Abstract
The issue of environmental nanoplastic (NPl) particle and microplastic (MPl) particle pollution is becoming increasingly severe, significantly impacting ecosystems and biological health. Research shows that NPl/MPl can penetrate the placental barrier and enter the fetus, leading to transgenerational effects. This review integrates the existing literature on the effects of prenatal NPl/MPl exposure on mammalian offspring, focusing particularly on its negative impacts on the central nervous system, liver, intestinal health, reproductive function, and skeletal muscles. The vast majority of previous studies on prenatal NPl/MPl in mammals have used polystyrene material. Future research should explore the effects of other prenatal NPl/MPl materials on offspring to better reflect the realities of the human environment. It is also essential to investigate the potential harm and underlying mechanisms associated with prenatal NPl/MPl exposure to offspring in greater depth. This will aid in developing appropriate prevention and treatment strategies in the future.
1. Introduction
Globally, up to 400 million tons of plastic are produced annually, with a recycling rate of only 9% since 2012 [1,2]. A substantial amount of plastic debris already exists in the natural environment, with an estimated 5 trillion plastic pieces weighing over 250,000 tons floating in the world’s oceans as of 2013 [3]. Plastic polymers are classified as permanent organic pollutant substances (POPSs) due to the additives they contain. In fact, plastic production includes many additives such as antioxidants, lubricants, corrosion inhibitors, plasticizers, adhesives, heat stabilizers, and flame retardants [4]. However, in environmental and biological systems, plastics undergo biotic and abiotic weathering and degradation, resulting in the generation of numerous tiny particles. These tiny plastic particles are a serious environmental threat, given their almost universal presence in all ecosystems [5]. Tiny plastic particles are transported over long distances through processes such as wind dispersal, river flow, and ocean currents. Consequently, they are widely distributed in water bodies, soils, and the atmosphere worldwide [6]. They enter the biological cycle of numerous species through ingestion and respiration, potentially harming the health and reproduction of these organisms. This may eventually lead human exposure to these tiny plastic particles via the consumption of contaminated seafood and water [7,8]. Consequently, the presence of tiny plastic particles has become a matter of heightened concern. According to research, each individual may ingest tiny plastic particles between 0.1 to 5.0 g per week, with sizes not exceeding 1 mm, which is equivalent to 74,000 to 121,000 particles per year [9,10]. The majority of ingested plastic particles, especially larger ones, are excreted through feces; however, smaller plastic particles are more likely to be absorbed by the individual [11]. According to ISO 24187:2023 [12], these tiny plastic particles are classified by their size as nanoplastics (NPls) (<1 µm) and microplastics (MPls) (>1 µm and <5 mm) [13]. Smaller particles often exhibit higher toxicity than larger plastic particles at equivalent mass concentrations. Based on accumulated evidence, plastic particles with a diameter of less than 150 μm can penetrate intestinal epithelial cells, while those ranging from 0.1 to 10.0 μm in diameter can cross the blood–brain barrier and biological membranes [14].
NPls/MPls have been detected in numerus human biological samples, including the saliva [15], breast milk [16], lungs [17,18], liver [19], kidneys [20], colon [21], and blood [22]. These findings can substantially expand our understanding of human exposure to NPl/MPl. Given the ongoing challenge in quantifying human exposure to NPl/MPl, assessing their impact on other organisms has become an important method of better understanding the effect of NPl/MPl exposure on the human body [23]. Although numerous studies have explored the effects of NPl/MPl on cells and aquatic animals, relatively few have focused on their impact on terrestrial animals [24]. In cell culture experiments, short-term exposure to high concentrations of polystyrene (PS) particles is commonly used for research purposes. This exposure induces oxidative stress [25,26], inflammatory responses [27], mitochondrial dysfunction [26], lysosomal impairment [28], apoptosis [27], and genetic toxicity [7,29,30]. Upon feeding mice with 5 and 20 µm of PS-MPl for 28 days, PS-MPls were detected in the liver, kidneys, and intestines [31]. Studies have indicated that MPl accumulation in mouse liver tissue can lead to an imbalance in energy and lipid metabolism, an increase in oxidative stress, neurotoxic responses, gut dysbiosis, and impairment of the intestinal barrier [31,32,33,34]. NPls/MPls can also pose health risks by adsorbing other chemical pollutants such as phthalates, bisphenol A, brominated flame retardants, polychlorinated biphenyls, and heavy metals [35,36].
Animal experiments and human placental studies have confirmed that NPls can traverse the placental barrier from mother to fetus through diffusion or by binding with cell transport proteins, reaching multiple tissues of the developing fetus [37,38,39]. In a recent observational study, Ragusa et al. [40] reported the presence of 12 MPl fragments, three of which were identified as stained polypropylene (PP), with only pigments identified for the other nine. These fragments ranged in size from approximately 5 to 10 µm in samples collected from four human placentas, demonstrating a substantially larger particle size than that detected in a previous study [39]. Accordingly, MPls can be transferred from the mother to the unborn fetus and pose a greater risk to offspring than previously understood.
Animal experiments have also revealed that maternal exposure to 0.5 μm NPl or 5 μm MPl can alter the energy and lipid metabolism of offspring, indicating the potential transgenerational effects of NPl/MPl particle exposure [41]. The Developmental Origins of Health and Disease (DOHaD) concept focuses on exploring how exposure to environmental factors during the perinatal period can affect the development of non-communicable diseases in later life, such as diabetes, fatty liver, hypertension, chronic kidney disease, asthma, and cognitive impairment [42]. According to this theory, physiological and structural changes in the fetus due to environmental stress may increase the likelihood of diseases in the future. This influence may involve metabolic processes, immune function, and tissue development, leading to long-term effects on health and potential disease risks. Considering the potential multigenerational adverse impacts and mechanisms of NPl/MPl exposure on biological systems, it is important to investigate the transgenerational effects of prenatal microplastic exposure and explore effective strategies for managing NPl/MPl. To date, most research on NPl/MPl has focused on their impact on the health of adult humans and animals. However, their influence on next-generation development has not been thoroughly studied. The purpose of this review was to summarize the existing literature on the effects of prenatal exposure to NPl/MPl on offspring, particularly focusing on mammals to provide new opportunities for the prevention or treatment of toxic hazards brought about by environmental NPl/MPl contamination.
