Convergent and Concurrent Validity between Clinical Recovery and Personal-Civic Recovery in Mental Health †
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.1.1. Sample Selection and Procedure
2.1.2. Exclusion Criteria
2.1.3. Sample Size Estimation
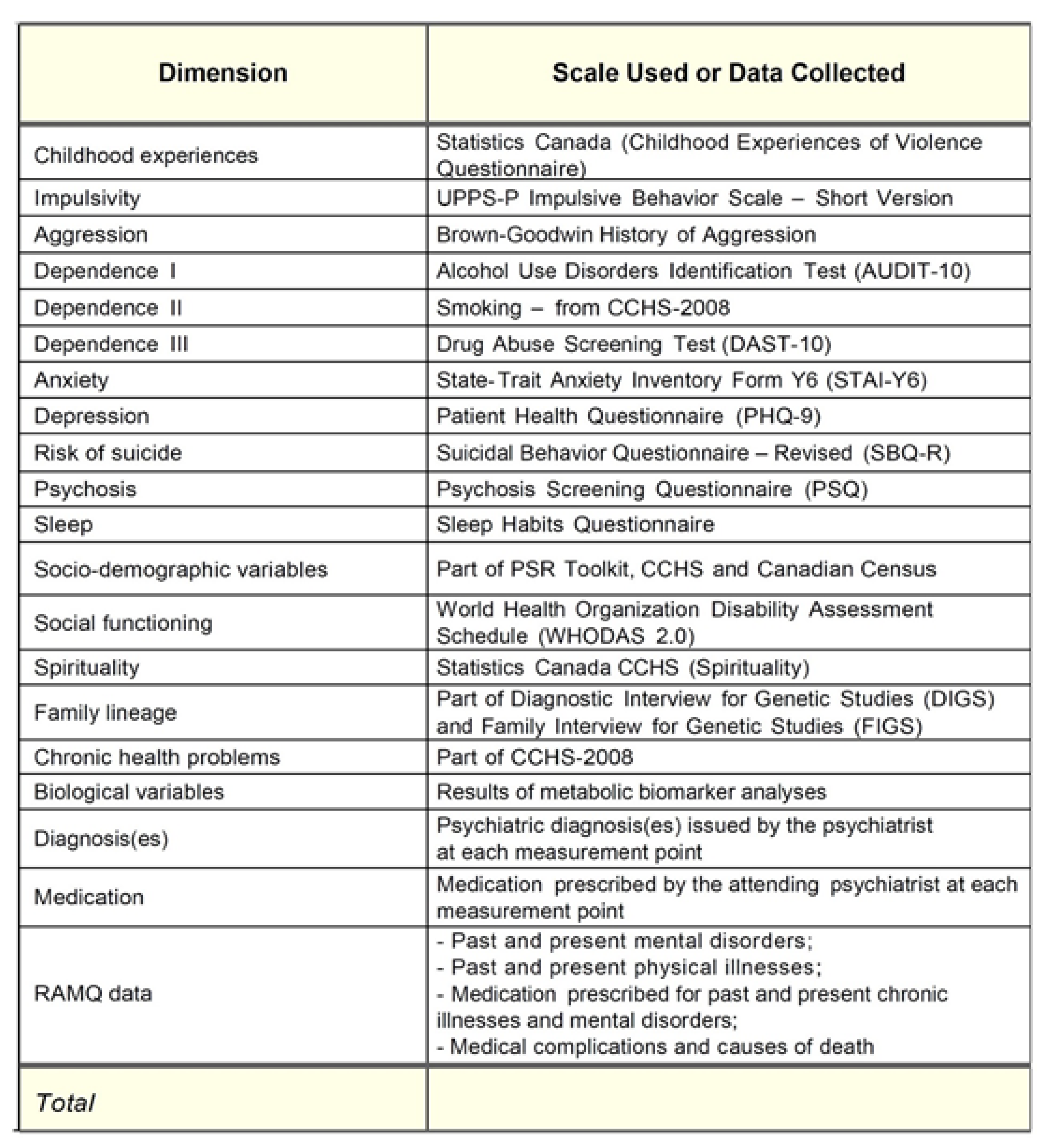
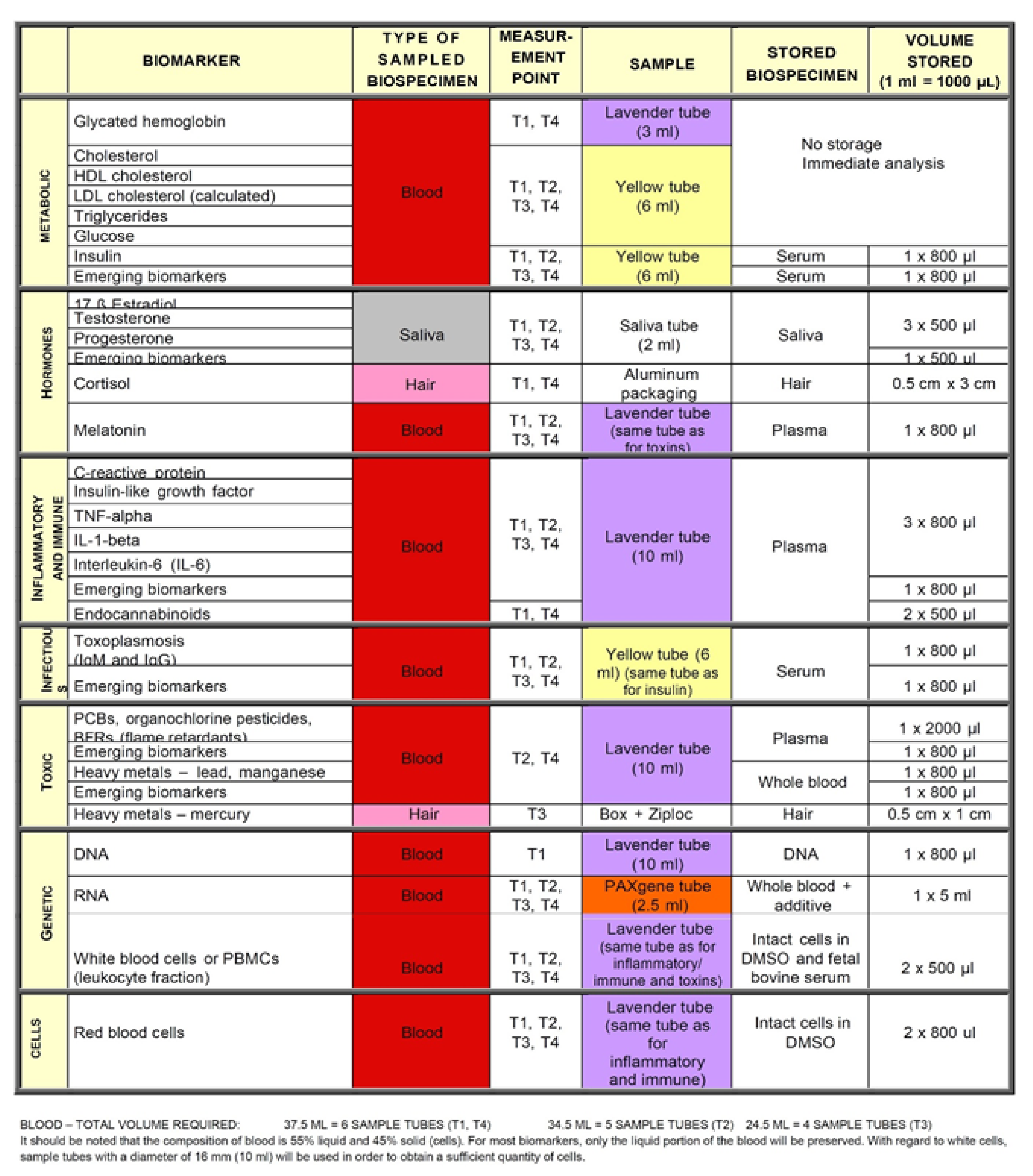
2.2. Measurements
2.2.1. Recovery Assessment Scale
2.2.2. The Citizenship Measure
2.2.3. The Recovery Self-Assessment
2.2.4. Measures of Clinical Recovery
2.3. Statistical Analysis
2.3.1. Internal Consistency
2.3.2. Convergent and Concurrent Validity
3. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
References
- HM Government. No Health without Mental Health. Delivering Better Mental Health Outcomes for People of All Ages; Department of Health: London, UK, 2011.
