The Potential Role of Sildenafil in Cancer Management through EPR Augmentation
Abstract
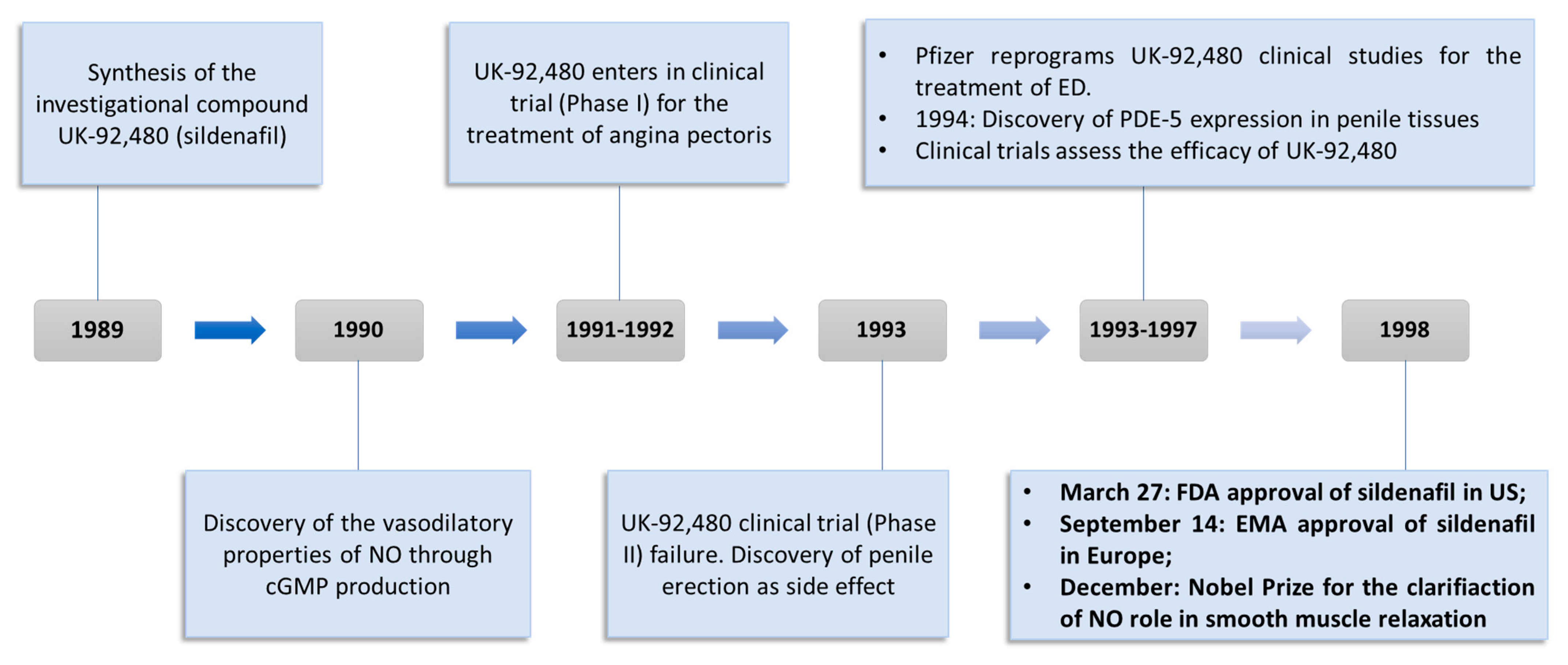
:1. Introduction
2. Drug Repurposing Approach for the Identification of New Therapeutic Application
3. In Vitro and In Vivo Applications of Sildenafil in Cancer Treatment
4. The Role of Sildenafil in Circumventing Anticancer Drug Resistance
5. Sildenafil and Anticancer Drug Delivery through EPR Augmentation
6. Clinical Studies
7. Conclusions and Future Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Utiger, R.D. A Pill for Impotence. N. Engl. J. Med. 1998, 338, 1458–1459. [Google Scholar] [CrossRef] [PubMed]
- Terrett, N.K.; Bell, A.S.; Brown, D.; Ellis, P. Sildenafil (Viagra(TM)), a potent and selective inhibitor of type 5 CGMP phosphodiesterase with utility for the treatment of male erectile dysfunction. Bioorg. Med. Chem. Lett. 1996, 6, 1819–1824. [Google Scholar] [CrossRef]
- Francis, S.H.; Blount, M.A.; Corbin, J.D. Mammalian cyclic nucleotide phosphodiesterases: Molecular mechanisms and physiological functions. Physiol. Rev. 2011, 91, 651–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rotella, D.P. Phosphodiesterase 5 inhibitors: Current status and potential applications. Nat. Rev. Drug Discov. 2002, 1, 674–682. [Google Scholar] [CrossRef] [PubMed]
- Beavo, J.A. Cyclic nucleotide phosphodiesterases: Functional implications of multiple isoforms. Physiol. Rev. 1995, 75, 725–748. [Google Scholar] [CrossRef] [PubMed]
- Andersson, K.E. PDE5 inhibitors—Pharmacology and clinical applications 20 years after sildenafil discovery. Br. J. Pharmacol. 2018, 175, 2554–2565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blount, M.A.; Beasley, A.; Zoraghi, R.; Sekhar, K.R.; Bessay, E.P.; Francis, S.H.; Corbin, J.D. Binding of tritiated sildenafil, tadalafil, or vardenafil to the phosphodiesterase-5 catalytic site displays potency, specificity, heterogeneity, and cGMP stimulation. Mol. Pharmacol. 2004, 66, 144–152. [Google Scholar] [CrossRef] [Green Version]
- Corbin, J.D.; Francis, S.H. Cyclic GMP phosphodiesterase-5: Target of sildenafil. J. Biol. Chem. 1999, 274, 13729–13732. [Google Scholar] [CrossRef] [Green Version]
- Corbin, J.D.; Turko, I.V.; Beasley, A.; Francis, S.H. Phosphorylation of phosphodiesterase-5 by cyclic nucleotide-dependent protein kinase alters its catalytic and allosteric cGMP-binding activities. Eur. J. Biochem. 2000, 267, 2760–2767. [Google Scholar] [CrossRef] [Green Version]
- Essayan, D.M. Cyclic nucleotide phosphodiesterases. J. Allergy Clin. Immunol. 2001, 108, 671–680. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, I.; Burnett, A.L.; Rosen, R.C.; Park, P.W.; Stecher, V.J. The Serendipitous Story of Sildenafil: An Unexpected Oral Therapy for Erectile Dysfunction. Sex. Med. Rev. 2019, 7, 115–128. [Google Scholar] [CrossRef]
- Ghofrani, H.A.; Osterloh, I.H.; Grimminger, F. Sildenafil: From angina to erectile dysfunction to pulmonary hypertension and beyond. Nat. Rev. Drug Discov. 2006, 5, 689–702. [Google Scholar] [CrossRef]
- Carson, C.C.; Lue, T.F. Phosphodiesterase type 5 inhibitors for erectile dysfunction. BJU Int. 2005, 96, 257–280. [Google Scholar] [CrossRef]
