Genetic Variants in KNDy Pathway Lack Association with Premature Ovarian Insufficiency in Mexican Women: A Sequencing-Based Cohort Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Patients and POI-Free Subjects
2.2. Genomic DNA Isolation
2.3. Genetic Screening and Genotyping
2.4. DNA Sequencing
2.5. Gene Variant Analysis
3. Results
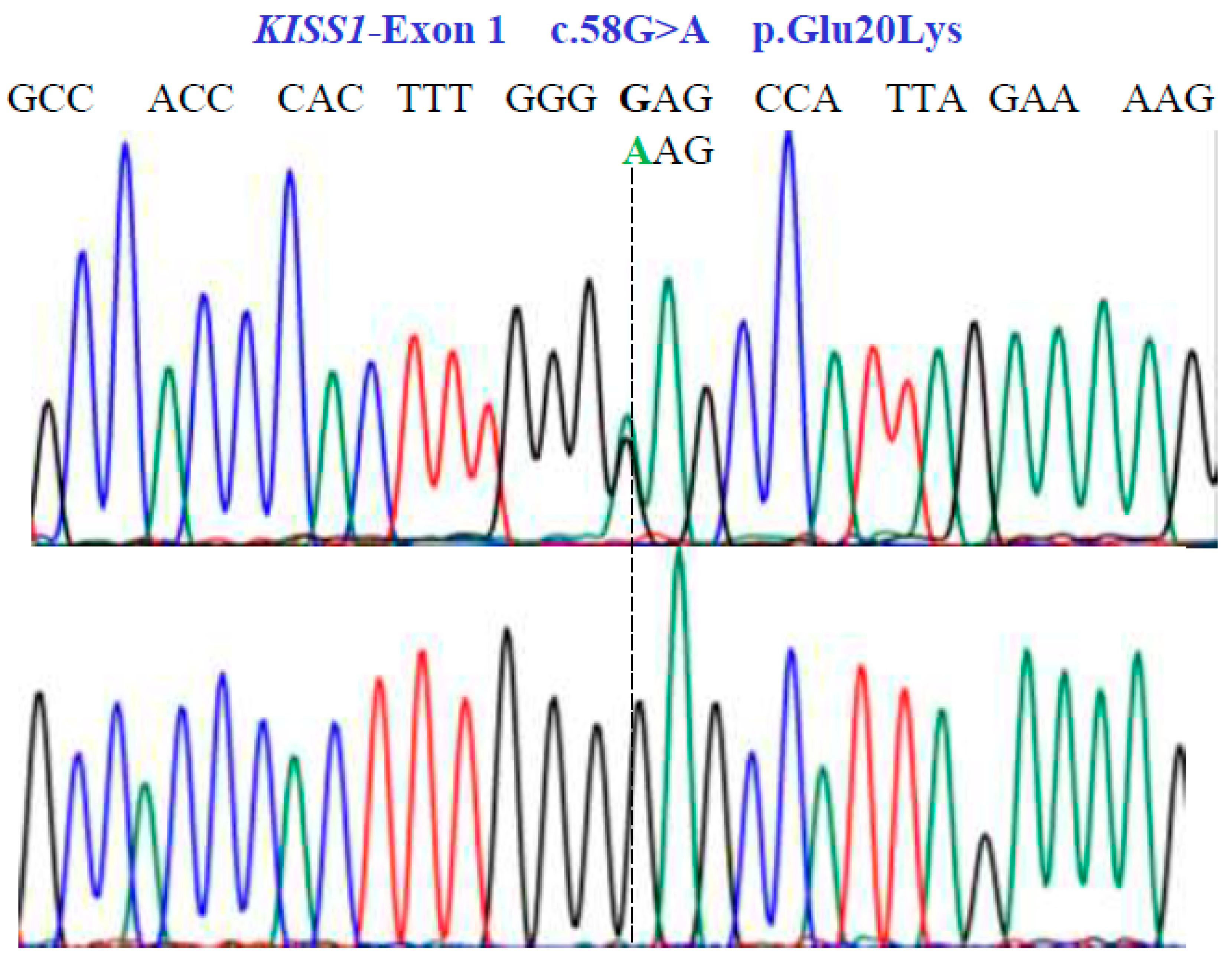
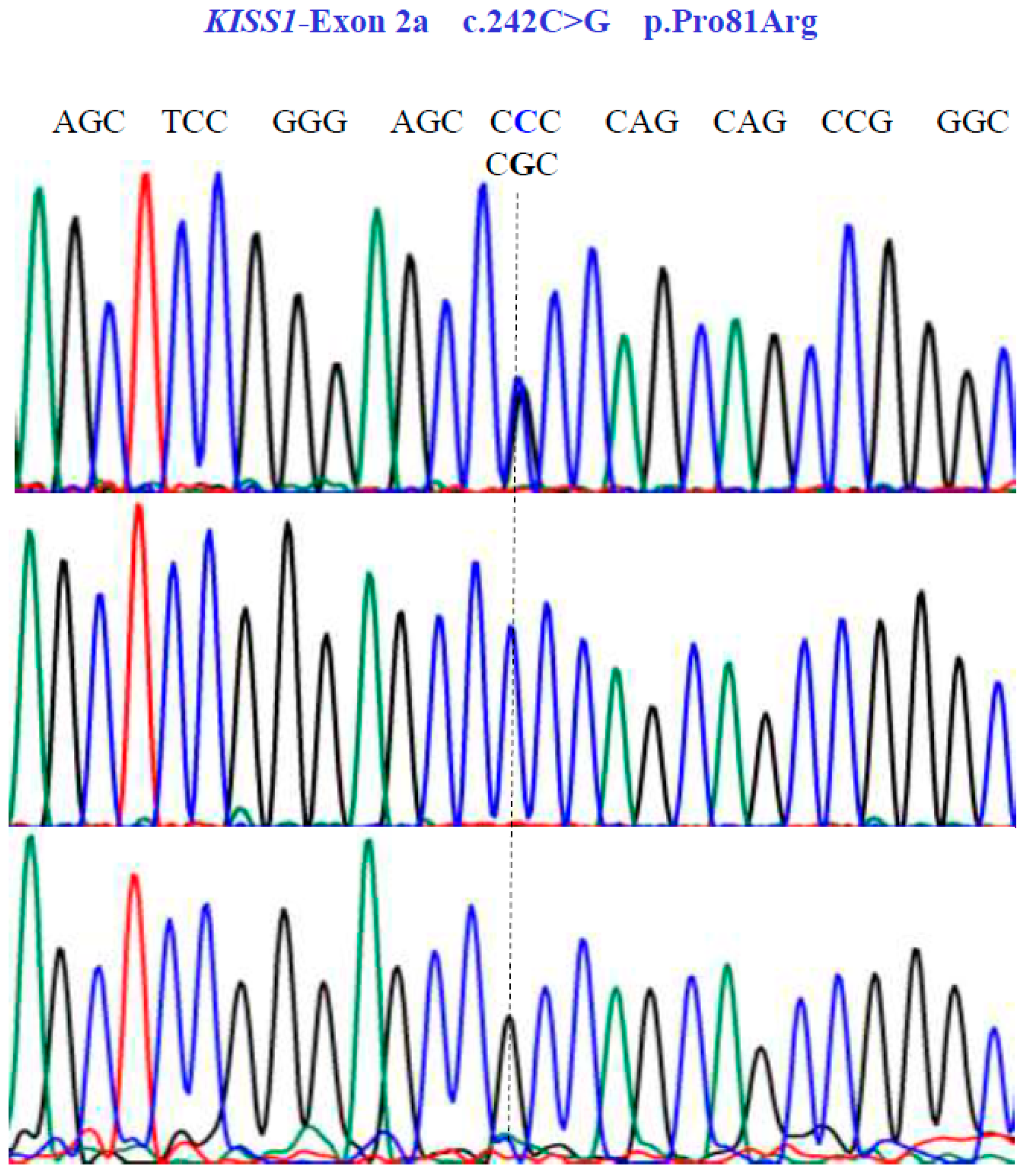
3.1. Coding Region Evaluation
3.2. Gene Variant Screening
3.3. Genomic Variant
3.4. Genotyping
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ramos, L. WT1, NR0B1, NR5A1, LHX9, ZFP92, ZNF275, INSL3, and NRIP1 genetic variants in patients with premature ovarian insufficiency in a Mexican cohort. Genes 2022, 13, 611. [Google Scholar] [CrossRef] [PubMed]
- Welt, C.K. Primary ovarian insufficiency: A more accurate term for premature ovarian failure. Clin. Endocrinol. 2008, 68, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Nelson, L.M. Clinical practice. Primary ovarian insufficiency. N. Engl. J. Med. 2009, 360, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Meczekalski, B.; Niwczyk, O.; Bala, G.; Szeliga, A. Managing early onset osteoporosis: The impact of premature ovarian insufficiency on bone health. J. Clin. Med. 2023, 12, 4042. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhou, X.Y.; Wang, A.; Lai, Y.H.; Zhang, X.F.; Liu, X.T.; Wang, Z.; Liu, Y.D.; Tang, S.Y.; Chen, S.L. Novel Tu translation elongation factor, mitochondrial (TUFM) homozygous variant in a consanguineous family with premature ovarian insufficiency. Clin. Genet. 2023, 104, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Gong, X.; Fan, Y.; Cao, J.; Zhao, J.; Zhang, Y.; Wang, X.; Meng, K. DNA double-strand break genetic variants in patients with premature ovarian insufficiency. J. Ovarian Res. 2023, 16, 135. [Google Scholar] [CrossRef] [PubMed]
- Shekari, S.; Stankovic, S.; Gardner, E.J.; Hawkes, G.; Kentistou, K.A.; Beaumont, R.N.; Mörseburg, A.; Wood, A.R.; Prague, J.K.; Mishra, G.D.; et al. Penetrance of pathogenic genetic variants associated with premature ovarian insufficiency. Nat. Med. 2023, 29, 1692–1699. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, H.; Bartram, S.; Charalambides, M.M.; Murthy, S.; Petitt, T.; Pradeep, A.; Vineall, O.; Abaraonye, I.; Lancaster, A.; Koysombat, K.; et al. Kisspeptin-neuron control of LH pulsatility and ovulation. Front. Endocrinol. 2022, 13, 951938. [Google Scholar] [CrossRef] [PubMed]
