Prevalence and Clinicopathological Characteristics of Moderate and High-Penetrance Genes in Non-BRCA1/2 Breast Cancer High-Risk Spanish Families
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. DNA Extraction
2.3. Next Generation Sequencing
2.4. Variant Classifications
2.5. Statistical Analysis
3. Results
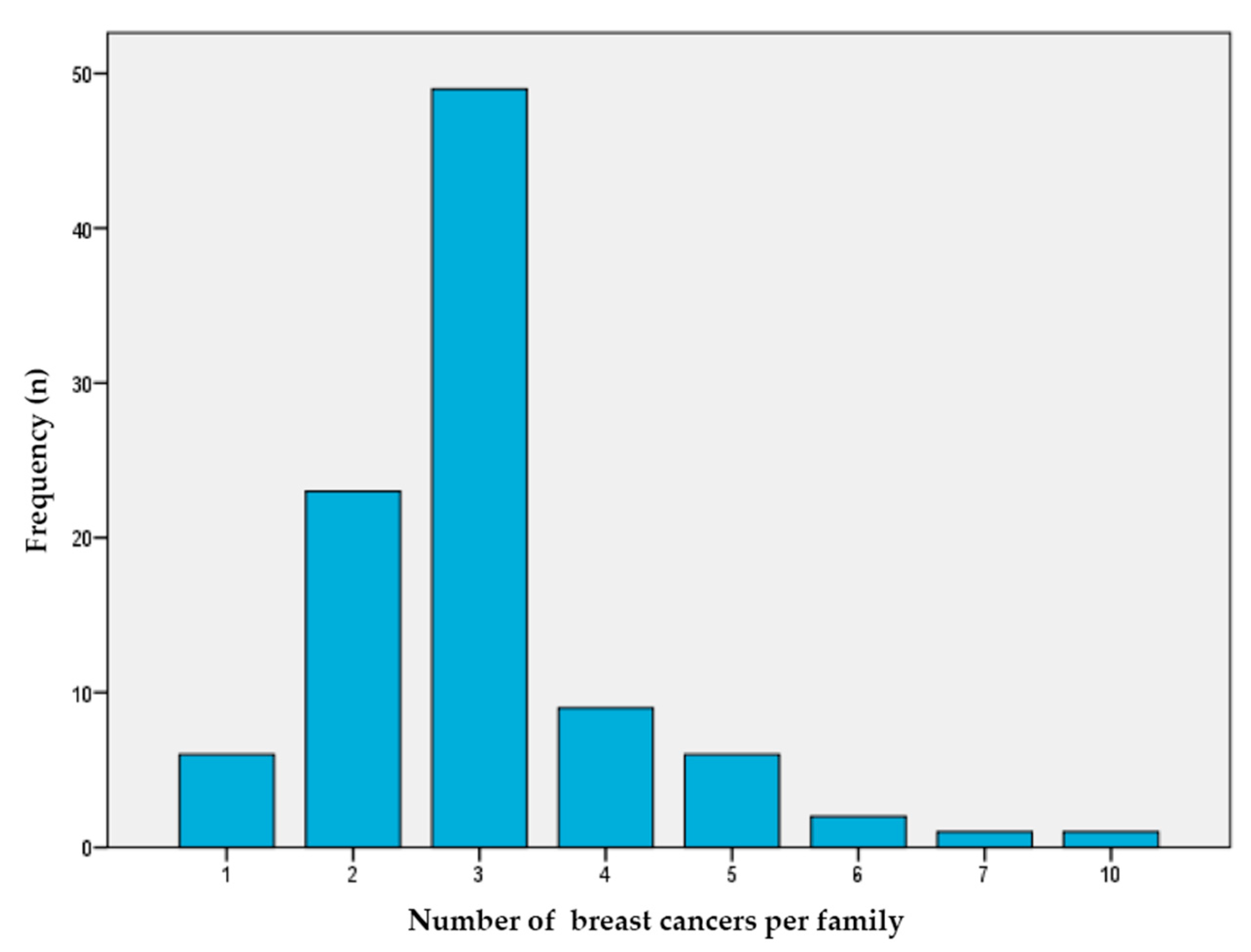
3.1. Characteristics of the Study Population
3.2. Next-Generation Sequencing Quality
3.3. Frequency of Deleterious Mutations
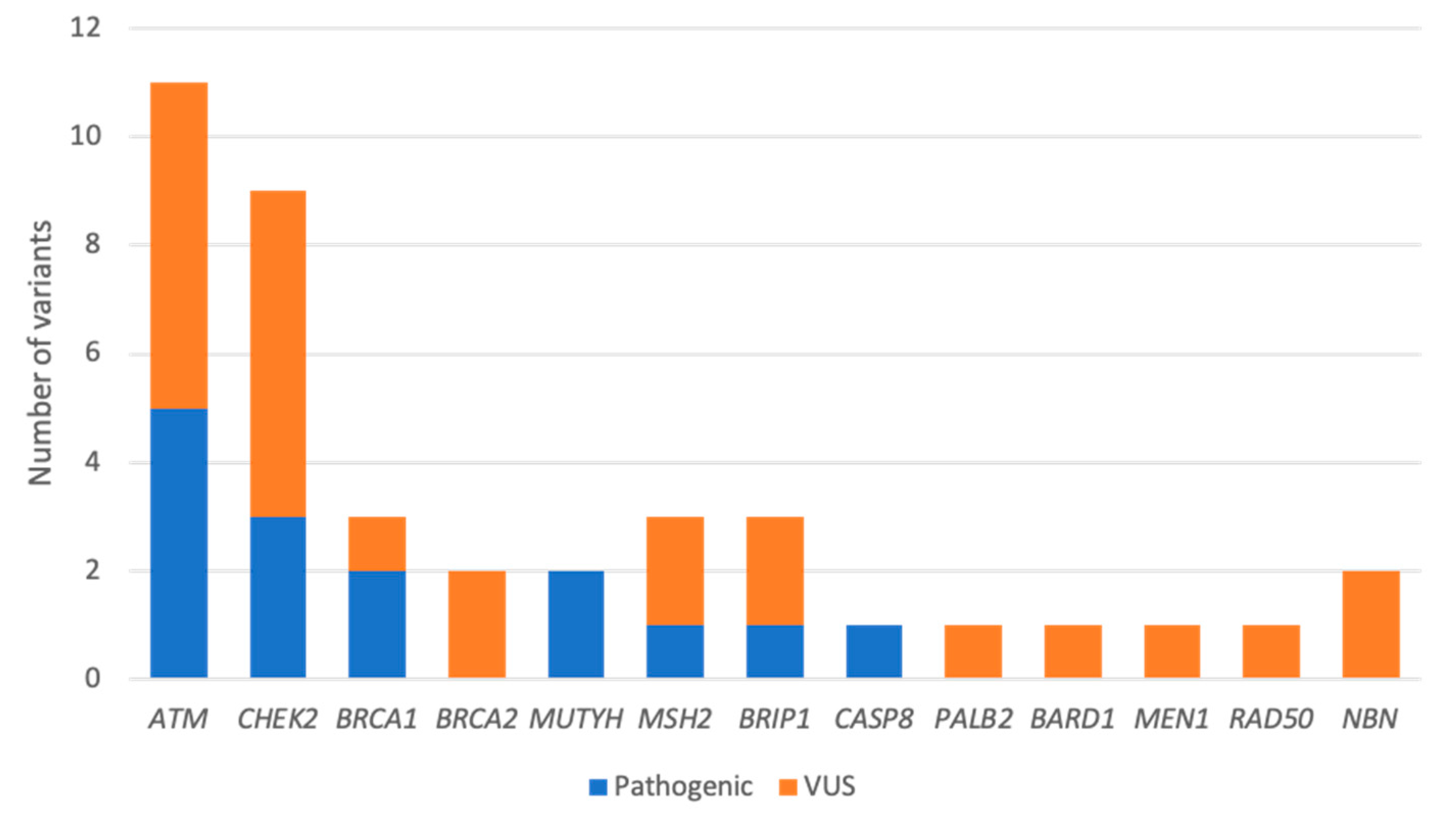
3.4. Clinical Characteristics in Cases with Pathogenic Variants
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Pineros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Kurian, A.W.; Hare, E.E.; Mills, M.A.; Kingham, K.E.; McPherson, L.; Whittemore, A.S.; McGuire, V.; Ladabaum, U.; Kobayashi, Y.; Lincoln, S.E.; et al. Clinical Evaluation of a Multiple-Gene Sequencing Panel for Hereditary Cancer Risk Assessment. J. Clin. Oncol. 2014, 32, 2001–2009. [Google Scholar] [CrossRef]
- Daly, M.B.; Pilarski, R.; Berry, M.P.; Buys, S.S. Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic. NCCN Clin. Pract. Guidel. Oncol. 2021, 19, 77–102. [Google Scholar] [CrossRef]
- Nielsen, F.C.; Van Overeem Hansen, T.; Sørensen, C.S. Hereditary breast and ovarian cancer: New genes in confined pathways. Nat. Rev. Cancer 2016, 16, 599–612. [Google Scholar] [CrossRef]
- Easton, D.F.; Pharoah, P.D.P.; Antoniou, A.C.; Tischkowitz, M.; Tavtigian, S.V.; Nathanson, K.L.; Devilee, P.; Meindl, A.; Couch, F.J.; Southey, M.; et al. Gene-panel sequencing and the prediction of breast-cancer risk. N. Engl. J. Med. 2015, 372, 2243–2257. [Google Scholar] [CrossRef]
- Castéra, L.; French Exome Project Consortium; Harter, V.; Muller, E.; Krieger, S.; Goardon, N.; Ricou, A.; Rousselin, A.; Paimparay, G.; Legros, A.; et al. Landscape of pathogenic variations in a panel of 34 genes and cancer risk estimation from 5131 HBOC families. Genet. Med. 2018, 20, 1677–1686. [Google Scholar] [CrossRef]
- Meiss, A.E.; Thomas, M.; Modesitt, S.C.; Ring, K.L.; Atkins, K.A.; Mills, A.M. Clinicopathologic characterization of breast carcinomas in patients with non-BRCA germline mutations: Results from a single institution’s high-risk population. Hum. Pathol. 2018, 82, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Thompson, E.R.; Rowley, S.M.; Li, N.; McInerny, S.; Devereux, L.; Wong-Brown, M.W.; Trainer, A.; Mitchell, G.; Scott, R.; James, P.; et al. Panel testing for familial breast cancer: Calibrating the tension between research and clinical care. J. Clin. Oncol. 2016, 34, 1455–1459. [Google Scholar] [CrossRef] [PubMed]