- New Freedom Commission on Mental. Health Achieving the Promise: Transforming Mental Health Care in America, Final Report; Department of Health and Human Services: Rockville, MD, USA, 2003. [CrossRef]
- Mental Health Commission of Canada. Changing Directions, Changing Lives. The Mental Health Strategy for Canada; Mental Health Commission of Canada: Calgary, AB, Canada, 2012. [Google Scholar]
- World Health Organization. Mental Health Action Plan 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Ministère de la Santé et des Services sociaux du Québec. Plan D’action en Santé Mentale 2015–2020: Faire Ensemble et Autrement; Government of Quebec: Quebec City, QC, Canada, 2015.
- Ministère de la Santé et des Services sociaux du Québec. Plan D’action En Santé Mentale 2005–2010: La Force Des Liens; Government of Quebec: Quebec City, QC, Canada, 2005.
- Davidson, L.; Rakfeldt, J.; Strauss, J. The Roots of the Recovery Movement in Psychiatry: Lessons Learned; Wiley-Blackwell: London, UK, 2010. [Google Scholar] [CrossRef]
- Anthony, W.A. Recovery from mental illness: The guiding vision of the mental health service system in the 1990s. Psychosoc. Rehabil. J. 1993, 16, 11. [Google Scholar] [CrossRef]
- Shanks, V.; Williams, J.; Leamy, M.; Bird, V.J.; Le Boutillier, C.; Slade, M. Measures of personal recovery: A systematic review. Psychiatr. Serv. 2013, 64, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Slade, M.; Longden, E. Empirical evidence about recovery and mental health. BMC Psychiatry 2015, 15, 285. [Google Scholar] [CrossRef] [PubMed]
- Hess, J.; Lacasse, J.; Harmon, J.; Williams, D.; Vierling-Glaassen, N. “Is there a getting better from this, or not?” Examining the meaning and possibility of recovery from mental health disorder. Child Youth Serv. 2014, 35, 116–136. [Google Scholar] [CrossRef]
- Secker, J.; Membrey, H.; Grove, B.; Seebohm, P. Recovering from Illness or Recovering your Life? Implications of Clinical versus Social Models of Recovery from Mental Health Problems for Employment Support Services. Disabil. Soc. 2002, 17, 403–418. [Google Scholar] [CrossRef]
- Slade, M. Personal Recovery and Mental Illness; Cambridge University Press: Cambridge, UK, 2009. [Google Scholar] [CrossRef]
- Mental Health Commission of Canada. Toward Recovery & Well-Being: A Framework for a Mental Health Strategy for Canada. 2009. Available online: https://www.mentalhealthcommission.ca/sites/default/files/FNIM_Toward_Recovery_and_Well_Being_ENG_0_1.pdf (accessed on 25 September 2020).
