Patient-Centered Care for Patients with Cardiometabolic Diseases: An Integrative Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Study Design
- How can the diagnostic evaluation of patients with cardiovascular and metabolic disease be performed, either through assessment instruments or other types of evaluation?
- What are the care planning strategies focused on patients with cardiovascular and metabolic disease developed with the objective of promoting health and preventing and/or reducing complications related to the aforementioned diagnoses?
- What intervention strategies aim to implement care processes focused on patients with cardiovascular and metabolic disease?
2.3. Search Strategy
2.4. Search Terms and Boolean Operators
2.5. Data Collection and Analysis
2.5.1. Selection of Studies
2.5.2. Data Extraction
2.5.3. Quality Appraisal
2.5.4. Strategy for Data Synthesis
3. Results
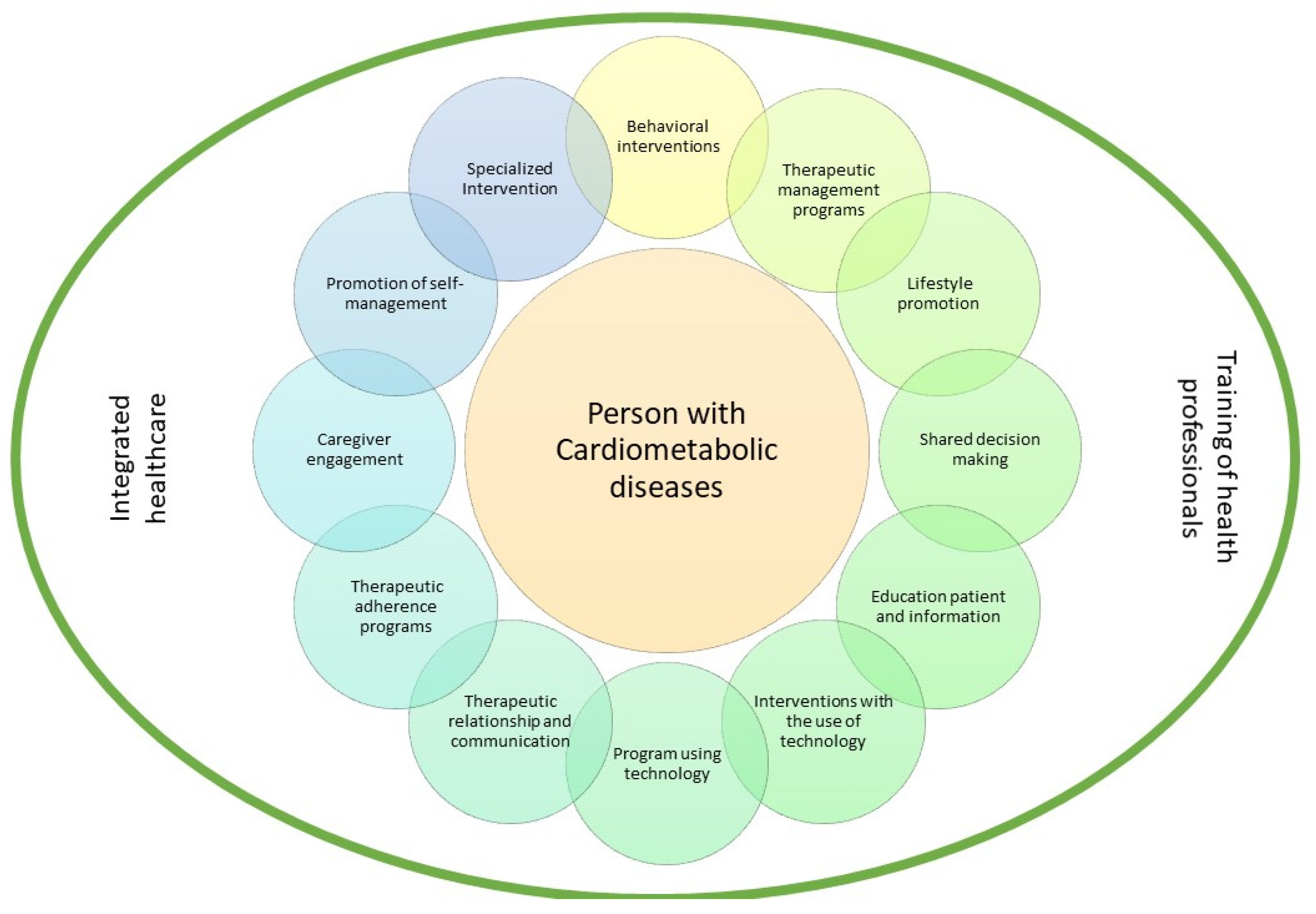
4. Discussion
4.1. Diagnostic Evaluation
4.2. Care Planning and Intervention
5. Conclusions
6. Content Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gagliardi, A.R.; Green, C.; Dunn, S.; Grace, S.L.; Khanlou, N.; Stewart, D.E. How do and could clinical guidelines support patient-centred care for women: Content analysis of guidelines. PLoS ONE 2019, 14, e0224507. [Google Scholar] [CrossRef] [Green Version]
- Eklund, J.H.; Holmström, I.K.; Kumlin, T.; Kaminsky, E.; Skoglund, K.; Höglander, J.; Meranius, M.S. Same same or different? A review of reviews of person-centered and patient-centered care. Patient Educ. Couns. 2019, 102, 3–11. [Google Scholar] [CrossRef]