- Tung, N.; Domchek, S.M.; Stadler, Z.; Nathanson, K.L.; Couch, F.; Garber, J.E.; Offit, K.; Robson, M.E. Counselling framework for moderate-penetrance cancer-susceptibility mutations. Nat. Rev. Clin. Oncol. 2016, 13, 581. [Google Scholar] [CrossRef]
- Kleiblova, P.; Stolarova, L.; Krizova, K.; Lhota, F.; Hojny, J.; Zemankova, P.; Havranek, O.; Vocka, M.; Cerna, M.; Lhotova, K.; et al. Identification of deleterious germline CHEK2 mutations and their association with breast and ovarian cancer. Int. J. Cancer 2019, 145, 1782–1797. [Google Scholar] [CrossRef] [PubMed]
- Le Calvez-Kelm, F.; Lesueur, F.; Damiola, F.; Vallée, M.; Voegele, C.; Babikyan, D.; Lesueur, F.; Byrnes, G.B.; Chuang, S.-C.; Forey, N.; et al. Rare, evolutionarily unlikely missense substitutions in CHEK2 contribute to breast cancer susceptibility: Results from a breast cancer family registry case-control mutation-screening study. Breast Cancer Res. 2011, 13, 1–12. [Google Scholar] [CrossRef]
- Ma, X.; Zhang, B.; Zheng, W. Genetic variants associated with colorectal cancer risk: Comprehensive research synopsis, meta-analysis, and epidemiological evidence. Lancet Oncol. 2014, 12, 477–488. [Google Scholar] [CrossRef]
- Lu, H.M.; Li, S.; Black, M.H.; Lee, S.; Hoiness, R.; Wu, S.; Mu, W.; Huether, R.; Chen, J.; Sridhar, S.; et al. Association of Breast and Ovarian Cancers with Predisposition Genes Identified by Large-Scale Sequencing. JAMA Oncol. 2019, 5, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Castéra, L.; Krieger, S.; Rousselin, A.; Legros, A.; Baumann, J.-J.; Bruet, O.; Brault, B.; Fouillet, R.; Goardon, N.; Letac, O.; et al. Next-generation sequencing for the diagnosis of hereditary breast and ovarian cancer using genomic capture targeting multiple candidate genes. Eur. J. Hum. Genet. 2014, 22, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.J.; Momand, J.; Finlay, C.A. The p53 tumour suppressor gene. Nature 1991, 351, 453–456. [Google Scholar] [CrossRef]
- Borras, E.; Chang, K.; Pande, M.; Cuddy, A.; Bosch, J.L.; Bannon, S.A.; Mork, M.E.; Rodriguez-Bigas, M.A.; Taggart, M.W.; Lynch, P.M.; et al. In silico systems biology analysis of variants of uncertain significance in lynch syndrome supports the prioritization of functional molecular validation. Cancer Prev. Res. 2017, 10, 580–587. [Google Scholar] [CrossRef]
