1. Introduction
Exoskeletons are robotic devices which aim to help both healthy and unhealthy people in performing activities or recover some of their natural movements. They are devices attached to humans whose kinematic chain maps onto the human limb anatomy to assist in certain tasks. They aim to effectively, efficiently, and seamlessly transfer power to the user’s assisted limbs or joints to assist in tasks of daily living/rehabilitation (medical exoskeletons) or in work related tasks (occupational exoskeletons). They could be fully attached to the user (wearable and portable) or external to the person (grounded), giving the possibility of performing tasks in clinics, at home, or at work [
1,
2,
3].
During the past few decades, researchers have been working towards the development of exoskeletons with improved capabilities and “intelligence” levels to solve problems related to aging, disabilities, overloading, and muscle strain, which may prevent people from conducting a normal life, leading to marginalization with serious repercussions on both their working and private lives.
These devices are expected to play an important role in human health in the field of rehabilitation, assistive robotics and human power augmentation since research by the World Health Organization (WHO) has shown that more than 1.7 billion people worldwide suffer from musculoskeletal disorders (MSD), and this number is set to grow [
4,
5,
6]. These problems and more specific work-related musculoskeletal disorders (WRMSD) have been known for a long time. Literature dating back to the 1700s shows that Bernardino Ramazzini, an Italian physician and scientist who dedicated himself to the systematic study of occupational diseases, the social defense of workers and the observation of working conditions, had already identified this problem and provided suggestions for preventing harm at work in
De Morbis Artificum Diatriba [Diseases of Workers] [
7,
8]. As still occurs today, he observed that the working environment and prolonged, violent, and irregular motions and prolonged postures are the cause of a variety of common ailments affecting joints, bones, muscles, tendons, and ligaments [
8,
9,
10]. These afflictions can be episodic or chronic in duration and can also progress from mild to severe and impair the quality of life of people, reducing mobility, dexterity and people’s ability to work and perform daily living activities (ADL).
As reported by the European Agency for Safety and Health at Work (EU-OSHA) and the Italian Workers’ Compensatory Authority (INAIL) [
6,
11], the most common health problems affect low back pain (more than 50%) and upper limbs (more than 40%).
The number of projects addressing wearable robotics has increased since the 2000s, thanks to research programs such as “
Exoskeleton for human performance augmentation” set up by the Defense Advanced Research Projects Agency (DARPA). Exoskeleton application areas are related to different fields such as military, medical, and industrial [
12,
13,
14,
15,
16].
However, relatively few of these studies have focused on wrist injuries, although they form the fourth most common site for musculoskeletal pain in the upper limbs [
17]. Review articles on upper limbs [
1,
13,
18,
19,
20,
21,
22,
23,
24] have reflected a similar lack of focus on the wrist and mostly do not differentiate between the hand and wrist or even the whole upper arm [
25]. It should be noted that from a clinical perspective, wrist pain and hand pain are very different entities, both in terms of diagnosis and management [
25]. From the other side, once wrist functionalities are impaired, there is a very significant impact on the hand and fingers, especially gripping [
26].
The wrist has to deal with heavy loads (up to 20 kg in ADL) while having complex kinematics and dynamics that are needed to achieve high mobility and precision movements in 3D. Note that for each N of gripping force, the wrist experiences axial compression loads up to 14 times greater that must be distributed among all the carpal bones [
12]. Frequently diagnosed wrist injuries include carpal tunnel syndrome (CTS), ganglion cysts, sprains, tendinitis, and tenosynovitis as a result of repetitive wrist motion while lifting and transporting loads, holding objects in uncomfortable static positions, or using different working tools [
10,
25,
27,
28,
29], as shown in
Figure 1.
To address these problems, many different devices have been designed over the years. The majority of them are externally grounded and used to perform rehabilitation processes in clinics or at home with the aim of restoring human hand/wrist functionalities and dexterity and muscular strength after an injury has occurred. The lack of portability limits their usefulness for unstructured environment, outdoor applications, at work, or in everyday life activities where the users should be able to move freely. Here there is the need for fully wearable devices in which the entire system (including actuators, electronics, and batteries) is attached to the human body. Devices of this format can provide assistance, augmentation or rehabilitation wherever needed and at any time, and this can be extended to prevention of injuries at work, where wearable and portable wrist exoskeletons are highly desired. However, only a few are available in the market, and these are mainly focused on the hand by improving the user’s grasping strength (e.g., Carbonhand
® and Ironhand
® by Bioservo Technologies). Therefore, there is a very real and current need for specific wearable and portable devices conceived to mitigate wrist-related problems [
25].
This paper somewhat uniquely aims at providing an in-depth analysis of the literature and the state of the art in wrist exoskeletons and more specifically fully wearable wrist exoskeletons. It has been divided into two parts, with a focus on both medical and occupational wrist exoskeletons. In part I, which is the focus of this paper, we have conducted a critical, in-depth review of the growth and current status of research and commercial systems, highlighting the requirements and the technologies adopted. Detailed description of these devices and their characteristics are covered part II of this work, where considerations about why the market is lacking with respect to research will be provided.
This paper is organized as follows: In
Section 2, there is a description of the research methodology in terms of data selection protocol.
Section 3 provides an overview of human wrist anatomy and bio-mechanics. In
Section 4, the system requirements and issues are defined and described, and this information is used to guide the design of the exoskeleton. Different design architectures are described in
Section 5, focusing on actuation type, power source, power transmission, and sensing and control strategies. Finally, in
Section 6, a summary of the most significant findings is presented.
2. Materials and Methods
The methodological approach in this paper consists in searching the market and several database, i.e., Google Scholar, MDPI, Scopus, Frontiers, Elsevier, ResearchGate, IEEE/ASME, ScienceDirect, Sage, John Wiley & Sons and Taylor&Francis, identifying all technologies explored and implemented related to wrist exoskeletons.
The main keywords for conducting the research were “Human Wrist Bio-mechanics” and “Wrist exoskeletons”. Given the large amount of information available, it was further refined using additional filtering keywords: “Rehabilitation”, “Assistive”, “Wearable”, “Portable”, “Occupational”, “Industrial”. This search identified several hundred candidate papers and these were individually analyzed to detect all technologies implemented on wrist exoskeletons within the areas of: Engineering, Robotics, Automation, Rehabilitation, Computer Science, Bio-mechanics, Medicine, Hand Surgery or Therapy, Human-Machine Systems, Medical Devices, Industrial Medicine, and Materials Science. Using this approach, a set of specific inclusion and exclusion criteria were implemented to further narrow down the literature. These criteria were further applied to the documentation available after pre-screening through the text (e.g., reading the title, abstract or conclusions) and subsequent in-depth reading. This methodology identified documents that included articles, reviews, conference papers, book chapters, technical reports, and regulations.
The methodical scheme is as proposed in
Figure 2.
Inclusion criteria consist of:
Description of human wrist bio-mechanics;
Upper limb or hand exoskeletons which include the wrist in their design;
Devices able to effectively support the wrist, relieve pain, or mitigate fatigue;
Devices which guarantee at least one wrist movement;
Devices intended for rehabilitation, assistance and occupational purposes;
Portable devices;
Scientific articles, reviews, books, technical reports, and regulations;
Only documents written in the English language are considered.
Exclusion criteria consist of:
Exoskeleton devices for other body parts or limbs other than the wrist;
Prosthesis, orthosis, robotic devices, or exoskeletons attached to the human wrist but which do not allow free wrist movements or do not effectively support the wrist;
Military devices;
Fixed/grounded devices;
Studies with insufficient information on the design and results, which made the analysis unclear.
3. Human Wrist Bio-Mechanics
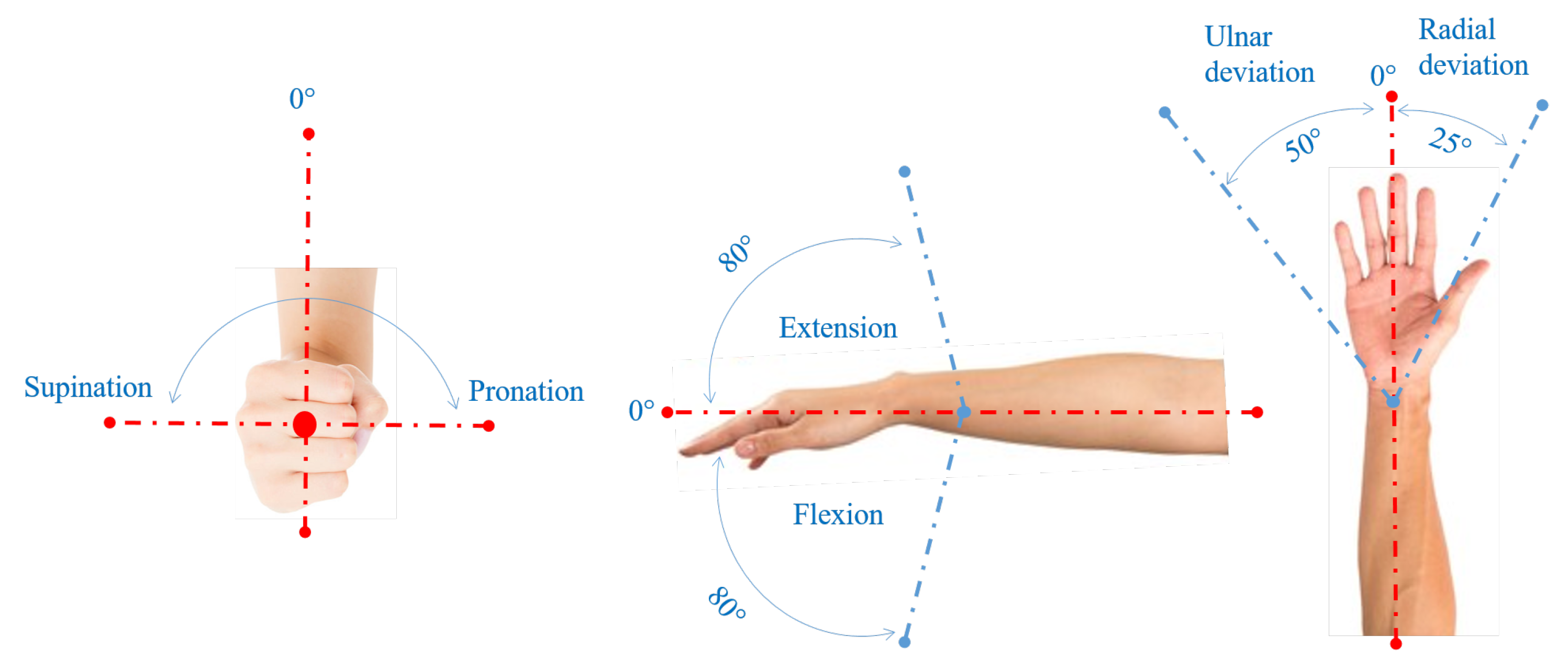
In this section there follows a brief overview of the wrist’s bio-mechanics highlighting its characteristics and range of motion (RoM). This is important in helping to define the features of devices that can have a positive impact on wrist well-being. From the functional point of view, the wrist is a single joint with two degrees of freedom (DoF): flexion/extension and radial deviation/ulnar deviation [
12,
18,
20,
30], although depending on the application, some texts will consider that there are three DoF, and within the third motion being considered is the pronation/supination movement [
31]. However, as this pronation/supination is mainly due to a combination of movements acting within the forearm and the elbow, we will neglect it in our consideration of wrist exoskeletons.
Several in vivo studies have suggested that wrist motions (flexion/extension and radial/ulnar deviation) occur due to movement about two orthogonal and non-intersecting axes in the proximal capitate. These axes have a slight offset of almost 5 mm, as shown in
Figure 3.
