Innovations in Phenotyping and Diagnostics Create Opportunities for Improved Treatment and Genetic Counseling for Rare Diseases
Funding
Acknowledgments
Conflicts of Interest
References
- Thompson, M.D.; Knaus, A. Rare Genetic Developmental Disabilities: Mabry Syndrome (MIM 239300) Index Cases and Glycophosphatidylinositol (GPI) Disorders. Genes 2024, 15, 619. [Google Scholar] [CrossRef]
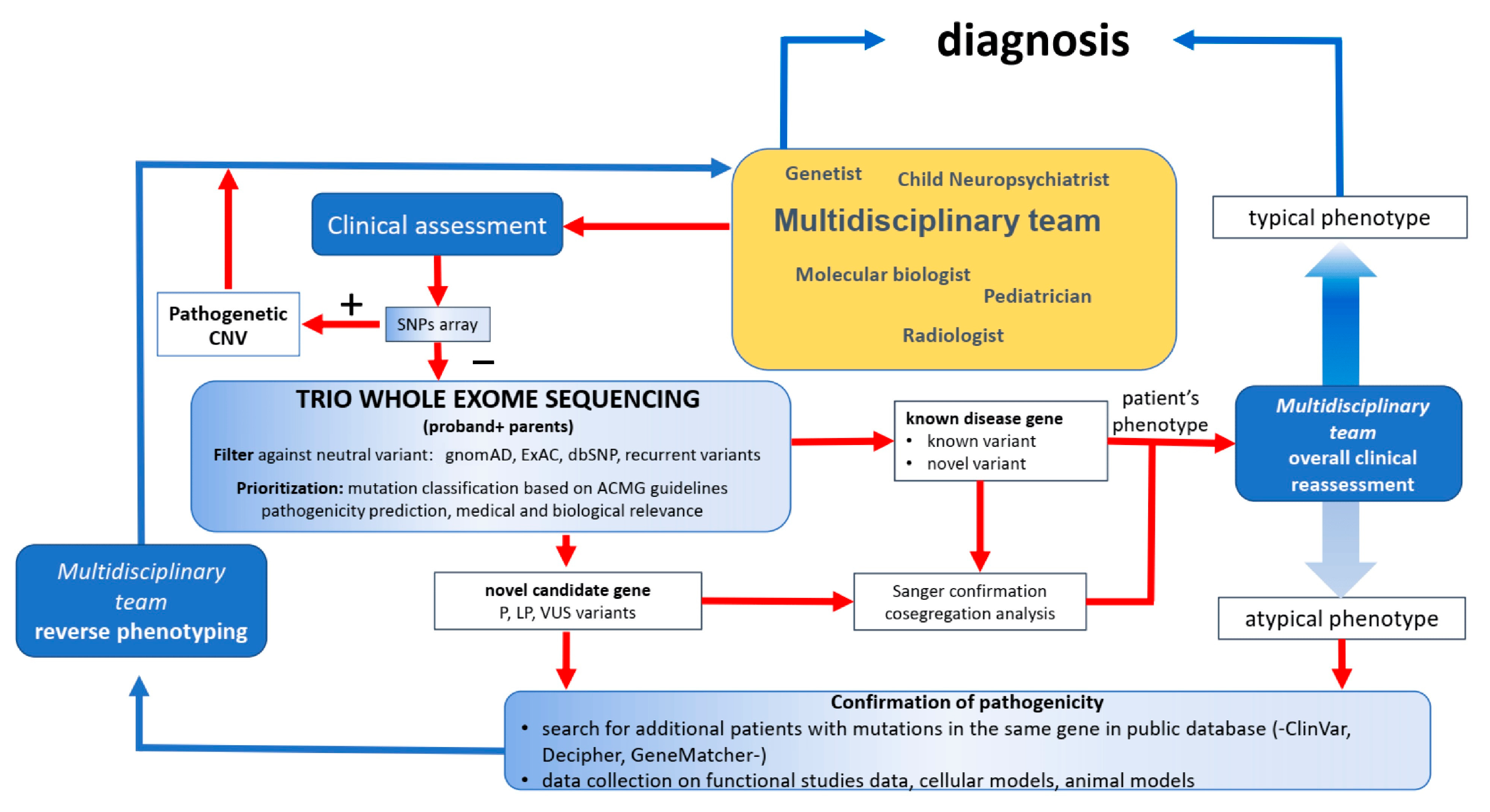
- Musante, L.; Costa, P.; Zanus, C.; Faletra, F.; Murru, F.M.; Bianco, A.M.; La Bianca, M.; Ragusa, G.; Athanasakis, E.; d’Adamo, A.P.; et al. The Genetic Diagnosis of Ultrarare DEEs: An Ongoing Challenge. Genes 2022, 13, 500. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.D.; Li, X.; Spencer-Manzon, M.; Andrade, D.M.; Murakami, Y.; Kinoshita, T.; Carpenter, T.O. Excluding Digenic Inheritance of PGAP2 and PGAP3 Variants in Mabry Syndrome (OMIM 239300) Patient: Phenotypic Spectrum Associated with PGAP2 Gene Variants in Hyperphosphatasia with Mental Retardation Syndrome-3 (HPMRS3). Genes 2023, 14, 359. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Miao, Z.; Umair, M.; Ullah, A.; Alshabeeb, M.A.; Bilal, M.; Ahmad, F.; Rappold, G.A.; Ansar, M.; Carapito, R. Two Cases of Recessive Intellectual Disability Caused by NDST1 and METTL23 Variants. Genes 2020, 11, 1021. [Google Scholar] [CrossRef] [PubMed]
- German, A.; Jukic, J.; Laner, A.; Arnold, P.; Socher, E.; Mennecke, A.; Schmidt, M.A.; Winkler, J.; Abicht, A.; Regensburger, M. Novel Homozygous FA2H Variant Causing the Full Spectrum of Fatty Acid Hydroxylase-Associated Neurodegeneration (SPG35). Genes 2024, 15, 14. [Google Scholar] [CrossRef] [PubMed]
- Riviello, F.N.; Daponte, A.; Ponzi, E.; Ficarella, R.; Orsini, P.; Bucci, R.; Ventura, M.; Antonacci, F.; Catacchio, C.R.; Gentile, M. A Rare Case of Concurrent 2q34q36 Duplication and 2q37 Deletion in a Neonate with Syndromic Features. Genes 2023, 14, 2194. [Google Scholar] [CrossRef] [PubMed]
- Cellamare, A.; Coccaro, N.; Nuzzi, M.C.; Casieri, P.; Tampoia, M.; Maggiolini, F.A.M.; Gentile, M.; Ficarella, R.; Ponzi, E.; Conserva, M.R.; et al. Cytogenetic and Array-CGH Characterization of a Simple Case of Reciprocal t(3;10) Translocation Reveals a Hidden Deletion at 5q12. Genes 2021, 12, 877. [Google Scholar] [CrossRef] [PubMed]
- Fyke, W.; Velinov, M. FMR1 and Autism, an Intriguing Connection Revisited. Genes 2021, 12, 1218. [Google Scholar] [CrossRef] [PubMed]
- Joga-Elvira, L.; Martinez-Olmo, J.; Joga, M.-L.; Jacas, C.; Roche-Martínez, A.; Brun-Gasca, C. Study of the Interaction between Executive Function and Adaptive Behavior at School in Girls with Fragile X Syndrome. Genes 2021, 12, 1108. [Google Scholar] [CrossRef]
