A Predictive Model and Risk Factors for Case Fatality of COVID-19
Abstract
:1. Introduction
2. Patients and Methods
2.1. Study Design and Patient Cohort
- Extremely low level corresponds to less than or equal to 80%.
- Low level between 81% and 90%.
- Medium between 91% and 94%.
- Adequate to >94%.
2.2. Data Analysis
2.3. Ethical Approval
3. Results
3.1. Patients Characteristics
3.2. Empirical Model and Results
3.3. Robustness Check
3.4. Final Models and Interpretation
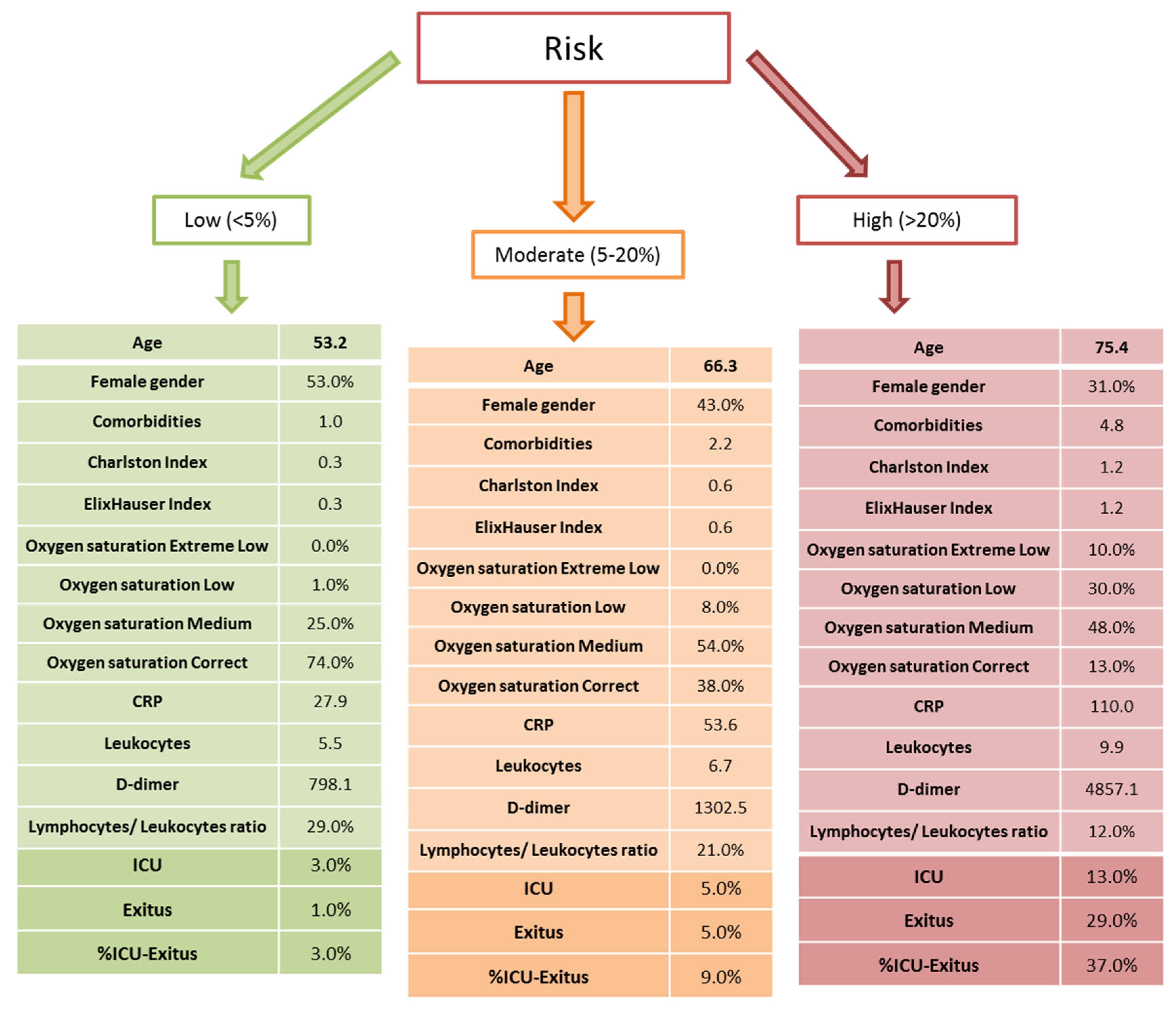
3.5. Categories of Individualized Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | Coronavirus disease 2019 |
| RT-qPCR | Real-time reverse transcription polymerase chain reaction |
| ICU | Intensive care unit |
| CRP | C-reactive protein |
References
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lai, C.-C.; Wang, C.-Y.; Wang, Y.-H.; Hsueh, S.-C.; Ko, W.-C.; Hsueh, P.-R. Global epidemiology of coronavirus disease 2019 (COVID-19): Disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int. J. Antimicrob. Agents 2020, 55, 105946. [Google Scholar] [CrossRef] [PubMed]
- Ceylan, Z. Estimation of COVID-19 prevalence in Italy, Spain, and France. Sci. Total. Environ. 2020, 729, 138817. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Mo, P.; Xing, Y.; Xiao, Y.; Deng, L.; Zhao, Q.; Wang, H.; Xiong, Y.; Cheng, Z.; Gao, S.; Liang, K.; et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [Green Version]
- Peng, Y.D.; Meng, K.; Guan, H.Q. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi 2020, 48, E004. [Google Scholar] [CrossRef]
- Available online: https://covid19.who.int/region/euro/country/es (accessed on 5 November 2020).
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Zheng, Z.; Peng, F.; Xu, B.; Zhao, J.; Liu, H.; Peng, J.; Li, Q.; Jiang, C.; Zhou, Y.; Liu, S.; et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020, 81, e16–e25. [Google Scholar] [CrossRef]
- Li, K.; Wu, J.; Wu, F.; Guo, D.; Chen, L.; Fang, Z.; Li, C. The Clinical and Chest CT Features Associated With Severe and Critical COVID-19 Pneumonia. Investig. Radiol. 2020, 55, 327–331. [Google Scholar] [CrossRef]
- Pourbagheri-Sigaroodi, A.; Bashash, D.; Fateh, F.; Abolghasemi, H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin. Chim. Acta 2020, 510, 475–482. [Google Scholar] [CrossRef]
