Endothelial Progenitor Cells May Be Related to Major Amputation after Angioplasty in Patients with Critical Limb Ischemia
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Population
2.3. Clinical Demographic Characteristics
2.4. Evaluation of Vascular Damage
2.5. Endothelial Dysfunction and Atherogenesis
2.6. Balloon Angioplasty
2.7. Endothelial Precursor Cells Determination
2.8. Clinical Follow-Up
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hardman, R.L.; Jazaeri, O.; Yi, J.; Smith, M.; Gupta, R. Overview of Classification Systems in Peripheral Artery Disease. Semin. Intervent. Radiol. 2014, 31, 378–388. [Google Scholar] [CrossRef] [PubMed]
- Serrano Hernando, F.J.; Conejero, A.M. Peripheral Artery Disease: Pathophysiology, Diagnosis and Treatment. Rev. Esp. Cardiol. 2007, 60, 969–982. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, S.S.; Vanella, L.; Abraham, N.G.; Scuto, S.; Marino, E.; Rocic, P. Pathophysiology of Chronic Peripheral Ischemia: New Perspectives. Ther. Adv. Chronic Dis. 2020, 11, 2040622319894466. [Google Scholar] [CrossRef]
- Agarwal, S.; Pitcavage, J.M.; Sud, K.; Thakkar, B. Burden of Readmissions Among Patients With Critical Limb Ischemia. J. Am. Coll. Cardiol. 2017, 69, 1897–1908. [Google Scholar] [CrossRef] [PubMed]
- Kolte, D.; Kennedy, K.F.; Shishehbor, M.H.; Abbott, J.D.; Khera, S.; Soukas, P.; Mamdani, S.T.; Hyder, O.N.; Drachman, D.E.; Aronow, H.D. Thirty-Day Readmissions After Endovascular or Surgical Therapy for Critical Limb Ischemia: Analysis of the 2013 to 2014 Nationwide Readmissions Databases. Circulation 2017, 136, 167–176. [Google Scholar] [CrossRef]
- Trujillo-Alcocer, J.C.; Hilarino Flores-Escartín, M.; López-Monterrubio, A.R.; Serrano-Lozano, J.A. Prevalencia de La Enfermedad Arterial Periférica En Población Mexicana Derechohabiente Del Hospital Regional Lic. Adolfo López Mateos, ISSSTE. Rev. Mex. Angiol. 2014, 42, 62–67. [Google Scholar]
- Cantú-Brito, C.; Chiquete, E.; Antezana-Castro, J.F.; Toapanta-Yanchapaxi, L.; Ochoa-Guzmán, A.; Ruiz-Sandoval, J.L. Peripheral Artery Disease in Outpatients with a Recent History of Acute Coronary Syndrome or at High Atherothrombotic Risk. Vascular 2020. [Google Scholar] [CrossRef] [PubMed]
- Murabito, J.M.; D’Agostino, R.B.; Silbershatz, H.; Wilson, P.W.F. Intermittent Claudication. A Risk Profile from The Framingham Heart Study. Circulation 1997, 96, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Criqui, M.H.; Vargas, V.; Denenberg, J.O.; Ho, E.; Allison, M.; Langer, R.D.; Gamst, A.; Bundens, W.P.; Fronek, A. Ethnicity and Peripheral Arterial Disease: The San Diego Population Study. Circulation 2005, 112, 2703–2707. [Google Scholar] [CrossRef]