Motions are generated around an instantaneous center of rotation (CoR) with the displacement typically being ignored as the path of the centrode is very small. Hence, the rotation axes for the flexion/extension and radial/ulnar deviation are considered fixed [
20,
30,
32]. Some studies point out that the two DoF of the wrist are activated through four different axes of rotations, one for each movement: flexion, extension, radial deviation, ulnar deviation [
32]. However, we ignore this assumption, considering the fact that even though flexion and extension have different axes, they are intersected in the same point in the head of the capitate, and the same happens for the radial and ulnar deviation axes [
32].
Defining 0° as the neutral position of each movement, it is possible to define the average RoM for each DoF of a healthy human wrist. As shown in
Figure 4, flexion and extension are approximately 70°–80°. Radial deviation is around 15°–25°, and ulnar deviation is around 40°–50°, while pronation and supination are between 70° and 85° [
18,
31,
33]. However, it is well known that during activities of daily living (ADL) people never put their wrist to its limits. In fact, when performing daily tasks, wrist RoM is around 15° for flexion, 35° for extension, 15° for radial deviation, and 20° for ulnar deviation [
34].
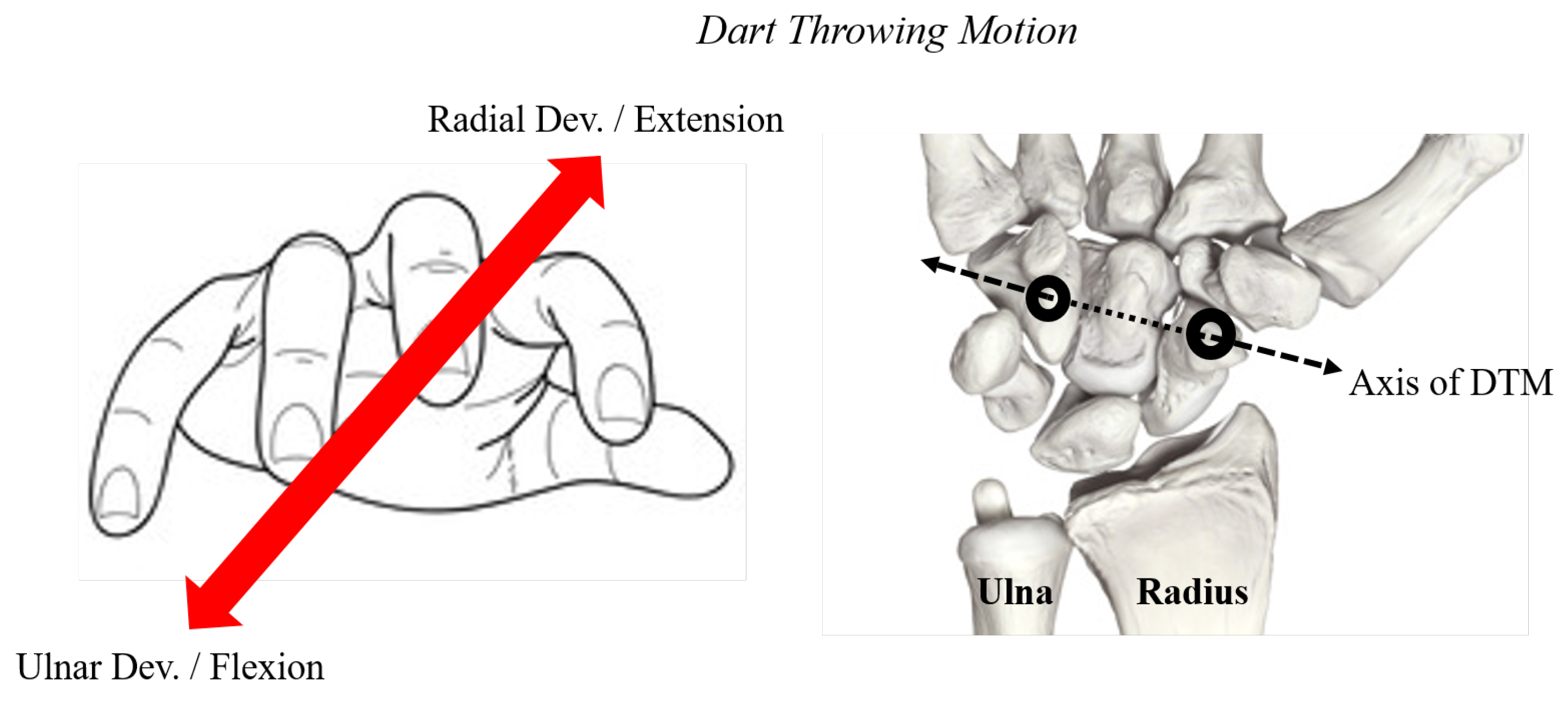
Furthermore, while performing many ADL, motions originating in the carpal bones (flexion/extension and radial/ulnar deviation) are coupled, meaning that one motion limits the other (e.g., radial deviation is reduced when fully extended) [
18,
31]. In fact, the wrist articulates about an oblique axis defined by
the Dart Throwing Motion (DTM) [
35,
36,
37,
38]. This movement proceeds from radial deviation-extension to ulnar deviation-flexion, as shown in
Figure 5 and
Figure 6 [
35].
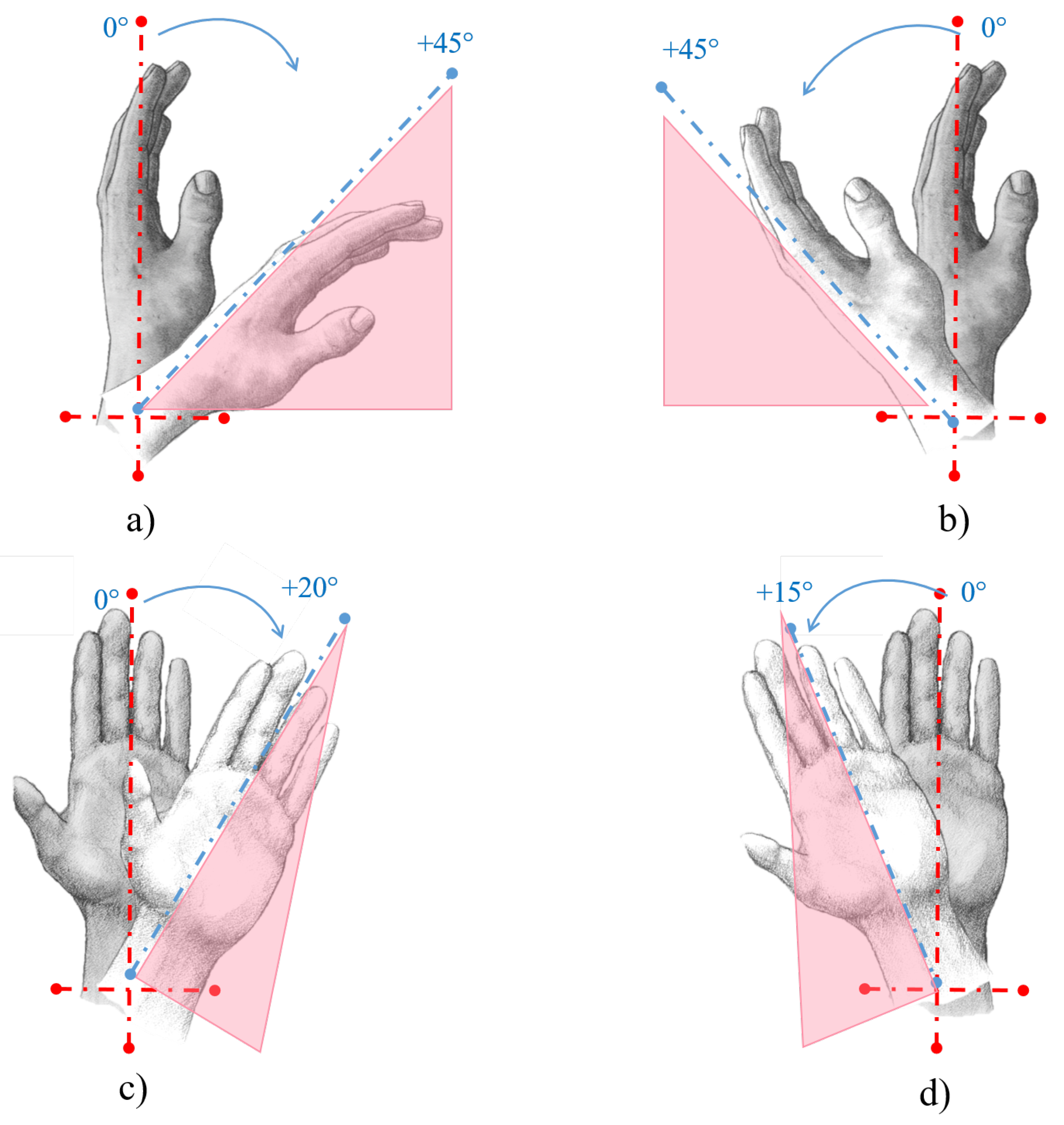
As depicted in
Figure 6, the orientation of the DTM plane does vary from person to person and has been quantified by researchers in ranging from 28° to 57° degrees relative to the flexion–extension axis [
35,
36,
37,
39,
40]. The intercept of the mean DTM plane indicated the wrist to be in 34° ulnar deviation at neutral flexion–extension as shown in
Figure 6 [
36]. With respect to the other movements, this is more important to the functional and mechanical aspects of the wrist since it defines the maximum RoM and requires minimal muscular effort for the movement (minimum stiffness and inertia direction of wrist motion) [
37,
39]. Moreover, the reduced stresses while performing this movement might provide an explanation of its frequent use in manual handling activities as it decreases the risk of overuse and injury [
41]. Recent and past in vivo analysis of unconstrained wrist motion have confirmed the use of the DTM plane in hammering, throwing, drinking, pouring, and twisting a jar lid [
38,
40,
42].
Knowledge of how loads are transferred on and through the wrist is an important factor in understanding the joint bio-mechanics and explaining pathogenesis and diseases. Since each N of muscle contraction forces applied with the hand equates to a wrist carpus axial compression loading of up to 14 N [
12]. According to Eschweiler et al. [
43], almost 80% of the load is transmitted across the radiocarpal joint in the following ratio: 45% crosses the radioscaphoid joint and 35% crosses the radiolunate joint. The remaining 20% is borne by the ulnocarpal joint. The peak loads across the wrist are lower than of other joints, ranging from 1.4 MPa (average value for scaphoid and lunate pressures) to 31.4 MPa. There is no significant difference in scaphoid and lunate pressures in all positions (flexion, neutral, extension) [
43].
Over-straining the wrist during manual activities generates problems such as carpal tunnel syndrome (CTS), carpal bone fractures, osteoarthritis, ganglion cysts, sprains and strains, tendinitis, and tenosynovitis [
44,
45]. These musculoskeletal disorders can occur both in the work environment (such as in food, manufacturing, and assembly plants), and in everyday life (e.g., certain diseases, accidental trauma, fall, sports). Of course, some sectors are more affected than others, depending on the working conditions, but the common factor associated with these problems is characterized by repetitive manual activities requiring the use of strength.
The specific signs and symptoms of individual wrist injuries depend on the specific problem, but pain is very common. One of the most famous is CTS, which usually causes a pins-and-needles feeling in the thumb and index and middle fingers, providing clues on the compression of the median nerve. Other symptoms include inability to move the wrist through its full range of motion, wrist stiffness, trouble in gripping objects, swelling, numbness, and tingling.
Knowing that, for designing such exoskeleton which allows that movements by transferring a proper assistive force during handling activities, several other factors, which will be described in the following chapter, have to be selected.
4. Design Requirements for Wrist Exoskeletons
The requirements in
Figure 7, and proposed hereafter, are is not intended to be exhaustive nor are they limited to only wrist exoskeletons, although that is the focus of this paper.
