Interaction between Gut Microbiota and Celiac Disease: From Pathogenesis to Treatment
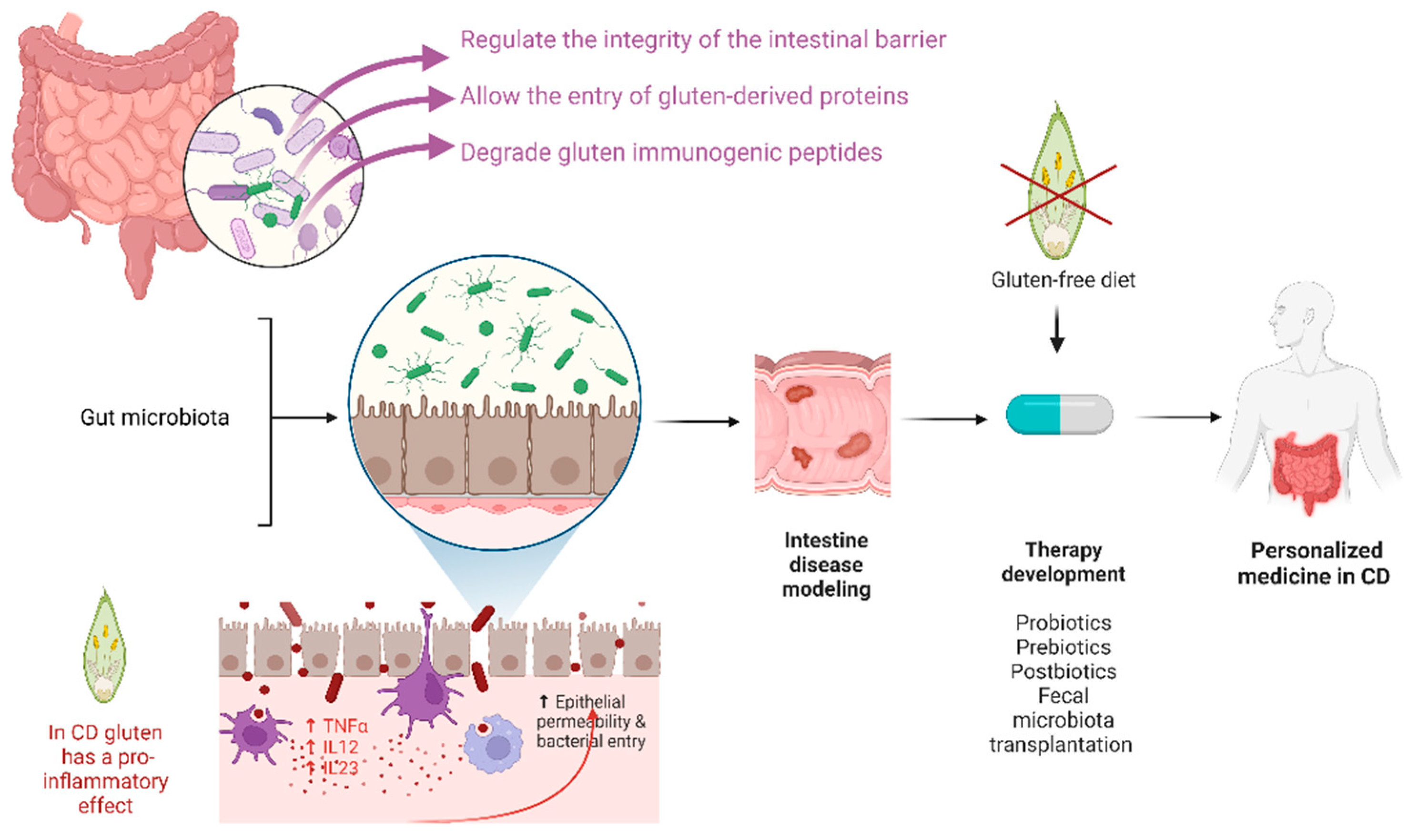
Abstract
:1. Introduction
1.1. Pathogenesis
1.2. The Role of Gut Microbiota in the Pathogenesis of Celiac Disease
1.3. Clinical and Therapeutic Implications
2. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Singh, P.; Arora, A.; Strand, T.A.; Leffler, D.A.; Catassi, C.; Green, P.H.; Kelly, C.P.; Ahuja, V.; Makharia, G.K. Global Prevalence of Celiac Disease: Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 823–836.e2. [Google Scholar] [CrossRef] [Green Version]
- Fasano, A.; Catassi, C. Celiac Disease. N. Engl. J. Med. 2012, 367, 2419–2426. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, B.; Rubio-Tapia, A. Epidemiology, Presentation, and Diagnosis of Celiac Disease. Gastroenterology 2021, 160, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Caio, G.; Volta, U.; Sapone, A.; Leffler, D.A.; De Giorgio, R.; Catassi, C.; Fasano, A. Celiac Disease: A Comprehensive Current Review. BMC Med. 2019, 17, 142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Toma, A.; Volta, U.; Auricchio, R.; Castillejo, G.; Sanders, D.S.; Cellier, C.; Mulder, C.J.; Lundin, K.E.A. European Society for the Study of Coeliac Disease (ESsCD) Guideline for Coeliac Disease and Other Gluten-Related Disorders. United Eur. Gastroenterol. J. 2019, 7, 583–613. [Google Scholar] [CrossRef]
- Green, P.H.R.; Lebwohl, B.; Greywoode, R. Celiac Disease. J. Allergy Clin. Immunol. 2015, 135, 1099–1106. [Google Scholar] [CrossRef] [PubMed]
- Lohi, S.; Mustalahti, K.; Kaukinen, K.; Laurila, K.; Collin, P.; Rissanen, H.; Lohi, O.; Bravi, E.; Gasparin, M.; Reunanen, A.; et al. Increasing Prevalence of Coeliac Disease over Time. Aliment. Pharmacol. Ther. 2007, 26, 1217–1225. [Google Scholar] [CrossRef]
- Integration of Genetic and Immunological Insights into a Model of Celiac Disease Pathogenesis—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/21219178/ (accessed on 28 November 2022).
- Dominguez-Bello, M.G.; Costello, E.K.; Contreras, M.; Magris, M.; Hidalgo, G.; Fierer, N.; Knight, R. Delivery Mode Shapes the Acquisition and Structure of the Initial Microbiota across Multiple Body Habitats in Newborns. Proc. Natl. Acad. Sci. USA 2010, 107, 11971–11975. [Google Scholar] [CrossRef] [Green Version]
- Decker, E.; Engelmann, G.; Findeisen, A.; Gerner, P.; Laass, M.; Ney, D.; Posovszky, C.; Hoy, L.; Hornef, M.W. Cesarean Delivery Is Associated with Celiac Disease but Not Inflammatory Bowel Disease in Children. Pediatrics 2010, 125, e1433–e1440. [Google Scholar] [CrossRef]