- Park, M.; Lee, M.; Jeong, H.; Jeong, M.; Go, Y. Patient-and family-centered care interventions for improving the quality of health care: A review of systematic reviews. Int. J. Nurs. Stud. 2018, 87, 69–83. [Google Scholar] [CrossRef] [PubMed]
- Zisman-Ilani, Y.; Obeidat, R.; Fang, L.; Hsieh, S.; Berger, Z. Shared Decision Making and Patient-Centered Care in Israel, Jordan, and the United States: Exploratory and Comparative Survey Study of Physician Perceptions. JMIR Res. 2020, 4, e18223. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.; McKinn, S.; Bonner, C.; Muscat, D.M.; Doust, J.; McCaffery, K. Tomada de decisão compartilhada sobre medicamentos para doenças cardiovasculares em pessoas idosas: Um estudo qualitativo de experiências de pacientes na prática geral. BMJ Aberto 2019, 9, e026342. [Google Scholar] [CrossRef] [Green Version]
- Eduard, M.-S.; Júlio, P.-F.; Alejandra, R.-F. Coocorrência de Fatores de Risco para Doenças Cardiometabólicas: Alimentação Não Saudável, Tabaco, Álcool, Estilo de Vida Sedentário e Aspetos Socioeconómicos. Arq. Bras. Cardiol. 2019, 113, 710–711. [Google Scholar] [CrossRef] [PubMed]
- da Saúde, D.G. Avaliação Do Risco Cardiovascular SCORE: Norma n.° 005/2013, de 19/03/2013, Atualizada em 21/01/2015. Lisboa: DGS. 2015. Available online: https://www.dgs.pt/directrizes-da-dgs/normas-e-circulares-normativas/norma-n-0052013-de-19032013-jpg.aspx (accessed on 2 July 2021).