- Barrington, D.A.; Champion, M.L.; Boitano, T.K.L.; Walters-Haygood, C.L.; Farmer, M.B.; Alvarez, R.D.; Estes, J.M.; Leath, C.A. Characteristics of African American women at high-risk for ovarian cancer in the southeast: Results from a Gynecologic Cancer Risk Assessment Clinic. Gynecol Oncol. 2018, 149, 337–340. [Google Scholar] [CrossRef] [PubMed]
- García-Pérez, M.A.; Allende, L.M.; Corell, A.; Varela, P.; Moreno, A.A.; Sotoca, A.; Moreno, A.; Paz-Artal, E.; Barreiro, E.; Arnaiz-Villena, A. Novel mutations and defective protein kinase C activation of T-lymphocytes in ataxia telangiectasia. Clin. Exp. Immunol. 2001, 123, 472–480. [Google Scholar] [CrossRef]
- Cock-Rada, A.M.; Ossa, C.A.; García, H.I.; Gomez, L.R. A multi-gene panel study in hereditary breast and ovarian cancer in Colombia. Fam. Cancer 2018, 17, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Telatar, M.; Wang, Z.; Castellvi-Bel, S.; Tai, L.-Q.; Sheikhavandi, S.; Regueiro, J.; Porras, O.; Gatti, R. A Model for ATM Heterozygote Identification in a Large Population: Four Founder-Effect ATM Mutations Identify Most of Costa Rican Patients with Ataxia Telangiectasia. Mol. Genet. Metab. 1998, 64, 36–43. [Google Scholar] [CrossRef]
- Maxwell, K.N.; Wubbenhorst, B.; Andrea, K.D.; Garman, B.; Long, J.M.; Lcgc, M.S.; Zhu, J.; Bradbury, A.R.; Simon, M.S.; DeMichele, A.; et al. Prevalence of mutations in a panel of breast cancer susceptibility genes in BRCA1/2 negative patients with early onset breast cancer. Genet. Med. 2016, 17, 630–638. [Google Scholar] [CrossRef]
- Decker, B.; Allen, J.; Luccarini, C.; Pooley, K.A.; Shah, M.; Bolla, M.K.; Wang, Q.; Ahmed, S.; Baynes, C.; Conroy, D.M.; et al. Rare, protein-truncating variants inATM, CHEK2 and PALB2, but not XRCC2, are associated with increased breast cancer risks. J. Med Genet. 2017, 54, 732–741. [Google Scholar] [CrossRef] [PubMed]
- Leedom, T.P.; LaDuca, H.; McFarland, R.; Li, S.; Dolinsky, J.S.; Chao, E.C. Breast cancer risk is similar for CHEK2 founder and non-founder mutation carriers. Cancer Genet. 2016, 209, 403–407. [Google Scholar] [CrossRef]
- Olivier, M.; Goldgar, D.E.; Sodha, N.; Ohgaki, H.; Kleihues, P.; Hainaut, P.; Eeles, R.A. Li-Fraumeni and related syndromes: Correlation between tumor type, family structure, and TP53 genotype. Cancer Res. 2003, 63, 6643–6650. [Google Scholar] [PubMed]
- ClinVar. Available online: https://www.ncbi.nlm.nih.gov/clinvar/ (accessed on 22 December 2020).
