James German and the Quest to Understand Human RECQ Helicase Deficiencies
Abstract
:1. Introduction
2. Getting Started Thinking about Human Disease
3. Werner Syndrome—First Steps, and a Disease Gene Cloning ‘Prequel’
4. 1996—The Werner Syndrome Positional Cloning ‘Annus Mirabilis’
5. WRN and Other RECQ Macromolecular Machines
6. Broader Roles for WRN in Sporadic Cancer
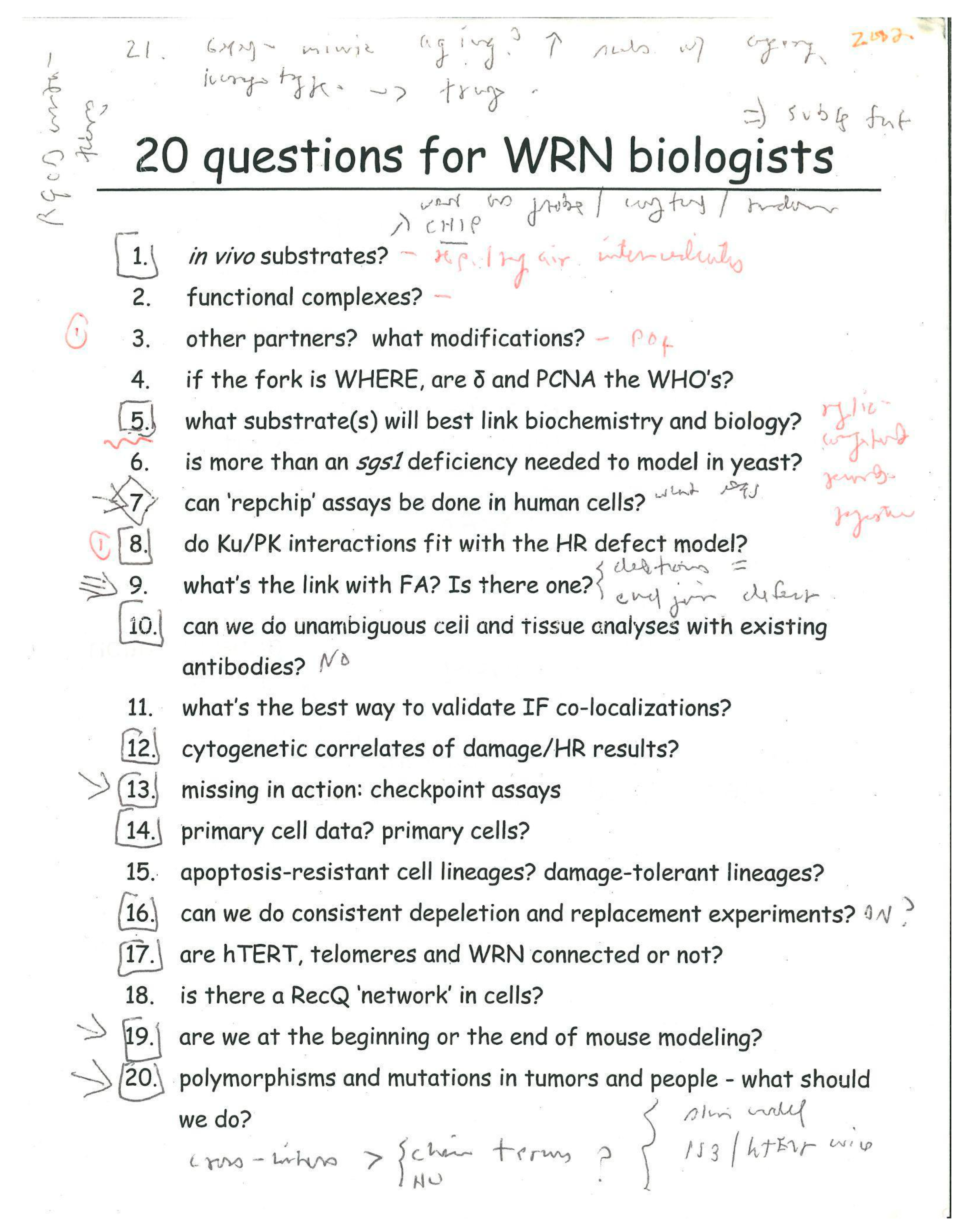
7. New Conceptual and Experimental Growing Points
8. Are Werner and Bloom Syndromes ‘Treatable’ Disease States?
9. The Essential Role of Rare Disease Communities in Advancing Knowledge
10. Coda
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- German, J. Why the Lupus Problem Remains Unsolved and I Am a Human Geneticist. Lupus 2003, 12, 181–189. [Google Scholar] [CrossRef] [PubMed]
- German, J. (Ed.) Chromosome Mutation and Neoplasia; A Volume in the ‘Chromosomes’ Monograph Series; Alan R. Liss: New York, NY, USA, 1983; 451p. [Google Scholar]
- Bloom, D. Congenital Telangiectatic Erythema Resembling Lupus Erythematosus in Dwarfs; Probably a Syndrome Entity. AMA Am. J. Dis. Child. 1954, 88, 754–758. [Google Scholar] [CrossRef] [PubMed]
- Oshima, J.; Martin, G.M.; Hisama, F.M. Werner Syndrome. In GeneReviews® [Internet]; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; 2 December 2002 [Updated 13 May 2021]; University of Washington: Seattle, WA, USA, 2002; Bookshelf ID: NBK1514. [Google Scholar] [PubMed]
- Wang, L.L.; Plon, S.E. Rothmund-Thomson Syndrome. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1999; Bookshelf ID: NBK1237. [Google Scholar] [PubMed]
- Abu-Libdeh, B.; Jhujh, S.S.; Dhar, S.; Sommers, J.A.; Datta, A.; Longo, G.M.; Grange, L.J.; Reynolds, J.J.; Cooke, S.L.; McNee, G.S.; et al. RECON Syndrome Is a Genome Instability Disorder Caused by Mutations in the DNA Helicase RECQL1. J. Clin. Investig. 2022, 132, e147301. [Google Scholar] [CrossRef] [PubMed]
- Langer, K.; Cunniff, C.M.; Kucine, N. Bloom Syndrome. In GeneReviews® [Internet]; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; 22 March 2006 [updated 12 October 2023]; University of Washington: Seattle, WA, USA, 2006; Bookshelf ID: NBK1398. [Google Scholar] [PubMed]
- Epstein, C.J.; Martin, G.M.; Schultz, A.L.; Motulsky, A.G. Werner’s Syndrome: A Review of Its Symptomatology, Natural History, Pathologic Features, Genetics and relationship to the natural aging process. Medicine 1966, 45, 177–221. [Google Scholar] [CrossRef] [PubMed]
- Miller, J. Amelia Louise Susman Schultz (1915–2021). Am. Anthropol. 2022, 124, 241–244. [Google Scholar] [CrossRef]
- German, J. Bloom Syndrome: A Mendelian Prototype of Somatic Mutational Disease. Medicine 1993, 72, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Martin, G.M.; Sprague, C.A.; Epstein, C.J. Replicative Life-Span of Cultivated Human Cells. Effects of Donor’s Age, Tissue, and Genotype. Lab. Investig. 1970, 23, 86–92. [Google Scholar] [PubMed]
- Salk, D.; Au, K.; Hoehn, H.; Martin, G.M. Cytogenetics of Werner’s Syndrome Cultured Skin Fibroblasts: Variegated Translocation Mosaicism. Cytogenet. Cell Genet. 1981, 30, 92–107. [Google Scholar] [CrossRef] [PubMed]
- Salk, D.; Fujiwara, Y.; Martin, G.M. (Eds.) Werner’s Syndrome and Human Aging; United States-Japan Cooperative Seminar on Werner’s Syndrome and Human Aging; Advances in Experimental Medicine and Biology; Plenum Press: New York, NY, USA, 1985; Volume 190. [Google Scholar]
- Ellis, N.A.; Groden, J.; Ye, T.Z.; Straughen, J.; Lennon, D.J.; Ciocci, S.; Proytcheva, M.; German, J. The Bloom’s Syndrome Gene Product Is Homologous to RecQ Helicases. Cell 1995, 83, 655–666. [Google Scholar] [CrossRef]
- Schellenberg, G.D.; Martin, G.M.; Wijsman, E.M.; Nakura, J.; Miki, T.; Ogihara, T. Homozygosity Mapping and Werner’s Syndrome. Lancet 1992, 339, 1002. [Google Scholar] [CrossRef]
- Goto, M.; Rubenstein, M.; Weber, J.; Woods, K.; Drayna, D. Genetic Linkage of Werner’s Syndrome to Five Markers on Chromosome 8. Nature 1992, 355, 735–738. [Google Scholar] [CrossRef]
