Personalized Orthodontics: From the Sagittal Position of Lower Incisors to the Facial Profile Esthetics
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic Characteristics of the Examined Patients
3.2. Cephalometric Assessment of the Sagittal Jaw Relationship
3.3. Analysis of the Facial Profile Convexity
3.4. Assessment of the Cephalometric Angles: FMIA, IMPA
3.5. Cephalometric Parameters Describing Patients with Convex Profile
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Williams, P. Lower incisor position in treatment planning. Br. J. Orthod. 1986, 13, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Sayago, E.; Espinar-Escalona, E.; Barrera-Mora, J.M.; Ruiz-Navarro, M.B.; Llamas-Carreras, J.M.; Solano-Reina, E. Lower incisor position in different malocclusions and facial patterns. Med. Oral. Patol. Oral. Cir. Bucal. 2013, 18, e343. [Google Scholar] [CrossRef]
- Miethke, R.R.; Behm-Menthel, A. Correlations between lower incisor crowding and lower incisor position and lateral craniofacial morphology. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 231–239. [Google Scholar] [CrossRef]
- Singh, S.; Shivaprakash, G. To Evaluate the Correlation Between Skeletal and Dental Parameters to the Amount of Crowding in Class II Div. 1 Malocclusions. J. Clin. Diagn. Res. 2017, 11, ZC22. [Google Scholar] [CrossRef]
- Dyer, K.C.; Vaden, J.L.; Harris, E.F. Relapse revisited-again. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Merrifield, L.L. Dimensions of the denture: Back to basics. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 535–542. [Google Scholar] [CrossRef]
- de Bernabé, P.G.; Montiel-Company, J.M.; Paredes-Gallardo, V.; Gandía-Franco, J.L.; Bellot-Arcís, C. Orthodontic treatment stability predictors: A retrospective longitudinal study. Angle Orthod. 2017, 87, 223–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Y.; Sun, J.; Lai, W.; Wu, T.; Koshy, S.; Shi, Z. Interventions for managing relapse of the lower front teeth after orthodontic treatment. Cochrane Database Syst. Rev. 2013, 9, CD008734. [Google Scholar] [CrossRef] [Green Version]