- Shen, B.; Yi, X.; Sun, Y.; Bi, X.; Du, J.; Zhang, C.; Quan, S.; Zhang, F.; Sun, R.; Qian, L.; et al. Proteomic and Metabolomic Characterization of COVID-19 Patient Sera. Cell 2020, 182, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Cevik, M.; Bamford, C.; Ho, A. COVID-19 pandemic—A focused review for clinicians. Clin. Microbiol. Infect. 2020, 26, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Cuñarro-López, Y.; Cano-Valderrama, Ó.; Pintado-Recarte, P.; Cueto-Hernández, I.; González-Garzón, B.; García-Tizón, S.; Buján, J.; Asúnsolo, Á.; Ortega, M.A.; De León-Luis, J.A. Maternal and Perinatal Outcomes in Patients with Suspected COVID-19 and Their Relationship with a Negative RT-PCR Result. J. Clin. Med. 2020, 9, 3552. [Google Scholar] [CrossRef]
- Dixon, B.E.; Wools-Kaloustian, K.; Fadel, W.F.; Duszynski, T.J.; Yiannoutsos, C.; Halverson, P.K.; Menachemi, N. Symptoms and symptom clusters associated with SARS-CoV-2 infection in community-based populations: Results from a statewide epidemiological study. medRxiv 2020. [Google Scholar] [CrossRef]
- Swann, O.V.; Holden, K.A.; Turtle, L.C.W.; Pollock, L.; Fairfield, C.J.; Drake, T.M.; Seth, S.; Fegan, C.; Hardwick, H.E.; Halpin, S.; et al. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: Prospective multicentre observational cohort study. BMJ 2020, 370. [Google Scholar] [CrossRef]
- Rubio-Rivas, M.; Corbella, X.; Mora-Luján, J.M.; Loureiro-Amigo, J.; Sampalo, A.L.; Bergua, C.Y.; Atiénzar, P.J.E.; García, L.F.D.; Ferrer, R.G.; Canteli, S.P.; et al. Predicting Clinical Outcome with Phenotypic Clusters in COVID-19 Pneumonia: An Analysis of 12,066 Hospitalized Patients from the Spanish Registry SEMI-COVID-19. J. Clin. Med. 2020, 9, 3488. [Google Scholar] [CrossRef]
- Initiative, F.T.S.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Lescure, F.-X.; Bouadma, L.; Nguyen, D.; Parisey, M.; Wicky, P.-H.; Behillil, S.; Gaymard, A.; Bouscambert-Duchamp, M.; Donati, F.; Le Hingrat, Q.; et al. Clinical and virological data of the first cases of COVID-19 in Europe: A case series. Lancet Infect. Dis. 2020, 20, 697–706. [Google Scholar] [CrossRef] [Green Version]
- Lagergren, J.; Brusselaers, N. The Charlson Comorbidity Index in Registry-based Research. Methods Inf. Med. 2017, 56, 401–406. [Google Scholar] [CrossRef]
- Elixhauser, A.; Steiner, C.; Harris, D.R.; Coffey, R.M. Comorbidity Measures for Use with Administrative Data. Med. Care 1998, 36, 8–27. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, S.M.; Lee, S. A unified approach to interpreting model predictions. Adv. Neural Inf. Process. Syst. 2017, 30, 1–10. [Google Scholar]
- Escobar, G.J.; Liu, V.X.; Schuler, A.; Lawson, B.; Greene, J.D.; Kipnis, P. Automated Identification of Adults at Risk for In-Hospital Clinical Deterioration. N. Engl. J. Med. 2020, 383, 1951–1960. [Google Scholar] [CrossRef] [PubMed]