- Corrigan, P.W.; Salzer, M.; Ralph, R.O.; Sangster, Y.; Keck, L. Examining the Factor Structure of the Recovery Assessment Scale. Schizophr. Bull. 2004, 30, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.; Clayton, A.; Benedict, P.; Bellamy, C.; Antunes, K.; Miller, R.; Pelletier, J.F.; Stern, E.; O’Connell, M.J. Going to the Source: Creating a Citizenship Outcome Measure by Community-Based Participatory Research Methods. Psychiatr. Serv. 2012, 63, 445–450. [Google Scholar] [CrossRef]
- Andresen, R.; Caputi, P.; Oades, L.G. Do clinical outcome measures assess consumer-defined recovery? Psychiatr. Res. 2010, 177, 309–317. [Google Scholar] [CrossRef]
- Simpson, A.; Hannigan, B.; Coffey, M.; Jones, A.; Barlow, S.; Cohen, R.; Vseteckova, J.; Faulkner, A. Cross-national comparative mixed-methods case study of recovery-focused mental health care planning and co-ordination: Collaborative Care Planning Project (COCAPP). Health Serv. Deliv. Res. 2016, 4, 190. [Google Scholar] [CrossRef]
- van Vugt, M.; Kroon, H.; Delespaul, P.; Mulder, C. Consumer-Providers in Assertive Community Treatment Programs: Associations with Client Outcomes. Psychiatr. Serv. 2012, 63, 477–481. [Google Scholar] [CrossRef]
- Mahlke, C.; Priebe, S.; Heumann, K.; Daubmann, A.; Wegscheider, K.; Bock, T. Effectiveness of one-to-one peer support for patients with severe mental illness—A randomised controlled trial. Eur. Psychiatry 2017, 42, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Mead, S.; Hilton, D.; Curtis, L. Peer support: A theoretical perspective. Psychiatr. Rehabil. J. 2001, 25, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Sunderland, K.; Mishkin, W. Guidelines for the Practice and Training of Peer Support; Mental Health Commission of Canada: Calgary, AB, Canada, 2013. [Google Scholar]
- Felton, C.J.; Stastny, P.; Shern, D.L.; Blanch, A.; Donahue, S.A.; Knight, E.; Brown, C. Consumers as peer specialists on intensive case management teams: Impact on client outcomes. Psychiatr. Serv. 1995, 46, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Chinman, M.; George, P.; Dougherty, R.; Daniels, A.; Ghose, S.; Swift, A.; Delphin-Rittmon, M. Peer support services for individuals with serious mental illnesses: Assessing the evidence. Psychiatr. Serv. 2014, 65, 429–441. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Mental Health. Strategic Plan for Research; NIMH: Bethesda, MD, USA, 2008.
- Lupien, S.J.; Sasseville, M.; François, N.; Giguère, C.E.; Boissonneault, J.; Plusquellec, P.; Godbout, R.; Xiong, L.; Potvin, S.; Kouassi, E.; et al. The DSM5/RDoC debate on the future of mental health research: Implication for studies on human stress and presentation of the signature bank. Stress 2017, 20, 95–111. [Google Scholar] [CrossRef]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 1993. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Lenth, R. Some Practical Guidelines for Effective Sample Size Determination. Am. Stat. 2001, 55, 187–193. [Google Scholar] [CrossRef]
- Vallerand, R.J. Toward a methodology for the transcultural validation of psychological questionnaires: Implications for research in the French language. Can. Psychol. 1989, 30, 662–680. [Google Scholar] [CrossRef]