- Kamak, G.; Kamak, H.; Keklik, H.; Gurel, H.G. The effect of changes in lower incisor inclination on gingival recession. Scientific World J. 2015, 2015, 193206. [Google Scholar] [CrossRef] [Green Version]
- Sheng, Y.; Guo, H.M.; Bai, Y.X.; Li, S. Dehiscence and fenestration in anterior teeth: Comparison before and after orthodontic treatment. J. Orofac. Orthop. 2020, 81, 1–9. [Google Scholar] [CrossRef]
- Ciavarella, D.; Tepedino, M.; Gallo, C.; Montaruli, G.; Zhurakivska, K.; Coppola, L.; Troiano, G.; Chimenti, C.; Laurenziello, M.; Lo Russo, L. Post-orthodontic position of lower incisors and gingival recession: A retrospective study. J. Clin. Exp. Dent. 2017, 9, e1425–e1430. [Google Scholar] [CrossRef]
- Klontz, H.A. Facial balance and harmony: An attainable objective for the patient with a high mandibular plane angle. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 176–188. [Google Scholar] [CrossRef]
- Merrifield, L.L. The profile line as an aid in critically evaluating facial esthetics. Am. J. Orthod. 1966, 52, 804–822. [Google Scholar] [CrossRef]
- Lu, W.; Zhang, X.; Mei, L.; Wang, P.; He, J.; Li, Y.; Zhao, Z. Orthodontic incisor retraction caused changes in the soft tissue chin area: A retrospective study. BMC Oral Health 2020, 20, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Margolis, H.I. The axial inclination of the mandibular incisors. Am. J. Orthod. Oral Surg. 1943, 29, 571–594. [Google Scholar] [CrossRef]
- Tweed, C. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am. J. Orthod. Oral Surg. 1946, 32, 175–230. [Google Scholar] [CrossRef]
- Cross, J.J. The Tweed philosophy: The Tweed years. Semin. Orthod. 1996, 2, 231–236. [Google Scholar] [CrossRef]