2. Methods
The data collection process involved a systematic literature analysis using two comprehensive databases, PubMed/Google Scholar (accessed on 8 August 2024), and a thorough search strategy. Different keyword combinations were used, including “microplastic”, “nanoplastic”, “prenatal”, “maternal”, “fetus”, and “offspring”, which were combined with one another. Each category was searched independently in the databases. The search focused solely on original articles published in English, which had to be accessible through open access or institutional subscriptions, while excluding review articles, conference abstracts, and book chapters. The initial search yielded 3110 items across all analysis groups, which were subsequently filtered. The filtering process began with a manual review of titles and abstracts to eliminate duplicate entries and exclude irrelevant publications. Irrelevant publications primarily fell into one of the following categories: (1) model studies (in vitro or computational); (2) NPl/MPl analyses in non-mammalian species; (3) studies related to NPl/MPl that involved only the maternal, placenta, or cell lines without reference to the fetus or offspring; (4) publications that only described microplastic tissue deposition without discussing histological or functional impacts; and (5) studies that solely explored the effects of other chemical components, such as plasticizers or bisphenol, A on offspring. After carefully reviewing and selecting the literature, a total of 20 of the most detailed original studies were ultimately included and analyzed in detail.
3. The Impact of Prenatal Exposure to NPl/MPl on the Offspring of Mammals
Regarding the effects of plastic particle exposure during pregnancy on the number of live births and birth weight of offspring in pregnant dams, different studies have shown inconsistent results. With PE-MPl administered by gavage to mice, the PE-MP treated group had fewer live births per dam and lighter pups compared to the control group [43]. Another study indicated that prenatal exposure to PS-NPl reduces the birth weight of offspring but does not affect the number or survival rate of the offspring [44,45]. This inconsistency may be related to variations in experimental design and the different species used in the studies. As a result, when choosing articles to read, it is essential to consider the specific details of each study’s experimental design. Next, the effects of prenatal NPl/MPl exposure on different organs will be discussed individually.
3.1. The Iimpact of Prenatal NPl/MPl Exposure on the Central NervousSystem and Retina of Mammalian Offspring (Table 1)
Upon ingestion by mammals, NPl/MPl may exert local effects or enter the bloodstream to reach different organs and tissues [46,47]. Regarding maternal–fetal transfer, after maternal ingestion, NPl/MPl can penetrate the placenta and accumulate in fetal tissues, although the precise mechanisms by which MPl and NPl cross the placental barrier remain elusive [38,39,40]. In mice, prenatal and postnatal exposure to PS particles resulted in their accumulation in several brain regions, including the brainstem [48]. This suggests that PS particles can penetrate the blood–brain barrier and accumulate in the brains of offspring. Yang et al. [49] administered PS-NPl (0.1 μm) and PS-MPl (1 μm) orally to pregnant C57BL mice from gestational days 1 to 17 at a dosage of 1 mg/day and observed the effects on fetuses. The authors found that maternal exposure to MPl and NPl during pregnancy can lead to the deposition of both types of particles in the placenta; however, only PS-NPl particles penetrated the fetal hypothalamus. Offspring showed reduced levels of γ-aminobutyric acid in the prefrontal cortex and amygdala before the 8th week and exhibited anxiety-like behavior.
In pregnant and lactating dams, Jeong et al. [38] found that oral exposure of pregnant and lactating dams to PS-NPl resulted in a higher transfer of these particles to the brains of offspring through lactation than through the placenta prenatally. The authors [38] found that transcriptional expression of genes associated with neurogenic stem cell proliferation was reduced in the hippocampal region of offspring mice, accompanied by an imbalance in energy metabolism in neuroglial cells, upon oral exposure of pregnant and lactating mice to PS-NPl. Prenatal and postpartum exposure to PS-NPl substantially reduced the thickness of the neuronal layer and corpus callosum in the CA3 region of the offspring. Moreover, exposure to high concentrations of PS-NPl could result in abnormal brain development, potentially inducing sex-specific neurological abnormalities and cognitive defects in females [38].
Shin et al. [48] administered PS-NPl orally to C57BL/6J dams during pregnancy and lactation. The authors found that PS-NPl exposure suppressed the expression of brain development-related genes (Gabra2, Fgf8, Shh, Wnt2b, Wnt3, Ccnd1, Ctnnb1, and Creb1) in the embryonic brain and altered the expression of the Gabra2 gene and protein in the brains of adult offspring mice. Exposure to PS-NPl during pregnancy and lactation led to anxiety- and depression-like behaviors, as well as social deficits in offspring mice. However, it did not affect cognitive function or nest-building behavior in the mouse offspring [48]. These studies were designed to simulate exposure to plastic particles during pregnancy and postpartum without specifically examining the effects of maternal ingestion of PS-NPl solely during pregnancy on the offspring’s brain. In C57BL/6J and CD-1 mice, prenatal polyethylene (PE)-MPl exposure resulted in repetitive and compulsive behaviors, increased social interaction, reduced social novelty, and reduced spatial working memory, indicating the occurrence of autism spectrum disorder-like behaviors [50].
During pregnancy and lactation, administering 0.05 μm PS-NPl via gavage to female SD rats resulted in changes to monoamine neurotransmitters in the cortex and amino acid neurotransmitters in the hippocampus (e.g., downregulation of GABA) in their offspring by the age of 22 days. Histological observations show disorganized cortical migration in the neocortex of 22-day-old offspring, characterized by reduced cortical plate thickness, excessive proliferation of superficial layer neurons, and a decrease in the number of deep-layer neurons. By the seventh week after birth, the offspring also exhibit anxiety behaviors and deficits in spatial memory [51].
In pregnant dams, PS-NPl exposure via the lungs resulted in NPl penetration of the placental barrier, ultimately reaching the fetus. Fournier et al. [37] administered 20 nm-sized PS-NPl (2.64 × 1014 particles) via tracheal instillation to Sprague Dawley (SD) rats on gestational day 19. After 24 h, fluorescence microscopy revealed the presence of PS-NPl in the placenta, fetal brain, liver, lungs, heart, and kidneys, indicating that NPl can traverse the placental barrier and cause deposition in fetal tissues upon late gestational maternal lung exposure.
The retina is an extension of the central nervous system that undergoes terminal differentiation, possessing a unique structure and function responsible for capturing light and converting it into neural signals for visual processing. Recent research indicates that maternal exposure to PS-NPl can adversely affect the retinal development and function of offspring mice [52]. Providing maternal mice with drinking water containing 10 mg/L of PS-NPl (0.1 μm) during gestation and lactation led to developmental and functional abnormalities of the neural retina in their offspring. The authors observed the deposition of PS-NPl in the retinal tissues of offspring along with a decrease in the number of retinal ganglion cells and bipolar cells. Furthermore, offspring exposed to prenatal PS-NPl exhibited delayed development of retinal vasculature and abnormal electroretinogram (ERG) responses, coupled with increased oxidative stress levels. At the molecular level, amino acid metabolism dysregulation and alterations in gene expression were noted in the retinal tissues of the exposed offspring. The pathways mediated by the Fos gene may be a potential target affected by PS-NPl exposure during retinal development.

