Evaluation of a Four-Gene Panel for Hereditary Cancer Risk Assessment
Abstract
:1. Introduction
2. Materials and Methods
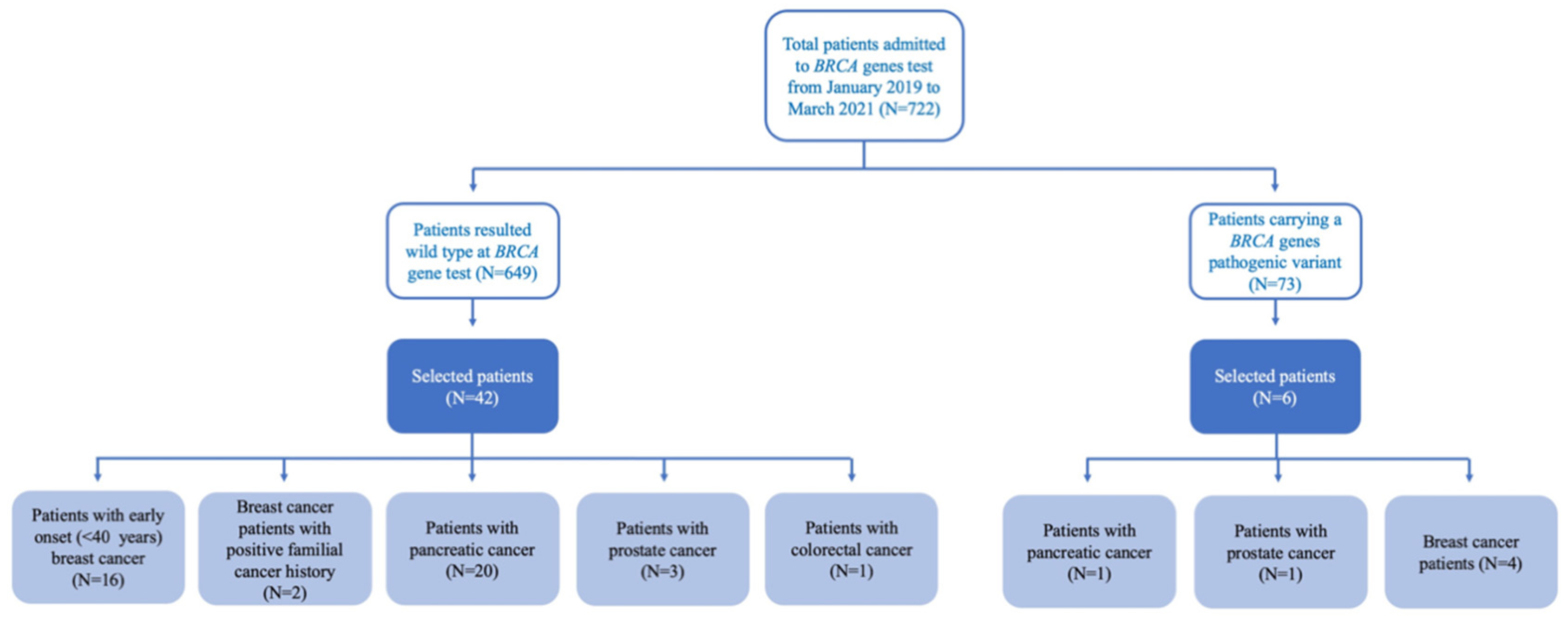
2.1. Patient Selection and DNA Sample Collection
2.2. DNA Library Preparation and Next-Generation Sequencing
2.3. Sequence Data Analysis
2.4. Variant Validation
3. Results
3.1. Assessment of Method Reliability in Variant Calling
3.2. Evaluation of Additional Variants Identified by the Tested Procedure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Narod, S.A. Breast cancer in young women. Nat. Rev. Clin. Oncol. 2012, 9, 460–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lord, C.J.; Ashworth, A. BRCAness revisited. Nat. Rev. Cancer 2016, 16, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Hawsawi, Y.M.; Al-Numair, N.S.; Sobahy, T.M.; Al-Ajmi, A.M.; Al-Harbi, R.M.; Baghdadi, M.A.; Oyouni, A.A.; Alamer, O.M. The role of BRCA1/2 in hereditary and familial breast and ovarian cancers. Mol. Genet. Genom. Med. 2019, 7, e879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weitzel, J.N.; Blazer, K.R.; MacDonald, D.J.; Culver, J.O.; Offit, K. Genetics, genomics, and cancer risk assessment: State of the Art and Future Directions in the Era of Personalized Medicine. CA Cancer J. Clin. 2011, 61, 327–359. [Google Scholar] [CrossRef] [PubMed]
- Roy, R.; Chun, J.; Powell, S.N. BRCA1 and BRCA2: Different roles in a common pathway of genome protection. Nat. Rev. Cancer 2011, 12, 68–78. [Google Scholar] [CrossRef] [Green Version]
- Hoogerbrugge, N.; Jongmans, M.C. Finding all BRCA pathogenic mutation carriers: Best practice models. Eur. J. Hum. Genet. 2016, 24, S19–S26. [Google Scholar] [CrossRef]
- Nelson, H.D.; Pappas, M.; Cantor, A.; Haney, E.; Holmes, R. Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA- Related Cancer in Women: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2019, 322, 666–685. [Google Scholar] [CrossRef] [Green Version]
- Metcalfe, K.A.; Kim-Sing, C.; Ghadirian, P.; Sun, P.; Narod, S.A. Health care provider recommendations for reducing cancer risks among women with a BRCA1 or BRCA2 mutation. Clin. Genet. 2014, 85, 21–30. [Google Scholar] [CrossRef]
- Wang, Q. Cancer predisposition genes: Molecular mechanisms and clinical impact on personalized cancer care: Examples of Lynch and HBOC syndromes. Acta Pharm. Sin. 2016, 37, 143–149. [Google Scholar] [CrossRef] [Green Version]
- Daly, M.B.; Axilbund, J.E.; Buys, S.; Crawford, B.; Farrell, C.D.; Friedman, S.; Garber, J.E.; Goorha, S.; Gruber, S.B.; Hampel, H.; et al. National Comprehensive Cancer Network. Genetic/familial high-risk assessment: Breast and ovarian. J. Natl. Compr. Cancer Netw. 2010, 8, 562–594. [Google Scholar] [CrossRef]
- Rajagopal, P.S.; Nielsen, S.; Olopade, O.I. USPSTF Recommendations for BRCA1 and BRCA2 Testing in the Context of a Transformative National Cancer Control Plan. JAMA Netw. Open 2019, 2, e1910142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daly, M.B.; Pilarski, R.; Yurgelun, M.B.; Berry, M.P.; Buys, S.S.; Dickson, P.; Domchek, S.M.; Elkhanany, A.; Friedman, S.; Garber, J.E.; et al. NCCN Guidelines Insights: Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic, Version 1.2020. J. Natl. Compr. Cancer Netw. 2020, 18, 380–391. [Google Scholar] [CrossRef] [PubMed]