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; McKenzie, J.E. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Iturralde, E.; Sterling, S.A.; Uratsu, C.S.; Mishra, P.; Ross, T.B.; Grant, R.W. Changing Results-Engage and Activate to Enhance Wellness: A Randomized Clinical Trial to Improve Cardiovascular Risk Management. J. Am. Heart Assoc. 2019, 8, e014021. [Google Scholar] [CrossRef]
- O’Leary, K.J.; Killarney, A.; Hansen, L.O.; Jones, S.; Malladi, M.; Marks, K.; Shah, H.M. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Qual. Saf. 2016, 25, 921–928. [Google Scholar] [CrossRef]
- Lenz, T.L.; Monaghan, M.S. Implementing lifestyle medicine with medication therapy management services to improve patient-centered health care. J. Am. Pharm. Assoc. 2011, 51, 184–188. [Google Scholar] [CrossRef]
- Chi, C.-L.; Nick Street, W.; Robinson, J.G.; Crawford, M.A. Individualized patient-centered lifestyle recommendations: An expert system for communicating patient specific cardiovascular risk information and prioritizing lifestyle options. J. Biomed. Inform. 2012, 45, 1164–1174. [Google Scholar] [CrossRef] [Green Version]
- Filler, T.; Dunn, S.; Grace, S.L.; Straus, S.E.; Stewart, D.E.; Gagliardi, A.R. Multi-level strategies to tailor patient-centred care for women: Qualitative interviews with clinicians. BMC Health Serv. Res. 2020, 20, 212. [Google Scholar] [CrossRef]
- Montori, V.M.; Brito, J.P.; Ting, H.H. Patient-centered and practical application of new high cholesterol guidelines to prevent cardiovascular disease. JAMA 2014, 311, 465–466. [Google Scholar] [CrossRef]
- Dhukaram, A.V.; Baber, C.; De Stefanis, P. Patient-centred cardio vascular disease management–end-user perceptions. J. Assist. Technol. 2012, 6, 105–122. [Google Scholar] [CrossRef]
- Kim, D.H.; Rich, M.W. Patient-Centred Care of Older Adults with Cardiovascular Disease and Multiple Chronic Conditions. Can. J. Cardiol. 2016, 32, 1097–1107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sassen, B.; Kok, G.; Schepers, J.; Vanhees, L. Supporting health care professionals to improve the processes of shared decision making and self-management in a web-based intervention: Randomized controlled trial. J. Med. Internet Res. 2014, 16, e211. [Google Scholar] [CrossRef] [Green Version]
- Kornelius, E.; Chiou, J.-Y.; Yang, Y.-S.; Lu, Y.-L.; Peng, C.-H.; Huang, C.-N. The Diabetes Shared Care Program and Risks of Cardiovascular Events in Type 2 Diabetes. Am. J. Med. 2015, 128, 977. [Google Scholar] [CrossRef] [PubMed]
- Ligthart, S.A.; van den Eerenbeemt, K.D.; Pols, J.; van Bussel, E.F.; Richard, E.; van Charante, E.P.M. Perspectives of older people engaging in nurse-led cardiovascular prevention programmes: A qualitative study in primary care in the Netherlands. British J. Gen. Pract. 2015, 65, e41–e48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McBride, A.; Burey, L.; Megahed, M.; Feldman, C.; Deaton, C. The role of patient-held alert cards in promoting continuity of care for heart failure patients. Eur. J. Cardiovasc. Nurs. 2014, 13, 71–77. [Google Scholar] [CrossRef]
- Warden, B.A.; Freels, J.P.; Furuno, J.P.; Mackay, J. Pharmacy-managed program for providing education and discharge instructions for patients with heart failure. Am. J. Health-Syst. Pharm. 2014, 71, 134–139. [Google Scholar] [CrossRef]
- Gibson, I.; Flaherty, G.; Cormican, S.; Jones, J.; Kerins, C.; Walsh, A.M.; Crowley, J. Translating guidelines to practice: Findings from a multidisciplinary preventive cardiology programme in the west of Ireland. Eur. J. Prev. Cardiol. 2014, 21, 366–376. [Google Scholar] [CrossRef]
- Dudas, K.; Olsson, L.E.; Wolf, A.; Swedberg, K.; Taft, C.; Schaufelberger, M.; Ekman, I. Uncertainty in illness among patients with chronic heart failure is less in person-centred care than in usual care. Eur. J. Cardiovasc. Nurs. 2013, 12, 521–528. [Google Scholar] [CrossRef]
- Rocha, E. Scores de risco cardiovascular: Utilidade e limitações. Rev. Port. Cardiol. 2016, 35, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Maggioni, A.P.; Anker, S.D.; Dahlström, U.; Filippatos, G.; Ponikowski, P.; Zannad, F.; Heart Failure Association of the ESC (HFA). Are hospitalized or ambulatory patients with he hart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12 440 patients of the ESC Heart Failure Long-Term Registry. Eur. J. Heart Fail. 2013, 15, 1173–1184. [Google Scholar] [CrossRef] [PubMed]
- Sasson, C.; Eckel, R.; Alger, H.; Bozkurt, B.; Carson, A.; Daviglus, M.; Sanchez, E. American heart association diabetes and cardiometabolic health summit: Summary and recommendations. J. Am. Heart Assoc. 2018, 7, e009271. [Google Scholar] [CrossRef] [Green Version]