- O’Connell, M.; Tondora, J.; Croog, G.; Evans, A.; Davidson, L. From rhetoric to routine: Assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatr Rehabil. J. 2005, 28, 378–386. [Google Scholar] [CrossRef]
- Pelletier, J.F.; Corbière, M.; Lecomte, T.; Briand, C.; Corrigan, P.; Davidson, L.; Rowe, M. Citizenship and recovery: Two intertwined concepts for civic-recovery. BMC Psychiatry 2015, 15, 37. [Google Scholar] [CrossRef]
- Salzer, M.; Brusilovskiy, E. Advancing Recovery Science: Reliability and Validity Properties of the Recovery Assessment Scale. Psychiatr. Serv. 2014, 65, 442–453. [Google Scholar] [CrossRef]
- Knupp, P. The Contribution of the Recovery Self Assessment to the Measurement of Illness Management and Recovery. Ph.D. Thesis, Drake University, Des Moines, IA, USA, 2013. [Google Scholar]
- Kidd, S.A.; George, L.; O’Connell, M.J.; Kirkpatrick, H.; Odueyungbo, A.O.; Davidson, L.; Sylvestre, J.; Browne, G. Recovery-oriented service provision and clinical outcomes in assertive community treatment. Psychiatr. Rehabil. J. 2011, 34, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Salyers, M.; Tsai, J.; Stultz, T. Measuring recovery orientation in a hospital setting. Psychiatr. Rehabil. J. 2007, 31, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Marteau, T.M.; Bekker, H. The development of a six-item short form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br. J. Clin. Psychol. 1992, 31, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Babor, T.; Higgins-Biddle, J.; Saunders, J.; Monteiro, M. AUDIT Guidelines for Use in Primary Care, 2nd ed.; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Lam, L.P.; Leung, W.C.; Ip, P.; Chow, C.B.; Chan, M.F.; Ng, J.W.; Sing, C.; Lam, Y.H.; Mak, W.L.; Chow, K.M.; et al. Validation of the Drug Abuse Screening Test (DAST-10): A study on illicit drug use among Chinese pregnant women. Sci. Rep. 2015, 19, 11420. [Google Scholar] [CrossRef]
- Bebbington, P.E.; Nayani, T. The Psychosis Screening Questionnaire. Int. J. Methods Psychiatr. Res. 1995, 5, 11–19. [Google Scholar]
- WHO Disability Assessment Schedule 2.0 WHODAS-2.0. Available online: http://www.who.int/classifications/icf/whodasii/en/index.htm (accessed on 25 September 2020).
- Khan, A.M. R-software: A Newer Tool in Epidemiological Data Analysis. Indian J. Community Med. 2013, 38, 56–58. [Google Scholar] [CrossRef]
- Revelle, W. psych: Procedures for Personality and Psychological Research. Northwestern University, Evanston. R package version 1 (1). 2014. Available online: https://www.scholars.northwestern.edu/en/publications/psych-procedures-for-personality-and-psychological-research (accessed on 25 September 2020).
- Lavaan, R. An R package for structural equation modeling. J Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Cronbach, L. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Campbell, D.; Fiske, D. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol. Bull. 1959, 56, 81–105. [Google Scholar] [CrossRef] [PubMed]
- Parizeau, M.H.; Lupien, S.; François, N.; Larocque, G. Management Framework: Signature medical/Psychological Data and Human Biological Materials Bank. Available online: https://www.banquesignature.ca/ (accessed on 28 September 2013).