- Nakura, J.; Wijsman, E.M.; Miki, T.; Kamino, K.; Yu, C.E.; Oshima, J.; Fukuchi, K.; Weber, J.L.; Piussan, C.; Melaragno, M.I. Homozygosity Mapping of the Werner Syndrome Locus (WRN). Genomics 1994, 23, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Martin, G.M. A brief history of research on the Werner syndrome. In From Premature Gray Hair to Helicase—Werner Syndrome: Implications for Aging and Cancer; Goto, M., Miller, R.W., Eds.; Gann Monograph on Cancer Research; Springer: Berlin/Heidelberg, Germany, 2001; Volume 49, pp. 1–10. [Google Scholar]
- Miller, R.W. The U.S.-Japan Cooperative Cancer Research Program: Some Highlights of Seminars, Interdisciplinary Program Area, 1981–1996. Jpn. J. Cancer Res. 1996, 87, 221–226. [Google Scholar] [CrossRef]
- Goto, M.; Miller, R.W.; Ishikawa, Y.; Sugano, H. Excess of Rare Cancers in Werner Syndrome (adult Progeria). Cancer Epidemiol. Biomarkers Prev. 1996, 5, 239–246. [Google Scholar]
- Ishikawa, Y.; Miller, R.W.; Machinami, R.; Sugano, H.; Goto, M. Atypical Osteosarcomas in Werner Syndrome (adult Progeria). Jpn. J. Cancer Res. 2000, 91, 1345–1349. [Google Scholar] [CrossRef]
- Lauper, J.M.; Krause, A.; Vaughan, T.L.; Monnat, R.J., Jr. Spectrum and Risk of Neoplasia in Werner Syndrome: A Systematic Review. PLoS ONE 2013, 8, e59709. [Google Scholar] [CrossRef] [PubMed]
- Gray, M.D.; Shen, J.C.; Kamath-Loeb, A.S.; Blank, A.; Sopher, B.L.; Martin, G.M.; Oshima, J.; Loeb, L.A. The Werner Syndrome Protein Is a DNA Helicase. Nat. Genet. 1997, 17, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.C.; Gray, M.D.; Oshima, J.; Kamath-Loeb, A.S.; Fry, M.; Loeb, L.A. Werner Syndrome Protein. I. DNA Helicase and Dna Exonuclease Reside on the Same Polypeptide. J. Biol. Chem. 1998, 273, 34139–34144. [Google Scholar] [CrossRef] [PubMed]
- Kamath-Loeb, A.S.; Shen, J.C.; Loeb, L.A.; Fry, M. Werner Syndrome Protein. II. Characterization of the Integral 3′→ 5′ DNA Exonuclease. J. Biol. Chem. 1998, 273, 34145–34150. [Google Scholar] [CrossRef]
- Moser, M.J.; Kamath-Loeb, A.S.; Jacob, J.E.; Bennett, S.E.; Oshima, J.; Monnat, R.J., Jr. WRN Helicase Expression in Werner Syndrome Cell Lines. Nucleic Acids Res. 2000, 28, 648–654. [Google Scholar] [CrossRef]
- Moser, M.J.; Bigbee, W.L.; Grant, S.G.; Emond, M.J.; Langlois, R.G.; Jensen, R.H.; Oshima, J.; Monnat, R.J., Jr. Genetic Instability and Hematologic Disease Risk in Werner Syndrome Patients and Heterozygotes. Cancer Res. 2000, 60, 2492–2496. [Google Scholar] [PubMed]
- Grandori, C.; Wu, K.-J.; Fernandez, P.; Ngouenet, C.; Grim, J.; Clurman, B.E.; Moser, M.J.; Oshima, J.; Russell, D.W.; Swisshelm, K.; et al. Werner Syndrome Protein Limits MYC-Induced Cellular Senescence. Genes Dev. 2003, 17, 1569–1574. [Google Scholar] [CrossRef] [PubMed]
- Prince, P.R.; Emond, M.J.; Monnat, R.J., Jr. Loss of Werner Syndrome Protein Function Promotes Aberrant Mitotic Recombination. Genes Dev. 2001, 15, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Saintigny, Y.; Makienko, K.; Swanson, C.; Emond, M.J.; Monnat, R.J., Jr. Homologous Recombination Resolution Defect in Werner Syndrome. Mol. Cell. Biol. 2002, 22, 6971–6978. [Google Scholar] [CrossRef] [PubMed]
- Swanson, C.; Saintigny, Y.; Emond, M.J.; Monnat, R.J., Jr. The Werner Syndrome Protein Has Separable Recombination and Survival Functions. DNA Repair 2004, 3, 475–482. [Google Scholar] [CrossRef]
- Wu, L.; Hickson, I.D. The Bloom’s Syndrome Helicase Suppresses Crossing over during Homologous Recombination. Nature 2003, 426, 870–874. [Google Scholar] [CrossRef]
- West, S.C.; Blanco, M.G.; Chan, Y.W.; Matos, J.; Sarbajna, S.; Wyatt, H.D.M. Resolution of Recombination Intermediates: Mechanisms and Regulation. Cold Spring Harb. Symp. Quant. Biol. 2015, 80, 103–109. [Google Scholar] [CrossRef]
- West, S.C.; Chan, Y.W. Genome Instability as a Consequence of Defects in the Resolution of Recombination Intermediates. Cold Spring Harb. Symp. Quant. Biol. 2017, 82, 207–212. [Google Scholar] [CrossRef]
- Hanaoka, F.; Yamada, M.; Takeuchi, F.; Goto, M.; Miyamoto, T.; Hori, T. Autoradiographic Studies of DNA Replication in Werner’s Syndrome Cells. Adv. Exp. Med. Biol. 1985, 190, 439–457. [Google Scholar]
- Takeuchi, F.; Hanaoka, F.; Goto, M.; Akaoka, I.; Hori, T.; Yamada, M.; Miyamoto, T. Altered Frequency of Initiation Sites of DNA Replication in Werner’s Syndrome Cells. Hum. Genet. 1982, 60, 365–368. [Google Scholar] [CrossRef]