- Miyoshi, H.; Otsuki, S.; Mukaida, K.; Kido, K.; Sumii, A.; Ikeda, T.; Noda, Y.; Yasuda, T.; Narasaki, S.; Kato, T.; et al. Effects of Remimazolam on Intracellular Calcium Dynamics in Myotubes Derived from Patients with Malignant Hyperthermia and Functional Analysis of Type 1 Ryanodine Receptor Gene Variants. Genes 2023, 14, 2009. [Google Scholar] [CrossRef]
- Morgenthau, A.; Margus, C.; Mackley, M.P.; Miller, A.P. Rare Disease Education Outside of the Classroom and Clinic: Evaluation of the RARE Compassion Program for Undergraduate Medical Students. Genes 2022, 13, 1707. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.D.; Killoran, A.; Percy, M.E.; Nezarati, M.; Cole, D.E.C.; Hwang, P.A. Hyperphosphatasia with neurologic deficit: A pyridoxine-responsive seizure disorder? Pediatr. Neurol. 2006, 34, 303–307. [Google Scholar] [CrossRef]
- Kuki, I.; Takahashi, Y.; Okazaki, S.; Kawawaki, H.; Ehara, E.; Inoue, N.; Kinoshita, T.; Murakami, Y. Vitamin B6-responsive epilepsy due to inherited GPI deficiency. Neurology 2013, 8, 1467–1469. [Google Scholar] [CrossRef] [PubMed]
- Chiyonobu, T.; Inoue, N.; Morimoto, M.; Kinoshita, T.; Murakami, Y. Glycosylphosphatidylinositol (GPI) anchor deficiency caused by mutations in PIGW is associated with West syndrome and hyperphosphatasia with mental retardation syndrome. J. Med. Genet. 2014, 51, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Messina, M.; Manea, E.; Cullup, T.; Tuschl, K.; Batzios, S. Hyperphosphatasia with mental retardation syndrome 3: Cerebrospinal fluid abnormalities and correction with pyridoxine and Folinic acid. JIMD Rep. 2022, 64, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, T.; Žigman, T.; Ramadža, D.P.; Omerza, L.; Pušeljić, S.; Hrvaćanin, Z.E.; Miyake, N.; Matsumoto, N.; Barić, I. A novel PGAP3 mutation in a Croatian boy with brachytelephalangy and a thin corpus callosum. Hum. Genome Var. 2018, 5, 18005. [Google Scholar] [CrossRef]
- Kuwayama, R.; Suzuki, K.; Nakamura, J.; Aizawa, E.; Yoshioka, Y.; Ikawa, M.; Nabatame, S.; Inoue, K.I.; Shimmyo, Y.; Ozono, K.; et al. Establishment of mouse model of inherited PIGO deficiency and therapeutic potential of AAV-based gene therapy. Nat. Commun. 2022, 13, 3107. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez de Los Santos, M.; Rivalan, M.; David, F.S.; Stumpf, A.; Pitsch, J.; Tsortouktzidis, D.; Velasquez, L.M.; Voigt, A.; Schilling, K.; Mattei, D.; et al. A CRISPR-Cas9-engineered mouse model for GPI-anchor deficiency mirrors human phenotypes and exhibits hippocampal synaptic dysfunctions. Proc. Natl. Acad. Sci. USA 2021, 118, e2014481118. [Google Scholar] [CrossRef]