- Allenbach, Y.; Saadoun, D.; Maalouf, G.; Vieira, M.; Hellio, A.; Boddaert, J.; Gros, H.; Salem, J.E.; Rigon, M.R.; Menyssa, C.; et al. Development of a multivariate prediction model of intensive care unit transfer or death: A French prospective cohort study of hospitalized COVID-19 patients. PLoS ONE 2020, 15, e0240711. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Hungerford, D.; Chen, H.; Abrams, S.T.; Li, S.; Wang, G.; Wang, Y.; Kang, H.; Bonnett, L.; Zheng, R.; et al. 2020. Development and external validation of a prognostic multivariable model on admission for hospitalized patients with COVID-19. MedRxiv 2020, 3, 20045997. Available online: https://www.medrxiv.org/content/10.1101/2020.03.28.20045997v2 (accessed on 7 November 2020).
- Velavan, T.P.; Meyer, C.G. Mild versus severe COVID-19: Laboratory markers. Int. J. Infect. Dis. 2020, 95, 304–307. [Google Scholar] [CrossRef]
- Akhavan, A.R.; Habboushe, J.P.; Gulati, R.; Iheagwara, O.; Watterson, J.; Thomas, S.; Swartz, J.L.; Koziatek, C.A.; Lee, D.C. Risk Stratification of COVID-19 Patients Using Ambulatory Oxygen Saturation in the Emergency Department. West. J. Emerg. Med. 2020, 21, 5–14. [Google Scholar] [CrossRef]
- O’Carroll, O.; MacCann, R.; O’Reilly, A.; Dunican, E.M.; Feeney, E.R.; Ryan, S.; Cotter, A.; Mallon, P.W.; Keane, M.P.; Butler, M.W.; et al. Remote monitoring of oxygen saturation in individuals with COVID-19 pneumonia. Eur. Respir. J. 2020, 56, 2001492. [Google Scholar] [CrossRef]
- Bhatraju, P.K.; Ghassemieh, B.J.; Nichols, M.; Kim, R.; Jerome, K.R.; Nalla, A.K.; Greninger, A.L.; Pipavath, S.; Wurfel, M.M.; Evans, L.; et al. Covid-19 in Critically Ill Patients in the Seattle Region—Case Series. N. Engl. J. Med. 2020, 382, 2012–2022. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Chen, A.; Hou, W.; Graham, J.M.; Li, H.; Richman, P.S.; Thode, H.C.; Singer, A.J.; Duong, T. Prediction model and risk scores of ICU admission and mortality in COVID-19. PLoS ONE 2020, 15, e0236618. [Google Scholar] [CrossRef]
- Luo, X.; Zhou, W.; Yan, X.; Guo, T.; Wang, B.; Xia, H.; Ye, L.; Xiong, J.; Jiang, Z.; Liu, Y.; et al. Prognostic Value of C-Reactive Protein in Patients With Coronavirus 2019. Clin. Infect. Dis. 2020, 71, 2174–2179. [Google Scholar] [CrossRef] [PubMed]
- Koozi, H.; Lengquist, M.; Frigyesi, A. C-reactive protein as a prognostic factor in intensive care admissions for sepsis: A Swedish multicenter study. J. Crit. Care 2020, 56, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Li, L.; Xu, M.; Wu, J.; Luo, D.; Zhu, Y.; Li, B.; Song, X.; Zhou, X. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J. Clin. Virol. 2020, 127, 104370. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Huang, Y.; Shi, F.; Tan, K.; Ma, Q.; Chen, Y.; Jiang, X.; Li, X. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J. Med. Virol. 2020, 92, 856–862. [Google Scholar] [CrossRef] [Green Version]