- Barbaro, G.; Scozzafava, A.; Mastrolorenzo, A.; Supuran, C. Highly Active Antiretroviral Therapy: Current State of the Art, New Agents and Their Pharmacological Interactions Useful for Improving Therapeutic Outcome. Curr. Pharm. Des. 2005, 11, 1805–1843. [Google Scholar] [CrossRef]
- Yafi, F.A.; Sharlip, I.D.; Becher, E.F. Update on the Safety of Phosphodiesterase Type 5 Inhibitors for the Treatment of Erectile Dysfunction. Sex. Med. Rev. 2018, 6, 242–252. [Google Scholar] [CrossRef]
- Laties, A.M.; Fraunfelder, F.T.; Flach, A.J.; Tasman, W. Ocular safety of Viagra, (sildenafil citrate). Trans. Am. Ophthalmol. Soc. 1999, 97, 115–128. [Google Scholar]
- Wang, H.; Liu, Y.; Huai, Q.; Cai, J.; Zoraghi, R.; Francis, S.H.; Corbin, J.D.; Robinson, H.; Xin, Z.; Lin, G.; et al. Multiple conformations of phosphodiesterase-5: Implications for enzyme function and drug development. J. Biol. Chem. 2006, 281, 21469–21479. [Google Scholar] [CrossRef] [Green Version]
- Sung, B.J.; Hwang, K.Y.; Jeon, Y.H.; Lee, J.I.; Heo, Y.S.; Kim, J.H.; Moon, J.; Yoon, J.M.; Hyun, Y.L.; Kim, E.; et al. Structure of the catalytic domain of human phosphodiesterase 5 with bound drug molecules. Nature 2003, 425, 98–102. [Google Scholar] [CrossRef]
- Supuran, C.; Mastrolorenzo, A.; Barbaro, G.; Scozzafava, A. Phosphodiesterase 5 Inhibitors—Drug Design and Differentiation Based on Selectivity, Pharmacokinetic and Efficacy Profiles. Curr. Pharm. Des. 2006, 12, 3459–3465. [Google Scholar] [CrossRef]
- Salentin, S.; Schreiber, S.; Haupt, V.J.; Adasme, M.F.; Schroeder, M. PLIP: Fully automated protein-ligand interaction profiler. Nucleic Acids Res. 2015, 43, W443–W447. [Google Scholar] [CrossRef]
- Ban, T.A. The role of serendipity in drug discovery. Dialogues Clin. Neurosci. 2006, 8, 335–344. [Google Scholar] [CrossRef]
- Deckers, J.W. Classification of myocardial infarction and unstable angina: A re-assessment. Int. J. Cardiol. 2013, 167, 2387–2390. [Google Scholar] [CrossRef]
- Jackson, G.; Benjamin, N.; Jackson, N.; Allen, M.J. Effects of sildenafil citrate on human hemodynamics. Am. J. Cardiol. 1999, 83, 13–20. [Google Scholar] [CrossRef]
- Boolell, M.; Allen, M.J.; Ballard, S.A.; Gepi-Attee, S.; Muirhead, G.J.; Naylor, A.M.; Osterloh, I.H.; Gingell, C. Sildenafil: An orally active type 5 cyclic GMP-specific phosphodiesterase inhibitor for the treatment of penile erectile dysfunction. Int. J. Impot. Res. 1996, 8, 47–52. [Google Scholar]
- Wallis, R.M.; Corbin, J.D.; Francis, S.H.; Ellis, P. Tissue distribution of phosphodiesterase families and the effects of sildenafil on tissue cyclic nucleotides, platelet function, and the contractile responses of trabeculae carneae and aortic rings in vitro. Am. J. Cardiol. 1999, 83, 3–12. [Google Scholar] [CrossRef]
- Ignarro, L.J.; Bush, P.A.; Buga, G.M.; Wood, K.S.; Fukuto, J.M.; Rajfer, J. Nitric oxide and cyclic GMP formation upon electrical field stimulation cause relaxation of corpus cavernosum smooth muscle. Biochem. Biophys. Res. Commun. 1990, 170, 843–850. [Google Scholar] [CrossRef]
- Perry, M.J.; Higgs, G.A. Chemotherapeutic potential of phosphodiesterase inhibitors. Curr. Opin. Chem. Biol. 1998, 2, 472–481. [Google Scholar] [CrossRef]
