Patient-Specific Implants for Pelvic Tumor Resections
Abstract
:1. Introduction
- (1)
- What where complication rates and revision free survivals following reconstruction with pelvic custom-made implants?
- (2)
- What was the oncological survival after extensive pelvic tumor resection?
- (3)
- What were functional outcomes and physical limitations?
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Surgical Approach and Extend of Reconstruction
2.4. Primary and Secondary Study Objectives
2.5. Ethical Approval
2.6. Statistical Analysis
3. Results
3.1. Complications Following Pelvic Reconstruction
3.2. Oncological Survival after Extensive Pelvic Tumor Resection and Reconstruction
3.3. Functional Outcomes and Physical Limitations
4. Discussion
4.1. Limitations
4.2. Complications after Extensive Pelvic Reconstructions
4.3. Overall Oncological Survival after Resection of Extensive Pelvic Tumors
4.4. Functional Results of Patients Mobilized with Custom-Made Prostheses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pant, R.; Moreau, P.; Ilyas, I.; Paramasivan, O.N.; Younge, D. Pelvic limb-salvage surgery for malignant tumors. Int. Orthop. 2001, 24, 311. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Min, L.; Lu, M.; Zhang, Y.; Wang, Y.; Luo, Y.; Zhou, Y.; Duan, H.; Tu, C. What are the Complications of Three-dimensionally Printed, Custom-made, Integrative Hemipelvic Endoprostheses in Patients with Primary Malignancies Involving the Acetabulum, and What is the Function of These Patients? Clin. Orthop. Relat. Res. 2020, 478, 2487. [Google Scholar] [CrossRef]
- Wilson, R.J.; Freeman, T.H., Jr.; Halpern, J.L.; Schwartz, H.S.; Holt, G.E. Surgical Outcomes After Limb-Sparing Resection and Reconstruction for Pelvic Sarcoma: A Systematic Review. JBJS Rev. 2018, 6, e10. [Google Scholar] [CrossRef] [PubMed]
- Enneking, W.F.; Dunham, W.K. Resection and reconstruction for primary neoplasms involving the innominate bone. J. Bone Jt. Surg. Am. 1978, 60, 731. [Google Scholar] [CrossRef]
- Campanacci, D.; Chacon, S.; Mondanelli, N.; Beltrami, G.; Scoccianti, G.; Caff, G.; Frenos, F.; Capanna, R. Pelvic massive allograft reconstruction after bone tumour resection. Int. Orthop. 2012, 36, 2529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gebert, C.; Wessling, M.; Hoffmann, C.; Roedl, R.; Winkelmann, W.; Gosheger, G.; Hardes, J. Hip transposition as a limb salvage procedure following the resection of periacetabular tumors. J. Surg. Oncol. 2011, 103, 269. [Google Scholar] [CrossRef]
- Donati, D.; Di Bella, C.; Frisoni, T.; Cevolani, L.; DeGroot, H. Alloprosthetic composite is a suitable reconstruction after periacetabular tumor resection. Clin. Orthop. Relat. Res. 2011, 469, 1450. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Min, L.; Lu, M.; Zhang, Y.; Wang, Y.; Luo, Y.; Zhou, Y.; Duan, H.; Tu, C. Three-dimensional-printed custom-made hemipelvic endoprosthesis for primary malignancies involving acetabulum: The design solution and surgical techniques. J. Orthop. Surg. Res. 2019, 14, 389. [Google Scholar] [CrossRef] [Green Version]