- Saadeldin, I.M.; Koo, O.J.; Kang, J.T.; Kwon, D.K.; Park, S.J.; Kim, S.J.; Moon, J.H.; Oh, H.J.; Jang, G.; Lee, B.C. Paradoxical effects of kisspeptin: It enhances oocyte in vitro maturation but has an adverse impact on hatched blastocysts during in vitro culture. Reprod. Fertil. Dev. 2012, 24, 656–668. [Google Scholar] [CrossRef]
- Zeydabadi Nejad, S.; Ramezani Tehrani, F.; Zadeh-Vakili, A. The role of kisspeptin in female reproduction. Int. J. Endocrinol. Metab. 2017, 15, e44337. [Google Scholar] [CrossRef]
- Nagae, M.; Uenoyama, Y.; Okamoto, S.; Tsuchida, H.; Ikegami, K.; Goto, T.; Majarune, S.; Nakamura, S.; Sanbo, M.; Hirabayashi, M.; et al. Direct evidence that KNDy neurons maintain gonadotropin pulses and folliculogenesis as the GnRH pulse generator. Proc. Natl. Acad. Sci. USA 2021, 118, e2009156118. [Google Scholar] [CrossRef] [PubMed]
- Uenoyama, Y.; Tsuchida, H.; Nagae, M.; Inoue, N.; Tsukamura, H. Opioidergic pathways and kisspeptin in the regulation of female reproduction in mammals. Front. Neurosci. 2022, 16, 958377. [Google Scholar] [CrossRef] [PubMed]
- Herbison, A.E. A simple model of estrous cycle negative and positive feedback regulation of GnRH secretion. Front. Neuroendocrinol. 2020, 57, 100837. [Google Scholar] [CrossRef] [PubMed]
- Xie, Q.; Kang, Y.; Zhang, C.; Xie, Y.; Wang, C.; Liu, J.; Yu, C.; Zhao, H.; Huang, D. The role of kisspeptin in the control of the hypothalamic-pituitary-gonadal axis and reproduction. Front. Endocrinol. 2022, 13, 925206. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.M.; Novak, A.G.; Lehman, M.N. KNDy neurons of the hypothalamus and their role in GnRH pulse generation: An update. Endocrinology 2023, 165, 2. [Google Scholar] [CrossRef] [PubMed]
- Semple, R.K.; Achermann, J.C.; Ellery, J.; Farooqi, I.S.; Karet, F.E.; Stanhope, R.G.; O’rahilly, S.; Aparicio, S.A. Two novel missense mutations in g protein-coupled receptor 54 in a patient with hypogonadotropic hypogonadism. J. Clin. Endocrinol. Metab. 2005, 90, 1849–1855. [Google Scholar] [CrossRef]
- Seminara, S.B.; Messager, S.; Chatzidaki, E.E.; Thresher, R.R.; Acierno, J.S., Jr.; Shagoury, J.K.; Bo-Abbas, Y.; Kuohung, W.; Schwinof, K.M.; Hendrick, A.G.; et al. The GPR54 gene as a regulator of puberty. N. Engl. J. Med. 2003, 349, 1614–1627. [Google Scholar] [CrossRef] [PubMed]