Table 1.
The impact of prenatal NPl/MPl exposure on the central nervous system of mammalian offspring.
Table 1.
The impact of prenatal NPl/MPl exposure on the central nervous system of mammalian offspring.
| Material | Design | Size | Species/Stage | Effects | Ref. |
|---|---|---|---|---|---|
| PS | Prenatal oral ingestion | 0.1 μm NPl + 1 μm MPl |
|
| [49] |
| PS | Prenatal and postpartum oral ingestion | 0.05 μm NPl |
|
| [38] |
| PS | Prenatal and postpartum oral ingestion | 0.193 μm MPl and 0.04 μm NPl |
|
| [48] |
| PE | Prenatal oral ingestion | 10–20 μm MPl |
|
| [50] |
| PS | Prenatal and lactation oral ingestion | 0.05 μm NPl |
|
| [51] |
| The impact of prenatal NPl/MPl exposure on the retina of mammalian offspring | |||||
| PS | Prenatal and lactation oral ingestion | 0.1 μm NPl |
|
| [52] |
Abbreviations: ASD, autism spectrum disorder; ERG, electroretinogram; GABA, γ-aminobutyric acid; MPl, microplastics; NPl, nanoplastics; PE, polyethylene; PND, postnatal day, PS, polystyrene; SD, Sprague Dawley.
3.2. The Impact of Prenatal NPl/MPl Exposure on the Liver and Metabolism of Mammalian Offspring (Table 2)
Luo et al. [41] administered pregnant mice with 0.5 μm of PS-NPl or 5.0 μm of PS-MPl in water at concentrations of 100 or 1000 μg/L. The authors detected the presence of metabolic disruptions in serum levels of triglycerides (TGs), total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol, as well as in the liver TC and TG levels of 6-week-old offspring, with 5 μm MPl having a greater impact than 0.5 μm particles. Prenatal NPl/MPl exposure can alter the expression of genes involved in fatty acid synthesis in the liver, which may be an underlying mechanism involved in the disruption of fatty acid metabolism [41].
In our literature review, we found that administering a high-fat diet and/or 5 µm PS-MPl to pregnant SD rats increased liver lipid accumulation, as determined by histological examination, in offspring on postnatal day 7 [53]. Simultaneous exposure to a prenatal high-fat diet and prenatal PS-MPl resulted in severe hepatic steatosis in the offspring. Higher prenatal doses of PS-MPl led to shortened small intestines in the offspring. Prenatal exposure to both a high-fat diet and PS-MPl increases hepatic interleukin-6 levels, apoptosis, and oxidative stress in pups. Moreover, simultaneous exposure to a prenatal high-fat diet and prenatal PS-MPl exacerbated hepatic apoptosis and oxidative stress in offspring [53]. These findings suggest that prenatal co-exposure to another adversity may exacerbate the liver damage caused by prenatal microplastic exposure in offspring.
Moreover, PS-MPl exposure during pregnancy and lactation in mice can lead to maternal metabolic disorders, gut microbiota dysbiosis, and intestinal barrier impairment [34]. Additionally, maternal exposure to PS-MPl was shown to induce transgenerational effects, resulting in decreased levels of glucose, acetate, TC, and TG in F1 female descendants; decreased TC levels in the liver; and changes in the mRNA expression of genes related to carbohydrate and lipid metabolism in F1 offspring. Exposure of animals to PS-MPl during pregnancy and lactation can have long-term metabolic consequences in both F1 and F2 generations [34]. The inflammatory response appears to play a pivotal role in these transgenerational effects. Huang et al. [44] found that Kunming mouse offspring exposed to PS-NPl (0.1 μm in size) during the prenatal and lactational stages exhibited a decrease in liver weight, hepatic oxidative stress, inflammatory cell infiltration, enhanced proinflammatory cytokine expression, and disturbed hepatic glycometabolism.
In contrast to oral ingestion, one study evaluated the impact of inhalation exposure to PS-NPl on the development of non-alcoholic fatty liver disease in mothers and offspring [54]. Maternal exposure to high doses of PS-NPl during the gestational stage led to hepatic steatosis in adult female offspring but not in male offspring. Hepatic gene expression related to free fatty acid uptake and TG synthesis in the glycerol 3-phosphate pathway was elevated in female offspring. This study highlighted the potential health hazards associated with inhaled MPl and NPl.

Table 2.
The impact of prenatal NPl/MPl exposure on the liver and metabolism of mammalian offspring.
Table 2.
The impact of prenatal NPl/MPl exposure on the liver and metabolism of mammalian offspring.
| Material | Design | Size | Species/Stage | Effects | Ref. |
|---|---|---|---|---|---|
| PS | Prenatal oral ingestion | 0.5 μm NPl and 5 μm MPl |
|
| [41] |
| PS | Prenatal oral ingestion | 5 μm MPl |
|
| [53] |
| PS | Prenatal intra-tracheal ingestion | 0.02 μm NPl |
|
| [37] |
| PS | Prenatal and postpartum oral ingestion | 0.1 μm NPl |
|
| [44] |
| PS | Prenatal and postpartum oral ingestion | 5 μm MPl |
|
| [34] |
| PS | Prenatal inhalation | ≈0.07 μm NPl |
|
| [54] |
Abbreviation: G3P, glycerol 3-phosphate; MPl, microplastics; NPls, nanoplastics; PND, postnatal day; PS, polystyrene; ROS, reactive oxygen species; SD, Sprague Dawley.
3.3. The Effects of Prenatal NPl/MPl Exposure on the Intestines of Mammalian Offspring (Table 3)
Prenatal MPl-exposure-induced gut damage has been characterized. In an SD rat model, prenatal PS-MPl exposure decreased ileum length [53]. Additionally, another study revealed the occurrence of histological changes in the small intestine, increased reactive oxygen species (ROS), and decreased abundance of glutathione peroxidase 4 (GPx4), ferritin heavy chain 1 (FTH1), and ferritin light chain (FTL) proteins, indicating the initiation of ferroptosis [55].

Table 3.
The effects of prenatal NPl/MPl exposure on the intestines of mammalian offspring.
Table 3.
The effects of prenatal NPl/MPl exposure on the intestines of mammalian offspring.
| Material | Design | Size | Species/Stage | Effects | Ref. |
|---|---|---|---|---|---|
| PS | Prenatal oral ingestion | 0.08 μm NPl |
|
| [55] |
| PS | Prenatal oral ingestion | 5 μm MPl |
|
| [53] |
Abbreviation: FTL, ferritin light chain; FTH1, ferritin heavy chain 1; GPx4, glutathione peroxidase 4; MPl, microplastics; NPl, nanoplastics; PND, postnatal day; PS, polystyrene; ROS, reactive oxygen species; SD, Sprague Dawley.
