Tertiary Lymphoid Structures (TLSs) and Stromal Blood Vessels Have Significant and Heterogeneous Impact on Recurrence, Lymphovascular and Perineural Invasion amongst Breast Cancer Molecular Subtypes
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients’ Selection and Ethical Issues
2.2. Primary Processing, Histopathology and FFPE Specimens’ Selection for Immunohistochemistry
2.3. Immunohistochemistry
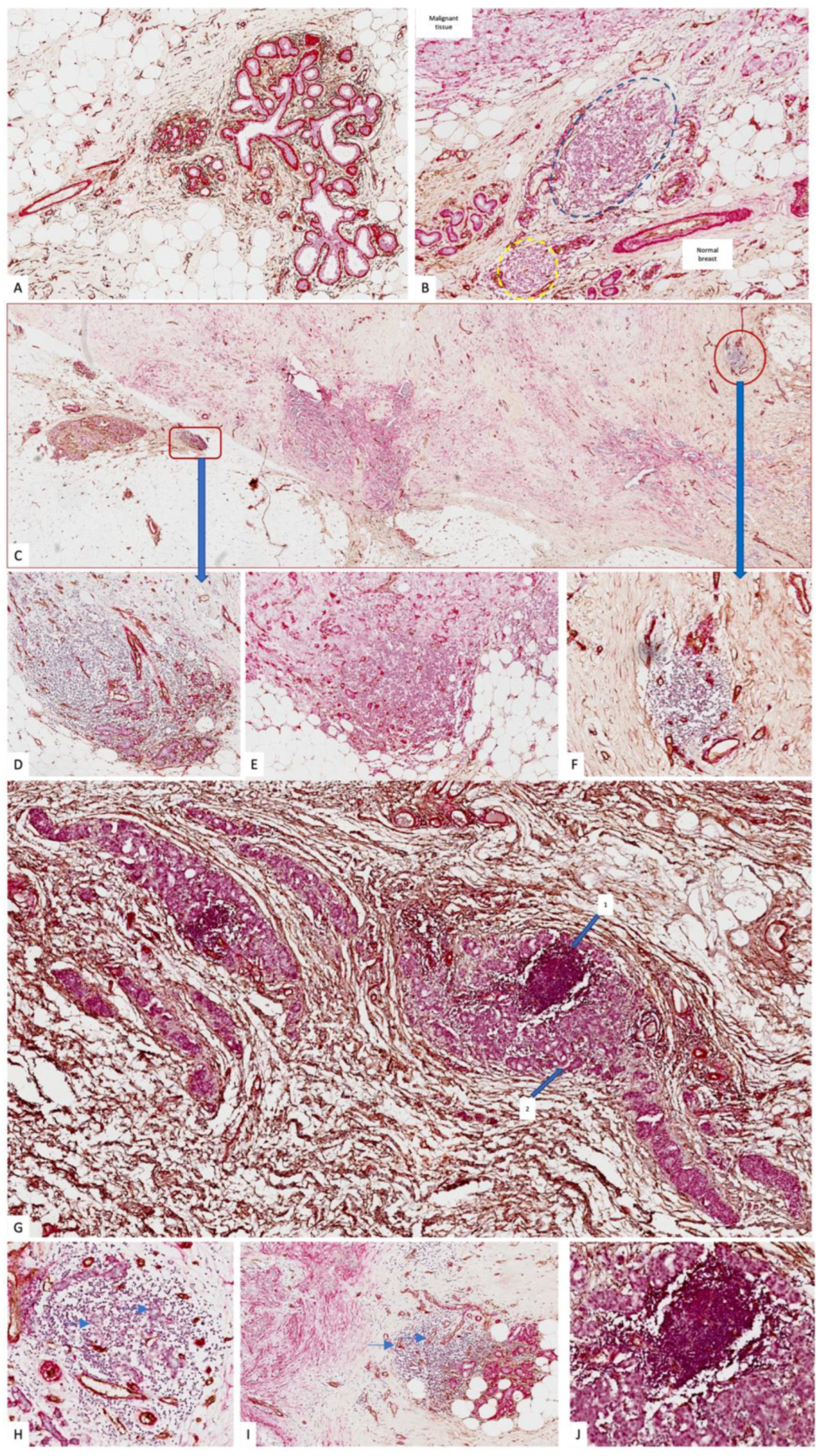
2.4. TLS Assessment and IHC Specimens’ Analysis
2.5. Statistical Analysis, Correlation with Clinical and Therapeutic Data
3. Results
3.1. Histopathology Assessment, BC Cases Molecular Classification, and TLSs
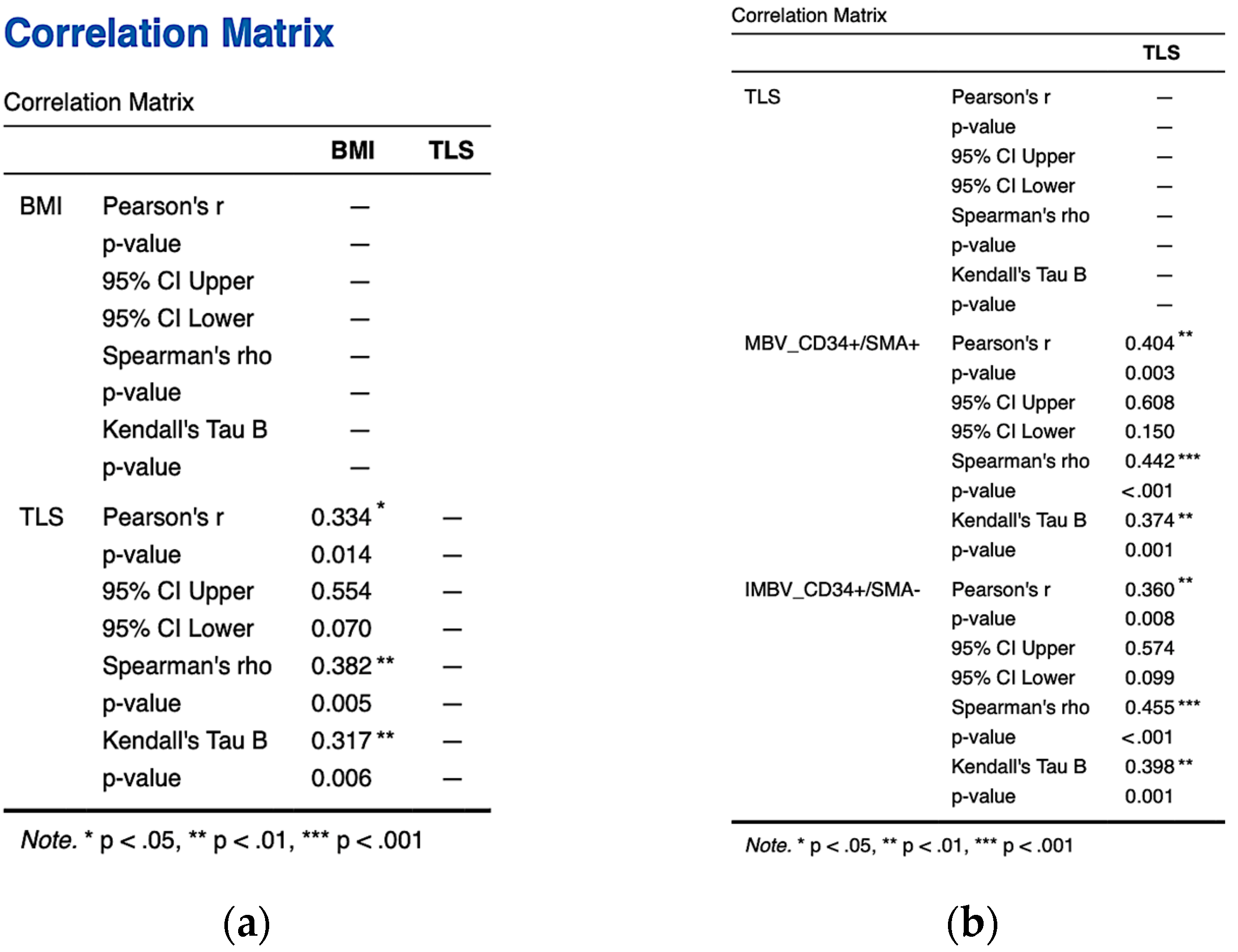
3.2. TLS Classification and Their Interrelation to Tumor Stroma Blood Vessels, Adipose Tissue, and BMI
3.3. TLS, BC Molecular Subtypes, and Stromal Tumor Blood Vessels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Olszewski, W.L. De novo lymph node formation in chronic inflammation of the human leg. Ann. N. Y. Acad. Sci. 2002, 979, 166–177; discussion 188–196. [Google Scholar] [CrossRef]
- Van den Oord, J.J.; De Wolf-Peeters, C.; Desmet, V.J.; Takahashi, K.; Ohtsuki, Y.; Akagi, T. Nodular alteration of the paracortical area. An in situ immunohistochemical analysis of primary, secondary, and tertiary T-nodules. Am. J. Pathol. 1985, 120, 55–66. [Google Scholar] [PubMed]
- Takemura, S.; Klimiuk, P.A.; Braun, A.; Goronzy, J.J.; Weyand, C.M. T cell activation in rheumatoid synovium is B cell dependent. J. Immunol. 2001, 167, 4710–4718. [Google Scholar] [CrossRef] [PubMed]
- Gaide, O.; Martinon, F.; Micheau, O.; Bonnet, D.; Thome, M.; Tschopp, J. Carma1, a CARD-containing binding partner of Bcl10, induces Bcl10 phosphorylation and NF-kappaB activation. FEBS Lett. 2001, 496, 121–127. [Google Scholar] [CrossRef]
- Dieu-Nosjean, M.C.; Antoine, M.; Danel, C.; Heudes, D.; Wislez, M.; Poulot, V.; Rabbe, N.; Laurans, L.; Tartour, E.; de Chaisemartin, L.; et al. Long-term survival for patients with non-small-cell lung cancer with intratumoral lymphoid structures. J. Clin. Oncol. 2008, 26, 4410–4417. [Google Scholar] [CrossRef] [PubMed]