- Canova, C.; Zabeo, V.; Pitter, G.; Romor, P.; Baldovin, T.; Zanotti, R.; Simonato, L. Association of Maternal Education, Early Infections, and Antibiotic Use with Celiac Disease: A Population-Based Birth Cohort Study in Northeastern Italy. Am. J. Epidemiol. 2014, 180, 76–85. [Google Scholar] [CrossRef] [Green Version]
- Medina, M.; Izquierdo, E.; Ennahar, S.; Sanz, Y. Differential Immunomodulatory Properties of Bifidobacterium Logum Strains: Relevance to Probiotic Selection and Clinical Applications. Clin. Exp. Immunol. 2007, 150, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Baba, N.; Samson, S.; Bourdet-Sicard, R.; Rubio, M.; Sarfati, M. Commensal Bacteria Trigger a Full Dendritic Cell Maturation Program That Promotes the Expansion of Non-Tr1 Suppressor T Cells. J. Leukoc. Biol. 2008, 84, 468–476. [Google Scholar] [CrossRef]
- Sanz, Y.; Sánchez, E.; Marzotto, M.; Calabuig, M.; Torriani, S.; Dellaglio, F. Differences in Faecal Bacterial Communities in Coeliac and Healthy Children as Detected by PCR and Denaturing Gradient Gel Electrophoresis. FEMS Immunol. Med. Microbiol. 2007, 51, 562–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collado, M.C.; Donat, E.; Ribes-Koninckx, C.; Calabuig, M.; Sanz, Y. Specific Duodenal and Faecal Bacterial Groups Associated with Paediatric Coeliac Disease. J. Clin. Pathol. 2009, 62, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohamadzadeh, M.; Olson, S.; Kalina, W.V.; Ruthel, G.; Demmin, G.L.; Warfield, K.L.; Bavari, S.; Klaenhammer, T.R. Lactobacilli Activate Human Dendritic Cells That Skew T Cells toward T Helper 1 Polarization. Proc. Natl. Acad. Sci. USA 2005, 102, 2880–2885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorenzo Pisarello, M.J.; Vintiñi, E.O.; González, S.N.; Pagani, F.; Medina, M.S. Decrease in Lactobacilli in the Intestinal Microbiota of Celiac Children with a Gluten-Free Diet, and Selection of Potentially Probiotic Strains. Can. J. Microbiol. 2015, 61, 32–37. [Google Scholar] [CrossRef]
- Schippa, S.; Iebba, V.; Barbato, M.; Di Nardo, G.; Totino, V.; Checchi, M.P.; Longhi, C.; Maiella, G.; Cucchiara, S.; Conte, M.P. A Distinctive “microbial Signature” in Celiac Pediatric Patients. BMC Microbiol. 2010, 10, 175. [Google Scholar] [CrossRef]
- Sánchez, E.; Ribes-Koninckx, C.; Calabuig, M.; Sanz, Y. Intestinal Staphylococcus spp. and Virulent Features Associated with Coeliac Disease. J. Clin. Pathol. 2012, 65, 830–834. [Google Scholar] [CrossRef]
- Petersen, J.; Ciacchi, L.; Tran, M.T.; Loh, K.L.; Kooy-Winkelaar, Y.; Croft, N.P.; Hardy, M.Y.; Chen, Z.; McCluskey, J.; Anderson, R.P.; et al. T Cell Receptor Cross-Reactivity between Gliadin and Bacterial Peptides in Celiac Disease. Nat. Struct. Mol. Biol. 2020, 27, 49–61. [Google Scholar] [CrossRef]
