Subclinical Cognitive and Neuropsychiatric Correlates and Hippocampal Volume Features of Brain White Matter Hyperintensity in Healthy People
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Cognitive Assessment
2.3. Psychiatric Assessment
2.4. Image Acquisition and Processing
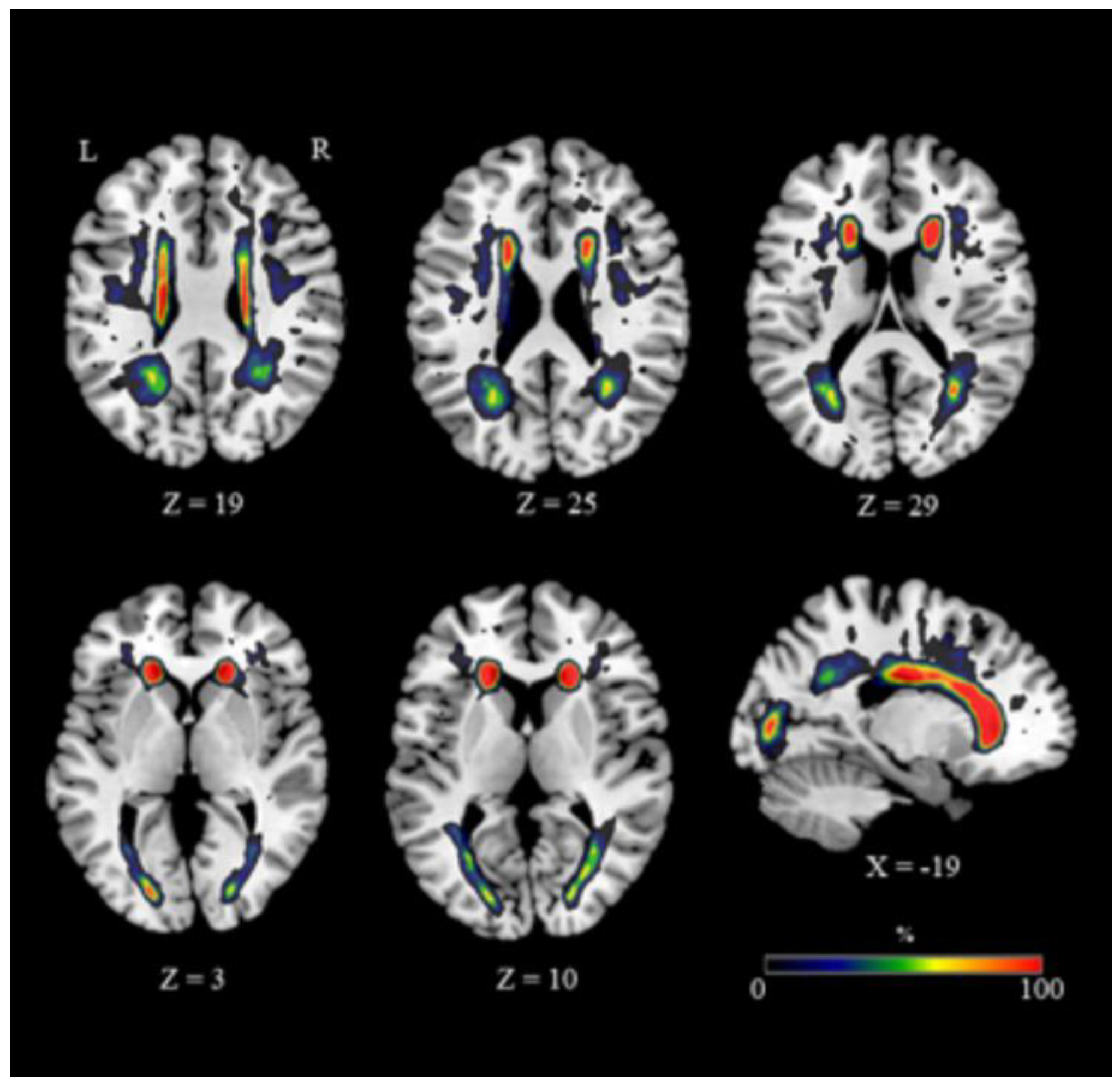
2.5. Regional Distribution and Volume Measurement of WMH
2.6. Hippocampal Volume Reduction
2.7. Statistical Analysis
2.7.1. Neuropsychological and Neuropsychiatric Data
2.7.2. Neuroimaging–ROI analysis: Differences between Groups
3. Results
3.1. Neuropsychological and Neuropsychiatric Measures
3.2. Regional Distribution and Volume Measurement of White Matter Hyperintensities (WMH)
3.3. Hippocampus–ROI Analyses
4. Discussion
4.1. WMH Are Associated with Decreased Cognitive Functioning
4.2. WMH Are Associated with Subclinical Neuropsychiatric Changes
4.3. WMH Are Associated with Hippocampal Atrophy
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hedden, T.; Gabrieli, J.D.E. Insights into the ageing mind: A view from cognitive neuroscience. Nat. Rev. Neurosci. 2004, 5, 87–96. [Google Scholar] [CrossRef]
- Gunning-Dixon, F.M.; Brickman, A.M.; Cheng, J.C.; Alexopoulos, G.S. Aging of cerebral white matter: A review of MRI findings. Int. J. Geriatr. Psychiatry 2009, 24, 109–117. [Google Scholar] [CrossRef] [Green Version]
- Peters, A. The effects of normal aging on myelin and nerve fibers: A review. J. Neurocytol. 2002, 31, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, E.V.; Adalsteinsson, E.; Pfefferbaum, A. Selective age-related degradation of anterior callosal fiber bundles quantified in vivo with fiber tracking. Cereb. Cortex 2006, 16, 1030–1039. [Google Scholar] [CrossRef] [PubMed]
- Madden, D.J.; Bennett, I.J.; Song, A.W. Cerebral white matter integrity and cognitive aging: Contributions from diffusion tensor imaging. Neuropsychol. Rev. 2009, 19, 415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zlokovic, B.V. Neurovascular pathways to neurodegeneration in Alzheimer’s disease and other disorders. Nat. Rev. Neurosci. 2011, 12, 723–738. [Google Scholar] [CrossRef] [PubMed]
- Wardlaw, J.M.; Smith, E.E.; Biessels, G.J. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013, 12, 822–838. [Google Scholar] [CrossRef] [Green Version]
- Debette, S.; Markus, H.S. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: Systematic review and meta-analysis. BMJ 2010, 341, c3666. [Google Scholar] [CrossRef] [Green Version]
- Hommet, C.; Mondon, K.; Constans, T.; Beaufils, E.; Desmidt, T.; Camus, V.; Cottier, J.P. Review of cerebral microangiopathy and Alzheimer’s disease: Relation between white matter hyperintensities and microbleeds. Dement. Geriatr. Cogn. Disord. 2012, 32, 367–378. [Google Scholar] [CrossRef]
- Shim, Y.S.; Yang, D.-W.; Roe, C.M.; Coats, M.A.; Benzinger, T.L.; Xiong, C.; Galvin, J.E.; Cairns, N.J.; Morris, J.C. Pathological correlates of white matter hyperintensities on magnetic resonance imaging. Dement. Geriatr. Cogn. Disord. 2015, 39, 92–104. [Google Scholar] [CrossRef] [Green Version]
- Iorio, M.; Spalletta, G.; Chiapponi, C.; Luccichenti, G.; Cacciari, C.; Orfei, M.D.; Caltagirone, C.; Piras, F. White matter hyperintensities segmentation: A new semi-automated method. Front. Aging Neurosci. 2013, 5, 76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.H.; Hwang, K.J.; Kim, J.-H.; Lee, Y.H.; Rhee, H.Y.; Park, K.C. Regional white matter hyperintensities in normal aging, single domain amnestic mild cognitive impairment, and mild Alzheimer’s disease. J. Clin. Neurosci. 2011, 18, 1101–1106. [Google Scholar] [CrossRef] [PubMed]
- Lopez, O.L.; Jagust, W.J.; Dulberg, C.; Becker, J.T.; DeKosky, S.T.; Fitzpatrick, A.; Breitner, J.; Lyketsos, C.; Jones, B.; Kawas, C. Risk factors for mild cognitive impairment in the Cardiovascular Health Study Cognition Study: Part 2. Arch. Neurol. 2003, 60, 1394–1399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, E.; Gao, F.; Black, S.E.; Lobaugh, N.J. Automatic segmentation of white matter hyperintensities in the elderly using FLAIR images at 3T. J. Magn. Reson. Imaging 2010, 31, 1311–1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, M.E.; Senjem, M.L.; Petersen, R.C.; Hollman, J.H.; Preboske, G.M.; Weigand, S.D.; Knopman, D.S.; Ferman, T.J.; Dickson, D.W.; Jack, C.R. Functional impact of white matter hyperintensities in cognitively normal elderly subjects. Arch. Neurol. 2010, 67, 1379–1385. [Google Scholar] [CrossRef] [Green Version]