- Coppola, D.; Mulé, J.J. Ectopic lymph nodes within human solid tumors. J. Clin. Oncol. 2008, 26, 4369–4370. [Google Scholar] [CrossRef]
- Aspord, C.; Pedroza-Gonzalez, A.; Gallegos, M.; Tindle, S.; Burton, E.C.; Su, D.; Marches, F.; Banchereau, J.; Palucka, A.K. Breast cancer instructs dendritic cells to prime interleukin 13-secreting CD4+ T cells that facilitate tumor development. J. Exp. Med. 2007, 204, 1037–1047. [Google Scholar] [CrossRef]
- Tseng, W.W.; Malu, S.; Zhang, M.; Chen, J.; Sim, G.C.; Wei, W.; Ingram, D.; Somaiah, N.; Lev, D.C.; Pollock, R.E.; et al. Analysis of the intratumoral adaptive immune response in well differentiated and dedifferentiated retroperitoneal liposarcoma. Sarcoma 2015, 2015, 547460. [Google Scholar] [CrossRef]
- Giraldo, N.A.; Becht, E.; Pagès, F.; Skliris, G.; Verkarre, V.; Vano, Y.; Mejean, A.; Saint-Aubert, N.; Lacroix, L.; Natario, I.; et al. Orchestration and Prognostic Significance of Immune Checkpoints in the Microenvironment of Primary and Metastatic Renal Cell Cancer. Clin. Cancer Res. 2015, 21, 3031–3040. [Google Scholar] [CrossRef]
- Helmink, B.A.; Reddy, S.M.; Gao, J.; Zhang, S.; Basar, R.; Thakur, R.; Yizhak, K.; Sade-Feldman, M.; Blando, J.; Han, G.; et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 2020, 577, 549–555. [Google Scholar] [CrossRef]
- Gu-Trantien, C.; Loi, S.; Garaud, S.; Equeter, C.; Libin, M.; de Wind, A.; Ravoet, M.; Le Buanec, H.; Sibille, C.; Manfouo-Foutsop, G.; et al. CD4+ follicular helper T cell infiltration predicts breast cancer survival. J. Clin. Investig. 2013, 123, 2873–2892. [Google Scholar] [CrossRef]
- Buisseret, L.; Garaud, S.; de Wind, A.; Van den Eynden, G.; Boisson, A.; Solinas, C.; Gu-Trantien, C.; Naveaux, C.; Lodewyckx, J.N.; Duvillier, H.; et al. Tumor-infiltrating lymphocyte composition, organization and PD-1/PD-L1 expression are linked in breast cancer. Oncoimmunology 2016, 6, e1257452. [Google Scholar] [CrossRef] [PubMed]
