Prevalence and Significance of Pyuria in Chronic Kidney Disease Patients in Saudi Arabia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Pyuric CKD Patients Are in Later Stages of CKD and Could Present with UTI Compared to Non-Pyuric Patients
3.3. Several Bacterial Species Were Associated with UTI in 22 Pyuric CKD Patients with E. coli Being the Most Common Causative Agent
3.4. Pyuric CKD Patients Diagnosed with UTI Have Increased Numbers of Urinary WBCs and Are in Later Stages of CKD Compared to Sterile Pyuric CKD Patients
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Couser, W.; Remuzzi, G.; Mendis, S.; Tonelli, M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011, 80, 1258–1270. [Google Scholar] [CrossRef] [Green Version]
- Collaboration, G.C.K.D. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef] [Green Version]
- Alsuwaida, A.O.; Farag, Y.M.K.; Al Sayyari, A.A.; Mousa, D.; Alhejaili, F.; Al-Harbi, A.; Housawi, A.; Mittal, B.V.; Singh, A.K. Epidemiology of chronic kidney disease in the Kingdom of Saudi Arabia (SEEK-Saudi investigators)—A pilot study. Saudi J. Kidney Dis. Transplant. Off. Publ. Saudi Cent. Organ Transplant. Saudi Arab. 2010, 21, 1066–1072. [Google Scholar]
- Kuo, I.C.; Lee, J.J.; Hwang, D.Y.; Lim, L.M.; Lin, H.Y.H.; Hwang, S.J.; Chen, H.C.; Hung, C.C. Pyuria, urinary tract infection and renal outcome in patients with chronic kidney disease stage 3–5. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Syed-Ahmed, M.; Narayanan, M. Immune Dysfunction and Risk of Infection in Chronic Kidney Disease. Adv. Chronic Kidney Dis. 2019, 26, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Dalrymple, L.S.; Go, A.S. Epidemiology of acute infections among patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1487–1493. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, E.R.; Tashkandi, M.A.; Nahrir, S.; Maulana, A. Retrospective analysis of factors affecting the progression of chronic renal failure in adult polycystic kidney disease. Saudi J. Kidney Dis. Transpl. 2006, 17, 511–515. [Google Scholar] [PubMed]
- Hwang, J.H.; Park, H.C.; Jeong, J.C.; Ha Baek, S.; Han, M.Y.; Bang, K.; Cho, J.Y.; Yu, S.H.; Yang, J.; Oh, K.H.; et al. Chronic asymptomatic pyuria precedes overt urinary tract infection and deterioration of renal function in autosomal dominant polycystic kidney disease. BMC Nephrol. 2013, 14, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Lees, J.A.; Falk, R.M.; Stone, W.J.; McDougal, W.S. Pyocystis, pyonephrosis and perinephric abscess in end stage renal disease. J. Urol. 1985, 134, 716–719. [Google Scholar] [CrossRef]