- Nielsen, M.; Morreau, H.; Vasen, H.F.A.; Hes, F.J. MUTYH-associated polyposis (MAP). Crit. Rev. Oncol. 2011, 79, 1–16. [Google Scholar] [CrossRef]
- Tung, N.; Lin, N.U.; Kidd, J.; Allen, B.A.; Singh, N.; Wenstrup, R.J.; Hartman, A.-R.; Winer, E.P.; Garber, J.E. Frequency of Germline Mutations in 25 Cancer Susceptibility Genes in a Sequential Series of Patients with Breast Cancer. J. Clin. Oncol. 2016, 34, 1460–1468. [Google Scholar] [CrossRef]
- Couch, F.J.; Shimelis, H.; Hu, C.; Hart, S.N.; Polley, E.C.; Na, J.; Hallberg, E.; Moore, R.; Thomas, A.; Lilyquist, J.; et al. Associations between Cancer Predisposition Testing Panel Genes and Breast Cancer. JAMA Oncol. 2017, 3, 1190–1196. [Google Scholar] [CrossRef]
- Eliade, M.; Skrzypski, J.; Baurand, A.; Jacquot, C.; Bertolone, G.; Loustalot, C.; Coutant, C.; Guy, F.; Fumoleau, P.; Duffourd, Y.; et al. The transfer of multigene panel testing for hereditary breast and ovarian cancer to healthcare: What are the implications for the management of patients and families? Oncotarget 2016, 8, 1957–1971. [Google Scholar] [CrossRef]
- Bonache, S.; Esteban, I.; Moles-Fernández, A.; Tenés, A.; Duran-Lozano, L.; Montalban, G.; Bach, V.; Carrasco, E.; Gadea, N.; López-Fernández, A.; et al. Multigene panel testing beyond BRCA1/2 in breast/ovarian cancer Spanish families and clinical actionability of findings. J. Cancer Res. Clin. Oncol. 2018, 144, 2495–2513. [Google Scholar] [CrossRef]
- Hauke, J.; Horvath, J.; Groß, E.; Gehrig, A.; Honisch, E.; Hackmann, K.; Schmidt, G.; Arnold, N.; Faust, U.; Sutter, C.; et al. Gene panel testing of 5589 BRCA1/2-negative index patients with breast cancer in a routine diagnostic setting: Results of the German Consortium for Hereditary Breast and Ovarian Cancer. Cancer Med. 2018, 7, 1349–1358. [Google Scholar] [CrossRef] [PubMed]
- Girard, E.; Eon-Marchais, S.; Olaso, R.; Renault, A.; Damiola, F.; Dondon, M.; Barjhoux, L.; Goidin, D.; Meyer, V.; Le Gal, D.; et al. Familial breast cancer and DNA repair genes: Insights into known and novel susceptibility genes from the GENESIS study, and implications for multigene panel testing. Int. J. Cancer 2019, 144, 1962–1974. [Google Scholar] [CrossRef]
- Dorling, L.; Carvalho, S.; Allen, J.; González-Neira, A.; Luccarini, C.; Wahlström, C.; Pooley, K.A.; Parsons, M.T.; Fortuno, C.; Wang, Q.; et al. Breast Cancer Risk Genes—Association Analysis in More than 113,000 Women. N. Engl. J. Med. 2021, 384, 428–439. [Google Scholar]
- p53IARC. Available online: https://p53.iarc.fr/ (accessed on 16 February 2021).