- Seow, D.Y.B.; Yeong, J.P.S.; Lim, J.X.; Chia, N.; Lim, J.C.T.; Ong, C.C.H.; Tan, P.H.; Iqbal, J. Tertiary lymphoid structures and associated plasma cells play an important role in the biology of triple-negative breast cancers. Breast Cancer Res. Treat. 2020, 180, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Boisson, A.; Noël, G.; Saiselet, M.; Rodrigues-Vitória, J.; Thomas, N.; Fontsa, M.L.; Sofronii, D.; Naveaux, C.; Duvillier, H.; Craciun, L.; et al. Fluorescent Multiplex Immunohistochemistry Coupled with Other State-of-the-Art Techniques to Systematically Characterize the Tumor Immune Microenvironment. Front. Mol. Biosci. 2021, 8, 673042. [Google Scholar] [CrossRef] [PubMed]
- Tzoras, E.; Zerdes, I.; Tsiknakis, N.; Manikis, G.C.; Mezheyeuski, A.; Bergh, J.; Matikas, A.; Foukakis, T. Dissecting Tumor-Immune Microenvironment in Breast Cancer at a Spatial and Multiplex Resolution. Cancers 2022, 14, 1999. [Google Scholar] [CrossRef]
- Mustapha, R.; Ng, K.; Monypenny, J.; Ng, T. Insights Into Unveiling a Potential Role of Tertiary Lymphoid Structures in Metastasis. Front. Mol. Biosci. 2021, 8, 661516. [Google Scholar] [CrossRef]
- Cuypers, A.; Truong, A.K.; Becker, L.M.; Saavedra-García, P.; Carmeliet, P. Tumor vessel co-option: The past & the future. Front. Oncol. 2022, 12, 965277. [Google Scholar] [CrossRef]
- Nagl, L.; Horvath, L.; Pircher, A.; Wolf, D. Tumor Endothelial Cells (TECs) as Potential Immune Directors of the Tumor Microenvironment—New Findings and Future Perspectives. Front. Cell Dev. Biol. 2020, 8, 766. [Google Scholar] [CrossRef]
- Chelvanambi, M.; Fecek, R.J.; Taylor, J.L.; Storkus, W.J. STING agonist-based treatment promotes vascular normalization and tertiary lymphoid structure formation in the therapeutic melanoma microenvironment. J. Immunother. Cancer 2021, 9, e001906. [Google Scholar] [CrossRef]