- Wang, L. C-reactive protein levels in the early stage of COVID-19. Médecine Mal. Infect. 2020, 50, 332–334. [Google Scholar] [CrossRef]
- Bastug, A.; Bodur, H.; Erdogan, S.; Gokcinar, D.; Kazancioglu, S.; Kosovali, B.D.; Ozbay, B.O.; Gok, G.; Turan, I.O.; Yilmaz, G.; et al. Clinical and laboratory features of COVID-19: Predictors of severe prognosis. Int. Immunopharmacol. 2020, 88, 106950. [Google Scholar] [CrossRef]
- Larsson, E.; Brattström, O.; Agvald-Öhman, C.; Grip, J.; Jalde, F.C.; Strålin, K.; Nauclér, P.; Oldner, A.; Konrad, D.; Persson, B.P.; et al. Characteristics and outcomes of patients with COVID-19 admitted to ICU in a tertiary hospital in Stockholm, Sweden. Acta Anaesthesiol. Scand. 2021, 65, 76–81. [Google Scholar] [CrossRef]
- Krieger, N.; Waterman, P.D.; Chen, J.T. COVID-19 and Overall Mortality Inequities in the Surge in Death Rates by Zip Code Characteristics: Massachusetts, January 1 to May 19, 2020. Am. J. Public Health 2020, 110, e1–e3. [Google Scholar] [CrossRef]
- Krieger, N.; Chen, J.T.; Waterman, P.D. Excess mortality in men and women in Massachusetts during the COVID-19 pandemic. Lancet 2020, 395, 1829. [Google Scholar] [CrossRef]
- Sanyaolu, A.O.; Okorie, C.; Marinkovic, A.; Patidar, R.; Younis, K.; Desai, P.; Hosein, Z.; Padda, I.; Mangat, J.; Altaf, M. Comorbidity and its Impact on Patients with COVID-19. SN Compr. Clin. Med. 2020, 2, 1069–1076. [Google Scholar] [CrossRef]
- Słomka, A.; Kowalewski, M.; Żekanowska, E. Coronavirus Disease 2019 (COVID–19): A Short Review on Hematological Manifestations. Pathogens 2020, 9, 493. [Google Scholar] [CrossRef] [PubMed]
- Haase, N.; Plovsing, R.; Christensen, S.; Poulsen, L.M.; Brøchner, A.C.; Rasmussen, B.S.; Helleberg, M.; Jensen, J.U.S.; Andersen, L.P.K.; Siegel, H.; et al. Characteristics, interventions, and longer term outcomes of COVID-19 ICU patients in Denmark—A nationwide, observational study. Acta Anaesthesiol. Scand. 2021, 65, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Roncon, L.; Zuin, M.; Rigatelli, G.; Zuliani, G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J. Clin. Virol. 2020, 127, 104354. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [Green Version]
- Palaiodimos, L.; Kokkinidis, D.G.; Li, W.; Karamanis, D.; Ognibene, J.; Arora, S.; Southern, W.N.; Mantzoros, C.S. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020, 108, 154262. [Google Scholar] [CrossRef]
- Gebhard, C.; Regitz-Zagrosek, V.; Neuhauser, H.K.; Morgan, R.; Klein, S.L. Impact of sex and gender on COVID-19 outcomes in Europe. Biol. Sex Differ. 2020, 11, 1–13. [Google Scholar] [CrossRef]
- Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.A.M.P.J.; Kant, K.M.; Kaptein, F.H.J.; van Paassen, J.; Stals, M.A.M.; Huisman, M.V.; et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020, 191, 145–147. [Google Scholar] [CrossRef]
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Gandet, F.F.; et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensiv. Care Med. 2020, 46, 1089–1098. [Google Scholar] [CrossRef]
- Zhang, L.; Yan, X.; Fan, Q.; Liu, H.; Liu, X.; Liu, Z.; Zhang, Z. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J. Thromb. Haemost. 2020, 18, 1324–1329. [Google Scholar] [CrossRef]
- Thierry, A.R. Host/genetic factors associated with COVID-19 call for precision medicine. Precis. Clin. Med. 2020, 3, 228–234. [Google Scholar] [CrossRef]
- Thierry, A.R.; Roch, B. Neutrophil Extracellular Traps and By-Products Play a Key Role in COVID-19: Pathogenesis, Risk Factors, and Therapy. J. Clin. Med. 2020, 9, 2942. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Han, P.; Wu, J.; Gong, J.; Tian, D.-A. Prevalence and predictive value of hypocalcemia in severe COVID-19 patients. J. Infect. Public Health 2020, 13, 1224–1228. [Google Scholar] [CrossRef] [PubMed]
| CH-HM | MH-HUPA | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| Group | Comorbidities | % | OR | % | OR | % | OR | Weight |
| Hypertension | Arterial hypertension | 42.5% | 1.90 | 65.6% | 1.77 | 45.6% | 1.90 | 1.90 |
| Total | 42.5% | 1.90 | 65.6% | 1.77 | 45.6% | 1.90 | - | |
| Cardiopathies | COR pulmonale | 6.8% | 2.37 | 9.8% | 1.67 | 7.3% | 2.14 | 2.33 |
| Ischemic heart disease | 6.9% | 1.69 | 10.4% | 1.72 | 7.1% | 1.77 | 1.81 | |
| Heart failure | 4.8% | 2.13 | 10.8% | 3.54 | 6.6% | 2.98 | 2.15 | |
| Total | 15.8% | 2.21 | 25.5% | 2.48 | 17.5% | 2.44 | - | |
| Metabolic–endocrine | Diabetes | 17.3% | 1.44 | 30.6% | 1.48 | 20.1% | 1.53 | 1.39 |
| Hypothyroidism | 6.8% | 0.74 | 6.8% | 0.73 | 6.3% | 0.70 | 0.85 | |
| Obesity | 7.5% | 1.16 | 13.5% | 1.23 | 8.8% | 1.35 | 1.17 | |
| Total | 28.1% | 1.21 | 42.6% | 1.30 | 30.3% | 1.31 | - | |
| Respiratory illnesses | ASTHMA | 4.7% | 0.91 | 11.6% | 0.68 | 6.4% | 0.78 | 1.05 |
| COPD | 7.8% | 2.20 | 12.2% | 1.79 | 7.9% | 2.18 | 2.05 | |
| Others | 2.1% | 1.37 | 4.7% | 1.67 | 2.6% | 1.56 | 1.41 | |
| Total | 13.7% | 1.55 | 24.5% | 1.25 | 15.3% | 1.46 | - | |
| Nephropathies | Acute renal failure | 8.9% | 6.36 | 16.9% | 3.04 | 11.5% | 4.64 | 6.03 |
| Chronic renal failure | 5.6% | 2.22 | 13.7% | 2.20 | 7.3% | 2.50 | 2.85 | |
| Total | 11.8% | 4.97 | 25.0% | 2.66 | 15.1% | 3.91 | - | |
| Solid neoplasia | Colon cancer | 0.7% | 6.85 | 0.7% | 2.53 | 0.6% | 5.36 | 6.01 |
| Breast cancer | 0.5% | 1.81 | 0.3% | 2.02 | 0.4% | 1.57 | 2.14 | |
| Respiratory/lung cancer | 1.2% | 2.56 | 1.5% | 0.79 | 1.0% | 1.86 | 2.72 | |