- Ridker, P.M.; Stampfer, M.J.; Rifai, N. Novel Risk Factors for Systemic Atherosclerosis: A Comparison of C-Reactive Protein, Fibrinogen, Homocysteine, Lipoprotein(a), and Standard Cholesterol Screening as Predictors of Peripheral Arterial Disease. JAMA 2001, 285, 2481–2485. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wu, P.; Jiang, D.; Zhang, H.; Zhang, J.; Zong, Y.; Han, Y. Relationship between Serum Homocysteine, Fibrinogen, Lipoprotein-a Level, and Peripheral Arterial Disease: A Dose-Response Meta-Analysis. Eur. J. Med. Res. 2022, 27. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.M.; Zalos, G.; Halcox, J.P.J.; Schenke, W.H.; Waclawiw, M.A.; Quyyumi, A.A.; Finkel, T. Circulating Endothelial Progenitor Cells, Vascular Function, and Cardiovascular Risk. N. Engl. J. Med. 2003, 348, 593–600. [Google Scholar] [CrossRef]
- Schmidt-Lucke, C.; Rössig, L.; Fichtlscherer, S.; Vasa, M.; Britten, M.; Kämper, U.; Dimmeler, S.; Zeiher, A.M. Reduced Number of Circulating Endothelial Progenitor Cells Predicts Future Cardiovascular Events: Proof of Concept for the Clinical Importance of Endogenous Vascular Repair. Circulation 2005, 111, 2981–2987. [Google Scholar] [CrossRef]
- Klaphake, S.; de Leur, K.; Mulder, P.G.H.; Ho, G.H.; de Groot, H.G.; Veen, E.J.; Verhagen, H.J.M.; Van Der Laan, L. Mortality after Major Amputation in Elderly Patients with Critical Limb Ischemia. Clin. Interv. Aging 2017, 12, 1985–1992. [Google Scholar] [CrossRef]
- Ras, R.T.; Streppel, M.T.; Draijer, R.; Zock, P.L. Flow-Mediated Dilation and Cardiovascular Risk Prediction: A Systematic Review with Meta-Analysis. Int. J. Cardiol. 2013, 168, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Smadja, D.M.; Duong-Van-Huyen, J.P.; Dal Cortivo, L.; Blanchard, A.; Bruneval, P.; Emmerich, J.; Gaussem, P. Early Endothelial Progenitor Cells in Bone Marrow Are a Biomarker of Cell Therapy Success in Patients with Critical Limb Ischemia. Cytotherapy 2012, 14, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Yip, H.K.; Chang, L.T.; Chang, W.N.; Lu, C.H.; Liou, C.W.; Lan, M.Y.; Liu, J.S.; Youssef, A.A.; Chang, H.W. Level and Value of Circulating Endothelial Progenitor Cells in Patients After Acute Ischemic Stroke. Stroke 2008, 39, 69–74. [Google Scholar] [CrossRef]
- Hu, Y.; Davison, F.; Zhang, Z.; Xu, Q. Endothelial Replacement and Angiogenesis in Arteriosclerotic Lesions of Allografts Are Contributed by Circulating Progenitor Cells. Circulation 2003, 108, 3122–3127. [Google Scholar] [CrossRef]