- Schneider, K.; Zelley, K.; Nichols, K.E.; Garber, J. Li-Fraumeni Syndrome. In Gene Reviews. Available online: https://www.ncbi.nlm.nih.gov/books/NBK1311/?report=classic (accessed on 17 March 2021).
- Bougeard, G.; Renaux-Petel, M.; Flaman, J.-M.; Charbonnier, C.; Fermey, P.; Belotti, M.; Gauthier-Villars, M.; Stoppa-Lyonnet, D.; Consolino, E.; Brugières, L.; et al. Revisiting Li-Fraumeni Syndrome From TP53 Mutation Carriers. J. Clin. Oncol. 2015, 33, 2345–2352. [Google Scholar] [CrossRef]
- Zerdoumi, Y.; Lanos, R.; Raad, S.; Flaman, J.M.; Bougeard, G.; Frebourg, T.; Tournier, I. Germline TP53 mutations result into a constitutive defect of p53 DNA binding and transcriptional response to DNA damage. Hum. Mol. Genet. 2017, 26, 2591–2602. [Google Scholar] [CrossRef] [PubMed]
- Li, F.P.; Fraumeni, J.F.; Mulvihill, J.J.; Blattner, W.A.; Dreyfus, M.G.; Tucker, M.A.; Miller, R.W. A cancer family syndrome in twenty-four kindreds. Cancer Res. 1988, 48, 5358–5362. [Google Scholar] [PubMed]
- Tinat, J.; Bougeard, G.; Baert-Desurmont, S.; Vasseur, S.; Martin, C.; Bouvignies, E.; Caron, O.; Paillerets, B.B.-D.; Berthet, P.; Dugast, C.; et al. 2009 Version of the Chompret Criteria for Li Fraumeni Syndrome. J. Clin. Oncol. 2009, 27, e108–e109. [Google Scholar] [CrossRef] [PubMed]
- Rath, M.G.; Masciari, S.; Gelman, R.; Miron, A.; Miron, P.; Foley, K.; Richardson, A.L.; Krop, I.E.; Verselis, S.J.; Dillon, D.A.; et al. Prevalence of germline TP53 mutations in HER2+ breast cancer patients. Breast Cancer Res. Treat. 2013, 139, 193–198. [Google Scholar] [CrossRef]
- Li, J.; Meeks, H.; Feng, B.-J.; Healey, S.; Thorne, H.; Makunin, I.; Ellis, J.; Campbell, I.; Southey, M.; Mitchell, G.; et al. Targeted massively parallel sequencing of a panel of putative breast cancer susceptibility genes in a large cohort of multiple-case breast and ovarian cancer families. J. Med Genet. 2016, 53, 34–42. [Google Scholar] [CrossRef]
- Lin, W.-Y.; Camp, N.J.; Ghoussaini, M.; Beesley, J.; Michailidou, K.; Hopper, J.L.; Apicella, C.; Southey, M.C.; Stone, J.; Schmidt, M.K.; et al. Identification and characterization of novel associations in the CASP8/ALS2CR12 region on chromosome 2 with breast cancer risk. Hum. Mol. Genet. 2015, 24, 285–298. [Google Scholar] [CrossRef]
- Camp, N.J.; Parry, M.; Knight, S.; Abo, R.; Elliott, G.; Rigas, S.H.; Balasubramanian, S.P.; Reed, M.; McBurney, H.; Latif, A.; et al. Fine-Mapping CASP8 Risk Variants in Breast Cancer. Cancer Epidemiol. Biomark. Prev. 2012, 21, 176–181. [Google Scholar] [CrossRef]
- Michailidou, K.; Beesley, J.; Lindstrom, S.; Canisius, S.; Dennis, J.; Lush, M.J.; Maranian, M.J.; Bolla, M.K.; Wang, Q.; Shah, M.; et al. Genome-wide association analysis of more than 120,000 individuals identifies 15 new susceptibility loci for breast cancer. Nat. Genet. 2015, 47, 373–380. [Google Scholar] [CrossRef]
- Yang, Y.; Shu, X.; Shu, X.-O.; Bolla, M.K.; Kweon, S.-S.; Cai, Q.; Michailidou, K.; Wang, Q.; Dennis, J.; Park, B.; et al. Re-evaluating genetic variants identified in candidate gene studies of breast cancer risk using data from nearly 280,000 women of Asian and European ancestry. EBioMedicine 2019, 48, 203–211. [Google Scholar] [CrossRef]
- Stephens, P.J.; Tarpey, P.S.; Davies, H.; Van Loo, P.; Greenman, C.; Wedge, D.C.; Nik-Zainal, S.; Martin, S.; Varela, I.; Bignell, G.R.; et al. The landscape of cancer genes and mutational processes in breast cancer. Nature 2012, 486, 400–404. [Google Scholar] [CrossRef]