- Guo, F.; Scholl, M.; Fuchs, E.L.; Berenson, A.B.; Kuo, Y.F. BRCA testing and testing results among women 18–65 years old. Prev. Med. Rep. 2022, 26, 101738. [Google Scholar] [CrossRef] [PubMed]
- Cortesi, L.; Rugo, H.S.; Jackisch, C. An Overview of PARP Inhibitors for the Treatment of Breast Cancer. Target. Oncol. 2021, 16, 255–282. [Google Scholar] [CrossRef]
- Lau, K.H.; Tan, A.M.; Shi, Y. New and Emerging Targeted Therapies for Advanced Breast Cancer. Int. J. Mol. Sci. 2022, 23, 2288. [Google Scholar] [CrossRef]
- Metcalfe, K.A.; Finch, A.; Poll, A.; Horsman, D.; Kim-Sing, C.; Scott, J.; Royer, R.; Sun, P.; Narod, S.A. Breast cancer risks in women with a family history of breast or ovarian cancer who have tested negative for a BRCA1 or BRCA2 mutation. Br. J. Cancer 2009, 100, 421–425. [Google Scholar] [CrossRef]
- Kotsopoulos, J.; Metcalfe, K.; Alston, J.; Nikitina, D.; Ginsburg, O.; Eisen, A.; Demsky, R.; Akbari, M.; Zbuk, K.; Narod, S.A. Prospective study of high-risk, BRCA1/2-mutation negative women: The ‘negative study’. BMC Cancer 2014, 14, 221. [Google Scholar] [CrossRef] [Green Version]
- Doddato, G.; Valentino, F.; Giliberti, A.; Papa, F.T.; Tita, R.; Bruno, L.P.; Resciniti, S.; Fallerini, C.; Benetti, E.; Palmieri, M.; et al. Corrigendum: Exome Sequencing in BRCA1-2 Candidate Familias: The Contribution of Other Cancer Susceptibility Genes. Front. Oncol. 2021, 11, 740860. [Google Scholar]
- Cortesi, L.; Piombino, C.; Toss, A. Germline Mutations in Other Homologous Recombination Repair-Related Genes Than BRCA1/2: Predictive or Prognostic Factors? J. Pers. Med. 2021, 11, 245. [Google Scholar] [CrossRef]
- Limongelli, G.; Nunziato, M.; D’Argenio, V.; Esposito, M.V.; Monda, E.; Mazzaccara, C.; Caiazza, M.; D’Aponte, A.; D’Andrea, A.; Bossone, E.; et al. Yield and clinical significance of genetic screening in elite and amateur athletes. Eur. J. Prev. Cardiol. 2021, 28, 1081–1090. [Google Scholar] [CrossRef]
- D’Argenio, V.; Cariati, F.; Tomaiuolo, R. One4Two®: An Integrated Molecular Approach to Optimize Infertile Couples’ Journey. Genes 2021, 12, 60. [Google Scholar] [CrossRef] [PubMed]
- D’Argenio, V.; Esposito, M.V.; Telese, A.; Precone, V.; Starnone, F.; Nunziato, M.; Cantiello, P.; Iorio, M.; Evangelista, E.; D’Aiuto, M.; et al. The molecular analysis of BRCA1 and BRCA2: Next-generation sequencing supersedes conventional approaches. Clin. Chim. Acta 2015, 446, 221–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Concolino, P.; Gelli, G.; Rizza, R.; Costella, A.; Scambia, G.; Capoluongo, E. BRCA1 and BRCA2 testing through next generation sequencing in a small cohort of italian breast/ovarian cancer patients: Novel pathogenic and unknown clinical significance variants. Int. J. Mol. Sci. 2019, 20, 3442. [Google Scholar] [CrossRef] [Green Version]