- Hand, R.; German, J. A Retarded Rate of DNA Chain Growth in Bloom’s Syndrome. Proc. Natl. Acad. Sci. USA 1975, 72, 758–762. [Google Scholar] [CrossRef]
- Lönn, U.; Lönn, S.; Nylen, U.; Winblad, G.; German, J. An Abnormal Profile of DNA Replication Intermediates in Bloom’s Syndrome. Cancer Res. 1990, 50, 3141–3145. [Google Scholar]
- Monnat, R.J., Jr. Human RECQ Helicases: Roles in DNA Metabolism, Mutagenesis and Cancer Biology. Semin. Cancer Biol. 2010, 20, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Sidorova, J.M.; Li, N.; Schwartz, D.C.; Folch, A.; Monnat, R.J., Jr. Microfluidic-Assisted Analysis of Replicating DNA Molecules. Nat. Protoc. 2009, 4, 849–861. [Google Scholar] [CrossRef] [PubMed]
- Sidorova, J.M.; Li, N.; Folch, A.; Monnat, R.J., Jr. The RecQ Helicase WRN Is Required for Normal Replication Fork Progression after DNA Damage or Replication Fork Arrest. Cell Cycle 2008, 7, 796–807. [Google Scholar] [CrossRef]
- Sidorova, J.M.; Kehrli, K.; Mao, F.; Monnat, R., Jr. Distinct Functions of Human RECQ Helicases WRN and BLM in Replication Fork Recovery and Progression after Hydroxyurea-Induced Stalling. DNA Repair 2013, 12, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Lazarchuk, P.; Nguyen, V.N.; Brunon, S.; Pavlova, M.N.; Sidorova, J.M. Innate Immunity Mediator STING Modulates Nascent DNA Metabolism at Stalled Forks in Human Cells. Front. Mol. Biosci. 2022, 9, 1048726. [Google Scholar] [CrossRef] [PubMed]
- Spillare, E.A.; Robles, A.I.; Wang, X.W.; Shen, J.C.; Yu, C.E.; Schellenberg, G.D.; Harris, C.C. p53-Mediated Apoptosis Is Attenuated in Werner Syndrome Cells. Genes Dev. 1999, 13, 1355–1360. [Google Scholar] [CrossRef]
- Yang, Q.; Zhang, R.; Wang, X.W.; Spillare, E.A.; Linke, S.P.; Subramanian, D.; Griffith, J.D.; Li, J.L.; Hickson, I.D.; Shen, J.C.; et al. The Processing of Holliday Junctions by BLM and WRN Helicases Is Regulated by p53* 210. J. Biol. Chem. 2002, 277, 31980–31987. [Google Scholar] [CrossRef]
- Spillare, E.A.; Wang, X.W.; von Kobbe, C.; Bohr, V.A.; Hickson, I.D.; Harris, C.C. Redundancy of DNA Helicases in p53-Mediated Apoptosis. Oncogene 2006, 25, 2119–2123. [Google Scholar] [CrossRef]
- Nguyen, G.H.; Tang, W.; Robles, A.I.; Beyer, R.P.; Gray, L.T.; Welsh, J.A.; Schetter, A.J.; Kumamoto, K.; Wang, X.W.; Hickson, I.D.; et al. Regulation of Gene Expression by the BLM Helicase Correlates with the Presence of G-Quadruplex DNA Motifs. Proc. Natl. Acad. Sci. USA 2014, 111, 9905–9910. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Robles, A.I.; Beyer, R.P.; Gray, L.T.; Nguyen, G.H.; Oshima, J.; Maizels, N.; Harris, C.C.; Monnat, R.J., Jr. The Werner Syndrome RECQ Helicase Targets G4 DNA in Human Cells to Modulate Transcription. Hum. Mol. Genet. 2016, 25, 2060–2069. [Google Scholar] [CrossRef] [PubMed]
- Haber, J.E. A Life Investigating Pathways That Repair Broken Chromosomes. Annu. Rev. Genet. 2016, 50, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Tokita, M.; Kennedy, S.R.; Risques, R.A.; Chun, S.G.; Pritchard, C.; Oshima, J.; Liu, Y.; Bryant-Greenwood, P.K.; Welcsh, P.; Monnat, R.J. Werner Syndrome through the Lens of Tissue and Tumour Genomics. Sci. Rep. 2016, 6, 32038. [Google Scholar] [CrossRef] [PubMed]
- Agrelo, R.; Cheng, W.-H.; Setien, F.; Ropero, S.; Espada, J.; Fraga, M.F.; Herranz, M.; Paz, M.F.; Sanchez-Cespedes, M.; Artiga, M.J.; et al. Epigenetic Inactivation of the Premature Aging Werner Syndrome Gene in Human Cancer. Proc. Natl. Acad. Sci. USA 2006, 103, 8822–8827. [Google Scholar] [CrossRef] [PubMed]
- Bosch, L.J.W.; Luo, Y.; Lao, V.V.; Snaebjornsson, P.; Trooskens, G.; Vlassenbroeck, I.; Mongera, S.; Tang, W.; Welcsh, P.; Herman, J.G.; et al. WRN Promoter CpG Island Hypermethylation Does Not Predict More Favorable Outcomes for Patients with Metastatic Colorectal Cancer Treated with Irinotecan-Based Therapy. Clin. Cancer Res. 2016, 22, 4612–4622. [Google Scholar] [CrossRef] [PubMed]
- Pavelitz, T.; Renfro, L.; Foster, N.R.; Caracol, A.; Welsch, P.; Lao, V.V.; Grady, W.B.; Niedzwiecki, D.; Saltz, L.B.; Bertagnolli, M.M.; et al. MRE11-Deficiency Associated with Improved Long-Term Disease Free Survival and Overall Survival in a Subset of Stage III Colon Cancer Patients in Randomized CALGB 89803 Trial. PLoS ONE 2014, 9, e108483. [Google Scholar] [CrossRef] [PubMed]