- Stol, D.M.; Over, E.A.; Badenbroek, I.F.; Hollander, M.; Nielen, M.M.; Kraaijenhagen, R.A.; Schellevis, F.G.; de Wit, N.J. Cost-effectiveness of a stepwise cardiometabolic disease prevention program: Results of a randomized controlled trial in primary care. BMC Med. 2021, 19, 1–10. [Google Scholar] [CrossRef]
- Lucini, D.; Malacarne, M.; Gatzemeier, W.; Pagani, M. A simple home-based lifestyle intervention program to improve cardiac autonomic regulation in patients with increased cardiometabolic risk. Sustainability 2020, 12, 7671. [Google Scholar] [CrossRef]

| Aim/Hypothesis | Author | Year | Study Type | Intervention/Strategy | Results/Conclusions |
|---|---|---|---|---|---|
| A behavioral intervention to increase patient activation, patient-centered care processes, and healthcare system engagement would lead to improved CVD risk factor control | Iturralde, Sterling, Uratsu, Mishra, Ross and Grant [11] | 2019 | Randomized controlled trial | CREATE Wellness was an intervention designed to develop knowledge and skills in patients systematically unable to achieve the therapeutic goals of management and control of CVD risk factors. This consisted of three group-based patient activation sessions two weeks apart that included between-session contacts with the interventionist (i.e., text message, voice or video call) to reinforce self-management behaviors and skills. | There were reports of improvements in the patient-centered care process. The intervention group was more frequently involved with the health system using online tools. The intervention increased patient’s engagement with the health team. Despite these significant changes, CVD risk factor control did not improve compared to control patients in response to the intervention, highlighting the challenge of improving CVD risk reduction among patients persistently not meeting therapeutic goals. |
| To evaluate the effect of patient centred bedside rounds (PCBRs) on measures of patient-centred care | O’Leary, Killarney, Hansen, Jones, Malladi, Marks and Shah [12] | 2016 | Cluster randomized controlled trial | Semi-structured interviews with input from patients, family members and frontline professionals were conducted at Northwestern Memorial Hospital (NMH) in units equipped with cardiac telemetry monitoring and with implemented daily interprofessional bedside rounds. | After discharge, there was no difference in patients’ perceptions of whether nurses and doctors worked as a team or whether the staff included them in treatment decisions. The intervention, designed in collaboration with the patients and their family members, had no impact on patients’ perception regarding shared decision making, activation or satisfaction with care, calling into question the intervention as a strategy to improve patient-centered care. More research studies are needed to identify approaches that can be implemented in hospital settings to improve patient-centered care. |
| To describe a patient-centered medication therapy management (MTM) program that focuses on lifestyle medicine. | Lenz and Monaghan [13] | 2011 | Quasi -experimental | A program was implemented to reduce cardiovascular risk based on the intervention of a community pharmacy located in Omaha, NE. The program used various tools (i.e., lifestyle adherence diary, nutrition diary, pedometer, home blood pressure monitor, monthly news bulletin, monthly support group meeting, blog site, and educational materials) to improve patient-centered care and patient outcomes. | Most participants, regardless of hypertension diagnosis, had improvements in blood pressure values, met cholesterol guidelines, lowered blood glucose levels, met exercise guidelines (>150 min/week), increased their combined intake of fresh fruits and vegetables, and lost weight. The individual CVD risk improved on average by 34%, and for heart diseases only, it improved on average by 47% after 12 months. More than half of the participants improved their communication with other health professionals. The vast majority commented that the program helped them become more aware of personal health needs and made them more responsible for actions related to lifestyle. |
