulatory networks, and translational potential. Stem Cells Transl. Med. 2020, 9, 328–341. [Google Scholar] [CrossRef]
- Takahashi, K.; Yamanaka, S. Induction of Pluripotent Stem Cells from Mouse Embryonic and Adult Fibroblast Cultures by Defined Factors. Cell 2006, 126, 663–676. [Google Scholar] [CrossRef]
- Chambers, S.M.; Fasano, C.A.; Papapetrou, E.P.; Tomishima, M.; Sadelain, M.; Studer, L. Highly efficient neural conversion of human ES and iPS cells by dual inhibition of SMAD signaling. Nat. Biotechnol. 2009, 27, 275–280. [Google Scholar] [CrossRef]
- Tomokiyo, A.; Hynes, K.; Ng, J.; Menicanin, D.; Camp, E.; Arthur, A.; Gronthos, S.; Bartold, P.M. Generation of Neural Crest-Like Cells From Human Periodontal Ligament Cell-Derived Induced Pluripotent Stem Cells. J. Cell. Physiol. 2017, 232, 402–416. [Google Scholar] [CrossRef]
- Otsu, K.; Kishigami, R.; Oikawa-Sasaki, A.; Fukumoto, S.; Yamada, A.; Fujiwara, N.; Ishizeki, K.; Harada, H.; Tomokiyo, A.; Hynes, K.; et al. Differentiation of Induced Pluripotent Stem Cells Into Dental Mesenchymal Cells. Stem Cells Dev. 2012, 21, 1156–1164. [Google Scholar] [CrossRef]
- Hamano, S.; Tomokiyo, A.; Hasegawa, D.; Yoshida, S.; Sugii, H.; Mitarai, H.; Fujino, S.; Wada, N.; Maeda, H.; Trubiani, O.; et al. Extracellular Matrix from Periodontal Ligament Cells Could Induce the Differentiation of Induced Pluripotent Stem Cells to Periodontal Ligament Stem Cell-Like Cells. Stem Cells Dev. 2018, 27, 100–111. [Google Scholar] [CrossRef]
- Biedler, J.L.; Helson, L.; Spengler, B.A. Morphology and Growth, Tumorigenicity, and Cytogenetics of Human Neuroblastoma Cells in Continuous Culture1. Cancer Res. 1973, 33, 2643–2652. [Google Scholar]
- Yusuf, M.; Leung, K.; Morris, K.J.; Volpi, E.V. Comprehensive cytogenomic profile of the in vitro neuronal model SH-SY5Y. Neurogenetics 2013, 14, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Bates, S.E.; Mickley, L.A.; Chen, Y.-N.; Richert, N.; Rudick, J.; Biedler, J.L.; Fojo, A.T. Expression of a Drug Resistance Gene in Human Neuroblastoma Cell Lines: Modulation by Retinoic Acid-Induced Differentiation. Mol. Cell. Biol. 1989, 9, 4337–4344. [Google Scholar] [CrossRef]
- Hou, W.-Y.; Song, X.; Wang, Y.; Chang, P.; Chen, R.; Wu, Y.-J. The alteration of the expression level of neuropathy target esterase in human neuroblastoma SK-N-SH cells disrupts cellular phospholipids homeostasis. Toxicol. Vitr. 2023, 86, 105509. [Google Scholar] [CrossRef]
- Yoshida, S.; Wada, N.; Hasegawa, D.; Miyaji, H.; Mitarai, H.; Tomokiyo, A.; Hamano, S.; Maeda, H. Semaphorin 3A Induces Odontoblastic Phenotype in Dental Pulp Stem Cells. J. Dent. Res. 2016, 95, 1282–1290. [Google Scholar] [CrossRef]
- Aruffo, A.; Stamenkovic, I.; Melnick, M.; Underhill, C.B.; Seed, B. CD44 is the principal cell surface receptor for hyaluronate. Cell 1990, 61, 1303–1313. [Google Scholar] [CrossRef]
- Tavianatou, A.G.; Caon, I.; Franchi, M.; Piperigkou, Z.; Galesso, D.; Karamanos, N.K. Hyaluronan: Molecular size-dependent signaling and biological functions in inflammation and cancer. FEBS J. 2019, 286, 2883–2908. [Google Scholar] [CrossRef]
