Systematic Review on the Mental Health and Treatment Impacts of COVID-19 on Neurocognitive Disorders
Abstract
:1. Introduction
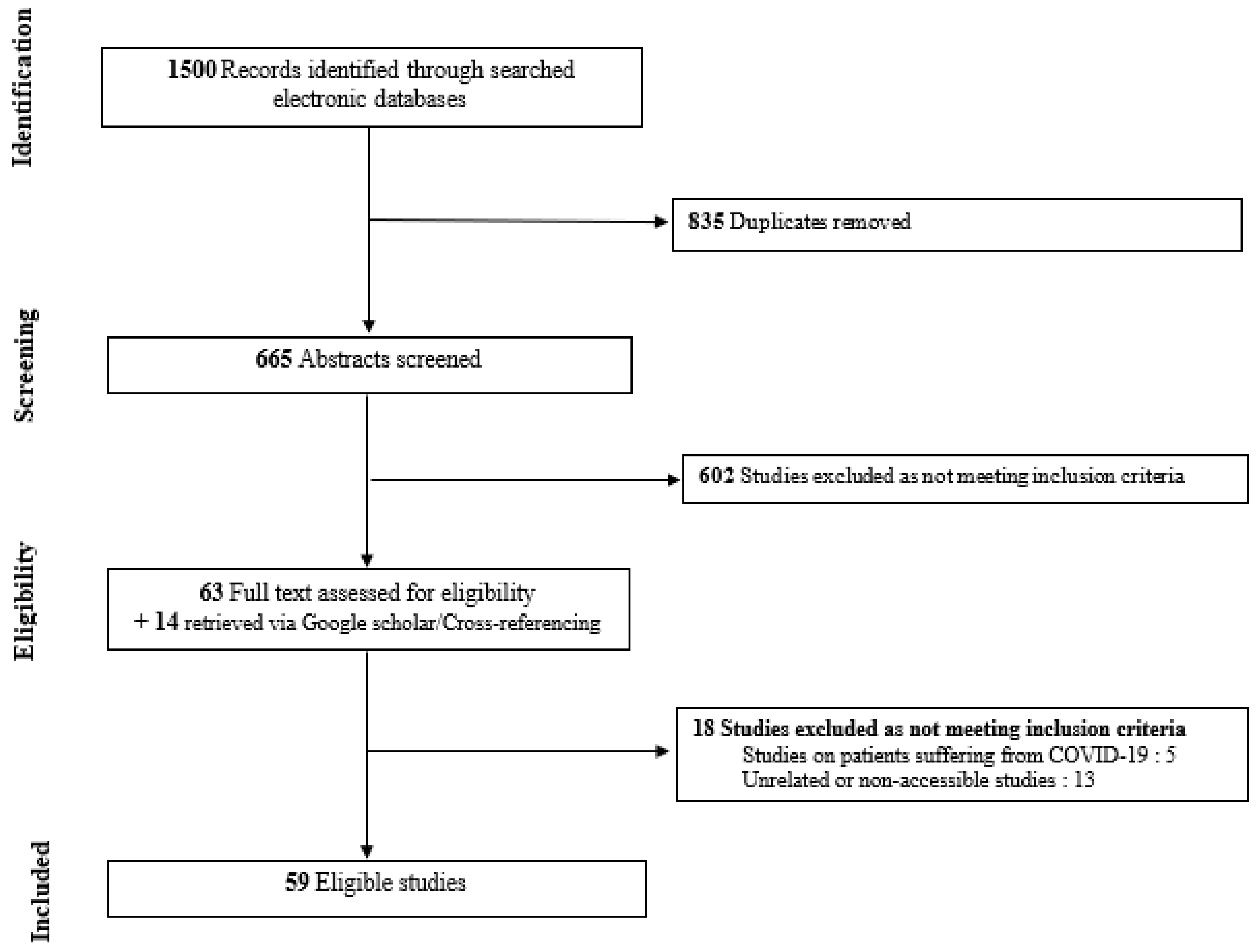
2. Methodology
2.1. Search Strategy
2.2. Study Eligibility
2.3. Data Extraction
3. Results
3.1. Psychiatric Effects
3.2. Therapeutic Effects
3.2.1. Challenges to Standard Care and Social Support Services
3.2.2. Increase in Telemedicine and Challenges
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. 2021. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 10 April 2021).