| Total | 2.4% | 3.24 | 2.6% | 1.30 | 1.9% | 2.53 | - | |
| Hematological neoplasia | Leukemia | 0.9% | 1.63 | 1.4% | 2.55 | 0.9% | 2.06 | 1.65 |
| Lymphoma | 0.8% | 1.92 | 1.0% | 0.46 | 0.6% | 1.65 | 1.88 | |
| Multiple myeloma | 0.6% | 1.58 | 0.7% | 1.73 | 0.6% | 1.52 | 1.62 | |
| Total | 2.3% | 1.73 | 3.1% | 1.53 | 2.1% | 1.79 | - | |
| Autoimmune intestinalis | Ulcerative colitis | 0.5% | 1.81 | 0.4% | 1.21 | 0.5% | 1.47 | 1.81 |
| Total | 0.5% | 1.81 | 0.4% | 1.21 | 0.5% | 1.47 | - | |
| Autoimmune rheumatological | Rheumatoid arthritis | 1.1% | 0.66 | 2.1% | 1.52 | 1.4% | 1.28 | 0.81 |
| Spondyloarthritis | 3.5% | 1.45 | 3.0% | 1.63 | 3.0% | 1.28 | 1.42 | |
| Psoriasis | 0.8% | 1.05 | 2.4% | 0.47 | 1.0% | 0.70 | 1.12 | |
| Vasculitis | 1.5% | 1.70 | 4.3% | 1.20 | 2.5% | 1.28 | 1.61 | |
| Total | 6.6% | 1.33 | 11.6% | 1.22 | 7.7% | 1.23 | - | |
| Urinary infection | Urinary infection | 4.6% | 2.04 | 7.2% | 1.46 | 5.3% | 1.85 | 2.04 |
| Total | 4.6% | 2.04 | 7.2% | 1.46 | 5.3% | 1.85 | - | |
| Neurological | Dementia | 3.7% | 1.94 | 4.0% | 1.05 | 3.5% | 1.52 | 1.94 |
| Total | 3.7% | 1.94 | 4.0% | 1.05 | 3.5% | 1.52 | - | |
| CH-HM (n = 1931) | MH-HUPA (n = 1558) | Total (n = 3489) | |
|---|---|---|---|
| Age | 68.4 (16.3) | 66.7 (16.2) | 67.6 (16.3) |
| Female gender | 41.0% | 42.5% | 41.7% |
| Comorbidities | 2.9 (3.4) | 3.8 (4.3) | 3.3 (3.9) |
| Charlson Index | 0.7 (1.0) | 1.0 (1.3) | 0.9 (1.2) |
| Elixhauser Index | 1.8 (1.7) | 2.2 (2.2) | 2.0 (1.9) |
| Oxygen saturation extremely low | 4.0% | 4.9% | 4.4% |
| Oxygen saturation low | 16.7% | 14.3% | 15.7% |
| Oxygen saturation medium | 30.1% | 68.5% | 45.7% |
| Oxygen saturation correct | 49.1% | 12.2% | 34.2% |
| CRP (μg/dL) | 73.8 (85.3) | 75.0 (80.6) | 74.3 (83.4) |
| Leukocytes (103/L) | 7.8 (4.9) | 7.8 (5.0) | 7.8 (4.9) |
| D-dimer (mg/L) | 2480.9 (6952.8) | 3180.2 (14,092.7) | 2753.1 (10,338.2) |
| Lymphocyte/leukocyte ratio | 18.9% (11.0%) | 18.5% (11.0%) | 18.7% (11.2%) |
| ICU | 6.9% | 7.0% | 6.9% |
| Death | 14.4% | 20.9% | 17.3% |
| %ICU or death | 19.2% | 25.6% | 22.1% |
| %ICU and death | 2.1% | 2.3% | 2.1% |
| EM-1 | p-Value | EM-2 | p-Value | EM-3 a | p-Value | |
|---|---|---|---|---|---|---|
| Age | 0.0394 *** | 0.0000 | 0.0364 *** | 0.0000 | 0.0299 *** | 0.0000 |
| (0.0050) | (0.0052) | (0.0061) | ||||
| Female gender | −0.5482 *** | 0.0000 | −0.4613 *** | 0.0007 | −0.3935 * | 0.0159 |
| (0.1313) | (0.1369) | (0.1632) | ||||
| Comorbidities | 0.1190 *** | 0.0000 | 0.01253 *** | 0.0000 | 0.1233 *** | 0.0000 |
| (0.0175) | (0.0179) | (0.0210) | ||||
| Oxygen saturation extremely low | - | - | 2.4175 *** | 0.0000 | 1.7599 *** | 0.0000 |
| - | (0.2680) | (0.3074) | ||||