- Hatzimouratidis, K.; Salonia, A.; Adaikan, G.; Buvat, J.; Carrier, S.; El-Meliegy, A.; McCullough, A.; Torres, L.O.; Khera, M. Pharmacotherapy for Erectile Dysfunction: Recommendations From the Fourth International Consultation for Sexual Medicine (ICSM 2015). J. Sex. Med. 2016, 13, 465–488. [Google Scholar] [CrossRef]
- Bermejo, J.; Yotti, R.; García-Orta, R.; Sánchez-Fernández, P.L.; Castaño, M.; Segovia-Cubero, J.; Escribano-Subías, P.; San Román, J.A.; Borrás, X.; Alonso-Gómez, A.; et al. Sildenafil for improving outcomes in patients with corrected valvular heart disease and persistent pulmonary hypertension: A multicenter, double-blind, randomized clinical trial. Eur. Heart J. 2018, 39, 1255–1264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galiè, N.; Ghofrani, H.A.; Torbicki, A.; Barst, R.J.; Rubin, L.J.; Badesch, D.; Fleming, T.; Parpia, T.; Burgess, G.; Branzi, A.; et al. Sildenafil Citrate Therapy for Pulmonary Arterial Hypertension. N. Engl. J. Med. 2005, 353, 2148–2157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolb, M.; Raghu, G.; Wells, A.U.; Behr, J.; Richeldi, L.; Schinzel, B.; Quaresma, M.; Stowasser, S.; Martinez, F.J. Nintedanib plus Sildenafil in Patients with Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2018, 379, 1722–1731. [Google Scholar] [CrossRef] [PubMed]
- Sastry, B.K.S.; Narasimhan, C.; Reddy, N.K.; Raju, B.S. Clinical efficacy of sildenafil in primary pulmonary hypertension: A randomized, placebo-controlled, double-blind, crossover study. J. Am. Coll. Cardiol. 2004, 43, 1149–1153. [Google Scholar] [CrossRef] [PubMed]
- Pushpakom, S.; Iorio, F.; Eyers, P.A.; Escott, K.J.; Hopper, S.; Wells, A.; Doig, A.; Guilliams, T.; Latimer, J.; McNamee, C.; et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug Discov. 2018, 18, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Marwick, C. AZT (zidovudine) just a step away from FDA approval for AIDS therapy. JAMA 1987, 257, 1281–1282. [Google Scholar] [CrossRef]
- Stewart, A.K. How thalidomide works against cancer. Science 2014, 343, 256–257. [Google Scholar] [CrossRef] [Green Version]
- Rezaee, M.E.; Ward, C.E.; Brandes, E.R.; Munarriz, R.M.; Gross, M.S. A Review of Economic Evaluations of Erectile Dysfunction Therapies. Sex. Med. Rev. 2020, 8, 497–503. [Google Scholar] [CrossRef]
- Sanchez, L.S.; De La Monte, S.M.; Filippov, G.; Jones, R.C.; Zapol, W.M.; Bloch, K.D. Cyclic-GMP-binding, cyclic-GMP-specific phosphodiesterase (PDE5) gene expression is regulated during rat pulmonary development. Pediatr. Res. 1998, 43, 163–168. [Google Scholar] [CrossRef] [Green Version]
- Bhogal, S.; Khraisha, O.; Al Madani, M.; Treece, J.; Baumrucker, S.J.; Paul, T.K. Sildenafil for Pulmonary Arterial Hypertension. Am. J. Ther. 2019, 26, e520–e526. [Google Scholar] [CrossRef] [Green Version]
- Mei, X.L.; Yang, Y.; Zhang, Y.J.; Li, Y.; Zhao, J.M.; Qiu, J.G.; Zhang, W.J.; Jiang, Q.W.; Xue, Y.Q.; Zheng, D.W.; et al. Sildenafil inhibits the growth of human colorectal cancer in vitro and in vivo. Am. J. Cancer Res. 2015, 5, 3311–3324. [Google Scholar]
- Keats, T.; Rosengren, R.J.; Ashton, J.C. The Rationale for Repurposing Sildenafil for Lung Cancer Treatment. Anticancer Agents Med. Chem. 2018, 18, 367–374. [Google Scholar] [CrossRef]