- Barry, H.E.; Hughes, C.M. Managing medicines in the time of COVID-19: Implications for community-dwelling people with dementia. Int. J. Clin. Pharm. 2021, 43, 275–279. [Google Scholar] [CrossRef]
- Luigi, M.; Dellazizzo, L.; Giguère, C.-E.; Goulet, M.-H.; Dumais, A. Shedding Light on “the Hole”: A Systematic Review and Meta-Analysis on Adverse Psychological Effects and Mortality Following Solitary Confinement in Correctional Settings. Front. Psychiatry 2020, 11, 840. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Hao, F.; Tan, W.; Jiang, L.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; Luo, X.; Jiang, X.; McIntyre, R.S.; et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, Behav. Immun. 2020, 87, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Campion, J.; Javed, A.; Sartorius, N.; Marmot, M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry 2020, 7, 657–659. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak, 18 March 2020; No. WHO/2019-nCoV/MentalHealth/2020.1; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- National Institute on Aging. What Is Dementia? Symptoms, Types, and Diagnosis; U.S. Department of Health & Human Services: Washington, DC, USA, 2017.
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Conhen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Tsapanou, A.; Papatriantafyllou, J.D.; Yiannopoulou, K.G.; Sali, D.; Kalligerou, F.; Ntanasi, E.; Zoi, P.; Margioti, E.; Vasiliki, K.; Maria, H.; et al. The impact of COVID-19 pandemic on people with Mild Cognitive Impairment/Dementia and on their caregivers. Int. J. Geriatr. Psychiatry 2020, 36, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Canevelli, M.; Valletta, M.; Blasi, M.T.; Remoli, G.; Sarti, G.; Nuti, F.; Sciancalepore, F.; Ruberti, E.; Cesari, M.; Bruno, G. Facing Dementia During the COVID -19 Outbreak. J. Am. Geriatr. Soc. 2020, 68, 1673–1676. [Google Scholar] [CrossRef] [PubMed]
- Koh, Z.Y.; Law, F.; Chew, J.; Ali, N.; Lim, W.S. Impact of Coronavirus Disease on Persons with Dementia and Their Caregivers: An Audit Study. Ann. Geriatr. Med. Res. 2020, 24, 316–320. [Google Scholar] [CrossRef]
- Cuffaro, L.; Di Lorenzo, F.; Bonavita, S.; Tedeschi, G.; Leocani, L.; Lavorgna, L. Dementia care and COVID-19 pandemic: A necessary digital revolution. Neurol. Sci. 2020, 41, 1977–1979. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Jhoo, J.H.; Jang, J.-W. The effect of telemedicine on cognitive decline in patients with dementia. J. Telemed. Telecare 2016, 23, 149–154. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- van Maurik, I.S.; Bakker, E.D.; van den Buuse, S.; Gillissen, F.; van de Beek, M.; Lemstra, E.; Mank, A.; van den Bosch, K.A.; van Leeuwenstijn, M.; Bouwman, F.H.; et al. Psychosocial Effects of Corona Measures on Patients With Dementia, Mild Cognitive Impairment and Subjective Cognitive Decline. Front. Psychiatry 2020, 11, 585686. [Google Scholar] [CrossRef]
- Penteado, C.T.; Loureiro, J.C.; Pais, M.V.; Carvalho, C.L.; Sant’Ana, L.F.G.; Valiengo, L.C.L.; Stella, F.; Forlenza, O.V. Mental Health Status of Psychogeriatric Patients During the 2019 New Coronavirus Disease (COVID-19) Pandemic and Effects on Caregiver Burden. Front. Psychiatry 2020, 11, 578672. [Google Scholar] [CrossRef] [PubMed]