- Reyes, M.; Dudek, A.; Jahagirdar, B.; Koodie, L.; Marker, P.H.; Verfaillie, C.M. Origin of Endothelial Progenitors in Human Postnatal Bone Marrow. J. Clin. Invest. 2002, 109, 337–346. [Google Scholar] [CrossRef]
- Shi, Q.; Rafii, S.; Wu Hong-De, M.; Wijelath, E.S.; Yu, C.; Ishida, A.; Fujita, Y.; Kothari, S.; Mohle, R.; Sauvage, L.R.; et al. Evidence for Circulating Bone Marrow-Derived Endothelial Cells. Blood 1998, 92, 362–367. [Google Scholar] [CrossRef]
- Bhattacharya, V.; McSweeney, P.A.; Shi, Q.; Bruno, B.; Ishida, A.; Nash, R.; Storb, R.F.; Sauvage, L.R.; Hammond, W.P.; Wu, M.H. De Enhanced Endothelialization and Microvessel Formation in Polyester Grafts Seeded with CD34+ Bone Marrow Cells: Presented to the Western Vascular Society, Whistler, BC, Canada, September 11, 1998. Blood 2000, 95, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Carmeliet, P. Mechanisms of Angiogenesis and Arteriogenesis. Nat. Med. 2000, 6, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Kerbel, R.; Folkman, J. Clinical Translation of Angiogenesis Inhibitors. Nat. Rev. Cancer 2002, 2, 727–739. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, A.; Bennett, M. Progenitor Cell-Derived Smooth Muscle Cells in Vascular Disease. Biochem. Pharmacol. 2010, 79, 1706–1713. [Google Scholar] [CrossRef]
- Raitakari, O.T.; Celermajer, D.S. Testing for Endothelial Dysfunction. Ann. Med. 2000, 32, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Playford, D.A.; Watts, G.F. Special Article: Non-Invasive Measurement of Endothelial Function. Clin. Exp. Pharmacol. Physiol. 1998, 25, 640–643. [Google Scholar] [CrossRef]
- Suárez-Cuenca, J.A.; Robledo-Nolasco, R.; Alcántara-Meléndez, M.A.; Díaz Hernández, L.J.; Vera-Gómez, E.; Hernández-Patricio, A.; Sánchez-Díaz, K.S.; Buendía-Gutiérrez, J.A.; Contreras-Ramos, A.; Ruíz-Hernández, A.S.; et al. Coronary circulating mononuclear progenitor cells and soluble biomarkers in the cardiovascular prognosis after coronary angioplasty. J. Cell. Mol. Med. 2019, 23, 4844–4849. [Google Scholar] [CrossRef]
- Heinen, Y.; Stegemann, E.; Sansone, R.; Benedens, K.; Wagstaff, R.; Balzer, J.; Rassaf, T.; Lauer, T.; Kelm, M.; Heiss, C. Local Association between Endothelial Dysfunction and Intimal Hyperplasia: Relevance in Peripheral Artery Disease. J. Am. Heart Assoc. 2015, 4. [Google Scholar] [CrossRef]
