A 33-mRNA Classifier Is Able to Produce Inflammopathic, Adaptive, and Coagulopathic Endotypes with Prognostic Significance: The Outcomes of Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in the Early Treatment of Sepsis (ORANGES) Trial
Abstract
:1. Introduction
2. Methods
3. Ethics Statement
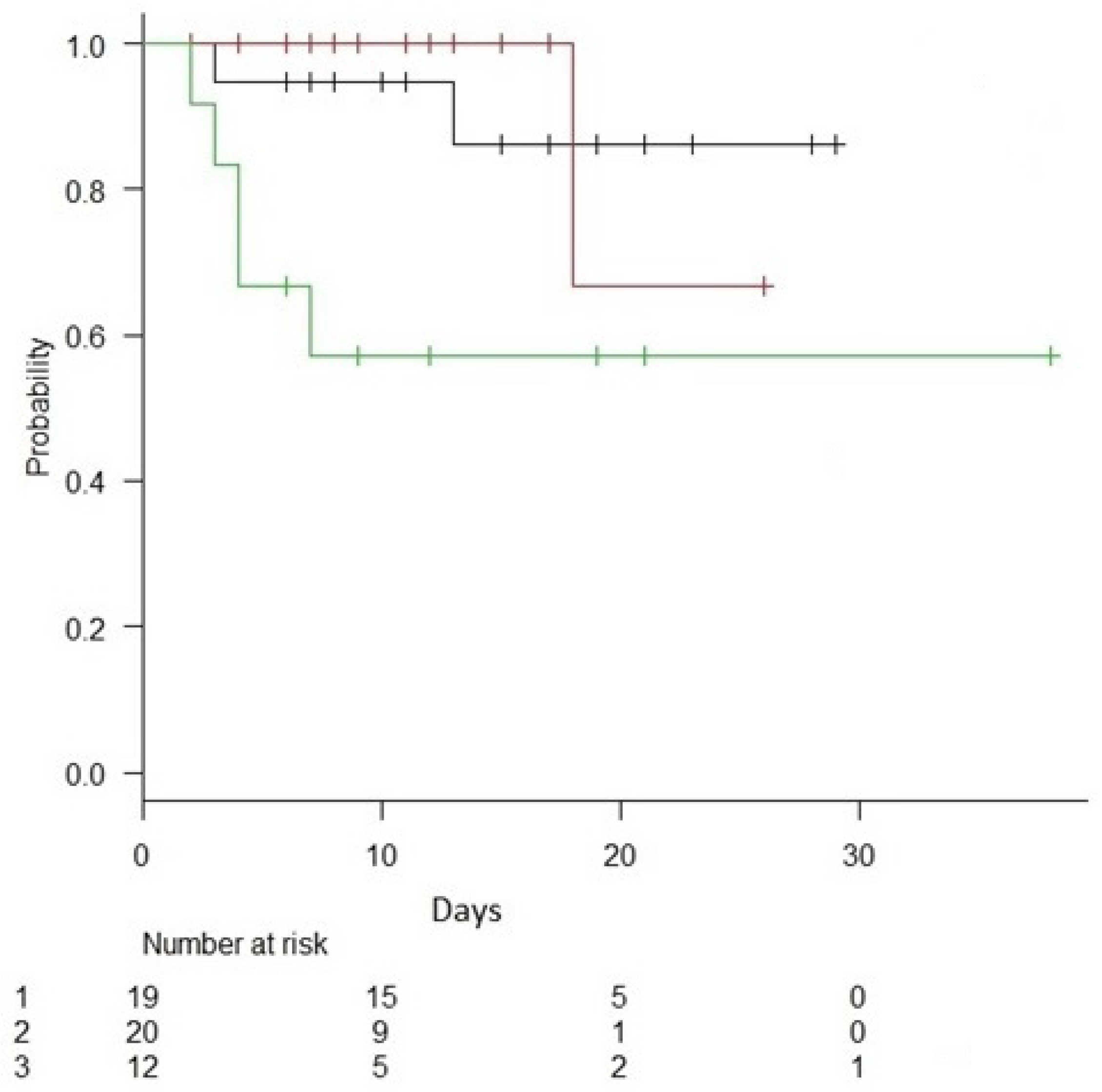
4. Results
5. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| IE | inflammatory endotype |
| AE | adaptive endotype |
| CE | coagulopathic endotype |
| CAD | coronary artery disease |
| HAT | hydrocortisone ascorbic acid thiamine |
| SOFA | Sepsis-Related Organ Failure Assessment |
| APACHE II | Acute Physiology and Chronic Health Evaluation II |
| APACHE IV | Acute Physiology and Chronic Health Evaluation IV |
| INR | international normalized ratio |
References
- Singer, M. Biomarkers in sepsis. Curr. Opin. Pulm. Med. 2013, 19, 305–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sweeney, T.E.; Wong, H.R. Risk Stratification and Prognosis in Sepsis: What Have We Learned from Microarrays? Clin. Chest Med. 2016, 37, 209–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, H.R. Sepsis genomics and precision medicine. In Genomic and Precision Medicine; Academic Press: Cambridge, MA, USA, 2019; pp. 83–93. [Google Scholar]
- Opal, S.M.; Dellinger, R.P.; Vincent, J.-L.; Masur, H.; Angus, D.C. The next generation of sepsis clinical trial designs: What is next after the demise of recombinant human activated protein C?*. Crit. Care Med. 2014, 42, 1714–1721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marik, P.E. Vitamin C for the treatment of sepsis: The scientific rationale. Pharmacol. Ther. 2018, 189, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.C.; Shaw, G.M.; Fowler, A.A.; Natarajan, R. Ascorbate-dependent vasopressor synthesis: A rationale for vitamin C administration in severe sepsis and septic shock? Crit. Care Lond. Engl. 2015, 19, 418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, X.-B.; Wang, Z.-H.; Liao, X.-L.; Guo, W.-X.; Wen, J.-Y.; Qin, T.-H.; Wang, S.H. Efficacy of vitamin C in patients with sepsis: An updated meta-analysis. Eur. J. Pharmacol. 2020, 868, 172889. [Google Scholar] [CrossRef] [PubMed]
- Marik, P.E.; Khangoora, V.; Rivera, R.; Hooper, M.H.; Catravas, J. Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study. Chest 2017, 151, 1229–1238. [Google Scholar] [CrossRef] [PubMed]
