Conjugated Bile Acids Promote Lymphangiogenesis by Modulation of the Reactive Oxygen Species–p90RSK–Vascular Endothelial Growth Factor Receptor 3 Pathway
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Model
2.2. Cell Culture
2.3. XTT Assay
2.4. RNA Extraction and Real-Time PCR
2.5. Protein Extraction and Western Blot Analysis
2.6. Immunoprecipitation and Detection of SUMOylation by Western Blot
2.7. Measurement of Total ROS and Mitochondrial ROS (mtROS)
2.8. Seahorse Assay
2.9. siRNA Transfection
2.10. Transwell Migration
2.11. Invasion Assays
2.12. Tube Formation Assay
2.13. Immunofluorescence (IF) and Immunohistochemistry (IHC)
2.14. Statistical Analysis
3. Results
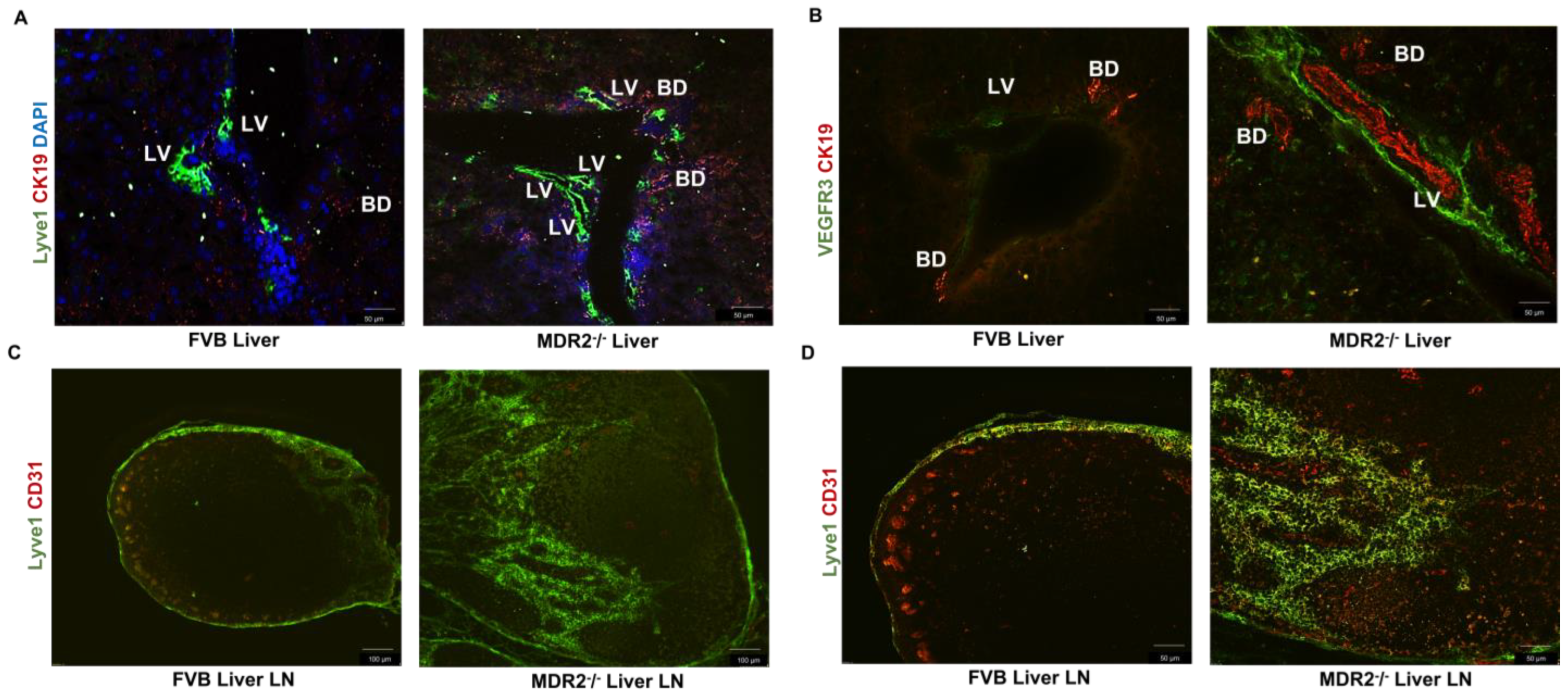
3.1. The Mouse Model of Liver Cholestasis has a High Level of Lymphangiogenesis
3.2. The Mouse Model of Liver Cholestasis has Enhanced Levels of Bas in Lymph Nodes and Serum
3.3. Conjugated BAs Enhance the Proliferation and Migration of HLECs
3.4. Conjugated BA Increased the Expression of Lymphangiogenic Growth factor Receptors
3.5. HLECs Express BA Receptors
3.6. Conjugated BAs Alters the Cellular Metabolism and Activate the Redox Pathway in HLECs through TGR5 Receptors
3.7. TCA Enhanced the Cellular Reactive Oxygen Species (ROS) Production and Induces Prox1 SUMOylation via p90RSK Activation and Promotes VEGFR3 Expression
3.8. TCA-Induced p90RSK Activation Promotes the Tube Formation and Invasion of HLECs
3.9. TCA Induced the YAP Expression and its Nuclear Translocation Mediated by the ROS
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, Y.; Lu, L.-G. Therapeutic Roles of Bile Acid Signaling in Chronic Liver Diseases. J. Clin. Transl. Hepatol. 2018, 6, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.-J.Y.; Sheng, L. Regulation of bile acid receptor activity. Liver Res. 2018, 2, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Meadows, V.; Kennedy, L.; Kundu, D.; Alpini, G.; Francis, H. Bile Acid Receptor Therapeutics Effects on Chronic Liver Diseases. Front. Med. 2020, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- Proungvitaya, S.; Sombattheera, S.; Boonsiri, P.; Limpaiboon, T.; Wongkham, S.; Wongkham, C.; Titapun, A.; Proungvitaya, T. Diagnostic value of serum bile acid composition patterns and serum glycocholic acid levels in cholangiocarcinoma. Oncol. Lett. 2017, 14, 4943–4948. [Google Scholar] [CrossRef]
- Xia, X.; Francis, H.; Glaser, S.; Alpini, G.; Lesage, G. Bile acid interactions with cholangiocytes. World J. Gastroenterol. 2006, 12, 3553–3563. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-K.; Jeong, S.-H.; Jang, C.; Bae, H.; Kim, Y.H.; Park, I.; Kim, S.K.; Koh, G.Y. Tumor metastasis to lymph nodes requires YAP-dependent metabolic adaptation. Science 2019, 363, 644–649. [Google Scholar] [CrossRef]
- Roy, S.; Banerjee, P.; Ekser, B.; Bayless, K.; Zawieja, D.; Alpini, G.; Glaser, S.S.; Chakraborty, S. Targeting Lymphangiogenesis and Lymph Node Metastasis in Liver Cancer. Am. J. Pathol. 2021, 191, 2052–2063. [Google Scholar] [CrossRef]
- O’Brien, A.; Gasheva, O.; Alpini, G.; Zawieja, D.; Gashev, A.; Glaser, S. The Role of Lymphatics in Cholestasis: A Comprehensive Review. Semin. Liver Dis. 2020, 40, 403–410. [Google Scholar] [CrossRef]
- Tanaka, M.; Iwakiri, Y. Lymphatics in the liver. Curr. Opin. Immunol. 2018, 53, 137–142. [Google Scholar] [CrossRef]
- Chakraborty, S.; Zawieja, S.; Wang, W.; Zawieja, D.C.; Muthuchamy, M. Lymphatic system: A vital link between metabolic syndrome and inflammation. Ann. N. Y. Acad. Sci. 2010, 1207, E94–E102. [Google Scholar] [CrossRef]