| The authors propose a proof-of-concept machine-learning expert system that learned knowledge of lifestyle and the associated 10-year cardiovascular disease (CVD) risks from individual-level data (i.e., Atherosclerosis Risk in Communities Study, ARIC). | Chi, Street, Robinson and Crawford [14] | 2012 | Qualitative Descriptive | Construction of an expert system that learned knowledge of lifestyle and associated CDV risks from the data from the Atherosclerosis Risk in Communities (ARIC) study using k-NN prediction models. | The results showed that the optimal individualized, patient-centered lifestyle consistently reduced the 10-year CVD risk. The top three recommended lifestyles were reduce cholesterol intake, quit smoking, and lose weight. The majority (54.4%) of smokers received recommendations to quit smoking, 37.2% received recommendations to control their cholesterol, and 4.8% received recommendations to control their weight (BMI). Clinically, weight control was usually recommended for diabetes and hypertension patients, and weight control was indeed the first recommendation for diabetes patients and the second recommendation for hypertension patients. In addition, the system showed that lowering cholesterol was among the top two recommendations for both diseases. It is expected that this interactive decision process (among patients, physicians and the system) will increase patients’ involvement and participation and subsequently may improve an individual’s commitment to a healthy lifestyle. |
| To explore how clinicians deliver patient-centred care for women (PCCW), challenges they face, and the strategies they suggest are needed to support PCCW. | Filler, Dunn, Grace, Straus, Stewart and Gagliardi [15] | 2020 | Qualitative | Semi-structured interviews with clinicians from the province of Ontario, Canada, whose script consisted of three questions: (1) How do you tailor patient-centered care for women? (2) What factors challenge patient-centered care for women? (3) What strategies or interventions would help you deliver or achieve patient-centered care for women? | Clinicians emphasized that women face unique challenges in seeking health care and communicating about health care issues that warrant tailoring of PCC. Approaches used by clinicians to adapt PCC to women were: fostering a healing relationship, exchanging information, addressing emotions/concerns, managing uncertainty, decision making, and allowing self-management. Participants reported that offering flexible options for follow-up appointments was essential to monitor the response to treatment and health status. |
| To apply the ACC/AHA guidelines in a patient centered and practical perspective, 3 cases illustrate the evidence-based approach espoused by the new guidelines, with 1 important modification | Montori, Brito and Ting [16] | 2014 | 2 Cases/Opinion | In 2013, the American College of Cardiology and the American Heart Association (ACC/AHA) published new guidelines for assessing CVD risk and for the treatment of high blood cholesterol levels to reduce CVD. These new guidelines replaced the Adult Treatment Panel III (ATPIII) guidelines for the detection, evaluation, and treatment of high blood cholesterol that guided clinical practice for more than a decade. The new guidelines divert focus from lowering low-density lipoprotein (LDL) cholesterol levels to treating CVD risk and therefore are no longer pure cholesterol guidelines and discourage the prescription of lipid-lowering medications. To demonstrate the ACC/AHA guidelines in a patient-centered perspective, three cases were presented. | Clinicians who consider applying the guidelines should determine the 10-year CVD risk for each patient and engage the patient in shared decision making using evidence-based approaches. The new ACC/AHA guidelines therefore create an opportunity to advance patient-centered care and shared decision making. Rather than routinely prescribing statins to the millions of adults who have a 10-year CVD risk of at least 7.5%, the realization of this opportunity requires clinicians to engage in deliberation with individual patients about the potential benefits, harms, and burdens of statin use. |
| To examine patient and caregiver perceptions of this technology to further develop an understanding of the benefits and functionalities that prospective patients deem as desirable, undesirable, inadequate or in need of further development. | Dhukaram, Baber and De Stefanis [17] | 2012 | Focus group studies | Focus group interviews and its results were used to understand patients’ concerns and perceptions toward pervasive healthcare systems and to explore potential barriers to the acceptance of the BraveHealth system, with participants recruited in Italy and England. After the presentation of the components of the system, the patients were asked to answer questions about the usability of biomedical devices, wearable units, touch screen technologies and virtual communities. | ITALY All participants had previously used biomedical