- Das, A.; Durrant, D.; Mitchell, C.; Mayton, E.; Hoke, N.N.; Salloum, F.N.; Park, M.A.; Qureshi, I.; Lee, R.; Dent, P.; et al. Sildenafil increases chemotherapeutic efficacy of doxorubicin in prostate cancer and ameliorates cardiac dysfunction. Proc. Natl. Acad. Sci. USA 2010, 107, 18202–18207. [Google Scholar] [CrossRef] [Green Version]
- Das, A.; Durrant, D.; Mitchell, C.; Dent, P.; Batra, S.K.; Kukreja, R.C. Sildenafil (Viagra) sensitizes prostate cancer cells to doxorubicin-mediated apoptosis through CD95. Oncotarget 2016, 7, 4399–4413. [Google Scholar] [CrossRef]
- Greish, K.; Fateel, M.; Abdelghany, S.; Rachel, N.; Alimoradi, H.; Bakhiet, M.; Alsaie, A. Sildenafil citrate improves the delivery and anticancer activity of doxorubicin formulations in a mouse model of breast cancer. J. Drug Target. 2018, 26, 610–615. [Google Scholar] [CrossRef]
- El-Naa, M.M.; Othman, M.; Younes, S. Sildenafil potentiates the antitumor activity of cisplatin by induction of apoptosis and inhibition of proliferation and angiogenesis. Drug Des. Dev. Ther. 2016, 10, 3661–3672. [Google Scholar] [CrossRef] [Green Version]
- Hassanvand, F.; Mohammadi, T.; Ayoubzadeh, N.; Tavakoli, A.; Hassanzadeh, N.; Sanikhani, N.S.; Azimi, A.I.; Mirzaei, H.R.; Khodamoradi, M.; Goudarzi, K.A.; et al. Sildenafil enhances cisplatin-induced apoptosis in human breast adenocarcinoma cells. J. Cancer Res. Ther. 2020, 16, 1412–1418. [Google Scholar] [CrossRef]
- Hsu, J.-L.; Leu, W.-J.; Hsu, L.-C.; Ho, C.-H.; Liu, S.-P.; Guh, J.-H. Phosphodiesterase Type 5 Inhibitors Synergize Vincristine in Killing Castration-Resistant Prostate Cancer Through Amplifying Mitotic Arrest Signaling. Front. Oncol. 2020, 10, 1274. [Google Scholar] [CrossRef]
- Roberts, J.L.; Poklepovic, A.; Booth, L. Curcumin interacts with sildenafil to kill GI tumor cells via endoplasmic reticulum stress and reactive oxygen/nitrogen species. Oncotarget 2017, 8, 99451–99469. [Google Scholar] [CrossRef] [Green Version]
- Dent, P.; Booth, L.; Roberts, J.L.; Poklepovic, A.; Hancock, J.F. (Curcumin + sildenafil) enhances the efficacy of 5FU and anti-PD1 therapies in vivo. J. Cell. Physiol. 2020, 235, 6862–6874. [Google Scholar] [CrossRef]
- Morales, J.C.; Li, L.; Fattah, F.J.; Dong, Y.; Bey, E.A.; Patel, M.; Gao, J.; Boothman, D.A. Review of poly (ADP-ribose) polymerase (PARP) mechanisms of action and rationale for targeting in cancer and other diseases. Crit. Rev. Eukaryot. Gene Expr. 2014, 24, 15–28. [Google Scholar] [CrossRef] [Green Version]
- Muniyan, S.; Rachagani, S.; Parte, S.; Halder, S.; Seshacharyulu, P.; Kshirsagar, P.; Siddiqui, J.A.; Vengoji, R.; Rauth, S.; Islam, R.; et al. Sildenafil potentiates the therapeutic efficacy of docetaxel in advanced prostate cancer by stimulating NO-cGMP signaling. Clin. Cancer Res. 2020, 26. [Google Scholar] [CrossRef]
- Chen, J.J.; Sun, Y.L.; Tiwari, A.K.; Xiao, Z.J.; Sodani, K.; Yang, D.H.; Vispute, S.G.; Jiang, W.Q.; Chen, S.D.; Chen, Z.S. PDE5 inhibitors, sildenafil and vardenafil, reverse multidrug resistance by inhibiting the efflux function of multidrug resistance protein 7 (ATP-binding Cassette C10) transporter. Cancer Sci. 2012, 103, 1531–1537. [Google Scholar] [CrossRef] [PubMed]