- Filderman, J.N.; Appleman, M.; Chelvanambi, M.; Taylor, J.L.; Storkus, W.J. STINGing the Tumor Microenvironment to Promote Therapeutic Tertiary Lymphoid Structure Development. Front. Immunol. 2021, 12, 690105. [Google Scholar] [CrossRef]
- He, T.; Hao, Z.; Lin, M.; Xin, Z.; Chen, Y.; Ouyang, W.; Yang, Q.; Chen, X.; Zhou, H.; Zhang, W.; et al. Oncolytic adenovirus promotes vascular normalization and nonclassical tertiary lymphoid structure formation through STING-mediated DC activation. Oncoimmunology 2022, 11, 2093054. [Google Scholar] [CrossRef] [PubMed]
- Kang, W.; Feng, Z.; Luo, J.; He, Z.; Liu, J.; Wu, J.; Rong, P. Tertiary Lymphoid Structures in Cancer: The Double-Edged Sword Role in Antitumor Immunity and Potential Therapeutic Induction Strategies. Front. Immunol. 2021, 12, 689270. [Google Scholar] [CrossRef] [PubMed]
- Ferician, O.; Cimpean, A.M.; Ceausu, A.R.; Dema, A.; Raica, M.; Cumpanas, A. Heterogeneous vascular patterns in renal cell carcinomas. Pol. J. Pathol. 2016, 67, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Cimpean, A.M.; Kovacs, J.; Jung, I. Counting of angiogenesis in colorectal carcinomas using double immunostain. Tumori J. 2012, 98, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, T.N.; Thommen, D.S. Tertiary lymphoid structures in cancer. Science 2022, 375, eabf9419. [Google Scholar] [CrossRef]
- Sautès-Fridman, C.; Petitprez, F.; Calderaro, J.; Fridman, W.H. Tertiary lymphoid structures in the era of cancer immunotherapy. Nat. Rev. Cancer 2019, 19, 307–325. [Google Scholar] [CrossRef]
- Dieudé, M.; Kaci, I.; Hébert, M.J. The Impact of Programmed Cell Death on the Formation of Tertiary Lymphoid Structures. Front. Immunol. 2021, 12, 696311. [Google Scholar] [CrossRef]
- Rous, P.; Kidd, J.G.; Smith, W.E. Experiments on the cause of the rabbit carcinomas derived from virus-induced papillomas. II. Loss by the Vx2 carcinoma of the power to immunize hosts against the papilloma virus. J. Exp. Med. 1952, 96, 159–174. [Google Scholar] [CrossRef]
- Available online: https://pubmed.ncbi.nlm.nih.gov/?term=cancer+immunotherapy&filter=years.2023-2023 (accessed on 1 March 2023).