- Truwit, J.D.; Hite, R.D.; Morris, P.E.; DeWilde, C.; Priday, A.; Fisher, B.; Thacker, L.R.; Natarajan, R.; Brophy, D.F.; Sculthorpe, R.; et al. Effect of Vitamin C Infusion on Organ Failure and Biomarkers of Inflammation and Vascular Injury in Patients with Sepsis and Severe Acute Respiratory Failure: The CITRIS-ALI Randomized Clinical Trial. JAMA 2019, 322, 1261–1270. [Google Scholar]
- Fujii, T.; Luethi, N.; Young, P.J.; Frei, D.R.; Eastwood, G.M.; French, C.J.; Deane, A.M.; Shehabi, Y.; Hajjar, L.A.; Oliveira, G.; et al. Effect of Vitamin C, Hydrocortisone, and Thiamine vs Hydrocortisone Alone on Time Alive and Free of Vasopressor Support Among Patients with Septic Shock: The Vitamins Randomized Clinical Trial. JAMA 2020, 323, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Iglesias, J.; Vassallo, A.V.; Patel, V.V.; Sullivan, J.B.; Cavanaugh, J.; Elbaga, Y. Outcomes of Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in the Early Treatment of Sepsis: The Oranges Trial. Chest 2020, 158, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Prescott, H.C.; Calfee, C.S.; Thompson, B.T.; Angus, D.C.; Liu, V.X. Toward Smarter Lumping and Smarter Splitting: Rethinking Strategies for Sepsis and Acute Respiratory Distress Syndrome Clinical Trial Design. Am. J. Respir. Crit. Care Med. 2016, 194, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, T.E.; Azad, T.D.; Donato, M.; Haynes, W.A.; Perumal, T.M.; Henao, R.; Bermejo-Martin, J.F.; Almansa, R.; Tamayo, E.; Howrylak, J.A.; et al. Unsupervised Analysis of Transcriptomics in Bacterial Sepsis across Multiple Datasets Reveals Three Robust Clusters. Crit. Care Med. 2018, 46, 915–925. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, T.E.; Perumal, T.M.; Henao, R.; Nichols, M.; Howrylak, J.A.; Choi, A.M.; Bermejo-Martin, J.F.; Almansa, R.; Tamayo, E.; Davenport, E.E.; et al. A community approach to mortality prediction in sepsis via gene expression analysis. Nat. Commun. 2018, 9, 694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayhew, M.B.; Buturovic, L.; Luethy, R.; Midic, U.; Moore, A.R.; Roque, J.A.; Shaller, B.D.; Asuni, T.; Rawling, D.; Remmel, M.; et al. A generalizable 29-mRNA neural-network classifier for acute bacterial and viral infections. Nat. Commun. 2020, 11, 1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunsolus, I.L.; Sweeney, T.E.; Liesenfeld, O.; Ledeboer, N.A. Diagnosing and Managing Sepsis by Probing the Host Response to Infection: Advances, Opportunities, and Challenges. J. Clin. Microbiol. 2019, 57, e00425-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]