- Kim, S.M.; Mayassi, T.; Jabri, B. Innate Immunity: Actuating the Gears of Celiac Disease Pathogenesis. Best Pract. Res. Clin. Gastroenterol. 2015, 29, 425–435. [Google Scholar] [CrossRef] [Green Version]
- Caminero, A.; McCarville, J.L.; Galipeau, H.J.; Deraison, C.; Bernier, S.P.; Constante, M.; Rolland, C.; Meisel, M.; Murray, J.A.; Yu, X.B.; et al. Duodenal Bacterial Proteolytic Activity Determines Sensitivity to Dietary Antigen through Protease-Activated Receptor-2. Nat. Commun. 2019, 10, 1198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Araya, R.E.; Jury, J.; Bondar, C.; Verdu, E.F.; Chirdo, F.G. Intraluminal Administration of Poly I:C Causes an Enteropathy That Is Exacerbated by Administration of Oral Dietary Antigen. PLoS ONE 2014, 9, e99236. [Google Scholar] [CrossRef] [PubMed]
- Cristofori, F.; Indrio, F.; Miniello, V.L.; De Angelis, M.; Francavilla, R. Probiotics in Celiac Disease. Nutrients 2018, 10, 1824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olivares, M.; Neef, A.; Castillejo, G.; Palma, G.D.; Varea, V.; Capilla, A.; Palau, F.; Nova, E.; Marcos, A.; Polanco, I.; et al. The HLA-DQ2 Genotype Selects for Early Intestinal Microbiota Composition in Infants at High Risk of Developing Coeliac Disease. Gut 2015, 64, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, E.; De Palma, G.; Capilla, A.; Nova, E.; Pozo, T.; Castillejo, G.; Varea, V.; Marcos, A.; Garrote, J.A.; Polanco, I.; et al. Influence of Environmental and Genetic Factors Linked to Celiac Disease Risk on Infant Gut Colonization by Bacteroides Species. Appl. Environ. Microbiol. 2011, 77, 5316–5323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Palma, G.; Capilla, A.; Nadal, I.; Nova, E.; Pozo, T.; Varea, V.; Polanco, I.; Castillejo, G.; López, A.; Garrote, J.A.; et al. Interplay between Human Leukocyte Antigen Genes and the Microbial Colonization Process of the Newborn Intestine. Curr. Issues Mol. Biol. 2010, 12, 1–10. [Google Scholar]
- Leonard, M.M.; Karathia, H.; Pujolassos, M.; Troisi, J.; Valitutti, F.; Subramanian, P.; Camhi, S.; Kenyon, V.; Colucci, A.; Serena, G.; et al. Multi-Omics Analysis Reveals the Influence of Genetic and Environmental Risk Factors on Developing Gut Microbiota in Infants at Risk of Celiac Disease. Microbiome 2020, 8, 130. [Google Scholar] [CrossRef]
- Akobeng, A.K.; Ramanan, A.V.; Buchan, I.; Heller, R.F. Effect of Breast Feeding on Risk of Coeliac Disease: A Systematic Review and Meta-Analysis of Observational Studies. Arch. Dis. Child. 2006, 91, 39–43. [Google Scholar] [CrossRef] [Green Version]