- Marques, J.G.; Gaspar, V.M.; Markl, D.; Costa, E.C.; Gallardo, E.; Correia, I.J. Co-delivery of Sildenafil (Viagra(®)) and Crizotinib for synergistic and improved anti-tumoral therapy. Pharm. Res. 2014, 31, 2516–2528. [Google Scholar] [CrossRef] [PubMed]
- Hajipour, H.; Ghorbani, M.; Kahroba, H.; Mahmoodzadeh, F.; Emameh, R.Z.; Taheri, R.A. Arginyl-glycyl-aspartic acid (RGD) containing nanostructured lipid carrier co-loaded with doxorubicin and sildenafil citrate enhanced anti-cancer effects and overcomes drug resistance. Process. Biochem. 2019, 84, 172–179. [Google Scholar] [CrossRef]
- Ji, L.; Li, H.; Gao, P.; Shang, G.; Zhang, D.D.; Zhang, N.; Jiang, T. Nrf2 Pathway Regulates Multidrug-Resistance-Associated Protein 1 in Small Cell Lung Cancer. PLoS ONE 2013, 8, e63404. [Google Scholar] [CrossRef] [Green Version]
- Mansoori, B.; Mohammadi, A.; Davudian, S.; Shirjang, S.; Baradaran, B. The Different Mechanisms of Cancer Drug Resistance: A Brief Review. Adv. Pharm. Bull. 2017, 7, 339–348. [Google Scholar] [CrossRef]
- Di Nicolantonio, F.; Mercer, S.J.; Knight, L.A.; Gabriel, F.G.; Whitehouse, P.A.; Sharma, S.; Fernando, A.; Glaysher, S.; Di Palma, S.; Johnson, P.; et al. Cancer cell adaptation to chemotherapy. BMC Cancer 2005, 5, 78. [Google Scholar] [CrossRef] [Green Version]
- Vasiliou, V.; Vasiliou, K.; Nebert, D.W. Human ATP-binding cassette (ABC) transporter family. Hum. Genom. 2009, 3, 281–290. [Google Scholar] [CrossRef]
- Cree, I.A.; Knight, L.; di Nicolantonio, F.; Sharma, S.; Gulliford, T. Chemosensitization of solid tumor cells by alteration of their susceptibility to apoptosis. Curr. Opin. Investig. Drugs 2002, 3, 641–647. [Google Scholar]
- Tewari, K.S.; Eskander, R.N.; Monk, B.J. Development of Olaparib for BRCA-Deficient Recurrent Epithelial Ovarian Cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2015, 21, 3829–3835. [Google Scholar] [CrossRef] [Green Version]
- Gottesman, M.M.; Ambudkar, S. V Overview: ABC transporters and human disease. J. Bioenerg. Biomembr. 2001, 33, 453–458. [Google Scholar] [CrossRef]
- Shi, Z.; Tiwari, A.K.; Shukla, S.; Robey, R.W.; Singh, S.; Kim, I.-W.; Bates, S.E.; Peng, X.; Abraham, I.; Ambudkar, S.V.; et al. Sildenafil reverses ABCB1- and ABCG2-mediated chemotherapeutic drug resistance. Cancer Res. 2011, 71, 3029–3041. [Google Scholar] [CrossRef] [Green Version]
- Shi, Z.; Tiwari, A.K.; Patel, A.S.; Fu, L.W.; Chen, Z.S. Roles of sildenafil in enhancing drug sensitivity in cancer. Cancer Res. 2011, 71, 3735–3738. [Google Scholar] [CrossRef] [Green Version]
- Preston, I.R.; Klinger, J.R.; Houtches, J.; Nelson, D.; Farber, H.W.; Hill, N.S. Acute and chronic effects of sildenafil in patients with pulmonary arterial hypertension. Respir. Med. 2005, 99, 1501–1510. [Google Scholar] [CrossRef] [Green Version]
- Yuan, F.; Salehi, H.A.; Boucher, Y.; Vasthare, U.S.; Tuma, R.F.; Jain, R.K. Vascular permeability and microcirculation of gliomas and mammary carcinomas transplanted in rat and mouse cranial windows. Cancer Res. 1994, 54, 4564–4568. [Google Scholar]
- Folkman, J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat. Med. 1995, 1, 27–31. [Google Scholar] [CrossRef]
- Hashizume, H.; Baluk, P.; Morikawa, S.; McLean, J.W.; Thurston, G.; Roberge, S.; Jain, R.K.; McDonald, D.M. Openings between defective endothelial cells explain tumor vessel leakiness. Am. J. Pathol. 2000, 156, 1363–1380. [Google Scholar] [CrossRef] [Green Version]