devices; they suggested a system they can wear and switch on or off manually. The device they imagined should even notify its state of functioning, making them aware if it is charged and situated correctly on the body. All the patients asked for the implementation of a button to warn doctors or caregivers about emergencies. Three of those interviewed would like a fully integrated unit, i.e., as part of their clothing. ENGLAND Overall, participants in these focus groups showed a positive response in regard to the potential benefits of the BraveHealth concept. In general, these responses were related to the benefits of real-time monitoring of a range of parameters and the capability to receive a quick response to potential problems. However, concerns remained about reliability, security, privacy and trust. |
| The Canadian Journal of Cardiology | Kim and Rich [18] | 2016 | 2 Cases/Opinion | Case Study | A disease management program led by a heart failure nurse specialist and involving close telephone follow-up and home visits may reduce heart failure and all-cause admissions and mortality. Older patients with mild-to-moderate frailty may benefit more from such a program. The rate control strategy in atrial fibrillation was associated with fewer adverse events and admissions than was the rhythm control strategy, without differences in mortality, cardiovascular events, or quality of life. To reduce the treatment burden and improve adherence, medication dosing should be changed to once daily, if possible. Importantly, the CVD management strategy should be part of the general practitioner’s overall management plan, which should also address the patient’s non-cardiovascular conditions. In discussing the management plan with a patient, it is important to ensure that the plan is consistent with the preferences of the patient and that the patient agrees with the recommendations. A written summary can facilitate clear communication of the rationale for and details of the management plan with the family and other members of the healthcare team. The management plan should be revised based on the prognosis, functional status, and personal preferences of the patient. Discussion of advance care planning should take place before cognitive impairment progresses. Cardiologists should work closely with general practitioners to adopt a patient-centered approach to manage CVD and non-cardiovascular health that will have the greatest impact on functioning and quality of life in older adults with CVD and multimorbidity. |
| To increase health care professionals’ intention and encouraging behavior toward patient self-management, following cardiovascular risk management guidelines. | Sassen, Kok, Schepers and Vanhees [19] | 2014 | Experimental | The effectiveness of a Web-based intervention in the clinical practice of patient-centered care was tested. The intervention was developed to optimize processes of shared decision making and self-management, following the protocol for intervention mapping. The objective was to increase health care professionals’ intention and behavior toward encouraging patient self-management. Participants were health care professionals with at least a bachelor’s degree in nursing or physiotherapy and who had regular consultations with patients with cardiovascular risk factors. All participants were offered a three-hour training session. | Professionals in the intervention group stated that 59% of their consultation time was devoted to health education. The module to improve professionals’ behavior to optimize processes of shared decision making and self-management was used by 45% of the professionals; 45% used the screen to encourage a patient to think about their personal risk; 39% provided attitudinal change and outcome expectations; 30% provided guidance for resistance to social pressure and seeking support; 28% encouraged subskill enactment. For 24% of the patients, the professional provided planning for behavioral changes; 19% provided guidance regarding putting behavior changes into practice; and 15% provided guidance regarding maintaining behavior changes. Only in one of every five patients was the guidelines for cardiovascular risk management used. Professionals in the intervention group experienced more barriers to encouraging patients than did professionals in the control group. |