- Kwon, Y.E.; Oh, D.J.; Kim, M.J.; Choi, H.M. Prevalence and Clinical Characteristics of Asymptomatic Pyuria in Chronic Kidney Disease. Ann. Lab. Med. 2020, 40, 238–244. [Google Scholar] [CrossRef]
- Wise, G.J.; Schlegel, P.N. Sterile Pyuria. N. Engl. J. Med. 2015, 372, 1048–1054. [Google Scholar] [CrossRef]
- Cabaluna, C.C.; Gary, N.E.; Eisinger, R.P. Urinalysis in patients on chronic hemodialysis. Urology 1977, 10, 103–104. [Google Scholar] [CrossRef]
- Fasolo, L.R.; Rocha, L.M.; Campbell, S.; Peixoto, A.J. Diagnostic relevance of pyuria in dialysis patients. Kidney Int. 2006, 70, 2035–2038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaudhry, A.; Stone, W.J.; Breyer, J.A. Occurrence of pyuria and bacteriuria in asymptomatic hemodialysis patients. Am. J. kidney Dis. Off. J. Natl. Kidney Found. 1993, 21, 180–183. [Google Scholar] [CrossRef]
- Orłowska, A.; Majdan, M.; Kozioł-Montewka, M.; Grzebalska, A.; Swatowski, A. Asymptomatic bacteriuria in patients on continuous ambulatory peritoneal dialysis. Ann. Univ. Mariae Curie-Sklodowska. Med. 2002, 57, 285–289. [Google Scholar] [PubMed]
- Hyodo, T.; Yoshida, K.; Sakai, T.; Baba, S. Asymptomatic hyperleukocyturia in hemodialysis patients analyzed by the automated urinary flow cytometer. Ther. Apher. Dial. Off. Peer-Rev. J. Int. Soc. Apher. Jpn. Soc. Apher. Jpn. Soc. Dial. Ther. 2005, 9, 402–406. [Google Scholar] [CrossRef]
- Firestein, G.S. Evolving concepts of rheumatoid arthritis. Nature 2003, 423, 356–361. [Google Scholar] [CrossRef]
- Oikonomou, K.G.; Alhaddad, A. The Diagnostic Value of Urinalysis in Hemodialysis Patients with Fever, Sepsis or Suspected Urinary Tract Infection. J. Clin. Diagn. Res. 2016, 10, OC11–OC13. [Google Scholar] [CrossRef] [PubMed]
- Pagels, A.A.; Söderkvist, B.K.; Medin, C.; Hylander, B.; Heiwe, S. Health-related quality of life in different stages of chronic kidney disease and at initiation of dialysis treatment. Health Qual. Life Outcomes 2012, 10, 71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schrier, R.W.; Gottschalk, C.W. Diseases of the Kidney Fourth Edition Volume 1; Little Brown and Company: Boston, MA, USA, 1988. [Google Scholar]
- Ojo, A. Addressing the global burden of chronic kidney disease through clinical and translational research. Trans. Am. Clin. Climatol. Assoc. 2014, 125, 226–229. [Google Scholar]
- James, M.T.; Hemmelgarn, B.R.; Tonelli, M. Early recognition and prevention of chronic kidney disease. Lancet 2010, 375, 1296–1309. [Google Scholar] [CrossRef]
- Levin, A.; Tonelli, M.; Bonventre, J.; Coresh, J.; Donner, J.-A.; Fogo, A.B.; Fox, C.S.; Gansevoort, R.T.; Heerspink, H.J.L.; Jardine, M.; et al. Global kidney health 2017 and beyond: A roadmap for closing gaps in care, research, and policy. Lancet 2017, 390, 1888–1917. [Google Scholar] [CrossRef]