- Bell, N.; Hann, V.; Redfern, C.P.; Cheek, T.R. Store-operated Ca2+ entry in proliferating and retinoic acid-differentiated N- and S-type neuroblastoma cells. Biochim. Biophys. Acta (BBA)—Mol. Cell Res. 2013, 1833, 643–651. [Google Scholar] [CrossRef]
- Boeva, V.; Louis-Brennetot, C.; Peltier, A.; Durand, S.; Pierre-Eugène, C.; Raynal, V.; Etchevers, H.C.; Thomas, S.; Lermine, A.; Daudigeos-Dubus, E.; et al. Heterogeneity of neuroblastoma cell identity defined by transcriptional circuitries. Nat. Genet. 2017, 49, 1408–1413. [Google Scholar] [CrossRef]
- A Ross, R.; A Spengler, B.; Domènech, C.; Porubcin, M.; Rettig, W.J.; Biedler, J.L. Human neuroblastoma I-type cells are malignant neural crest stem cells. Chemotherapy 1995, 6, 449–456. [Google Scholar]
- von Levetzow, C.; Jiang, X.; Gwye, Y.; von Levetzow, G.; Hung, L.; Cooper, A.; Hsu, J.H.-R.; Lawlor, E.R. Modeling Initiation of Ewing Sarcoma in Human Neural Crest Cells. PLoS ONE 2011, 6, e19305. [Google Scholar] [CrossRef] [PubMed]
- Kimata, K.; Honma, Y.; Okayama, M.; Oguri, K.; Hozumi, M.; Suzuki, S. Increased synthesis of hyaluronic acid by mouse mammary carcinoma cell variants with high metastatic potential. Cancer Res. 1983, 43, 1347–1354. [Google Scholar] [PubMed]
- Dahiya, P.; Kamal, R. Hyaluronic acid: A boon in periodontal therapy. N. Am. J. Med. Sci. 2013, 5, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Yeh, Y.; Yang, Y.; Yuan, K. Importance of CD44 in the proliferation and mineralization of periodontal ligament cells. J. Periodontal Res. 2014, 49, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Al-Rekabi, Z.; Fura, A.M.; Juhlin, I.; Yassin, A.; Popowics, T.E.; Sniadecki, N.J. Hyaluronan-CD44 interactions mediate contractility and migration in periodontal ligament cells. Cell Adhes. Migr. 2019, 13, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Gracz, A.D.; Samsa, L.A.; Fordham, M.J.; Trotier, D.C.; Zwarycz, B.; Lo, Y.-H.; Bao, K.; Starmer, J.; Raab, J.R.; Shroyer, N.F.; et al. Sox4 Promotes Atoh1-Independent Intestinal Secretory Differentiation Toward Tuft and Enteroendocrine Fates. Gastroenterology 2018, 155, 1508–1523. [Google Scholar] [CrossRef] [PubMed]
- Mylona, E.; Jones, K.A.; Mills, S.T.; Pavlath, G.K. CD44 regulates myoblast migration and differentiation. J. Cell. Physiol. 2006, 209, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Zhao, N.; Wang, X.; Qin, L.; Guo, Z.; Li, D. Effect of molecular weight and concentration of hyaluronan on cell proliferation and osteogenic differentiation in vitro. Biochem. Biophys. Res. Commun. 2015, 465, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Park, Y.; Tae, G.; Lee, K.B.; Hwang, C.M.; Hwang, S.J.; Kim, I.S.; Noh, I.; Sun, K. Characterization of low-molecular-weight hyaluronic acid-based hydrogel and differential stem cell responses in the hydrogel microenvironments. J. Biomed. Mater. Res. Part A 2009, 88, 967–975. [Google Scholar] [CrossRef]
- Della Sala, F.; di Gennaro, M.; Lista, G.; Messina, F.; Ambrosio, L.; Borzacchiello, A. Effect of Hyaluronic Acid on the Differentiation of Mesenchymal Stem Cells into Mature Type II Pneumocytes. Polymers 2021, 13, 2928. [Google Scholar] [CrossRef]
- David-Raoudi, M.; Tranchepain, F.; Deschrevel, B.; Vincent, J.-C.; Bogdanowicz, P.; Boumediene, K.; Pujol, J.-P. Differential effects of hyaluronan and its fragments on fibroblasts: Relation to wound healing. Wound Repair Regen. 2008, 16, 274–287. [Google Scholar] [CrossRef]