- Buys, S.S.; Sandbach, J.F.; Gammon, A.; Patel, G.; Kidd, J.; Brown, K.L.; Sharma, L.; Saam, J.; Lancaster, J.; Daly, M.B. A study of over 35,000 women with breast cancer tested with a 25-gene panel of hereditary cancer genes. Cancer 2017, 123, 1721–1730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nunziato, M.; Esposito, M.V.; Starnone, F.; Diroma, M.A.; Calabrese, A.; Del Monaco, V.; Buono, P.; Frasci, G.; Botti, G.; D’Aiuto, M.; et al. A multi-gene panel beyond BRCA1/BRCA2 to identify new breast cancer-predisposing mutations by a picodroplet PCR followed by a next-generation sequencing strategy: A pilot study. Anal. Chim. Acta 2019, 1046, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Catana, A.; Apostu, A.P.; Antemie, R.G. Multi gene panel testing for hereditary breast cancer–is it ready to be used? Med. Pharm. Rep. 2019, 92, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, S.D.C.E.S.; Cury, N.M.; Brotto, D.B.; De Araujo, L.F.; Rosa, R.C.A.; Texeira, L.A.; Plaça, J.R.; Marques, A.A.; Peronni, K.C.; Ruy, P.D.C.; et al. Germline variants in DNA repair genes associated with hereditary breast and ovarian cancer syndrome: Analysis of a 21 gene panel in the Brazilian population. BMC Med. Genom. 2020, 13, 21. [Google Scholar]
- Shin, H.C.; Lee, H.B.; Yoo, T.K.; Lee, E.S.; Kim, R.N.; Park, B.; Yoon, K.A.; Park, C.; Lee, E.S.; Moon, H.G.; et al. Detection of Germline Mutations in Breast Cancer Patients with Clinical Features of Hereditary Cancer Syndrome Using a Multi-Gene Panel Test. Cancer Res. Treat. 2020, 52, 697–713. [Google Scholar] [CrossRef] [Green Version]
- D’Argenio, V. The High-Throughput Analyses Era: Are We Ready for the Data Struggle? High. Throughput 2018, 7, 8. [Google Scholar] [CrossRef] [Green Version]
- Wallace, A.J. New challenges for BRCA testing: A view from the diagnostic laboratory. Eur. J. Hum. Genet. 2016, 24, S10–S18. [Google Scholar] [CrossRef] [Green Version]
- Desmond, A.; Kurian, A.W.; Gabree, M.; Mills, M.A.; Anderson, M.J.; Kobayashi, Y.; Horick, N.; Yang, S.; Shannon, K.M.; Tung, N.; et al. Clinical Actionability of Multigene Panel Testing for Hereditary Breast and Ovarian Cancer Risk Assessment. JAMA Oncol. 2015, 1, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, S.; Ballif, B.A.; Smogorzewska, A.; McDonald, E.R., 3rd; Hurov, K.E.; Luo, J.; Bakalarski, C.E.; Zhao, Z.; Solimini, N.; Lerenthal, Y.; et al. ATM and ATR substrate analysis reveals extensive protein networks responsive to DNA damage. Science 2007, 316, 1160–1166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cybulski, C.; Wokołorczyk, D.; Jakubowska, A.; Huzarski, T.; Byrski, T.; Gronwald, J.; Masojć, B.; Deebniak, T.; Górski, B.; Blecharz, P.; et al. Risk of breast cancer in women with a CHEK2 mutation with and without a family history of breast cancer. J. Clin. Oncol. 2011, 29, 3747–3752. [Google Scholar] [CrossRef] [PubMed]
- Ducy, M.; Sesma-Sanz, L.; Guitton-Sert, L.; Lashgari, A.; Gao, Y.; Brahiti, N.; Rodrigue, A.; Margaillan, G.; Caron, M.C.; Côté, J.; et al. The Tumor Suppressor PALB2: Inside Out. Trends Biochem. Sci. 2019, 44, 226–240. [Google Scholar] [CrossRef]
- Yang, X.; Leslie, G.; Doroszuk, A.; Schneider, S.; Allen, J.; Decker, B.; Dunning, A.M.; Redman, J.; Scarth, J.; Plaskocinska, I.; et al. Cancer Risks Associated With Germline PALB2 Pathogenic Variants: An International Study of 524 Families. J. Clin. Oncol. 2020, 38, 674–685. [Google Scholar] [CrossRef]