- Gilbert, D.N. Urinary tract infections in patients with chronic renal insufficiency. Clin. J. Am. Soc. Nephrol. 2006, 1, 327–331. [Google Scholar] [CrossRef]
- Chawla, L.S.; Eggers, P.W.; Star, R.A.; Kimmel, P.L. Acute kidney injury and chronic kidney disease as interconnected syndromes. N. Engl. J. Med. 2014, 371, 58–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ronco, C.; Bellomo, R.; Kellum, J.A. Acute kidney injury. Lancet 2019, 394, 1949–1964. [Google Scholar] [CrossRef]
- Chen, H.-S.; Su, L.-T.; Lin, S.-Z.; Sung, F.-C.; Ko, M.-C.; Li, C.-Y. Increased risk of urinary tract calculi among patients with diabetes mellitus—A population-based cohort study. Urology 2012, 79, 86–92. [Google Scholar] [CrossRef]
| Patients’ Characteristics | N = 754 56 ± 17 | ||
|---|---|---|---|
| Age (Years; Mean ± SD) | |||
| N | % | ||
| Gender | Male | 472 | 62.6 |
| Female | 282 | 37.4 | |
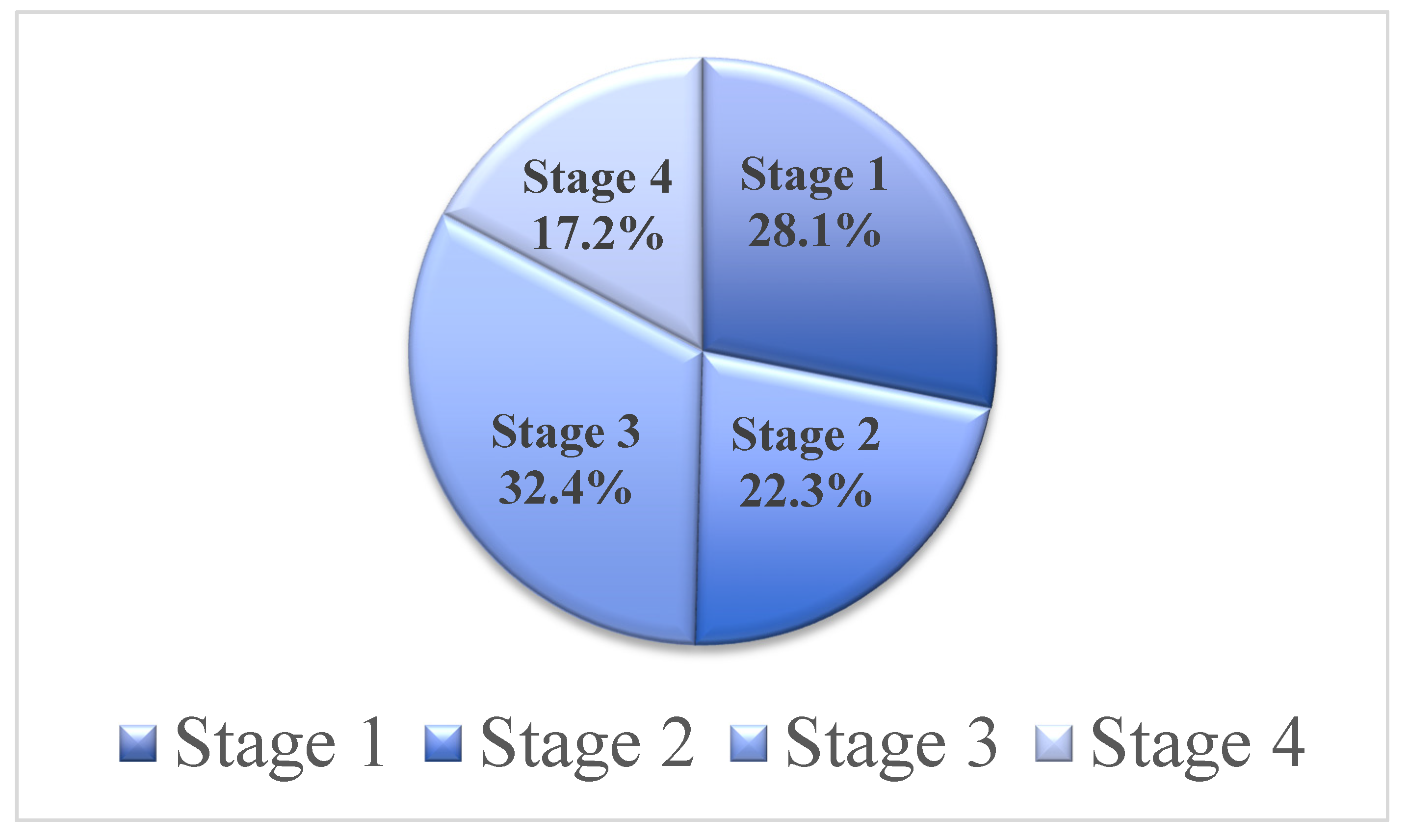
| CKD Stage | Stage 1 | 212 | 28.1 |
| Stage 2 | 168 | 22.3 | |
| Stage 3 | 244 | 32.4 | |
| Stage 4 | 130 | 17.2 | |
| Diabetes | 433 | 57.4 | |
| Hypertension | 564 | 74.8 | |
| Albuminuria | 366 | 48.5 | |
| Hematuria | 153 | 20.3 | |
| Urinary Tract Infection (UTI) | 22 | 2.9 | |
| Urinary Leukocyte Esterase | 125 | 16.6 | |
| Urinary Nitrite | 17 | 2.3 | |
| Mean ± SD | |||
| Serum Urea (mmol/L) | 10.8 ± 7.9 | ||
| Serum Creatinine (μmol/L) | 192.5 ± 146.2 | ||
| Hemoglobin (g/dL) | 13.02± 2.23 | ||
| Variables | No Pyuria N = 590 | Pyuria N = 164 | p-Value | |||
|---|---|---|---|---|---|---|
| Age (years; mean ± SD) | 56.2 ± 16 | 53.2 ± 19.5 | 0.151 | |||
| N | % | N | % | |||
| Gender | Male | 421 | 71.4 | 51 | 31.1 | 0.001 |
| Female | 169 | 28.6 | 113 | 68.9 | ||
| CKD Stage | Stage 1 | 183 | 31 | 29 | 17.7 | 0.002 |
| Stage 2 | 137 | 23.2 | 31 | 18.9 | ||
| Stage 3 | 200 | 33.9 | 44 | 26.8 | ||
| Stage 4 | 70 | 11.9 | 60 | 36.6 | ||
| Diabetes | 353 | 59.8 | 80 | 48.8 | 0.008 | |
| Hypertension | 455 | 77.1 | 109 | 66.5 | 0.004 | |
| Albuminuria | 261 | 44.2 | 105 | 64 | 0.001 | |
| Hematuria | 81 | 13.7 | 72 | 43.9 | 0.004 | |
| Urinary Tract Infection (UTI) | 0 | 0 | 22 | 13.4 | 0.003 | |
| Urinary Leukocyte Esterase | 14 | 2.4 | 111 | 67.7 | 0.002 | |
| Urinary Nitrite | 4 | 0.7 | 13 | 7.9 | 0.002 | |
| Mean ± SD | ||||||
| Serum Urea (mmol/L) | 10 ± 6.7 | 13.8 ± 10.7 | 0.006 | |||
| Serum Creatinine (μmol/L) | 175.9 ± 136.9 | 252.5 ± 228.7 | 0.001 | |||
| Hemoglobin (g/dL) | 13.32 ± 2.209 | 11.98 ± 1.963 | 0.001 | |||
| Organism | Number of Patients |
|---|---|
| Acinetobacter lwoffii | 1 |
| Candida Species | 1 |
| Citrobacter freundii | 1 |
| E. coli | 10 |
| Staphylococcus aureus | 1 |