- Cagnin, A.; Di Lorenzo, R.; Marra, C.; Bonanni, L.; Cupidi, C.; Laganà, V.; Rubino, E.; Vacca, A.; Provero, P.; Isella, V.; et al. Behavioral and Psychological Effects of Coronavirus Disease-19 Quarantine in Patients with Dementia. Front. Psychiatry 2020, 11, 578015. [Google Scholar] [CrossRef]
- Cohen, G.; Russo, M.J.; Campos, J.A.; Allegri, R.F. COVID-19 Epidemic in Argentina: Worsening of Behavioral Symptoms in Elderly Subjects with Dementia Living in the Community. Front. Psychiatry 2020, 11, 866. [Google Scholar] [CrossRef] [PubMed]
- Cohen, G.; Russo, M.J.; Campos, J.A.; Allegri, R.F. Living with dementia: Increased level of caregiver stress in times of COVID-19. Int. Psychogeriatr. 2020, 32, 1377–1381. [Google Scholar] [CrossRef] [PubMed]
- Tsugawa, A.; Sakurai, S.; Inagawa, Y.; Hirose, D.; Kaneko, Y.; Ogawa, Y.; Serisawa, S.; Takenoshita, N.; Sakurai, H.; Kanetaka, H.; et al. Awareness of the COVID-19 Outbreak and Resultant Depressive Tendencies in Patients with Severe Alzheimer’s Disease. J Alzheimers Dis. 2020, 77, 539–541. [Google Scholar] [CrossRef]
- Howard, R.; Burns, A.; Schneider, L. Antipsychotic prescribing to people with dementia during COVID-19. Lancet Neurol. 2020, 19, 892. [Google Scholar] [CrossRef]
- Borges-Machado, F.; Barros, D.; Ribeiro, Ó.; Carvalho, J. The Effects of COVID-19 Home Confinement in Dementia Care: Physical and Cognitive Decline, Severe Neuropsychiatric Symptoms and Increased Caregiving Burden. Am. J. Alzheimers Dis. Other Dement. 2020, 35, 1533317520976720. [Google Scholar] [CrossRef] [PubMed]
- Lara, B.B.; Carnes, A.; Dakterzada, F.; Benítez, I.D.; Piñol-Ripoll, G. Neuropsychiatric symptoms and quality of life in Spanish patients with Alzheimer’s disease during the COVID-19 lockdown. Eur. J. Neurol. 2020, 27, 1744–1747. [Google Scholar] [CrossRef]
- Capozzo, R.; Zoccolella, S.; Frisullo, M.E.; Barone, R.; Dell’Abate, M.T.; Barulli, M.R.; Musio, M.; Accogli, M.; Logroscino, G. Telemedicine for Delivery of Care in Frontotemporal Lobar Degeneration During COVID-19 Pandemic: Results from Southern Italy. J. Alzheimers Dis. 2020, 76, 481–489. [Google Scholar] [CrossRef]
- Boutoleau-Bretonnière, C.; Pouclet-Courtemanche, H.; Gillet, A.; Bernard, A.; Deruet, A.L.; Gouraud, I.; Mazoue, A.; Lamy, E.; Rocher, L.; Kapogiannis, D.; et al. The Effects of Confinement on Neuropsychiatric Symptoms in Alzheimer’s Disease During the COVID-19 Crisis. J. Alzheimers Dis. 2020, 76, 41–47. [Google Scholar] [CrossRef]
- El Haj, M.; Altintas, E.; Chapelet, G.; Kapogiannis, D.; Gallouj, K. High depression and anxiety in people with Alzheimer’s disease living in retirement homes during the covid-19 crisis. Psychiatry Res. 2020, 291, 113294. [Google Scholar] [CrossRef]
- Barguilla, A.; Fernández-Lebrero, A.; Estragués-Gázquez, I.; García-Escobar, G.; Navalpotro-Gómez, I.; Manero, R.M.; Puente-Periz, V.; Roquer, J.; Puig-Pijoan, A. Effects of COVID-19 Pandemic Confinement in Patients with Cognitive Impairment. Front Neurol. 2020, 11, 589901. [Google Scholar] [CrossRef] [PubMed]
- Mok, V.C.T.; Pendlebury, S.; Wong, A.; Alladi, S.; Au, L.; Bath, P.M.; Biessels, G.J.; Chen, C.; Cordonnier, C.; Dichgans, M.; et al. Tackling challenges in care of Alzheimer’s disease and other dementias amid the COVID-19 pandemic, now and in the future. Alzheimers Dement. 2020, 16, 1571–1581. [Google Scholar] [CrossRef] [PubMed]