3.4. The Effects of Prenatal NPl/MPl Exposure on the Reproductive System of Mammalian Offspring (Table 4)
There have been many studies and reviews on the reproductive toxicity of NPl/MPl in mammals, revealing that NPl/MPl [56,57,58] can induce reproductive toxicity through various mechanisms. However, most of these studies have been conducted using adult rodents, with less exploration of the effects during early developmental stages. Upon exploring the toxic effects of pre- and postnatal exposure to NPl on testicular development and reproductive function, one study reported that exposure to 0.5 μm PS-NPl pre- and postnatally leads to testicular dysplasia in offspring at day 35 (pre-puberty stage) and sperm production dysfunction at day 70 (sexual maturity stage) after birth [59]. Zhao et al. [59] administered drinking water containing varying concentrations (0.5, 5, and 50 mg/L) of PS-NPl to pregnant mice and their offspring from gestational day 1 to postnatal day (PND) 35 or PND 70. The authors found that exposure to 5 and 50 mg/L NPl delayed the onset of puberty in the offspring at PND 35. Transcriptome analysis of immature testes revealed the hormone-mediated signaling pathway, G1/S transition of the mitotic cell cycle, coregulation of androgen receptor activity, and the Hippo signaling pathway were involved upon exposure to PS-NPl [59]. In a study conducted by Huang et al. [44], pre- and postnatal PS-NPl exposure led to decreased testicular weight, seminiferous epithelium disruption, and decreased sperm count in mouse offspring. Testicular damage induced by prenatal and postnatal PS-NPl exposure was associated with oxidative injury [44].
Regarding the toxic effects of perinatal PE-MPl exposure on female reproduction in offspring, a recent study showed that perinatal (prenatal and lactation stage) PE-MPl exposure reduced oocyte maturation, fertilization rate, and embryo development in female offspring [60]. Despite the lack of a specific focus on prenatal exposure, these studies revealed that perinatal exposure to NPl/MPl could exert toxic effects on the reproductive systems of both males and females.
Recently, Dou et al. published an important study. The authors fed lactating female mice with PS-MPl at concentrations corresponding to those detected in baby formula prepared using plastic bottles [61]. The results led to reproductive toxicity in F0 female mice, manifested as delayed puberty, disturbed estrous cyclicity, decreased fertility, elevated testosterone levels, abnormal follicle development, and autoimmune ovarian inflammation. Notably, the experimental results showed that F1 male offspring exhibited decreased sperm count, reduced sperm motility, and altered testicular gene expression profiles. Furthermore, F2 male offspring also showed a pattern of reduced sperm count. These results indicate that male offspring are significantly more susceptible to intergenerational and transgenerational reproductive toxicity caused by maternal exposure to PS-MPl compared to female offspring.

Table 4.
The effects of prenatal NPl/MPl exposure on the reproductive system of mammalian offspring.
Table 4.
The effects of prenatal NPl/MPl exposure on the reproductive system of mammalian offspring.
| Material | Design | Size | Species/Stage | Effects | Ref. |
|---|---|---|---|---|---|
| PS | Prenatal and postpartum oral ingestion | 0.5 μm NPl |
|
| [59] |
| PS | Prenatal and postpartum oral ingestion | 0.1 μm NPl |
|
| [44] |
| PE | Prenatal and postpartum oral ingestion | 10–150 μm MPl |
|
| [60] |
| PS | F0 exposure at lactational stage | 1 μm MPl |
|
| [61] |
Abbreviation: MPl, microplastics; NPl, nanoplastics; PE, polyethylene; PND, postnatal day; PS, polystyrene.
3.5. The Effects of Prenatal NPl Exposure on the Skeletal Muscle System of Mammalian Offspring (Table 5)
The skeletal muscle is a metabolically active organ that communicates with other organs through the secretion of proteins to regulate energy metabolism. Chen et al. [45] investigated the effects of maternal PS-NPl exposure during pregnancy using transcriptomic and metabolomic analyses. Maternal PS-NPl exposure (0.1 μm; 10 mg/L) via drinking water led to substantial gene dysregulation in cholesterol and lipid metabolism, muscle tissue development, and skin formation in the muscle tissue. This study offers new insights into fetal effects in mice exposed to prenatal PS-NPl.

Table 5.
The impact of prenatal NPl/MPl exposure on the skeletal muscle of mammalian offspring.
Table 5.
The impact of prenatal NPl/MPl exposure on the skeletal muscle of mammalian offspring.
| Material | Design | Size | Species/Stage | Effects | Ref. |
|---|---|---|---|---|---|
| PS | Prenatal oral ingestion | 0.1 μm NPl |
|
| [45] |
Abbreviation: NPl, nanoplastics; PS, polystyrene.
3.6. Limitations and Future Research Directions
Based on the accumulated literature, five main types of MPl have been detected in the human body: general polyester (39%), polyamide (17%), polyurethane (15%), polypropylene (9%), polyacrylate (8%), and PS (2%) [62]. Among these materials, polystyrene (PS) is widely used in packaging, food storage, and textiles due to its excellent thermal stability and moldability [61]. It is also considered the most representative source of environmental emissions. Therefore, PS-NPls/MPls have often been selected as research materials to explore the potential toxicity of NPl/MPl in animals. In the past, nearly 80% of the research focused on the toxicological effects of single-sized PS spheres on animals [62]. These studies provide evidence regarding the effects of specific types and characteristics of NPls or MPls on animals. Nevertheless, studies on the toxicity of different microplastic polymer types in rodents remain limited. Therefore, additional investigations are needed to explore the impact of NPl/MPl combinations by simulating exposure in organisms as closely as possible to real-world environmental conditions. The generated evidence would facilitate the establishment of more reliable and thorough conclusions regarding their potential health risks.
Due to the challenges involved in detecting NPl/MPl exposure in humans, there are currently only a limited number of human studies that explore NPl/MPl in reproductive tissues and assess their correlation with fertility and pregnancy outcomes. A recent study demonstrated a negative correlation between the accumulation of MPl in the placenta and neonatal birth weight, length, head circumference, and 1 min APGAR scores [63]. Additionally, reports have suggested a negative correlation between the concentration of MPl found in amniotic fluid collected at delivery and gestational age, indicating that MPl exposure during pregnancy may lead to preterm birth [64]. However, these studies generally have small sample sizes, and data on the prevalence of NPl/MPl in humans and the placenta remain insufficient, highlighting the gaps in current research. Identifying prevention and management strategies based on research findings is another urgent priority.