- Li, J.; Zhang, F.; Zhang, N.; Geng, X.; Meng, C.; Wang, X.; Yang, Y. Osteogenic capacity and cytotherapeutic potential of periodontal ligament cells for periodontal regeneration in vitro and in vivo. PeerJ 2019, 7, e6589. [Google Scholar] [CrossRef]
- Yan, Y.; Zhang, H.; Liu, L.; Chu, Z.; Ge, Y.; Wu, J.; Liu, Y.; Tang, C. Periostin reverses high glucose-inhibited osteogenesis of periodontal ligament stem cells via AKT pathway. Life Sci. 2020, 242, 117184. [Google Scholar] [CrossRef]
- Cui, C.; Bi, R.; Liu, W.; Guan, S.; Li, P.; Song, D.; Xu, R.; Zheng, L.; Yuan, Q.; Zhou, X.; et al. Role of PTH1R Signaling in Prx1+ Mesenchymal Progenitors during Eruption. J. Dent. Res. 2020, 99, 1296–1305. [Google Scholar] [CrossRef]
- Bowman, E.N.; Hallock, J.D.; Throckmorton, T.W.; Azar, F.M. Hyaluronic acid injections for osteoarthritis of the knee: Predictors of successful treatment. Int. Orthop. 2018, 42, 733–740. [Google Scholar] [CrossRef]
- Bengestrate, L.; Virtue, S.; Campbell, M.; Vidal-Puig, A.; Hadaschik, D.; Hahn, P.; Bielke, W. Genome-Wide Profiling of MicroRNAs in Adipose Mesenchymal Stem Cell Differentiation and Mouse Models of Obesity. PLoS ONE 2011, 6, e21305. [Google Scholar] [CrossRef]
- Tiwari, G.; Tiwari, R.; Sriwastawa, B.; Bhati, L.; Pandey, S.; Pandey, P.; Bannerjee, S.K. Drug delivery systems: An updated review. Int. J. Pharm. Investig. 2012, 2, 2–11. [Google Scholar] [CrossRef]
- Vellayappan, M.V.; Venugopal, J.R.; Ramakrishna, S.; Ray, S.; Ismail, A.F.; Mandal, M.; Manikandan, A.; Seal, S.; Jaganathan, S.K. Electrospinning applications from diagnosis to treatment of diabetes. RSC Adv. 2016, 6, 83638–83655. [Google Scholar] [CrossRef]
- Malikmammadov, E.; Tanir, T.E.; Kiziltay, A.; Hasirci, V.; Hasirci, N. PCL and PCL-based materials in biomedical applications. J. Biomater. Sci. Polym. Ed. 2018, 29, 863–893. [Google Scholar] [CrossRef]
- Jiang, W.; Li, L.; Zhang, D.; Huang, S.; Jing, Z.; Wu, Y.; Zhao, Z.; Zhao, L.; Zhou, S. Incorporation of aligned PCL–PEG nanofibers into porous chitosan scaffolds improved the orientation of collagen fibers in regenerated periodontium. Acta Biomater. 2015, 25, 240–252. [Google Scholar] [CrossRef] [PubMed]
- Farag, A.; Hashimi, S.M.; Vaquette, C.; Bartold, P.M.; Hutmacher, D.W.; Ivanovski, S. The effect of decellularized tissue engineered constructs on periodontal regeneration. J. Clin. Periodontol. 2018, 45, 586–596. [Google Scholar] [CrossRef] [PubMed]
- Khatami, S.M.; Parivar, K.; Sohi, A.N.; Soleimani, M.; Hanaee-Ahvaz, H. Acetylated hyaluronic acid effectively enhances chondrogenic differentiation of mesenchymal stem cells seeded on electrospun PCL scaffolds. Tissue Cell 2020, 65, 101363. [Google Scholar] [CrossRef] [PubMed]





| Target Gene (Abbreviation) | Gene Bank ID | Forward (Top) and Reverse (Bottom) Primer Sequences | Size of Amplified Products (bp) |
|---|---|---|---|
| Aggrecan (ACAN) | NM_001411096.1 | AGTCCTCAAGCCTCCTGTACTCA | 185 |
| CGGGAAGTGGCGGTAACA | |||
| Adiponectin (ADIPOQ) | NM_001177800.2 | CAGGAAACCACGACTCAAGGG | 200 |
| CCGGTTTCACCGATGTCTCC | |||
| Angiopoietin Like 4 (ANGPTL4) | NM_001039667.3 | CCACTTGGGACCAGGATCAC | 123 |
