Changes in the Prevalence of Metabolic Syndrome and Its Components as Well as in Relevant Preventive Medication between 2006 and 2018 in the Northeast Hungarian Population
Abstract
1. Introduction
2. Materials and Methods
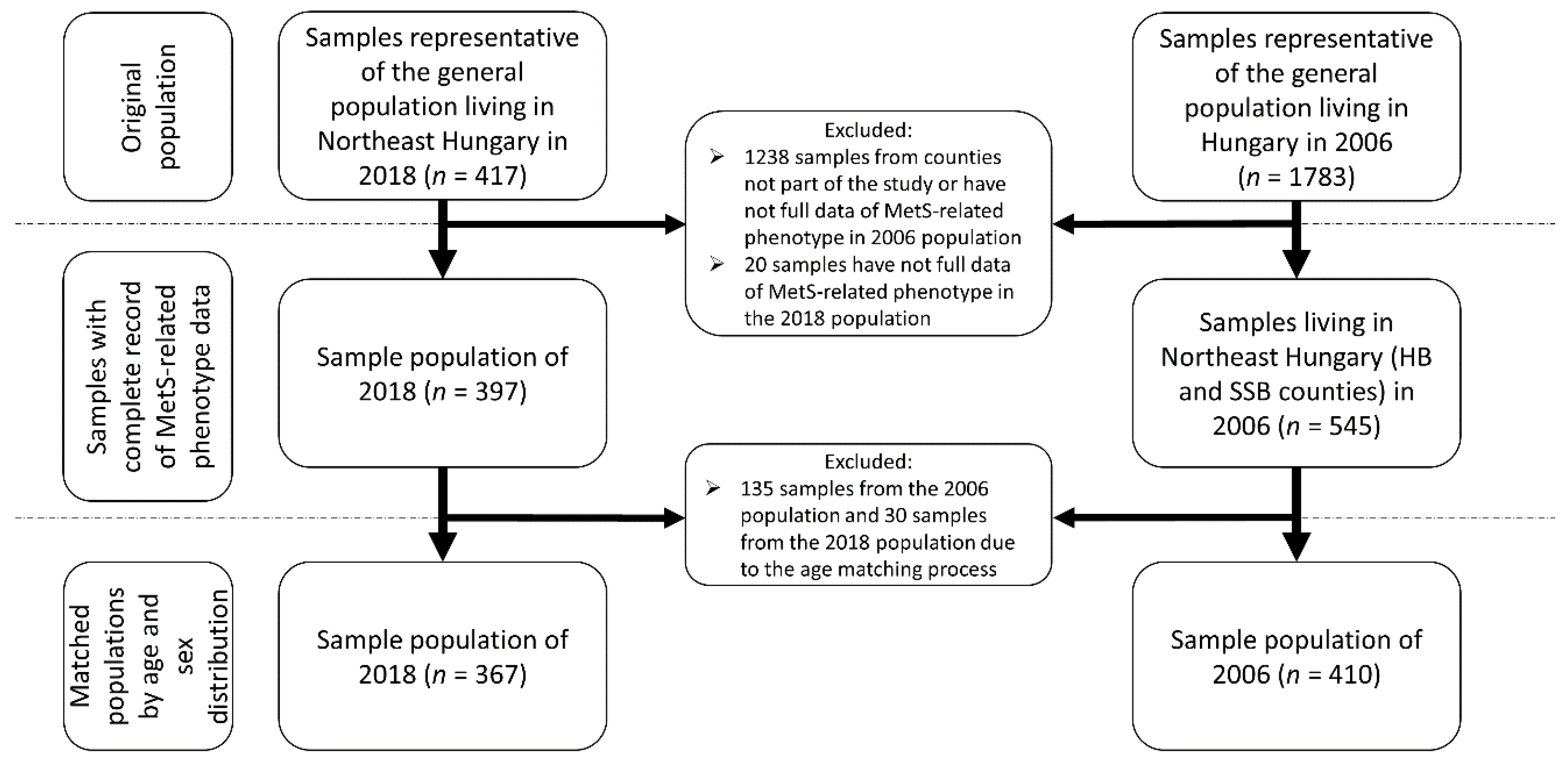
2.1. Study Populations for Comparison from 2006 and 2018
2.2. Determination of the Prevalence of Metabolic Syndrome and Its Components
- raised concentration of triglycerides (≥1.7 mmol/L) or specific treatment for this lipid abnormality;
- reduced concentration of HDL cholesterol: (<1.03 mmol/L in men and <1.29 mmol/L in women) or specific treatment for this lipid abnormality;
- raised blood pressure (systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg) or treatment of previously diagnosed hypertension;
- raised fasting plasma glucose concentration (≥5.6 mmol/L) or previously diagnosed type 2 diabetes.