|
Survivors (n = 43) |
Non-Survivors (n = 8) | p | OR | 95% CI | |
|---|---|---|---|---|---|
| Age | 65 (59, 70) | 79 (71, 86) | 0.011 | ||
| Race (Caucasian) | 41 (95%) | 7 (88%) | 0.41 | 0.34 | 0.027–4.29 |
| Wt. (kg) | 75 (66, 91) | 76 (71, 96) | 0.24 | ||
| Sex (male) | 20 (47%) | 3 (38%) | 0.71 | 0.69 | 0.14–3.25 |
| Diabetes | 17 (40%) | 4 (50%) | 0.7 | 1.52 | 0.33–6.9 |
| CHF | 9 (21%) | 1 (13%) | 1 | 0.54 | 0.059–5.0 |
| CAD | 8(19%) | 7(87%) | <0.001 | 30 | 3.2–265 |
| COPD | 14 (33%) | 4 (50%) | 0.43 | 2.07 | 0.45–9.52 |
| CKD | 7 (16.3%) | 2 (25%) | 0.62 | 1.71 | 0.28–10.3 |
| Pneumonia | 17 (40%) | 3 (38%) | 1 | 0.91 | 0.15–4.35 |
| Primary bacteremia | 7 (16%) | 1 (13%) | 1 | 0.73 | 0.073–6.94 |
| Mechanical ventilation | 16 (37%) | 7 (88%) | 0.016 | 11.2 | 1.33–105 |
| Vasopressors | 32 (74.4%) | 5 (62%) | 0.66 | 0.57 | 0.51–2.8 |
| AKI | 35 (81%) | 7 (88%) | 1 | 1.6 | 0.17–14.9 |
| HD | 6 (14%) | 1 (13%) | 1 | 0.88 | 0.091–8.4 |
| Inflammatory | 17 (39.5%) | 2 (25%) | 0.42 | 0.51 | 0.092–2.82 |
| Inflammatory Score | 0.18 (0.001, 0.69) | 0.18 (0.08, 0.63) | 0.42 | ||
| Coagulopathic | 7 (16%) | 5 (62%) | 0.012 | 8.57 | 1.65–44.0 |
| Coagulopathic Score | 0.09 (0.003, 0.35) | 0.77 (0.19, 0.84) | 0.031 | ||
| Adaptive | 19 (44%) | 1 (13%) | 0.12 | 0.2 | 0.020–1.65 |
| Adaptive Score | 0.17 (0.0001, 0.1) | 0.01 (0.0007, 0.05) | 0.16 | ||
| WBC × 109/L | 15 (11, 22) | 15 (6, 22) | 0.99 | ||
| Lactate (mM/L) | 3.1 (2, 4) | 4.9 (2.4, 9) | 0.2 | ||
| SCr (mg/dL) | 1.7 (1, 3.4) | 1.5 (1.1, 2.1) | 0.74 | ||
| Platelets (× 109/L) | 228 (168, 333) | 192 (90, 334) | 0.68 | ||
| Procalcitonin (ng/mL) | 3.7 (0.8, 15) | 1.65 (0.16, 8.5) | 0.8 | ||
| Tbili (mg/dL) | 0.7 (0.4, 1.6) | 1.4 (0.6, 2.2) | 0.34 | ||
| Ascorbic acid(mg/dL) | 0.3 (0.1, 0.4) | 0.52 (0.24, 0.67) | 0.13 | ||
| Thiamine(nmol/L) | 139 (113, 208) | 118 (105, 138) | 0.19 | ||
| SOFA | 8 (5, 8) | 9 (7.5, 10) | 0.45 | ||
| APACHE II | 21 (17, 28) | 26 (22, 33) | 0.12 | ||
| Apache IV | 76 (66, 91) | 107 (90, 119) | 0.002 | ||