- Tamburini, B.A.J.; Finlon, J.M.; Gillen, A.E.; Kriss, M.S.; Riemondy, K.A.; Fu, R.; Schuyler, R.P.; Hesselberth, J.R.; Rosen, H.R.; Burchill, M.A. Chronic Liver Disease in Humans Causes Expansion and Differentiation of Liver Lymphatic Endothelial Cells. Front. Immunol. 2019, 10, 1036. [Google Scholar] [CrossRef] [PubMed]
- Vaahtomeri, K.; Karaman, S.; Makinen, T.; Alitalo, K. Lymphangiogenesis guidance by paracrine and pericellular factors. Genes Dev. 2017, 31, 1615–1634. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Park, J.S.; Kim, D.; Hong, H.S. Substance P Hinders Bile Acid-Induced Hepatocellular Injury by Modulating Oxidative Stress and Inflammation. Antioxidants 2022, 11, 920. [Google Scholar] [CrossRef]
- Adachi, T.; Kaminaga, T.; Yasuda, H.; Kamiya, T.; Hara, H. The involvement of endoplasmic reticulum stress in bile acid-induced hepatocellular injury. J. Clin. Biochem. Nutr. 2014, 54, 129–135. [Google Scholar] [CrossRef]
- Monaghan, R.M.; Page, D.J.; Ostergaard, P.; Keavney, B.D. The physiological and pathological functions of VEGFR3 in cardiac and lymphatic development and related diseases. Cardiovasc. Res. 2020, 117, 1877–1890. [Google Scholar] [CrossRef]
- Ma, W.; Gil, H.J.; Liu, X.; Diebold, L.P.; Morgan, M.A.; Oxendine-Burns, M.J.; Gao, P.; Chandel, N.S.; Oliver, G. Mitochondrial respiration controls the Prox1-Vegfr3 feedback loop during lymphatic endothelial cell fate specification and maintenance. Sci. Adv. 2021, 7, eabe7359. [Google Scholar] [CrossRef]
- Pan, M.-R.; Chang, T.-M.; Chang, H.-C.; Su, J.-L.; Wang, H.-W.; Hung, W.-C. Sumoylation of Prox1 controls its ability to induce VEGFR3 expression and lymphatic phenotypes in endothelial cells. J. Cell Sci. 2009, 122, 3358–3364. [Google Scholar] [CrossRef]
- Heo, K.-S.; Le, N.-T.; Cushman, H.J.; Giancursio, C.J.; Chang, E.; Woo, C.-H.; Sullivan, M.A.; Taunton, J.; Yeh, E.T.; Fujiwara, K.; et al. Disturbed flow-activated p90RSK kinase accelerates atherosclerosis by inhibiting SENP2 function. J. Clin. Investig. 2015, 125, 1299–1310. [Google Scholar] [CrossRef] [PubMed]
- Abe, J.-I.; Okuda, M.; Huang, Q.; Yoshizumi, M.; Berk, B.C. Reactive Oxygen Species Activate p90 Ribosomal S6 Kinase via Fyn and Ras. J. Biol. Chem. 2000, 275, 1739–1748. [Google Scholar] [CrossRef]
- Booth, D.M.; Murphy, J.A.; Mukherjee, R.; Awais, M.; Neoptolemos, J.P.; Gerasimenko, O.V.; Tepikin, A.V.; Petersen, O.H.; Sutton, R.; Criddle, D.N. Reactive Oxygen Species Induced by Bile Acid Induce Apoptosis and Protect Against Necrosis in Pancreatic Acinar Cells. Gastroenterology 2011, 140, 2116–2125. [Google Scholar] [CrossRef]
- Cho, Y.; Park, M.J.; Kim, K.; Kim, S.W.; Kim, W.; Oh, S.; Lee, J.H. Reactive oxygen species-induced activation of Yes-associated protein-1 through the c-Myc pathway is a therapeutic target in hepatocellular carcinoma. World J. Gastroenterol. 2020, 26, 6599–6613. [Google Scholar] [CrossRef] [PubMed]
- Grimm, L.; Nakajima, H.; Chaudhury, S.; Bower, N.; Okuda, K.S.; Cox, A.G.; Harvey, N.L.; Koltowska, K.; Mochizuki, N.; Hogan, B.M. Yap1 promotes sprouting and proliferation of lymphatic progenitors downstream of Vegfc in the zebrafish trunk. Elife 2019, 8, e42881. [Google Scholar] [CrossRef] [PubMed]
- Anakk, S.; Bhosale, M.; Schmidt, V.A.; Johnson, R.L.; Finegold, M.J.; Moore, D.D. Bile Acids Activate YAP to Promote Liver Carcinogenesis. Cell Rep. 2013, 5, 1060–1069. [Google Scholar] [CrossRef]
- McDaniel, K.; Meng, F.; Wu, N.; Sato, K.; Venter, J.; Bernuzzi, F.; Invernizzi, P.; Zhou, T.; Kyritsi, K.; Wan, Y.; et al. Forkhead box A2 regulates biliary heterogeneity and senescence during cholestatic liver injury in mice‡. Hepatology 2016, 65, 544–559. [Google Scholar] [CrossRef]