- Jia, W.; Zhang, T.; Yao, Q.; Li, J.; Nie, Y.; Lei, X.; Mao, Z.; Wang, Y.; Shi, W.; Song, W. Tertiary Lymphatic Structures in Primary Hepatic Carcinoma: Controversy Cannot Overshadow Hope. Front. Immunol. 2022, 13, 870458. [Google Scholar] [CrossRef]
- Fleig, S.; Kapanadze, T.; Bernier-Latmani, J.; Lill, J.K.; Wyss, T.; Gamrekelashvili, J.; Kijas, D.; Liu, B.; Hüsing, A.M.; Bovay, E.; et al. Loss of vascular endothelial notch signaling promotes spontaneous formation of tertiary lymphoid structures. Nat. Commun. 2022, 13, 2022. [Google Scholar] [CrossRef]
- Mueller, C.G.; Nayar, S.; Gardner, D.; Barone, F. Cellular and Vascular Components of Tertiary Lymphoid Structures. Methods Mol. Biol. 2018, 1845, 17–30. [Google Scholar] [CrossRef]
- Sato, Y.; Mii, A.; Hamazaki, Y.; Fujita, H.; Nakata, H.; Masuda, K.; Nishiyama, S.; Shibuya, S.; Haga, H.; Ogawa, O.; et al. Heterogeneous fibroblasts underlie age-dependent tertiary lymphoid tissues in the kidney. JCI Insight 2016, 1, e87680. [Google Scholar] [CrossRef]
- Rodriguez, A.B.; Peske, J.D.; Woods, A.N.; Leick, K.M.; Mauldin, I.S.; Meneveau, M.O.; Young, S.J.; Lindsay, R.S.; Melssen, M.M.; Cyranowski, S.; et al. Immune mechanisms orchestrate tertiary lymphoid structures in tumors via cancer-associated fibroblasts. Cell Rep. 2021, 36, 109422. [Google Scholar] [CrossRef]
- Wu, Y.H.; Wu, F.; Yan, G.R.; Zeng, Q.Y.; Jia, N.; Zheng, Z.; Fang, S.; Liu, Y.Q.; Zhang, G.L.; Wang, X.L. Features and clinical significance of tertiary lymphoid structure in cutaneous squamous cell carcinoma. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 2043–2050. [Google Scholar] [CrossRef]
- Lee, H.J.; Park, I.A.; Song, I.H.; Shin, S.J.; Kim, J.Y.; Yu, J.H.; Gong, G. Tertiary lymphoid structures: Prognostic significance and relationship with tumour-infiltrating lymphocytes in triple-negative breast cancer. J. Clin. Pathol. 2016, 69, 422–430. [Google Scholar] [CrossRef]
- López, C.; Bosch-Príncep, R.; Orero, G.; Balagueró, L.F.; Korzynska, A.; García-Rojo, M.; Bueno, G.; Fernández-Carrobles, M.D.M.; Roszkowiak, L.; Casanova, C.C.; et al. Peritumoral immune infiltrates in primary tumours are not associated with the presence of axillary lymph node metastasis in breast cancer: A retrospective cohort study. PeerJ 2020, 8, e9779. [Google Scholar] [CrossRef]
- Posch, F.; Silina, K.; Leibl, S.; Mündlein, A.; Moch, H.; Siebenhüner, A.; Samaras, P.; Riedl, J.; Stotz, M.; Szkandera, J.; et al. Maturation of tertiary lymphoid structures and recurrence of stage II and III colorectal cancer. Oncoimmunology 2017, 7, e1378844. [Google Scholar] [CrossRef]
- Zeng, L.; Koh, V.C.Y.; Chen, X.Y.; Tan, P.H. Tertiary lymphoid structures in breast ductal carcinoma in situ correlate with adverse pathological parameters. Histopathology 2023, 82, 779–788. [Google Scholar] [CrossRef]
- Wang, B.; Liu, J.; Han, Y.; Deng, Y.; Li, J.; Jiang, Y. The Presence of Tertiary Lymphoid Structures Provides New Insight Into the Clinicopathological Features and Prognosis of Patients With Breast Cancer. Front. Immunol. 2022, 13, 868155. [Google Scholar] [CrossRef]
- Ribeiro, R.; Carvalho, M.J.; Goncalves, J.; Moreira, J.N. Immunotherapy in triple-negative breast cancer: Insights into tumor immune landscape and therapeutic opportunities. Front. Mol. Biosci. 2022, 9, 903065. [Google Scholar] [CrossRef]
- Agostinetto, E.; Losurdo, A.; Nader-Marta, G.; Santoro, A.; Punie, K.; Barroso, R.; Popovic, L.; Solinas, C.; Kok, M.; de Azambuja, E.; et al. Progress and pitfalls in the use of immunotherapy for patients with triple negative breast cancer. Expert Opin. Investig. Drugs 2022, 31, 567–591. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Wang, P.; He, S.; Zhu, J.; Shi, Y.; Wang, J. Progress and Prospect of Immunotherapy for Triple-Negative Breast Cancer. Front. Oncol. 2022, 12, 919072. [Google Scholar] [CrossRef] [PubMed]
- Na, H.; Song, Y.; Lee, H.W. Emphasis on Adipocyte Transformation: Anti-Inflammatory Agents to Prevent the Development of Cancer-Associated Adipocytes. Cancers 2023, 15, 502. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; He, S. Multi-faceted role of cancer associated adipocytes in the tumor microenvironment (Review). Mol. Med. Rep. 2021, 24, 866. [Google Scholar] [CrossRef]