4. Conclusions
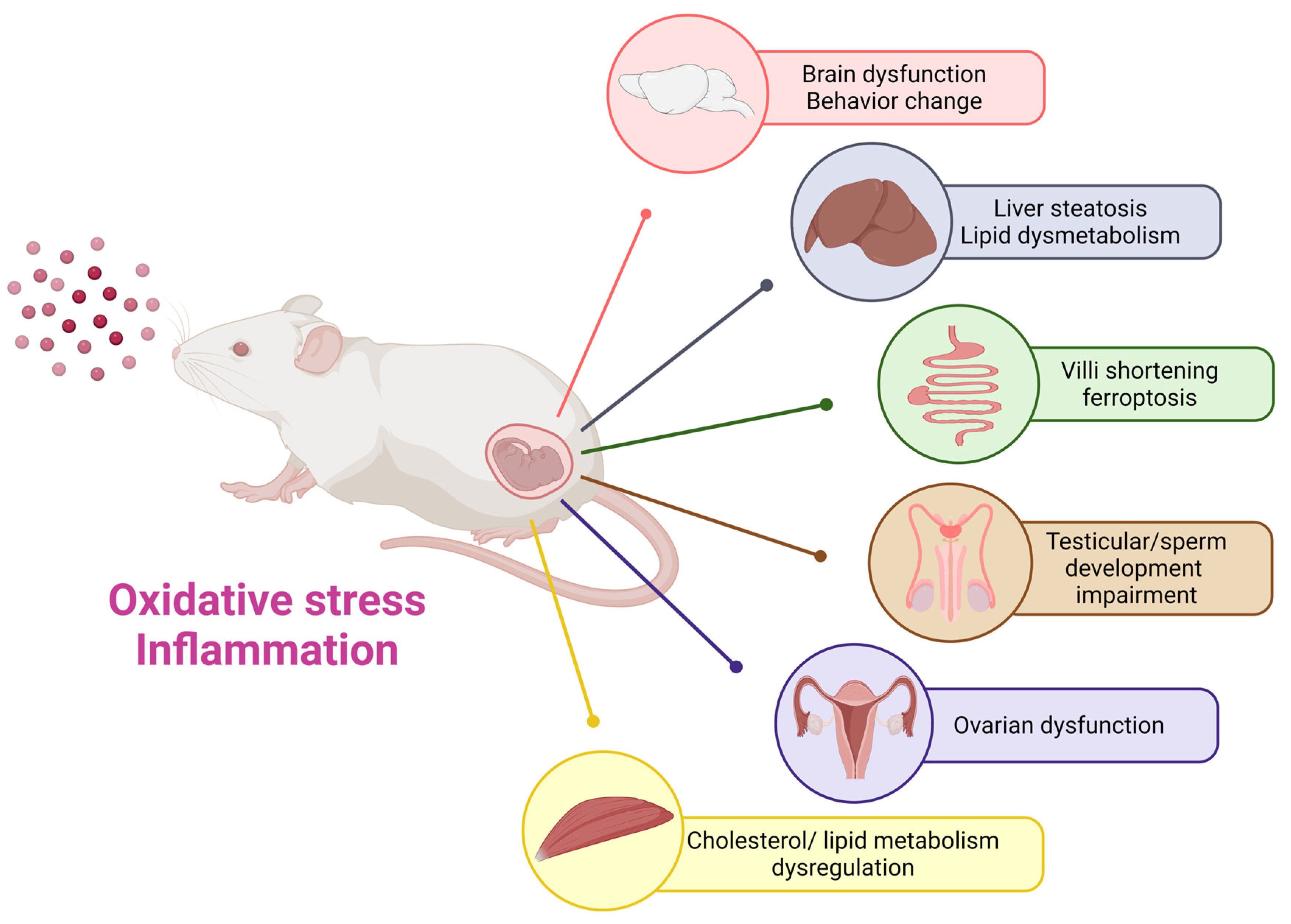
NPls/MPls have already invaded our lives and may impact the health of future generations. During the perinatal period, embryos and individual organs develop rapidly and become extremely sensitive. Existing research suggests that prenatal exposure to NPl/MPl can adversely affect the central nervous system, liver, intestine, reproductive system, and skeletal muscles of mammalian offspring through oxidative stress, inflammatory and other mechanisms (Figure 1). Previous research on prenatal NPl and MPl in mammals has predominantly focused on polystyrene materials. To more accurately represent the realities of the human environment, future studies should examine the effects of other prenatal microplastic materials on offspring. Moreover, it is crucial to delve deeper into the potential harms and mechanisms linked to prenatal NPl/MPl exposure in offspring. This research will aid in formulating effective prevention and treatment strategies moving forward.
Figure 1.
The impact of prenatal microplastic exposure on various organs of the offspring, including the brain, liver, intestine, reproductive system, and skeletal muscle. This diagram emphasizes the potential risks linked to maternal exposure to nanoplastics and microplastics, highlighting the necessity of further research to comprehensively clarify long-term effects on the health of offspring.