- Donati, D.; D’Apote, G.; Boschi, M.; Cevolani, L.; Benedetti, M.G. Clinical and functional outcomes of the saddle prosthesis. J. Orthop. Traumatol. 2012, 13, 79. [Google Scholar] [CrossRef] [Green Version]
- Fisher, N.E.; Patton, J.T.; Grimer, R.J.; Porter, D.; Jeys, L.; Tillman, R.M.; Abudu, A.; Carter, S.R. Ice-cream cone reconstruction of the pelvis: A new type of pelvic replacement: Early results. J. Bone Jt. Surg. Br. 2011, 93, 684. [Google Scholar] [CrossRef] [Green Version]
- Windhager, R.; Karner, J.; Kutschera, H.P.; Polterauer, P.; Salzer-Kuntschik, M.; Kotz, R. Limb salvage in periacetabular sarcomas: Review of 21 consecutive cases. Clin. Orthop. Relat. Res. 1996, 331, 265. [Google Scholar] [CrossRef]
- Khan, F.A.; Lipman, J.D.; Pearle, A.D.; Boland, P.J.; Healey, J.H. Surgical technique: Computer-generated custom jigs improve accuracy of wide resection of bone tumors. Clin. Orthop. Relat. Res. 2013, 471, 2007. [Google Scholar] [CrossRef] [Green Version]
- Windhager, R.; Leithner, A.; Hochegger, M. Revision of tumour endoprostheses around the knee joint. Review and own results. Orthopade 2006, 35, 176. [Google Scholar] [CrossRef]
- Puchner, S.E.; Funovics, P.T.; Böhler, C.; Kaider, A.; Stihsen, C.; Hobusch, G.M.; Panotopoulos, J.; Windhager, R. Oncological and surgical outcome after treatment of pelvic sarcomas. PLoS ONE 2017, 12, e0172203. [Google Scholar] [CrossRef]
- Henderson, E.R.; O’Connor, M.I.; Ruggieri, P.; Windhager, R.; Funovics, P.T.; Gibbons, C.L.; Guo, W.; Hornicek, F.J.; Temple, H.T.; Letson, G.D. Classification of failure of limb salvage after reconstructive surgery for bone tumours: A modified system Including biological and expandable reconstructions. Bone Jt. J. 2014, 96, 1436. [Google Scholar] [CrossRef]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. Am. 1969, 51, 737. [Google Scholar] [CrossRef]
- Chua, A.W.; Chua, M.J.; Kam, P.C.; Broekhuis, D.; Karunaratne, S.; Stalley, P.D. Anaesthetic challenges for pelvic reconstruction with custom three-dimensional-printed titanium implants: A retrospective cohort study. Anaesth. Intensive Care 2019, 47, 368. [Google Scholar] [CrossRef] [PubMed]
- Fröschen, F.S.; Randau, T.M.; Hischebeth, G.T.R.; Gravius, N.; Gravius, S.; Walter, S.G. Mid-term results after revision total hip arthroplasty with custom-made acetabular implants in patients with Paprosky III acetabular bone loss. Arch. Orthop. Trauma Surg. 2020, 140, 263. [Google Scholar] [CrossRef] [PubMed]
- Burastero, G.; Cavagnaro, L.; Chiarlone, F.; Zanirato, A.; Mosconi, L.; Felli, L.; de Lorenzo, F.D.R. Clinical study of outcomes after revision surgery using porous titanium custom-made implants for severe acetabular septic bone defects. Int. Orthop. 2020, 44, 1957. [Google Scholar] [CrossRef] [PubMed]
- Chiarlone, F.; Zanirato, A.; Cavagnaro, L.; Alessio-Mazzola, M.; Felli, L.; Burastero, G. Acetabular custom-made implants for severe acetabular bone defect in revision total hip arthroplasty: A systematic review of the literature. Arch. Orthop. Trauma Surg. 2020, 140, 415. [Google Scholar] [CrossRef]