- Sanchez, A.; Furberg, H.; Kuo, F.; Vuong, L.; Ged, Y.; Patil, S.; Ostrovnaya, I.; Petruzella, S.; Reising, A.; Patel, P.; et al. Transcriptomic signatures related to the obesity paradox in patients with clear cell renal cell carcinoma: A cohort study. Lancet Oncol. 2020, 21, 283–293. [Google Scholar] [CrossRef]
- Guedj, K.; Abitbol, Y.; Cazals-Hatem, D.; Morvan, M.; Maggiori, L.; Panis, Y.; Bouhnik, Y.; Caligiuri, G.; Corcos, O.; Nicoletti, A. Adipocytes orchestrate the formation of tertiary lymphoid organs in the creeping fat of Crohn’s disease affected mesentery. J. Autoimmun. 2019, 103, 102281. [Google Scholar] [CrossRef]
- Gkegka, A.G.; Koukourakis, M.I.; Katotomichelakis, M.; Giatromanolaki, A. Cancer Microenvironment Defines Tumor-Infiltrating Lymphocyte Density and Tertiary Lymphoid Structure Formation in Laryngeal Cancer. Head Neck Pathol. 2022; Epub ahead of print. [Google Scholar] [CrossRef]
- Blanchard, L.; Girard, J.P. High endothelial venules (HEVs) in immunity, inflammation and cancer. Angiogenesis 2021, 24, 719–753. [Google Scholar] [CrossRef]
- Vella, G.; Guelfi, S.; Bergers, G. High Endothelial Venules: A Vascular Perspective on Tertiary Lymphoid Structures in Cancer. Front. Immunol. 2021, 12, 736670. [Google Scholar] [CrossRef]
- Sawada, J.; Hiraoka, N.; Qi, R.; Jiang, L.; Fournier-Goss, A.E.; Yoshida, M.; Kawashima, H.; Komatsu, M. Molecular Signature of Tumor-Associated High Endothelial Venules That Can Predict Breast Cancer Survival. Cancer Immunol. Res. 2022, 10, 468–481. [Google Scholar] [CrossRef]
- Liu, X.; Tsang, J.Y.S.; Hlaing, T.; Hu, J.; Ni, Y.B.; Chan, S.K.; Cheung, S.Y.; Tse, G.M. Distinct Tertiary Lymphoid Structure Associations and Their Prognostic Relevance in HER2 Positive and Negative Breast Cancers. Oncologist 2017, 22, 1316–1324. [Google Scholar] [CrossRef]
- Available online: https://pubmed.ncbi.nlm.nih.gov/?term=tertiary%20lymphoid%20structure%20HER2%20breast%20cancer&page=2 (accessed on 1 March 2023).
- Jézéquel, P.; Kerdraon, O.; Hondermarck, H.; Guérin-Charbonnel, C.; Lasla, H.; Gouraud, W.; Canon, J.L.; Gombos, A.; Dalenc, F.; Delaloge, S.; et al. Identification of three subtypes of triple-negative breast cancer with potential therapeutic implications. Breast Cancer Res. BCR 2019, 21, 65. [Google Scholar] [CrossRef]
- Kim, A.; Heo, S.H.; Kim, Y.A.; Gong, G.; Lee, H.J. An Examination of the Local Cellular Immune Response to Examples of Both Ductal Carcinoma In Situ (DCIS) of the Breast and DCIS With Microinvasion, With Emphasis on Tertiary Lymphoid Structures and Tumor Infiltrating Lymphoctytes. Am. J. Clin. Pathol. 2016, 146, 137–144. [Google Scholar] [CrossRef]
- Akhouayri, L.; Ostano, P.; Mello-Grand, M.; Gregnanin, I.; Crivelli, F.; Laurora, S.; Liscia, D.; Leone, F.; Santoro, A.; Mulè, A.; et al. Identification of a minimum number of genes to predict triple-negative breast cancer subgroups from gene expression profiles. Hum. Genom. 2022, 16, 70. [Google Scholar] [CrossRef]
- Hachim, M.Y.; Hachim, I.Y.; Talaat, I.M.; Yakout, N.M.; Hamoudi, R. M1 Polarization Markers Are Upregulated in Basal-Like Breast Cancer Molecular Subtype and Associated With Favorable Patient Outcome. Front. Immunol. 2020, 11, 560074. [Google Scholar] [CrossRef]
- Amer, H.T.; Stein, U.; El Tayebi, H.M. The Monocyte, a Maestro in the Tumor Microenvironment (TME) of Breast Cancer. Cancers 2022, 14, 5460. [Google Scholar] [CrossRef]
- Da Graça, C.G.; van Baarsen, L.G.M.; Mebius, R.E. Tertiary Lymphoid Structures: Diversity in Their Development, Composition, and Role. J. Immunol. 2021, 206, 273–281. [Google Scholar] [CrossRef]
- Fridman, W.H.; Remark, R.; Goc, J.; Giraldo, N.A.; Becht, E.; Hammond, S.A.; Damotte, D.; Dieu-Nosjean, M.C.; Sautès-Fridman, C. The immune microenvironment: A major player in human cancers. Int. Arch. Allergy Immunol. 2014, 164, 13–26. [Google Scholar] [CrossRef]