4.1. Purpose
The “purpose” criterion, as shown in
Figure 8, refers to the target objective of the device and knowledge of the end users [
19]. This is the starting point from which the device design should flow and begins with identification of intended application domain (e.g., healthcare, manufacturing, construction, agriculture, logistics and transport, consumers, etc.). It is important at this early stage that users (companies, hospitals, or research institutes) are fully involved in the design specification to ensure that the designers have a clear focus on real needs and user requirements/expectations. This should be a fully interactive and iterative process that values and prioritizes the input from stakeholders and potential customers on the product feasibility, design proof of concept and choices, and users’ needs and expectations. In parallel with the sector definition and user requirements and expectation assessment, it is vital to identify the targeted condition that the device aims to help (e.g., recovery of motor deficit, assistance during ADL tasks, strength augmentation, lowering fatigue at work, injury prevention, etc.). This entails close study (again involving active interaction with the users) of all details of the tasks (e.g., lifting and transporting loads, maintaining awkward postures or holding a static position, hand screwing or use of tools such as screwdrivers, etc.). It is particularly important to emphasize the key role played by the stakeholders and users who can help to identify critical case studies.
4.2. Kinematic Compliance
In case of wearable devices, the kinematic compliance deals with the design characteristics a robot should have to comply with the movements, DoF and RoM of a human, as schematised in
Figure 9. Often when designing human–robot interfaces there is the tendency to represent human limbs as a serial chain of rigid links linked by joints that can broadly be imitated through knowledge of RoM and DoF. However, as noted when considering the anatomy of the wrist, it is clear that the kinematics of human joints is often much more complex than single DoF or even multiple DoF robot joints. They have more DoF than they need to move in a three dimensional space [
12]. So, to be kinematically compliant with the human limb to which exoskeletons are attached, it is necessary to choose a combination of joints and DoFs to achieve a desired task. In particular, every anatomical joint involves a combination of rotational and translational movements since the instantaneous center of rotation (ICR) of human joints is not fixed in a specific position but migrates. Therefore, it has to be taken into account by designing kinematic chains with rotational and translational joints, both active and passive, which can help to compensate for constrained displacements between the device and the human limb. Note that kinematic mismatch could hinder human movement and give rise to discomfort and undesired forces at the human–robot interface [
12]. Some tips for the design of exoskeletons, reported in [
12], are that the device should be easily worn, suitable for people of different sizes, comfortable, lightweight, should never have more than six DoFs between two consecutive attachments, and does not need to copy exactly the kinematic structure of the human limb.
From the human wrist kinematic perspective, the device should support the main wrist movements (flexion/extension and radial/ulnar deviation [
46]. One of the most interesting movements to be actuated would be the DTM since it is the most complete and natural for the human wrist, but few examples of this format exist in the literature [
39], maybe because the choice and positioning of appropriate joints and links could be enough to guarantee a wrist natural movement. However, sometimes this leads to complex and bulky devices.
The development of devices which provide wrist assistance along the DTM, for both health care and occupational applications, seems to be a more promising line of development since, in the former case, it would allow a more rapid recovery from injuries or surgery intervention as mobilization through the DTM plane may be considered more stable and controllable [
35,
37,
40], while for the latter, it would follow the movement of the wrist in a more natural through a less complex kinematic architecture. From the occupational perspective, the DTM plane has been investigated as one of the major sources of hand osteoarthritis (OA), CTS, and ulnar impaction syndrome. A recent analysis of wrist injuries by Park et al. [
28], which was conducted on Korean fishermen, reported that oyster shuckers perform tasks which have been classified as a basic risk factor for wrist and hand musculoskeletal disorders (MSD) due to the performance of hand-bearing tasks that use repetitive or improper postures while simultaneously applying power. That study noted that during oyster shucker’s work, the hand holding the knife and applying force moves repeatedly along the
dart throwing motion plane, as shown in
Figure 10.
For RoM, this is strictly dependant on the type of activities to be performed. Even if the human wrist RoM is well known, not all its workspace would be covered during manual handling activities. For safety reasons, it is highly recommended that motions at, or near, the endpoints are avoided to prevent problems such as hyper-extension or hyper-flexion.
4.3. Dynamics (Forces and Torques)
When designing exoskeletons in general, it is important to take into account how much force you need to apply to assist the human limb when performing a certain task, in which directions and with which intensity, as schematised in
Figure 11. The same assumptions are also valuable for wrist exoskeletons and depend on the specific activity you should perform. Several researchers have studied this topic [
43,
46].
For a healthy wrist, without external loads, the maximum exercisable torque in ADL is 6–10 Nm for pronation/supination, 8–14 Nm for flexion/extension [
33,
47], and the average estimated for radial/ulnar deviation is 1.3 Nm [
48]. In general males exert larger torque than females. It has also been experimentally determined that healthy males exert naturally an average maximum grip force of 311 N (SD = 80), while females exert 192 N (SD = 47) [
47]. However, the maximum prehension force required in daily activities is almost 70 N [
49,
50]. Note that the grip force almost changes linearly as the wrist angles change [
47].
For rehabilitation purposes, since patients often have impairments, muscular spasticity, bone weaknesses, etc., it is better to apply lower torque values to avoid worsening medical conditions. Therapists and researchers indicate that, to complete rehabilitation therapy successfully, the required torque for flexion/extension should be greater than 0.35 Nm (minimum requirement of wrist torque during ADL) but not exceeding 1.5 Nm [
39,
51,
52,
53] while not exceeding 0.5 Nm in radial/ulnar deviation [
34].
In the occupational sector, the situation may change due to different workloads for different activities. In these cases higher torques are required to lower muscular fatigue. Juul-Kristensenet et al. [
29] reported that for manual deboning of poultry, the muscular activities of the arm measured using electromyographic (EMG) signals could be estimated to have a median level of 6.25 N and a peak level of 20.71 N at the wrist during cutting, with a maximum hand grip force of 107.91 N (almost 11 kg) [
29].
In general, 3 kg is considered the weight above which loads have the potential to cause a risk of injury for manual handling activities (further details are provided in
Section 4.6). Usually, a torque equal to or greater than 3 Nm provides adequate assistance at the wrist while lifting 3 kg of load [
54] placed in the palm 0.1 m far from the joint. However this supported should be increased with the load and distance. Suggested values of torque depending on the application are shown in
Figure 12. These values match Hope and McDaid [
55] and suggest that typical maximum torque values for each DoF in a healthy wrist are 20 Nm (for flexion/extension and radial/ulnar deviation) and 9 Nm (for pronation/supination) when maintaining the wrist in a static position, 9 Nm (for flexion/extension and radial/ulnar deviation), and 7 Nm (for pronation/supination) when moving the wrist at a constant speed of 90°/s, while the values are 0.21 Nm (for flexion/extension), 0.25 Nm (for radial/ulnar deviation), and 0.72 Nm (for prontation and supination) when performing ADL.
4.4. Rigidity
Referring to [
19], the rigidity criterion is mainly related to the stiffness of the device and, in particular, the stiffness of the materials of the parts which form the exoskeleton structure and provide the required torques and forces. This characteristic can sub-group robotic devices into rigid, soft, or hybrid, as shown in
Figure 13.
A device can be considered rigid if, at the interface between the device and the user, it is mostly composed of hard and stiff materials.
A device is
soft if its human–robot interfaces are composed of soft and compliant materials such as foam, rubber, or silicon. This has the advantage of not hindering the natural movement of joints and can solve the kinematics problems of joint axis mismatch between the robot and the human. Some exoskeletons are often made rigid to provide high transmission efficiency and controllability [
57,
58,
59,
60,
61,
62], while others adopt soft mobile parts to better adapt to humans [
39,
48,
54,
56,
63,
64,
65,
66,
67,
68,
69,
70,
71].
Softness is closely associated with comfort and ergonomic devices since hard components, such as battery casings and actuation units, can be placed remotely from the affected joint. This relieves the user from bearing localized weights and encumbrance. However, controllability, reliability, and power transmission efficiency become more challenging.
In all cases, special emphasis has to be put on the parts directly attached to the human body because they need to be rigid to properly transfer the assistive torque or force. They have to be designed in such a way to mitigate medical issues due to long-term pressure points caused by shear forces and tight anchor sites on the body. Hence,
hybrid/compliant devices are increasingly seen as a good compromise between totally rigid or soft [
34,
52,
53,
72,
73,
74].
4.5. Ergonomics
Wearable devices should optimize, where possible, ergonomics, making the device easy to wear, tailored, customizable, lightweight, and safe, as schematised in
Figure 14.
To achieve this, any ergonomic wearable robot must address human kinematics compliance. As stated before, this starts with a proper choice of the type and number of DoFs (both active and passive) and of their placement. In a recent development, to make parts that are well tailored to the users’ limbs, 3D scanner technologies have been considered a reliable and increasingly common approach [
54,
75]. Scan data are useful since they provide information on the shape, size, and metrics of a real object. In fact, using these data, it is possible to directly make a CAD model of human limbs such as a hand, wrist, arm, head, trunk, lower limbs, etc. In addition, it is possible to trace their shapes and design mechanical parts or garments where forces and torques should be applied.
In any wearable device, being lightweight is a must. To distribute the weights and reduce the inertia of mechanical components, one solution is to design parts that wrap around the limb following the longitudinal axis (in direction of the limb) rather than being perpendicular to the axis.
An additional solution to reduce weight is in the placement of the actuation. Remote actuation moves the actuators from the actuated joints/limbs, locally lowering and better distributing the weights and pressure points on the human body; however, implementation is not always easy. Although the use of rigid parts provides a stable platform to accurately and repeatedly apply forces and torques, the use of soft materials, textiles, and foams is highly recommended, whenever possible, especially on human–robot interfaces or as a coating for rigid parts, as it increases both comfort and safety.
Since one of the major limitations in developing wearable technology is the acceptance of the wearers, a human-centered approach is vital. Acceptance is a condition of the human psyche with various different meanings depending on the context. Regarding technological advances, there are several different models [
76]. Although these are based on different hypotheses, they share the assumption that users’ acceptance is influenced by several factors which predict the intention to use new technology. Among those factors are perceived usefulness, effort expectancy (or perceived ease-of-use), performance expectancy, social influence, and facilitating conditions which determine the self-predicted future usage. These are further influenced by moderating variables such as gender, age, experience and voluntariness of use [
76]. To improve the quality of exoskeletons and accelerate their adoption in real scenarios, these acceptance factors must be considered from the earliest stages of the design. An example is proposed by
Collinder and
Ekstrand [
77], where they investigated risks of hand injuries in automobile manufacturing plants with a predictive assessment of hand ergonomics in early stages of production, providing explanations for the increase in injuries among operators and recommendations that could improve the design process of specific tasks where hand ergonomics are compromised.
A better understanding of the factors that prevent the widespread use of some types of exoskeletons could help to speed up their adoption, reducing both industrial and societal skepticism [
76].
4.6. Safety
As exoskeletons are physically attached to the user, safety is a paramount consideration. Since exoskeletons have both hardware and software elements, as shown in
Figure 15, it is vital to fully consider different levels of safety for the 1—mechanical; 2—electrical; and 3—software systems [
20]. Safety precautions in the mechanical design consist of physical stops to prevent segments from excessive excursions and from causing harm to the user (e.g., cover forbidden spaces of the robot, cover empty or open spaces at joints to avoid injuring human skin while moving or pinching fingers, avoid floating cables). The electrical system should be equipped with different emergency shutoff switches (e.g., emergency button) to stop and release motor commands when something goes wrong. The software should have multiple control routines which check sensor status, joint angles, and joint torques to prevent sudden unexpected motion and by limiting maximum torque and velocity. It is something overlooked that also the software architecture must cover specific characteristics which are prescribed in standards [
16,
20].
Safety requirements are important commercialization issues possibly preventing certification. In this respect, it is important to more clearly define the purpose and application domain of since medical and non-medical exoskeletons have their own regulatory requirements. Assistive exoskeletons for workers and healthy people with or without reduced physical capabilities (e.g., elderly people) are considered
machines, and they must comply with EC Machine Directive 2006/42/EC and ISO 12100:2010 [
16]. Exoskeletons used by disabled people who have lost some functionalities or for rehabilitation purposes are considered
medical devices, and they must comply with EC Medical Directive 93/42/EEC and IEC 60601 [
16]. Furthermore, for every electrical/electronic apparatus (including exoskeletons), Electromagnetic Compatibility (EMC) Directive 2014/30/EU must be observed [
16].