Author Contributions
Conceptualization, H.-R.Y., J.-M.S. and M.-M.T.; methodology, H.-R.Y., J.-M.S. and M.-M.T.; software, H.-R.Y.; validation, H.-R.Y., J.-M.S. and M.-M.T.; formal analysis, H.-R.Y., J.-M.S. and M.-M.T.; investigation, H.-R.Y., J.-M.S. and M.-M.T.; resources, M.-M.T.; data curation, H.-R.Y., J.-M.S. and M.-M.T.; writing—original draft preparation, H.-R.Y.; writing—review and editing, H.-R.Y. and M.-M.T.; visualization, H.-R.Y., J.-M.S. and M.-M.T.; supervision, H.-R.Y., J.-M.S. and M.-M.T.; project administration, H.-R.Y.; funding acquisition, H.-R.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This article was supported in part by grants CMRPG8L1541, CMRPG8L1542, CORPG8P0361, CORPG8P0381 (H.-R.Y.) from Chang Gung Memorial Hospital and NSTC 112-2314-B-182-029-MY3 (H.-R.Y.) from the National Science and Technology Council, Taiwan.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Maitlo, G.; Ali, I.; Maitlo, H.A.; Ali, S.; Unar, I.N.; Ahmad, M.B.; Bhutto, D.K.; Karmani, R.K.; Naich, S.u.R.; Sajjad, R.U.; et al. Plastic Waste Recycling, Applications, and Future Prospects for a Sustainable Environment. Sustainability 2022, 14, 11637. [Google Scholar] [CrossRef]
- Geyer, R.; Jambeck, J.R.; Law, K.L. Production, use, and fate of all plastics ever made. Sci. Adv. 2017, 3, e1700782. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, M.; Lebreton, L.C.; Carson, H.S.; Thiel, M.; Moore, C.J.; Borerro, J.C.; Galgani, F.; Ryan, P.G.; Reisser, J. Plastic Pollution in the World’s Oceans: More than 5 Trillion Plastic Pieces Weighing over 250,000 Tons Afloat at Sea. PLoS ONE 2014, 9, e111913. [Google Scholar] [CrossRef] [PubMed]
- Maddela, N.R.; Kakarla, D.; Venkateswarlu, K.; Megharaj, M. Additives of plastics: Entry into the environment and potential risks to human and ecological health. J. Environ. Manag. 2023, 348, 119364. [Google Scholar] [CrossRef] [PubMed]
- Dusaucy, J.; Gateuille, D.; Perrette, Y.; Naffrechoux, E. Microplastic pollution of worldwide lakes. Environ. Pollut. 2021, 284, 117075. [Google Scholar] [CrossRef]
- Khodabakhshloo, N.; Abbasi, S.; Turner, A. Resuspension of microplastics and microrubbers in a semi-arid urban environment (Shiraz, Iran). Environ. Pollut. 2023, 316, 120575. [Google Scholar] [CrossRef]
- Pironti, C.; Ricciardi, M.; Motta, O.; Miele, Y.; Proto, A.; Montano, L. Microplastics in the Environment: Intake through the Food Web, Human Exposure and Toxicological Effects. Toxics 2021, 9, 224. [Google Scholar] [CrossRef]
- Senathirajah, K.; Attwood, S.; Bhagwat, G.; Carbery, M.; Wilson, S.; Palanisami, T. Estimation of the mass of microplastics ingested—A pivotal first step towards human health risk assessment. J. Hazard. Mater. 2021, 404, 124004. [Google Scholar] [CrossRef]
- Cox, K.D.; Covernton, G.A.; Davies, H.L.; Dower, J.F.; Juanes, F.; Dudas, S.E. Human Consumption of Microplastics. Environ. Sci. Technol. 2019, 53, 7068–7074. [Google Scholar] [CrossRef]
- Kannan, K.; Vimalkumar, K. A Review of Human Exposure to Microplastics and Insights Into Microplastics as Obesogens. Front. Endocrinol. 2021, 12, 724989. [Google Scholar] [CrossRef]
- Peng, C.; He, N.; Wu, Y.; Lu, Y.; Sun, H.; Wang, L. Excretion characteristics of nylon microplastics and absorption risk of nanoplastics in rats. Ecotoxicol. Environ. Saf. 2022, 238, 113586. [Google Scholar] [CrossRef] [PubMed]
- Mattsson, K.; Johnson, E.V.; Malmendal, A.; Linse, S.; Hansson, L.A.; Cedervall, T. Brain damage and behavioural disorders in fish induced by plastic nanoparticles delivered through the food chain. Sci. Rep. 2017, 7, 11452. [Google Scholar] [CrossRef]
- Geiss, O.; El Hadri, H.; Giechaskiel, B.; al Wasif Ruiz, T.; Putaud, J.-P.; Barrero, J. Micro- and Nanoplastics in the Air: Sources, Transport & Analytical Methods for Their Determination; Publications Office of the European Union: Luxembourg, 2024. [Google Scholar]
- Campanale, C.; Massarelli, C.; Savino, I.; Locaputo, V.; Uricchio, V.F. A Detailed Review Study on Potential Effects of Microplastics and Additives of Concern on Human Health. Int. J. Environ. Res. Public Health 2020, 17, 1212. [Google Scholar] [CrossRef]
- Abbasi, S.; Turner, A. Human exposure to microplastics: A study in Iran. J. Hazard. Mater. 2021, 403, 123799. [Google Scholar] [CrossRef] [PubMed]
- Ragusa, A.; Notarstefano, V.; Svelato, A.; Belloni, A.; Gioacchini, G.; Blondeel, C.; Zucchelli, E.; De Luca, C.; D’Avino, S.; Gulotta, A.; et al. Raman Microspectroscopy Detection and Characterisation of Microplastics in Human Breastmilk. Polymers 2022, 14, 2700. [Google Scholar] [CrossRef] [PubMed]
- Jenner, L.C.; Rotchell, J.M.; Bennett, R.T.; Cowen, M.; Tentzeris, V.; Sadofsky, L.R. Detection of microplastics in human lung tissue using muFTIR spectroscopy. Sci. Total Environ. 2022, 831, 154907. [Google Scholar] [CrossRef]
- Amato-Lourenco, L.F.; Carvalho-Oliveira, R.; Junior, G.R.; Dos Santos Galvao, L.; Ando, R.A.; Mauad, T. Presence of airborne microplastics in human lung tissue. J. Hazard. Mater. 2021, 416, 126124. [Google Scholar] [CrossRef]
- Horvatits, T.; Tamminga, M.; Liu, B.; Sebode, M.; Carambia, A.; Fischer, L.; Puschel, K.; Huber, S.; Fischer, E.K. Microplastics detected in cirrhotic liver tissue. eBioMedicine 2022, 82, 104147. [Google Scholar] [CrossRef]
- Exacoustos, O.; Artini, C.; Massardo, S.; Caboni, C.; Pastorino, A.; Chiarenza, S.; Zaza, G.; Stallone, G.; Ghiggeri, G.M.; Angeletti, A.; et al. #6111 First identification and characterization of microplastics in human kidney and urine. Nephrol. Dial. Transplant. 2023, 38, gfad063a_6111. [Google Scholar] [CrossRef]