- Li, B. Why do tumor-infiltrating lymphocytes have variable efficacy in the treatment of solid tumors? Front. Immunol. 2022, 13, 973881. [Google Scholar] [CrossRef]
- Liu, J.; Wang, Y.; Tian, Z.; Lin, Y.; Li, H.; Zhu, Z.; Liu, Q.; Su, S.; Zeng, Y.; Jia, W.; et al. Multicenter phase II trial of Camrelizumab combined with Apatinib and Eribulin in heavily pretreated patients with advanced triple-negative breast cancer. Nat. Commun. 2022, 13, 3011. [Google Scholar] [CrossRef]
- Zhan, Z.; Shi-Jin, L.; Yi-Ran, Z.; Zhi-Long, L.; Xiao-Xu, Z.; Hui, D.; Pan, Y.L.; Pan, J.H. High endothelial venules proportion in tertiary lymphoid structure is a prognostic marker and correlated with anti-tumor immune microenvironment in colorectal cancer. Ann. Med. 2023, 55, 114–126. [Google Scholar] [CrossRef]
- Johansson-Percival, A.; Ganss, R. Therapeutic Induction of Tertiary Lymphoid Structures in Cancer Through Stromal Remodeling. Front. Immunol. 2021, 12, 674375. [Google Scholar] [CrossRef] [PubMed]
| BC Molecular Subtype | Parameters | G | NPI | Recurrence | LVI | PnI |
|---|---|---|---|---|---|---|
| TLS+_LUMINAL A | G | - | p = 0.004 | NS | NS | NS |
| NPI | p = 0.004 | - | NS | NS | NS | |
| RECURRENCE | NS | NS | - | NS | NS | |
| LVI | NS | NS | NS | - | p < 0.001 | |
| PnI | NS | NS | NS | p < 0.001 | - | |
| TLS−_LUMINAL A | G | - | NS | NS | NS | NS |
| NPI | NS | - | NS | NS | NS | |
| RECURRENCE | NS | NS | - | NS | NS | |
| LVI | NS | NS | NS | - | NS | |
| PnI | NS | NS | NS | NS | - | |
| TLS+_LUMINAL B | G | - | p = 0.024 | NS | NS | NS |
| NPI | p = 0.024 | - | NS | NS | NS | |
| RECURRENCE | NS | NS | - | NS | NS | |
| LVI | NS | NS | NS | - | NS | |
| PnI | NS | NS | NS | NS | - | |
| TLS−_LUMINAL B | G | - | p = 0.008 | p = 0.024 | NS | NS |
| NPI | p = 0.008 | - | p = 0.008 | NS | NS | |
| RECURRENCE | p = 0.024 | p = 0.008 | - | NS | NS | |
| LVI | NS | NS | NS | - | p = 0.019 | |
| PnI | NS | NS | NS | p = 0.019 | - | |
| TLS+_LUMINAL B-HER2 | G | - | NS | NS | NS | NS |
| NPI | NS | - | NS | NS | NS | |
| RECURRENCE | NS | NS | - | NS | NS | |
| LVI | NS | NS | NS | - | ||
| PnI | NS | NS | NS | NS | - | |
| TLS−_LUMINAL B-HER2 | G | - | NS | NS | NS | NS |
| NPI | NS | - | NS | NS | NS | |
| RECURRENCE | NS | NS | - | p < 0.001 | p < 0.001 | |
| LVI | NS | NS | p < 0.001 | - | p < 0.001 | |
| PnI | NS | NS | p < 0.001 | p < 0.001 | - | |
| TLS+_HER2 | G | - | - | - | - | - |
| NPI | - | - | - | - | - | |
| RECURRENCE | - | - | - | - | - | |
| LVI | - | - | - | - | - | |
| PnI | - | - | - | - | - | |
| TLS−_HER2 | G | - | NS | NS | NS | NS |
| NPI | NS | - | NS | NS | NS | |
| RECURRENCE | NS | NS | - | p < 0.001 | p < 0.001 | |
| LVI | NS | NS | p < 0.001 | - | p < 0.001 | |
| PnI | NS | NS | p < 0.001 | p < 0.001 | - | |
| TLS+_TNBC | G | - | p = 0.042 | NS | NS | NS |
| NPI | p = 0.042 | - | NS | NS | NS | |
| RECURRENCE | NS | NS | - | NS | p < 0.001 | |
| LVI | NS | NS | NS | - | NS | |
| PnI | NS | NS | p < 0.001 | NS | - | |
| TLS−_TNBC | G | - | NS | p < 0.001 | p < 0.001 | p < 0.001 |
| NPI | NS | - | NS | NS | NS | |
| RECURRENCE | p < 0.001 | NS | - | p < 0.001 | p < 0.001 | |
| LVI | p < 0.001 | NS | p < 0.001 | - | p < 0.001 | |
| PnI | p < 0.001 | NS | p < 0.001 | p < 0.001 | - |
| Study Title and Publication Year | Main Findings | Present Study Related Findings | Critical Discussions | Ref. |
|---|---|---|---|---|
| Tertiary lymphoid structures in breast ductal carcinoma in situ correlate with adverse pathological parameters. Zeng et al., 2023 | TLSs in DCIS were associated with unfavorable prognostic features. No significant associations between TLSs and recurrence. | TLSs were assessed in invasive ductal carcinomas classified according to molecular profile. TLSs were significantly correlated with recurrences depending on BC molecular subtypes. | Recurrence rate increased with BC progression from an in situ to invasive state highly dependent on molecular subtypes. | [39] |