- Mabry, C.C.; Bautista, A.; Kirk, R.F.; Dubilier, L.D.; Braunstein, H.; Koepke, J.A. Familial hyperphosphatase with mental retardation, seizures, and neurologic deficits. J. Pediatr. 1970, 77, 74–85. [Google Scholar] [CrossRef]
- Thompson, M.D.; Knaus, A.A.; Barshop, B.A.; Caliebe, A.; Muhle, H.; Nguyen, T.T.M.; Baratang, N.V.; Kinoshita, T.; Percy, M.E.; Campeau, P.M.; et al. A post glycosylphosphatidylinositol (GPI) attachment to proteins, type 2 (PGAP2) variant identified in Mabry syndrome index cases: Molecular genetics of the prototypical inherited GPI disorder. Eur. J. Med. Genet. 2020, 63, 103822. [Google Scholar] [CrossRef]
- Cole, D.E.; Thompson, M.D. Neurogenetic aspects of hyperphosphatasia in Mabry syndrome. Subcell. Biochem. 2015, 76, 343–361. [Google Scholar] [PubMed]
- Thompson, M.D.; Nezarati, M.M.; Gillessen-Kaesbach, G.; Meinecke, P.; Mendoza-Londono, R.; Mornet, E.; Brun-Heath, I.; Squarcioni, C.P.; Legeai-Mallet, L.; Munnich, A.; et al. Hyperphosphatasia with seizures, neurologic deficit, and characteristic facial features: Five new patients with Mabry syndrome. Am. J. Med. Genet. A 2010, 152, 1661–1669. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.D.; Roscioli, T.; Marcelis, C.; Nezarati, M.M.; Stolte-Dijkstra, I.; Sharom, F.J.; Lu, P.; Phillips, J.A.; Sweeney, E.; Robinson, P.N.; et al. Phenotypic variability in hyperphosphatasia with seizures and neurologic deficit (Mabry syndrome). Am. J. Med. Genet. A 2012, 158A, 553–558. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thompson, M.D. Innovations in Phenotyping and Diagnostics Create Opportunities for Improved Treatment and Genetic Counseling for Rare Diseases. Genes 2024, 15, 715. https://doi.org/10.3390/genes15060715
Thompson MD. Innovations in Phenotyping and Diagnostics Create Opportunities for Improved Treatment and Genetic Counseling for Rare Diseases. Genes. 2024; 15(6):715. https://doi.org/10.3390/genes15060715
Chicago/Turabian StyleThompson, Miles D. 2024. "Innovations in Phenotyping and Diagnostics Create Opportunities for Improved Treatment and Genetic Counseling for Rare Diseases" Genes 15, no. 6: 715. https://doi.org/10.3390/genes15060715
APA StyleThompson, M. D. (2024). Innovations in Phenotyping and Diagnostics Create Opportunities for Improved Treatment and Genetic Counseling for Rare Diseases. Genes, 15(6), 715. https://doi.org/10.3390/genes15060715