- Szajewska, H.; Chmielewska, A.; Pieścik-Lech, M.; Ivarsson, A.; Kolacek, S.; Koletzko, S.; Mearin, M.L.; Shamir, R.; Auricchio, R.; Troncone, R.; et al. Systematic Review: Early Infant Feeding and the Prevention of Coeliac Disease. Aliment. Pharmacol. Ther. 2012, 36, 607–618. [Google Scholar] [CrossRef] [Green Version]
- Mårild, K.; Ludvigsson, J.; Sanz, Y.; Ludvigsson, J.F. Antibiotic Exposure in Pregnancy and Risk of Coeliac Disease in Offspring: A Cohort Study. BMC Gastroenterol. 2014, 14, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Myléus, A.; Hernell, O.; Gothefors, L.; Hammarström, M.-L.; Persson, L.-Å.; Stenlund, H.; Ivarsson, A. Early Infections Are Associated with Increased Risk for Celiac Disease: An Incident Case-Referent Study. BMC Pediatr. 2012, 12, 194. [Google Scholar] [CrossRef] [PubMed]
- Kemppainen, K.M.; Vehik, K.; Lynch, K.F.; Larsson, H.E.; Canepa, R.J.; Simell, V.; Koletzko, S.; Liu, E.; Simell, O.G.; Toppari, J.; et al. Association Between Early-Life Antibiotic Use and the Risk of Islet or Celiac Disease Autoimmunity. JAMA Pediatr. 2017, 171, 1217–1225. [Google Scholar] [CrossRef]
- Mårild, K.; Ye, W.; Lebwohl, B.; Green, P.H.R.; Blaser, M.J.; Card, T.; Ludvigsson, J.F. Antibiotic Exposure and the Development of Coeliac Disease: A Nationwide Case-Control Study. BMC Gastroenterol. 2013, 13, 109. [Google Scholar] [CrossRef] [Green Version]
- Dydensborg Sander, S.; Nybo Andersen, A.-M.; Murray, J.A.; Karlstad, Ø.; Husby, S.; Størdal, K. Association Between Antibiotics in the First Year of Life and Celiac Disease. Gastroenterology 2019, 156, 2217–2229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stene, L.C.; Honeyman, M.C.; Hoffenberg, E.J.; Haas, J.E.; Sokol, R.J.; Emery, L.; Taki, I.; Norris, J.M.; Erlich, H.A.; Eisenbarth, G.S.; et al. Rotavirus Infection Frequency and Risk of Celiac Disease Autoimmunity in Early Childhood: A Longitudinal Study. Am. J. Gastroenterol. 2006, 101, 2333–2340. [Google Scholar] [CrossRef] [PubMed]
- Gatti, S.; Lionetti, E.; Balanzoni, L.; Verma, A.K.; Galeazzi, T.; Gesuita, R.; Scattolo, N.; Cinquetti, M.; Fasano, A.; Catassi, C.; et al. Increased Prevalence of Celiac Disease in School-Age Children in Italy. Clin. Gastroenterol. Hepatol. 2020, 18, 596–603. [Google Scholar] [CrossRef]
- Lindfors, K.; Lin, J.; Lee, H.-S.; Hyöty, H.; Nykter, M.; Kurppa, K.; Liu, E.; Koletzko, S.; Rewers, M.; Hagopian, W.; et al. Metagenomics of the Faecal Virome Indicate a Cumulative Effect of Enterovirus and Gluten Amount on the Risk of Coeliac Disease Autoimmunity in Genetically at Risk Children: The TEDDY Study. Gut 2020, 69, 1416–1422. [Google Scholar] [CrossRef] [Green Version]