- Dai, K.R.; Yan, M.N.; Zhu, Z.A.; Sun, Y.H. Computer-aided custom-made hemipelvic prosthesis used in extensive pelvic lesions. J. Arthroplast. 2007, 22, 981. [Google Scholar] [CrossRef]
- Abudu, A.; Grimer, R.J.; Cannon, S.R.; Carter, S.R.; Sneath, R.S. Reconstruction of the hemipelvis after the excision of malignant tumours. Complications and functional outcome of prostheses. J. Bone Jt. Surg. Br. 1997, 79, 773. [Google Scholar] [CrossRef]
- Ozaki, T.; Hoffmann, C.; Hillmann, A.; Gosheger, G.; Lindner, N.; Winkelmann, W. Implantation of hemipelvic prosthesis after resection of sarcoma. Clin. Orthop. Relat. Res. 2002, 396, 197. [Google Scholar] [CrossRef]
- Holzapfel, B.M.; Pilge, H.; Prodinger, P.M.; Toepfer, A.; Mayer-Wagner, S.; Hutmacher, D.W.; von Eisenhart-Rothe, R.; Rudert, M.; Gradinger, R.; Rechl, H. Customised osteotomy guides and endoprosthetic reconstruction for periacetabular tumours. Int. Orthop. 2014, 38, 1435. [Google Scholar] [CrossRef] [Green Version]
- Witte, D.; Bernd, L.; Bruns, J.; Gosheger, G.; Hardes, J.; Hartwig, E.; Lehner, B.; Melcher, I.; Mutschler, W.; Schulte, M.; et al. Limb-salvage reconstruction with MUTARS hemipelvic endoprosthesis: A prospective multicenter study. Eur. J. Surg. Oncol. 2009, 35, 1318. [Google Scholar] [CrossRef]
- Barrientos-Ruiz, I.; Ortiz-Cruz, E.J.; Peleteiro-Pensado, M. Reconstruction After Hemipelvectomy With the Ice-Cream Cone Prosthesis: What Are the Short-term Clinical Results? Clin. Orthop. Relat. Res. 2017, 475, 735. [Google Scholar] [CrossRef] [Green Version]
- Jansen, J.A.; van de Sande, M.A.J.; Dijkstra, P.D.S. Poor long-term clinical results of saddle prosthesis after resection of periacetabular tumors. Clin. Orthop. Relat. Res. 2013, 471, 324. [Google Scholar] [CrossRef] [Green Version]
- Wang, B.; Hao, Y.; Pu, F.; Jiang, W.; Shao, Z. Computer-aided designed, three dimensional-printed hemipelvic prosthesis for peri-acetabular malignant bone tumour. Int. Orthop. 2018, 42, 687. [Google Scholar] [CrossRef] [PubMed]
- Jovičić, M.S.; Vuletić, F.; Ribičić, T.; Šimunić, S.; Petrović, T.; Kolundžić, R. Implementation of the three-dimensional printing technology in treatment of bone tumours: A case series. Int. Orthop. 2021, 45, 1079. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, P.K.; Aston, W.J.; Grimer, R.J.; Abudu, A.; Carter, S.; Blunn, G.; Briggs, T.W.; Cannon, S. Peri-acetabular resection and endoprosthetic reconstruction for tumours of the acetabulum. J. Bone Jt. Surg. Br. 2008, 90, 1222. [Google Scholar] [CrossRef] [PubMed]







| Parameter | Patients (n = 20) | RFS |
|---|---|---|
| Median age at surgery | 25 (13–63) years | 0.9 T |
| Median follow up after surgery | 5 (1–17) years | 0.7 T |
| Sex | ||
| Male/Female | 9/11 | 0.7 * |
| Primary tumor size and localization | ||
| Median tumor size | 343 (min = 22, max = 3600) cm3 | 0.9 T |
| Ilium | 19 | 0.3 * |
| Pubis | 1 | |
| Tumor entity | ||
| Chondrosarcoma | 8 | 0.5 * |
| Ewing sarcoma | 5 | 0.7 * |
| Osteosarcoma | 4 | 0.6 * |
| PNET | 2 | 0.2 * |
| Hemangiopericytoma | 1 | |
| Grade | ||
| Low (G1–G2) | 5 | 0.5 * |
| High (G3–G4) | 14 | 0.3 * |
| N/A | 1 |
| Parameter | Included (n = 20) | Lost to Follow Up (n = 6) | p |