- Brickman, A.M.; Muraskin, J.; Zimmerman, M.E. Structural neuroimaging in Alzheimer’s disease: Do white matter hyperintensities matter? Dialogues Clin. Neurosci. 2009, 11, 181–190. [Google Scholar] [PubMed]
- Van der Flier, W.M.; van Straaten, E.C.W.; Barkhof, F.; Verdelho, A.; Madureira, S.; Pantoni, L.; Inzitari, D.; Erkinjuntti, T.; Crisby, M.; Waldemar, G. Small vessel disease and general cognitive function in nondisabled elderly the LADIS study. Stroke 2005, 36, 2116–2120. [Google Scholar] [CrossRef]
- Raz, N.; Rodrigue, K.M.; Kennedy, K.M.; Acker, J.D. Vascular health and longitudinal changes in brain and cognition in middle-aged and older adults. Neuropsychology 2007, 21, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Kloppenborg, R.P.; Nederkoorn, P.J.; Geerlings, M.I.; Berg, E.V.D. Presence and progression of white matter hyperintensities and cognition A meta-analysis. Neurology 2014, 82, 2127–2138. [Google Scholar] [CrossRef] [Green Version]
- Firbank, M.J.; Lloyd, A.J.; Ferrier, N.; O’Brien, J. A volumetric study of MRI signal hyperintensities in late-life depression. Am. J. Geriatr. Psychiatry 2004, 12, 606–612. [Google Scholar] [CrossRef]
- Greenwald, B.S.; Kramer-Ginsberg, E.; Krishnan, R.R.; Ashtari, M.; Aupperle, P.M.; Patel, M. MRI signal hyperintensities in geriatric depression. Am. J. Psychiatry 1996, 153, 1212–1215. [Google Scholar] [PubMed]
- Lavretsky, H.; Zheng, L.; Weiner, M.W.; Mungas, D.; Reed, B.; Kramer, J.H.; Jagust, W.; Chui, H.; Mack, W.J. The MRI brain correlates of depressed mood, anhedonia, apathy, and anergia in older adults with and without cognitive impairment or dementia. Int. J. Geriatr. Psychiatry 2008, 23, 1040–1050. [Google Scholar] [CrossRef]
- Staekenborg, S.S.; Su, T.; Van Straaten, E.C.W.; Lane, R.; Scheltens, P.; Barkhof, F.; Van Der Flier, W.M. Behavioural and psychological symptoms in vascular dementia; differences between small and large vessel disease. J. Neurol. Neurosurg. Psychiatry 2009, 81, 547–551. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.T.; Firbank, M.J.; Krishnan, M.S.; Van Straaten, E.C.; Van Der Flier, W.M.; Petrovic, K.; Pantoni, L.; Simoni, M.; Erkinjuntti, T.; Wallin, A.; et al. White matter hyperintensities rather than lacunar infarcts are associated with depressive symptoms in older people: The LADIS study. Am. J. Geriatr. Psychiatry 2006, 14, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Godin, O.; Dufouil, C.; Maillard, P.; Delcroix, N.; Mazoyer, B.; Crivello, F.; Alpérovitch, A.; Tzourio, C. White matter lesions as a predictor of depression in the elderly: The 3C-Dijon study. Biol. Psychiatry 2008, 63, 663–669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Groot, J.C.; De Leeuw, F.-E.; Oudkerk, M.; Hofman, A.; Jolles, J.; Breteler, M.M.B. Cerebral white matter lesions and depressive symptoms in elderly adults. Arch. Gen. Psychiatry 2000, 57, 1071–1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, W.D.; MacFall, J.R.; Payne, M.E.; McQuoid, D.R.; Steffens, D.C.; Provenzale, J.M.; Krishnan, R.R. Greater MRI lesion volumes in elderly depressed subjects than in control subjects. Psychiatry Res. Neuroimaging 2005, 139, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cervilla, J.A.; Prince, M.J.; Rabe-Hesketh, S. Vascular disease risk factors as determinants of incident depressive symptoms: A prospective community-based study. Psychol. Med. 2004, 34, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Versluis, C.E.; Van Der Mast, R.; Van Buchem, M.A.; Bollen, E.L.E.M.; Blauw, G.J.; Eekhof, J.A.H.; Van Der Wee, N.J.A.; De Craen, A.J.M. On behalf of the PROSPER Study Group Progression of cerebral white matter lesions is not associated with development of depressive symptoms in elderly subjects at risk of cardiovascular disease. The PROSPER study. Int. J. Geriatr. Psychiatry 2006, 21, 375–381. [Google Scholar] [CrossRef]