- Topaloglu, A.K.; Tello, J.A.; Kotan, L.D.; Ozbek, M.N.; Yilmaz, M.B.; Erdogan, S.; Gurbuz, F.; Temiz, F.; Millar, R.P.; Yuksel, B. Inactivating KISS1 mutation and hypogonadotropic hypogonadism. N. Engl. J. Med. 2012, 366, 629–635. [Google Scholar] [CrossRef]
- Albalawi, F.S.; Daghestani, M.H.; Daghestani, M.H.; Eldali, A.; Warsy, A.S. rs4889 polymorphism in KISS1 gene, its effect on polycystic ovary syndrome development and anthropometric and hormonal parameters in Saudi women. J. Biomed. Sci. 2018, 25, 50. [Google Scholar] [CrossRef]
- Branavan, U.; Muneeswaran, K.; Wijesundera, W.S.S.; Senanayake, A.; Chandrasekharan, N.V.; Wijeyaratne, C.N. Association of KISS1 and GPR54 gene polymorphisms with polycystic ovary syndrome among Sri Lankan women. Biomed. Res. Int. 2019, 2019, 6235680. [Google Scholar] [CrossRef]
- Daghestani, M.H.; Daghestani, M.H.; Daghistani, M.; Ambreen, K.; Albalawi, F.S.; AlNeghery, L.M.; Warsy, A.S. Influence of KISS1 gene polymorphisms on the risk of polycystic ovary syndrome and its associated variables, in Saudi women. BMC Endocr Disord. 2020, 20, 59. [Google Scholar] [CrossRef] [PubMed]
- Farsimadan, M.; Moammadzadeh Ghosi, F.; Takamoli, S.; Vaziri, H. Association analysis of KISS1 polymorphisms and haplotypes with polycystic ovary syndrome. Br. J. Biomed. Sci. 2021, 78, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Zhang, Q.; Xiao, X.; Tao, X.; Gao, M.; He, W.; Wu, X.; Yuan, T. Associations of the KISS-1 and GPR54 genetic polymorphism with polycystic ovary syndrome in Yunnan, China. Gynecol. Endocrinol. 2022, 38, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Wu, Y.; Cheng, J.; Liu, L.; Li, X.; Chen, D.; Huang, S.; Wen, Y.; Ke, Y.; Yao, Y.; et al. Association of polymorphisms in the Kisspeptin/GPR54 pathway genes with risk of early puberty in Chinese girls. J. Clin. Endocrinol. Metab. 2020, 105, e1458–e1467. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.W.D.; Wallace, M.R.; Staud, R.; Fillingim, R.B. OPRM1, OPRK1, and COMT genetic polymorphisms associated with opioid effects on experimental pain: A randomized, double-blind, placebo-controlled study. Pharmacogenomics J. 2020, 20, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Zhao, A.; Lu, H.; Zou, D.; Dong, B.; Wang, X.; Liu, L.; Zhou, S. KISS1 gene variations and susceptibility to idiopathic recurrent pregnancy loss. Reprod Sci. 2023, 30, 2573–2579. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Xiong, W.; Yang, Y.; Li, H.; Xiong, C. A comprehensive meta-analysis to identify susceptibility genetic variants for precocious puberty. Ann. Hum. Genet. 2024, 88, 138–153. [Google Scholar] [CrossRef] [PubMed]