Although countries may have their own national regulations, general market rules are usually driven by international standards such as ISO and IEC (or EN standards), and this provide manufacturers with a legal presumption of conformity almost everywhere. For wrist exoskeletons in a working environment, the most pertinent safety and ergonomic considerations are regulations for manual handling of loads activities (ISO 11228, [
78]) and the assessment of static working postures (ISO 11226).
ISO 11228-1 is related to lifting, lowering, and carrying of loads with a mass of 3 kg or more, and to moderate walking speed, i.e., 0.5 m/s to 1.0 m/s on a horizontal level surface. This is based on working periods of 8–12 h. It covers moderate and high loads since 3 kg is considered the weight above which loads are considered a risk of injury for manual handling activities; 15 kg and 20 kg are considered the limiting weights which should not be exceeded for women and men, respectively. For weights between 3 and 15 kg, these should be handled with some precautions and under particular conditions (e.g., height from ground, shape of the object, number of repetitions per minute, the speed of the movement, the posture, the use of force, the presence of regular breaks, etc.) [
78]. In particular, for the wrist, ISO 11228-1 states that the ideal condition for lifting loads consists in a firm grip with neutral wrist posture, avoiding extreme deviations from the neutral position [
78].
ISO 11228-3 addresses handling of low loads at high frequency. Low loads are considered to be below 3 kg. In this range, musculoskeletal problems are mainly caused by the repetitiveness and speed of the task rather than the weight. As shown in
Figure 16, awkward postures are those that cause a wrist at flexion > 45°, extension > 45°, ulnar deviation > 20°, radial deviation > 15° [
79], as experimentally measured by Marras et al. in [
80]. Wrist flexion causes increased pressure in its deep structures (carpal tunnel), and this pressure increases if incorrect and forceful gripping force is exerted simultaneously. Hence, this risk addresses the question: “
is the force used lower than that needed to handle 200 g with the fingers (e.g., pinching) or 2 kg with the whole hand (e.g., gripping)?” [
79].
Markers which should be taken into account for a correct risk assessment in working environments are
repetitiveness,
use of strength,
incongruous posture, and
repeated impacts [
79], as shown in
Figure 17.
These regulations provide a guide for risk injury assessment, with advice on the design and redesign of the working activities and the workplace. It considers a wide range of pertinent variables and factors. In each of these standards, there are several methods of injury risk assessment. OCRA (occupational repetitive actions) and HAL (hand activity level) are two of the quantitative methods used for the risk assessment of the wrist. OCRA is the most common and uses the OCRA index to evaluate each risk factor (repetitiveness, posture, strength, recovery, etc.) and then relates this to the frequency of specific movements actually being performed. The risk is then assessed as absent, low, or critical [
78,
79].
Before any machine can be placed on the market, manufacturers must compile a fully detailed technical report (TR) describing each aspect of the machine, with drawings, calculation notes, risk assessment, instructions, standards used, and EC declaration of conformity.
Due to all of these considerations, there is a significant gap between research and commercialization.
5. Design Architecture
Requirements, described in the previous sections, lead the design. In this section, a classification criteria, based on technical characteristics, is proposed to gain a better understanding of available (and future) technologies for wrist-based robotic devices. This will pinpoint the leading approaches and identify gaps in the state of the art. Six key characterization criteria have been identified:
actuation type,
portability,
power source,
power transmission,
sensing, and
control architecture. As shown in
Figure 18, these classes can be further sub-divided to create the full characterization of the device. In the following section, a brief description of all these classes will be provided, focusing only on the technologies already implemented in wearable wrist exoskeletons. For more general details for all exoskeletons, see [
1,
12,
13,
16,
18,
19,
20].
5.1. Actuation Type
This is the most common classification for all types of exoskeletons.
As schematised in
Figure 19, a
passive system includes parts that store potential energy (such as springs or any elastic material, linkages, and dampers) and has no external power source. Their use is mainly for weight re-distribution by transferring the load from the affected limb or joint; as energy store-and-release systems to support the affected limb or joint or as a “spring-dynamo” design, to recharge batteries; and as dampers to absorb shocks or vibrations [
1,
13,
18]. Examples of these devices are reported in [
53,
57,
62,
65,
73,
81,
82].
In rehabilitation, these systems are designed to assist the patient in the latter stages of training to strengthen their motor skills and muscles. They are made to be lightweight, compact, and easy to manage to provide continuing rehabilitation at home or in any non-clinical environments. In the occupational sector, the main purpose is to transfer the load from the affected limb/joint to different body parts, reducing muscle fatigue.
An
active system, as schematised in
Figure 19, has joints and links that are driven by any external source, which could be electric motors, hydraulics, pneumatics, levers, or a grouping of different technologies. They rely on sensors, control units, and power supplies to function and provide assistive torque to the limb. Hence, active exoskeletons are more complex than passive ones [
1,
13,
18]. Examples of these devices are reported in [
34,
39,
48,
52,
54,
56,
58,
59,
60,
61,
62,
63,
64,
66,
67,
68,
69,
70,
71,
72,
74,
83,
84,
85].
Sometimes, it is also possible to combine both solutions leading to
quasi-passive devices [
1,
13].
Historically, due to their light weight, cost-effectiveness, compactness, and good power-to-weight ratio, passive exoskeletons have been preferred by companies and workers. However, they provide less assistance than the active devices, and this is crucial in some specific tasks or where high dynamics are required (e.g., screwing, cutting, knitting). Furthermore, they hinder some movements due to their intrinsic stiffness, which cannot be removed, whereas in active exoskeletons, transparency and backdrivability working modes can overcome these hindrances.
5.2. Portability
The portability requirement should answer the question: is the device designed for fixed use or free movement?
Portability essentially means a device can be easily worn and transported by a user and is crucial to this is the application domain for which the device is intended.
Fixed devices are physically grounded structures that cannot be fully worn and transported by the user.
Understanding this distinction is very important in appreciating wrist exoskeleton design and operation.
The first wrist exoskeletons were fixed devices designed solely for rehabilitation and training in clinics, as shown in
Figure 20a.
With increasing life expectancy and aging populations, there is greater need for home-based rehabilitation and particularly systems that operate without caregiver assistance. Researchers have started to design wrist exoskeletons to address this medical need. Several devices have been designed as wearable and portable to guarantee freedom of movement for the patient while performing rehabilitation activities, as shown in
Figure 20b.
Moreover, because of the increase in WMSDs, there has been an emerging interest in transferring the knowledge acquired in designing wearable and portable wrist rehabilitation exoskeletons to the occupational domain, as with that shown in
Figure 20c. However, the majority of these devices are still in a prototype phase due to even more design difficulties respect to rehabilitation devices. A few examples are available in [
54,
64,
65,
85].
5.3. Power Source
Various actuating methods have been explored for active wrist exoskeletons, including electric motors, pneumatics, thermal energy (shape memory alloy—SMA),
Figure 21.
Actuation using
electric motors is the most common method. There are many examples in the literature of wrist exoskeletons powered by DC motors, brushless DC motors, linear actuators, and servo motors [
39,
52,
54,
59,
60,
61,
62,
64,
67,
72,
74,
83,
84,
85]. Electric motors in general are preferred for their simplicity, controllability, repeatability, costs, and backdrivability. However, low cost is not always true, and backdrivaility usually needs active control, e.g., for DC motors with high reduction ratios or in linear motors which use lead screws to convert the rotational motion into linear action. Moreover, electric motors can be relatively heavy, noisy, and large and can require careful maintenance, introducing difficulties in their integration into wearable devices.
Pneumatic actuation relies on the use of compressed air to apply the required force/torque. Various methods have been developed to generate the ROM and proper torque assistance, including the use of inflatable flexible materials [
48], bellow-shaped systems [
71], or artificial muscles [
56,
66,
70]. The actuators are commonly sited on the dorsal side of the palm of the hand and/or on the forearm. They have mostly been tested in rehabilitation and training, but the high power-to-weight ratio is promising also for augmentation and assistance purposes. The inherent compliance makes these devices safer for human–robot interactions. However, their use in wearable applications is challenging since pneumatic systems need a portable compressed air supply or the capability of generating compressed air. This can make the overall device bulky and heavy due to the need for compressors, storage tanks, valves, air tubes, etc. [
18].
Hydraulics has an actuation system similar to that of pneumatics but relies on liquids rather than air. There are no examples of its application for wearable wrist exoskeletons, probably due to complexity, weights, and encumbrances that are even greater than with pneumatic technology. Additionally, the extremely high power generated by hydraulic systems and the inherent dangers of the compressed fluids are not well suited to devices in direct contact with the user.
Thermal power sources are used by shape memory alloy (SMA) actuators that have been explored by [
34,
55,
68,
69] for wrist applications. These systems work on the principle of material deformation (contraction and expansion) due to heating and cooling at certain phase transition temperatures. Usually the device is in the form of metallic alloy rods or wires. Heat is generated by the Joule effect. This actuation method has a high power-to-weight ratio, but its behavior is highly nonlinear. Furthermore, the heat produced during operation is high and may compromise the user safety [
18].
The search for an ideal actuator is still open, and on-going research in this area could pave the way for better and more efficient design solutions, which could be accepted more easily by users, speeding up the introduction into the market of novel wrist exoskeletons.
5.4. Power Transmission
Power transmission is how the power generated by the actuation source is transmitted to the relevant joint in the form of forces or torques. In wearable devices and wrist exoskeletons, various methods have been explored involving rigid structures, cables, or compliant elements, as shown in
Figure 22.
Rigid structures include direct drive, mechanical links, or gears [
34,
52,
59,
60,
61,
62]. These are the simplest and most reliable ways of transferring power to the joint. Direct drive consists of a motor directly connected to the actuated joint so that efficiency losses are minimized. It reduces the complexity of the actuation system, improves portability, and facilitates integration into wearable devices since it is mounted close to the limb or joint. However, it increases the overall weight and encumbrance, possibly causing discomfort on the user. Moreover, one actuator per DoF should be implemented for actuating multi-DoF systems, further increasing the overall complexity. No examples are available in the literature for wearable wrist exoskeletons which involve a direct drive. Mechanical links and gears are widely used to solve the problem of maintaining a portable system which fits multi-DoF by adopting fewer actuators than DoF (under-actuation). These actuators could be placed remotely and through a series of mechanical linkages and gears, and the motion can be transferred to the required joint. However, this increases the complexity of the system and its maintenance due to the increase in the number of mechanical components, but the major drawback is the axis mismatch with the bio-mechanical joint, which may cause discomfort.
Cable transmission includes Bowden cable devices and tendon-driven devices. Examples of these types of transmission can be found in [
39,
53,
54,
64,
67,
72,
74,
83,
84,
85]. Bowden cables are usually steel cables routed in a teflon tube, while tendons are cables (e.g., Dyneema wires) which could be easily flexed without any external sleeve and which tend to mimic human muscle anatomy. They usually rely on tendon-pulley driven mechanisms to generate the required torque. Examples can be found in [
54,
64,
72,
74]. Because cables can only be pulled, one cable can execute a single function (e.g., flexion or extension), and thus this type of transmission is normally unidirectional. Two cables should be used to give antagonistic actuation. Cable transmission suffers from breakage, friction, and backlash, which are difficult to control and affect transmission efficiency, causing losses. However, inertia is reduced locally on the affected limb.