- Brookes, R.L.; Herbert, V.; Lawrence, A.J.; Morris, R.G.; Markus, H.S. Depression in small-vessel disease relates to white matter ultrastructural damage, not disability. Neurology 2014, 83, 1417–1423. [Google Scholar] [CrossRef] [Green Version]
- Marin, R.S. Differential diagnosis of apathy and related disorders of diminished motivation. Psychiatr. Ann. 1997, 27, 30–33. [Google Scholar] [CrossRef]
- Steunenberg, B.; Braam, A.W.; Beekman, A.T.F.; Deeg, R.J.H.; Kerkhof, A.J.F.M. Evidence for an association of the big five personality factors with recurrence of depressive symptoms in later life. Int. J. Geriatr. Psychiatry 2009, 24, 1470–1477. [Google Scholar] [CrossRef] [PubMed]
- Hollocks, M.J.; Lawrence, A.J.; Brookes, R.L.; Barrick, T.R.; Morris, R.G.; Husain, M.; Markus, H.S. Differential relationships between apathy and depression with white matter microstructural changes and functional outcomes. Brain 2015, 138, 3803–3815. [Google Scholar] [CrossRef] [PubMed]
- Jokinen, H.; Lipsanen, J.; Schmidt, R.; Fazekas, F.; Gouw, A.; Van Der Flier, W.M.; Barkhof, F.; Madureira, S.; Verdelho, A.; Ferro, J.M.; et al. Brain atrophy accelerates cognitive decline in cerebral small vessel disease: The LADIS study. Neurology. 2012, 78, 1785–1792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishio, K.; Ihara, M.; Yamasaki, N.; Kalaria, R.N.; Maki, T.; Fujita, Y.; Ito, H.; Oishi, N.; Fukuyama, H.; Miyakawa, T.; et al. A mouse model characterizing features of vascular dementia with hippocampal atrophy. Stroke 2010, 41, 1278–1284. [Google Scholar] [CrossRef] [Green Version]
- Godin, O.; Maillard, P.; Crivello, F.; Alpérovitch, A.; Mazoyer, B.; Tzourio, C.; Dufouil, C. Association of white-matter lesions with brain atrophy markers: The Three-City Dijon MRI study. Cerebrovasc. Dis. 2009, 28, 177–184. [Google Scholar] [CrossRef]
- Kloppenborg, R.P.; Nederkoorn, P.J.; Grool, A.M.; Vincken, K.L.; Mali, W.P.T.M.; Vermeulen, M.; Van Der Graaf, Y.; Geerlings, M.I. Cerebral small-vessel disease and progression of brain atrophy: The SMART-MR study. Neurology 2012, 79, 2029–2036. [Google Scholar] [CrossRef] [PubMed]
- Heijer, T.D.; Launer, L.J.; Prins, N.D.; van Dijk, E.J.; Vermeer, S.E.; Hofman, A.; Koudstaal, P.J.; Breteler, M.M.B. Association between blood pressure, white matter lesions and atrophy. Neurology 2005, 64, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Kril, J.J.; Patel, S.; Harding, A.J.; Halliday, G.M. Patients with vascular dementia due to microvascular pathology have significant hippocampal neuronal loss. J. Neurol. Neurosurg. Psychiatry 2002, 72, 747–751. [Google Scholar] [CrossRef] [Green Version]
- Fiford, C.M.; Manning, E.N.; Bartlett, J.W.; Cash, D.M.; Malone, I.B.; Ridgway, G.R.; Lehmann, M.; Leung, K.K.; Sudre, C.H.; Ourselin, S.; et al. White matter hyperintensities are associated with disproportionate progressive hippocampal atrophy. Hippocampus 2017, 27, 249–262. [Google Scholar] [CrossRef] [Green Version]
- Barnes, J.; Carmichael, O.T.; Neuroimaging, D. Vascular and Alzheimer’s disease markers independently predict brain atrophy rate in Alzheimer’s Disease Neuroimaging Initiative controls. Neurobiol. Aging 2013, 34, 1996–2002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spalletta, G.; Fagioli, S.; Caltagirone, C.; Epiras, F. Brain microstructure of subclinical apathy phenomenology in healthy individuals. Hum. Brain Mapp. 2012, 34, 3193–3203. [Google Scholar] [CrossRef] [PubMed]
- Lampe, L.; Kharabian-Masouleh, S.; Kynast, J.; Arelin, K.; Steele, C.J.; Löffler, M.; Witte, A.V.; Schroeter, M.L.; Villringer, A.; Bazin, P.-L. Lesion location matters: The relationships between white matter hyperintensities on cognition in the healthy elderly. Br. J. Pharmacol. 2017, 39, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Al-Janabi, O.M.; Bauer, C.E.; Goldstein, L.B.; Murphy, R.R.; Bahrani, A.A.; Smith, C.D.; Wilcock, D.M.; Gold, B.T.; Jicha, G.A. White Matter Hyperintensity Regression: Comparison of Brain Atrophy and Cognitive Profiles with Progression and Stable Groups. Brain Sci. 2019, 9, 170. [Google Scholar] [CrossRef] [Green Version]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Carlesimo, G.; Caltagirone, C.; Gainotti, G.; Fadda, L.; Gallassi, R.; Lorusso, S.; Marfia, G.; Marra, C.; Nocentini, U.; Parnetti, L. The mental deterioration battery: Normative data, diagnostic reliability and qualitative analyses of cognitive impairment. Eur. Neurol. 1996, 36, 378–384. [Google Scholar] [CrossRef]