- Vaden, J.L. The Tweed-Merrifield philosophy. Semin. Orthod. 1996, 2, 237–240. [Google Scholar] [CrossRef]
- Tweed, C.H. The diagnostic facial triangle in the control of treatment objectives. Am. J. Orthod. 1969, 55, 651–657. [Google Scholar] [CrossRef]
- Merrifield, L.L. Differential diagnosis. Semin. Orthod. 1996, 2, 241–253. [Google Scholar] [CrossRef]
- Tweed, C.H. The Frankfort-Mandibular Incisor Angle (FMIA) in orthodontic diagnosis, treatment planning, and prognosis. Angle Orthod. 1954, 24, 121–169. [Google Scholar] [CrossRef]
- Merrifield, L.L.; Klontz, H.A.; Vaden, J.L. Differential diagnostic analysis system. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 641–648. [Google Scholar] [CrossRef]
- Derwich, M.; Mitus-Kenig, M.; Pawlowska, E. Is the Temporomandibular Joints’ Reciprocal Clicking Related to the Morphology and Position of the Mandible, as Well as to the Sagittal Position of Lower Incisors?—A Case-Control Study. Int. J. Environ. Res. Public Health 2021, 18, 4994. [Google Scholar] [CrossRef]
- Linjawi, A.I. Age- and gender-related incisor changes in different vertical craniofacial relationships. J. Orthod. Sci. 2016, 5, 132–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhammadi, M.S. Dentoalveolar compensation in different anterioposterior and vertical skeletal malocclusions. J. Clin. Exp. Dent. 2019, 11, e745–e753. [Google Scholar] [CrossRef] [PubMed]
- Siécola, G.S.; Capelozza, L.F.; Lorenzoni, D.C.; Janson, G.; Henriques, J.F.C. Subjective facial analysis and its correlation with dental relationships. Dental Press J. Orthod. 2017, 22, 87–94. [Google Scholar] [CrossRef] [Green Version]
- Solem, R.C.; Marasco, R.; Guiterrez-Pulido, L.; Nielsen, I.; Kim, S.H.; Nelson, G. Three-dimensional soft-tissue and hard-tissue changes in the treatment of bimaxillary protrusion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 218–228. [Google Scholar] [CrossRef]