- Ibrahim, Y.S.; Tuan Anuar, S.; Azmi, A.A.; Wan Mohd Khalik, W.M.A.; Lehata, S.; Hamzah, S.R.; Ismail, D.; Ma, Z.F.; Dzulkarnaen, A.; Zakaria, Z.; et al. Detection of microplastics in human colectomy specimens. JGH Open Open Access J. Gastroenterol. Hepatol. 2021, 5, 116–121. [Google Scholar] [CrossRef]
- Rotchell, J.M.; Jenner, L.C.; Chapman, E.; Bennett, R.T.; Bolanle, I.O.; Loubani, M.; Sadofsky, L.; Palmer, T.M. Detection of microplastics in human saphenous vein tissue using muFTIR: A pilot study. PLoS ONE 2023, 18, e0280594. [Google Scholar] [CrossRef]
- Kutralam-Muniasamy, G.; Shruti, V.C.; Perez-Guevara, F.; Roy, P.D. Microplastic diagnostics in humans: “The 3Ps” Progress, problems, and prospects. Sci. Total Environ. 2023, 856, 159164. [Google Scholar] [CrossRef]
- Schell, T.; Rico, A.; Vighi, M. Occurrence, Fate and Fluxes of Plastics and Microplastics in Terrestrial and Freshwater Ecosystems. Rev. Environ. Contam. Toxicol. 2020, 250, 1–43. [Google Scholar] [CrossRef] [PubMed]
- Schirinzi, G.F.; Perez-Pomeda, I.; Sanchis, J.; Rossini, C.; Farre, M.; Barcelo, D. Cytotoxic effects of commonly used nanomaterials and microplastics on cerebral and epithelial human cells. Environ. Res. 2017, 159, 579–587. [Google Scholar] [CrossRef]
- Wu, B.; Wu, X.; Liu, S.; Wang, Z.; Chen, L. Size-dependent effects of polystyrene microplastics on cytotoxicity and efflux pump inhibition in human Caco-2 cells. Chemosphere 2019, 221, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Ruenraroengsak, P.; Tetley, T.D. Differential bioreactivity of neutral, cationic and anionic polystyrene nanoparticles with cells from the human alveolar compartment: Robust response of alveolar type 1 epithelial cells. Part. Fibre Toxicol. 2015, 12, 19. [Google Scholar] [CrossRef]
- Meindl, C.; Kueznik, T.; Bösch, M.; Roblegg, E.; Fröhlich, E. Intracellular calcium levels as screening tool for nanoparticle toxicity. J. Appl. Toxicol. 2015, 35, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Poma, A.; Vecchiotti, G.; Colafarina, S.; Zarivi, O.; Aloisi, M.; Arrizza, L.; Chichiriccò, G.; Di Carlo, P. In vitro genotoxicity of polystyrene nanoparticles on the human fibroblast Hs27 cell line. Nanomaterials 2019, 9, 1299. [Google Scholar] [CrossRef]
- Ferraro, D.; Anselmi-Tamburini, U.; Tredici, I.G.; Ricci, V.; Sommi, P. Overestimation of nanoparticles-induced DNA damage determined by the comet assay. Nanotoxicology 2016, 10, 861–870. [Google Scholar] [CrossRef]
- Deng, Y.; Zhang, Y.; Lemos, B.; Ren, H. Tissue accumulation of microplastics in mice and biomarker responses suggest widespread health risks of exposure. Sci. Rep. 2017, 7, 46687. [Google Scholar] [CrossRef]
- Stock, V.; Bohmert, L.; Lisicki, E.; Block, R.; Cara-Carmona, J.; Pack, L.K.; Selb, R.; Lichtenstein, D.; Voss, L.; Henderson, C.J.; et al. Uptake and effects of orally ingested polystyrene microplastic particles in vitro and in vivo. Arch. Toxicol. 2019, 93, 1817–1833. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Wan, Z.; Luo, T.; Fu, Z.; Jin, Y. Polystyrene microplastics induce gut microbiota dysbiosis and hepatic lipid metabolism disorder in mice. Sci. Total Environ. 2018, 631–632, 449–458. [Google Scholar] [CrossRef]
- Luo, T.; Wang, C.; Pan, Z.; Jin, C.; Fu, Z.; Jin, Y. Maternal Polystyrene Microplastic Exposure during Gestation and Lactation Altered Metabolic Homeostasis in the Dams and Their F1 and F2 Offspring. Environ. Sci. Technol. 2019, 53, 10978–10992. [Google Scholar] [CrossRef] [PubMed]
- Amato-Lourenco, L.F.; Dos Santos Galvao, L.; de Weger, L.A.; Hiemstra, P.S.; Vijver, M.G.; Mauad, T. An emerging class of air pollutants: Potential effects of microplastics to respiratory human health? Sci. Total Environ. 2020, 749, 141676. [Google Scholar] [CrossRef]
- Wright, S.L.; Kelly, F.J. Plastic and Human Health: A Micro Issue? Environ. Sci. Technol. 2017, 51, 6634–6647. [Google Scholar] [CrossRef]
- Fournier, S.B.; D’Errico, J.N.; Adler, D.S.; Kollontzi, S.; Goedken, M.J.; Fabris, L.; Yurkow, E.J.; Stapleton, P.A. Nanopolystyrene translocation and fetal deposition after acute lung exposure during late-stage pregnancy. Part. Fibre Toxicol. 2020, 17, 55. [Google Scholar] [CrossRef]
- Jeong, B.; Baek, J.Y.; Koo, J.; Park, S.; Ryu, Y.K.; Kim, K.S.; Zhang, S.; Chung, C.; Dogan, R.; Choi, H.S.; et al. Maternal exposure to polystyrene nanoplastics causes brain abnormalities in progeny. J. Hazard. Mater. 2022, 426, 127815. [Google Scholar] [CrossRef]
- Wick, P.; Malek, A.; Manser, P.; Meili, D.; Maeder-Althaus, X.; Diener, L.; Diener, P.A.; Zisch, A.; Krug, H.F.; von Mandach, U. Barrier capacity of human placenta for nanosized materials. Environ. Health Perspect. 2010, 118, 432–436. [Google Scholar] [CrossRef]
- Ragusa, A.; Svelato, A.; Santacroce, C.; Catalano, P.; Notarstefano, V.; Carnevali, O.; Papa, F.; Rongioletti, M.C.A.; Baiocco, F.; Draghi, S.; et al. Plasticenta: First evidence of microplastics in human placenta. Environ. Int. 2021, 146, 106274. [Google Scholar] [CrossRef]
- Luo, T.; Zhang, Y.; Wang, C.; Wang, X.; Zhou, J.; Shen, M.; Zhao, Y.; Fu, Z.; Jin, Y. Maternal exposure to different sizes of polystyrene microplastics during gestation causes metabolic disorders in their offspring. Environ. Pollut. 2019, 255, 113122. [Google Scholar] [CrossRef] [PubMed]
- Mandy, M.; Nyirenda, M. Developmental Origins of Health and Disease: The relevance to developing nations. Int. Health 2018, 10, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Park, E.J.; Han, J.S.; Park, E.J.; Seong, E.; Lee, G.H.; Kim, D.W.; Son, H.Y.; Han, H.Y.; Lee, B.S. Repeated-oral dose toxicity of polyethylene microplastics and the possible implications on reproduction and development of the next generation. Toxicol. Lett. 2020, 324, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Zhang, W.; Lin, T.; Liu, S.; Sun, Z.; Liu, F.; Yuan, Y.; Xiang, X.; Kuang, H.; Yang, B.; et al. Maternal exposure to polystyrene nanoplastics during gestation and lactation induces hepatic and testicular toxicity in male mouse offspring. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2022, 160, 112803. [Google Scholar] [CrossRef]