2.3. Statistical Analyses
2.4. Ethical Statement
3. Results
3.1. Characteristics of Study Populations for Comparative Analysis Used to Estimate the Prevalence of Metabolic Syndrome
3.1.1. Anthropometric and Demographic Characteristics of the Study Populations
3.1.2. Parameters used to Estimate the Prevalence of Metabolic Syndrome in the Study Populations
3.2. The Prevalence of MetS and Its Components in the Study Populations
3.3. Age Specific Prevalence of Metabolic Syndrome and Its Components in the Study Populations
3.4. Results Related to Risk for Development of MetS and Its Components Obtained in Multivariate Regression Models
3.5. The Change of the Proportion of Those with Untreated Metabolic Syndrome Component in Sample Populations from 2006 and 2018
4. Discussion
- Primary health care should be reoriented toward public health services. As is described previously, general medical practice is basically limited to patient care and referral to specialized care in Hungary, and there is a lack of screening examinations ensuring early detection of high blood pressure, diabetes and lipid disorders, and lifestyle counselling aimed at preventing the development of chronic noncommunicable diseases [57];
- Nutritional counselling in primary care is rather sporadic; to insert it into the regular services of family practices would require changes in insurance regulation and the reimbursement system together with an increase in resources [58];
- Not only nutritional counselling, but other preventive services (as, for example, regular measurement of laboratory parameters indicative of the development and progression of cardio-metabolic diseases, assisting cancer screening, measuring anthropometric parameters relevant to the early detection of metabolic syndrome, etc.) are severely underutilized in Hungarian primary care [59,60];
- The patients’ willingness to utilize preventive services is also insufficient; our statement as we conclude on the basis of observation in a primary care model program we had conceptually developed and implemented in collaboration with other consortium members [57,61] that “The future of general practices lays in multidisciplinary teams in which health mediators recruited from the serviced communities can be valuable members, especially in deprived areas” [62] should be emphasized.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Welty, F.K.; Alfaddagh, A.; Elajami, T.K. Targeting inflammation in metabolic syndrome. Transl. Res. 2016, 167, 257–280. [Google Scholar] [CrossRef] [PubMed]
- Bluher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Collaborators, G.B.D.R.F.; Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. The metabolic syndrome--a new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Pitsavos, C.; Panagiotakos, D.; Weinem, M.; Stefanadis, C. Diet, exercise and the metabolic syndrome. Rev. Diabet. Stud. 2006, 3, 118–126. [Google Scholar] [CrossRef]
- Hirode, G.; Wong, R.J. Trends in the Prevalence of Metabolic Syndrome in the United States, 2011–2016. JAMA 2020, 323, 2526–2528. [Google Scholar] [CrossRef]
- Rurik, I.; Ungvari, T.; Szidor, J.; Torzsa, P.; Moczar, C.; Jancso, Z.; Sandor, J. Obese Hungary. Trend and prevalence of overweight and obesity in Hungary, 2015. Orv. Hetil. 2016, 157, 1248–1255. [Google Scholar] [CrossRef]
- Nittari, G.; Scuri, S.; Petrelli, F.; Pirillo, I.; di Luca, N.M.; Grappasonni, I. Fighting obesity in children from European World Health Organization member states. Epidemiological data, medical-social aspects, and prevention programs. Clin. Ter. 2019, 170, e223–e230. [Google Scholar] [CrossRef]
- Hungary: Country Health Profile 2019; OECD/European Observatory on Health Systems and Policies: Brussels, Belgium, 2019.