- Kumaravel, S.; Singh, S.; Roy, S.; Venkatasamy, L.; White, T.K.; Sinha, S.; Glaser, S.S.; Safe, S.H.; Chakraborty, S. CXCL11-CXCR3 Axis Mediates Tumor Lymphatic Cross Talk and Inflammation-Induced Tumor, Promoting Pathways in Head and Neck Cancers. Am. J. Pathol. 2020, 190, 900–915. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Zhao, R.; Zhou, X.; Liang, X.; Campbell, D.J.; Zhang, X.; Zhang, L.; Shi, R.; Wang, G.; Pandak, W.M.; et al. Conjugated bile acids promote cholangiocarcinoma cell invasive growth through activation of sphingosine 1-phosphate receptor 2. Hepatology 2014, 60, 908–918. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Li, X.; Qiang, X.; Luo, L.; Hylemon, P.B.; Jiang, Z.; Zhang, L.; Zhou, H. Taurocholate Induces Cyclooxygenase-2 Expression via the Sphingosine 1-phosphate Receptor 2 in a Human Cholangiocarcinoma Cell Line. J. Biol. Chem. 2015, 290, 30988–31002. [Google Scholar] [CrossRef]
- Liu, R.; Li, X.; Hylemon, P.B.; Zhou, H. Conjugated Bile Acids Promote Invasive Growth of Esophageal Adenocarcinoma Cells and Cancer Stem Cell Expansion via Sphingosine 1-Phosphate Receptor 2–Mediated Yes-Associated Protein Activation. Am. J. Pathol. 2018, 188, 2042–2058. [Google Scholar] [CrossRef]
- Chakraborty, S.; Zawieja, D.C.; Davis, M.J.; Muthuchamy, M. MicroRNA signature of inflamed lymphatic endothelium and role of miR-9 in lymphangiogenesis and inflammation. Am. J. Physiol. Physiol. 2015, 309, C680–C692. [Google Scholar] [CrossRef] [PubMed]
- Jan, C.-I.; Tsai, M.-H.; Chiu, C.-F.; Huang, Y.-P.; Liu, C.J.; Chang, N.W. Fenofibrate Suppresses Oral Tumorigenesis via Reprogramming Metabolic Processes: Potential Drug Repurposing for Oral Cancer. Int. J. Biol. Sci. 2016, 12, 786–798. [Google Scholar] [CrossRef]
- Lee, Y.; Chakraborty, S.; Meininger, C.J.; Muthuchamy, M. Insulin resistance disrupts cell integrity, mitochondrial function, and inflammatory signaling in lymphatic endothelium. Microcirculation 2018, 25, e12492. [Google Scholar] [CrossRef] [PubMed]
- Pathak, T.; Gueguinou, M.; Walter, V.; Delierneux, C.; Johnson, M.T.; Zhang, X.; Xin, P.; E Yoast, R.; Emrich, S.M.; Yochum, G.S.; et al. Dichotomous role of the human mitochondrial Na+/Ca2+/Li+ exchanger NCLX in colorectal cancer growth and metastasis. Elife 2020, 9, e59686. [Google Scholar] [CrossRef] [PubMed]
- Barnoud, T.; Parris, J.L.; Murphy, M.E. Tumor cells containing the African-Centric S47 variant ofTP53show increased Warburg metabolism. Oncotarget 2019, 10, 1217–1223. [Google Scholar] [CrossRef]
- Singh, S.; Kumaravel, S.; Dhole, S.; Roy, S.; Pavan, V.; Chakraborty, S. Neuropeptide Substance P Enhances Inflammation-Mediated Tumor Signaling Pathways and Migration and Proliferation of Head and Neck Cancers. Indian J. Surg. Oncol. 2020, 12, 93–102. [Google Scholar] [CrossRef]
- Kumaravel, S.; Abbey, C.A.; Bayless, K.J.; Chakraborty, S. The β1-integrin plays a key role in LEC invasion in an optimized 3-D collagen matrix model. Am. J. Physiol. Physiol. 2020, 319, C1045–C1058. [Google Scholar] [CrossRef]
- Sha, M.; Jeong, S.; Wang, X.; Tong, Y.; Cao, J.; Sun, H.-Y.; Xia, L.; Xu, N.; Xi, Z.-F.; Zhang, J.-J.; et al. Tumor-associated lymphangiogenesis predicts unfavorable prognosis of intrahepatic cholangiocarcinoma. BMC Cancer 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Liao, S.; Von Der Weid, P.-Y. Inflammation-induced lymphangiogenesis and lymphatic dysfunction. Angiogenesis 2014, 17, 325–334. [Google Scholar] [CrossRef]