- Simonetti, A.; Pais, C.; Jones, M.; Cipriani, M.C.; Janiri, D.; Monti, L.; Landi, F.; Bernabei, R.; Liperoti, R.; Sani, G. Neuropsychiatric Symptoms in Elderly With Dementia During COVID-19 Pandemic: Definition, Treatment, and Future Directions. Front. Psychiatry 2020, 11, 579842. [Google Scholar] [CrossRef] [PubMed]
- Manca, R.; De Marco, M.; Venneri, A. The Impact of COVID-19 Infection and Enforced Prolonged Social Isolation on Neuropsychiatric Symptoms in Older Adults With and Without Dementia: A Review. Front. Psychiatry 2020, 11, 585540. [Google Scholar] [CrossRef] [PubMed]
- Gil, R.; Arroyo-Anlló, E.M. Alzheimer’s Disease and Face Masks in Times of COVID-19. J. Alzheimer’s Dis. 2021, 79, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Killen, A.; Olsen, K.; McKeith, I.G.; Thomas, A.J.; O’Brien, J.T.; Donaghy, P.; Taylor, J. The challenges of COVID -19 for people with dementia with Lewy bodies and family caregivers. Int. J. Geriatr. Psychiatry 2020, 35, 1431–1436. [Google Scholar] [CrossRef]
- Migliaccio, R.; Bouzigues, A. Dementia and COVID-19 Lockdown: More Than a Double Blow for Patients and Caregivers. J. Alzheimers Dis. Rep. 2020, 4, 231–235. [Google Scholar] [CrossRef]
- Sm-Rahman, A.; Lo, C.H.; Ramic, A.; Jahan, Y. Home-Based Care for People with Alzheimer’s Disease and Related Dementias (ADRD) during COVID-19 Pandemic: From Challenges to Solutions. Int. J. Environ. Res. Public Health 2020, 17, 9303. [Google Scholar] [CrossRef]
- Tousi, B. Dementia Care in the Time of COVID-19 Pandemic. J. Alzheimers Dis. 2020, 76, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Canevelli, M.; Bruno, G.; Cesari, M. Providing Simultaneous COVID-19—Sensitive and Dementia-Sensitive Care as We Transition from Crisis Care to Ongoing Care. J. Am. Med. Dir. Assoc. 2020, 21, 968–969. [Google Scholar] [CrossRef]
- Brown, E.E.; Kumar, S.; Rajji, T.K.; Pollock, B.G.; Mulsant, B.H. Anticipating and Mitigating the Impact of the COVID-19 Pandemic on Alzheimer’s Disease and Related Dementias. Am. J. Geriatr. Psychiatry 2020, 28, 712–721. [Google Scholar] [CrossRef]
- Shea, Y.F.; Wan, W.H.; Chan, M.M.K.; DeKosky, S.T. Time-to-change: Dementia care in COVID-19. Psychogeriatrics 2020, 20, 792–793. [Google Scholar] [CrossRef]
- Wang, H.; Li, T.; Barbarino, P.; Gauthier, S.; Brodaty, H.; Molinuevo, J.L.; Xie, H.; Sun, Y.; Yu, E.; Tang, Y.; et al. Dementia care during COVID-19. Lancet 2020, 395, 1190–1191. [Google Scholar] [CrossRef]
- Korczyn, A.D. Dementia in the COVID-19 Period. J. Alzheimers Dis. 2020, 75, 1071–1072. [Google Scholar] [CrossRef]
- Velayudhan, L.; Aarsland, D.; Ballard, C. Mental health of people living with dementia in care homes during COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1253–1254. [Google Scholar] [CrossRef]
- Padala, S.P.; Jendro, A.M.; Orr, L.C. Facetime to reduce behavioral problems in a nursing home resident with Alzheimer’s dementia during COVID-19. Psychiatry Res. 2020, 288, 113028. [Google Scholar] [CrossRef] [PubMed]
- El Haj, M.; Larøi, F.; Gallouj, K. Hallucinations in a Patient with Alzheimer’s Disease During the COVID-19 Crisis: A Case Study. J. Alzheimers Dis. Rep. 2020, 4, 455–458. [Google Scholar] [CrossRef]