- Pagani, S.; Calcaterra, V.; Acquafredda, G.; Montalbano, C.; Bozzola, E.; Ferrara, P.; Gasparri, M.; Villani, A.; Bozzola, M. MKRN3 and KISS1R mutations in precocious and early puberty. Ital. J. Pediatr. 2020, 46, 39. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.A.; Bhanarkar, S.R.; Keshwani, R.; Pande, S.; Modi, D.N.; Mehta, A.; Bombe, S.; Pathak, B.R.; Joshi, B.; Tandon, D.; et al. Relevance of augmented kisspeptin signaling through H(364) KISS1R in central precocious puberty. Gene 2024, 895, 148016. [Google Scholar] [CrossRef]
- Dong, L.; Zhou, W.; Lin, Z.; Tang, L.; Deng, X.; Chen, B.; Huang, W.; Xiong, Q. Polymorphism rs5780218, rs12998 and rs10158616 in KISS1 gene among the Hubei province Chinese girls with the central precocious puberty. Endocrine 2024. Online ahead of print. [Google Scholar] [CrossRef]
- Cruz Quevedo, E.G.; Mimendi Aguilar, G.M.; Juarez Aguilar, L.A.; Gutierrez Rubio, S.A.; Flores Martinez, S.E.; Davalos Rodriguez, I.P.; Sanchez Corona, J.; Torres Moran, M.I.; Rosales Gomez, R.C.; Moran Moguel, M.C. Polymorphisms rs12998 and rs5780218 in KISS1 suppressor metastasis gene in Mexican patients with breast cancer. Dis. Markers 2015, 2015, 365845. [Google Scholar] [CrossRef]
- Uenoyama, Y.; Tsukamura, H. KNDy neurones and GnRH/LH pulse generation: Current understanding and future aspects. J. Neuroendocrinol. 2023, 35, e13285. [Google Scholar] [CrossRef] [PubMed]
- Levran, O.; Yuferov, V.; Kreek, M.J. The genetics of the opioid system and specific drug addictions. Hum. Genet. 2012, 131, 823–842. [Google Scholar] [CrossRef] [PubMed]
- Yuferov, V.; Ji, F.; A Nielsen, D.; Levran, O.; Ho, A.; Morgello, S.; Shi, R.; Ott, J.; Kreek, M.J. A functional haplotype implicated in vulnerability to develop cocaine dependence is associated with reduced PDYN expression in human brain. Neuropsychopharmacology 2009, 4, 1185–1197. [Google Scholar] [CrossRef] [PubMed]
- Taqi, M.M.; Bazov, I.; Watanabe, H.; Sheedy, D.; Harper, C.; Alkass, K.; Druid, H.; Wentzel, P.; Nyberg, F.; Yakovleva, T.; et al. Prodynorphin CpG-SNPs associated with alcohol dependence: Elevated methylation in the brain of human alcoholics. Addict. Biol. 2011, 16, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Karpyak, V.M.; Winham, S.J.; Preuss, U.W.; Zill, P.; Cunningham, J.M.; Walker, D.L.; Lewis, K.A.; Geske, J.R.; Colby, C.L.; Abulseoud, O.A.; et al. Association of the PDYN gene with alcohol dependence and the propensity to drink in negative emotional states. Int. J. Neuropsychopharmacol. 2013, 16, 975–985. [Google Scholar] [CrossRef]