|---|---|---|---|
| Median Age at surgery | 25 (13–63) years | 40 (10-61) years | 0.7 T |
| Follow up after surgery | 5 (1–17) years | 3 (0-8) months | 0.007 T |
| Sex | |||
| Male/Female | 9/11 | 2/4 | 0.6 # |
| Oncological status | |||
| No evidence of disease | 12 (60%) | 0 (0%) | 0.01 # |
| Dead of disease | 7 (35%) | 6 (100%) | 0.005 # |
| Dead of other cause | 1 (5%) | 0 (0%) | |
| Conversion to hemipelvectomy | 3 (15%) | 3 (50%) | 0.07 # |
| Infection | 9 (45%) | 3 (50%) | 0.8 # |
| Thromboembolic event | 5 (25%) | 2 (33%) | 0.7 # |
| Conservative/surgical treatment | 2/3 | 0/2 |
| Surgical Complications | Patients (n = 20) | Median Time to Revision |
|---|---|---|
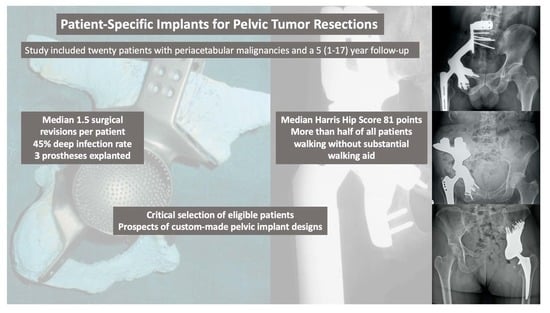
| Median sum surgical revisions per patient | 1.5 (0–7) | |
| Prosthesis explantation | 3 | 15 months (95 days–16 years) |
| Deep infection | 9 | 86 days (13 days–5 years) |
| Aseptic loosening | 4 | 38.5 (10–80) months |
| Dislocation | 3 | 5 months (14 days–20 months) |
| Sciatic nerve lesions | 4 | 26 (24–28) months |
| Conservative/surgical treatment | 2/2 | |
| Thromboembolic event | 5 | 0 (0–0) days |
| Conservative/surgical treatment | 2/3 |
| Parameter | Patients (n = 20) | RFS |
|---|---|---|
| Surgical approach | ||
| Ventral + Dorsal | 12 | 0.9 * |
| Ventral | 7 | 0.5 * |
| N/A | 1 | |
| Type of internal hemipelvectomy (Enneking/Dunham) | ||
| I–IV | 8 | 0.6 * |
| I, II, III | 3 | 0.6 * |
| I, II | 3 | 0.5 * |
| II, III | 2 | 0.8 * |
| I, II, IV | 2 | 0.7 * |
| N/A | 2 | 0.5 * |
| Femoral stem | ||
| Zweymueller | 12 | 0.7 * |
| Austroprosthesis | 3 | 0.5 * |
| N/A | 5 | 0.9 * |
| Cemented Polyethylene Cup | ||
| Brunswick | 9 | 0.4 * |
| N/A | 9 | 0.9 * |
| Mueller | 2 | 0.3 * |
| Surgical margin | ||
| Negative | 19 | 0.6 * |
| Positive | 1 | |
| Oncologic status at final follow up | ||
| No evidence of disease | 12 | 0.7 * |
| Dead of disease | 7 | 0.3 * |
| Dead of other cause | 1 | |
| Functional status at final follow up | ||
| Median Harris Hip Score (n = 11) | 81 (37–92) points | |
| Mobilized with hip orthosis | 4 | 0.2 * |
| Walking without aid | 6 | 0.4 * |
| Walking with a walking stick | 6 | 0.98 * |
| Walking with two crutches | 3 | 0.1 * |
| No information | 5 | 0.93 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Döring, K.; Staats, K.; Puchner, S.; Windhager, R. Patient-Specific Implants for Pelvic Tumor Resections. J. Pers. Med. 2021, 11, 683. https://doi.org/10.3390/jpm11080683
Döring K, Staats K, Puchner S, Windhager R. Patient-Specific Implants for Pelvic Tumor Resections. Journal of Personalized Medicine. 2021; 11(8):683. https://doi.org/10.3390/jpm11080683
Chicago/Turabian StyleDöring, Kevin, Kevin Staats, Stephan Puchner, and Reinhard Windhager. 2021. "Patient-Specific Implants for Pelvic Tumor Resections" Journal of Personalized Medicine 11, no. 8: 683. https://doi.org/10.3390/jpm11080683
APA StyleDöring, K., Staats, K., Puchner, S., & Windhager, R. (2021). Patient-Specific Implants for Pelvic Tumor Resections. Journal of Personalized Medicine, 11(8), 683. https://doi.org/10.3390/jpm11080683