- Bacsne Baba, E.; Rathonyi, G.; Muller, A.; Rathonyi-Odor, K.; Balogh, P.; Adany, R.; Bacs, Z. Physical Activity of the Population of the Most Obese Country in Europe, Hungary. Front. Public Health 2020, 8, 203. [Google Scholar] [CrossRef]
- Nagy, K.; Fiatal, S.; Sandor, J.; Adany, R. Distinct Penetrance of Obesity-Associated Susceptibility Alleles in the Hungarian General and Roma Populations. Obes. Facts 2017, 10, 444–457. [Google Scholar] [CrossRef] [PubMed]
- Llanaj, E.; Piko, P.; Nagy, K.; Racz, G.; Janos, S.; Kosa, Z.; Fiatal, S.; Adany, R. Applicability of Obesity-Related SNPs and their Effect Size Measures Defined on Populations with European Ancestry for Genetic Risk Estimation among Roma. Genes 2020, 11, 516. [Google Scholar] [CrossRef] [PubMed]
- Werissa, N.A.; Piko, P.; Fiatal, S.; Kosa, Z.; Sandor, J.; Adany, R. SNP-Based Genetic Risk Score Modeling Suggests No Increased Genetic Susceptibility of the Roma Population to Type 2 Diabetes Mellitus. Genes 2019, 10, 942. [Google Scholar] [CrossRef] [PubMed]
- Soltesz, B.; Piko, P.; Sandor, J.; Kosa, Z.; Adany, R.; Fiatal, S. The genetic risk for hypertension is lower among the Hungarian Roma population compared to the general population. PLoS ONE 2020, 15, e0234547. [Google Scholar] [CrossRef]
- Piko, P.; Fiatal, S.; Kosa, Z.; Sandor, J.; Adany, R. Genetic factors exist behind the high prevalence of reduced high-density lipoprotein cholesterol levels in the Roma population. Atherosclerosis 2017, 263, 119–126. [Google Scholar] [CrossRef]
- Piko, P.; Fiatal, S.; Kosa, Z.; Sandor, J.; Adany, R. Data to genetic risk assessment on high-density cholesterol level associated polymorphisms in Hungarian general and Roma populations. Data Brief. 2017, 14, 354–359. [Google Scholar] [CrossRef]
- Piko, P.; Fiatal, S.; Werissa, N.A.; Bekele, B.B.; Racz, G.; Kosa, Z.; Sandor, J.; Adany, R. The Effect of Haplotypes in the CETP and LIPC Genes on the Triglycerides to HDL-C Ratio and Its Components in the Roma and Hungarian General Populations. Genes 2020, 11, 56. [Google Scholar] [CrossRef]
- Piko, P.; Werissa, N.A.; Fiatal, S.; Sandor, J.; Adany, R. Impact of Genetic Factors on the Age of Onset for Type 2 Diabetes Mellitus in Addition to the Conventional Risk Factors. J. Pers. Med. 2020, 11, 6. [Google Scholar] [CrossRef]
- Li, W.; Wang, D.; Wang, X.; Gong, Y.; Cao, S.; Yin, X.; Zhuang, X.; Shi, W.; Wang, Z.; Lu, Z. The association of metabolic syndrome components and diabetes mellitus: Evidence from China National Stroke Screening and Prevention Project. BMC Public Health 2019, 19, 192. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Borschmann, R. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Kempler, P.; Putz, Z.; Kiss, Z.; Wittmann, I.; Abonyi-Tóth, Z.; Rokszin, G.; Jermendy, G. Prevalence and financial burden of type 2 diabetes mellitus in Hungary between 2001–2014—results of the analysis of the National Health Insurance Fund database. Diabetol. Hung 2016, 14, 177–188. [Google Scholar]
- Domjan, B.A.; Ferencz, V.; Tanczer, T.; Szili-Janicsek, Z.; Barkai, L.; Hidvegi, T.; Jermendy, G.; Kempler, P.; Winkler, G.; Gero, L.; et al. Large increase in the prevalence of self-reported diabetes based on a nationally representative survey in Hungary. Prim. Care Diabetes 2017, 11, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Szigethy, E.; Szeles, G.; Horvath, A.; Hidvegi, T.; Jermendy, G.; Paragh, G.; Blasko, G.; Adany, R.; Voko, Z. Epidemiology of the metabolic syndrome in Hungary. Public Health 2012, 126, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Kósa, Z.; Moravcsik-Kornyicki, Á.; Diószegi, J.; Roberts, B.; Szabó, Z.; Sándor, J.; Ádány, R. Prevalence