- Shiovitz, S.; Bertagnolli, M.M.; Renfro, L.A.; Nam, E.; Foster, N.R.; Dzieciatkowski, S.; Luo, Y.; Lao, V.V.; Monnat, R.J., Jr.; Emond, M.J.; et al. CpG Island Methylator Phenotype Is Associated with Response to Adjuvant Irinotecan-Based Therapy for Stage III Colon Cancer. Gastroenterology 2014, 147, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Lao, V.V.; Welcsh, P.; Luo, Y.; Carter, K.T.; Dzieciatkowski, S.; Dintzis, S.; Meza, J.; Sarvetnick, N.E.; Monnat, R.J.; Loeb, L.A.; et al. Altered RECQ Helicase Expression in Sporadic Primary Colorectal Cancers. Transl. Oncol. 2013, 6, 458-IN10. [Google Scholar] [CrossRef]
- Knijnenburg, T.A.; Wang, L.; Zimmermann, M.T.; Chambwe, N.; Gao, G.F.; Cherniack, A.D.; Fan, H.; Shen, H.; Way, G.P.; Greene, C.S.; et al. Genomic and Molecular Landscape of DNA Damage Repair Deficiency across The Cancer Genome Atlas. Cell Rep. 2018, 23, 239–254.e6. [Google Scholar] [CrossRef]
- Kategaya, L.; Perumal, S.K.; Hager, J.H.; Belmont, L.D. Werner Syndrome Helicase Is Required for the Survival of Cancer Cells with Microsatellite Instability. iScience 2019, 13, 488–497. [Google Scholar] [CrossRef]
- Chan, E.M.; Shibue, T.; McFarland, J.M.; Gaeta, B.; Ghandi, M.; Dumont, N.; Gonzalez, A.; McPartlan, J.S.; Li, T.; Zhang, Y.; et al. WRN Helicase Is a Synthetic Lethal Target in Microsatellite Unstable Cancers. Nature 2019, 568, 551–556. [Google Scholar] [CrossRef]
- Picco, G.; Cattaneo, C.M.; Esmée, J.; Crisafulli, G.; Rospo, G.; Consonni, S.; Vieira, S.F.; Rodríguez, I.S.; Cancelliere, C.; Banerjee, R.; et al. Werner Helicase Is a Synthetic-Lethal Vulnerability in Mismatch Repair–Deficient Colorectal Cancer Refractory to Targeted Therapies, Chemotherapy, and Immunotherapy. Cancer Discov. 2021, 11, 1923–1937. [Google Scholar] [CrossRef]
- Aggarwal, M.; Sommers, J.A.; Shoemaker, R.H.; Brosh, R.M., Jr. Inhibition of Helicase Activity by a Small Molecule Impairs Werner Syndrome Helicase (WRN) Function in the Cellular Response to DNA Damage or Replication Stress. Proc. Natl. Acad. Sci. USA 2011, 108, 1525–1530. [Google Scholar] [CrossRef]
- Parker, M.J.; Lee, H.; Yao, S.; Irwin, S.; Hwang, S.; Belanger, K.; de Mare, S.W.; Surgenor, R.; Yan, L.; Gee, P.; et al. Identification of 2-Sulfonyl/Sulfonamide Pyrimidines as Covalent Inhibitors of WRN Using a Multiplexed High-Throughput Screening Assay. Biochemistry 2023, 62, 2147–2160. [Google Scholar] [CrossRef]
- van Wietmarschen, N.; Sridharan, S.; Nathan, W.J.; Tubbs, A.; Chan, E.M.; Callen, E.; Wu, W.; Belinky, F.; Tripathi, V.; Wong, N.; et al. Repeat Expansions Confer WRN Dependence in Microsatellite-Unstable Cancers. Nature 2020, 586, 292–298. [Google Scholar] [CrossRef]
- Hao, S.; Tong, J.; Jha, A.; Risnik, D.; Lizardo, D.; Lu, X.; Goel, A.; Opresko, P.L.; Yu, J.; Zhang, L. Synthetical Lethality of Werner Helicase and Mismatch Repair Deficiency Is Mediated by p53 and PUMA in Colon Cancer. Proc. Natl. Acad. Sci. USA 2022, 119, e2211775119. [Google Scholar] [CrossRef]
- Mengoli, V.; Ceppi, I.; Sanchez, A.; Cannavo, E.; Halder, S.; Scaglione, S.; Gaillard, P.-H.; McHugh, P.J.; Riesen, N.; Pettazzoni, P.; et al. WRN Helicase and Mismatch Repair Complexes Independently and Synergistically Disrupt Cruciform DNA Structures. EMBO J. 2023, 42, e111998. [Google Scholar] [CrossRef]
- Porter, R. The Greatest Benefit to Mankind: A Medical History of Humanity (The Norton History of Science); W. W. Norton & Company: New York, NY, USA, 1999; ISBN 9780393242447. [Google Scholar]
- Weatherall, D.J. Science and the Quiet Art: The Role of Research in Medicine; W. W. Norton & Company: New York, NY, USA, 1995; ISBN 0393037444. [Google Scholar]
- Pradeu, T.; Daignan-Fornier, B.; Ewald, A.; Germain, P.-L.; Okasha, S.; Plutynski, A.; Benzekry, S.; Bertolaso, M.; Bissell, M.; Brown, J.S.; et al. Reuniting Philosophy and Science to Advance Cancer Research. Biol. Rev. Camb. Philos. Soc. 2023, 98, 1668–1686. [Google Scholar] [CrossRef]
- Schaffer, L.V.; Ideker, T. Mapping the Multiscale Structure of Biological Systems. Cell Syst. 2021, 12, 622–635. [Google Scholar] [CrossRef]