Compliant mechanisms include springs, artificial muscles, and flexible joint-less structures [
48,
53,
56,
66,
68,
69,
70,
71,
81,
82]. Artificial muscles (e.g., Mckibben actuators) are made of a flexible material surrounded by a braided sheath that contracts or elongates when inflated using compressed air (pneumatics) or occasionally liquids (hydraulics). Their major drawback is the ballooning effect happening when the material cannot extend or contract anymore because the increase in fluid pressure is too high. This may lead to a subsequent explosion and breakage of the device, with possible damage to the user. Flexible jointless structures, contrary to artificial muscles, are made from silicone rubber molded in a specific shape which allows them to bend along a certain direction and does not require any braided sheath. Examples of these are soft origami actuators (SOA). Compliant mechanisms have the advantage of being lightweight and comfortable, allowing remote placement of the actuation unit, but their control and reliability are difficult.
5.5. Sensing
This functionality consists in using sensors placed in various parts of the exoskeleton structure or the human body to provide feedback to exoskeleton control system. It is strictly necessary for all devices to work properly. In wrist exoskeletons, the key sensing parameters are position, force/torque, and bio-signals; see
Figure 23.
For
position detection, various sensors have been used, such us encoders, potentiometers, inertial magnetic units (IMU), 3D motion-capture sensors, and flex sensors [
34,
39,
48,
53,
54,
59,
61,
67,
68,
69,
70,
71,
72,
74].
These data are vital in ensuring accurate, safe control of the exoskeleton. Encoders (optical or magnetic), integrated in electric motors, are used to track the angular velocity and position. Potentiometers are used to detect joint position by mounting them directly on the linkages of the exoskeleton structure. IMUs are a high accuracy sensor that provides information about angular position, velocity, and acceleration of a physical part in motion. They are widely used to detect the relative position of the human wrist while moving with respect to the forearm. Flex sensors could be also used but their application is not so common and they are less accurate than the others.
Since manual activities require handling of objects which differ in shape, size, and weight,
force/torque detection is very important to provide the required level of assistance when needed. In wearable wrist exoskeletons, force/torque is generally sensed using load cells, pressure sensors (also implemented in pneumatic or hydraulic circuits), or force resistive sensors (FSR) placed on the finger tips, on the hand (palm or back), or in contact with the object held or manipulated, e.g., [
48,
52,
56,
59,
62,
64,
66,
70,
71,
83,
84,
85].
Bio-signal detection is a way to detect the user’s intentions by measuring electrical activities from muscles or the brain. Depending on the field of application, these signals are measured to evaluate whether the human wrist is active or to observe the recovery of certain muscular functions. In wearable wrist exoskeletons, the main type of bio-signal detected is the surface electromyography signals (sEMG) from the muscles in the forearm. These signals can be used as feedback to control the exoskeleton by modulating the assistance provided or to observe the progress in the training, determining if the patient’s muscles are recovering and strengthening. Their use is challenging, especially in case of home rehabilitation without caregivers or occupational purposes, because users usually do not know how to handle them. These challenges include electrode cross-talk interference, environmental interference (e.g., electromagnetic noise, dirt, dust, etc.), placement issues, and sliding on the skin. They have to be placed directly in contact with the limb skin (e.g., forearm), every time in the same place for the best repeatability. Examples include [
56,
59,
60,
67].
In general, the majority of exoskeletons use more than one type of sensing to have better controllability and estimation of functional parameters and to improve redundancy.
5.6. Control Architecture
A review of the state of the art about control aspects in different wrist rehabilitation robotic devices has been proposed by Hussain et al. in [
23]. The control architecture relies on micro-controllers and algorithms to process sensory information and send commands to the actuation units to perform a desired function. It can be classified by the type of input signals processed, the control paradigm adopted for a specific task, or the control scheme used to process information and execute the tasks [
18]; see
Figure 24.
The
signals acquired are those described in
Section 5.5, but they are processed in different ways to generate the desired output signals. When
manually triggered by a user, for example by pressing a button, a device can execute a certain predefined task, such as flexing or extending the wrist. This is common for rehabilitation devices designed to repeatedly perform the same task, but it is not common in occupational environments where it is difficult to establish predefined movements due to the high variability and dynamics of the activities.
An interactive control mode uses position, force or sEMG signals, processed by algorithms and compared with predefined thresholds. This provides the requested assistance needed to help the user in manipulating objects.
Different types of control paradigms have been explored to address different tasks.
Continuous passive motion (CPM) is a widely used method for rehabilitation to help recover mobility at the initial stage of an injury and to prevent the development of stiffness in the affected joint. It ignores the intentions of the user and actuates the exoskeleton along a predefined trajectory [
18]. These trajectories are obtained from healthy subjects as well as from the literature. The drawbacks of this technique are that it does not consider the patient’s disability level, and thus it can create discomfort by preventing free motion for the patient [
23,
87].
With
active resistance, the exoskeleton applies a force/torque to resist the motion of the subject. It is mainly used in rehabilitation programs to enhance the training of the patient, for example, by controlling the force applied to the limb by setting the springs stiffness depending on the patient’s progress [
18].
To overcome the above mentioned limitations,
assist-as-needed (AAN) control can be implemented to provide customized assistance [
23,
87]. By continuously reading sensors signals, AAN can estimate the patient’s intent and modify accordingly the device assistance to enhance the patient’s participation. In the rehabilitation field it generates an increased level of recovery with respect to the CPM and active resistance, while in occupational tasks, it can lower the muscular fatigue by providing an appropriate level of assistance, but only when needed. AAN control is more compliant, natural, and comfortable than trajectory tracking control. However, CPM and AAN control strategies require predefined dynamics models to characterize the equations of motion of the user and the exoskeleton and determine the required torques. To avoid defining the dynamics of the system, researchers have been starting developing advanced machine learning techniques to predict users’ motion intention [
87,
88,
89].
Machine learning (ML) is a relatively new control paradigm for wrist exoskeletons. It involves in developing algorithms that are able to predict human motion patterns before being trained on measured clinical data of both healthy and injured patients. The use of this technique is becoming increasingly popular when used with sEMG signals to obtain specific muscular activation patterns that can predict which action a user is going to execute [
87,
88,
89].
All these strategies should be included in a control scheme inside the control architecture. Two control schemes have been implemented in exoskeletons in general: high-level and low-level control. High-level control interacts with the user and the environment through sensors. It processes information coming from the human–robot interaction, such as sEMG signals amplitude and/or position, force, impedance, and admittance of the affected joint. Then, looking at the actual state of these parameters, it establishes the necessary amount of assistance to be provided, and accordingly generates a reference command signal for the low-level controller. It is responsible for the extent and timing of the generated assistance.
Low-level control is usually a closed-loop on a reference parameter (e.g., force, torque, position, speed, etc.) to guarantee that each actuator properly tracks the reference signals coming from the high-level controller. It regulates and generates the output at the actuators based on that references [
18,
23]. Usually, the control scheme of a robotic device is structured on both these two levels, interconnected, with the goal of allowing the user to move freely and experience assistance with appropriate timing and extent.
6. Discussion and Conclusions
Exoskeletons are robotic devices which aim to help both healthy and unhealthy people in performing activities or to assist recovery of some or all of their natural movements.
In the part I of this study, a comprehensive analysis has been conducted by exploring the current state of the art of wearable and portable wrist exoskeletons since the 2000s.
This paper aims to identify:
The main important aspects of wrist bio-mechanics and common wrist injuries.
Design requirements to be fulfilled.
Existing design architectures and technologies.
This will provide expert guidance on how to orient the design, which technologies can be implemented or improved, and how much remains to be explored in wearable wrist exoskeletons.
The wrist is one of the most anatomically complex joints in the body due to its very small and compact size, its great mobility, and need to provide support for significant forces. It is able to move in a 3D space with very complex kinematics and dynamics. However, excessive strain on this joint, due to repeated manual handling activities, increases the possibility of incurring injuries (e.g., CTS, tendinitis, tenosynovitis). Such knowledge is necessary to define the requirements and design challenges of a wrist exoskeleton.
The requirements define the specifications which should be satisfied by the design architecture and should include:
Purpose: what task a device is intended to perform and what is based on the application domain (e.g., healthcare, manufacturing, construction, agriculture, logistics and transport, consumer, etc.), the target condition (e.g., recovery of motor deficit, assistance during ADL, strength augmentation, lowering fatigue at work), and the current technology readiness level (TRL).
Kinematics: this refers to the kinematics compliance of the limb to which the exoskeletons are attached and considers the number of DoFs, the RoM which should be achieved, and the types of joints selected to guarantee those DoFs and RoMs (e.g., rotational, translational, cylindrical, spherical).
Dynamics: addresses the forces and torques to be experienced and applied. Usually, torques for rehabilitation and training are between 0.3 Nm and 3 Nm, while for occupational purposes, torques vary from 0.3 to 20 Nm depending on the task and application.
Rigidity: the stiffness of the materials used to fabricate the components in the exoskeleton structure and provide the required torques and forces. They can be classified as rigid, soft, or hybrid.
Ergonomics: refers to the design of the device which should be easy to wear and use, tailored, customizable, lightweight, perceived as useful, able to guarantee a real improvement in the user’s condition and safe.
Safety: focuses on all the precautions taken to prevent causing harm to the user, other people, and the operational environment. It includes both hardware and software elements (mechanical, electrical, electronics, and software components). Safety requirements are vital when involving humans and the environment, also being an important commercialization issue. If not satisfied according to international or European regulations, a product cannot be sold.
Hardware designs of wrist exoskeleton can be classified according to the actuation type, power source, power transmission methods, sensing and control strategy. Based on these, a macroscopic categorization of wearable and portable wrist exoskeletons can be produced; see
Figure 25 and
Figure 26.
A first distinction between passive and active exoskeletons, in
Figure 25, shows that there are more active wrist exoskeletons than passive ones. Although passive devices are, in general, preferred because of the light weight, safety, and simplicity, active systems do bring significant advantages such as applying higher forces/torques, ensuring a wider application area, and being much more operationally flexible due to being programmable for different tasks and sub-tasks.
Usually, passive exoskeletons are driven by springs storing potential energy, while active ones use different sources of power: electrical, pneumatic, and thermal. Electrical motors are usually preferred due to their robust controllability, great power-to-weight ratio, weight, and price. However, the actuation technology is a huge field yet to be investigated for wearable wrist exoskeletons. It should be improved to develop miniaturized drives that are more durable and have higher performance. Moreover, noise and bulkiness influence negatively the user’s acceptance.
In terms of power transmission, some systems are rigid, with linkages and gears, for better reliability in motion control and force/torque transmission. However, because of the potential application in daily activities, often soft or compliant devices are preferred due to their inherent compliance, which makes them more comfortable, lighter, safer, and able to overcome axis mismatch. Furthermore, with soft or compliant devices, generally the actuation unit can be placed remotely, permitting localized weight and space-saving at the wrist joint.
The sensing and control paradigms are of great importance for wearable robotic devices. Their choice so often depends on the application and final goal. Controllers can be designed to exert predefined trajectories and forces/torques (CPM strategy) on a passive user or provide assistance only when needed (AAN). The former are mainly conceived for recovery of natural motion and strength capabilities in rehabilitation protocols, while the latter have broader applications due to the higher flexibility and adaptability to the user.
Alongside classical rigid and robust sensors (such as IMU, encoders, load cells) for position and force control, bio-signals have been gaining great attention. EMG signals have been used as inputs to the controller of power-assisted exoskeletons. The device can then be controlled based on the user motion intention by measuring the human muscular activation. To process this information, sophisticated machine learning algorithms have been developed. This could remove or reduce the use of classical rigid sensors, making the whole device more compliant. Nevertheless, bio-signal implementation in wearable devices is challenging especially for occupational or outdoor environments since their accuracy is effected by external disturbances and signals can only be measured directly on the human skin.
It is not easy to design wrist exoskeletons, especially for the requirements and specifications needed in certain applications. Most of devices cited in this paper are still under development, with promising practical outcomes, only tested and used in a laboratory setting. Significant further research and development are needed in every field.