| Oxygen saturation low | - | - | 1.1536 *** | 0.0000 | 0.7813 *** | 0.0001 |
| - | (0.1666) | (0.2021) | ||||
| Oxygen saturation medium | - | - | 0.6068 *** | 0.0000 | 0.5772 ** | 0.0016 |
| (0.1561) | (0.1826) | |||||
| CRP (μg/dL) | - | - | - | - | 0.0031 *** | 0.0001 |
| - | - | (0.0008) | ||||
| Leukocytes (103/L) | - | - | - | - | 0.0596 *** | 0.0001 |
| - | - | (0.0154) | ||||
| Lymphocyte/leukocyte ratio | - | - | - | - | −3.8257 *** | 0.0000 |
| - | - | (0.8623) | ||||
| D-dimer/Reference value 1 | - | - | - | - | 0.0149 ** | 0.0011 |
| - | - | (0.0046) | ||||
| No. observations | 1.931 | - | 1.931 | - | 1.622 | - |
| AUC | 0.7470 | - | 0.7845 | - | 0.8187 | - |
| EM-3 | p-Value | EM-4 | p-Value | EM-5 | p-Value | |
|---|---|---|---|---|---|---|
| Age | 0.0299 *** | 0.0000 | −0.0386 *** | 0.0000 | −0.0342 *** | 0.0000 |
| (0.0061) | (0.0037) | (0.0060) | ||||
| Female gender | −0.3935 * | 0.0159 | −0.4541 ** | 0.0048 | −0.4593 ** | 0.0044 |
| (0.1632) | (0.1611) | (0.1937) | ||||
| Comorbidities | 0.1233 *** | 0.0000 | - | - | - | - |
| (0.0210) | - | - | ||||
| Charlson Index | - | - | 0.1898 ** | 0.0064 | - | |
| - | (0.0696) | - | ||||
| Elixhauser Index | - | - | - | - | 0.1937 *** | 0.0000 |
| - | - | (0.0451) | ||||
| Oxygen saturation extremely low | 1.7599 *** | 0.0000 | 1.7108 *** | 0.0000 | 1.6997 *** | 0.0000 |
| (0.3074) | (0.3058) | (0.3048) | ||||
| Oxygen saturation low | 0.7813 *** | 0.0001 | 0.8157 *** | 0.0000 | 0.8020 ** | 0.0001 |
| (0.2021) | (0.1995) | (0.1998) | ||||
| Oxygen saturation medium | 0.5772 ** | 0.0016 | 0.5751 ** | 0.0014 | 0.5818 ** | 0.0013 |
| (0.1826) | (0.1805) | (0.1813) | ||||
| CRP (μg/dL) | 0.0031 *** | 0.0001 | 0.0028 *** | 0.0002 | 0.0031 *** | 0.0001 |
| (0.0008) | (0.0008) | (0.0008) | ||||
| Leukocytes (103/L) | 0.0596 *** | 0.0001 | 0.0612 *** | 0.0000 | 0.0623 *** | 0.0000 |
| (0.0154) | (0.0151) | (0.0153) | ||||
| Lymphocyte/leukocyte ratio | −3.8257 *** | 0.0000 | −3.9553 *** | 0.0000 | −3.8329 *** | 0.0000 |
| (0.8623) | (0.8534) | (0.8623) | ||||
| D-dimer/Reference value 1 | 0.0149 ** | 0.0011 | 0.0155 *** | 0.0009 | 0.0149 ** | 0.0013 |
| (0.0046) | (0.0047) | (0.0046) | ||||
| No. Observations | 1.622 | - | 1.622 | - | 1.622 | - |
| AUC | 0.8187 | - | 0.8059 | - | 0.8107 | - |
| EM-1 | EM-2 | EM-3 | |
|---|---|---|---|
| AUC CH-HM | 0.7494 | 0.7862 | 0.8247 |
| AUC MH-HUPA | 0.7273 | 0.7773 | 0.8076 |
| EM-6 | p-Value | EM-7 | p-Value | EM-8 | p-Value | |
|---|---|---|---|---|---|---|
| Age | 0.0417 *** | 0.0000 | 0.0393 *** | 0.0000 | 0.0254 *** | 0.0000 |
| (0.0035) | (0.0038) | (0.0044) | ||||
| Female gender | −0.4843 *** | 0.0000 | −3762 *** | 0.0001 | −0.2733 * | 0.0229 |
| (0.0912) | (0.1369) | (0.1632) | ||||