- Cho, H.N.; Yoon, H.J.; Park, J.H.; Park, Y.G.; Kim, S.J. Effect of extraction treatment on upper airway dimensions in patients with bimaxillary skeletal protrusion relative to their vertical skeletal pattern. Korean J. Orthod. 2021, 51, 166–178. [Google Scholar] [CrossRef]
- Araújo, T.M.; Caldas, L.D. Tooth extractions in Orthodontics: First or second premolars? Dental Press J. Orthod. 2019, 24, 88–98. [Google Scholar] [CrossRef] [Green Version]
- Contini, E.; Orthod, D.; Campi, S.; Caprioglio, A. Profile changes following lower incisor repositioning: A comparison between patients with different growth pattern. Minerva Stomatol. 2015, 64, 75–85. [Google Scholar]
- Krooks, L.; Pirttiniemi, P.; Tolvanen, M.; Kanavakis, G.; Lähdesmäki, R.; Silvola, A.S. Association of facial sagittal and vertical characteristics with facial aesthetics in the Northern Finland Birth Cohort 1966. Eur. J. Orthod. 2019, 41, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, Y.; Ezura, A.; Nomintsetseg, B. The relationship between the incisor position and lingual surface morphology in normal occlusion. Odontology 2017, 105, 84–90. [Google Scholar] [CrossRef]
- Wennström, J.L. Mucogingival considerations in orthodontic treatment. Semin. Orthod. 1996, 2, 46–54. [Google Scholar] [CrossRef]
- Gütermann, C.; Peltomäki, T.; Markic, G.; Hänggi, M.; Schätzle, M.; Signorelli, L.; Patcas, R. The inclination of mandibular incisors revisited. Angle Orthod. 2014, 84, 109–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Dyck, C.; Dekeyser, A.; Vantricht, E.; Manders, E.; Goeleven, A.; Fieuws, S.; Willems, G. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: A pilot study. Eur. J. Orthod. 2016, 38, 227–234. [Google Scholar] [CrossRef] [Green Version]
- Srinivasan, B.; Chitharanjan, A.B. Skeletal and dental characteristics in subjects with ankyloglossia. Prog. Orthod. 2013, 14, 44. [Google Scholar] [CrossRef] [Green Version]