- Lähdeaho, M.L.; Lehtinen, M.; Rissa, H.R.; Hyöty, H.; Reunala, T.; Mäki, M. Antipeptide Antibodies to Adenovirus E1b Protein Indicate Enhanced Risk of Celiac Disease and Dermatitis Herpetiformis. Int. Arch. Allergy Immunol. 1993, 101, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Bouziat, R.; Hinterleitner, R.; Brown, J.J.; Stencel-Baerenwald, J.E.; Ikizler, M.; Mayassi, T.; Meisel, M.; Kim, S.M.; Discepolo, V.; Pruijssers, A.J.; et al. Reovirus Infection Triggers Inflammatory Responses to Dietary Antigens and Development of Celiac Disease. Science 2017, 356, 44–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corouge, M.; Loridant, S.; Fradin, C.; Salleron, J.; Damiens, S.; Moragues, M.D.; Souplet, V.; Jouault, T.; Robert, R.; Dubucquoi, S.; et al. Humoral Immunity Links Candida Albicans Infection and Celiac Disease. PLoS ONE 2015, 10, e0121776. [Google Scholar] [CrossRef]
- Baldi, S.; Menicatti, M.; Nannini, G.; Niccolai, E.; Russo, E.; Ricci, F.; Pallecchi, M.; Romano, F.; Pedone, M.; Poli, G.; et al. Free Fatty Acids Signature in Human Intestinal Disorders: Significant Association between Butyric Acid and Celiac Disease. Nutrients 2021, 13, 742. [Google Scholar] [CrossRef] [PubMed]
- Olivares, M.; Benítez-Páez, A.; de Palma, G.; Capilla, A.; Nova, E.; Castillejo, G.; Varea, V.; Marcos, A.; Garrote, J.A.; Polanco, I.; et al. Increased Prevalence of Pathogenic Bacteria in the Gut Microbiota of Infants at Risk of Developing Celiac Disease: The PROFICEL Study. Gut Microbes 2018, 9, 551–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sellitto, M.; Bai, G.; Serena, G.; Fricke, W.F.; Sturgeon, C.; Gajer, P.; White, J.R.; Koenig, S.S.K.; Sakamoto, J.; Boothe, D.; et al. Proof of Concept of Microbiome-Metabolome Analysis and Delayed Gluten Exposure on Celiac Disease Autoimmunity in Genetically at-Risk Infants. PLoS ONE 2012, 7, e33387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kristensen, K.; Henriksen, L. Cesarean Section and Disease Associated with Immune Function. J. Allergy Clin. Immunol. 2016, 137, 587–590. [Google Scholar] [CrossRef] [Green Version]
- Kverka, M.; Zakostelska, Z.; Klimesova, K.; Sokol, D.; Hudcovic, T.; Hrncir, T.; Rossmann, P.; Mrazek, J.; Kopecny, J.; Verdu, E.F.; et al. Oral Administration of Parabacteroides Distasonis Antigens Attenuates Experimental Murine Colitis through Modulation of Immunity and Microbiota Composition. Clin. Exp. Immunol. 2011, 163, 250–259. [Google Scholar] [CrossRef]
- Olshan, K.L.; Leonard, M.M.; Serena, G.; Zomorrodi, A.R.; Fasano, A. Gut Microbiota in Celiac Disease: Microbes, Metabolites, Pathways and Therapeutics. Expert Rev. Clin. Immunol. 2020, 16, 1075–1092. [Google Scholar] [CrossRef]