| Apache IV predicted mortality (%) | 21 (11, 31) | 64 (11, 31) | 0.017 | ||
| PaO2/FiO2 | 256 (151, 341) | 186 (95, 321) | 0.58 | ||
| Total Lymphocyte | 0.5 (0.3, 1) | 0.35 (0.12, 0.7) | 0.09 | ||
| INR | 1.2 (1, 1.5) | 2 (1.5, 2.3) | 0.002 |
| Inflammatory (n = 19) | Adaptive (n = 20) | Coagulopathic (n = 12) | p | |
|---|---|---|---|---|
| Age | 64 (59, 73) | 67 (54, 81) | 76 (64, 82) | 0.16 |
| Race (Caucasian) | 19 (100%) | 18 (90%) | 11 (84%) | 0.53 |
| Weight (kg) | 70 (60, 84) | 86 (63, 100) | 76 (70, 100) | 0.54 |
| Sex (male) | 10 (53%) | 5 (25%) | 8 (61%) | 0.061 |
| CAD | 5 (26%) | 4 (20%) | 6 (46%) | 0.18 |
| Diabetes | 4 (20%) | 10 (50%) | 7 (54%) | 0.071 |
| CHF | 2 (10%) | 5 (25%) | 3 (23%) | 0.28 |
| COPD | 8 (42%) | 5 (25%) | 5 (38%) | 0.46 |
| CKD | 5 (26%) | 4 (20%) | 0 (0%) | 0.16 |
| Morbid obesity (BMI > 40) | 2 (10%) | 5 (25%) | 1 (8%) | 0.33 |
| Pneumonia | 8 (42%) | 6 (30%) | 6 (46%) | 0.66 |
| Primary bacteremia | 6 (31%) | 1 (5%) | 1 (8%) | 0.05 |
| Mechanical ventilation | 10 (53%) | 5 (25%) | 8 (61%) | 0.051 |
| Vasopressors | 14 (74%) | 13 (65%) | 10 (77%) | 0.52 |
| AKI | 15 (79%) | 16 (80%) | 11 (85%) | 0.62 |
| Positive blood cultures | 11 (58%) | 3 (15%) | 2 (15%) | 0.007 |
| WBC × 109/L | 14 (5, 27) | 14 (10, 20) | 18 (15, 22) | 0.12 |
| Lactate (mM/L) | 3.8 (2.8, 3.6) | 2.7 (1.6, 3.6) | 4.5 (2, 6.5) | 0.19 |
| SCr (mg/dL) | 2 (1.3, 3.6) | 1.36 (0.96, 2.1) | 1.6 (1.2, 2.1) | 0.21 |
| Platelets (× 109/L) | 189 (93, 235) | 263 (205, 370) | 213 (167, 350) | 0.024 |
| Procalcitonin (ng/mL) | 22 (4.6, 60) | 0.8 (0.2, 3.6) | 3.6 (1.6, 7) | <0.001 |
| Tbili (mg/dL) | 0.9 (0.6, 2) | 0.5 (0.4, 0.7) | 1.2 (0.62, 2) | 0.006 |
| PaO2/FiO2 | 211 (133, 293) | 277 (166, 366) | 224 (86, 347) | 0.43 |
| SOFA | 9 (7, 13) | 6 (4, 9) | 8 (6, 10) | 0.036 |
| INR | 1.28 (1.1, 1.5) | 1.25 (0.96, 1.6) | 1.4 (1, 2) | 0.87 |
| Total lymphocytes | 0.4 (0.2, 0.6) | 0.9 (0.4, 1.4) | 0.4 (0.25, 0.8) | 0.038 |
| APACHE II | 25 (18, 32) | 20 (15, 30) | 23 (20, 32) | 0.079 |
| Mortality across endotypes (%) | 10% | 5% | 40% | 0.032 |
| APACHE IV | 89 (65, 113) | 74 (65, 79) | 93 (73, 115) | 0.053 |
| Apache IV predicted mortality (%) | 0.29 (0.12, 0.62) | 0.17 (0.1, 0.26) | 0.3 (0.23, 0.7) | 0.023 |
| Ascorbic acid (mg/dL) | 0.3 (0.1, 0.4) | 0.3 (0.12, 0.4) | 0.4 (0.28, 0.65) | 0.19 |
| Thiamine(nmol/L) | 187 (117, 253) | 126 (104, 153) | 139 (107, 175) | 0.20 |