- Matsumura, Y.; Maeda, H. A new concept for macromolecular therapeutics in cancer chemotherapy: Mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986, 46, 6387–6392. [Google Scholar]
- Seymour, L.W.; Miyamoto, Y.; Maeda, H.; Brereton, M.; Strohalm, J.; Ulbrich, K.; Duncan, R. Influence of molecular weight on passive tumour accumulation of a soluble macromolecular drug carrier. Eur. J. Cancer 1995, 31A, 766–770. [Google Scholar] [CrossRef]
- Greish, K.; Sawa, T.; Fang, J.; Akaike, T.; Maeda, H. SMA-doxorubicin, a new polymeric micellar drug for effective targeting to solid tumours. J. Control. Release 2004, 97, 219–230. [Google Scholar] [CrossRef]
- Nagamitsu, A.; Inuzuka, T.; Greish, K.; Maeda, H. SMANCS dynamic therapy for various advanced solid tumors and promising clinical effects. Drug Deliv. Syst. 2007, 22, 510–521. [Google Scholar] [CrossRef] [Green Version]
- Black, K.L.; Yin, D.; Ong, J.M.; Hu, J.; Konda, B.M.; Wang, X.; Ko, M.K.; Bayan, J.-A.; Sacapano, M.R.; Espinoza, A.; et al. PDE5 inhibitors enhance tumor permeability and efficacy of chemotherapy in a rat brain tumor model. Brain Res. 2008, 1230, 290–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, P.; Zhang, Y.; Ding, X.; Xiao, C.; Chen, X. Enhanced nanoparticle accumulation by tumor-acidity-activatable release of sildenafil to induce vasodilation. Biomater. Sci. 2020, 8, 3052–3062. [Google Scholar] [CrossRef] [PubMed]
- Sheffield-Moore, M.; Wiktorowicz, J.E.; Soman, K.V.; Danesi, C.P.; Kinsky, M.P.; Dillon, E.L.; Randolph, K.M.; Casperson, S.L.; Gore, D.C.; Horstman, A.M.; et al. Sildenafil increases muscle protein synthesis and reduces muscle fatigue. Clin. Transl. Sci. 2013, 6, 463–468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treon, S.P.; Tournilhac, O.; Branagan, A.R.; Hunter, Z.; Xu, L.; Hatjiharissi, E.; Santos, D.D. Clinical Responses to Sildenafil in Waldenstrom’s Macroglobulinemia. Clin. Lymphoma 2004, 5, 205–207. [Google Scholar] [CrossRef]
- Danial, C.; Tichy, A.L.; Tariq, U.; Swetman, G.L.; Khuu, P.; Leung, T.H.; Benjamin, L.; Teng, J.; Vasanawala, S.S.; Lane, A.T. An open-label study to evaluate sildenafil for the treatment of lymphatic malformations. J. Am. Acad. Dermatol. 2014, 70, 1050–1057. [Google Scholar] [CrossRef] [Green Version]
- Poklepovic, A.; Qu, Y.; Dickinson, M.; Kontos, M.C.; Kmieciak, M.; Schultz, E.; Bandopadhyay, D.; Deng, X.; Kukreja, R.C. Randomized study of doxorubicin-based chemotherapy regimens, with and without sildenafil, with analysis of intermediate cardiac markers. CardioOncology 2018, 4. [Google Scholar] [CrossRef]
- Booth, L.; Roberts, J.L.; Rais, R.; Cutler, R.E.J.; Diala, I.; Lalani, A.S.; Hancock, J.F.; Poklepovic, A.; Dent, P. Neratinib augments the lethality of [regorafenib + sildenafil]. J. Cell. Physiol. 2019, 234, 4874–4887. [Google Scholar] [CrossRef]



| Cancer | Type of Study | Tumor Model | Therapy | Therapeutic Outcome | Ref. |
|---|---|---|---|---|---|
| Prostate Cancer | In vitro | PC-3 and DU145 prostate cancer cells | Sildenafil (10 μM) | No significant changes in % Cell death compared to control | [41] |
| DOX (1.5 μM with PC-3 and 0.5 μM with DU145) | 7.52% and 45.01% cell death in PC-3 and DU145 cells, respectively. | ||||