- Ghafar, M.; Miptah, H.; O’Caoimh, R. Cognitive screening instruments to identify vascular cognitive impairment: A systematic review. Int. J. Geriatr. Psychiatry. 2019, 34, 1114–1127. [Google Scholar] [CrossRef]
- Lucas, J.A.; Ivnik, R.J.; Smith, G.E.; Bohac, D.L.; Tangalos, E.G.; Graff-Radford, N.R.; Petersen, R.C. Mayo’s older americans normative studies: Category fluency norms. J. Clin. Exp. Neuropsychol. 1998, 20, 194–200. [Google Scholar] [CrossRef]
- Osterrieth, P.A. Test of copying a complex figure; contribution to the study of perception and memory. Arch. Psychol. 1944, 30, 206–355. [Google Scholar]
- Reitan, R.M. Validity of the Trail Making Test as an indicator of organic brain damage. Percept. Mot. Skills 1958, 8, 271–276. [Google Scholar] [CrossRef]
- Reitan, R.M. The relation of the Trail Making Test to organic brain damage. J. Consult. Psychol 1955, 19, 393–394. [Google Scholar] [CrossRef] [PubMed]
- Barbarotto, R.; Laiacona, M.; Frosio, R.; Vecchio, M.; Farinato, A.; Capitani, E. A normative study on visual reaction times and two Stroop colour-word tests. Neurol. Sci. 1998, 19, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Nyström, O.; Wallin, A.; Nordlund, A.I.K. MCI of different etiologies differ on the Cognitive Assessment Battery. Acta Neurol. Scand. 2014, 132, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [Green Version]
- Marin, R.S. Apathy: A neuropsychiatric syndrome. J. Neuropsychiatry Clin. Neurosci. 1991, 3, 243–254. [Google Scholar] [CrossRef]
- Cerasa, A.; Quattrone, A.; Piras, F.; Mangone, G.; Magariello, A.; Fagioli, S.; Girardi, P.; Muglia, M.; Caltagirone, C.; Spalletta, G. 5-HTTLPR, anxiety and gender interaction moderates right amygdala volume in healthy subjects. Soc. Cogn. Affect. Neurosci. 2013, 9, 1537–1545. [Google Scholar] [CrossRef] [Green Version]
- Spielberger, C.D. State-Trait Anger Expression Inventory. In The Corsini Encyclopedia of Psychology; John Wiley & Sons: New York, NY, USA, 2010; p. 1. [Google Scholar]
- Hamilton, M.C.; Schutte, N.S.; Malouff, J.M. Hamilton Anxiety Scale (HAMA); Hamilton, M.C., Ed.; Source Book of Adult Assessment (Applied Clinical Psychology); Plenum Press: New York, NY, USA, 1959; pp. 154–157. [Google Scholar]
- Spielberger, C.D.; Sydeman, S.J. State-trait anxiety inventory and state-trait anger expression inventory. In The Use of Psychological Testing for Treatment Planning and Outcome Assessment; Maruish, M.E., Ed.; Erlbaum Psych Press: Hillsdale, NJ, USA, 1994; pp. 292–321. ISBN 978-0-8058-1162-9. [Google Scholar]
- Chalder, T.; Berelowitz, G.; Pawlikowska, T.; Watts, L.; Wessely, S.; Wright, D.; Wallace, E. Development of a fatigue scale. J. Psychosom. Res. 1993, 37, 147–153. [Google Scholar] [CrossRef] [Green Version]
- Clegg, A.P.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Loge, J.H.; Ekeberg, Ø.; Kaasa, S. Fatigue in the general norwegian population. J. Psychosom. Res. 1998, 45, 53–65. [Google Scholar] [CrossRef]
- Deichmann, R.; Schwarzbauer, C.; Turner, R. Optimisation of the 3D MDEFT sequence for anatomical brain imaging: Technical implications at 1.5 and 3 T. NeuroImage 2004, 21, 757–767. [Google Scholar] [CrossRef]
- Ashburner, J.; Friston, K.J. Unified segmentation. NeuroImage 2005, 26, 839–851. [Google Scholar] [CrossRef] [PubMed]
- Coupé, P.; Yger, P.; Barillot, C. Fast Non Local Means Denoising for 3D MR Images. In Lecture Notes Computer Science; Springer: Berlin/Heidelberg, Germany, 2006; Volume 9, pp. 33–40. [Google Scholar] [CrossRef] [Green Version]
- Wiest-Daesslé, N.; Prima, S.; Coupé, P.; Morrissey, S.P.; Barillot, C. Rician Noise Removal by Non-Local Means Filtering for Low Signal-to-Noise Ratio MRI: Applications to DT-MRI. Lect. Notes Comput. Sci. 2008, 11, 171–179. [Google Scholar] [CrossRef] [Green Version]