- Giebel, C.; Cannon, J.; Hanna, K.; Butchard, S.; Eley, R.; Gaughan, A.; Komuravelli, A.; Shenton, J.; Callaghan, S.; Tetlow, H.; et al. Impact of COVID-19 related social support service closures on people with dementia and unpaid carers: A qualitative study. Aging Ment. Health 2021, 25, 1281–1288. [Google Scholar] [CrossRef]
- Giebel, C.; Lord, K.; Cooper, C.; Shenton, J.; Cannon, J.; Pulford, D.; Shaw, L.; Gaughan, A.; Tetlow, H.; Butchard, S.; et al. A UK survey of COVID-19 related social support closures and their effects on older people, people with dementia, and carers. Int. J. Geriatr. Psychiatry 2021, 36, 393–402. [Google Scholar] [CrossRef]
- Spalletta, G.; Porcari, D.E.; Banaj, N.; Ciullo, V.; Palmer, K. Effects of COVID-19 Infection Control Measures on Appointment Cancelation in an Italian Outpatient Memory Clinic. Front. Psychiatry 2020, 11, 599844. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; She, R.; Qin, P.; Kershenbaum, A.; Fernandez-Egea, E.; Nelder, J.R.; Ma, C.; Lewis, J.; Wang, C.; Cardinal, R.N. The Medium-Term Impact of COVID-19 Lockdown on Referrals to Secondary Care Mental Health Services: A Controlled Interrupted Time Series Study. Front Psychiatry. 2020, 11, 585915. [Google Scholar] [CrossRef] [PubMed]
- Michalowsky, B.; Hoffmann, W.; Bohlken, J.; Kostev, K. Effect of the COVID-19 lockdown on disease recognition and utilisation of healthcare services in the older population in Germany: A cross-sectional study. Age Ageing 2021, 50, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Ousset, P.J.; Vellas, B. Viewpoint: Impact of the Covid-19 Outbreak on the Clinical and Research Activities of Memory Clinics: An Alzheimer’s Disease Center Facing the Covid-19 Crisis. J. Prev. Alzheimers Dis. 2020, 7, 197–198. [Google Scholar] [PubMed]
- Barros, D.; Borges-Machado, F.; Ribeiro, O.; Carvalho, J. Dementia and COVID-19: The Ones Not to Be Forgotten. Am. J. Alzheimers Dis. Other Dement. 2020, 35, 1533317520947505. [Google Scholar] [CrossRef] [PubMed]
- Goodman-Casanova, J.M.; Dura-Perez, E.; Guzman-Parra, J.; Cuesta-Vargas, A.; Mayoral-Cleries, F. Telehealth Home Support During COVID-19 Confinement for Community-Dwelling Older Adults With Mild Cognitive Impairment or Mild Dementia: Survey Study. J. Med. Internet Res. 2020, 22, e19434. [Google Scholar] [CrossRef] [PubMed]
- Benaque, A.; Gurruchaga, M.J.; Abdelnour, C.; Hernández, I.; Cañabate, P.; Alegret, M.; Rodríguez, I.; Rosende-Roca, M.; Tartari, J.P.; Esteban, E.; et al. Dementia Care in Times of COVID-19: Experience at Fundació ACE in Barcelona, Spain. J. Alzheimers Dis. 2020, 76, 33–40. [Google Scholar] [CrossRef]
- Lai, F.H.-Y.; Yan, E.W.-H.; Yu, K.K.-Y.; Tsui, W.-S.; Chan, D.T.-H.; Yee, B.K. The Protective Impact of Telemedicine on Persons With Dementia and Their Caregivers During the COVID-19 Pandemic. Am. J. Geriatr. Psychiatry 2020, 28, 1175–1184. [Google Scholar] [CrossRef] [PubMed]
- Geddes, M.R.; O’Connell, M.E.; Fisk, J.D.; Gauthier, S.; Camicioli, R.; Ismail, Z. Remote cognitive and behavioral assessment: Report of the Alzheimer Society of Canada Task Force on dementia care best practices for COVID-19. Alzheimers Dement. Diagn. Assess. Dis. Monit. 2020, 12, e12111. [Google Scholar] [CrossRef] [PubMed]