- Roy, S.; Glaser, S.; Chakraborty, S. Inflammation and Progression of Cholangiocarcinoma: Role of Angiogenic and Lymphangiogenic Mechanisms. Front. Med. 2019, 6, 293. [Google Scholar] [CrossRef] [PubMed]
- Ikenaga, N.; Liu, S.B.; Sverdlov, D.Y.; Yoshida, S.; Nasser, I.; Ke, Q.; Kang, P.M.; Popov, Y. A New Mdr2−/− Mouse Model of Sclerosing Cholangitis with Rapid Fibrosis Progression, Early-Onset Portal Hypertension, and Liver Cancer. Am. J. Pathol. 2014, 185, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Kaminsky-Kolesnikov, Y.; Rauchbach, E.; Abu-Halaka, D.; Hahn, M.; García-Ruiz, C.; Fernandez-Checa, J.C.; Madar, Z.; Tirosh, O. Cholesterol Induces Nrf-2- and HIF-1α-Dependent Hepatocyte Proliferation and Liver Regeneration to Ameliorate Bile Acid Toxicity in Mouse Models of NASH and Fibrosis. Oxidative Med. Cell. Longev. 2020, 2020, 1–18. [Google Scholar] [CrossRef]
- Chiang, J.Y.L.; Ferrell, J.M. Bile Acid Metabolism in Liver Pathobiology. Gene Expr. 2018, 18, 71–87. [Google Scholar] [CrossRef]
- Teuwen, L.-A.; Geldhof, V.; Carmeliet, P. How glucose, glutamine and fatty acid metabolism shape blood and lymph vessel development. Dev. Biol. 2019, 447, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-W.; Yu, P.; Simons, M. Recent advances in understanding lymphangiogenesis and metabolism. F1000Research 2018, 7, 1114. [Google Scholar] [CrossRef] [PubMed]
- Lechner, S.; Müller-Ladner, U.; Schlottmann, K.; Jung, B.; McClelland, M.; Rüschoff, J.; Welsh, J.; Schölmerich, J.; Kullmann, F. Bile acids mimic oxidative stress induced upregulation of thioredoxin reductase in colon cancer cell lines. Carcinogenesis 2002, 23, 1281–1288. [Google Scholar] [CrossRef]
- Yerushalmi, B.; Dahl, R.; Devereaux, M.W.; Gumpricht, E.; Sokol, R.J. Bile acid-induced rat hepatocyte apoptosis is inhibited by antioxidants and blockers of the mitochondrial permeability transition. Hepatology 2001, 33, 616–626. [Google Scholar] [CrossRef] [PubMed]
- AlHayaza, R.; Haque, E.; Karbasiafshar, C.; Sellke, F.W.; Abid, M.R. The Relationship between Reactive Oxygen Species and Endothelial Cell Metabolism. Front. Chem. 2020, 8, 1043. [Google Scholar] [CrossRef] [PubMed]
- Le, N.-T.; Heo, K.-S.; Takei, Y.; Lee, H.; Woo, C.-H.; Chang, E.; McClain, C.; Hurley, C.; Wang, X.; Li, F.; et al. A Crucial Role for p90RSK-Mediated Reduction of ERK5 Transcriptional Activity in Endothelial Dysfunction and Atherosclerosis. Circulation 2013, 127, 486–499. [Google Scholar] [CrossRef] [PubMed]
- Heo, K.-S.; Berk, B.C.; Abe, J.-I. Disturbed Flow-Induced Endothelial Proatherogenic Signaling via Regulating Post-Translational Modifications and Epigenetic Events. Antioxidants Redox Signal. 2016, 25, 435–450. [Google Scholar] [CrossRef]
- Han, Z.-J.; Feng, Y.-H.; Gu, B.-H.; Li, Y.-M.; Chen, H. The post-translational modification, SUMOylation, and cancer (Review). Int. J. Oncol. 2018, 52, 1081–1094. [Google Scholar] [CrossRef]
- Park, J.A.; Kwon, Y.-G. Hippo-YAP/TAZ signaling in angiogenesis. BMB Rep. 2018, 51, 157–162. [Google Scholar] [CrossRef]
- Azad, T.; Ghahremani, M.; Yang, X. The Role of YAP and TAZ in Angiogenesis and Vascular Mimicry. Cells 2019, 8, 407. [Google Scholar] [CrossRef]
- Cha, B.; Moon, S.; Kim, W. A novel role of Hippo-Yap/TAZ signaling pathway in lymphatic vascular development. BMB Rep. 2021, 54, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Cha, B.; Ho, Y.-C.; Geng, X.; Mahamud, R.; Chen, L.; Kim, Y.; Choi, D.; Kim, T.H.; Randolph, G.J.; Cao, X.; et al. YAP and TAZ maintain PROX1 expression in the developing lymphatic and lymphovenous valves in response to VEGF-C signaling. Development 2020, 147, dev195453. [Google Scholar] [CrossRef]