| The Presence of Tertiary Lymphoid Structures Provides New Insight Into the Clinicopathological Features and Prognosis of Patients With Breast Cancer. Wang et al., 2022 | A review based on 15 papers from the literature. HER2 high expression was associated with high TLS presence. | All HER2 positive cases did not present TLSs and had significant correlation of recurrence with LVI, PnI, and young age but also with immature stromal blood vessels. HER2 positivity association to Luminal B (LB-HER2 subtype) showed similar findings with HER2 subtype. | Contradictory findings between these two studies support further research development to elucidate HER2 positivity impact on TLSs dynamic in BC. TLSs assessment on LB-HER2 subtype may be considered a novelty of the present study together with associated stromal blood vessels assessment. | [40] |
| Multicenter phase II trial of Camrelizumab combined with Apatinib and Eribulin in heavily pretreated patients with advanced triple-negative breast cancer. Liu et al., 2022 | Camrelizumab plus apatinib and eribulin induced a better objective response rate and a higher progression free survival for TLS positive TNBC patients. | Lack of TLSs in TNBC was significantly correlated with lymphovascular and perineural invasion, and recurrence. TLS positive TNBC has mature blood vessels which induce a low perineural invasion | High rate of lymphovascular/perineural invasion and high recurrence related to TLSs may select TNBC patients who may have a low objective rate response to therapy and a lower progression free survival. Mature blood vessels are the proper route for drug delivery, and thus, their presence may be evaluated before therapy. TLS_stromal blood vessels type has not been previously studied. | [62] |
| Therapeutic Induction of Tertiary Lymphoid Structures in Cancer Through Stromal Remodeling. Johansson & Ganss, 2021 | Insights into TLS development in normal and malignant conditions. TLSs in pancreatic cancer is associated with a more mature vascular network suggesting a possible link between TLS formation and stabilized tumor vessels. | TLS presence was significantly correlated with mature blood vessels surrounded by perivascular SMA positive cells which lack correlation with lymphovascular invasion. | Present study results related to TLSs and blood vessel maturation proved interplay between TLSs and the BC stromal vascular network in breast malignant tissue not found in other BC studies. Our findings are preliminary and supported by similar findings from other cancer types such as pancreatic cancer. Further studies are needed for validating these preliminary data. | [64] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barb, A.C.; Pasca Fenesan, M.; Pirtea, M.; Margan, M.M.; Tomescu, L.; Melnic, E.; Cimpean, A.M. Tertiary Lymphoid Structures (TLSs) and Stromal Blood Vessels Have Significant and Heterogeneous Impact on Recurrence, Lymphovascular and Perineural Invasion amongst Breast Cancer Molecular Subtypes. Cells 2023, 12, 1176. https://doi.org/10.3390/cells12081176
Barb AC, Pasca Fenesan M, Pirtea M, Margan MM, Tomescu L, Melnic E, Cimpean AM. Tertiary Lymphoid Structures (TLSs) and Stromal Blood Vessels Have Significant and Heterogeneous Impact on Recurrence, Lymphovascular and Perineural Invasion amongst Breast Cancer Molecular Subtypes. Cells. 2023; 12(8):1176. https://doi.org/10.3390/cells12081176
Chicago/Turabian StyleBarb, Alina Cristina, Mihaela Pasca Fenesan, Marilena Pirtea, Madalin Marius Margan, Larisa Tomescu, Eugen Melnic, and Anca Maria Cimpean. 2023. "Tertiary Lymphoid Structures (TLSs) and Stromal Blood Vessels Have Significant and Heterogeneous Impact on Recurrence, Lymphovascular and Perineural Invasion amongst Breast Cancer Molecular Subtypes" Cells 12, no. 8: 1176. https://doi.org/10.3390/cells12081176
APA StyleBarb, A. C., Pasca Fenesan, M., Pirtea, M., Margan, M. M., Tomescu, L., Melnic, E., & Cimpean, A. M. (2023). Tertiary Lymphoid Structures (TLSs) and Stromal Blood Vessels Have Significant and Heterogeneous Impact on Recurrence, Lymphovascular and Perineural Invasion amongst Breast Cancer Molecular Subtypes. Cells, 12(8), 1176. https://doi.org/10.3390/cells12081176