- Provance, J.B.; Spertus, J.A.; Jones, P.G.; Hoffman, M.A.; Bunte, M.C.; Vogel, T.R.; Mena-Hurtado, C.; Smolderen, K.G. Variability in 30-day major amputation rates following endovascular peripheral vascular intervention for critical limb ischemia. Vasc. Med. 2022, 27, 350–357. [Google Scholar] [CrossRef]
- Jupiter, D.C.; LaFontaine, J.; Barshes, N.; Wukich, D.K.; Shibuya, N. Transmetatarsal and Minor Amputation Versus Major Leg Amputation: 30-Day Readmissions, Reamputations, and Complications. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 2020, 59, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L.; Whealon, M.D.; Kabutey, N.K.; Kuo, I.J.; Sgroi, M.D.; Fujitani, R.M. Outcomes of open and endovascular lower extremity revascularization in active smokers with advanced peripheral arterial disease. J. Vasc. Surg. 2017, 65, 1680–1689. [Google Scholar] [CrossRef]
- Shishehbor, M.H.; Griffin, J.; Crowder, W.; Kucher, T.; León, L.R., Jr.; McClure, J.M., 2nd; Sood, A.; Montero-Baker, M. Acute Real-World Outcomes From the Phoenix Post-Approval Registry. J. Invasive Cardiol. 2022, 34, E1–E7. [Google Scholar] [PubMed]
- Cheun, T.J.; Jayakumar, L.; Sideman, M.J.; Ferrer, L.; Mitromaras, C.; Miserlis, D.; Davies, M.G. Short-term contemporary outcomes for staged versus primary lower limb amputation in diabetic foot disease. J. Vasc. Surg. 2020, 72, 658–666.e2. [Google Scholar] [CrossRef]
- Sung, S.H.; Wu, T.C.; Chen, J.S.; Chen, Y.H.; Huang, P.H.; Lin, S.J.; Shih, C.C.; Chen, J.W. Reduced Number and Impaired Function of Circulating Endothelial Progenitor Cells in Patients with Abdominal Aortic Aneurysm. Int. J. Cardiol. 2013, 168, 1070–1077. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, F.; Pasceri, V.; Cianfrocca, C.; Vitale, C.; Speciale, G.; Gaudio, C.; Rosano, G.M.C.; Mercuro, G. Angiotensin II Receptor Antagonism with Telmisartan Increases Number of Endothelial Progenitor Cells in Normotensive Patients with Coronary Artery Disease: A Randomized, Double-Blind, Placebo-Controlled Study. Atherosclerosis 2010, 210, 510–515. [Google Scholar] [CrossRef]
- Denollet, J.; van Felius, R.A.; Lodder, P.; Mommersteeg, P.M.; Goovaerts, I.; Possemiers, N.; Vanhees, L.; Beckers, P.; Pattyn, N.; Van Craenenbroeck, E.M. Predictive Value of Type D Personality for Impaired Endothelial Function in Patients with Coronary Artery Disease. Int. J. Cardiol. 2018, 259, 205–210. [Google Scholar] [CrossRef]
- Berezin, A.E.; Kremzer, A.A. Circulating Endothelial Progenitor Cells as Markers for Severity of Ischemic Chronic Heart Failure. J. Card. Fail. 2014, 20, 438–447. [Google Scholar] [CrossRef]