- Crocetto, F.; Barone, B.; Caputo, V.F.; Fontana, M.; de Cobelli, O.; Ferro, M. BRCA Germline Mutations in Prostate Cancer: The Future Is Tailored. Diagnostics 2021, 11, 908. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Lu, L.; Resurreccion, W.K.; Yang, W.; Wei, J.; Wang, Q.; Engelmann, V.; Zheng, S.L.; Cooney, K.A.; Isaacs, W.B.; et al. Association of germline rare pathogenic mutations in guideline-recommended genes with prostate cancer progression: A meta-analysis. Prostate 2022, 82, 107–119. [Google Scholar] [CrossRef]
- Macchini, M.; Centonze, F.; Peretti, U.; Orsi, G.; Militello, A.M.; Valente, M.M.; Cascinu, S.; Reni, M. Epidemiology and geographic distribution of BRCA1-2 and DNA Damage response genes pathogenic variants in pancreatic ductal adenocarcinoma patients. Cancer Treat. Rev. 2022, 104, 102357. [Google Scholar] [CrossRef]
- Martin, A.P.; Pedra, G.; Downing, J.; Collins, B.; Godman, B.; Alfirevic, A.; Pirmohamed, M.; Lynn Greenhalgh, K. Trends in BRCA testing and socioeconomic deprivation. Eur. J. Hum. Genet. 2019, 27, 1351–1360. [Google Scholar] [CrossRef] [Green Version]
- Nunziato, M.; Starnone, F.; Lombardo, B.; Pensabene, M.; Condello, C.; Verdesca, F.; Carlomagno, C.; De Placido, S.; Pastore, L.; Salvatore, F.; et al. Fast Detection of a BRCA2 Large Genomic Duplication by Next Generation Sequencing as a Single Procedure: A Case Report. Int. J. Mol. Sci. 2017, 18, 2487. [Google Scholar] [CrossRef] [Green Version]
| Gene | Single-Nucleotide Variants and Ins/del | Copy Number Variants | Total |
|---|---|---|---|
| BRCA1 | 138 | 3 | 141 |
| BRCA2 | 85 | 1 | 86 |
| CHEK2 | 0 | 1 | 1 |
| PALB2 | 26 | 0 | 26 |
| Total | 249 | 5 | 254 |
| Sample ID | Gender | Age at Diagnosis (y) | Kind of Cancer | Gene | Cdna * | Protein * | Reference SNP ID | Status | Clinvar Classification |
|---|---|---|---|---|---|---|---|---|---|
| P1 | M | 60 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.2596C > T | p.(Arg866Cys) | rs41286300 | Het | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| c.1067A > G | p.(Gln356Arg) | rs1799950 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| PALB2 | c.2993G > A | p.(Gly998Glu) | rs45551636 | Het | Benign | ||||
| c.2014G > C | p.(Glu672Gln) | rs45532440 | Het | Benign | |||||
| c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | |||||
| P2 | M | 42 | Pancreas | BRCA1 | c.3119G > A | p.(Ser1040Asn) | rs4986852 | Het | Benign |
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P3 | M | 66 | Pancreas | BRCA2 | c.3055C > G | p.(Leu1019Val) | rs55638633 | Het | Benign |
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | ||||
| P4 | M | 69 | Pancreas | BRCA2 | c.67+1G > A | p.(?) | rs81002796 | Het | Pathogenic |
| c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.2993G > A | p.(Gly998Glu) | rs45551636 | Het | Benign | ||||
| c.2014G > C | p.(Glu672Gln) | rs45532440 | Het | Benign | |||||
| c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | |||||
| P5 | M | 81 | Colorectal | BRCA1 | c.1067A > G | p.(Gln356Arg) | rs1799950 | Hom | Benign |
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P6 | M | 45 | Prostate | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P7 | M | 65 | Prostate | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3119G > A | p.(Ser1040Asn) | rs4986852 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| c.7940T > C | p.(Leu2647Pro) | rs80359021 | Het | Pathogenic | |||||