of metabolic syndrome among Roma: A comparative health examination survey in Hungary. Eur. J. Public Health 2015, 25, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Adany, R.; Piko, P.; Fiatal, S.; Kosa, Z.; Sandor, J.; Biro, E.; Kosa, K.; Paragh, G.; Bacsne Baba, E.; Veres-Balajti, I.; et al. Prevalence of Insulin Resistance in the Hungarian General and Roma Populations as Defined by Using Data Generated in a Complex Health (Interview and Examination) Survey. Int. J. Environ. Res. Public Health 2020, 17, 4833. [Google Scholar] [CrossRef]
- Szeles, G.; Voko, Z.; Jenei, T.; Kardos, L.; Pocsai, Z.; Bajtay, A.; Papp, E.; Pasti, G.; Kosa, Z.; Molnar, I.; et al. A preliminary evaluation of a health monitoring programme in Hungary. Eur. J. Public Health 2005, 15, 26–32. [Google Scholar] [CrossRef]
- Gurka, M.J.; Filipp, S.L.; DeBoer, M.D. Geographical variation in the prevalence of obesity, metabolic syndrome, and diabetes among US adults. Nutr. Diabetes 2018, 8, 14. [Google Scholar] [CrossRef]
- Toms, R.; Bonney, A.; Mayne, D.J.; Feng, X.; Walsan, R. Geographic and area-level socioeconomic variation in cardiometabolic risk factor distribution: A systematic review of the literature. Int. J. Health Geogr. 2019, 18, 1. [Google Scholar] [CrossRef]
- DeBoer, M.D.; Filipp, S.L.; Gurka, M.J. Geographical variation in the prevalence of obesity and metabolic syndrome among US adolescents. Pediatr. Obes. 2019, 14, e12483. [Google Scholar] [CrossRef]
- Herningtyas, E.H.; Ng, T.S. Prevalence and distribution of metabolic syndrome and its components among provinces and ethnic groups in Indonesia. BMC Public Health 2019, 19, 377. [Google Scholar] [CrossRef]
- The IDF Consensus Worldwide Definition of the Metabolic Syndrome; International Diabetes Federation: Brussels, Belgium, 2006.
- Ford, E.S.; Giles, W.H.; Mokdad, A.H. Increasing prevalence of the metabolic syndrome among u.s. Adults. Diabetes Care 2004, 27, 2444–2449. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, M.; Bhuket, T.; Torres, S.; Liu, B.; Wong, R.J. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 2015, 313, 1973–1974. [Google Scholar] [CrossRef] [PubMed]
- Ajlouni, K.; Khader, Y.; Alyousfi, M.; Al Nsour, M.; Batieha, A.; Jaddou, H. Metabolic syndrome amongst adults in Jordan: Prevalence, trend, and its association with socio-demographic characteristics. Diabetol. Metab. Syndr. 2020, 12, 100. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Shin, H.; Song, J.H.; Kwak, S.H.; Kang, S.M.; Won Yoon, J.; Choi, S.H.; Cho, S.I.; Park, K.S.; Lee, H.K.; et al. Increasing prevalence of metabolic syndrome in Korea: The Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care 2011, 34, 1323–1328. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.T.; Jeong, B.Y.; Oh, J.K. The prevalence trend of metabolic syndrome and its components and risk factors in Korean adults: Results from the Korean National Health and Nutrition Examination Survey 2008–2013. BMC Public Health 2017, 17, 71. [Google Scholar] [CrossRef]
- Nolan, P.B.; Carrick-Ranson, G.; Stinear, J.W.; Reading, S.A.; Dalleck, L.C. Prevalence of metabolic syndrome and metabolic syndrome components in young adults: A pooled analysis. Prev. Med. Rep. 2017, 7, 211–215. [Google Scholar] [CrossRef]
- Sekgala, M.D.; Monyeki, K.D.; Mogale, A.; McHiza, Z.J.; Parker, W.; Choma, S.R.; Makgopa, H.M. The risk of metabolic syndrome as a result of lifestyle among Ellisras rural young adults. J. Hum. Hypertens 2018, 32, 572–584. [Google Scholar] [CrossRef]
- Al-Hussein, F.A.; Tamimi, W.; Al Banyan, E.; Al-Twaijri, Y.A.; Tamim, H. Cardiometabolic risk among Saudi children and adolescents: Saudi childrens overweight, obesity, and lifestyles (S.Ch.O.O.Ls) study. Ann. Saudi Med. 2014, 34, 46–53. [Google Scholar] [CrossRef]