- Didier, H.; Assandri, F.; Gaffuri, F.; Cavagnetto, D.; Abate, A.; Villanova, M.; Maiorana, C. The Role of Dental Occlusion and Neuromuscular Behavior in Professional Ballet Dancers Performance: A Pilot Study. Healthcare 2021, 9, 251. [Google Scholar] [CrossRef]




| Criteria | List of Specific Criteria |
|---|---|
| Inclusion criteria | - Generally healthy patients (no systemic diseases) - Age between 15 and 25 years old - Willingness to participate in the study - No previous orthodontic treatment |
| Exclusion criteria | - Age below 15 and above 25 years old - History of traumas in the area of head and neck - History of surgeries in the area of head and neck - Craniofacial deformities - Cleft lip and cleft palate- Genetic syndromes - Temporomandibular joint disorders - Rheumatological diseases, oncological diseases - History of radiotherapy (especially in the area of the head and neck) - People treated orthodontically at least once in the past - Pregnancy - Patients who did not agree to take part in the study |
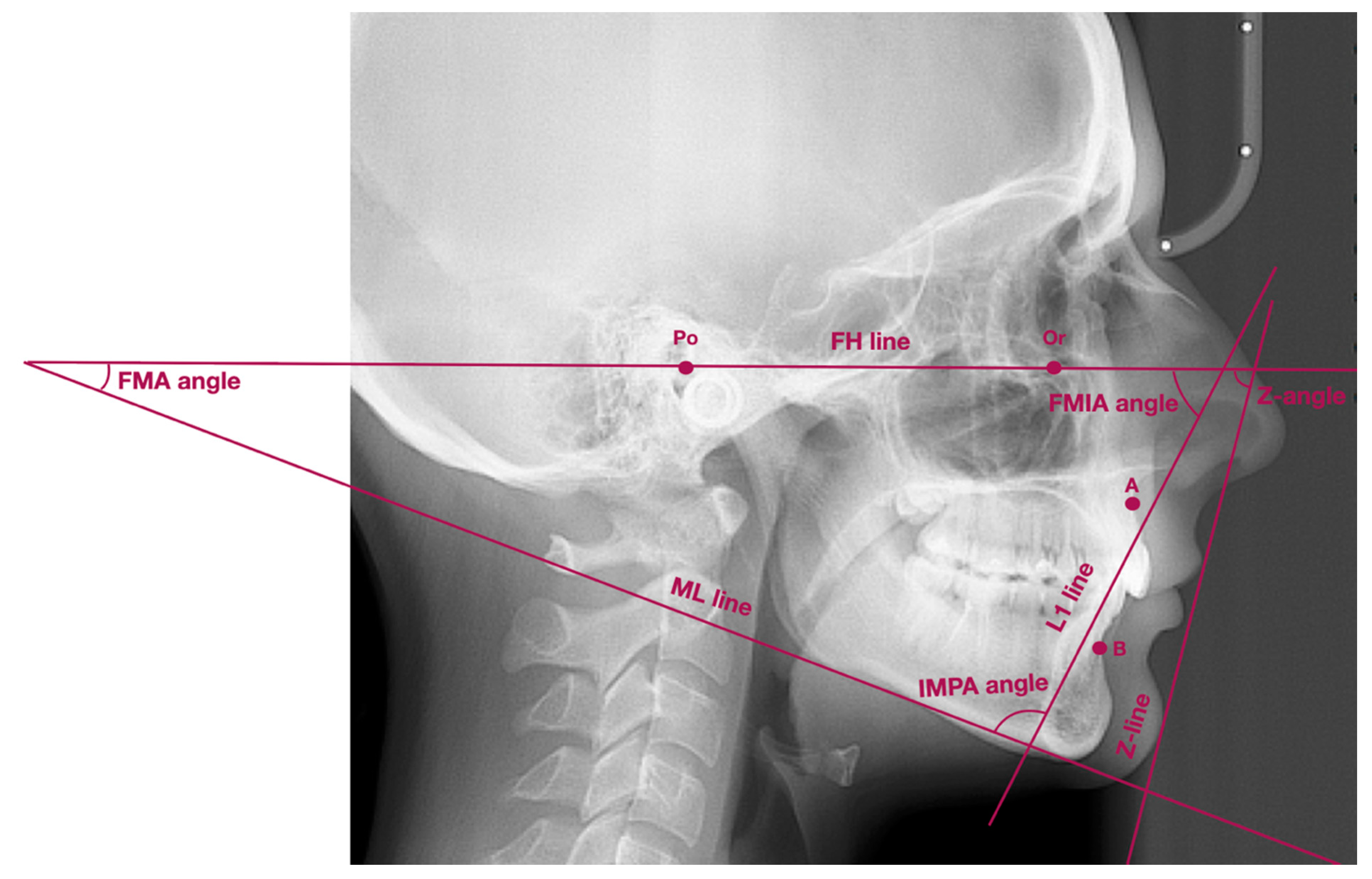
| Points/Lines/Angles | Description of Points/Lines/Angles |
|---|---|
| Point Po | Porion—the most superior part of external acoustic opening |
| Point Or | Orbitale—the most inferior point localized in the lower margin of the orbit |
| Point A | Subspinale—the deepest point localized in the anterior outline of the maxilla, below the anterior nasal spine |
| Point B | Supramentale—the deepest point localized in the anterior outline of the mandible, above the pogonion |
| Wits | AO-BO—distance between the perpendicular projection of points A and B onto the functional occlusal plane |
| ML line | Mandibular line—line between gnathion and the lowest point localized in the masseteric tuberosity (also known as GoGn line) |
| FH line | Frankfort horizontal line—line between points: porion and orbitale |
| L1 line | Long axis of lower incisor—line which connects the incisal edge with the radiological apex of lower incisor |