- Wang, S.C.; Tsou, H.H.; Chung, R.H.; Chang, Y.S.; Fang, C.P.; Chen, C.H.; Ho, K.; Kuo, H.W.; Liu, S.C.; Shih, Y.H.; et al. The association of genetic polymorphisms in the kappa-opioid receptor 1 gene with body weight, alcohol use, and withdrawal symptoms in patients with methadone maintenance. J. Clin. Psychopharmacol. 2014, 34, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.J.; Rhie, Y.J.; Nam, H.K.; Kim, H.R.; Lee, K.H. Genetic variations of the KISS1R gene in Korean girls with central precocious puberty. J. Korean Med. Sci. 2017, 32, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Senormanci, G.; Turan, C.; Celik, S.K.; Celik, A.; Edgunlu, T.G.; Akbas, D.; Şenormancı, Ö. Prodynorphin (PDYN) gene polymorphisms in Turkish patients with methamphetamine use disorder, changes in PDYN serum levels in withdrawal and the relationship between PDYN, temperament and depression. J. Ethn. Subst. Abuse. 2022, 21, 522–537. [Google Scholar] [CrossRef] [PubMed]
- European Society for Human R, Embryology Guideline Group on POI; Webber, L.; Davies, M.; Anderson, R.; Bartlett, J.; Braat, D.; Cartwright, B.; Cifkova, R.; Keizer-Schrama, S.d.M.; Hogervorst, E.; et al. ESHRE Guideline: Management of women with premature ovarian insufficiency. Hum. Reprod. 2016, 31, 926–937. [Google Scholar]
- Yatsenko, S.A.; Witchel, S.F.; Gordon, C.M. Primary Amenorrhea and Premature Ovarian Insufficiency. Endocrinol. Metab. Clin. N. Am. 2024, 53, 293–305. [Google Scholar] [CrossRef]





| Gene | cDNA Variant | Genotype | Function | Genotype Frequencies (POI Patients) | Allele Frequencies (POI Patients) | Genotype Frequencies (Healthy Females) | Allele Frequencies (Healthy Females) | Genotype Frequencies (Healthy Males) | Allele Frequencies (Healthy Males) |
|---|---|---|---|---|---|---|---|---|---|
| KISS1 | c.58G>A | G/G | 0.86 | p = 0.93 | 0.96 | p = 0.98 | 1.0 | p = 1.0 | |
| A/A | Non-Synonymous | 0.0 | q = 0.07 | 0.0 | q = 0.02 | 0.0 | q = 0.0 | ||
| G/A | 0.14 | 0.04 | 0.0 | ||||||
| c.242C>G | C/C | 0.29 | p = 0.58 | 0.36 | p = 0.61 | 0.34 | p = 0.6 | ||
| G/G | Non-Synonymous | 0.14 | q = 0.42 | 0.14 | q = 0.39 | 0.14 | q = 0.4 | ||