- Molina, L.; Nejak-Bowen, K.; Monga, S.P. Role of YAP1 Signaling in Biliary Development, Repair, and Disease. Semin. Liver Dis. 2022, 42, 017–033. [Google Scholar] [CrossRef]
- Zhou, T.; Chang, L.; Luo, Y.; Zhou, Y.; Zhang, J. Mst1 inhibition attenuates non-alcoholic fatty liver disease via reversing Parkin-related mitophagy. Redox Biol. 2019, 21, 101120. [Google Scholar] [CrossRef]
- Siciliano, M.; Milani, A.; Rossi, L.; Mannes, G.A.; Thieme, C.; Paumgartner, G. Correspondence. Hepatology 1986, 6, 1445. [Google Scholar] [CrossRef]
- Wang, X.; Wang, X.; Xie, G.; Zhou, M.; Yu, H.; Lin, Y.; Du, G.; Luo, G.; Jia, W.; Liu, P. Urinary Metabolite Variation Is Associated with Pathological Progression of the Post-Hepatitis B Cirrhosis Patients. J. Proteome Res. 2012, 11, 3838–3847. [Google Scholar] [CrossRef]
- Wang, X.; Xie, G.; Zhao, A.; Zheng, X.; Huang, F.; Wang, Y.; Yao, C.; Jia, W.; Liu, P. Serum Bile Acids Are Associated with Pathological Progression of Hepatitis B-Induced Cirrhosis. J. Proteome Res. 2016, 15, 1126–1134. [Google Scholar] [CrossRef] [PubMed]
- Horvatits, T.; Drolz, A.; Roedl, K.; Rutter, K.; Ferlitsch, A.; Fauler, G.; Trauner, M.; Fuhrmann, V. Serum bile acids as marker for acute decompensation and acute-on-chronic liver failure in patients with non-cholestatic cirrhosis. Liver Int. 2016, 37, 224–231. [Google Scholar] [CrossRef]
- Carreira, C.M.; Nasser, S.M.; Di Tomaso, E.; Padera, T.; Boucher, Y.; Tomarev, S.I.; Jain, R.K. LYVE-1 is not restricted to the lymph vessels: Expression in normal liver blood sinusoids and down-regulation in human liver cancer and cirrhosis. Cancer Res. 2001, 61, 8079–8084. [Google Scholar]
- Yamauchi, Y.; Michitaka, K.; Onji, M. Morphometric Analysis of Lymphatic and Blood Vessels in Human Chronic Viral Liver Diseases. Am. J. Pathol. 1998, 153, 1131–1137. [Google Scholar] [CrossRef] [PubMed]
- Tugues, S.; Morales-Ruiz, M.; Fern’ández-Varo, G.; Ros, J.; Arteta, D.; Muñoz, J.; Arroyo, V.; Rodés, J.; Jiménez, W. Microarray Analysis of Endothelial Differentially Expressed Genes in Liver of Cirrhotic Rats. Gastroenterology 2005, 129, 1686–1695. [Google Scholar] [CrossRef]
- Goldberg, A.R.; Ferguson, M.; Pal, S.; Cohen, R.; Orlicky, D.J.; McCullough, R.L.; Rutkowski, J.M.; Burchill, M.A.; Tamburini, B.A.J. Oxidized low density lipoprotein in the liver causes decreased permeability of liver lymphatic-but not liver sinusoidal-endothelial cells via VEGFR-3 regulation of VE-Cadherin. Front. Physiol. 2022, 13, 2223. [Google Scholar] [CrossRef]
- Mancinelli, R.; Ceci, L.; Kennedy, L.; Francis, H.; Meadows, V.; Chen, L.; Carpino, G.; Kyritsi, K.; Wu, N.; Zhou, T.; et al. The Effects of Taurocholic Acid on Biliary Damage and Liver Fibrosis Are Mediated by Calcitonin-Gene-Related Peptide Signaling. Cells 2022, 11, 1591. [Google Scholar] [CrossRef]
- Mariotti, V.; Strazzabosco, M.; Fabris, L.; Calvisi, D.F. Animal models of biliary injury and altered bile acid metabolism. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2017, 1864, 1254–1261. [Google Scholar] [CrossRef]
- Kong, B.; Wang, L.; Chiang, J.Y.; Zhang, Y.; Klaassen, C.D.; Guo, G.L. Mechanism of tissue-specific farnesoid X receptor in suppressing the expression of genes in bile-acid synthesis in mice. Hepatology 2012, 56, 1034–1043. [Google Scholar] [CrossRef] [PubMed]
- Dent, P.; Fang, Y.; Gupta, S.; Studer, E.; Mitchell, C.; Spiegel, S.; Hylemon, P.B. Conjugated bile acids promote ERK1/2 and AKT activation via a pertussis toxin-sensitive mechanism in murine and human hepatocytes. Hepatology 2005, 42, 1291–1299. [Google Scholar] [CrossRef]