| To evaluated whether participating patients had reduced risks of cardiovascular events, including coronary heart disease, stroke, and all-cause mortality. | Kornelius, Chiou, Yang, Lu, Peng and Huang [20] | 2015 | Retrospective cohort study | The Diabetes Shared Care Program (DSCP), an integrated diabetes care model designed to increase the quality of diabetes care in Taiwan, was analyzed. Data were obtained from the National Health Insurance Research Database of Taiwan. DSCP participants received integrated care from a physician, diabetes educator, and dietitian. | Compared to nonparticipants, DSCP participants had significantly lower risks of overall CVD events. Patients with a history of hypertension and chronic lung diseases had a higher risk of CVD events. At the end of the study, the provision of integrated care arrangements for diabetic feet had a positive impact on the knowledge of primary care staff and on patients’ attitudes, resulting in an increased number of appropriate referrals to acute specialist services. Diabetic patients with a lower monthly income also had a higher risk of CVD events. Participation in the DSCP was associated with lower risks of overall CVD events, including stroke and all-cause mortality. |
| To gain insight into what motivates older people living in the community to partake in a cardiovascular prevention programme, and reasons for subsequent continuation or withdrawal. | Ligthart, Eerenbeemt, Pols, Van Bussel, Richard and Van Charante [21] | 2015 | Qualitative | The sample consisted of PreDIVA participants (all people aged 70–78 years were invited to participate through a letter from their general practitioner). Semi-structured interviews were conducted in six different healthcare centers. | Almost all participants emphasized the importance of the relationship with the practice nurse. In general, participants wished to be involved in medical decisions, such as starting medication or getting additional diagnostic tests, but they were prepared to follow the advice of their health professional, even if they did not always fully understand the rationale. Some interviewees expressed the importance of their autonomy being respected; the perception of being ‘checked up on’ gave a sense of control, safety or being looked after. It was seen as an essential component of the program and a reason for starting and continuing participation. The personal approach of the practice nurse appeared to be crucial. In addition to the nurses’ medical expertise, their ability to listen and to build a personal relationship was strongly linked to trust and prolonged participation. Participants wanted nurses to have a coach-like and supportive attitude. |
| To explored the potential of patient-held alert cards to improve communication and continuity of care for heart failure patients moving between CHFSNs and hospital settings | McBride, Burey, Megahed, Feldman and Deaton [22] | 2014 | Qualitative Mixed Approach | This study investigated the management of patients with heart failure (HF) by community heart failure specialist nurses (CHFSNs) by exploring the potential of patient-held alert cards to improve communication and continuity of care for patients with HF. The follow-up was 12 months. Alert cards were issued to 119 patients. The CHFSNs excluded patients with cognitive impairments or frailty. | The involvement of CHFSNs facilitated the continuity of care for HF patients at different levels and sectors of the healthcare system, in addition to improving safety and effectiveness. The alert cards empowered both patients and caregivers to take a more active role in their care. First, although CHFSNs explained an HF diagnosis as part of their assessment, the card itself appeared to prompt patients to ask questions about their condition. In the absence of immediate technological solutions to bridge the primary and secondary interface, this study illustrated how a patient-held alert card can provide informational continuity, as it encouraged general wards to liaise with specialist nurses on admission to ensure the continuation and appropriateness of care. |
| The impact of a pharmacy-managed program for providing education and discharge instructions for patients with heart failure (HF) was evaluated. | Warden, Freels, Furuno and Mackay [23] | 2014 | Quasi-experimental Therapeutic Reconciliation | Intervention performed with adult patients admitted to Oregon Health and Science University’s cardiology unit with systolic HF exacerbation as their primary diagnosis. The HF-MED study evaluated the impact of pharmacist involvement in providing education and discharge instructions. Eighty-two percent of patients had an ejection fraction of <30%, 88% had functional class III or IV HF based on the New York Heart Association criteria, and 99% had functional class C or D HF based on the American College of Cardiology-American Heart Association criteria. | The HF-MED program was associated with a significant difference in favor of the pharmaceutical intervention group for both analyzed central measures of the Joint Commission, with adherence that exceeded their respective UHC reference parameters mentioned previously and 30-day readmissions for all causes. There was also a nonsignificant trend in reductions in 30-day readmissions related to HF. When evaluating the experience of patients with the service, 86% believed that medication counseling was important, 91% were satisfied with the service, and 74% were more likely to return to OHSU because of this program. |