- Manjón, J.V.; Tohka, J.; Garcia-Martí, G.; Carbonell-Caballero, J.; Lull, J.J.; Martí-Bonmatí, L.; Robles, M. Robust MRI brain tissue parameter estimation by multistage outlier rejection. Magn. Reson. Med. 2008, 59, 866–873. [Google Scholar] [CrossRef]
- Cuadra, M.B.; Cammoun, L.; Butz, T.; Cuisenaire, O.; Thiran, J.-P. Comparison and validation of tissue modelization and statistical classification methods in T1-weighted MR brain images. IEEE Trans. Med. Imaging 2005, 24, 1548–1565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashburner, J. A fast diffeomorphic image registration algorithm. Neuroimage 2007, 38, 95–113. [Google Scholar] [CrossRef] [PubMed]
- Bergouignan, L.; Chupin, M.; Czechowska, Y.; Kinkingnéhun, S.; Lemogne, C.; Le Bastard, G.; Lepage, M.; Garnero, L.; Colliot, O.; Fossati, P. Can voxel based morphometry, manual segmentation and automated segmentation equally detect hippocampal volume differences in acute depression? NeuroImage 2009, 45, 29–37. [Google Scholar] [CrossRef]
- Klein, A.; Andersson, J.; Ardekani, B.A.; Ashburner, J.; Avants, B.; Chiang, M.-C.; Christensen, G.E.; Collins, D.L.; Gee, J.; Hellier, P.; et al. Evaluation of 14 nonlinear deformation algorithms applied to human brain MRI registration. NeuroImage 2009, 46, 786–802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berk, K.N. Tolerance and Condition in Regression Computations. J. Am. Stat. Assoc. 1977, 72, 863. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics 5; Harper Collins Publisher: New York, NY, USA, 2007. [Google Scholar] [CrossRef]
- Appelman, A.P.; Exalto, L.G.; Van Der Graaf, Y.; Biessels, G.J.; Mali, W.P.; I Geerlings, M. White matter lesions and brain atrophy: More than shared risk factors? A systematic review. Cerebrovasc. Dis. 2009, 28, 227–242. [Google Scholar] [CrossRef]
- Desikan, R.S.; Ségonne, F.; Fischl, B.; Quinn, B.T.; Dickerson, B.C.; Blacker, D.; Buckner, R.L.; Dale, A.M.; Maguire, R.P.; Hyman, B.T.; et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 2006, 31, 968–980. [Google Scholar] [CrossRef]
- Mori, S.; Oishi, K.; Jiang, H.; Jiang, L.; Li, X.; Akhter, K.; Hua, K.; Faria, A.V.; Mahmood, A.; Woods, R.; et al. Stereotaxic white matter atlas based on diffusion tensor imaging in an ICBM template. Neuroimage 2008, 40, 570–582. [Google Scholar] [CrossRef] [Green Version]
- Lockhart, S.N.; Roach, A.E.M.; Luck, S.J.; Geng, J.J.; Beckett, L.A.; Carmichael, O.; DeCarli, C. White matter hyperintensities are associated with visual search behavior independent of generalized slowing in aging. Neuropsychology 2013, 52, 93–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, E.E.; Salat, D.H.; Jeng, J.; McCreary, C.R.; Fischl, B.; Schmahmann, J.D.; Dickerson, B.C.; Viswanathan, A.; Albert, M.S.; Blacker, D.; et al. Correlations between MRI white matter lesion location and executive function and episodic memory. Neurology 2011, 76, 1492–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prins, N.D.; Scheltens, P. White matter hyperintensities, cognitive impairment and dementia: An update. Nat. Rev. Neurol. 2015, 11, 157–165. [Google Scholar] [CrossRef]
- Reyes, S.; Viswanathan, A.; Godin, O.; Dufouil, C.; Benisty, S.; Hernandez, K.; Kurtz, A.; Jouvent, E.; O’Sullivan, M.; Czernecki, V.; et al. Apathy: A major symptom in CADASIL. Neurology 2009, 72, 905–910. [Google Scholar] [CrossRef] [PubMed]
- Staekenborg, S.S.; Koedam, E.L.; Henneman, W.J.; Stokman, P.; Barkhof, F.; Scheltens, P.; Van Der Flier, W.M. Progression of Mild Cognitive Impairment to Dementia. Stroke 2009, 40, 1269–1274. [Google Scholar] [CrossRef] [PubMed]
- Starkstein, S.E.; Mizrahi, R.; Capizzano, A.A. Neuroimaging correlates of apathy and depression in Alzheimer’s disease. J. Neuropsychiatry Clin. Neurosci. 2009, 21, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.J.; O’Brien, J.T.; Davis, S.; Ballard, C.G.; Barber, R.; Kalaria, R.N.; Perry, R.H. Ischemic Basis for Deep White Matter Hyperintensities in Major Depression. Arch. Gen. Psychiatry 2002, 59, 785–792. [Google Scholar] [CrossRef] [Green Version]