| DOX (1.5 μM with PC-3 and 0.5 μM with DU145) + Sildenafil (10 μM) | 18.71% and 56.82% cell death in PC-3 and DU145 cells, respectively. | ||||
| In vivo | Athymic male BALB/cAnNCr-nu/nu mice injected with PC-3 cells and 50-μL matrigel matrices | DOX (1.5 mg/kg) | Tumor weight/Body weight ratio = 0.015 | ||
| Intraperitoneal DOX (1.5 mg/kg) + Sildenafil (5 mg/kg) OR intraperitoneal DOX (3 mg/kg) + oral Sildenafil (10 mg/kg) | Tumor weight/Body weight ratio = 0.010 | ||||
| Breast Cancer | In vitro | 4T1 mammary carcinoma cells | DOX (1μM) | 50% cell death | [43] |
| Sildenafil (10,30,100μM) | No significant changes compared to control | ||||
| DOX (1μM) + Sildenafil (1μM) | 72.2% cell death | ||||
| DOX (1μM) + Sildenafil (30μM) | 91.9% cell death | ||||
| DOX (1μM) + Sildenafil (100μM) | 97.6% cell death | ||||
| In vivo | Female Balb/c mice injected with 4T1 mammary carcinoma cells | DOX (5 mg/kg) | Tumor volume = 570% | ||
| Sildenafil (1 mg/kg) | Tumor volume = 400% | ||||
| DOX (5 mg/kg) + Sildenafil (1 mg/kg) | Tumor volume = 121.3% | ||||
| Breast Cancer | In vitro | MCF-7 breast cancer cells | Sildenafil | IC50 = 14 µg/mL | [44] |
| Cisplatin | IC50 = 4.43 µg/mL | ||||
| Sildenafil + Cisplatin | IC50 = 3.98 µg/mL | ||||
| In vivo | Swiss albino female mice injected with Ehrlich ascites carcinoma (EAC) cells | Sildenafil (5 mg/kg) | 30.4% decrease in tumor volume | ||
| Cisplatin (7.5 mg/kg) | 58.8% decrease in tumor volume | ||||
| Sildenafil (5 mg/kg) + Cisplatin (7.5 mg/kg) | 79% decrease in tumor volume | ||||
| Colorectal Cancer | In vitro | HT-29, SW480, SW620, HCT116 and SW1116 colorectal cancer cells | Sildenafil | IC50 (72hrs) = 190.91 μM in HT-29 217.27 μM SW480 206.68 μM SW620 246.20 μM HCT116 271.22 μM SW1116 | [39] |
| In vivo | Balb/c nude mice injected with SW480 or HCT116 colorectal cancer cells | Sildenafil (50 mg/kg) and (150 mg/kg) | In SW480, 40.1% and 57.8% tumor inhibition with 50 mg/kg and 150 mg/kg, respectively. | ||
| In HCT116, 13.3% and 61.4% tumor inhibition with 50 mg/kg and 150 mg/kg, respectively. | |||||
| Prostate Cancer | In vivo | Nude mice were injected with PC-3 prostate cancer cells | Sildenafil (10 mg/kg) | Tumor weight = 969.9 ± 92.2 mg | [46] |
| Vincristine (0.5 mg/kg) | Tumor weight = 623.5 ± 132.2 mg | ||||
| Sildenafil (10 mg/kg) + Vincristine (0.5 mg/kg) | Tumor weight = 207.6 ± 36.7 mg | ||||
| Breast Cancer | In vitro | MCF-7 Breast cancer cells | Sildenafil | No significant changes in % cell viability compared to control | [52] |
| Crizotinib | IC50 = 34.19 and 22% cell viability | ||||
| Crizotinib + Sildenafil | IC50 = 3.34 and 10% cell viability | ||||
| Blank PEG-PLA micelles | No significant changes in % cell viability compared to control | ||||
| Crizotinib loaded PEG-PLA micelles | 14% cell viability | ||||
| Crizotinib (55.25 μM)/Sildenafil (40.33 μM)- coloaded PEG-PLA micelles | 4% cell viability | ||||
| Lung Cancer | In vitro | A549 human lung carcinoma cells | DOX | 29.87% cell death | [53] |
| DOX + Sildenafil | 34.69% cell death | ||||
| DOX/Sildenafil-coloaded NLC | 38.37% cell death | ||||
| DOX/Sildenafil-coloaded NLC-RGD | 44.32% cell death |
| Types of Cancer | Treatment | Objective | Stage |