- Li, N.; Rowley, S.M.; Thompson, E.R.; McInerny, S.; Devereux, L.; Amarasinghe, K.C.; Zethoven, M.; Lupat, R.; Goode, D.; Li, J.; et al. Evaluating the breast cancer predisposition role of rare variants in genes associated with low-penetrance breast cancer risk SNPs. Breast Cancer Res. 2018, 20, 3. [Google Scholar] [CrossRef]
- Aloraifi, F.; McDevitt, T.; Martiniano, R.; McGreevy, J.; McLaughlin, R.; Egan, C.M.; Cody, N.; Meany, M.; Kenny, E.; Green, A.J.; et al. Detection of novel germline mutations for breast cancer in non-BRCA1/2 families. FEBS J. 2015, 282, 3424–3437. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Hart, S.N.; Gnanaolivu, R.; Huang, H.; Lee, K.Y.; Na, J.; Gao, C.; Lilyquist, J.; Yadav, S.; Boddicker, N.J.; et al. A Population-Based Study of Genes Previously Implicated in Breast Cancer. N. Engl. J. Med. 2021, 384, 440–451. [Google Scholar] [CrossRef]
- Buys, S.S.; Sandbach, J.F.; Gammon, A.; Patel, G.; Kidd, J.; Brown, K.L.; Sharma, L.; Saam, J.; Lancaster, J.; Daly, M.B. A study of over 35,000 women with breast cancer tested with a 25-gene panel of hereditary cancer genes. Cancer 2017, 123, 1721–1730. [Google Scholar] [CrossRef]
- Rana, H.Q.; Gelman, R.; LaDuca, H.; McFarland, R.; Dalton, E.; Thompson, J.; Speare, V.; Dolinsky, J.S.; Chao, E.C.; Garber, J.E. Differences in TP53 Mutation Carrier Phenotypes Emerge from Panel-Based Testing. J. Natl. Cancer Inst. 2018, 110, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Beitsch, P.D.; Whitworth, P.W.; Hughes, K.; Patel, R.; Rosen, B.; Compagnoni, G.; Baron, P.; Simmons, R.; Smith, L.A.; Grady, I.; et al. Underdiagnosis of hereditary breast cancer: Are genetic testing guidelines a tool or an obstacle? J. Clin. Oncol. 2019, 37, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Young, S.R.; Pilarski, R.T.; Donenberg, T.; Shapiro, C.; Hammond, L.S.; Miller, J.; Brooks, K.A.; Cohen, S.; Tenenholz, B.; DeSai, D.; et al. The prevalence of BRCA1 mutations among young women with triple-negative breast cancer. BMC Cancer 2009, 9, 86. [Google Scholar] [CrossRef] [PubMed]
| All | With Mutation 1 | Without Mutation | |
|---|---|---|---|
| Total patients (n) | 95 | 14 | 81 |
| Sex | |||
| Female | 91 (95.7%) | 13 (92.8%) | 78 (96.2%) |
| Male | 4 (4.2%) | 1 (7.14%) | 3 (3.7%) |
| Median age at diagnosis (range) | 46 (23–73) | 45 (28–66) | 46 (23–73) |
| Age at diagnosis | |||
| <30 | 8 (8.4%) | 1 (7.1%) | 7 (8.6%) |
| 30–40 | 22 (23.1%) | 4 (28.5%) | 18 (22.2%) |
| 41–50 | 43 (45.2%) | 6 (42.8%) | 37 (45.6%) |
| 51–60 | 17 (17.8%) | 1 (7.1%) | 16 (19.7%) |
| 61–70 | 5 (5.2%) | 1 (7.1%) | 4 (4.9%) |
| >70 | 1 (1.0%) | 0 | 1 (1.2%) |
| T stage | |||
| Tis | 9 (9.4%) | 0 | 9 (11.1%) |
| T1 | 43 (45.2%) | 4 (28.1%) | 39 (48.1%) |
| T2 | 31 (32.6%) | 4 (28.1%) | 27 (33.3%) |
| T3 | 8 (8.4%) | 2 (14.2%) | 5 (6.1%) |
| T4 | 2 (2.1%) | 1 (7.1%) | 1 (1.2%) |
| N stage | |||
| N0 | 56 (58.9%) | 4 (28.5%) | 52 (64.1%) |
| N1 | 30 (31.5%) | 5 (35.7%) | 25 (30.8%) |
| N2–N3 | 8 (8.4%) | 3 (21.4%) | 5 (6.1%) |
| Grade | |||
| 1 | 22 (23.1%) | 5 (35.7%) | 17 (20.9%) |
| 2 | 41 (43.1%) | 6 (42.8%) | 35 (43.2%) |
| 3 | 21 (22.1%) | 1 (7.1%) | 20 (24.6%) |
| Unknown | 13 (13.6%) | 2 (14.2%) | 11 (13.5%) |
| Hormonal receptor status | |||