| GGATGGAGCGGAAGTACTGG | |||
| ADIPSIN | NM_001317335.2 | GTGCGCGGAGAGCAATCG | 131 |
| AGATCCCGGGCTTCTTGCG | |||
| Actin Alpha 2, Smooth Muscle (αSMA) | NM_001613.4 | GACAATGGCTCTGGGCTCTGTA | 147 |
| CTGTGCTTCGTCACCCACGTA | |||
| B-actin | NM_001101.5 | TGGCACCCAGCACAATGAA | 89 |
| CTAAGTCATAGTCCGCCTAGAAGCA | |||
| Bone Morphogenetic Protein 2 (BMP2) | NM_001200.4 | TCCACTAATCATGCCATTGTTCA | 73 |
| GGGACACAGCATGCCTTAGGA | |||
| Bone Sialoprotein (BSP) | MN_004967.3 | CTGGCACAGGGTATACAGGGTTAG | 181 |
| ACTGGTGCCGTTTATGCCTTG | |||
| CD44 | NM_001202555.2 | CTGCAGGTATGGGTTCATAG | 123 |
| ATATGTGTCATACTGGGAGGTG | |||
| Collagen Type I Alpha 1 (COL1A1) | NM_000088 | CCCGGGTTTCAGAGACAACTTC | 148 |
| TCCACATGCTTTATTCCAGCAATC | |||
| Fibrillin-1 (FBN1) | NM_000138.4 | AAGTGATCCACTGTGTGCCAACTC | 189 |
| TGCACCTATGGAACCATGTGATAG | |||
| Fat-Specific Protein FSP27 (FSP27) | NM_001199551.2 | CTTCATTGGCTGCCTGAACG | 195 |
| CCTTCCTCCGTAGCATCGAG | |||
| Inter-Alpha-Trypsin Inhibitor Heavy Chain 3 (ITIH3) | NM_001392025.1 | GCCTACCTCACCATTGAGCA | 142 |
| GCTTGGTCACCACCATTGAG | |||
| Hyaluronan and Proteoglycan Link protein 1 (HAPLN1) | AK313713.1 | TGGTGAGAAAGTGCCTCCTT | 151 |
| TAGCGCTCTTTCTCCTCACC | |||
| Hyaluronan Synthase 3 (HAS3) | NM_005329.3 | GGACCGTGTGCGGGATGTGG | 142 |
| AGTGTCAGAGTCGCACACCTGGA | |||
| Leptin (LEP) | NM_000230.3 | GCTGTGCCCATCCAAAAAGTC | 178 |
| CCAGTGTCTGGTCCATCTTGG | |||
| Osteoprotegerin (OPG) | NM_002546.3 | TGGCACCAAAGTAAACGCAGAG | 195 |
| CTCGAAGGTGAGGTTAGCATGTC | |||
| Osteopontin (OPN) | NM_000582.3 | ACACATATGATGGCCGAGGTGA | 115 |
| TGTGAGGTGATGTCCTCGTCTGT | |||
| Periodontal Ligament-Associated Protein 1 (PLAP1) | NM_017680.5 | ATGGGAGTCTTGCTAACATACCAC | 154 |
| CAGAAGTCATTTACTCCCACTCTTG | |||
| Periostin (POSTN) | NM_006475.2 | CATTGATGGAGTGCCTGTGGA | 167 |
| CAATGAATTTGGTGACCTTGGTG | |||
| Runt-Related Transcription Factor 2 (RUNX2) | NM_001015051.4 | AACCCTTAATTTGCACTGGGTCA | 145 |
| CAAATTCCAGCAATGTTTGTGCTAC | |||
| Semaphorin 3A (SEMA3A) | NM_006080.3 | AACGGCCGTGGGAAGAGTCCAT | 137 |
| TGGTGGTGCCCAAGAGTTCGG | |||
| Tenomodulin (TNMD) | NM_022144.3 | CTGGTGTTTGGTATCCTGGC | 192 |
| ATCAGTGCCATTTCCGCTTC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhasan, M.A.; Tomokiyo, A.; Hamano, S.; Sugii, H.; Ono, T.; Ipposhi, K.; Yamashita, K.; Mardini, B.; Minowa, F.; Maeda, H. Hyaluronic Acid Induction Promotes the Differentiation of Human Neural Crest-like Cells into Periodontal Ligament Stem-like Cells. Cells 2023, 12, 2743. https://doi.org/10.3390/cells12232743
Alhasan MA, Tomokiyo A, Hamano S, Sugii H, Ono T, Ipposhi K, Yamashita K, Mardini B, Minowa F, Maeda H. Hyaluronic Acid Induction Promotes the Differentiation of Human Neural Crest-like Cells into Periodontal Ligament Stem-like Cells. Cells. 2023; 12(23):2743. https://doi.org/10.3390/cells12232743
Chicago/Turabian StyleAlhasan, M. Anas, Atsushi Tomokiyo, Sayuri Hamano, Hideki Sugii, Taiga Ono, Keita Ipposhi, Kozue Yamashita, Bara Mardini, Fumiko Minowa, and Hidefumi Maeda. 2023. "Hyaluronic Acid Induction Promotes the Differentiation of Human Neural Crest-like Cells into Periodontal Ligament Stem-like Cells" Cells 12, no. 23: 2743. https://doi.org/10.3390/cells12232743