| Z-line | Z-line (the profile line)—line which connects the most prominent point on soft-tissue chin with the most prominent point on either upper or lower lip, depending on which lip was more protruded |
| FMA angle | Angle between FH line and ML line |
| FMIA angle | Angle between FH line and long axis of lower incisor |
| IMPA angle | Angle between long axis of lower incisor and ML line |
| Z-angle | Angle between Z-line and FH line |
| Comparable Characteristic | Control group (n = 76) FMA 22°–28° | Group 1 (n = 51) FMA < 22° | Group 2 (n = 73) FMA > 28° | Together (n = 200) | p-Value |
|---|---|---|---|---|---|
| AGE | 0.006 1 | ||||
| av. (SD) | 18.6 (3.5) | 18.5 (3.2) | 17.1 (2.8) | 18.0 (3.2) | |
| range | 15.0–25.0 | 15.0–25.0 | 15.0–25.0 | 15.0–25.0 | |
| median (Q1;Q3) | 17 (15;20) | 17 (15;21) | 16 (15;18) | 17 (15;20) | |
| SEX | 0.802 2 | ||||
| Female (%) | 55 (72.4%) | 37 (72.5%) | 56 (76.7%) | 148 (74.0%) | |
| Male (%) | 21 (27.6%) | 14 (27.5%) | 17 (23.3%) | 52 (26.0%) |
| Measurement | Control Group (n = 76) FMA 22°–28° | Group 1 (n = 51) FMA < 22° | Group 2 (n = 73) FMA > 28° | Together (n = 200) | p-Value |
|---|---|---|---|---|---|
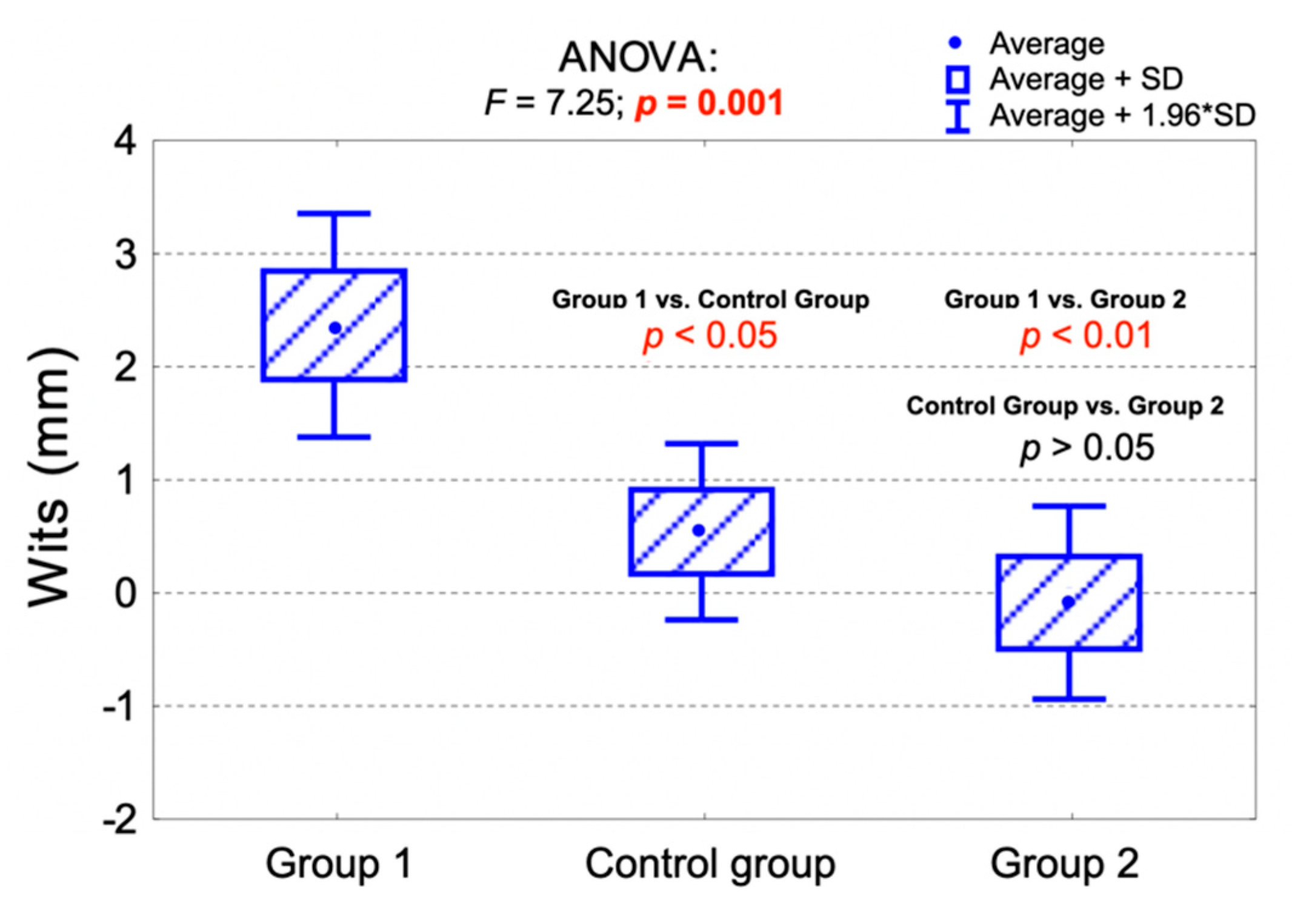
| Wits analysis | 0.010 1 | ||||
| Skeletal class I (Wits = 0 ± 2 mm) | 35 (46.1%) | 17 (33.3%) | 33 (45.2%) | 85 (42.5%) | |
| Skeletal class II (Wits > 2 mm) | 26 (34.2%) | 29 (56.9%) | 20 (27.4%) | 75 (37.5%) | |
| Skeletal class III (Wits < −2 mm) | 15 (19.7%) | 5 (9.8%) | 20 (27.4%) | 40 (20.0%) | |
| Wits (mm) | 0.001 2 | ||||
| av. (SD) | 0.5 (3.5) | 2.3 (3.6) | −0.1 (3.7) | 0.8 (3.7) | |
| range | −7.0–8.0 | −9.0–9.0 | −9.0–9.0 | −9.0–9.0 | |
| median (Q1;Q3) | 0 (−2;3) | 3 (0;5) | 0 (−2;2) | 1 (−1;4) |
| Measurement | Control Group (n = 76) FMA 22°–28° | Group 1 (n = 51) FMA < 22° | Group 2 (n = 73) FMA > 28° | Together (n = 200) | p-Value |
|---|---|---|---|---|---|
| Z-line position | 0.003 1 | ||||