| P8 | F | 76 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.1151C > T | p.(Ser384Phe) | rs41293475 | Hom | Benign | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P9 | M | 71 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Hom | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Hom | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Hom | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Hom | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | ||||
| P10 | M | 71 | Prostate | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P11 | M | 70 | Pancreas | BRCA1 | c.4054G > A | p.(Glu1352Lys) | rs80357202 | Het | Benign |
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P12 | M | 69 | Pancreas | BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign |
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.2014G > C | p.(Glu672Gln) | rs45532440 | Het | Benign | ||||
| c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | |||||
| P13 | M | 61 | Pancreas | BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign |
| P14 | F | 58 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.865A > C | p.(Asn289His) | rs766173 | Het | Benign | ||||
| c.2971A > G | p.(Asn991Asp) | rs1799944 | Het | Benign | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P15 | F | 58 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Hom | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Hom | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Hom | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Hom | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| PALB2 | c.2014G > C | p.(Glu672Gln) | rs45532440 | Het | Benign | ||||
| c.1676A > G | p.Gln559Arg | rs152451 | Het | Benign | |||||
| P16 | F | 80 | Pancreas | BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign |
| PALB2 | c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | ||||
| P17 | M | 75 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Hom | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P18 | M | 57 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P19 | F | 70 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P20 | M | 78 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Hom | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Hom | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Hom | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Hom | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| PALB2 | c.3451C > T | p.(Leu1151Phe) | rs786203462 | Het | UCV | ||||
| c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | |||||
| P21 | M | 60 | Prostate | BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign |
| P22 | F | 75 | Pancreas | BRCA2 | c.7057G > C | p.(Gly2353Arg) | rs80358935 | Het | UCV |
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.2993G > A | p.(Gly998Glu) | rs45551636 | Het | Benign | ||||
| c.2014G > C | p.(Glu672Gln) | rs45532440 | Het | Benign | |||||
| c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | |||||
| P23 | M | 28 | Pancreas | BRCA1 | c.5019G > A | p.(Met1673Ile) | rs1799967 | Het | Benign |
| c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign | |||||
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Hom | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P24 | F | 70 | Pancreas | BRCA1 | c.3119G > A | p.(Ser1040Asn) | rs4986852 | Het | Benign |