- Rollo, J.; Crawford, J.; Hardy, J. A Dynamical Systems Approach for Multiscale Synthesis of Alzheimer’s Pathogenesis. Neuron 2023, 111, 2126–2139. [Google Scholar] [CrossRef]
- Kakiuchi, N.; Ogawa, S. Clonal Expansion in Non-Cancer Tissues. Nat. Rev. Cancer 2021, 21, 239–256. [Google Scholar] [CrossRef]
- Rane, J.K.; Frankell, A.M.; Weeden, C.E.; Swanton, C. Clonal Evolution in Healthy and Premalignant Tissues: Implications for Early Cancer Interception Strategies. Cancer Prev. Res. 2023, 16, 369–378. [Google Scholar] [CrossRef]
- Domcke, S.; Shendure, J. A Reference Cell Tree Will Serve Science Better than a Reference Cell Atlas. Cell 2023, 186, 1103–1114. [Google Scholar] [CrossRef]
- Qiu, C.; Martin, B.K.; Welsh, I.C.; Daza, R.M.; Le, T.-M.; Huang, X.; Nichols, E.K.; Taylor, M.L.; Fulton, O.; O’Day, D.R.; et al. A Single-Cell Transcriptional Timelapse of Mouse Embryonic Development, from Gastrula to Pup. bioRxiv 2023. [Google Scholar] [CrossRef]
- Coorens, T.H.H.; Moore, L.; Robinson, P.S.; Sanghvi, R.; Christopher, J.; Hewinson, J.; Przybilla, M.J.; Lawson, A.R.J.; Spencer Chapman, M.; Cagan, A.; et al. Extensive Phylogenies of Human Development Inferred from Somatic Mutations. Nature 2021, 597, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.; Cagan, A.; Coorens, T.H.H.; Neville, M.D.C.; Sanghvi, R.; Sanders, M.A.; Oliver, T.R.W.; Leongamornlert, D.; Ellis, P.; Noorani, A.; et al. The Mutational Landscape of Human Somatic and Germline Cells. Nature 2021, 597, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, P.; Bandlamudi, C.; Jonsson, P.; Kemel, Y.; Chavan, S.S.; Richards, A.L.; Penson, A.V.; Bielski, C.M.; Fong, C.; Syed, A.; et al. The Context-Specific Role of Germline Pathogenicity in Tumorigenesis. Nat. Genet. 2021, 53, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Carter, H.; Marty, R.; Hofree, M.; Gross, A.M.; Jensen, J.; Fisch, K.M.; Wu, X.; DeBoever, C.; Van Nostrand, E.L.; Song, Y.; et al. Interaction Landscape of Inherited Polymorphisms with Somatic Events in Cancer. Cancer Discov. 2017, 7, 410–423. [Google Scholar] [CrossRef]
- Huang, K.-L.; Mashl, R.J.; Wu, Y.; Ritter, D.I.; Wang, J.; Oh, C.; Paczkowska, M.; Reynolds, S.; Wyczalkowski, M.A.; Oak, N.; et al. Pathogenic Germline Variants in 10,389 Adult Cancers. Cell 2018, 173, 355–370.e14. [Google Scholar] [CrossRef]
- Moiseeva, V.; Cisneros, A.; Sica, V.; Deryagin, O.; Lai, Y.; Jung, S.; Andrés, E.; An, J.; Segalés, J.; Ortet, L.; et al. Senescence atlas reveals an aged-like inflamed niche that blunts muscle regeneration. Nature 2023, 613, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.E.; Cropley, V.; Maier, A.B.; Lautenschlager, N.T.; Breakspear, M.; Zalesky, A. Heterogeneous Aging across Multiple Organ Systems and Prediction of Chronic Disease and Mortality. Nat. Med. 2023, 29, 1221–1231. [Google Scholar] [CrossRef] [PubMed]
- Rosen, Y.; Roohani, Y.; Agarwal, A.; Samotorčan, L.; Consortium, T.S.; Quake, S.R.; Leskovec, J. Universal Cell Embeddings: A Foundation Model for Cell Biology. bioRxiv 2023. [Google Scholar] [CrossRef]
- Fleck, J.S.; Jansen, S.M.J.; Wollny, D.; Zenk, F.; Seimiya, M.; Jain, A.; Okamoto, R.; Santel, M.; He, Z.; Camp, J.G.; et al. Inferring and Perturbing Cell Fate Regulomes in Human Brain Organoids. Nature 2022, 621, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Moder, M.; Velimezi, G.; Owusu, M.; Mazouzi, A.; Wiedner, M.; Ferreira da Silva, J.; Robinson-Garcia, L.; Schischlik, F.; Slavkovsky, R.; Kralovics, R.; et al. Parallel Genome-Wide Screens Identify Synthetic Viable Interactions between the BLM Helicase Complex and Fanconi Anemia. Nat. Commun. 2017, 8, 1238. [Google Scholar] [CrossRef] [PubMed]
- German, J. Bloom’s syndrome. I. Genetical and clinical observations in the first twenty-seven patients. Am. J. Hum. Genet. 1969, 21, 196–227. [Google Scholar] [PubMed]
- Rolland, Y.; Sierra, F.; Ferrucci, L.; Barzilai, N.; De Cabo, R.; Mannick, J.; Oliva, A.; Evans, W.; Angioni, D.; De Souto Barreto, P.; et al. Challenges in Developing Geroscience Trials. Nat. Commun. 2023, 14, 5038. [Google Scholar] [CrossRef] [PubMed]
- Moqri, M.; Herzog, C.; Poganik, J.R.; Biomarkers of Aging Consortium; Justice, J.; Belsky, D.W.; Higgins-Chen, A.; Moskalev, A.; Fuellen, G.; Cohen, A.A.; et al. Biomarkers of Aging for the Identification and Evaluation of Longevity Interventions. Cell 2023, 186, 3758–3775. [Google Scholar] [CrossRef] [PubMed]