| In front of the nose (convex profile) | 9 (11.8%) | 4 (7.8%) | 21 (28.8%) | 34 (17.0%) | |
| Crossing the nose (normal profile) | 61 (80.3%) | 47 (92.2%) | 48 (65.8%) | 156 (78.0%) | |
| Crossing the tip of the nose (borderline profile) | 6 (7.9%) | 0 (0.0%) | 4 (5.5%) | 10 (5.0%) | |
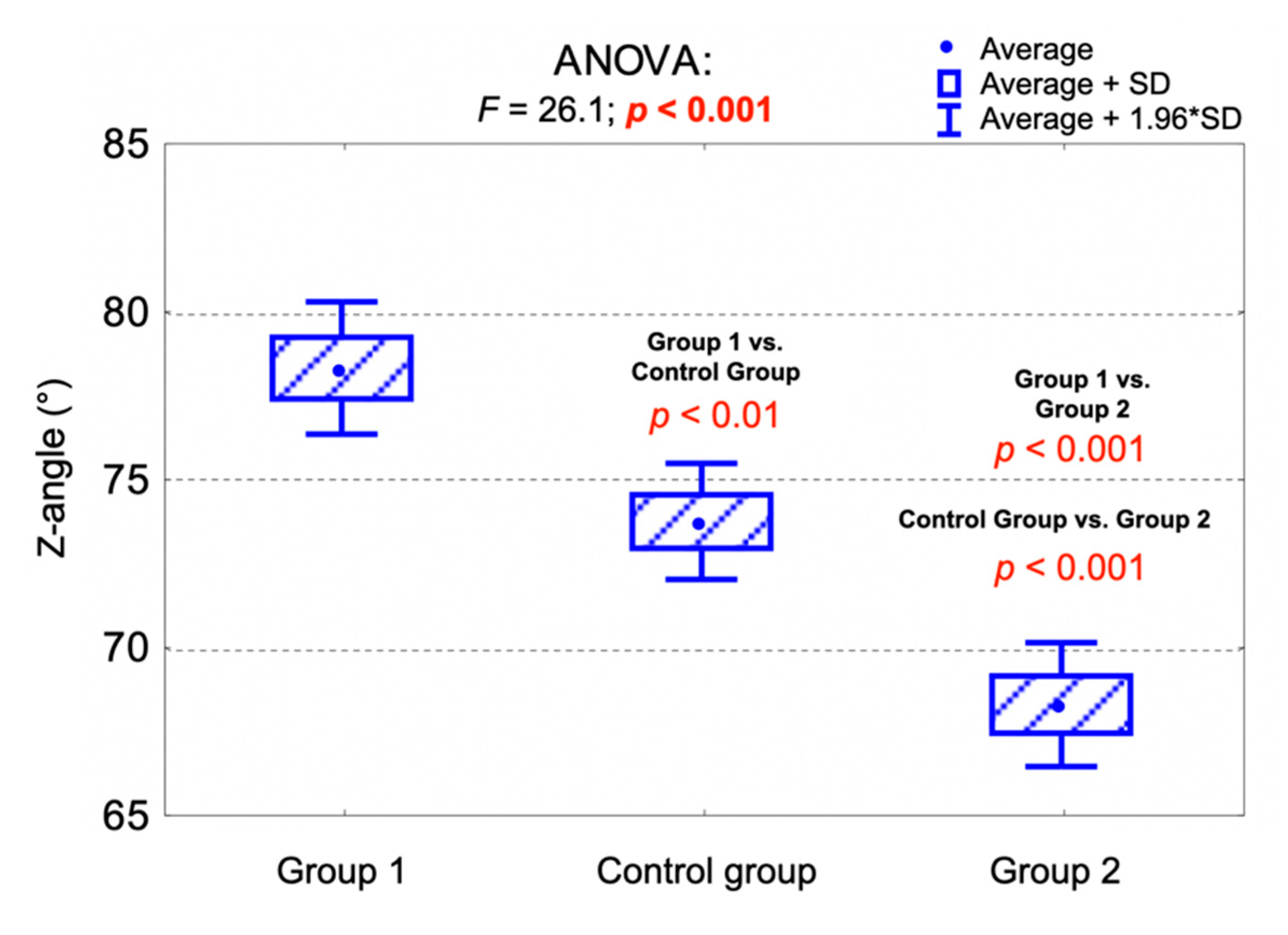
| Z-angle (°) | <0.001 2 | ||||
| av. (SD) | 73.7 (7.7) | 78.2 (7.2) | 68.2 (8.0) | 72.8 (8.6) | |
| range | 50.0–87.0 | 60.0–102.0 | 44.0–82.0 | 44.0–102.0 | |
| median (Q1;Q3) | 75 (68;79) | 78 (74;83) | 69 (65;75) | 74 (68;79) |
| Measurement | Convex Profile (n = 34) Z-Line in front of the Nose | Borderline Profile (n = 10) Z-Line Crossing the Tip of the Nose | Normal Profile (n = 156) Z-LineCrossing the Nose | p-Value |
|---|---|---|---|---|
| Z-angle (°) | <0.001 1 | |||
| av. (SD) | 60.5 (6.8) | 66.5 (3.8) | 75.9 (6.2) | |
| range | 44.0–74.0 | 61.0–70.0 | 63.0–102.0 | |
| median (Q1;Q3) | 61 (57;65) | 68 (63;70) | 76 (71;80) |
| Measurement | Control Group (n = 76) FMA 22°–28° | Group 1 (n = 51) FMA < 22° | Group 2 (n = 73) FMA > 28° | Together (n = 200) | p-Value |
|---|---|---|---|---|---|
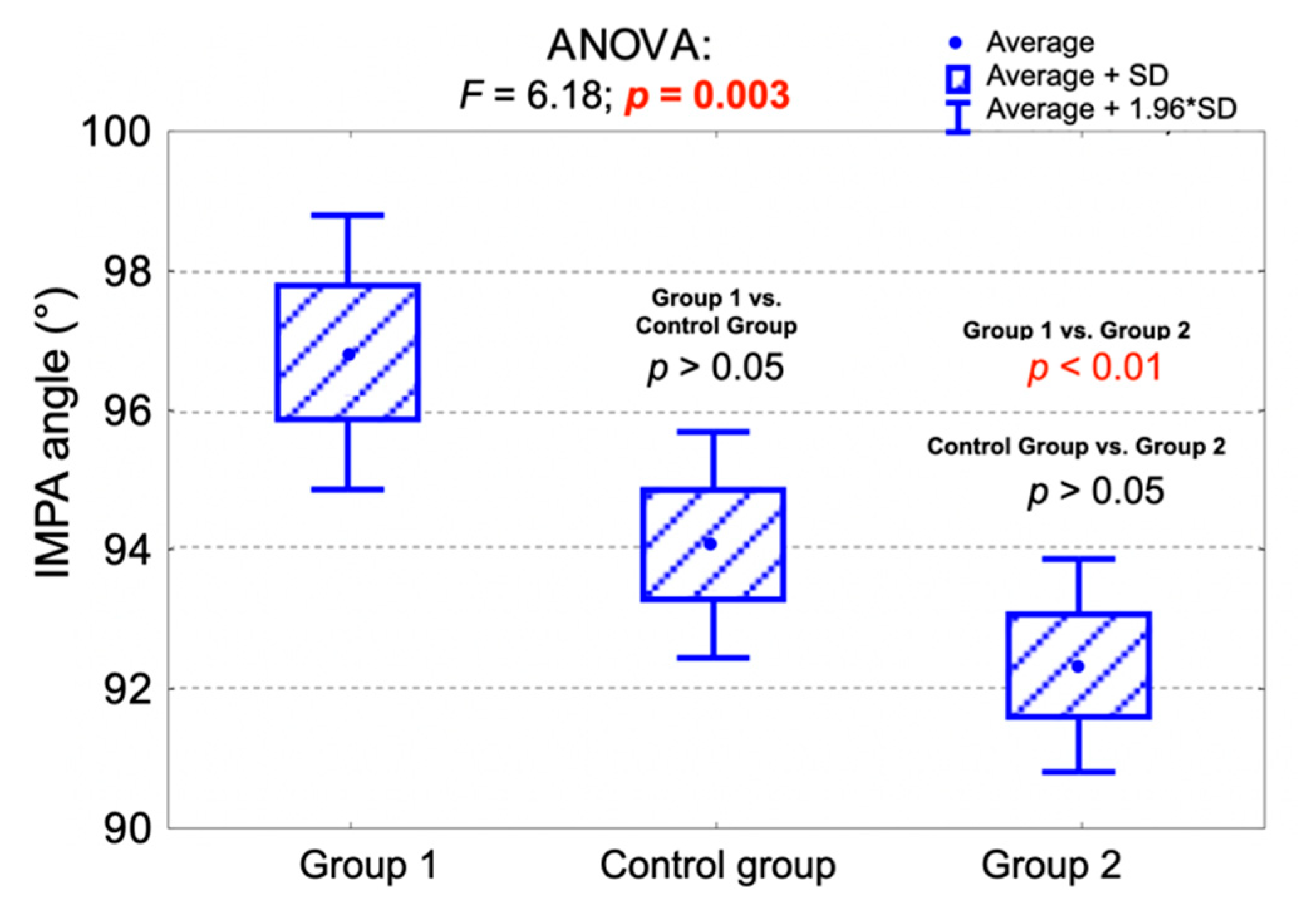
| IMPA (°) | 0.003 1 | ||||
| av. (SD) | 94.0 (7.2) | 96.8 (7.2) | 92.3 (6.7) | 94.1 (7.2) | |
| range | 80.0–110.0 | 78.0–115.0 | 79.0–106.0 | 78.0–115.0 | |
| median (Q1;Q3) | 94 (89;98) | 96 (91;101) | 92 (87;97) | 93 (90;99) | |
| FMIA (°) | <0.001 1 | ||||
| av. (SD) | 60.7 (7.6) | 65.1 (8.2) | 54.9 (6.6) | 59.7 (8.4) | |
| range | 42.0–78.0 | 50.0–91.0 | 36.0–72.0 | 36.0–91.0 | |
| median (Q1;Q3) | 61 (56;67) | 65 (60;70) | 56 (50;59) | 60 (54;65) |
| Measurement | Convex Profile (n = 34) Z-Line in front of the Nose | Borderline Profile (n = 10) Z-Line Crossing the Tip of the Nose | Normal Profile (n = 156) Z-LineCrossing the Nose | p-Value |
|---|---|---|---|---|
| IMPA (°) | <0.001 1 | |||
| av. (SD) | 100.6 (5.9) | 98.1 (6.9) | 92.4 (6.6) | |