- Balistreri, C.R.; Buffa, S.; Pisano, C.; Lio, D.; Ruvolo, G.; Mazzesi, G. Are Endothelial Progenitor Cells the Real Solution for Cardiovascular Diseases? Focus on Controversies and Perspectives. BioMed Res. Int. 2015, 2015, 835934. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Zhao, Z.; Jiang, W.; Zhu, P.; Zhou, N.; Huang, X. A Review Into the Insights of the Role of Endothelial Progenitor Cells on Bone Biology. Front. Cell Dev. Biol. 2022, 10, 925. [Google Scholar] [CrossRef]

| Antibody | Cell Marker | Fluorochrome/ Dilution | EPC Subpopulations Identified |
|---|---|---|---|
| CD45 | Lymphocytes, endothelial, and/or vascular cells. | Vioblue 1:60 | CD45+CD34+CD133+ CD45+CD34+CD184+ CD45+CD34+CD133+CD184+ CD45+CD34+KDR+ CD45+CD34+KDR+CD133+ CD45+CD34+KDR+CD184+ |
| CD34 | Endothelial and/or vascular cells | FITC 1:20 | |
| KDR(VEGFR-2) | Membrane marker of endothelial cells | APC 1:60 | |
| CD133 | Endothelial progenitor cells | PE 1:50 | |
| CD184 | Hematopoietic stem cells and endothelial cells | PE-Vio770 1:20 |
| All (n = 20) | Non-Limb Amputation (n = 12) | Limb Amputation * (n = 8) | p-Value | |
|---|---|---|---|---|
| Age (years old) | 68.0 (64.7–76.5) | 66.0 (55.0, 69.0) | 68.0 (62.0, 70.5) | 0.19 |
| Smoking | 10 (50.0) | 2 (25.0) | 8 (66.6) | 0.03 |
| Comorbidities | ||||
| DM | 9 (45.0) | 5 (41.6) | 4 (50.0) | 0.53 |
| DM + Hyp | 4 (20.0) | 3 (25.0) | 1 (12.5) | 0.46 |
| DM + Hyp + CVD | 4 (20.0) | 2 (16.7) | 2 (25.0) | 0.53 |
| DM + Hyp + CVD + Others | 3 (15.0) | 2 (16.7) | 1 (12.5) | 0.66 |
| Vascular profile | ||||
| Rutherford | ||||
| 3 (15.0) 17 (85.0) | 1 (8.3) 11 (91.7) | 2 (25.0) 6 (75) | 0.34 0.34 |
| Wifi | ||||
| 6 (30.0) 2 (10.0) 8 (40.0) 4 (20.0) | 6 (50.0) 2 (16.7) 3 (25.0) 1 (8.3) | 0 (0.0) 0 (0.0) 5 (62.5) 3 (37.5) | 0.02 0.34 0.11 0.15 |
| Ankle-to-Brachial Ratio | 0.52 ± 0.19 | 0.60 (0.50, 0.60) | 0.53 (0.42, 0.67) | 0.44 |
| Flow-Mediated Dilation | −2.27 ± 8.98 | 7.66 (4.91, 11.3) | −9.2 (−10.6, −6.03) | <0.001 |
| Angioplasty Site Femoral + tibial and/or popliteal 11 (55.0) 5 (40.0) 6 (75.0) 0.16 Tibial alone and/or tibial + popliteal 9 (45.0) 7 (60.0) 2 (25.0) 0.16 Endothelial Progenitor Cells | ||||
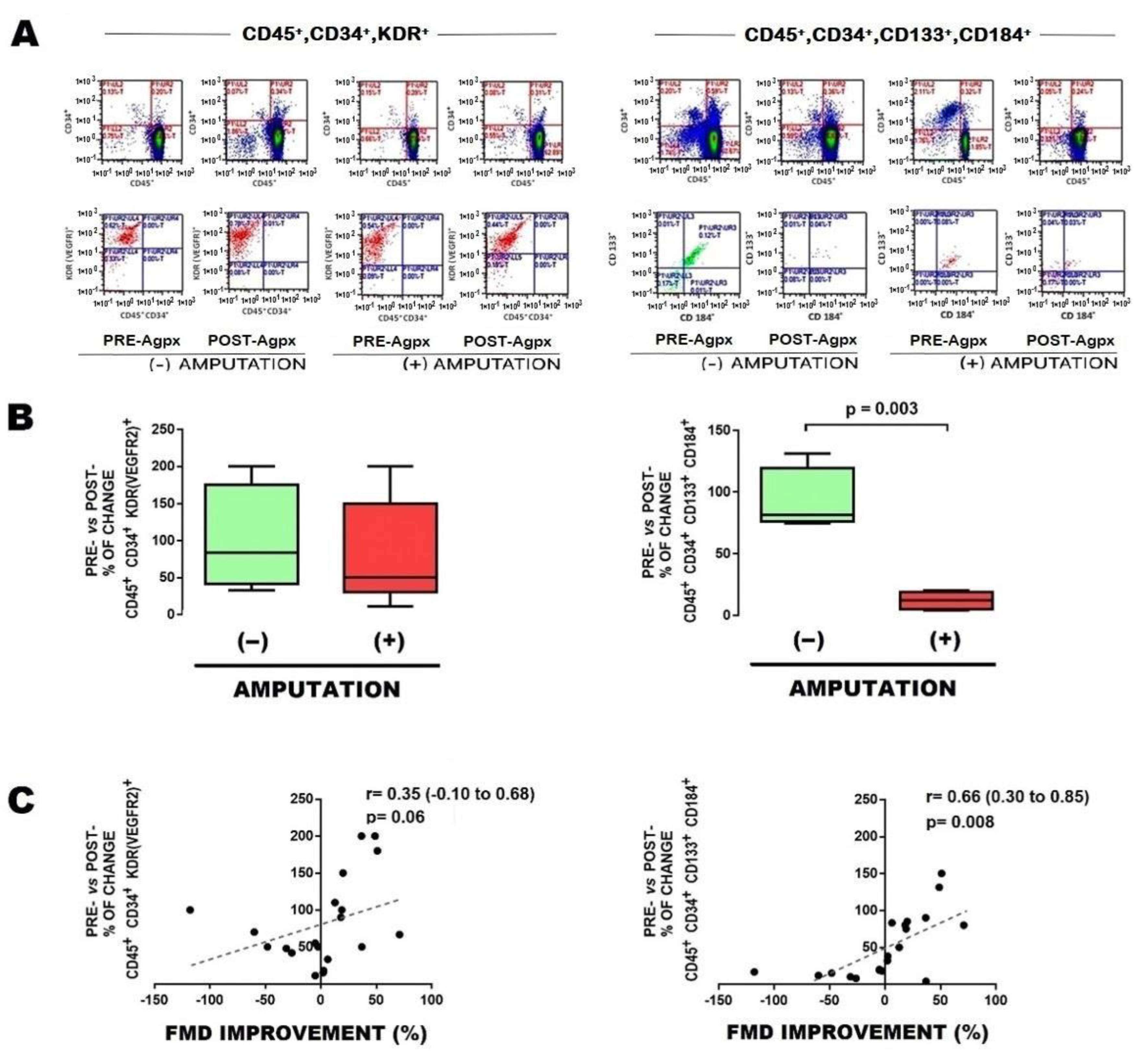
| CD45,CD34, KDR | ||||
| Pre-aptx | 0.03 (0.03, 0.06) | 0.03 (0.02, 0.03) | 0.04 (0.03, 0.09) | 0.04 |
| Post-aptx | 0.02 (0.15, 0.05) | 0.02 (0.01, 0.03) | 0.02 (0.01, 0.08) | 0.21 |
| % of change | 66.7 (41.7, 150.0) | 83.3 (41.7, 175.0) | 50.0 (30.6, 150.0) | 0.36 |
| CD45,CD34,CD133,184 | ||||
| Pre-aptx | 0.16 (0.05, 0.23) | 0.16 (0.06, 0.28) | 0.13 (0.05, 0.23) | 0.34 |