| To evaluate the impact of an intensive, evidence-based preventive cardiology programme on medical and lifestyle risk factors in patients at high risk of developing cardiovascular disease (CVD) | Gibson, Flaherty, Cormican, Jones, Kerins, Walsh, Costello, Windle, Connolly and Crowley [24] | 2014 | Descriptive | The impact of an intensive evidence-based preventive cardiology program (Croi MyAction program-London) on medical and lifestyle risk factors in patients at high risk of developing CVD was evaluated. All participants were invited to bring a partner to the program, with an uptake rate of 61% among those who had a partner. | Among diabetic patients, glycemic control improved during the program. The prescription of all cardioprotective medications, with the exception of beta-blockers, increased significantly during the program. In addition to biomedical improvements, patients derived significant psychosocial benefits from the program, with fewer patients having raised levels of anxiety or depression at the end of the program (after one year). Participants in the current study completed a program that involved risk factor reduction through lifestyle modification, supplemented by target-driven pharmacological interventions. High cessation rates were observed among smokers, there was increased adherence to the cardioprotective diet, and physical activity increased with an associated improvement in physical fitness. Reductions in BMI and abdominal circumference were observed. Improvements were observed in blood pressure and glycemic control and in all blood lipid fractions. |
| To evaluate whether PCC is associated with less self-reported uncertainty in illness compared with usual care in patients hospitalized for worsening CHF. | Dudas, Olsson, Wolf, Swedberg, Taft, Schaufelberger and Ekman [25] | 2013 | Experimental | The study evaluated whether person-centered care with less uncertainty in illness was comparable to usual care (UC) in patients hospitalized for worsening chronic heart failure (CHF). All patients with a prior diagnosis of CHF admitted to five designated wards at the Department of Medicine at Sahlgrenska University Hospital/Östra in Gothenburg, Sweden, were screened for symptoms of worsening CHF (mainly dyspnea and/or fatigue). The patients were assessed by a physician before study inclusion, following the ESC guidelines for diagnosing CHF. | The results of the study suggest that compared to UC, PCC in patients hospitalized for worsening CHF seems to have a positive effect in reducing self-reported uncertainty in illness. When caregivers and patients worked together as partners in a structured PCC plan, many of the issues and uncertainties with which the patients struggled were cleared up and resolved during hospitalization. Many patients reported that in today’s healthcare system, they often have to navigate through a fragmented healthcare system where the perspective of the health professional prevails, instead of receiving care designed to focus on individual needs, preferences and values. PCC strengthened the patients’ perception of treatment effectiveness. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marques, M.d.C.; Pires, R.; Perdigão, M.; Sousa, L.; Fonseca, C.; Pinho, L.G.; Lopes, M. Patient-Centered Care for Patients with Cardiometabolic Diseases: An Integrative Review. J. Pers. Med. 2021, 11, 1289. https://doi.org/10.3390/jpm11121289
Marques MdC, Pires R, Perdigão M, Sousa L, Fonseca C, Pinho LG, Lopes M. Patient-Centered Care for Patients with Cardiometabolic Diseases: An Integrative Review. Journal of Personalized Medicine. 2021; 11(12):1289. https://doi.org/10.3390/jpm11121289
Chicago/Turabian StyleMarques, Maria do Céu, Rute Pires, Miguel Perdigão, Luis Sousa, César Fonseca, Lara Guedes Pinho, and Manuel Lopes. 2021. "Patient-Centered Care for Patients with Cardiometabolic Diseases: An Integrative Review" Journal of Personalized Medicine 11, no. 12: 1289. https://doi.org/10.3390/jpm11121289