- Sekhon, H.; Sekhon, K.; Launay, C.; Afililo, M.; Innocente, N.; Vahia, I.; Rej, S.; Beauchet, O. Telemedicine and the rural dementia population: A systematic review. Maturitas 2021, 143, 105–114. [Google Scholar] [CrossRef]
- Cheung, G.; Peri, K. Challenges to dementia care during COVID-19: Innovations in remote delivery of group Cognitive Stimulation Therapy. Aging Ment. Health 2021, 25, 977–979. [Google Scholar] [CrossRef]
- Dai, R.; Spector, A.; Wong, G. e-Mental health care for people living with dementia: A lesson on digital equality from COVID-19. Alzheimers Dement. Diagn. Assess. Dis. Monit. 2020, 12, e12100. [Google Scholar] [CrossRef] [PubMed]
- Dourado, M.C.N.; Belfort, T.; Monteiro, A.; De Lucena, A.T.; Lacerda, I.B.; Gaigher, J.; Baptista, M.A.T.; Brandt, M.; Kimura, N.R.; De Souza, N.; et al. COVID-19: Challenges for dementia care and research. Dement. Neuropsychology 2020, 14, 340–344. [Google Scholar] [CrossRef]
- Rais, N.C.; Au, L.; Tan, M. COVID-19 Impact in Community Care—A Perspective on Older Persons with Dementia in Singapore. J. Am. Med. Dir. Assoc. 2020, 21, 997. [Google Scholar] [CrossRef]
- Ibanez, A.; Santamaria-Garcia, H.; Guerrero Barragan, A.; Kornhuber, A.; Ton, A.M.M.; Slachevsky, A.; Teixeira, A.L.; Meza, B.M.M.; Serrano, C.M.; Cano, C.; et al. The impact of SARS-CoV-2 in dementia across Latin America: A call for an urgent regional plan and coordinated response. Alzheimers Dement. 2020, 6, e12092. [Google Scholar]
- Desai, A.K.; Grossberg, G.T.; Sheth, D.N. Activities of daily living in patients with dementia: Clinical relevance, methods of assessment and effects of treatment. CNS Drugs 2004, 18, 853–875. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.-C.; Barbu, M.-G.; Beiu, C.; Popa, L.G.; Mihai, M.M.; Berteanu, M.; Popescu, M.N. The Impact of COVID-19 Pandemic on Long-Term Care Facilities Worldwide: An Overview on International Issues. BioMed. Res. Int. 2020, 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Koonin, L.M.; Hoots, B.; Tsang, C.A.; Leroy, Z.; Farris, K.; Jolly, B.; Antall, P.; McCabe, B.; Zelis, C.B.; Tong, I.; et al. Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic—United States, January–March 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, N.E.; Wallick, A.; Brown, L.M. Impact of COVID-19 pandemic restrictions on community-dwelling caregivers and persons with dementia. Psychol. Trauma Theory Res. Pr. Policy 2020, 12, S220–S221. [Google Scholar] [CrossRef]
- Vaitheswaran, S.; Lakshminarayanan, M.; Ramanujam, V.; Sargunan, S.; Venkatesan, S. Experiences and Needs of Caregivers of Persons With Dementia in India During the COVID-19 Pandemic—A Qualitative Study. Am. J. Geriatr. Psychiatry 2020, 28, 1185–1194. [Google Scholar] [CrossRef]
- Rainero, I.; Bruni, A.C.; Marra, C.; Cagnin, A.; Bonanni, L.; Cupidi, C.; Laganà, V.; Rubino, E.; Vacca, A.; Di Lorenzo, R.; et al. The Impact of COVID-19 Quarantine on Patients with Dementia and Family Caregivers: A Nation-Wide Survey. Front. Aging Neurosci. 2021, 12, 625781. [Google Scholar] [CrossRef]
- Iodice, F.; Cassano, V.; Rossini, P.M. Direct and indirect neurological, cognitive, and behavioral effects of COVID-19 on the healthy elderly, mild-cognitive-impairment, and Alzheimer’s disease populations. Neurol. Sci. 2021, 42, 455–465. [Google Scholar] [CrossRef]