| c.1067A > G | p.(Gln356Arg) | rs1799950 | Het | Benign | |||||
| BRCA2 | c.865A > C | p.(Asn289His) | rs766173 | Het | Benign | ||||
| c.2971A > G | p.(Asn991Asp) | rs1799944 | Het | Benign | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P25 | M | 70 | Pancreas | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.1067A > G | p.(Gln356Arg) | rs1799950 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | ||||
| P26 | M | 51 | Pancreas | BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Hom | Benign |
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P27 | F | 43 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.1067A > G | p.(Gln356Arg) | rs1799950 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.6468_6469delTC | p.(Gln2157IlefsTer18) | rs80359596 | Het | Pathogenic | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P28 | F | 71 | Breast | BRCA1 | c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign |
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P29 | F | 65 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.457A > T | p.(Ser153Cys) | n.r. | Het | UCV | |||||
| BRCA2 | c.865A > C | p.(Asn289His) | rs766173 | Hom | Benign | ||||
| c.2971A > G | p.(Asn991Asp) | rs1799944 | Hom | Benign | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P30 | F | 70 | Breast | BRCA2 | c.5796_5797delTA | p.(His1932GInfsTer12) | rs80359537 | Het | Pathogenic |
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P31 | F | 36 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P32 | F | 33 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.1067A > G | p.(Gln356Arg) | rs1799950 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.5744C > T | p.(Thr1915Met) | rs4987117 | Het | Benign | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P33 | F | 34 | Breast | BRCA1 | c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign |
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P34 | F | 35 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Hom | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Hom | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Hom | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Hom | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P35 | F | 39 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Hom | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Hom | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Hom | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Hom | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P36 | F | 41 | Breast | BRCA1 | c.3119G > A | p.(Ser1040Asn) | rs4986852 | Het | Benign |
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P37 | F | 39 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P38 | F | 38 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P39 | F | 27 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P40 | F | 29 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Hom | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.2993G > A | p.(Gly998Glu) | rs45551636 | Het | Benign | ||||
| c.2014G > C | p.(Glu672Gln) | rs45532440 | Het | Benign | |||||
| c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | |||||
| P41 | F | 39 | Breast | BRCA1 | c.3119G > A | p.(Ser1040Asn) | rs4986852 | Het | Benign |