| C/G | 0.57 | 0.5 | 0.52 | ||||||
| KISS1R | c.1091A>T | A/A | 0.43 | p = 0.72 | 0.46 | p = 0.73 | 44 | p = 0.72 | |
| T/T | Non-Synonymous | 0.0 | q = 0.28 | 0.0 | q = 0.27 | 0.0 | q = 0.28 | ||
| A/T | 0.57 | 0.54 | 56 | ||||||
| PDYN | c.600C>T | C/C | 0.0 | p = 0.04 | 0.0 | p = 0.08 | 0.0 | p = 0.07 | |
| T/T | Synonymous | 0.93 | q = 0.96 | 0.84 | q = 0.92 | 0.86 | q = 0.93 | ||
| C/T | 0.07 | 0.16 | 0.14 | ||||||
| OPRK1 | c.36G>T | G/G | 0.93 | p = 0.97 | 0.96 | p = 0.98 | 0.96 | p = 0.98 | |
| T/T | Synonymous | 0.0 | q = 0.03 | 0.0 | q = 0.02 | 0.0 | q = 0.02 | ||
| G/T | 0.07 | 0.04 | 0.04 |
| Gene | Location | SNV | Amino Acid Substitution | Reference SNV | DDGun | VarSite | SIFT | PolyPhen |
|---|---|---|---|---|---|---|---|---|
| KISS1 | Exon 1 | c.58G>A | p.E20K | rs12998 | Decrease of stability (−0.9) | Possibly Deleterious (2.44) | Likely Bening (0.03) | Likely Bening (0.37) |
| Exon 2a | c.242C>G | p.P81R | rs4889 | Decrease of stability (−1.5) | Likely Bening (1.52) | Likely Bening (0.28) | Likely Bening (0.2) | |
| KISS1R | Exon 5c | c.1091A>T | p.L364H | rs350132 | Decrease of stability (−0.1) | Likely Bening (0.77) | Likely Bening (1.0) | Likely Bening (0.0) |
| PDYN | Exon 2c | c.600C>T | p.H200= | rs6045819 | Neutral (0.0) | Likely Bening (−0.52) | Likely Bening (0.0) | Likely Bening (0.0) |
| OPRK1 | Exon 1a | c.36G>T | p.Pro12= | rs1051660 | Neutral (0.0) | Likely Bening (0.27) | Likely Bening (0.0) | Likely Bening (0.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz, A.; Ramos, L. Genetic Variants in KNDy Pathway Lack Association with Premature Ovarian Insufficiency in Mexican Women: A Sequencing-Based Cohort Study. Genes 2024, 15, 788. https://doi.org/10.3390/genes15060788
Ruiz A, Ramos L. Genetic Variants in KNDy Pathway Lack Association with Premature Ovarian Insufficiency in Mexican Women: A Sequencing-Based Cohort Study. Genes. 2024; 15(6):788. https://doi.org/10.3390/genes15060788
Chicago/Turabian StyleRuiz, Aidet, and Luis Ramos. 2024. "Genetic Variants in KNDy Pathway Lack Association with Premature Ovarian Insufficiency in Mexican Women: A Sequencing-Based Cohort Study" Genes 15, no. 6: 788. https://doi.org/10.3390/genes15060788
APA StyleRuiz, A., & Ramos, L. (2024). Genetic Variants in KNDy Pathway Lack Association with Premature Ovarian Insufficiency in Mexican Women: A Sequencing-Based Cohort Study. Genes, 15(6), 788. https://doi.org/10.3390/genes15060788