- Suárez-González, A.; Rajagopalan, J.; Livingston, G.; Alladi, S. The effect of Covid-19 isolation measures on the cognition and mental health of people living with dementia: A rapid systematic review of one year of evidence. Medicine 2021, preprint. [Google Scholar] [CrossRef]
- Liu, K.Y.; Howard, R.; Banerjee, S.; Comas-Herrera, A.; Goddard, J.; Knapp, M.; Livingston, G.; Manthorpe, J.; O’Brien, J.T.; Paterson, R.W.; et al. Dementia wellbeing and COVID-19: Review and expert consensus on current research and knowledge gaps. Int. J. Geriatr. Psychiatry 2021. [Google Scholar] [CrossRef] [PubMed]
- Bacsu, J.R.; O’Connell, M.E.; Webster, C.; Poole, L.; Wighton, M.B.; Sivananthan, S. A scoping review of COVID-19 experiences of people living with dementia. Can. J. Public Health 2021, 112, 400–411. [Google Scholar] [CrossRef] [PubMed]
- Thyrian, J.R.; Kracht, F.; Nikelski, A.; Boekholt, M.; Schumacher-Schönert, F.; Rädke, A.; Michalowsky, B.; Vollmar, H.C.; Hoffmann, W.; Rodriguez, F.S.; et al. The situation of elderly with cognitive impairment living at home during lockdown in the Corona-pandemic in Germany. BMC Geriatr. 2020, 20, 540. [Google Scholar] [CrossRef] [PubMed]
- Sorbara, M.; Graviotto, H.; Lage-Ruiz, G.; Turizo-Rodriguez, C.; Sotelo-López, L.; Serra, A.; Gagliardi, C.; Heinemann, G.; Martinez, P.; Ces-Magliano, F.; et al. COVID-19 and the forgotten pandemic: Follow-up of neurocognitive disorders during lockdown in Argentina. Neurología 2021, 36, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Bacsu, J.-D.; E O’Connell, M.; Cammer, A.; Azizi, M.; Grewal, K.; Poole, L.; Green, S.; Sivananthan, S.; Spiteri, R.J. Using Twitter to Understand the COVID-19 Experiences of People With Dementia: Infodemiology Study. J. Med. Internet Res. 2021, 23, e26254. [Google Scholar] [CrossRef]
- Roach, P.; Zwiers, A.; Cox, E.; Fischer, K.; Charlton, A.; Josephson, C.B.; Patten, S.B.; Seitz, D.; Ismail, Z.; E Smith, E. Understanding the impact of the COVID-19 pandemic on well-being and virtual care for people living with dementia and care partners living in the community. Dementia 2020, 2021. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dellazizzo, L.; Léveillé, N.; Landry, C.; Dumais, A. Systematic Review on the Mental Health and Treatment Impacts of COVID-19 on Neurocognitive Disorders. J. Pers. Med. 2021, 11, 746. https://doi.org/10.3390/jpm11080746
Dellazizzo L, Léveillé N, Landry C, Dumais A. Systematic Review on the Mental Health and Treatment Impacts of COVID-19 on Neurocognitive Disorders. Journal of Personalized Medicine. 2021; 11(8):746. https://doi.org/10.3390/jpm11080746
Chicago/Turabian StyleDellazizzo, Laura, Nayla Léveillé, Clara Landry, and Alexandre Dumais. 2021. "Systematic Review on the Mental Health and Treatment Impacts of COVID-19 on Neurocognitive Disorders" Journal of Personalized Medicine 11, no. 8: 746. https://doi.org/10.3390/jpm11080746
APA StyleDellazizzo, L., Léveillé, N., Landry, C., & Dumais, A. (2021). Systematic Review on the Mental Health and Treatment Impacts of COVID-19 on Neurocognitive Disorders. Journal of Personalized Medicine, 11(8), 746. https://doi.org/10.3390/jpm11080746