- Spalletta, G.; Piras, F.; Caltagirone, C.; Fagioli, S. Hippocampal multimodal structural changes and subclinical depression in healthy individuals. J. Affect. Disord. 2014, 154, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Starkstein, S.E.; Brockman, S. Apathy and Parkinson’s Disease. Curr. Treat. Opt. Neurol. 2011, 13, 267–273. [Google Scholar] [CrossRef]
- Spalletta, G.; Cravello, L.; Epiras, F.; Eiorio, M.; Sancesario, G.; Marchi, A.; Caltagirone, C.; Ecacciari, C. Rapid-onset apathy may be the only clinical manifestation after dorsal striatum hemorrhagic lesion. Alzheimer Dis. Assoc. Disord. 2013, 27, 192–194. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.; Di Iulio, F.; Varsi, A.E.; Gianni, W.; Sancesario, G.; Caltagirone, C.; Spalletta, G. Neuropsychiatric Predictors of Progression from Amnestic-Mild Cognitive Impairment to Alzheimer’s Disease: The Role of Depression and Apathy. J. Alzheimer Dis. 2010, 20, 175–183. [Google Scholar] [CrossRef] [Green Version]
- Roth, R.M.; Koven, N.S.; Pendergrass, J.C.; Flashman, L.A.; McAllister, T.W.; Saykin, A.J. Apathy and the processing of novelty in schizophrenia. Schizophr. Res. 2008, 98, 232–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torso, M.; Serra, L.; Giulietti, G.; Spano, B.; Tuzzi, E.; Koch, G.; Caltagirone, C.; Cercignani, M.; Bozzali, M. Strategic Lesions in the Anterior Thalamic Radiation and Apathy in Early Alzheimer’s Disease. PLoS ONE 2015, 10, e0124998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le Heron, C.; Apps, M.; Husain, M. The anatomy of apathy: A neurocognitive framework for amotivated behaviour. Neuropsychology 2018, 118, 54–67. [Google Scholar] [CrossRef]
- Harris, A.L.; Elder, J.; Schiff, N.D.; Victor, J.D.; Goldfine, A.M. Post-stroke apathy and hypersomnia lead to worse outcomes from acute rehabilitation. Transl. Stroke Res. 2013, 5, 292–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Starkstein, S.E.; Leentjens, A.F.G. The nosological position of apathy in clinical practice. J. Neurol. Neurosurg. Psychiatry 2008, 79, 1088–1092. [Google Scholar] [CrossRef]
- Nobis, L.; Husain, M. Apathy in Alzheimer’s disease. Curr. Opin. Behav. Sci. 2018, 22, 7–13. [Google Scholar] [CrossRef]
- Ayers, E.; Shapiro, M.; Holtzer, R.; Barzilai, N.; Milman, S.; Verghese, J. Symptoms of apathy independently predict incident frailty and disability in community-dwelling older adults. J. Clin. Psychiatry 2017, 78, 529–536. [Google Scholar] [CrossRef] [Green Version]
- Mendez, M.F.; Adams, N.L.; Lewandowski, K.S. Neurobehavioral changes associated with caudate lesions. Neurology 1989, 39, 349. [Google Scholar] [CrossRef]
- Bhatia, K.P.; Marsden, C. The behavioural and motor consequences of focal lesions of the basal ganglia in man. Brain 1994, 117, 859–876. [Google Scholar] [CrossRef] [PubMed]
- Engelborghs, S.; Marien, P.; Pickut, B.A.; Verstraeten, S.; De Deyn, P.P. Loss of psychic self-activation after paramedian bithalamic infarction. Stroke 2000, 31, 1762–1765. [Google Scholar] [CrossRef] [Green Version]
- Taylor, W.D.; Aizenstein, H.J.; Alexopoulos, G.S. The vascular depression hypothesis: Mechanisms linking vascular disease with depression. Mol. Psychiatry 2013, 18, 963–974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mezzapesa, D.M.; Rocca, M.A.; Pagani, E.; Comi, G.; Filippi, M. Evidence of subtle gray-matter pathologic changes in healthy elderly individuals with nonspecific white-matter hyperintensities. Arch. Neurol. 2003, 60, 1109–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Udaka, F.; Sawada, H.; Kameyama, M. White matter lesions and dementia: MRI-pathological correlation. Ann. N. Y. Acad. Sci. 2002, 977, 411–415. [Google Scholar] [CrossRef]
- Mega, M.S.; Cummings, J.L. Frontal-subcortical circuits and neuropsychiatric disorders. J. Neuropsychiatry Clin. Neurosci. 1994, 6, 358–370. [Google Scholar] [CrossRef] [PubMed]
- Tay, J.; Tuladhar, A.M.; Hollocks, M.J.; Brookes, R.L.; Tozer, D.J.; Barrick, T.R.; Husain, M.; De Leeuw, F.-E.; Markus, H.S. Apathy is associated with large-scale white matter network disruption in small vessel disease. Neurology 2019, 92, e1157–e1167. [Google Scholar] [CrossRef] [Green Version]