- Fang, Y.; Han, S.I.; Mitchell, C.; Gupta, S.; Studer, E.; Grant, S.; Hylemon, P.B.; Dent, P. Bile acids induce mitochondrial ROS, which promote activation of receptor tyrosine kinases and signaling pathways in rat hepatocytes. Hepatology 2004, 40, 961–971. [Google Scholar] [CrossRef]
- Zhang, X.; Nan, D.; Zha, C.; He, G.; Zhang, W.; Duan, Z. Long-term intervention of taurocholic acid over-expressing in cholestatic liver disease inhibits the growth of hepatoma cells. Cell Mol. Biol. 2020, 66, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Lasseègue, B.; Griendling, K.K. NADPH Oxidases: Functions and Pathologies in the Vasculature. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 653–661. [Google Scholar] [CrossRef]
- Matute, J.D.; Arias, A.A.; Dinauer, M.C.; Patiño, P.J. p40phox: The last NADPH oxidase subunit. Blood Cells Mol. Dis. 2005, 35, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Abid, R.; Kachra, Z.; Spokes, K.C.; Aird, W.C. NADPH oxidase activity is required for endothelial cell proliferation and migration. FEBS Lett. 2000, 486, 252–256. [Google Scholar] [CrossRef]
- Abid, R.; Shih, S.-C.; Otu, H.; Spokes, K.C.; Okada, Y.; Curiel, D.T.; Minami, T.; Aird, W.C. A Novel Class of Vascular Endothelial Growth Factor-responsive Genes That Require Forkhead Activity for Expression. J. Biol. Chem. 2006, 281, 35544–35553. [Google Scholar] [CrossRef] [PubMed]
- Abid, R.; Spokes, K.C.; Shih, S.-C.; Aird, W.C. NADPH Oxidase Activity Selectively Modulates Vascular Endothelial Growth Factor Signaling Pathways. J. Biol. Chem. 2007, 282, 35373–35385. [Google Scholar] [CrossRef] [PubMed]
- Abid, R.; Tsai, J.C.; Spokes, K.C.; Deshpande, S.S.; Irani, K.; Aird, W.C. Vascular endothelial growth factor induces manganese-superoxide dismutase expression in endothelial cells by a Racl-regulated NADPH oxidase-dependent mechanism. FASEB J. 2001, 15, 2548–2550. [Google Scholar] [CrossRef]
- Wang, X.; Liu, Z.; Sun, J.; Song, X.; Bian, M.; Wang, F.; Yan, F.; Yu, Z. Inhibition of NADPH oxidase 4 attenuates lymphangiogenesis and tumor metastasis in breast cancer. FASEB J. 2021, 35, e21531. [Google Scholar] [CrossRef] [PubMed]
- Shan, S.-F.; Wang, L.-F.; Zhai, J.-W.; Qin, Y.; Ouyang, H.-F.; Kong, Y.-Y.; Liu, J.; Wang, Y.; Xie, Y.-H. Modulation of transcriptional corepressor activity of prospero-related homeobox protein (Prox1) by SUMO modification. FEBS Lett. 2008, 582, 3723–3728. [Google Scholar] [CrossRef]
- Yu, P.; Wu, G.; Lee, H.-W.; Simons, M. Endothelial Metabolic Control of Lymphangiogenesis. Bioessays 2018, 40, e1700245. [Google Scholar] [CrossRef]
- Yu, P.; Wilhelm, K.; Dubrac, A.; Tung, J.K.; Alves, T.C.; Fang, J.S.; Xie, Y.; Zhu, J.; Chen, Z.; De Smet, F.; et al. FGF-dependent metabolic control of vascular development. Nature 2017, 545, 224–228. [Google Scholar] [CrossRef]
- Potente, M.; Carmeliet, P. The Link Between Angiogenesis and Endothelial Metabolism. Annu. Rev. Physiol. 2017, 79, 43–66. [Google Scholar] [CrossRef]
- Xu, Y.; Feingold, P.L.; Surman, D.R.; Brown, K.; Xi, S.; Davis, J.L.; Hernandez, J.; Schrump, D.S.; Ripley, R.T. Bile acid and cigarette smoke enhance the aggressive phenotype of esophageal adenocarcinoma cells by downregulation of the mitochondrial uncoupling protein-2. Oncotarget 2017, 8, 101057–101071. [Google Scholar] [CrossRef] [PubMed]
- Lang, L.; Chemmalakuzhy, R.; Shay, C.; Teng, Y. PFKP Signaling at a Glance: An Emerging Mediator of Cancer Cell Metabolism. Rev. Biomark. Stud. Metab. Metab.-Relat. Disord. 2019, 1134, 243–258. [Google Scholar] [CrossRef]