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P42 | F | 38 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Hom | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | ||||
| P43 | F | 38 | Breast | BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign |
| P44 | F | 39 | Breast | BRCA1 | c.4900A > G | p.(Ser1634Gly) | rs1799966 | Hom | Benign |
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Hom | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Hom | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Hom | Benign | |||||
| c.2077G > A | p.(Asp693Asn) | rs4986850 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P45 | F | 36 | Breast | BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign |
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| P46 | F | 43 | Breast | BRCA1 | c.1067A > G | p.(Gln356Arg) | rs1799950 | Het | Benign |
| BRCA2 | c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | ||||
| P47 | F | 42 | Breast | BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign |
| c.5508T > G | p.(Asn1836Lys) | rs80358774 | Het | Benign | |||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign | |||||
| PALB2 | c.2993G > A | p.(Gly998Glu) | rs45551636 | Het | Benign | ||||
| c.2014G > C | p.(Glu672Gln) | rs45532440 | Het | Benign | |||||
| c.1676A > G | p.(Gln559Arg) | rs152451 | Het | Benign | |||||
| P48 | F | 74 | Breast | BRCA1 | c.5019G > A | p.(Met1673Ile) | rs1799967 | Het | Benign |
| c.4900A > G | p.(Ser1634Gly) | rs1799966 | Het | Benign | |||||
| c.3548A > G | p.(Lys1183Arg) | rs16942 | Het | Benign | |||||
| c.3113A > G | p.(Glu1038Gly) | rs16941 | Het | Benign | |||||
| c.2612C > T | p.(Pro871Leu) | rs799917 | Het | Benign | |||||
| BRCA2 | c.1114A > C | p.(Asn372His) | rs144848 | Het | Benign | ||||
| c.7397T > C | p.(Val2466Ala) | rs169547 | Hom | Benign |
| Sample ID | Gender | Age at Diagnosis (y) | Kind of Cancer | Gene | Chr Position | Kind of CNV | Confirmed by MLPA |
|---|---|---|---|---|---|---|---|
| P3 | M | 66 | Pancreas | CHEK2 | Chr22: 29091641-29091919 | ex12Del | No |
| P12 | M | 69 | Pancreas | BRCA1 | Chr17: 41249247-41251890 | ex8-9Del | No |
| P28 | F | 71 | Breast | BRCA1 | Chr17: 41219572-41223313 | ex16-17Del | Yes |
| P29 | F | 65 | Breast | BRCA1 | Chr17: 41275950-41277259 | ex2Dup | Yes |
| P48 | F | 74 | Breast | BRCA2 | Chr13: 32906693-32906915 | ex10Del | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Secondino, A.; Starnone, F.; Veneruso, I.; Di Tella, M.A.; Conato, S.; De Angelis, C.; De Placido, S.; D’Argenio, V. Evaluation of a Four-Gene Panel for Hereditary Cancer Risk Assessment. Genes 2022, 13, 682. https://doi.org/10.3390/genes13040682
Secondino A, Starnone F, Veneruso I, Di Tella MA, Conato S, De Angelis C, De Placido S, D’Argenio V. Evaluation of a Four-Gene Panel for Hereditary Cancer Risk Assessment. Genes. 2022; 13(4):682. https://doi.org/10.3390/genes13040682
Chicago/Turabian StyleSecondino, Angela, Flavio Starnone, Iolanda Veneruso, Maria Antonietta Di Tella, Serena Conato, Carmine De Angelis, Sabino De Placido, and Valeria D’Argenio. 2022. "Evaluation of a Four-Gene Panel for Hereditary Cancer Risk Assessment" Genes 13, no. 4: 682. https://doi.org/10.3390/genes13040682