- Dias Pitangueira, J.C.; Rodrigues Silva, L.; Portela de Santana, M.L.; Monteiro da Silva Mda, C.; de Farias Costa, P.R.; D’Almeida, V.; de Oliveira Assis, A.M. Metabolic syndrome and associated factors in children and adolescents of a Brazilian municipality. Nutr. Hosp. 2014, 29, 865–872. [Google Scholar] [CrossRef]
- Reisinger, C.; Nkeh-Chungag, B.N.; Fredriksen, P.M.; Goswami, N. The prevalence of pediatric metabolic syndrome-a critical look on the discrepancies between definitions and its clinical importance. Int. J. Obes. 2021, 45, 12–24. [Google Scholar] [CrossRef]
- Li, S.; Chen, W.; Srinivasan, S.R.; Berenson, G.S. Influence of metabolic syndrome on arterial stiffness and its age-related change in young adults: The Bogalusa Heart Study. Atherosclerosis 2005, 180, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Mattsson, N.; Ronnemaa, T.; Juonala, M.; Viikari, J.S.; Jokinen, E.; Hutri-Kahonen, N.; Kahonen, M.; Laitinen, T.; Raitakari, O.T. Arterial structure and function in young adults with the metabolic syndrome: The Cardiovascular Risk in Young Finns Study. Eur. Heart J. 2008, 29, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Tzou, W.S.; Douglas, P.S.; Srinivasan, S.R.; Bond, M.G.; Tang, R.; Chen, W.; Berenson, G.S.; Stein, J.H. Increased subclinical atherosclerosis in young adults with metabolic syndrome: The Bogalusa Heart Study. J. Am. Coll. Cardiol. 2005, 46, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Birmaher, B.; Rooks, B.; Gill, M.K.; Hower, H.; Axelson, D.A.; Dickstein, D.P.; Goldstein, T.R.; Liao, F.; Yen, S.; et al. High Prevalence of Metabolic Syndrome Among Adolescents and Young Adults With Bipolar Disorder. J. Clin. Psychiatry 2019, 80. [Google Scholar] [CrossRef] [PubMed]
- Nam, G.E.; Kim, S.M.; Han, K.; Kim, N.H.; Chung, H.S.; Kim, J.W.; Han, B.; Cho, S.J.; Yu, J.H.; Park, Y.G.; et al. Metabolic syndrome and risk of Parkinson disease: A nationwide cohort study. PLoS Med. 2018, 15, e1002640. [Google Scholar] [CrossRef] [PubMed]
- Boruzs, K.; Juhasz, A.; Nagy, C.; Adany, R.; Biro, K. Relationship between Statin Utilization and Socioeconomic Deprivation in Hungary. Front. Pharmacol. 2016, 7, 66. [Google Scholar] [CrossRef] [PubMed]
- Boruzs, K.; Juhasz, A.; Nagy, C.; Szabo, Z.; Jakovljevic, M.; Biro, K.; Adany, R. High Inequalities Associated With Socioeconomic Deprivation in Cardiovascular Disease Burden and Antihypertensive Medication in Hungary. Front. Pharmacol. 2018, 9, 839. [Google Scholar] [CrossRef] [PubMed]
- Juhasz, A.; Nagy, C.; Varga, O.; Boruzs, K.; Csernoch, M.; Szabo, Z.; Adany, R. Antithrombotic Preventive Medication Prescription Redemption and Socioeconomic Status in Hungary in 2016: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 6855. [Google Scholar] [CrossRef]
- Kóti, T. Spatial differences regarding the chance to leave supported public employment in Hungary’s rural periphery. Reg. Stat. 2019, 8, 109–134. [Google Scholar] [CrossRef]
- Bansal, R.; Gubbi, S.; Muniyappa, R. Metabolic Syndrome and COVID 19: Endocrine-Immune-Vascular Interactions Shapes Clinical Course. Endocrinology 2020, 161. [Google Scholar] [CrossRef]
- Assessment of the Impact of a Public Health Product Tax: Hungary; National Institute for Food and Nutrition Science Directorate General: Budapest, Hungary, 2015.
- Public Health Product Tax in Hungary: An Example of Successful Intersectoral Action Using a Fiscal Tool to Promote Healthier Food Choices and Raise Revenues for Public Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2015.