- Goto, M.; Sugimoto, K.; Hayashi, S.; Ogino, T.; Sugimoto, M.; Furuichi, Y.; Matsuura, M.; Ishikawa, Y.; Iwaki-Egawa, S.; Watanabe, Y. Aging-Associated Inflammation in Healthy Japanese Individuals and Patients with Werner Syndrome. Exp. Gerontol. 2012, 47, 936–939. [Google Scholar] [CrossRef]
- Goto, M.; Hayata, K.; Chiba, J.; Matsuura, M.; Iwaki-Egawa, S.; Watanabe, Y. Multiplex Cytokine Analysis of Werner Syndrome. Intractable Rare Dis. Res. 2015, 4, 190–197. [Google Scholar] [CrossRef]
- Mengelkoch, S.; Gassen, J.; Lev-Ari, S.; Alley, J.C.; Schüssler-Fiorenza Rose, S.M.; Snyder, M.P.; Slavich, G.M. Multi-omics in stress and health research: Study designs that will drive the field forward. Stress. 2024, 27, 2321610. [Google Scholar] [CrossRef] [PubMed]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. Hallmarks of Aging: An Expanding Universe. Cell 2023, 186, 243–278. [Google Scholar] [CrossRef] [PubMed]
- Aumailley, L.; Garand, C.; Dubois, M.J.; Johnson, F.B.; Marette, A.; Lebel, M. Metabolic and Phenotypic Differences between Mice Producing a Werner Syndrome Helicase Mutant Protein and Wrn Null Mice. PLoS ONE 2015, 10, e0140292. [Google Scholar] [CrossRef] [PubMed]
- Wishart, D.S.; Guo, A.; Oler, E.; Wang, F.; Anjum, A.; Peters, H.; Dizon, R.; Sayeeda, Z.; Tian, S.; Lee, B.L.; et al. HMDB 5.0: The Human Metabolome Database for 2022. Nucleic Acids Res. 2022, 50, D622–D631. [Google Scholar] [CrossRef] [PubMed]
- Maierhofer, A.; Flunkert, J.; Oshima, J.; Martin, G.M.; Haaf, T.; Horvath, S. Accelerated Epigenetic Aging in Werner Syndrome. Aging 2017, 9, 1143–1152. [Google Scholar] [CrossRef] [PubMed]
- Lu, A.T.; Fei, Z.; Haghani, A.; Robeck, T.R.; Zoller, J.A.; Li, C.Z.; Lowe, R.; Yan, Q.; Zhang, J.; Vu, H.; et al. Universal DNA Methylation Age across Mammalian Tissues. Nat Aging 2023, 3, 1144–1166. [Google Scholar] [CrossRef] [PubMed]
- Haghani, A.; Li, C.Z.; Robeck, T.R.; Zhang, J.; Lu, A.T.; Ablaeva, J.; Acosta-Rodríguez, V.A.; Adams, D.M.; Alagaili, A.N.; Almunia, J.; et al. DNA Methylation Networks Underlying Mammalian Traits. Science 2023, 381, eabq5693. [Google Scholar] [CrossRef] [PubMed]
- Timmons, J.A.; Brenner, C. The Information Theory of Aging Has Not Been Tested. Cell 2024, 187, 1101–1102. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-H.; Hayano, M.; Rajman, L.A.; Sinclair, D.A. Response to: The Information Theory of Aging Has Not Been Tested. Cell 2024, 187, 1103–1105. [Google Scholar] [CrossRef]
- Oh, H.S.-H.; Rutledge, J.; Nachun, D.; Pálovics, R.; Abiose, O.; Moran-Losada, P.; Channappa, D.; Urey, D.Y.; Kim, K.; Sung, Y.J.; et al. Organ Aging Signatures in the Plasma Proteome Track Health and Disease. Nature 2023, 624, 164–172. [Google Scholar] [CrossRef]
- Evans, M.A.; Walsh, K. Clonal Hematopoiesis, Somatic Mosaicism, and Age-Associated Disease. Physiol. Rev. 2023, 103, 649–716. [Google Scholar] [CrossRef]
- Avagyan, S.; Zon, L.I. Clonal Hematopoiesis and Inflammation—The Perpetual Cycle. Trends Cell Biol. 2023, 33, 695–707. [Google Scholar] [CrossRef] [PubMed]
- Dawoud, A.A.Z.; Gilbert, R.D.; Tapper, W.J.; Cross, N.C.P. Clonal Myelopoiesis Promotes Adverse Outcomes in Chronic Kidney Disease. Leukemia 2022, 36, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Weeks, L.D.; Ebert, B.L. Causes and Consequences of Clonal Hematopoiesis. Blood 2023, 142, 2235–2246. [Google Scholar] [CrossRef] [PubMed]
- Langlois, R.G.; Bigbee, W.L.; Jensen, R.H.; German, J. Evidence for Increased in Vivo Mutation and Somatic Recombination in Bloom’s Syndrome. Proc. Natl. Acad. Sci. USA 1989, 86, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Leslie, M. NIH Project Probes the Human Body’s Multitude of Genomes. Science 2023, 381, 719–720. [Google Scholar] [CrossRef] [PubMed]
- Schneider, G.; Schmidt-Supprian, M.; Rad, R.; Saur, D. Tissue-Specific Tumorigenesis: Context Matters. Nat. Rev. Cancer 2017, 17, 239–253. [Google Scholar] [CrossRef] [PubMed]
- Haigis, K.M.; Cichowski, K.; Elledge, S.J. Tissue-Specificity in Cancer: The Rule, Not the Exception. Science 2019, 363, 1150–1151. [Google Scholar] [CrossRef] [PubMed]