| Positive | 74 (77.8%) | 11 (78.5%) | 63 (77.7%) |
| Negative | 14 (14.7%) | 2 (14.2%) | 12 (14.8%) |
| Unknown | 8 (8.4%) | 1 (7.1%) | 7 (8.6%) |
| Estrogen receptor status | |||
| Positive | 71 (73.6%) | 9 (64.2%) | 61 (75.3%) |
| Negative | 17 (17.8%) | 4 (28.5%) | 14 (17.2%) |
| Unknown | 7 (8.4%) | 1 (7.1%) | 6 (7.4%) |
| Her2 status | |||
| Positive | 16 (16.8%) | 2 (14.2%) | 14 (17.2%) |
| Negative | 63 (66.3%) | 10 (71.4%) | 53 (65.4%) |
| Unknown | 18 (18.9%) | 2 (14.2%) | 16 (19.7%) |
| Immunophenotype | |||
| Luminal A | 35 (36.8%) | 6 (42.8%) | 29 (35.8%) |
| Luminal B | 22 (23.1%) | 3 (21.4%) | 19 (23.4%) |
| Triple negative | 7 (7.3%) | 1 (7.1%) | 6 (7.4%) |
| Her2 + Hormonal Receptor - | 5 (5.2%) | 1 (7.1%) | 4 (12.3%) |
| Triple positive | 11 (11.5%) | 1 (7.1%) | 10 (12.3%) |
| Unknown | 17 (17.8%) | 2 (14.2%) | 15 (18.5%) |
| Bilateral breast cancer | 18 (18.9%) | 3 (21.4%) | 15 (18.5%) |
| Family history of cancer | |||
| Breast | 95 (100%) | 14 (100%) | 81 (100%) |
| Melanoma | 2 (2.1%) | 0 | 2 (2.4%) |
| Ovarian | 17 (17.8%) | 2 (14.2%) | 15 (17.8%) |
| Prostate | 17 (17.8%) | 2 (14.2%) | 15 (17.8%) |
| Colorectal | 9 (9.4%) | 3 (21.4%) | 6 (7.4%) |
| Pancreatic | 5 (5.2%) | 1 (7.1%) | 4 (4.7%) |
| Others | 13 (13.6%) | 3 (21.4%) | 10 (12.3%) |
| Gene Variants | Personal History | Family History | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study ID | Gene | Variant Type | Class 1 | HGVS Coding | HGVS Protein | Transcripts | rsID | 2nd Variant | BC Age | Subtype (ER/PR/HER2) | Bilateral BC | No. Cancers | No. BCs | No. OCs |
| 35022 | BRCA1 | Splicing | 5 | c.5152 + 5G > A | - | NM_007294.3 | rs80358165 | - | 45 | −/+/− | No | 2 | 2 | 0 |
| 30983 | BRCA1 | Missense | 4 | c.5324T > G | p.Met1775Arg | NM_07300.4 | rs41293463 | - | 31 | −/−/− | Yes | 1 | 1 | 0 |
| 24247 | ATM | Stop codon | 5 | c.2413C > T | p.Arg805Ter | NM_000051.4 | rs780619951 | - | 34 | +/+/− | Yes | 3 | 2 | 0 |
| 45434 | ATM | Splicing | 5 | c.2921 + 1G > A | - | NM_000051.4 | rs587781558 | - | 42 | +/+/− | No | 3 | 3 | 0 |
| 36845 | ATM | Splicing | 5 | c.2921 + 1G > A | - | NM_000051.4 | rs587781558 | - | 45 | +/+/− | No | 4 | 2 | 1 |
| 26672 | ATM | Frameshift | 5 | c.43delC | p.Leu15Terfs | NM_000051.4 | rs771887195 | - | 48 | +/+/− | No | 2 | 2 | 0 |
| 47150 | ATM | Stop Codon | 5 | c.4507C > T | p.Gln1503Ter | NM_000051.4 | rs1131691164 | CHEK2 c.1555C > T (p.Arg519Ter)Class 5 | 48 | +/+/− | No | 3 | 2 | 1 |
| 60766 | CHEK2 | Stop Codon | 5 | c.279G > A | p.Trp93Ter | NM_007194.4 | rs587782070 | - | 66 | +/+/− | Yes | 10 | 10 | 0 |
| 36497 | CHEK2 | Frameshift | 5 | c.591delA | p.Val198Phefs | NM_007194.4 | rs587782245 | - | 37 | +/+/+ | No | 3 | 2 | 0 |
| 55930 | TP53 | Missense | 5 | c.743G > A | p.Arg248Gln | NM_000546.6 | rs11540652 | - | 28 | −/−/+ | No | 3 | 2 | 0 |
| 18358 | TP53 | Missense | 5 | c.638G > A | p.Arg213Gln | NM_000546.6 | rs587778720 | - | 32 | −/+/? | No | 6 | 3 | 0 |
| 61221 | BRIP1 | Splicing | 5 | c.508−2A > T | - | NM_032043.2 | rs876659707 | - | 62 | +/+/− | No | 3 | 1 | 0 |
| 39477 | MSH2 | Missense | 4 | c.2320A > G | p.Ile774Phe | NM_000251.2 | rs775464903 | - | 50 | +/+/− | No | 5 | 2 | 0 |
| 36984 | MUTYH | Missense | 5 | c.1187G > A | p.Gly396Asp | NM_001048174.2 | rs36053993 | - | 50 | +/+/− | No | 3 | 3 | 0 |