- Sandor, J.; Kosa, Z.; Boruzs, K.; Boros, J.; Tokaji, I.; McKee, M.; Adany, R. The decade of Roma Inclusion: Did it make a difference to health and use of health care services? Int. J. Public Health 2017, 62, 803–815. [Google Scholar] [CrossRef] [PubMed]
- Pfinder, M.; Heise, T.L.; Hilton Boon, M.; Pega, F.; Fenton, C.; Griebler, U.; Gartlehner, G.; Sommer, I.; Katikireddi, S.V.; Lhachimi, S.K. Taxation of unprocessed sugar or sugar-added foods for reducing their consumption and preventing obesity or other adverse health outcomes. Cochrane Database Syst. Rev. 2020, 4, CD012333. [Google Scholar] [CrossRef] [PubMed]
- Adany, R.; Kosa, K.; Sandor, J.; Papp, M.; Furjes, G. General practitioners’ cluster: A model to reorient primary health care to public health services. Eur. J. Public Health 2013, 23, 529–530. [Google Scholar] [CrossRef] [PubMed]
- Rurik, I.; Ruzsinko, K.; Jancso, Z.; Antal, M. Nutritional counseling for diabetic patients: A pilot study in hungarian primary care. Ann. Nutr. Metab. 2010, 57, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Sandor, J.; Nagy, A.; Foldvari, A.; Szabo, E.; Csenteri, O.; Vincze, F.; Sipos, V.; Kovacs, N.; Palinkas, A.; Papp, M.; et al. Delivery of cardio-metabolic preventive services to Hungarian Roma of different socio-economic strata. Fam. Pract. 2017, 34, 83–89. [Google Scholar] [CrossRef]
- Sandor, J.; Nagy, A.; Jenei, T.; Foldvari, A.; Szabo, E.; Csenteri, O.; Vincze, F.; Sipos, V.; Kovacs, N.; Palinkas, A.; et al. Influence of patient characteristics on preventive service delivery and general practitioners’ preventive performance indicators: A study in patients with hypertension or diabetes mellitus from Hungary. Eur. J. Gen. Pract. 2018, 24, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Sandor, J.; Kosa, K.; Papp, M.; Furjes, G.; Korosi, L.; Jakovljevic, M.; Adany, R. Capitation-Based Financing Hampers the Provision of Preventive Services in Primary Health Care. Front. Public Health 2016, 4, 200. [Google Scholar] [CrossRef]
- Kosa, K.; Katona, C.; Papp, M.; Furjes, G.; Sandor, J.; Biro, K.; Adany, R. Health mediators as members of multidisciplinary group practice: Lessons learned from a primary health care model programme in Hungary. BMC Fam. Pract. 2020, 21, 19. [Google Scholar] [CrossRef]
| A | Sample of 2006 | Sample of 2018 | p-Value |
| Mean (95% CI) | Mean (95% CI) | ||
| Fasting glucose (mmol/L) | 4.6 (4.4–4.8) | 5.2 (5.0–5.4) | <0.001 |
| Fasting TG (mmol/L) | 1.7 (1.5–1.8) | 1.6 (1.5–1.7) | 0.721 |
| HDL-C (mmol/L) | 1.5 (1.4–1.5) | 1.4 (1.3–1.4) | 0.086 |
| Waist circumference (cm) | 94.5 (93.1–95.9) | 95.9 (94.4–97.4) | 0.279 |
| Systolic blood pressure (mmHg) | 126.6 (125.0–128.1) | 126.8 (125.2–128.3) | 0.352 |
| Diastolic blood pressure (mmHg) | 79.8 (78.9–80.6) | 78.8 (77.8–79.7) | 0.522 |
| B | Prevalence (95% CI) | Prevalence (95% CI) | p-Value |
| Prevalence of antihypertensive treatment (%) | 29.8 (25.5–34.3) | 29.7 (25.2–34.5) | 0.986 |
| Prevalence of antidiabetic treatment (%) | 4.6 (2.9–7.0) | 6.3 (4.1–9.1) | 0.315 |
| Prevalence of lipid-lowering therapy (%) | 15.9 (12.6–19.6) | 7.1 (4.8–10.1) | <0.001 |