Author Contributions
Conceptualization, R.F.P., D.P., G.B. and J.O.; methodology, R.F.P., D.P., G.B. and J.O.; formal analysis, R.F.P. and D.P.; investigation, R.F.P.; resources, R.F.P.; writing—original draft preparation, R.F.P.; writing—review and editing, R.F.P., D.P., D.G.C., G.B. and J.O.; visualization, D.P., D.G.C., G.B. and J.O.; supervision, D.P., D.G.C., G.B. and J.O.; project administration, D.G.C. and J.O.; funding acquisition, D.G.C. and J.O. All authors have read and agreed to the published version of the manuscript.
Funding
This work is funded by the Italian Workers’ Compensation Authority (INAIL).
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the pure use of literature to obtain the results.
Informed Consent Statement
Not applicable since this study did not involve humans.
Data Availability Statement
Data sharing is not applicable to this review paper. No new data were created in this study.
Acknowledgments
Our thanks go to INAIL (Italian Worker’s Compensation Authority) for its ongoing support, collaboration, and funding in the development of novel types of industrial exoskeletons under the project Collaborative Exoskeletons-EC-2 in collaboration with Istituto Italiano di Tecnologia (IIT) and the University of Genoa.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MSD | Musculoskeletal Disorder |
| WRMSD | Work-Related Musculoskeletal Disorder |
| WHO | World Health Organization |
| INAIL | Italian’s Workers Compensatory Authority |
| DARPA | Defense Advanced Research Projects Agency |
| OE | Occupational Exoskeletons |
| CTS | Carpal Tunnel Syndrome |
| DoF | Degree of Freedom |
| RoM | Range of Motion |
| CoR | left of Rotation |
| ADL | Activities of Daily Living |
| DTM | Dart Throwing Motion |
| TRL | Technology Readiness Level |
| ICR | Instantaneous Centre of Rotation |
| OA | Hand Osteoarthritis |
| SD | Standard Deviation |
| OCRA | Occupational Repetitive Actions |
| HAL | Hand Activity Level |
| TR | Technical Report |
| IMU | Inertial Magnetic Unit |
| FSR | Force Resistive Sensor |
| sEMG | Surface Electromyography Signals |
| CPM | Continuous Passive Motion |
| AAN | Assist-As-Needed |
| ML | Machine Learning |
| WearRA | Wearable Robotics Association |
| SEM | Soft Extra Muscle |
| SCI | Spinal Cord Injury |
| EU-MDR | European Medical Device Regulation |
| JAS | Joint Active Systems Inc. |
| PWE | Portable Wrist Exoskeleton |
| NN | Neural Network |
| SVM | Support Vector Machine |
| FMG | Force-Myography Signal |
| CIMT | Constraint-Induced Movement Therapy |
| MVC | Maximum Voluntary Contraction |
| SOA | Soft Origami Actuator |
| PMA | Pneumatic Muscle Actuator |
| SMA | Shape Memory Alloy |
| SWA | Soft Wrist Assist |
| RMSE | Root Means Squared Error |
References
- Nikhil, G.; Yedukondalu, G.; Rao, S. Robotic exoskeletons: A review on development. Int. J. Mech. Prod. Eng. Res. Dev. 2019, 9, 529–542. Available online: https://archive.org/details/52.ijmperdaug201952 (accessed on 13 December 2022).
- Sylla, N.; Bonnet, V.; Colledani, F.; Fraisse, P. Ergonomic contribution of ABLE exoskeleton in automotive industry. Int. J. Ind. Ergon. 2014, 44, 475–481. [Google Scholar] [CrossRef]
- Voilqué, A.; Masood, J.; Fauroux, J.; Sabourin, L.; Guezet, O. Industrial exoskeleton technology: Classification, structural analysis, and structural complexity indicator. In Proceedings of the 2019 Wearable Robotics Association Conference (WearRAcon), Scottsdale, AZ, USA, 25–27 March 2019; pp. 13–20. [Google Scholar]
- HSE-Health and Safety Executive of Britain. Work-Related Musculoskeletal Disorders Statistics in Great Britain. 2021. Available online: https://www.hse.gov.uk/statistics/fatals.htm (accessed on 6 January 2022).
- European Agency for Safety and Health at Work (EU-OSHA). Working with Chronic Musculoskeletal Disorders. 2020. Available online: https://www.healthy-workplaces.eu (accessed on 6 January 2022).
- European Agency for Safety and Health at Work (EU-OSHA). Work-Related Musculoskeletal Disorders—Facts and Figures; Standard, European Agency for Safety and Health atWork (EU-OSHA); Publications Office of the European Union: Luxembourg, 2020. [Google Scholar] [CrossRef]
- Ramazzini, B. De morbis artificum diatriba [diseases of workers]. Am. J. Public Health 2001, 91, 1380–1382. [Google Scholar] [CrossRef] [PubMed]
- Franco, G.; Franco, F. Bernardino Ramazzini: The father of occupational medicine. Am. J. Public Health 2001, 91, 1382. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.J.; Fine, L.J.; Goldstein, S.A.; Lifshitz, Y.R.; Silverstein, B.A. Ergonomics considerations in hand and wrist tendinitis. J. Hand Surg. 1987, 12, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Sluiter, J.K.; Rest, K.M.; Frings-Dresen, M.H. Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scand. J. Work. Environ. Health 2001, 27, 1–102. Available online: http://www.jstor.org/stable/40967163 (accessed on 31 March 2022). [CrossRef] [Green Version]
- INAIL-Italian Workers’ Compensatory Authority. Occupational Exoskeletons: Wearable Robotic Devices to Prevent Work Related Musculoskeletal Disorders in the Workplace of the Future. 2020. Available online: https://osha.europa.eu/en/publications/occupational-exoskeletons-wearable-robotic-devices-and-preventing-work-related (accessed on 1 November 2021).
- Pons, J.L. Wearable Robots: Biomechatronic Exoskeletons; John Wiley & Sons: Hoboken, NJ, USA, 2008; ISBN 9780470512944. [Google Scholar]
- Crea, S.; Beckerle, P.; De Looze, M.; De Pauw, K.; Grazi, L.; Kermavnar, T.; Masood, J.; O’Sullivan, L.W.; Pacifico, I.; Rodriguez-Guerrero, C.; et al. Occupational exoskeletons: A roadmap toward large-scale adoption. Methodology and challenges of bringing exoskeletons to workplaces. Wearable Technol. 2021, 2, e11. [Google Scholar] [CrossRef]
- Marinov, B.; Dao, T. ExoskeletonReport. 2016. Available online: https://exoskeletonreport.com/ (accessed on 7 July 2022).
- Borislav, M. The Number of Companies Making Industrial Exoskeletons Has Been Quietly Increasing for The Past Five Years. 2020. Available online: https://www.forbes.com/sites/borislavmarinov/2020/09/24/the-number-of-companies-making-industrial-exoskeletons-has-been-quietly-increasing-for-the-past-five-years/?sh=231b1c067bf4 (accessed on 5 August 2022).
- Bai, S.; Virk, G.S.; Sugar, T.G. Wearable Exoskeleton Systems: Design, Control and Applications; Institution of Engineering and Technology: London, UK, 2018; ISBN 9781785613029. [Google Scholar]
- Borislav, M. Updated Directory of Exoskeleton Companies and Industry Statistics. 2021. Available online: https://exoskeletonreport.com/2021/12/updated-directory-of-exoskeleton-companies-and-industry-statistics/ (accessed on 5 August 2022).
- du Plessis, T.; Djouani, K.; Oosthuizen, C. Review of Active Hand Exoskeletons for Rehabilitation and Assistance. Robotics 2021, 10, 40. [Google Scholar] [CrossRef]
- Noronha, B.; Accoto, D. Exoskeletal devices for hand assistance and rehabilitation: A comprehensive analysis of state-of-the-art technologies. IEEE Trans. Med Robot. Bionics 2021, 3, 525–538. [Google Scholar] [CrossRef]
- Gopura, R.; Kiguchi, K. Mechanical designs of active upper-limb exoskeleton robots: State-of-the-art and design difficulties. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009; pp. 178–187. [Google Scholar] [CrossRef]
- Gopura, R.; Bandara, D.; Kiguchi, K.; Mann, G.K. Developments in hardware systems of active upper-limb exoskeleton robots: A review. Robot. Auton. Syst. 2016, 75, 203–220. [Google Scholar] [CrossRef]
- Tiboni, M.; Borboni, A.; Vérité, F.; Bregoli, C.; Amici, C. Sensors and actuation technologies in exoskeletons: A review. Sensors 2022, 22, 884. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Jamwal, P.K.; Van Vliet, P.; Ghayesh, M.H. State-of-the-art robotic devices for wrist rehabilitation: Design and control aspects. IEEE Trans. Hum. Mach. Syst. 2020, 50, 361–372. [Google Scholar] [CrossRef]
- Cornejo, J.; Huamanchahua, D.; Huamán-Vizconde, S.; Terrazas-Rodas, D.; Sierra-Huertas, J.; Janampa-Espinoza, A.; Gonzáles, J.; Cardona, M. Mechatronic exoskeleton systems for supporting the biomechanics of shoulder-elbow-wrist: An innovative review. In Proceedings of the 2021 IEEE International IOT, Electronics and Mechatronics Conference (IEMTRONICS), Toronto, ON, Canada, 21–24 April 2021; pp. 1–9. [Google Scholar] [CrossRef]
- Ferguson, R.; Riley, N.D.; Wijendra, A.; Thurley, N.; Carr, A.J. Wrist pain: A systematic review of prevalence and risk factors–what is the role of occupation and activity? BMC Musculoskelet. Disord. 2019, 20, 542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ambike, S.; Paclet, F.; Zatsiorsky, V.M.; Latash, M.L. Factors affecting grip force: Anatomy, mechanics, and referent configurations. Exp. Brain Res. 2014, 232, 1219–1231. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, H.; Cardoso, A.; Mattos, D.; Deola Borges, G.; Anacleto, P.; Colim, A.; Carneiro, P.; Arezes, P.M. Assessment of Work-Related Musculoskeletal Disorders by Observational Methods in Repetitive Tasks—A Systematic Review. Occup. Environ. Saf. Health III 2022, 406, 455–463. [Google Scholar] [CrossRef]
- Park, J.S.; Yoo, J.I.; Na, J.B.; Song, H.S. The prevalence and risk factors of musculoskeletal disorders in the hands of fishermen working as oyster shuckers. Int. J. Occup. Med. Environ. Health 2021, 34, 603–615. [Google Scholar] [CrossRef]
- Juul-Kristensen, B.; Fallentin, N.; Hansson, G.Å.; Madeleine, P.; Andersen, J.; Ekdahl, C. Physical workload during manual and mechanical deboning of poultry. Int. J. Ind. Ergon. 2002, 29, 107–115. [Google Scholar] [CrossRef]
- Youm, Y.; Flatt, A.E. Design of a total wrist prosthesis. Ann. Biomed. Eng. 1984, 12, 247–262. [Google Scholar] [CrossRef]
- Bajaj, N.M.; Spiers, A.J.; Dollar, A.M. State of the art in artificial wrists: A review of prosthetic and robotic wrist design. IEEE Trans. Robot. 2019, 35, 261–277. [Google Scholar] [CrossRef]
- Neu, C.; Crisco, J.J.; Wolfe, S. In vivo kinematic behavior of the radio-capitate joint during wrist flexion–extension and radio-ulnar deviation. J. Biomech. 2001, 34, 1429–1438. [Google Scholar] [CrossRef]