| HAT Therapy (n = 23) | Control (+ Steroids) (n = 6) | Control (no Steroids) (n = 22) | p | |
|---|---|---|---|---|
| Race (Caucasian) | 22 (96%) | 6 (100%) | 20 (91%) | 0.64 |
| Age | 64 (58, 80) | 73 (64, 79) | 67 (60, 77) | 0.77 |
| Sex (M) | 13 (57%) | 13 (50%) | 7 (32%) | 0.24 |
| Weight | 74 (60, 89) | 105 (78, 121) | 74 (63, 96) | 0.076 |
| Pneumonia | 9 (39%) | 5 (83%) | 6 (27%) | 0.045 |
| Primary Bacteremia | 3 (13%) | 2 (33%) | 3 (14%) | 0.44 |
| CAD | 5 (21%) | 1 (17%) | 9 (41%) | 0.28 |
| CHF | 4 (17%) | 2 (33%) | 4 (18%) | 0.66 |
| DM | 6 (26%) | 3 (50%) | 12 (54%) | 0.14 |
| Mechanical ventilation | 11 (48%) | 4 (67%) | 8 (30%) | 0.38 |
| Vasopressors | 20 (87%) | 4 (67%) | 13 (59%) | 0.1 |
| ARF | 12 (52%) | 3 (50%) | 7 (32%) | 0.1 |
| HD | 3 (13%) | 0 (0%) | 4 (18%) | 0.51 |
| Inflammopathic | 9 (37%) | 1 (5%) | 10 (50%) | 0.46 |
| Inflammatory Score | 0.31 (0.0001, 0.73) | 0.36 (0.002, 0.81) | 0.15 (0.007, 0.6) | 0.58 |
| Coagulopathic | 10 (43%) | 2 (33%) | 7 (32%) | 0.73 |
| Coagulopathic Score | 0.13 (0.002, 0.35) | 0.39 (0.13, 0.77) | 0.074 (0.003, 0.50) | 0.33 |
| Adaptive | 4 (17%) | 3 (50%) | 5 (13%) | 0.57 |
| Adaptive Score | 0.009 (0.0001, 0.9) | 0.035 (0.0001, 0.39) | 0.09 (0.007, 0.9) | 0.48 |
| WBC (K/mL) | 14 (7, 20) | 18 (12, 23) | 16 (12, 25) | 0.29 |
| Lactate (mM/L) | 2.6 (1.9, 4.1) | 4 (1.72, 4.5) | 3.5 (2.9, 6.5) | 0.29 |
| Creatinine (mg/dL) | 1.63 (1.26, 3.62) | 1.7 (1.25, 2.01) | 2.5 (0.74, 4.63) | 0.46 |
| Total Lympocyte | 0.4 (0.2, 0.8) | 0.8 (0.45, 1.6) | 1.4 (1.06, 1.55) | 0.096 |
| Platelets (K/mL) | 200 (85, 277) | 185 (161, 273) | 269 (203, 311) | 0.2 |
| INR | 1.28 (1.1, 2.1) | 1.04 (1.03, 1.05) | 1.4 (1.06, 1.55) | 0.23 |
| Procalcitonin (ng/mL) | 3 (0.19, 8) | 7 (6.4, 22) | 2.5 (0.74, 4.7) | 0.1 |
| Tbili (mg/dL) | 0.8 (0.5, 1.7) | 0.85 (0.47, 1.2) | 0.7 (0.4, 1.85) | 0.98 |
| PaO2/FiO2 | 200 (85, 277) | 185 (161, 273) | 96 (69, 206) | 0.06 |
| SOFA | 9 (7, 11) | 8.5 (5.5, 10.7) | 6 (4, 9) | 0.16 |
| APACHE II | 23 (19, 30) | 21 (15, 39) | 21 (17, 30) | 0.76 |
| APACHE IV | 82 (73, 91) | 84 (57, 121) | 70 (65, 97) | 0.49 |
| APACHE IV predicted mortality (%) | 27 (17, 41) | 34 (12, 69) | 16 (10, 31) | 0.26 |
| Ascorbic acid (mg/dL) | 0.3 (0.1, 0.4) | 0.3 (0.12, 0.4) | 0.45 (0.12, 0.67) | 0.14 |
| Thiamine (nmol/L) | 187 (151, 153) | 126 (104, 153) | 140 (115, 178) | 0.19 |