| Sample of 2006 | Sample of 2018 | p-Value | Male Samples of 2006 (n = 177) | Male Samples of 2018 (n = 147) | p-value | Female Samples of 2006 (n = 233) | Female Samples of 2018 (n = 220) | p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| MetS and Its Components | Prevalence % (95% CI) | Prevalence % (95% CI) | Prevalence % (95% CI) | Prevalence % (95% CI) | Prevalence % (95% CI) | Prevalence % (95% CI) | |||
| Central obesity | 70.7 (66.2–75.0) | 75.5 (70.9–79.7) | 0.137 | 62.7 (55.4–69.6) | 64.6 (56.7–72.0) | 0.722 | 76.8 (71.1–81.9) | 82.7 (77.3–87.3) | 0.119 |
| Raised BP or treated hypertension | 45.6 (40.8–50.5) | 57.0 (51.8–61.9) | 0.002 | 49.7 (42.4–57.0) | 60.6 (52.5–68.2) | 0.051 | 42.5 (36.3–48.9) | 54.6 (47.9–61.0) | 0.010 |
| Raised FPG concentration or previously diagnosed diabetes mellitus | 13.2 (10.2–16.7) | 24.8 (20.6–29.4) | <0.001 | 17.0 (12.0–23.0) | 26.5 (19.9–34.1) | 0.036 | 10.3 (6.9–14.7) | 23.6 (18.4–29.6) | <0.001 |
| Raised TG level or treated lipid disorder | 40.2 (35.6–45.1) | 39.5 (34.6–44.6) | 0.835 | 49.7 (42.4–57.0) | 46.3 (38.3–54.3) | 0.535 | 33.1 (27.3–39.3) | 35.0 (28.9–41.5) | 0.661 |
| Reduced HDL-C level or treated lipid disorder | 38.8 (34.2–43.6) | 37.6 (32.8–42.6) | 0.736 | 39.0 (32.0–46.3) | 34.7 (27.4–42.6) | 0.426 | 38.6 (32.6–45.0) | 39.6 (33.3–46.1) | 0.841 |
| Metabolic syndrome | 34.9 (30.4–39.6) | 42.2 (37.3–47.3) | 0.035 | 36.7 (29.9–44.0) | 40.8 (33.1–48.9) | 0.451 | 33.5 (27.7–39.7) | 43.2 (36.8–49.8) | 0.034 |
| Sample of 2006 | Sample of 2018 | p-Value | ||
|---|---|---|---|---|
| Age Groups | MetS and Its Components | Prevalence% (95% CI) | Prevalence% (95% CI) | |
| 20–34 | Central obesity | 44.4 (34.9–54.3) | 62.2 (52.4–71.4) | 0.012 |
| Raised BP or treated hypertension | 13.1 (7.6–20.8) | 36.7 (27.7–46.5) | <0.001 | |
| Raised FPG concentration or previously diagnosed diabetes mellitus | 1.0 (0.1–4.6) | 7.1 (3.3–13.5) | 0.029 | |
| Raised TG level or treated lipid disorder | 21.2 (14.1–30.0) | 30.6 (22.2–40.2) | 0.132 | |
| Reduced HDL-C level or treated lipid disorder | 21.2 (14.1–30.0) | 36.7 (27.7–46.6) | 0.016 | |
| Metabolic syndrome | 12.1 (6.8–19.6) | 31.6 (23.1–41.3) | 0.001 | |
| 35–49 | Central obesity | 70.4 (62.6–77.5) | 76.8 (68.8–83.5) | 0.239 |
| Raised BP or treated hypertension | 36.6 (29.0–44.8) | 50.4 (41.7–59.1) | 0.023 | |
| Raised FPG concentration or previously diagnosed diabetes mellitus | 6.3 (3.2–11.3) | 20.8 (14.4–28.5) | <0.001 | |
| Raised TG level or treated lipid disorder | 42.3 (34.4–50.5) | 33.6 (25.8–42.2) | 0.146 | |
| Reduced HDL-C level or treated lipid disorder | 42.3 (34.4–50.5) | 36.0 (28.0–44.7) | 0.297 | |
| Metabolic syndrome | 32.4 (25.1–40.4) | 33.6 (25.8–42.2) | 0.834 | |
| 50–64 | Central obesity | 86.4 (80.6–90.9) | 83.3 (76.6–88.7) | 0.569 |
| Raised BP or treated hypertension | 72.2 (65.1–78.5) | 76.4 (69.0–82.8) | 0.450 | |
| Raised FPG concentration or previously diagnosed diabetes mellitus | 26.0 (19.9–33.0) | 40.3 (32.5–48.4) | 0.007 | |
| Raised TG level or treated lipid disorder | 49.7 (42.2–57.2) | 50.7 (42.6–58.8) | 0.861 | |
| Reduced HDL-C level or treated lipid disorder | 46.2 (38.8–53.7) | 39.6 (31.9–47.7) | 0.242 | |
| Metabolic syndrome | 50.3 (42.8–57.8) | 56.9 (48.8–64.8) | 0.240 | |
| 20–34 | 35–49 | 50–64 | ||||
|---|---|---|---|---|---|---|
| MetS and Its Components | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value |