- Myers-Schulz, B.; Koenigs, M. Functional anatomy of ventromedial prefrontal cortex: Implications for mood and anxiety disorders. Mol. Psychiatry 2011, 17, 132–141. [Google Scholar] [CrossRef]
- Kim, M.J.; Whalen, P.J. The structural integrity of an amygdala-prefrontal pathway predicts trait anxiety. J. Neurosci. 2009, 29, 11614–11618. [Google Scholar] [CrossRef] [Green Version]
- Phan, K.L.; Orlichenko, A.; Boyd, E.; Angstadt, M.; Coccaro, E.F.; Liberzon, I.; Arfanakis, K. Preliminary evidence of white matter abnormality in the uncinate fasciculus in generalized social anxiety disorder. Biol. Psychiatry 2009, 66, 691–694. [Google Scholar] [CrossRef] [Green Version]
- Blackmon, K.; Barr, W.B.; Carlson, C.; Devinsky, O.; Dubois, J.; Pogash, D.; Quinn, B.T.; Kuzniecky, R.; Halgren, E.; Thesen, T. Structural evidence for involvement of a left amygdala-orbitofrontal network in subclinical anxiety. Psychiatry Res. Neuroimaging 2011, 194, 296–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cannistraro, A.P.; Rauch, S.L. Neural circuitry of anxiety: Evidence from structural and functional neuroimaging studies. Psychopharmacol. Bull. 2003, 37, 8–25. [Google Scholar] [PubMed]
- Morgan, M.A.; LeDoux, J.E. Differential contribution of dorsal and ventral medial prefrontal cortex to the acquisition and extinction of conditioned fear in rats. Behav. Neurosci. 1995, 109, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Arvanitakis, Z.; Fleischman, D.A.; Arfanakis, K.; Leurgans, S.E.; Barnes, L.L.; Bennett, D.A. Association of white matter hyperintensities and gray matter volume with cognition in older individuals without cognitive impairment. Brain Struct. Funct. 2015, 221, 2135–2146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pantoni, L. Pathophysiology of age-related cerebral white matter changes. Cerebrovasc. Dis. 2002, 13, 7–10. [Google Scholar] [CrossRef]
- Young, V.G.; Halliday, G.; Kril, J.J. Neuropathologic correlates of white matter hyperintensities. Neurololgy 2008, 71, 804–811. [Google Scholar] [CrossRef]
- Vinters, H.V.; Gilbert, J.J. Cerebral amyloid angiopathy: Incidence and complications in the aging brain. II. The distribution of amyloid vascular changes. Stroke 1983, 14, 924–928. [Google Scholar] [CrossRef] [Green Version]
- Villain, N.; Desgranges, B.; Viader, F.; De La Sayette, V.; Mézenge, F.; Landeau, B.; Baron, J.C.; Eustache, F.; Chételat, G. Relationships between hippocampal atrophy, white matter disruption, and gray matter hypometabolism in Alzheimer’s disease. J. Neurosci. 2008, 28, 6174–6181. [Google Scholar] [CrossRef] [PubMed]

| HC (WMH−) (n = 30) | HC (WMH+) (n = 30) | ||||
|---|---|---|---|---|---|
| Variables | Mean (SD) | Mean (SD) | t | df | P |
| Age | 64 (7) | 64.6 (7) | −0.37 | 58 | 0.7 |
| Education | 13.8 (3.1) | 12.23 (3.3) | 1.79 | 58 | 0.07 |
| Mini Mental State Examination (MMSE) | 29.23 (0.89) | 29.10 (1.21) | 0.48 | 58 | 0.63 |
| Model | Predictor | ||||
|---|---|---|---|---|---|
| Neuropsychological Variables | χ2(1df) | p Value | OR | 95% CI | p Value |
| MDB Rey’s 15-word Immediate Recall (RIR) | 1.12 | 0.29 | 0.97 | 0.92–1.03 | 0.30 |
| MDB Rey’s 15-word Delayed Recall (RDR) | 0.39 | 0.53 | 0.94 | 0.78–1.14 | 0.53 |
| Copy of Rey–Osterrieth Complex Figure Test (RROF) | 3.34 | 0.07 | 0.85 | 0.71–1.02 | 0.09 |
| Recall of Rey–Osterrieth Complex Figure Test (RROF) | 4.29 | 0.04 | 0.90 | 0.81–1.0 | 0.047 |
| Stroop test-word reading (STwr)-time (s) | 2.01 | 0.15 | 1.18 | 0.93–1.50 | 0.17 |
| Stroop test-color naming (STcn)-time (s) | 4.53 | 0.03 | 1.17 | 1.0–1.36 | 0.05 |
| Stroop test-interference (STi)-time (s) | 1.80 | 0.18 | 1.04 | 0.98–1.11 | 0.20 |
| Raven’s Progressive Matrices ‘47 | 3.77 | 0.05 | 0.90 | 0.80–1.0 | 0.06 |
| Copying Drawings | 2.23 | 0.13 | 0.69 | 0.41–1.14 | 0.14 |
| Copying Drawings with Landmarks | 3.94 | 0.05 | 0.87 | 0.74–1.01 | 0.07 |
| Double Barrage Test (DBT)-time (s) | 2.21 | 0.14 | 1.02 | 1.0–1.05 | 0.17 |
| Double Barrage Test (DBT)-Recognition | 0.67 | 0.41 | 1.14 | 0.82–1.58 | 0.42 |