| HAT Therapy | n = 10 | n = 9 | n = 4 |
| IE | AE | CE | |
| survival | 9 | 8 | 2 |
| mortality | 1 | 1 | 2 |
| Controls given steroids off protocol | n = 2 | n = 1 | n = 3 |
| IE | AE | CE | |
| survival | 1 | 1 | 3 |
| mortality | 1 | 0 | 0 |
| Controls no steroids | n = 7 | n = 10 | n = 5 |
| IE | AE | CE | |
| survival | 7 | 10 | 2 |
| mortality | 0 | 0 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iglesias, J.; Vassallo, A.V.; Liesenfeld, O.; Levine, J.S.; Patel, V.V.; Sullivan, J.B.; Cavanaugh, J.B.; Elbaga, Y.; Sweeney, T.E. A 33-mRNA Classifier Is Able to Produce Inflammopathic, Adaptive, and Coagulopathic Endotypes with Prognostic Significance: The Outcomes of Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in the Early Treatment of Sepsis (ORANGES) Trial. J. Pers. Med. 2021, 11, 9. https://doi.org/10.3390/jpm11010009
Iglesias J, Vassallo AV, Liesenfeld O, Levine JS, Patel VV, Sullivan JB, Cavanaugh JB, Elbaga Y, Sweeney TE. A 33-mRNA Classifier Is Able to Produce Inflammopathic, Adaptive, and Coagulopathic Endotypes with Prognostic Significance: The Outcomes of Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in the Early Treatment of Sepsis (ORANGES) Trial. Journal of Personalized Medicine. 2021; 11(1):9. https://doi.org/10.3390/jpm11010009
Chicago/Turabian StyleIglesias, Jose, Andrew V. Vassallo, Oliver Liesenfeld, Jerrold S. Levine, Vishal V. Patel, Jesse B. Sullivan, Joseph B. Cavanaugh, Yasmine Elbaga, and Timothy E. Sweeney. 2021. "A 33-mRNA Classifier Is Able to Produce Inflammopathic, Adaptive, and Coagulopathic Endotypes with Prognostic Significance: The Outcomes of Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in the Early Treatment of Sepsis (ORANGES) Trial" Journal of Personalized Medicine 11, no. 1: 9. https://doi.org/10.3390/jpm11010009
APA StyleIglesias, J., Vassallo, A. V., Liesenfeld, O., Levine, J. S., Patel, V. V., Sullivan, J. B., Cavanaugh, J. B., Elbaga, Y., & Sweeney, T. E. (2021). A 33-mRNA Classifier Is Able to Produce Inflammopathic, Adaptive, and Coagulopathic Endotypes with Prognostic Significance: The Outcomes of Metabolic Resuscitation Using Ascorbic Acid, Thiamine, and Glucocorticoids in the Early Treatment of Sepsis (ORANGES) Trial. Journal of Personalized Medicine, 11(1), 9. https://doi.org/10.3390/jpm11010009