| Central obesity | 1.12 (1.03–1.22) | 0.008 | 1.05 (0.97–1.14) | 0.237 | 0.94 (0.86–1.04) | 0.234 |
| Raised BP or treated hypertension | 1.24 (1.12–1.38) | <0.001 | 1.08 (1.00–1.16) | 0.047 | 1.02 (0.95–1.10) | 0.542 |
| Raised FPG concentration or previously diagnosed diabetes mellitus | 1.33 (0.98–1.80) | 0.066 | 1.21 (1.08–1.36) | 0.001 | 1.10 (1.02–1.18) | 0.009 |
| Raised TG level or treated lipid disorder | 1.10 (0.99–1.21) | 0.066 | 0.94 (0.88–1.01) | 0.110 | 1.00 (0.94–1.07) | 0.976 |
| Reduced HDL-C level or treated lipid disorder | 1.124 (1.03–1.23) | 0.012 | 0.97 (0.90–1.04) | 0.324 | 0.96 (0.90–1.02) | 0.211 |
| Metabolic syndrome | 1.21 (1.09–1.35) | 0.001 | 1.00 (0.93–1.08) | 0.976 | 1.03 (0.97–1.10) | 0.373 |
| A | ||||||
| MetS Components | Sample of 2006 | Sample of 2018 | p -Value | |||
| Untreated in % (95% CI) | ||||||
| Raised BP or treated hypertension | 34.8 (28.2–41.8) | 47.9 (41.1–54.6) | 0.008 | |||
| Raised FPG concentration or previously diagnosed diabetes mellitus | 64.8 (51.6–76.5) | 74.7 (65.1–82.8) | 0.203 | |||
| Raised TG level or treated lipid disorder | 60.6 (53.0–67.8) | 82.1 (75.2–87.7) | <0.001 | |||
| Reduced HDL-C level or treated lipid disorder | 59.1 (51.4–66.5) | 81.2 (74.0–87.0) | <0.001 | |||
| B | ||||||
| MetS Components | Males | Females | ||||
| Sample of 2006 | Sample of 2018 | p-Value | Sample of 2006 | Sample of 2018 | p-Value | |
| Untreated in % (95% CI) | Untreated in % (95% CI) | |||||
| Raised BP or treated hypertension | 43.2 (33.2–53.6) | 55.1 (44.7–65.1) | 0.114 | 27.3 (19.2–36.6) | 42.5 (33.9–51.4) | 0.019 |
| Raised FPG concentration or previously diagnosed diabetes mellitus | 80.0 (63.3–91.2) | 74.4 (59.3–86.0) | 0.582 | 45.8 (27.3–65.3) | 75.00 (62.1–85.2) | 0.013 |
| Raised TG level or treated lipid disorder | 60.2 (49.8–70.0) | 80.9 (70.4–88.8) | 0.006 | 61.0 (49.9–71.4) | 83.1 (73.6–90.2) | 0.002 |
| Reduced HDL-C level or treated lipid disorder | 49.3 (37.7–60.9) | 74.5 (61.4–84.9) | 0.005 | 66.7 (56.5–75.8) | 85.1 (76.5–91.4) | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piko, P.; Dioszegi, J.; Sandor, J.; Adany, R. Changes in the Prevalence of Metabolic Syndrome and Its Components as Well as in Relevant Preventive Medication between 2006 and 2018 in the Northeast Hungarian Population. J. Pers. Med. 2021, 11, 52. https://doi.org/10.3390/jpm11010052
Piko P, Dioszegi J, Sandor J, Adany R. Changes in the Prevalence of Metabolic Syndrome and Its Components as Well as in Relevant Preventive Medication between 2006 and 2018 in the Northeast Hungarian Population. Journal of Personalized Medicine. 2021; 11(1):52. https://doi.org/10.3390/jpm11010052
Chicago/Turabian StylePiko, Peter, Judit Dioszegi, Janos Sandor, and Roza Adany. 2021. "Changes in the Prevalence of Metabolic Syndrome and Its Components as Well as in Relevant Preventive Medication between 2006 and 2018 in the Northeast Hungarian Population" Journal of Personalized Medicine 11, no. 1: 52. https://doi.org/10.3390/jpm11010052
APA StylePiko, P., Dioszegi, J., Sandor, J., & Adany, R. (2021). Changes in the Prevalence of Metabolic Syndrome and Its Components as Well as in Relevant Preventive Medication between 2006 and 2018 in the Northeast Hungarian Population. Journal of Personalized Medicine, 11(1), 52. https://doi.org/10.3390/jpm11010052