- Mårild, K.; Kahrs, C.R.; Tapia, G.; Stene, L.C.; Størdal, K. Infections and Risk of Celiac Disease in Childhood: A Prospective Nationwide Cohort Study. Am. J. Gastroenterol. 2015, 110, 1475–1484. [Google Scholar] [CrossRef]
- Arcila-Galvis, J.E.; Loria-Kohen, V.; Ramírez de Molina, A.; Carrillo de Santa Pau, E.; Marcos-Zambrano, L.J. A Comprehensive Map of Microbial Biomarkers along the Gastrointestinal Tract for Celiac Disease Patients. Front. Microbiol. 2022, 13, 956119. [Google Scholar] [CrossRef] [PubMed]
- Chibbar, R.; Dieleman, L.A. The Gut Microbiota in Celiac Disease and Probiotics. Nutrients 2019, 11, 2375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Francavilla, R.; Cristofori, F.; Vacca, M.; Barone, M.; De Angelis, M. Advances in Understanding the Potential Therapeutic Applications of Gut Microbiota and Probiotic Mediated Therapies in Celiac Disease. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, A.; Cerrone, R.; Capobianco, D.; Filardo, S.; Mancini, P.; Zanni, F.; Fanelli, S.; Mastromarino, P.; Mosca, L. A Probiotic Preparation Hydrolyzes Gliadin and Protects Intestinal Cells from the Toxicity of Pro-Inflammatory Peptides. Nutrients 2020, 12, 495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liptak, R.; Gromova, B.; Maronek, M.; Gardlik, R. Reverse Phenotype Transfer via Fecal Microbial Transplantation in Inflammatory Bowel Disease. Med. Hypotheses 2019, 122, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Al, K.F.; Craven, L.J.; Gibbons, S.; Parvathy, S.N.; Wing, A.C.; Graf, C.; Parham, K.A.; Kerfoot, S.M.; Wilcox, H.; Burton, J.P.; et al. Fecal Microbiota Transplantation Is Safe and Tolerable in Patients with Multiple Sclerosis: A Pilot Randomized Controlled Trial. Mult. Scler. J. Exp. Transl. Clin. 2022, 8, 20552173221086664. [Google Scholar] [CrossRef]
- Wang, S.; Xu, M.; Wang, W.; Cao, X.; Piao, M.; Khan, S.; Yan, F.; Cao, H.; Wang, B. Systematic Review: Adverse Events of Fecal Microbiota Transplantation. PLoS ONE 2016, 11, e0161174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belvoncikova, P.; Maronek, M.; Gardlik, R. Gut Dysbiosis and Fecal Microbiota Transplantation in Autoimmune Diseases. Int. J. Mol. Sci. 2022, 23, 10729. [Google Scholar] [CrossRef]
- van Beurden, Y.H.; van Gils, T.; van Gils, N.A.; Kassam, Z.; Mulder, C.J.J.; Aparicio-Pagés, N. Serendipity in Refractory Celiac Disease: Full Recovery of Duodenal Villi and Clinical Symptoms after Fecal Microbiota Transfer. J. Gastrointest. Liver. Dis. 2016, 25, 385–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Golfeyz, S. Celiac Disease and Fecal Microbiota Transplantation: A New Beginning? Am. J. Gastroenterol. 2018, 113, 1256. [Google Scholar] [CrossRef]