| Double Barrage Test (DBT)-False | 0.06 | 0.80 | 1.13 | 0.43–2.93 | 0.80 |
| Trail Making Test (TMT A)-time (s) | 2.63 | 0.10 | 1.02 | 1.0–1.06 | 0.14 |
| Trail Making Test (TMT B)-time (s) | 6.94 | 0.001 | 1.02 | 1.0–1.04 | 0.04 |
| Phonological verbal fluency | 0.58 | 0.45 | 0.98 | 0.94–1.03 | 0.45 |
| Semantic verbal fluency | 0.70 | 0.40 | 0.97 | 0.88–1.05 | 0.40 |
| Wisconsin Card Sorting Test (WCST)-Pers Err | 0.32 | 0.57 | 1.18 | 0.65–2.12 | 0.58 |
| Wisconsin Card Sorting Test (WCST)-non Pers Err | 1.68 | 0.19 | 1.46 | 0.8–2.68 | 0.21 |
| Neuropsychiatric variables | |||||
| Hamilton Depression Rating Scale score | 2.82 | 0.09 | 1.12 | 0.98–1.28 | 0.11 |
| Beck depression inventory (BDI) score | 6.44 | 0.01 | 1.18 | 1.03–1.36 | 0.02 |
| Apathy Rating Scale (ARS) score | 6.40 | 0.01 | 1.18 | 1.03–1.35 | 0.01 |
| State Anxiety Inventory Stai Y 1 score | 10.66 | 0.001 | 1.18 | 1.05–1.31 | 0.003 |
| Trait Anxiety Inventory Stai-Y 2 score | 7.88 | 0.005 | 1.11 | 1.02–1.22 | 0.01 |
| Hamilton Anxiety Rating Scale (HAMA) score | 1.24 | 0.27 | 1.06 | 0.95–1.17 | 0.28 |
| State-Trait Anger Expression Inventory (STAXI)-S score | 1.07 | 0.30 | 1.91 | 0.39–9-48 | 0.43 |
| State-Trait Anger Expression Inventory (STAXI)-T score | 4.76 | 0.03 | 1.17 | 1.0–1.35 | 0.04 |
| State-Trait Anger Expression Inventory (STAXI)-R score | 4.05 | 0.04 | 1.07 | 1.0–1.14 | 0.06 |
| Fatigue Rating Scale score | 7.65 | 0.005 | 1.24 | 1.04–1.48 | 0.02 |
| Model | Predictor | ||||
|---|---|---|---|---|---|
| Neuropsychiatric Variables | χ2(6df) | p Value | AOR | 95% CI | p Value |
| Whole model fit | 20.70 | 0.002 | |||
| Beck depression inventory (BDI) score | 0.99 | 0.79–1.26 | 0.98 | ||
| Apathy Rating Scale (ARS) score | 1.20 | 0.99–1.44 | 0.04 | ||
| State Anxiety Inventory Stai Y 1 score | 1.51 | 1.0–1.32 | 0.04 | ||
| Trait Anxiety Inventory-Stai Y 2 score | 0.98 | 0.85–1.12 | 0.73 | ||
| State-Trait Anger Expression Inventory (STAXI)-T score | 1.04 | 0.86–1.25 | 0.70 | ||
| Fatigue Rating Scale score | 1.24 | 0.97–1.59 | 0.09 | ||
| Participant | Periventricular WMH Volume | Subcortical WMH Volume | Total WMH Volume |
|---|---|---|---|
| 1 | 3012 | 281 | 3293 |
| 2 | 5853 | 1783 | 7636 |
| 3 | 4453 | 1236 | 5689 |
| 4 | 2237 | 172 | 2409 |
| 5 | 1483 | 275 | 1758 |
| 6 | 84 | 835 | 919 |
| 7 | 2008 | 410 | 2418 |
| 8 | 6317 | 5329 | 11646 |
| 9 | 2014 | 198 | 2212 |
| 10 | 920 | 272 | 1192 |
| 11 | 1187 | 4708 | 5895 |
| 12 | 1878 | 528 | 2406 |
| 13 | 939 | 1055 | 1994 |
| 14 | 8801 | 22,727 | 31,528 |
| 15 | 1287 | 1273 | 2560 |
| 16 | 4895 | 1301 | 6196 |
| 17 | 13362 | 16,489 | 29,851 |
| 18 | 2445 | 674 | 3119 |
| 19 | 15436 | 21,103 | 36,539 |
| 20 | 1621 | 541 | 2162 |
| 21 | 3973 | 1234 | 5207 |
| 22 | 5643 | 2537 | 8180 |
| 23 | 4493 | 1513 | 6006 |
| 24 | 7378 | 6072 | 13450 |
| 25 | 2022 | 317 | 2339 |
| 26 | 6421 | 3796 | 10217 |
| 27 | 8271 | 3815 | 12,086 |
| 28 | 2990 | 1324 | 4314 |
| 29 | 5248 | 2967 | 8215 |
| 30 | 3156 | 1507 | 4663 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spalletta, G.; Iorio, M.; Vecchio, D.; Piras, F.; Ciullo, V.; Banaj, N.; Sensi, S.L.; Gianni, W.; Assogna, F.; Caltagirone, C.; et al. Subclinical Cognitive and Neuropsychiatric Correlates and Hippocampal Volume Features of Brain White Matter Hyperintensity in Healthy People. J. Pers. Med. 2020, 10, 172. https://doi.org/10.3390/jpm10040172
Spalletta G, Iorio M, Vecchio D, Piras F, Ciullo V, Banaj N, Sensi SL, Gianni W, Assogna F, Caltagirone C, et al. Subclinical Cognitive and Neuropsychiatric Correlates and Hippocampal Volume Features of Brain White Matter Hyperintensity in Healthy People. Journal of Personalized Medicine. 2020; 10(4):172. https://doi.org/10.3390/jpm10040172
Chicago/Turabian StyleSpalletta, Gianfranco, Mariangela Iorio, Daniela Vecchio, Federica Piras, Valentina Ciullo, Nerisa Banaj, Stefano L. Sensi, Walter Gianni, Francesca Assogna, Carlo Caltagirone, and et al. 2020. "Subclinical Cognitive and Neuropsychiatric Correlates and Hippocampal Volume Features of Brain White Matter Hyperintensity in Healthy People" Journal of Personalized Medicine 10, no. 4: 172. https://doi.org/10.3390/jpm10040172