- Monnat, R.J., Jr. Cancer pathogenesis in the human RecQ helicase deficiency syndromes. In From Premature Gray Hair to Helicase—Werner Syndrome: Implications for Aging and Cancer; Goto, M., Miller, R.W., Eds.; Gann Monograph on Cancer Research; Springer: Berlin/Heidelberg, Germany, 2001; Volume 49, pp. 83–94. [Google Scholar]
- Opresko, P.L.; Otterlei, M.; Graakjaer, J.; Bruheim, P.; Dawut, L.; Kølvraa, S.; May, A.; Seidman, M.M.; Bohr, V.A. The Werner Syndrome Helicase and Exonuclease Cooperate to Resolve Telomeric D Loops in a Manner Regulated by TRF1 and TRF2. Mol. Cell 2004, 14, 763–774. [Google Scholar] [CrossRef]
- Ballinger, M.L.; Pattnaik, S.; Mundra, P.A.; Zaheed, M.; Rath, E.; Priestley, P.; Baber, J.; Ray-Coquard, I.; Isambert, N.; Causeret, S.; et al. Heritable Defects in Telomere and Mitotic Function Selectively Predispose to Sarcomas. Science 2023, 379, 253–260. [Google Scholar] [CrossRef]
- DeBoy, E.A.; Tassia, M.G.; Schratz, K.E.; Yan, S.M.; Cosner, Z.L.; McNally, E.J.; Gable, D.L.; Xiang, Z.; Lombard, D.B.; Antonarakis, E.S.; et al. Familial Clonal Hematopoiesis in a Long Telomere Syndrome. N. Engl. J. Med. 2023, 388, 2422–2433. [Google Scholar] [CrossRef] [PubMed]
- Nassour, J.; Aguiar, L.G.; Correia, A.; Schmidt, T.T.; Mainz, L.; Przetocka, S.; Haggblom, C.; Tadepalle, N.; Williams, A.; Shokhirev, M.N.; et al. Telomere-to-Mitochondria Signalling by ZBP1 Mediates Replicative Crisis. Nature 2023, 614, 767–773. [Google Scholar] [CrossRef]
- Gulen, M.F.; Samson, N.; Keller, A.; Schwabenland, M.; Liu, C.; Glück, S.; Thacker, V.V.; Favre, L.; Mangeat, B.; Kroese, L.J.; et al. cGAS–STING Drives Ageing-Related Inflammation and Neurodegeneration. Nature 2023, 620, 374–380. [Google Scholar] [CrossRef]
- De Rosa, M.; Opresko, P.L. Translating the Telomeres. Trends Genet. 2023, 39, 593–595. [Google Scholar] [CrossRef] [PubMed]
- Mouchiroud, L.; Houtkooper, R.H.; Moullan, N.; Katsyuba, E.; Ryu, D.; Cantó, C.; Mottis, A.; Jo, Y.-S.; Viswanathan, M.; Schoonjans, K.; et al. The NAD(+)/Sirtuin Pathway Modulates Longevity through Activation of Mitochondrial UPR and FOXO Signaling. Cell 2013, 154, 430–441. [Google Scholar] [CrossRef] [PubMed]
- Houtkooper, R.H.; Mouchiroud, L.; Ryu, D.; Moullan, N.; Katsyuba, E.; Knott, G.; Williams, R.W.; Auwerx, J. Mitonuclear Protein Imbalance as a Conserved Longevity Mechanism. Nature 2013, 497, 451–457. [Google Scholar] [CrossRef]
- Patel, J.; Baptiste, B.A.; Kim, E.; Hussain, M.; Croteau, D.L.; Bohr, V.A. DNA Damage and Mitochondria in Cancer and Aging. Carcinogenesis 2020, 41, 1625–1634. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Wang, K.; Stock, A.J.; Gong, Y.; Demarest, T.G.; Yang, B.; Giri, N.; Harrington, L.; Alter, B.P.; Savage, S.A.; et al. Re-Equilibration of Imbalanced NAD Metabolism Ameliorates the Impact of Telomere Dysfunction. EMBO J. 2020, 39, e103420. [Google Scholar] [CrossRef]
- Kim, S.; Ramalho, T.R.; Haynes, C.M. Regulation of Proteostasis and Innate Immunity via Mitochondria-Nuclear Communication. J. Cell Biol. 2024, 223, e202310005. [Google Scholar] [CrossRef]
- Murphy, M.P.; O’Neill, L.A.J. A Break in Mitochondrial Endosymbiosis as a Basis for Inflammatory Diseases. Nature 2024, 626, 271–279. [Google Scholar] [CrossRef]
- Carbone, M.; Arron, S.T.; Beutler, B.; Bononi, A.; Cavenee, W.; Cleaver, J.E.; Croce, C.M.; D’Andrea, A.; Foulkes, W.D.; Gaudino, G.; et al. Tumour Predisposition and Cancer Syndromes as Models to Study Gene–environment Interactions. Nat. Rev. Cancer 2020, 20, 533–549. [Google Scholar] [CrossRef] [PubMed]
- Weeden, C.E.; Hill, W.; Lim, E.L.; Grönroos, E.; Swanton, C. Impact of Risk Factors on Early Cancer Evolution. Cell 2023, 186, 1541–1563. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.L.W.; Chadha, S.; Liu, Y.; Gabasova, E.; Perera, D.; Ahmed, K.; Constantinou, S.; Renaudin, X.; Lee, M.; Aebersold, R.; et al. A Class of Environmental and Endogenous Toxins Induces BRCA2 Haploinsufficiency and Genome Instability. Cell 2017, 169, 1105–1118.e15. [Google Scholar] [CrossRef] [PubMed]