- Chen, G.; Xiong, S.; Jing, Q.; van Gestel, C.A.M.; van Straalen, N.M.; Roelofs, D.; Sun, L.; Qiu, H. Maternal exposure to polystyrene nanoparticles retarded fetal growth and triggered metabolic disorders of placenta and fetus in mice. Sci. Total Environ. 2023, 854, 158666. [Google Scholar] [CrossRef]
- Lee, C.W.; Hsu, L.F.; Wu, I.L.; Wang, Y.L.; Chen, W.C.; Liu, Y.J.; Yang, L.T.; Tan, C.L.; Luo, Y.H.; Wang, C.C.; et al. Exposure to polystyrene microplastics impairs hippocampus-dependent learning and memory in mice. J. Hazard. Mater. 2022, 430, 128431. [Google Scholar] [CrossRef]
- Ferrante, M.C.; Monnolo, A.; Del Piano, F.; Mattace Raso, G.; Meli, R. The Pressing Issue of Micro- and Nanoplastic Contamination: Profiling the Reproductive Alterations Mediated by Oxidative Stress. Antioxidants 2022, 11, 193. [Google Scholar] [CrossRef]
- Shin, H.S.; Lee, S.H.; Moon, H.J.; So, Y.H.; Lee, H.R.; Lee, E.H.; Jung, E.M. Exposure to polystyrene particles causes anxiety-, depression-like behavior and abnormal social behavior in mice. J. Hazard. Mater. 2023, 454, 131465. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Zhu, J.; Zhou, X.; Pan, D.; Nan, S.; Yin, R.; Lei, Q.; Ma, N.; Zhu, H.; Chen, J.; et al. Polystyrene micro- and nano-particle coexposure injures fetal thalamus by inducing ROS-mediated cell apoptosis. Environ. Int. 2022, 166, 107362. [Google Scholar] [CrossRef]
- Zaheer, J.; Kim, H.; Ko, I.O.; Jo, E.K.; Choi, E.J.; Lee, H.J.; Shim, I.; Woo, H.J.; Choi, J.; Kim, G.H.; et al. Pre/post-natal exposure to microplastic as a potential risk factor for autism spectrum disorder. Environ. Int. 2022, 161, 107121. [Google Scholar] [CrossRef]
- Tian, L.; Zhang, Y.; Chen, J.; Liu, X.; Nie, H.; Li, K.; Liu, H.; Lai, W.; Shi, Y.; Xi, Z.; et al. Effects of nanoplastic exposure during pregnancy and lactation on neurodevelopment of rat offspring. J. Hazard. Mater. 2024, 474, 134800. [Google Scholar] [CrossRef]
- Xiong, S.; He, J.; Qiu, H.; van Gestel, C.A.M.; He, E.; Qiao, Z.; Cao, L.; Li, J.; Chen, G. Maternal exposure to polystyrene nanoplastics causes defective retinal development and function in progeny mice by disturbing metabolic profiles. Chemosphere 2024, 352, 141513. [Google Scholar] [CrossRef] [PubMed]
- Tiao, M.M.; Sheen, J.M.; Lin, I.C.; Khwepeya, M.; Yu, H.R. Prenatal High-Fat Diet Combined with Microplastic Exposure Induces Liver Injury via Oxidative Stress in Male Pups. Int. J. Mol. Sci. 2023, 24, 13457. [Google Scholar] [CrossRef]
- Wang, X.; Zhao, Z.; Wang, X.; Hu, W.; Chao, L.; Chu, X.; Qian, M.; Wang, R.; Yu, S.; Wu, Q.; et al. Effects of polystyrene nanoplastic gestational exposure on mice. Chemosphere 2023, 324, 138255. [Google Scholar] [CrossRef]
- Tang, J.; Bu, W.; Hu, W.; Zhao, Z.; Liu, L.; Luo, C.; Wang, R.; Fan, S.; Yu, S.; Wu, Q.; et al. Ferroptosis Is Involved in Sex-Specific Small Intestinal Toxicity in the Offspring of Adult Mice Exposed to Polystyrene Nanoplastics during Pregnancy. ACS Nano 2023, 17, 2440–2449. [Google Scholar] [CrossRef]
- Peng, Y.; He, Q. Reproductive toxicity and related mechanisms of micro(nano)plastics in terrestrial mammals: Review of current evidence. Ecotoxicol. Environ. Saf. 2024, 279, 116505. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wu, Y.; Li, G.; Xiong, Y.; Zhang, Y.; Zhang, M. The hidden threat: Unraveling the impact of microplastics on reproductive health. Sci. Total Environ. 2024, 935, 173177. [Google Scholar] [CrossRef]
- He, Y.; Yin, R. The reproductive and transgenerational toxicity of microplastics and nanoplastics: A threat to mammalian fertility in both sexes. J. Appl. Toxicol. JAT 2024, 44, 66–85. [Google Scholar] [CrossRef]
- Zhao, T.; Shen, L.; Ye, X.; Bai, G.; Liao, C.; Chen, Z.; Peng, T.; Li, X.; Kang, X.; An, G. Prenatal and postnatal exposure to polystyrene microplastics induces testis developmental disorder and affects male fertility in mice. J. Hazard. Mater. 2023, 445, 130544. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, X.; Zhao, Y.; Zhao, J.; Yu, T.; Yao, Y.; Zhao, R.; Yu, R.; Liu, J.; Su, J. Reproductive toxicity of microplastics in female mice and their offspring from induction of oxidative stress. Environ. Pollut. 2023, 327, 121482. [Google Scholar] [CrossRef]
- Dou, Y.; Zhang, M.; Zhang, H.; Zhang, C.; Feng, L.; Hu, J.; Gao, Y.; Yuan, X.Z.; Zhao, Y.; Zhao, H.; et al. Lactating exposure to microplastics at the dose of infants ingested during artificial feeding induced reproductive toxicity in female mice and their offspring. Sci. Total Environ. 2024, 949, 174972. [Google Scholar] [CrossRef]
- Vdovchenko, A.; Resmini, M. Mapping Microplastics in Humans: Analysis of Polymer Types, and Shapes in Food and Drinking Water-A Systematic Review. Int. J. Mol. Sci. 2024, 25, 7074. [Google Scholar] [CrossRef] [PubMed]
- Amereh, F.; Amjadi, N.; Mohseni-Bandpei, A.; Isazadeh, S.; Mehrabi, Y.; Eslami, A.; Naeiji, Z.; Rafiee, M. Placental plastics in young women from general population correlate with reduced foetal growth in IUGR pregnancies. Environ. Pollut. 2022, 314, 120174. [Google Scholar] [CrossRef] [PubMed]
- Xue, J.; Xu, Z.; Hu, X.; Lu, Y.; Zhao, Y.; Zhang, H. Microplastics in maternal amniotic fluid and their associations with gestational age. Sci. Total Environ. 2024, 920, 171044. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).