| Comorbidities | 0.0964 *** | 0.0000 | 0.0888 *** | 0.0000 | 0.0830 *** | 0.0000 |
| (0.0122) | (0.0132) | (0.0140) | ||||
| Oxygen saturation extremely low | - | - | 3.1240 *** | 0.0000 | 2.4006 *** | 0.0000 |
| - | (0.2255) | (0.2571) | ||||
| Oxygen saturation low | - | - | 1.4683 *** | 0.0000 | 1.0468 *** | 0.0000 |
| - | (0.1400) | (0.1687) | ||||
| Oxygen saturation medium | - | - | 0.7976 *** | 0.0000 | 0.6528 *** | 0.0000 |
| (0.1218) | (0.1474) | |||||
| CRP (μg/dL) | - | - | - | - | 0.0039 *** | 0.0000 |
| - | - | (0.0006) | ||||
| Leukocytes (103/L) | - | - | - | - | 0.0562 *** | 0.0000 |
| - | - | (0.0105) | ||||
| Lymphocyte/leukocyte ratio | - | - | - | - | −3.1445 *** | 0.0000 |
| - | - | (0.6027) | ||||
| D-dimer/Reference value 1 | - | - | - | - | 0.0206 *** | 0.0000 |
| - | - | (0.0041) | ||||
| No. Observations | 3.489 | - | 3.247 | - | 2.664 | - |
| AUC | 0.7317 | - | 0.7841 | - | 0.8177 | - |
| EM-6 | EM-7 | EM-8 | |
|---|---|---|---|
| Age | 50.9% | 36.2% | 17.7% |
| Female gender | 24.4% | 12.6% | 6.9% |
| Comorbidities | 24.7% | 16.5% | 12.5% |
| Oxygen saturation | - | 34.6% | 20.3% |
| CRP (μg/dL) | - | - | 12.5% |
| Leukocytes (103/L) | - | - | 8.9% |
| Lymphocyte/leukocyte ratio | - | - | 14.4% |
| D-dimer (mg/L) | - | - | 6.7% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Álvarez-Mon, M.; Ortega, M.A.; Gasulla, Ó.; Fortuny-Profitós, J.; Mazaira-Font, F.A.; Saurina, P.; Monserrat, J.; Plana, M.N.; Troncoso, D.; Moreno, J.S.; et al. A Predictive Model and Risk Factors for Case Fatality of COVID-19. J. Pers. Med. 2021, 11, 36. https://doi.org/10.3390/jpm11010036
Álvarez-Mon M, Ortega MA, Gasulla Ó, Fortuny-Profitós J, Mazaira-Font FA, Saurina P, Monserrat J, Plana MN, Troncoso D, Moreno JS, et al. A Predictive Model and Risk Factors for Case Fatality of COVID-19. Journal of Personalized Medicine. 2021; 11(1):36. https://doi.org/10.3390/jpm11010036
Chicago/Turabian StyleÁlvarez-Mon, Melchor, Miguel A. Ortega, Óscar Gasulla, Jordi Fortuny-Profitós, Ferran A. Mazaira-Font, Pablo Saurina, Jorge Monserrat, María N. Plana, Daniel Troncoso, José Sanz Moreno, and et al. 2021. "A Predictive Model and Risk Factors for Case Fatality of COVID-19" Journal of Personalized Medicine 11, no. 1: 36. https://doi.org/10.3390/jpm11010036
APA StyleÁlvarez-Mon, M., Ortega, M. A., Gasulla, Ó., Fortuny-Profitós, J., Mazaira-Font, F. A., Saurina, P., Monserrat, J., Plana, M. N., Troncoso, D., Moreno, J. S., Muñoz, B., Arranz, A., Varona, J. F., Lopez-Escobar, A., & Barco, A. A.-d. (2021). A Predictive Model and Risk Factors for Case Fatality of COVID-19. Journal of Personalized Medicine, 11(1), 36. https://doi.org/10.3390/jpm11010036