| Enterococcus fecalis | 2 |
| Klebsiella pneumoniae | 3 |
| Pseudomonas Aeruginosa | 2 |
| Salmonella Species | 1 |
| Total | 22 |
| Variables | UTI | Sterile Pyuria | p-Value | |||
|---|---|---|---|---|---|---|
| N = 22 | N = 142 | |||||
| Age (years; mean ± SD) | 55 ± 22 | 53 ± 19 | 0.095 | |||
| N | % | N | % | |||
| Gender | Males | 7 | 31.8 | 44 | 31 | 0.063 |
| Females | 15 | 68.2 | 98 | 69 | ||
| CKD Stage | Stage 1 | 2 | 9.1 | 27 | 19.1 | 0.004 |
| Stage 2 | 3 | 13.6 | 28 | 19.9 | ||
| Stage 3 | 6 | 27.3 | 38 | 27 | ||
| Stage 4 | 11 | 50 | 49 | 34.5 | ||
| Urinary WBCs/HPF | 5–9 | 4 | 18.2 | 44 | 31 | 0.002 |
| 10–19 | 3 | 13.6 | 39 | 27.5 | ||
| 20–49 | 1 | 4.6 | 31 | 21.8 | ||
| >50 | 14 | 63.6 | 28 | 19.7 | ||
| Diabetes | 12 | 54.5 | 68 | 44.7 | 0.6 | |
| Hypertension | 13 | 59.1 | 96 | 67.6 | 0.44 | |
| Albuminuria | 14 | 63.6 | 91 | 64.1 | 0.353 | |
| Hematuria | 8 | 36.4 | 64 | 45.1 | 0.037 | |
| Urinary Nitrite | 4 | 18.2 | 9 | 6.3 | 0.003 | |
| Urinary Leukocyte Esterase | 19 | 86.4 | 92 | 64.8 | 0.002 | |
| Mean ± SD | ||||||
| Serum Urea (mmol/L) | 17.1 ± 10.4 | 13.3 ± 10.7 | 0.072 | |||
| Serum Creatinine (μmol/L) | 269.05 ± 206.62 | 250.08 ± 232.49 | 0.061 | |||
| Hemoglobin (g/dL) | 13.08 ± 2.212 | 11.27 ± 2.021 | 0.121 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almaiman, L.; Allemailem, K.S.; El-Kady, A.M.; Alrasheed, M.; Almatroudi, A.; Alekezem, F.S.; Elrasheedy, A.; Al-Megrin, W.A.; Alobaid, H.M.; Elshabrawy, H.A. Prevalence and Significance of Pyuria in Chronic Kidney Disease Patients in Saudi Arabia. J. Pers. Med. 2021, 11, 831. https://doi.org/10.3390/jpm11090831
Almaiman L, Allemailem KS, El-Kady AM, Alrasheed M, Almatroudi A, Alekezem FS, Elrasheedy A, Al-Megrin WA, Alobaid HM, Elshabrawy HA. Prevalence and Significance of Pyuria in Chronic Kidney Disease Patients in Saudi Arabia. Journal of Personalized Medicine. 2021; 11(9):831. https://doi.org/10.3390/jpm11090831
Chicago/Turabian StyleAlmaiman, Lina, Khaled S. Allemailem, Asmaa M. El-Kady, Mishaal Alrasheed, Ahmad Almatroudi, Fahad S. Alekezem, Abdelrahman Elrasheedy, Wafa Abdullah Al-Megrin, Hussah M. Alobaid, and Hatem A. Elshabrawy. 2021. "Prevalence and Significance of Pyuria in Chronic Kidney Disease Patients in Saudi Arabia" Journal of Personalized Medicine 11, no. 9: 831. https://doi.org/10.3390/jpm11090831
APA StyleAlmaiman, L., Allemailem, K. S., El-Kady, A. M., Alrasheed, M., Almatroudi, A., Alekezem, F. S., Elrasheedy, A., Al-Megrin, W. A., Alobaid, H. M., & Elshabrawy, H. A. (2021). Prevalence and Significance of Pyuria in Chronic Kidney Disease Patients in Saudi Arabia. Journal of Personalized Medicine, 11(9), 831. https://doi.org/10.3390/jpm11090831