- Zoghi, S.; Abbasi, A.; Heravi, F.S.; Somi, M.H.; Nikniaz, Z.; Moaddab, S.Y.; Ebrahimzadeh Leylabadlo, H. The Gut Microbiota and Celiac Disease: Pathophysiology, Current Perspective and New Therapeutic Approaches. Crit. Rev. Food Sci. Nutr. 2022, 1–21. [Google Scholar] [CrossRef]
| Mechanisms | Study |
|---|---|
| Role of Environmental Factors | |
| Bacterial expression of epitopes that mimic gliadin | Petersen [20] |
| Gram- negative bacterial lipopolysaccharide expression as a trigger for both the innate and adaptive immune systems | Kim [21] |
| Pseudomonas aeruginosa + gluten causes increased inflammation | Caminero [22] |
| Viral infections as a trigger for activation of the innate immune system | Araya [23] |
| Role of Microbiota Itself | |
| Cristofori [24] |
| Role of Genetics | |
| The genotype of infants at familial risk for CD influences the composition of the early gut microbiota | Olivares [25] |
| Infants genetically predisposed to CD show different gut microbiota composition (i.e., prevalence of Bacteroides) | Sanchez [26] De Palma [27] |
| Microbiome shifts observed in the first 6 months after birth in infants with a first-degree relative with CD can increase the risk for developing autoimmune diseases | Leonard [28] |
| Role of Perinatal Factors | |
| Cesarian section Higher risk of CD due to an increased amount of Enterococcus faecalis vs. a decreased abundance of Bacteroides and Parabacteroides | Leonard [28] |
Feeding type
| Akobeng [29] Szajewska [30] Leonard [28] |
Antibiotic use
| Marild [31] Myleus [32] Kemppainen [33] Marild [34] Dydensborg Sander [35] Canova [11] |
Gastrointestinal (GI) infections
| Marild [34] Stene [36] Gatti [37] Lindfors [38] Lahdeaho [39] Bouziat [40] Corouge [41] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, R.E.; Dispinzieri, G.; Elvevi, A.; Massironi, S. Interaction between Gut Microbiota and Celiac Disease: From Pathogenesis to Treatment. Cells 2023, 12, 823. https://doi.org/10.3390/cells12060823
Rossi RE, Dispinzieri G, Elvevi A, Massironi S. Interaction between Gut Microbiota and Celiac Disease: From Pathogenesis to Treatment. Cells. 2023; 12(6):823. https://doi.org/10.3390/cells12060823
Chicago/Turabian StyleRossi, Roberta Elisa, Giulia Dispinzieri, Alessandra Elvevi, and Sara Massironi. 2023. "Interaction between Gut Microbiota and Celiac Disease: From Pathogenesis to Treatment" Cells 12, no. 6: 823. https://doi.org/10.3390/cells12060823
APA StyleRossi, R. E., Dispinzieri, G., Elvevi, A., & Massironi, S. (2023). Interaction between Gut Microbiota and Celiac Disease: From Pathogenesis to Treatment. Cells, 12(6), 823. https://doi.org/10.3390/cells12060823