|---|---|---|---|
| Pancreatic Cancer | Sildenafil | Management of fatigue in cancer patient undergoing chemotherapy | Phase I |
| Non-small Cell Lung Cancer | Sildenafil, Paclitaxel, Carboplatin | Improvement in distribution and efficacy of cytotoxic anticancer agents | Phase II, III |
| Prostate Cancer | Sildenafil | Management of ED during and after radiotherapy with or without hormone Therapy | Phase III |
| Sildenafil, Alprostadil | Management of ED post-operatively in patients undergoing nerve-sparing robotic-assisted radical prostatectomy | Phase III | |
| Sildenafil | Investigate the effect of dosage regimen on ED in patients after nerve-sparing laparoscopic radical prostatectomy | Not applicable | |
| Sildenafil, Hyperbaric oxygen therapy | Management of ED in patients after nerve-sparing radical retropubic prostatectomy | Phase IV | |
| Solid Tumor | Regorafenib Sildenafil | Investigation of the antitumor effects of the regorafenib and sildenafil combination, the pre-treatment expression of phosphodiesterase type 5 (PDE5) in tumor samples, and the impact of sildenafil on the pharmacokinetics of regorafenib | Phase I |
| Kidney Tumor | Sildenafil | Improving Postoperative Kidney Function in Patients With Kidney Cancer undergoing Robotic Partial Nephrectomy | Phase I |
| Colorectal Cancer | Sildenafil Vacuum erection device (VED) | Management of ED After Laparoscopic Resection | Phase IV |
| Breast Cancer | Sildenafil Doxorubicin | Improving antitumor effects of DOX and protection from cardiac toxicity | Phase I |
| Brain Cancer and Glioblastoma | Sildenafil Sorafenib Tosylate Valproic Acid | Increase the concentration of anticancer drug in the brain and stop the growth of tumor cells by blocking BCG2 drug efflux pump in the blood–brain barrier | Phase II |
| Waldenstrom Macroglobulinemia | Sildenafil | Treatment by blocking the function of several proteins necessary to the survival of cancer cells | Phase II |
| Myelodysplastic Syndrome (MDS) | Nivolumab Cytarabine Sildenafil | Studying the pathogenesis and resistance of myelodysplastic syndrome using combination therapy | Phase I, II |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haider, M.; Elsherbeny, A.; Pittalà, V.; Fallica, A.N.; Alghamdi, M.A.; Greish, K. The Potential Role of Sildenafil in Cancer Management through EPR Augmentation. J. Pers. Med. 2021, 11, 585. https://doi.org/10.3390/jpm11060585
Haider M, Elsherbeny A, Pittalà V, Fallica AN, Alghamdi MA, Greish K. The Potential Role of Sildenafil in Cancer Management through EPR Augmentation. Journal of Personalized Medicine. 2021; 11(6):585. https://doi.org/10.3390/jpm11060585
Chicago/Turabian StyleHaider, Mohamed, Amr Elsherbeny, Valeria Pittalà, Antonino N. Fallica, Maha Ali Alghamdi, and Khaled Greish. 2021. "The Potential Role of Sildenafil in Cancer Management through EPR Augmentation" Journal of Personalized Medicine 11, no. 6: 585. https://doi.org/10.3390/jpm11060585
APA StyleHaider, M., Elsherbeny, A., Pittalà, V., Fallica, A. N., Alghamdi, M. A., & Greish, K. (2021). The Potential Role of Sildenafil in Cancer Management through EPR Augmentation. Journal of Personalized Medicine, 11(6), 585. https://doi.org/10.3390/jpm11060585