- Roy, S.; Kumaravel, S.; Banerjee, P.; White, T.K.; O’Brien, A.; Seelig, C.; Chauhan, R.; Ekser, B.; Bayless, K.J.; Alpini, G.; et al. Tumor Lymphatic Interactions Induce CXCR2-CXCL5 Axis and Alter Cellular Metabolism and Lymphangiogenic Pathways to Promote Cholangiocarcinoma. Cells 2021, 10, 3093. [Google Scholar] [CrossRef] [PubMed]
- Bastos, D.C.; Paupert, J.; Maillard, C.; Seguin, F.; A Carvalho, M.; Agostini, M.; Coletta, R.D.; Noël, A.; Graner, E. Effects of fatty acid synthase inhibitors on lymphatic vessels: An in vitro and in vivo study in a melanoma model. Lab. Investig. 2017, 97, 194–206. [Google Scholar] [CrossRef] [PubMed]
- Falci, S.G.M.; Mesquita, A.T.M.; de Andrade, B.A.B.; de Miranda, J.L.; León, J.E.; de Almeida, O.P.; dos Santos, C.R.R. FASN expression, angiogenesis and lymphangiogenesis in central and peripheral giant cell lesions. J. Appl. Oral Sci. 2014, 22, 131–137. [Google Scholar] [CrossRef]
- Yu, F.-X.; Zhao, B.; Panupinthu, N.; Jewell, J.L.; Lian, I.; Wang, L.H.; Zhao, J.; Yuan, H.; Tumaneng, K.; Li, H.; et al. Regulation of the Hippo-YAP Pathway by G-Protein-Coupled Receptor Signaling. Cell 2012, 150, 780–791. [Google Scholar] [CrossRef] [PubMed]
- Totaro, A.; Panciera, T.; Piccolo, S. YAP/TAZ upstream signals and downstream responses. Nat. Cell Biol. 2018, 20, 888–899. [Google Scholar] [CrossRef]
- Yu, B.; Jin, G.-N.; Ma, M.; Liang, H.-F.; Zhang, B.-X.; Chen, X.-P.; Ding, Z.-Y. Taurocholate Induces Connective Tissue Growth Factor Expression in Hepatocytes Through ERK-YAP Signaling. Cell. Physiol. Biochem. 2018, 50, 1711–1725. [Google Scholar] [CrossRef]






| Primers | Species | Forward | Reverse |
|---|---|---|---|
| ANKR1 | Human | 5′-AGACTCCTTCAGCCAACATGATG-3′ | 5′-CTCTCCATCTCTGAAATCCTCAGG-3′ |
| AX1 | Human | 5′-AACCTTCAACTCCTGCCTTCTCG-3′ | 5′-CAGCTTCTCCTTCAGCTCTTCAC-3′ |
| CTGF | Human | 5′-AATGCTGCGAGGAGTGGGT-3′ | 5′-CGGCTCTAATCATAGTTGGGTCT-3′ |
| eNOS | Human | 5′-GAAGGCGACAATCCTGTATGGC-3′ | 5′-TGTTCGAGGGACACCACGTCAT-3′ |
| FGFR1 | Human | 5′-TTAATAGCTCGGATGCGGAG-3′ | 5′-ACGCAGACTGGTTAGCTTCAATG-3′ |
| FGFR2 | Human | 5′-GATAAATACTTCCAATGCAGAAGTGCT-3′ | 5′-TGCCCTATATAATTGGAGACCTTACA-3′ |
| FGFR4 | Human | 5′-AGCACCCTACTGGACACACC-3′ | 5′-ACGCTCTCCATCACGAGACT-3′ |
| KLF2 | Human | 5′-CCAAGAGTTCGCATCTGAAGGC-3′ | 5′-CCGTGTGCTTTCGGTAGTGGC-3′ |
| Lyve-1 | Human | 5′-AGCCTGCGAAAGCCTTTTGGTG-3′ | 5′-GGCTTCACATTCAGCAAACCTGG-3′ |
| Nox4 | Human | 5′-CTGCTGACGTTGCATGTTTC-3′ | 5′-TTCTGAGAGCTGGTTCGGTT-3′ |
| PDPN | Human | 5′-GTGCCGAAGATGATGTGGTGAC-3′ | 5′-GGACTGTGCTTTCTGAAGTTGGC-3′ |
| Prox-1 | Human | 5′-CTGAAGACCTACTTCTCCGACG-3′ | 5′-GATGGCTTGACGTGCGTACTTC-3′ |
| PPARg | Human | 5′-AGCCTGCGAAAGCCTTTTGGTG-3′ | 5′-GGCTTCACATTCAGCAAACCTGG-3′ |
| p21CIP | Human | 5′-GGACAGCAGAGGAAGACCATGT-3′ | 5′-TGGAGTGGTAGAAATCTGTCATGC-3′ |
| RAC1 | Human | 5′-GCGTTGCCATTGAACTCACC-3′ | 5′-GAGCTGCTACGCTCACTCCATTAC-3′ |
| RPL19 | Human | 5′-GGGCATAGGTAAGCGGAAGG-3′ | 5′-TCAGGTACAGGCTGTGATACA-3′ |
| Ubiquitin | Human | 5′-AGTCCCTTCTCGGCGATTCT-3′ | 5′-GCATTGTCAAGTGACGATCACAGC-3′ |
| VEGFC | Human | 5′-TTCCTGCCGATGCATGTCTAA-3′ | 5′-TGTTCGCTGCCTGACACTGT-3′ |
| VEGFR1 | Human | 5′-CTGCCACTCTAATTGTCAATGTGAA-3′ | 5′-AAACGATGACACGGCCTTTT-3′ |
| VEGFR2 | Human | 5′-CCAGCAAAAGCAGGGAGTCTGT-3′ | 5′-TGTCTGTGTCATCGGAGTGATATCC-3′ |
| VEGFR3 | Human | 5′-CCTGAAGAAGATCGCTGTTC-3′ | 5′-GAGAGCTGGTTCCTGGAGAT-3′ |
| YAP1 | Human | 5′-TGTCCCAGATGAACGTCACAGC-3′ | 5′-TGGTGGCTGTTTCACTGGAGCA-3′ |
| PFKP | Human | 5′-CGGAAGTTCCTGGAGCACCTCTC-3′ | 5′-AAGTACACCTTGGCCCCCACGTA-3′ |
| HK2 | Human | 5′-GAGCCACCACTCACCCTACT-3′ | 5′-CCAGGCATTCGGCAATGTG-3′ |