| range | 87.0–115.0 | 90.0–110.0 | 78.0–109.0 | |
| median (Q1;Q3) | 100 (97;104) | 97 (92;103) | 92 (88;97) | |
| FMIA (°) | <0.001 1 | |||
| av. (SD) | 49.6 (5.4) | 53.1 (6.0) | 62.3 (7.1) | |
| range | 36.0–59.0 | 45.0–62.0 | 49.0–91.0 | |
| median (Q1;Q3) | 50 (46;53) | 54 (47;57) | 62 (57;67) |
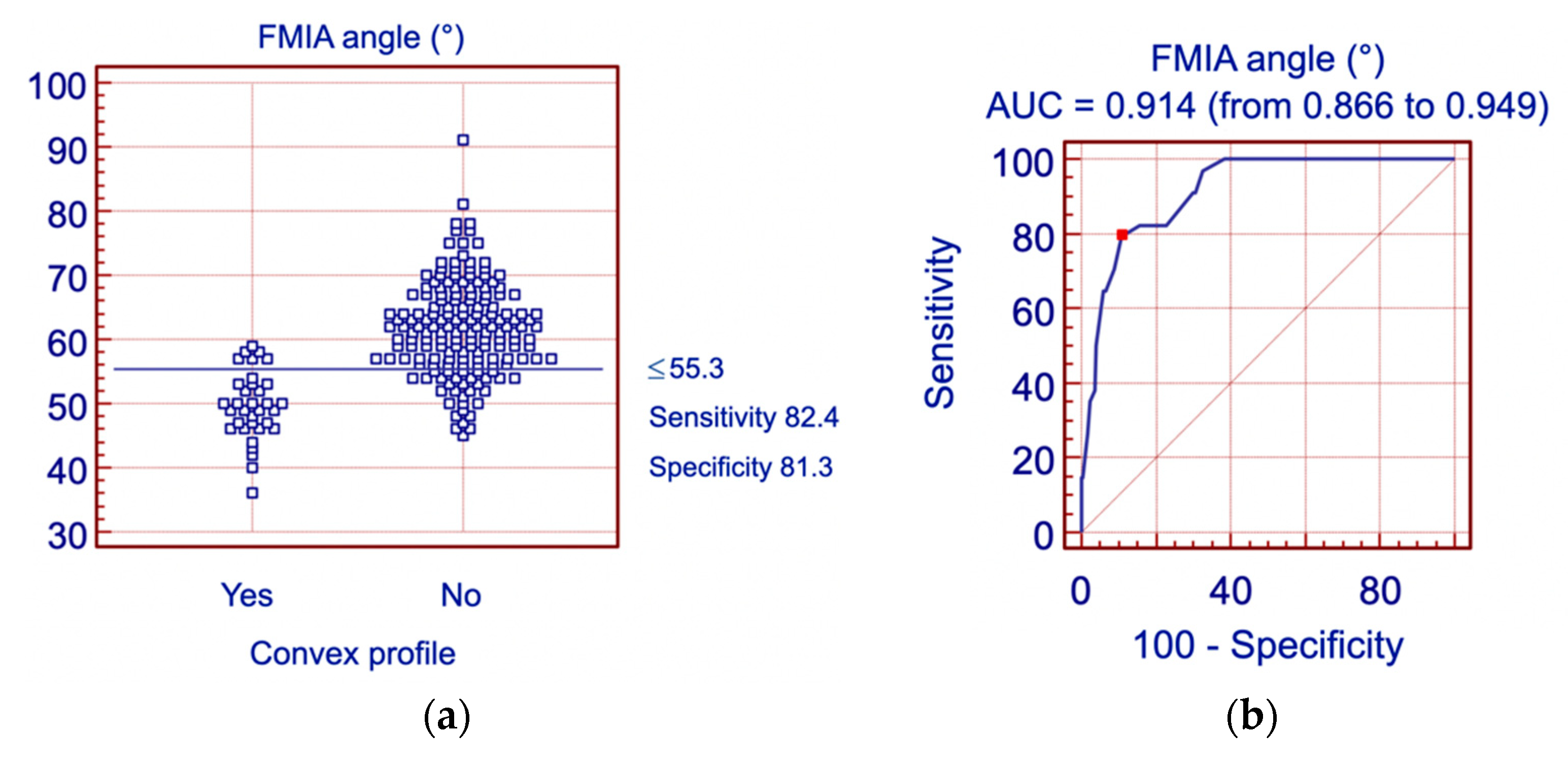
| Parameter | Cutoff Value | Sensitivity | Specificity | Area under the Curve (AUC) | 95% CI for AUC |
|---|---|---|---|---|---|
| FMA angle | >29.0° | 61.8% | 72.3% | 0.700 | (0.632;0.763) |
| FMIA angle | ≤55.3° | 82.4% | 81.3% | 0.914 | (0.866;0.949) |
| IMPA angle | >99.0° | 67.6% | 85.5% | 0.815 | (0.755;0.867) |
| Z angle | ≤68.0° | 94.1% | 84.3% | 0.957 | (0.918;0.980) |
| Wits | >2.1 mm | 58.8% | 68.7% | 0.657 | (0.587;0.722) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Derwich, M.; Minch, L.; Mitus-Kenig, M.; Zoltowska, A.; Pawlowska, E. Personalized Orthodontics: From the Sagittal Position of Lower Incisors to the Facial Profile Esthetics. J. Pers. Med. 2021, 11, 692. https://doi.org/10.3390/jpm11080692
Derwich M, Minch L, Mitus-Kenig M, Zoltowska A, Pawlowska E. Personalized Orthodontics: From the Sagittal Position of Lower Incisors to the Facial Profile Esthetics. Journal of Personalized Medicine. 2021; 11(8):692. https://doi.org/10.3390/jpm11080692
Chicago/Turabian StyleDerwich, Marcin, Liwia Minch, Maria Mitus-Kenig, Agata Zoltowska, and Elzbieta Pawlowska. 2021. "Personalized Orthodontics: From the Sagittal Position of Lower Incisors to the Facial Profile Esthetics" Journal of Personalized Medicine 11, no. 8: 692. https://doi.org/10.3390/jpm11080692
APA StyleDerwich, M., Minch, L., Mitus-Kenig, M., Zoltowska, A., & Pawlowska, E. (2021). Personalized Orthodontics: From the Sagittal Position of Lower Incisors to the Facial Profile Esthetics. Journal of Personalized Medicine, 11(8), 692. https://doi.org/10.3390/jpm11080692