- Bajaj, N.M.; Spiers, A.J.; Dollar, A.M. State of the art in prosthetic wrists: Commercial and research devices. In Proceedings of the 2015 IEEE International Conference on Rehabilitation Robotics (ICORR), Singapore, 11–14 August 2015; pp. 331–338. [Google Scholar] [CrossRef]
- Serrano, D.; Copaci, D.S.; Moreno, L.; Blanco, D. SMA based wrist exoskeleton for rehabilitation therapy. In Proceedings of the 2018 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Madrid, Spain, 1–5 October 2018; pp. 2318–2323. [Google Scholar] [CrossRef]
- Kaufman-Cohen, Y.; Friedman, J.; Levanon, Y.; Jacobi, G.; Doron, N.; Portnoy, S. Wrist plane of motion and range during daily activities. Am. J. Occup. Ther. 2018, 72, 7206205080p1–7206205080p10. [Google Scholar] [CrossRef] [PubMed]
- Vardakastani, V.; Bell, H.; Mee, S.; Brigstocke, G.; Kedgley, A.E. Clinical measurement of the dart throwing motion of the wrist: Variability, accuracy and correction. J. Hand Surg. Eur. Vol. 2018, 43, 723–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braidotti, F.; Atzei, A.; Fairplay, T. Dart-Splint: An innovative orthosis that can be integrated into a scapho-lunate and palmar midcarpal instability re-education protocol. J. Hand Ther. 2015, 28, 329–335. [Google Scholar] [CrossRef]
- Fischer, G.; Wirth, M.A.; Balocco, S.; Calcagni, M. In Vivo Measurement of Wrist Movements during the Dart-Throwing Motion Using Inertial Measurement Units. Sensors 2021, 21, 5623. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Kang, B.B.; Jung, B.K.; Cho, K.J. Exo-wrist: A soft tendon-driven wrist-wearable robot with active anchor for dart-throwing motion in hemiplegic patients. IEEE Robot. Autom. Lett. 2019, 4, 4499–4506. [Google Scholar] [CrossRef]
- Kane, P.M.; Vopat, B.G.; Mansuripur, P.K.; Gaspar, M.P.; Wolfe, S.W.; Crisco, J.J.; Got, C. Relative contributions of the midcarpal and radiocarpal joints to dart-thrower’s motion at the wrist. J. Hand Surg. 2018, 43, 234–240. [Google Scholar] [CrossRef]
- Mahpari, V.; Levanon, Y.; Kaufman-Cohen, Y.; Zilberman, M.; Portnoy, S. Internal mechanics of a subject-specific wrist in the sagittal versus dart-throwing motion plane in adult and elder models: Finite element analyses. Appl. Sci. 2021, 11, 5275. [Google Scholar] [CrossRef]
- Brigstocke, G.; Hearnden, A.; Holt, C.; Whatling, G. In-vivo confirmation of the use of the dart thrower’s motion during activities of daily living. J. Hand Surg. Eur. Vol. 2014, 39, 373–378. [Google Scholar] [CrossRef]
- Eschweiler, J.; Li, J.; Quack, V.; Rath, B.; Baroncini, A.; Hildebrand, F.; Migliorini, F. Anatomy, Biomechanics, and Loads of the Wrist Joint. Life 2022, 12, 188. [Google Scholar] [CrossRef]
- Wild, E.; Gerberich, S.G.; Hunt, K.; Coe, K. Analyses of wrist injuries in workers engaged in repetitive tasks. AAOHN J. 1987, 35, 356–366. [Google Scholar] [CrossRef]
- Buckle, P.W. Fortnightly review: Work factors and upper limb disorders. BMJ 1997, 315, 1360–1363. [Google Scholar] [CrossRef] [PubMed]
- Eschweiler, J.; Praster, M.; Quack, V.; Michalik, R.; Hildebrand, F.; Rath, B.; Migliorini, F. Musculoskeletal Modeling of the Wrist via a Multi Body Simulation. Life 2022, 12, 581. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.L.; Jung, M.C.; Bashford, G.R.; Hallbeck, M.S. Maximal dynamic grip force and wrist torque: The effects of gender, exertion direction, angular velocity, and wrist angle. Appl. Ergon. 2006, 37, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Fang, Z.; Liu, J.; Tang, K.; Luo, J.; Yi, J.; Hu, X.; Wang, Z. A compact soft robotic wrist brace with origami actuators. Front. Robot. AI 2021, 8, 34. [Google Scholar] [CrossRef]
- Rose, C.G.; O’Malley, M.K. Hybrid rigid-soft hand exoskeleton to assist functional dexterity. IEEE Robot. Autom. Lett. 2018, 4, 73–80. [Google Scholar] [CrossRef]
- Kutz, M. Standard Handbook of Biomedical Engineering & Design; McGraw-Hill Education: New York, NY, USA, 2003; Chapter 32; pp. 32.1–32.61. [Google Scholar]
- Snook, S.H.; Ciriello, V.M.; Webster, B.S. Maximum acceptable forces for repetitive wrist extension with a pinch grip. Int. J. Ind. Ergon. 1999, 24, 579–590. [Google Scholar] [CrossRef]
- Higuma, T.; Kiguchi, K.; Arata, J. Low-profile two-degree-of-freedom wrist exoskeleton device using multiple spring blades. IEEE Robot. Autom. Lett. 2017, 3, 305–311. [Google Scholar] [CrossRef]
- Ates, S.; Haarman, C.J.; Stienen, A.H. SCRIPT passive orthosis: Design of interactive hand and wrist exoskeleton for rehabilitation at home after stroke. Auton. Robot. 2017, 41, 711–723. [Google Scholar] [CrossRef] [Green Version]
- Chiaradia, D.; Tiseni, L.; Xiloyannis, M.; Solazzi, M.; Masia, L.; Frisoli, A. An assistive soft wrist exosuit for flexion movements with an ergonomic reinforced glove. Front. Robot. AI 2021, 7, 595862. [Google Scholar] [CrossRef]
- Hope, J.; McDaid, A. Development of wearable wrist and forearm exoskeleton with shape memory alloy actuators. J. Intell. Robot. Syst. 2017, 86, 397. [Google Scholar] [CrossRef]
- Sasaki, D.; Noritsugu, T.; Takaiwa, M. Development of active support splint driven by pneumatic soft actuator (ASSIST). In Proceedings of the 2005 IEEE International Conference on Robotics and Automation, Barcelona, Spain, 18–22 April 2005; pp. 520–525. [Google Scholar] [CrossRef] [Green Version]
- JAS-Joint Active Systems. JAS Wrist. 2017. Available online: https://www.jointactivesystems.com/products/areas/wrist (accessed on 5 August 2022).
- Myomo Inc. MyoPro Orthosis. 2006. Available online: https://myomo.com/what-is-a-myopro-orthosis/ (accessed on 8 August 2022).
- Lambelet, C.; Temiraliuly, D.; Siegenthaler, M.; Wirth, M.; Woolley, D.G.; Lambercy, O.; Gassert, R.; Wenderoth, N. Characterization and wearability evaluation of a fully portable wrist exoskeleton for unsupervised training after stroke. J. Neuroeng. Rehabil. 2020, 17, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.G.; Menon, C. Towards the development of a portable wrist exoskeleton. In Proceedings of the 2011 IEEE International Conference on Robotics and Biomimetics, Karon Beach, Thailand, 7–11 December 2011; pp. 1884–1889. [Google Scholar] [CrossRef]
- Lambelet, C.; Lyu, M.; Woolley, D.; Gassert, R.; Wenderoth, N. The eWrist—A wearable wrist exoskeleton with sEMG-based force control for stroke rehabilitation. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 726–733. [Google Scholar] [CrossRef]
- Sangha, S.; Elnady, A.M.; Menon, C. A compact robotic orthosis for wrist assistance. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; pp. 1080–1085. [Google Scholar] [CrossRef]
- Hyttinge, M.; Einarsson, F. Bioservo Technologies; Technical Report; Redeye, Equity Research and Investment Banking Company: Stockholm, Sweden, 2021. [Google Scholar]
- Bioservo Technologies. Bioservo Strength for Life—Professional and Healthcare. Available online: https://www.bioservo.com/ (accessed on 7 September 2022).
- Ottobock. Paexo Wrist Exoskeleton. Available online: https://paexo.com/paexo-wrist/?lang=it (accessed on 5 August 2022).
- Bartlett, N.W.; Lyau, V.; Raiford, W.A.; Holland, D.; Gafford, J.B.; Ellis, T.D.; Walsh, C.J. A soft robotic orthosis for wrist rehabilitation. J. Med Devices 2015, 9, 030918. [Google Scholar] [CrossRef]
- Li, N.; Yang, T.; Yang, Y.; Yu, P.; Xue, X.; Zhao, X.; Song, G.; Elhajj, I.H.; Wang, W.; Xi, N.; et al. Bioinspired musculoskeletal model-based soft wrist exoskeleton for stroke rehabilitation. J. Bionic Eng. 2020, 17, 1163–1174. [Google Scholar] [CrossRef]
- Jeong, J.; Yasir, I.B.; Han, J.; Park, C.H.; Bok, S.K.; Kyung, K.U. Design of shape memory alloy-based soft wearable robot for assisting wrist motion. Appl. Sci. 2019, 9, 4025. [Google Scholar] [CrossRef] [Green Version]
- Jeong, J.; Hyeon, K.; Han, J.; Park, C.H.; Ahn, S.Y.; Bok, S.K.; Kyung, K.U. Wrist assisting soft wearable robot with stretchable coolant vessel integrated SMA muscle. IEEE/ASME Trans. Mechatronics 2021, 27, 1046–1058. [Google Scholar] [CrossRef]
- Andrikopoulos, G.; Nikolakopoulos, G.; Manesis, S. Motion control of a novel robotic wrist exoskeleton via pneumatic muscle actuators. In Proceedings of the 2015 IEEE 20th Conference on Emerging Technologies & Factory Automation (ETFA), Luxembourg, 8–11 September 2015; pp. 1–8. [Google Scholar] [CrossRef]
- Zhu, M.; Adams, W.; Polygerinos, P. Carpal tunnel syndrome soft relief device for typing applications. In Proceedings of the Frontiers in Biomedical Devices. American Society of Mechanical Engineers, Minneapolis, MN, USA, 10–13 April 2017; Volume 40672, p. V001T03A003. [Google Scholar] [CrossRef] [Green Version]
- Dragusanu, M.; Iqbal, M.Z.; Baldi, T.L.; Prattichizzo, D.; Malvezzi, M. Design, Development, and Control of a Hand/Wrist Exoskeleton for Rehabilitation and Training. IEEE Trans. Robot. 2022, 38, 1472–1488. [Google Scholar] [CrossRef]
- Saebo Inc. SaeboFlex. Available online: https://www.saebo.com/shop/saeboflex/ (accessed on 30 November 2022).
- Dragusanu, M.; Baldi, T.L.; Iqbal, Z.; Prattichizzo, D.; Malvezzi, M. Design, development, and control of a tendon-actuated exoskeleton for wrist rehabilitation and training. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA), Paris, France, 31 May–31 August 2020; pp. 1749–1754. [Google Scholar] [CrossRef]
- Harte, D.; Paterson, A. The fastest field sport in the world: A case report on 3-dimensional printed hurling gloves to help prevent injury. J. Hand Ther. 2018, 31, 398–410. [Google Scholar] [CrossRef] [Green Version]
- Elprama, S.A.; Vanderborght, B.; Jacobs, A. An industrial exoskeleton user acceptance framework based on a literature review of empirical studies. Appl. Ergon. 2022, 100, 103615. [Google Scholar] [CrossRef]
- Collinder, A.; Ekstrand, E. Hand Ergonomics in Early Phases of Production Development. Master’s Thesis, Chalmers University of Technology, Gothenburg, Sweden, 2018. [Google Scholar]
- ISO 11228-1:2021; ISO/TC 159/SC 3 Anthropometry and Biomechanics. Ergonomics—Manual Handling—Part 1: Lifting, Lowering and Carrying. ISO: Geneva, Switzerland, 2021. Available online: https://www.iso.org/standard/76820.html (accessed on 9 September 2022).
- ISO 11228-3:2007; ISO/TC 159/SC 3 Anthropometry and Biomechanics. Ergonomics—Manual Handling—Part 3: Handling of Low Loads at High Frequency. ISO: Geneva, Switzerland, 2007. Available online: https://www.iso.org/standard/26522.html (accessed on 9 September 2022).