| CO I | Human | 5′-CTCTTGCGGTACTCATTGAAG-3′ | 5′-GAGCTGCTGTTCGGTGTC-3′ |
| GLUT3 | Human | 5′-ACTTTGACGGACAAGGGAAATG-3′ | 5′-ACCAGTGACAGCCAACAGG-3′ |
| ATP6 | Human | 5′-GAAGCGCCACCCTAGCAATA-3′ | 5′-GCTTGGATTAAGGCGACAGC-3′ |
| AMPK1a | Human | 5′-TGCGTGTACGAAGGAAGAATCC-3′ | 5′-TGTGACTTCCAGGTCTTGGAGTT-3′ |
| FASN | Human | 5′-CGCGTGGCCGGCTACTCCTAC-3′ | 5′-CGGCTGCCACACGCTCCTCT-3′ |
| eNOS | Mouse | 5′-TCCGGAAGGCGTTTGATC-3′ | 5′-GCCAAATGTGCTGGTCACC-3′ |
| KLF2 | Mouse | 5′-CACCTAAAGGCGCATCTGCGTA-3′ | 5′-GTGACCTGTGTGCTTTCGGTAG-3′ |
| Nox1 | Mouse | 5′-AATGCCCAGGATCGAGGT-3′ | 5′-GATGGAAGCAAAGGGAGTGA-3′ |
| Nox2 | Mouse | 5′-CCCTTTGGTACAGCCAGTGAAGAT-3′ | 5′-CAATCCCGGCTCCCACTAACATCA-3′ |
| Nox4 | Mouse | 5′-GGATCACAGAAGGTCCCTAGCAG-3′ | 5′-GCGGCTACATGCACACCTGAGAA-3′ |
| p22phox | Mouse | 5′-ATGGGGCAGATCGAGTGGGCCATGT-3′ | 5′-ATAGATCACACTGGCAATGGCCAA-3′ |
| p40phox | Mouse | 5′-GCTTCACCAGCCACTTTGTT-3′ | 5′-TCTTGTTTTGCGCCCATGTA-3′ |
| p67phox | Mouse | 5′-CCACTCGAGGATTTGCTTCA-3′ | 5′-ATCTTGGAATGCCTGGGCTC-3′ |
| p21 | Mouse | 5′-CGAGAACGGTGGAACTTTGAC-3′ | 5′-CAGGGCTCAGGTAGACCTTG-3′ |
| RPL19 | Mouse | 5′-ATGAGTATGCTCAGGCTACAGA-3′ | 5′-GCATTGGCCGATTTCATTGGTC-3′ |
| Ubiquitin | Mouse | 5′-GCCCAGTGTTACCACCAAGAAG-3′ | 5′-GCTCTTTTTAGATACTGTGGTGAGGAA-3′ |
| Name of the Antibodies | Assays | Dilution | Manufacturer | Catalog Number | RRID |
|---|---|---|---|---|---|
| Phospho-p90RSK (Ser380) | WB | 1:1000 | Cell Signaling Technology | 12032 | AB_2797804 |
| RSK1/RSK2/RSK3 | WB | 1:1000 | Cell Signaling Technology | 9355 | AB_659900 |
| Flt4/VEGFR3 | WB | 1:400 | Santa Cruz | SC321 | AB_2105107 |
| Prox1 | IP, WB | 1:1000 | Cell Signaling Technology | 14963 | AB_2783562 |
| Lyve1 | WB | 1:1000 | |||
| YAP1 | WB | 1:1000 | Novus | NB110-58358 | AB_922796 |
| pYAP Y357 | IF | 1:100 | Sigma Aldrich | Y4645 | AB_1080624 |
| SUMO1 | IP, WB | 1:1000 | Cell Signaling Technology | 4940 | AB_2302825 |
| GPCR TGR5 | IF, WB | 1:100, 1:1000 | Abcam | ab72608 | AB_2112165 |
| S1PR2 | IF, WB | 1:100, 1:1000 | Thermo Fisher Scientific | PA523208 | AB_2540734 |
| FXR | IF, WB | 1:100, 1:1000 | Thermo Fisher Scientific | 417200 | AB_2532196 |
| Beta actin | WB | 1:20,000 | Sigma Aldrich | A3854 | AB_262011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banerjee, P.; Kumaravel, S.; Roy, S.; Gaddam, N.; Odeh, J.; Bayless, K.J.; Glaser, S.; Chakraborty, S. Conjugated Bile Acids Promote Lymphangiogenesis by Modulation of the Reactive Oxygen Species–p90RSK–Vascular Endothelial Growth Factor Receptor 3 Pathway. Cells 2023, 12, 526. https://doi.org/10.3390/cells12040526
Banerjee P, Kumaravel S, Roy S, Gaddam N, Odeh J, Bayless KJ, Glaser S, Chakraborty S. Conjugated Bile Acids Promote Lymphangiogenesis by Modulation of the Reactive Oxygen Species–p90RSK–Vascular Endothelial Growth Factor Receptor 3 Pathway. Cells. 2023; 12(4):526. https://doi.org/10.3390/cells12040526
Chicago/Turabian StyleBanerjee, Priyanka, Subhashree Kumaravel, Sukanya Roy, Niyanshi Gaddam, Johnny Odeh, Kayla J. Bayless, Shannon Glaser, and Sanjukta Chakraborty. 2023. "Conjugated Bile Acids Promote Lymphangiogenesis by Modulation of the Reactive Oxygen Species–p90RSK–Vascular Endothelial Growth Factor Receptor 3 Pathway" Cells 12, no. 4: 526. https://doi.org/10.3390/cells12040526
APA StyleBanerjee, P., Kumaravel, S., Roy, S., Gaddam, N., Odeh, J., Bayless, K. J., Glaser, S., & Chakraborty, S. (2023). Conjugated Bile Acids Promote Lymphangiogenesis by Modulation of the Reactive Oxygen Species–p90RSK–Vascular Endothelial Growth Factor Receptor 3 Pathway. Cells, 12(4), 526. https://doi.org/10.3390/cells12040526