| 43701 | MUTYH | Missense | 5 | c.1187G > A | p.Gly396Asp | NM_001048174.2 | rs36053993 | - | 51 | +/−/− | No | 4 | 3 | 0 |
| 38266 | CASP8 | Frameshift | 4 | c.331delG | p.Ala111Leufs*22 | NM_01228.4 | rs776712453 | NBN c.1238A > G (p.Asn413Ser) Class 3 | 57 | +/+/− | No | 7 | 3 | 0 |
| Clinical Factors | Level | PV Ratio | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Age | ≤45 | 17.78% (8/45) | 1.32 (0.38, 4.74) | 0.77927 |
| > 45 | 14.00% (7/50) | |||
| Bilateral involvement | No | 15.79% (12/76) | 0.94 (0.21, 5.82) | 1 |
| Yes | 16.67% (3/18) | |||
| Luminal | No | 15.00% (6/40) | 0.90 (0.24, 3.16) | 1 |
| Yes | 16.36% (9/55) | |||
| Her2 positive | No | 19.05% (12/63) | 1.64 (0.31, 16.78) | 0.72285 |
| Yes | 12.50% (2/16) | |||
| Triple negative | No | 15.91% (14/88) | 1.13 (0.12, 55.90) | 1 |
| Yes | 14.29% (1/7) | |||
| Family ovarian cancer | No | 16.25% (13/80) | 1.26 (0.24, 12.80) | 1 |
| Yes | 13.33% (2/15) | |||
| Stage | 0 | 0.00% (0/10) | 0.12418 | |
| I | 13.79% (4/29) | |||
| II | 13.16% (5/38) | |||
| III | 37.5% (6/16) | |||
| IV | 0.00% (0/1) |
| Genes | Patients with Luminal BC (n = 57) | Patients with HER2 Positive BC (n = 16) | Patients with Triple Negative BC (n = 7) | |||
|---|---|---|---|---|---|---|
| No. | % (95% CI) | No. | % (95% CI) | No. | % (95% CI) | |
| Any deleterious mutation | 9 | 9.5 (3.5–15.3) | 2 | 2.1 (0–4.9) | 1 | 1.1 (0.1–3.1) |
| Genes related to breast cancer | ||||||
| BRCA1 | 1 | 1.1 (0.1–3.1) | 0 | 1 | 1.1 (0.1–3.1) | |
| ATM | 5 | 5.3 (0.7–9.7) | 0 | 0 | ||
| CHEK2 | 3 | 3.2 (0.3–6.6) | 1 | 1.1 (0.1–3.1) | 0 | |
| TP53 | 1 | 1.1 (0.1–3.1) | 1 | 1.1 (0.1–3.1) | 0 | |
| Genes not clearly related to breast cancer | ||||||
| MSH2 | 1 | 1.1 (0.1–3.1) | 0 | 0 | ||
| BRIP1 | 1 | 1.1 (0.1–3.1) | ||||
| Candidate genes | 0 | 0 | ||||
| CASP8 | 1 | 1.1 (0.1–3.1) | 0 | 0 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fonfria, M.; de Juan Jiménez, I.; Tena, I.; Chirivella, I.; Richart-Aznar, P.; Segura, A.; Sánchez-Heras, A.B.; Martinez-Dueñas, E. Prevalence and Clinicopathological Characteristics of Moderate and High-Penetrance Genes in Non-BRCA1/2 Breast Cancer High-Risk Spanish Families. J. Pers. Med. 2021, 11, 548. https://doi.org/10.3390/jpm11060548
Fonfria M, de Juan Jiménez I, Tena I, Chirivella I, Richart-Aznar P, Segura A, Sánchez-Heras AB, Martinez-Dueñas E. Prevalence and Clinicopathological Characteristics of Moderate and High-Penetrance Genes in Non-BRCA1/2 Breast Cancer High-Risk Spanish Families. Journal of Personalized Medicine. 2021; 11(6):548. https://doi.org/10.3390/jpm11060548
Chicago/Turabian StyleFonfria, Maria, Inmaculada de Juan Jiménez, Isabel Tena, Isabel Chirivella, Paula Richart-Aznar, Angel Segura, Ana Beatriz Sánchez-Heras, and Eduardo Martinez-Dueñas. 2021. "Prevalence and Clinicopathological Characteristics of Moderate and High-Penetrance Genes in Non-BRCA1/2 Breast Cancer High-Risk Spanish Families" Journal of Personalized Medicine 11, no. 6: 548. https://doi.org/10.3390/jpm11060548
APA StyleFonfria, M., de Juan Jiménez, I., Tena, I., Chirivella, I., Richart-Aznar, P., Segura, A., Sánchez-Heras, A. B., & Martinez-Dueñas, E. (2021). Prevalence and Clinicopathological Characteristics of Moderate and High-Penetrance Genes in Non-BRCA1/2 Breast Cancer High-Risk Spanish Families. Journal of Personalized Medicine, 11(6), 548. https://doi.org/10.3390/jpm11060548