- Pelletier, J.F.; Davidson, L.; Gaulin, D.; Bordet, J. Recovery Mentors as continuing professional development trainers for better recognition of the epistemic value of the experiential knowledge and improved access to recovery-oriented practices. AIMS Public Health 2019, 6, 447–460. [Google Scholar] [CrossRef] [PubMed]
- Pétré, B.; Gagnayre, R.; De Andrade, V.; Ziegler, O.; Guillaume, M. From therapeutic patient education principles to educative attitude: The perceptions of health care professionals—A pragmatic approach for defining competencies and resources. Patient Prefer. Adherence 2017, 11, 603–617. [Google Scholar] [CrossRef] [PubMed]
- Peteuil, A.; Rat, C.; Moussa-Badran, S.; Carpentier, M.; Pelletier, J.F.; Denis, F. A Therapeutic Educational Program in Oral Health for Persons with Schizophrenia: A Qualitative Feasibility Study. Int. J. Dent. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Lagger, G.; Pataky, Z.; Golay, A. Efficacy of therapeutic patient education in chronic diseases and obesity. Patient Educ. Couns. 2010, 79, 283–286. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Peer Support Groups by and for People with Lived Experience. WHO Quality Rights Guidance Module; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
| Dimension | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. CM-Self-determination | 0.67 | |||||||||
| 2. CM-Respect by others | 0.37 | 0.74 | ||||||||
| 3. CM-Involvement in community | 0.18 | 0.30 | 0.65 | |||||||
| 4. CM-Fundamental needs | 0.36 | 0.46 | 0.32 | 0.60 | ||||||
| 5. CM-Access to services | 0.38 | 0.29 | 0.26 | 0.28 | 0.60 | |||||
| 6. RAS-Personal confidences | 0.33 | 0.46 | 0.36 | 0.48 | 0.27 | 0.86 | ||||
| 7. RAS-Willingness to ask for help | 0.34 | 0.45 | 0.33 | 0.43 | 0.38 | 0.75 | 0.61 | |||
| 8. RAS-Goal and success orientation | 0.48 | 0.44 | 0.30 | 0.52 | 0.33 | 0.77 | 0.67 | 0.80 | ||
| 9. RAS-Reliance on others | 0.27 | 0.40 | 0.39 | 0.30 | 0.22 | 0.51 | 0.46 | 0.49 | 0.60 | |
| 10. RAS-No domination by symptoms | 0.37 | 0.21 | 0.37 | 0.23 | 0.37 | 0.55 | 0.47 | 0.58 | 0.41 | 0.77 |
| Dimension | Name of the Instrument | Abbreviation | Number of Items | Reference |
|---|---|---|---|---|
| i—Personal recovery | Recovery Assessment Scale | RAS | 24 | [15] |
| ii—Citizenship | Citizenship Measure | CM | 23 | [16] |
| iii—Organizational recovery | Recovery Self-Assessment | RSA | 32 | [31] |
| iv—Anxiety | Anxiety State-Trait Anxiety Inventory Form Y6 | STAI-Y6 | 6 | [37] |
| v—Depression | Depression Patient Health Questionnaire | PHQ-9 | 9 | [38] |
| vi—Alcohol Dependence | Alcohol Use Disorders Identification Test | AUDIT-10 | 10 | [39] |
| vii—Drug Dependence | Drug Abuse Screening Test | DAST-10 | 10 | [40] |
| viii—Psychosis | Psychosis Screening Questionnaire | PSQ | 12 | [41] |
| ix—Social functioning | World Health Organization Disability Assessment Schedule | WHODAS 2.0 | 12 | [42] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pelletier, J.-F.; Davidson, L.; Giguère, C.-É.; Franck, N.; Bordet, J.; Rowe, M. Convergent and Concurrent Validity between Clinical Recovery and Personal-Civic Recovery in Mental Health. J. Pers. Med. 2020, 10, 163. https://doi.org/10.3390/jpm10040163
Pelletier J-F, Davidson L, Giguère C-É, Franck N, Bordet J, Rowe M. Convergent and Concurrent Validity between Clinical Recovery and Personal-Civic Recovery in Mental Health. Journal of Personalized Medicine. 2020; 10(4):163. https://doi.org/10.3390/jpm10040163
Chicago/Turabian StylePelletier, Jean-François, Larry Davidson, Charles-Édouard Giguère, Nicolas Franck, Jonathan Bordet, and Michael Rowe. 2020. "Convergent and Concurrent Validity between Clinical Recovery and Personal-Civic Recovery in Mental Health" Journal of Personalized Medicine 10, no. 4: 163. https://doi.org/10.3390/jpm10040163
APA StylePelletier, J.-F., Davidson, L., Giguère, C.-É., Franck, N., Bordet, J., & Rowe, M. (2020). Convergent and Concurrent Validity between Clinical Recovery and Personal-Civic Recovery in Mental Health. Journal of Personalized Medicine, 10(4), 163. https://doi.org/10.3390/jpm10040163