| Post-aptx | 0.02 (0.01, 0.14) | 0.13 (0.05, 0.35) | 0.01 (0.01, 0.01) | 0.04 |
| % of change | 47.5 (7.9, 82.5) | 81.7 (76.3, 119.3) | 10.8 (4.3, 19.2) | <0.01 |
| EPC Subpopulation | Non-Limb Amputation (n = 12) | Limb Amputation (n = 8) | SE | SP | RR (CI95%) p-Value | |
|---|---|---|---|---|---|---|
| CD45,CD34, KDR (Pre-aptx) | 2 (16.7) | 6 (75) | 0.75 | 0.83 | 4.5 (1.2, 17.0) 0.01 |  |
| CD45,CD34,CD133,184 (Pre-aptx) | 9 (75.0) | 3 (37.5) | 0.37 | 0.25 | 0.4 (0.1, 1.2) 0.11 | |
| CD45,CD34, KDR (% of change) | 9 (75.0) | 3 (37.5) | 0.37 | 0.25 | 0.4 (0.1, 1.2) 0.11 | |
| CD45,CD34,CD133,184 (% of change) | 9 (75.0) | 2 (25.0) | 0.25 | 0.25 | 0.3 (0.1, 1.0) 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santillán-Cortez, D.; Vera-Gómez, E.; Hernández-Patricio, A.; Ruíz-Hernández, A.S.; Gutiérrez-Buendía, J.A.; De la Vega-Moreno, K.; Rizo-García, Y.A.; Loman-Zuñiga, O.A.; Escotto-Sánchez, I.; Rodríguez-Trejo, J.M.; et al. Endothelial Progenitor Cells May Be Related to Major Amputation after Angioplasty in Patients with Critical Limb Ischemia. Cells 2023, 12, 584. https://doi.org/10.3390/cells12040584
Santillán-Cortez D, Vera-Gómez E, Hernández-Patricio A, Ruíz-Hernández AS, Gutiérrez-Buendía JA, De la Vega-Moreno K, Rizo-García YA, Loman-Zuñiga OA, Escotto-Sánchez I, Rodríguez-Trejo JM, et al. Endothelial Progenitor Cells May Be Related to Major Amputation after Angioplasty in Patients with Critical Limb Ischemia. Cells. 2023; 12(4):584. https://doi.org/10.3390/cells12040584
Chicago/Turabian StyleSantillán-Cortez, Daniel, Eduardo Vera-Gómez, Alejandro Hernández-Patricio, Atzín Suá Ruíz-Hernández, Juan Ariel Gutiérrez-Buendía, Karen De la Vega-Moreno, Yasser Alberto Rizo-García, Oscar Antonio Loman-Zuñiga, Ignacio Escotto-Sánchez, Juan Miguel Rodríguez-Trejo, and et al. 2023. "Endothelial Progenitor Cells May Be Related to Major Amputation after Angioplasty in Patients with Critical Limb Ischemia" Cells 12, no. 4: 584. https://doi.org/10.3390/cells12040584
APA StyleSantillán-Cortez, D., Vera-Gómez, E., Hernández-Patricio, A., Ruíz-Hernández, A. S., Gutiérrez-Buendía, J. A., De la Vega-Moreno, K., Rizo-García, Y. A., Loman-Zuñiga, O. A., Escotto-Sánchez, I., Rodríguez-Trejo, J. M., Téllez-González, M. A., Toledo-Lozano, C. G., Ortega-Rosas, T., García, S., Mondragón-Terán, P., & Suárez-Cuenca, J. A. (2023). Endothelial Progenitor Cells May Be Related to Major Amputation after Angioplasty in Patients with Critical Limb Ischemia. Cells, 12(4), 584. https://doi.org/10.3390/cells12040584