- Marras, W.S.; SCHOENMARXLIN, R.W. Wrist motions in industry. Ergonomics 1993, 36, 341–351. [Google Scholar] [CrossRef]
- Ates, S.; Lobo-Prat, J.; Lammertse, P.; Van Der Kooij, H.; Stienen, A.H. SCRIPT passive orthosis: Design and technical evaluation of the wrist and hand orthosis for rehabilitation training at home. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; pp. 1–6. [Google Scholar] [CrossRef]
- Hoffman, H.B.; Blakey, G.L. New design of dynamic orthoses for neurological conditions. NeuroRehabilitation 2011, 28, 55–61. [Google Scholar] [CrossRef]
- Rogers, J.; Peters, B.; Laske, E.; McBryan, E. Development and testing of robotically assisted extravehicular activity gloves. In Proceedings of the 47th International Conference on Environmental Systems, Charleston, SC, USA, 16–20 July 2017; Available online: http://hdl.handle.net/2346/73043 (accessed on 17 August 2022).
- Diftler, M.A.; Ihrke, C.; Bridgwater, L.; Rogers, J.; Davis, D.; Linn, D.; Laske, E.; Ensley, K.; Lee, J. RoboGlove-A grasp assist device for earth and space. In Proceedings of the International Conference on Environmental Systems, Bellevue, WA, USA, 11 June 2015; p. JSC-CN-33541. Available online: https://ntrs.nasa.gov/citations/20150010420 (accessed on 17 August 2022).
- Nilsson, M.; Ingvast, J.; Wikander, J.; von Holst, H. The Soft Extra Muscle system for improving the grasping capability in neurological rehabilitation. In Proceedings of the 2012 IEEE-EMBS Conference on Biomedical Engineering and Sciences, Langkawi, Malaysia, 17–19 December 2012; pp. 412–417. [Google Scholar] [CrossRef]
- D’Antonio, E.; Galofaro, E.; Zenzeri, J.; Patané, F.; Konczak, J.; Casadio, M.; Masia, L. Robotic assessment of wrist proprioception during kinaesthetic perturbations: A neuroergonomic approach. Front. Neurorobotics 2021, 15, 640551. [Google Scholar] [CrossRef] [PubMed]
- Rose, L.; Bazzocchi, M.C.; Nejat, G. A model-free deep reinforcement learning approach for control of exoskeleton gait patterns. Robotica 2022, 40, 2189–2214. [Google Scholar] [CrossRef]
- Huang, Z.; Liu, J.; Li, Z.; Su, C.Y. Adaptive impedance control of robotic exoskeletons using reinforcement learning. In Proceedings of the 2016 International Conference on Advanced Robotics and Mechatronics (ICARM), Macau, China, 18–20 August 2016; pp. 243–248. [Google Scholar] [CrossRef]
- Ren, J.L.; Chien, Y.H.; Chia, E.Y.; Fu, L.C.; Lai, J.S. Deep learning based motion prediction for exoskeleton robot control in upper limb rehabilitation. In Proceedings of the 2019 International Conference on Robotics and Automation (ICRA), Montreal, QC, Canada, 20–24 May 2019; pp. 5076–5082. [Google Scholar] [CrossRef]
Figure 1.
Example of some repetitive tasks which affect wrist health.
Figure 1.
Example of some repetitive tasks which affect wrist health.
Figure 2.
This flow chart represents the methodology adopted in order to identify and screen all information available from online database and conduct our review.
Figure 2.
This flow chart represents the methodology adopted in order to identify and screen all information available from online database and conduct our review.
Figure 3.
Highlighting the displacement between flexion/extension axis (B) and radial/ulnar deviation axis (A).
Figure 3.
Highlighting the displacement between flexion/extension axis (B) and radial/ulnar deviation axis (A).
Figure 4.
Healthy wrist range of motion.
Figure 4.
Healthy wrist range of motion.
Figure 5.
Schematic drawing showing the orientation of the DTM axis.
Figure 5.
Schematic drawing showing the orientation of the DTM axis.
Figure 6.
Theil−Sen estimator of the DTM plane (solid line) for the optical motion capture data of a single representative subject. Reprinted/adapted with permission from Vardakastani et al. [
36], published by SAGE, Journal of Hand Surgery (European Volume), 2018.
Figure 6.
Theil−Sen estimator of the DTM plane (solid line) for the optical motion capture data of a single representative subject. Reprinted/adapted with permission from Vardakastani et al. [
36], published by SAGE, Journal of Hand Surgery (European Volume), 2018.
Figure 7.
Flow of requirements for exoskeletons in general.
Figure 7.
Flow of requirements for exoskeletons in general.
Figure 8.
Purposes for exoskeletons in general.
Figure 8.
Purposes for exoskeletons in general.
Figure 9.
Kinematics requirements for exoskeletons in general.
Figure 9.
Kinematics requirements for exoskeletons in general.
Figure 10.
The movement of the hand during oyster shucker’s work. Right hand holding the knife experienced repeated “dart throw motion”: (
a) wrist ulnar deviation + flexion; (
b) wrist radial deviation + flexion. The other hand holding the oyster experienced repeated: (
c) wrist flexion; (
d) wrist extension. Reprinted/adapted with permission from J. S. Park et al. [
28], published by Nofer Institute of Occupational Medicine, Łódź, Poland, International Journal of Occupational Medicine and Environmental Health, 2021.
Figure 10.
The movement of the hand during oyster shucker’s work. Right hand holding the knife experienced repeated “dart throw motion”: (
a) wrist ulnar deviation + flexion; (
b) wrist radial deviation + flexion. The other hand holding the oyster experienced repeated: (
c) wrist flexion; (
d) wrist extension. Reprinted/adapted with permission from J. S. Park et al. [
28], published by Nofer Institute of Occupational Medicine, Łódź, Poland, International Journal of Occupational Medicine and Environmental Health, 2021.
Figure 11.
Force and torque requirements to be evaluated for wrist exoskeletons.
Figure 11.
Force and torque requirements to be evaluated for wrist exoskeletons.
Figure 12.
Torque assistance according to applications. Consider applying torque to the center of the rear of the hand, about 0.1 m far from the wrist axis, as done by [
54]. Assistance is
not required (N.R) if the task requires less than 0.3 Nm of aid, since it is below that required for support a bare hand [
39,
51,
52,
56]. In
rehabilitation tasks, a torque ranging from 0.3 to 1.5 Nm is common [
39,
51,
52,
53]. These are minimum and maximum acceptable values to guarantee movements recovery and muscular strengthening, and they are dependent on the severity level of the impairment. In the
occupational sector, where users are considered healthy, possible ranges are wider due to different loads which have to be handled: a
light level of assistance is needed for fast, repetitive activities with small loads; a
moderate level of assistance is needed for tasks which require torque between 3 and 5 Nm, a range which, according to safety regulations, is the onset point of WRMSDs; a
high level of assistance is needed for tasks which require torque above 5 Nm, usually tasks in which heavy loads are managed.
Figure 12.
Torque assistance according to applications. Consider applying torque to the center of the rear of the hand, about 0.1 m far from the wrist axis, as done by [
54]. Assistance is
not required (N.R) if the task requires less than 0.3 Nm of aid, since it is below that required for support a bare hand [
39,
51,
52,
56]. In
rehabilitation tasks, a torque ranging from 0.3 to 1.5 Nm is common [
39,
51,
52,
53]. These are minimum and maximum acceptable values to guarantee movements recovery and muscular strengthening, and they are dependent on the severity level of the impairment. In the
occupational sector, where users are considered healthy, possible ranges are wider due to different loads which have to be handled: a
light level of assistance is needed for fast, repetitive activities with small loads; a
moderate level of assistance is needed for tasks which require torque between 3 and 5 Nm, a range which, according to safety regulations, is the onset point of WRMSDs; a
high level of assistance is needed for tasks which require torque above 5 Nm, usually tasks in which heavy loads are managed.
![Machines 11 00458 g012]()
Figure 13.
Rigidity requirements for wrist exoskeletons.
Figure 13.
Rigidity requirements for wrist exoskeletons.
Figure 14.
Ergonomic requirements for wrist exoskeletons.
Figure 14.
Ergonomic requirements for wrist exoskeletons.
Figure 15.
Safety requirements for wrist exoskeletons.
Figure 15.
Safety requirements for wrist exoskeletons.
Figure 16.
Awkward wrist postures according to ISO 11226, for a static posture, and 11228-3, while performing dynamic and repetitive movements. (a) Wrist palmar flexion awkward posture > 45°; (b) wrist dorsal extension awkward posture > 45°; (c) wrist ulnar deviation awkward posture > 20°; (d) Wrist radial deviation awkward posture > 15°.
Figure 16.
Awkward wrist postures according to ISO 11226, for a static posture, and 11228-3, while performing dynamic and repetitive movements. (a) Wrist palmar flexion awkward posture > 45°; (b) wrist dorsal extension awkward posture > 45°; (c) wrist ulnar deviation awkward posture > 20°; (d) Wrist radial deviation awkward posture > 15°.
Figure 17.
Some of the main situations which should be taken into account for a correct risk assessment.
Figure 17.
Some of the main situations which should be taken into account for a correct risk assessment.
Figure 18.
Classification criteria based on the design architecture of exoskeleton devices for wrist support.
Figure 18.
Classification criteria based on the design architecture of exoskeleton devices for wrist support.
Figure 19.
Classification criteria based on the type of actuation: passive or active.
Figure 19.
Classification criteria based on the type of actuation: passive or active.
Figure 20.
Different wrist exoskeletons focusing on portability: (
a) Wristbot: a fixed wrist exoskeleton for rehabilitation, designed by Masia. Reprinted/adapted with permission from D’Antonio et al. [
86], published by Frontiers in Neurorobotics, 2021; (
b) SCRIPT: a hand/wrist exoskeleton prototype for rehabilitation, reprinted/adapted with permission from Ates et al. [
53], published by Springer in Autonomous Robot, 2017; (
c) a prototype wrist exosuit for working assistance reprinted/adapted with permission from Chiaradia et al. [
54], published by Frontiers in Robotics and AI, Sec. Soft Robotics, 2021.
Figure 20.
Different wrist exoskeletons focusing on portability: (
a) Wristbot: a fixed wrist exoskeleton for rehabilitation, designed by Masia. Reprinted/adapted with permission from D’Antonio et al. [
86], published by Frontiers in Neurorobotics, 2021; (
b) SCRIPT: a hand/wrist exoskeleton prototype for rehabilitation, reprinted/adapted with permission from Ates et al. [
53], published by Springer in Autonomous Robot, 2017; (
c) a prototype wrist exosuit for working assistance reprinted/adapted with permission from Chiaradia et al. [
54], published by Frontiers in Robotics and AI, Sec. Soft Robotics, 2021.
Figure 21.
Different types of power source adopted in different designs.
Figure 21.
Different types of power source adopted in different designs.
Figure 22.
Different types of power transmission adopted in different designs.
Figure 22.
Different types of power transmission adopted in different designs.
Figure 23.
Different sensing adopted in different designs.
Figure 23.
Different sensing adopted in different designs.
Figure 24.
Different control signals, control paradigms, and control schemes adopted in different designs.
Figure 24.
Different control signals, control paradigms, and control schemes adopted in different designs.
Figure 25.
Wearable and portable wrist exoskeletons classified by actuation type, power source, and power transmission. A total of 22 devices have been analysed.
Figure 25.
Wearable and portable wrist exoskeletons classified by actuation type, power source, and power transmission. A total of 22 devices have been analysed.
Figure 26.
The percentage of wearable and portable wrist exoskeletons classified by sensing technologies implemented and control strategies. Percentage have been used to report the device distribution since, usually, devices may have multiple sensors and control strategies.
Figure 26.
The percentage of wearable and portable wrist exoskeletons classified by sensing technologies implemented and control strategies. Percentage have been used to report the device distribution since, usually, devices may have multiple sensors and control strategies.
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).