- Swanton, C.; Bernard, E.; Abbosh, C.; André, F.; Auwerx, J.; Balmain, A.; Bar-Sagi, D.; Bernards, R.; Bullman, S.; DeGregori, J.; et al. Embracing Cancer Complexity: Hallmarks of Systemic Disease. Cell 2024, 187, 1589–1616. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.; Ashley, E.A. Artificial Intelligence in Molecular Medicine. N. Engl. J. Med. 2023, 388, 2456–2465. [Google Scholar] [CrossRef] [PubMed]
- Haug, C.J.; Drazen, J.M. Artificial Intelligence and Machine Learning in Clinical Medicine, 2023. N. Engl. J. Med. 2023, 388, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Fu, T.; Du, Y.; Gao, W.; Huang, K.; Liu, Z.; Chandak, P.; Liu, S.; Van Katwyk, P.; Deac, A.; et al. Scientific Discovery in the Age of Artificial Intelligence. Nature 2023, 620, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Woicik, A.; Poon, H.; Altman, R.B.; Wang, S. Multilingual Translation for Zero-Shot Biomedical Classification Using BioTranslator. Nat. Commun. 2023, 14, 738. [Google Scholar] [CrossRef] [PubMed]
- Fang, E.F.; Hou, Y.; Lautrup, S.; Jensen, M.B.; Yang, B.; SenGupta, T.; Caponio, D.; Khezri, R.; Demarest, T.G.; Aman, Y.; et al. NAD+ Augmentation Restores Mitophagy and Limits Accelerated Aging in Werner Syndrome. Nat. Commun. 2019, 10, 5284. [Google Scholar] [CrossRef]
- Kulkarni, A.S.; Gubbi, S.; Barzilai, N. Benefits of Metformin in Attenuating the Hallmarks of Aging. Cell Metab. 2020, 32, 15–30. [Google Scholar] [CrossRef]
- Lincoff, A.M.; Brown-Frandsen, K.; Colhoun, H.M.; Deanfield, J.; Emerson, S.S.; Esbjerg, S.; Hardt-Lindberg, S.; Hovingh, G.K.; Kahn, S.E.; Kushner, R.F.; et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. N. Engl. J. Med. 2023, 389, 2221–2232. [Google Scholar] [CrossRef]
- Chaib, S.; Tchkonia, T.; Kirkland, J.L. Cellular Senescence and Senolytics: The Path to the Clinic. Nat. Med. 2022, 28, 1556–1568. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, A.S.; Aleksic, S.; Berger, D.M.; Sierra, F.; Kuchel, G.A.; Barzilai, N. Geroscience-Guided Repurposing of FDA-Approved Drugs to Target Aging: A Proposed Process and Prioritization. Aging Cell 2022, 21, e13596. [Google Scholar] [CrossRef] [PubMed]
- Sanmarco, L.M.; Rone, J.M.; Polonio, C.M.; Fernandez Lahore, G.; Giovannoni, F.; Ferrara, K.; Gutierrez-Vazquez, C.; Li, N.; Sokolovska, A.; Plasencia, A.; et al. Lactate Limits CNS Autoimmunity by Stabilizing HIF-1α in Dendritic Cells. Nature 2023, 620, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Koblan, L.W.; Erdos, M.R.; Wilson, C.; Cabral, W.A.; Levy, J.M.; Xiong, Z.-M.; Tavarez, U.L.; Davison, L.M.; Gete, Y.G.; Mao, X.; et al. In Vivo Base Editing Rescues Hutchinson-Gilford Progeria Syndrome in Mice. Nature 2021, 589, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Oshima, J.; Kato, H.; Maezawa, Y.; Yokote, K. RECQ Helicase Disease and Related Progeroid Syndromes: RECQ2018 Meeting. Mech. Ageing Dev. 2018, 173, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Gawande, A. The Bell Curve. The New Yorker, 6 December 2004; 82–91. [Google Scholar]
- Gawande, A. The Heroism of Incremental Care. The New Yorker, 23 January 2017. [Google Scholar]
- Kato, H.; Koshizaka, M.; Kaneko, H.; Maezawa, Y.; Yokote, K. Lifetime Extension and the Recent Cause of Death in Werner Syndrome: A Retrospective Study from 2011 to 2020. Orphanet J. Rare Dis. 2022, 17, 226. [Google Scholar] [CrossRef] [PubMed]
- Yokote, K.; Saito, Y. Extension of the Life Span in Patients with Werner Syndrome. J. Am. Geriatr. Soc. 2008, 56, 1770–1771. [Google Scholar] [CrossRef]
- Takemoto, M.; Yokote, K. Preface to Management Guideline for Werner Syndrome 2020. Geriatr. Gerontol. Int. 2021, 21, 131–132. [Google Scholar] [CrossRef]
- Keller, C.; Keller, K.R.; Shew, S.B.; Plon, S.E. Growth Deficiency and Malnutrition in Bloom Syndrome. J. Pediatr. 1999, 134, 472–479. [Google Scholar] [CrossRef]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monnat, R.J., Jr. James German and the Quest to Understand Human RECQ Helicase Deficiencies. Cells 2024, 13, 1077. https://doi.org/10.3390/cells13131077
Monnat RJ Jr. James German and the Quest to Understand Human RECQ Helicase Deficiencies. Cells. 2024; 13(13):1077. https://doi.org/10.3390/cells13131077
Chicago/Turabian StyleMonnat, Raymond J., Jr. 2024. "James German and the Quest to Understand Human RECQ Helicase Deficiencies" Cells 13, no. 13: 1077. https://doi.org/10.3390/cells13131077




