Potential Use of Pharmacogenetics to Reduce Drug-Induced Syndrome of Inappropriate Antidiuretic Hormone (SIADH)
Abstract
:1. Background
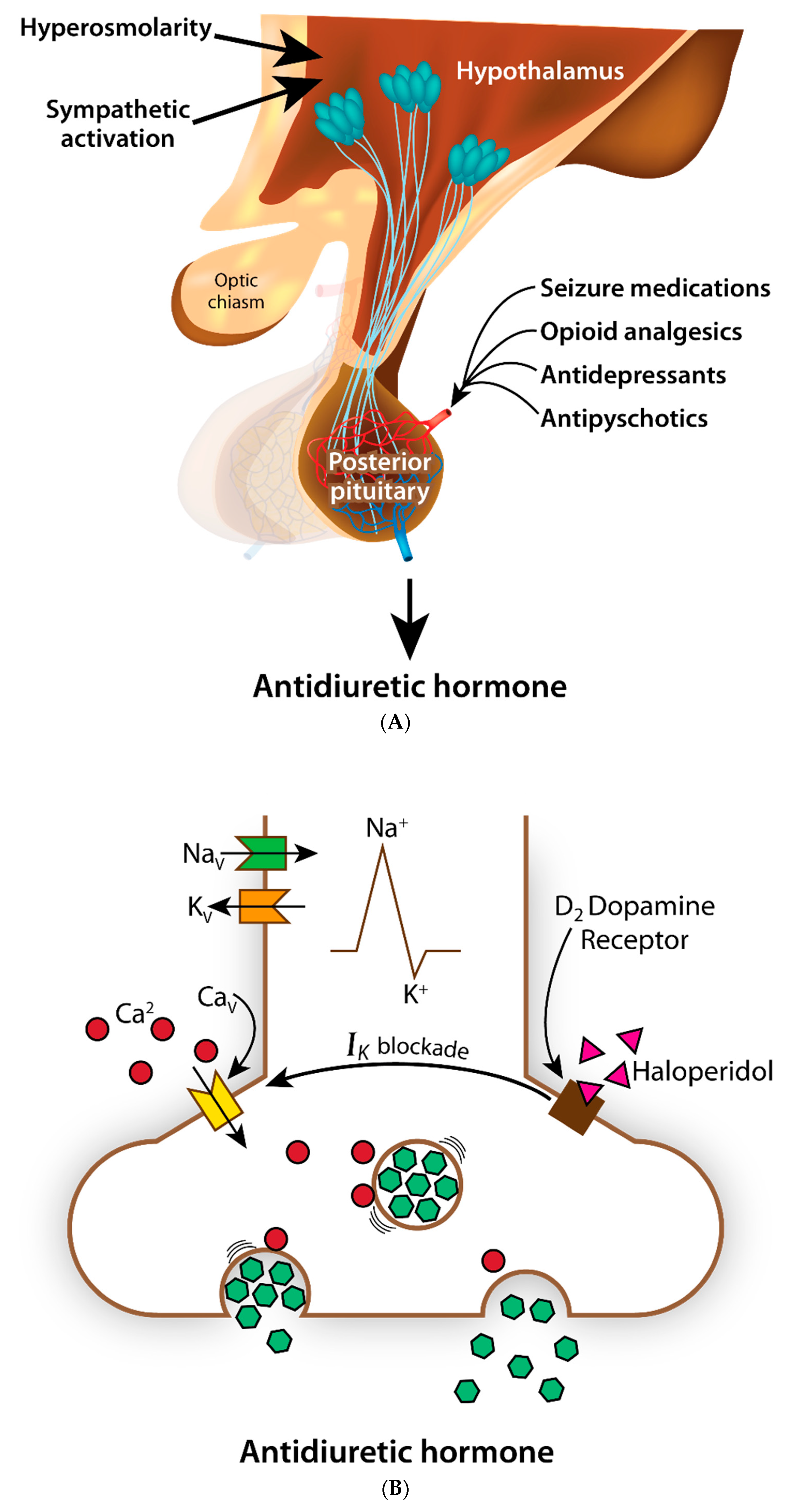
2. Excessive Antidiuretic Hormone
3. SIADH as an Adverse Drug Reaction
4. Importance of Establishing Mechanism
5. The Need for Risk Stratification
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Hoorn, E.J.; Zietse, R. Diagnosis and treatment of hyponatremia: Compilation of the guidelines. J. Am. Soc. Nephrol. 2017, 28, 1340–1349. [Google Scholar] [CrossRef] [PubMed]
- Peri, A. Management of hyponatremia: Causes, clinical aspects, differential diagnosis and treatment. Expert Rev. Endocrinol. Metab. 2019, 14, 13–21. [Google Scholar] [CrossRef]
- Burst, V. Etiology and epidemiology of hyponatremia. Front. Horm. Res. 2019, 52, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Berni, A.; Malandrino, D.; Corona, G.; Maggi, M.; Parenti, G.; Fibbi, B.; Poggesi, L.; Bartoloni, A.; Lavorini, F.; Fanelli, A.; et al. Serum sodium alterations in SARS CoV-2 (COVID-19) infection: Impact on patient outcome. Eur. J. Endocrinol. 2021, 185, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Sterns, R.H.; Silver, S.M. Complications and management of hyponatremia. Curr. Opin. Nephrol. Hypertens. 2016, 25, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, C.R.; Hammouda, N.; Linton, E.A.; Doering, M.; Ohuabunwa, U.K.; Ko, K.J.; Hung, W.W.; Shah, M.N.; Lindquist, L.A.; Biese, K.; et al. Delirium Prevention, Detection, and Treatment in Emergency Medicine Settings: A Geriatric Emergency Care Applied Research (GEAR) Network Scoping Review and Consensus Statement. Acad. Emerg. Med. 2021, 28, 19–35. [Google Scholar] [CrossRef]
- Hoel, R.W.; Giddings Connolly, R.M.; Takahashi, P.Y. Polypharmacy management in older patients. Mayo Clin. Proc. 2021, 96, 242–256. [Google Scholar] [CrossRef] [PubMed]
- Mannesse, C.K.; Vondeling, A.M.; van Marum, R.J.; van Solinge, W.W.; Egberts, T.C.; Jansen, P.A. Prevalence of hyponatremia on geriatric wards compared to other settings over four decades: A systematic review. Ageing Res. Rev. 2013, 12, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Boyer S, Gayot C, Bimou C, Mergans T, Kajeu P, Castelli M, Dantoine T, Tchalla A. Prevalence of mild hyponatremia and its association with falls in older adults admitted to an emergency geriatric medicine unit (the MUPA unit). BMC Geriatr. 2019, 19, 265. [Google Scholar] [CrossRef] [Green Version]
- Ramírez, E.; Rodríguez, A.; Queiruga, J.; García, I.; Díaz, L.; Martínez, L.; Muñoz, R.; Muñoz, M.; Tong, H.Y.; Martínez, J.C.; et al. Severe Hyponatremia Is Often Drug Induced: 10-Year Results of a Prospective Pharmacovigilance Program. Clin. Pharmacol. Ther. 2019, 106, 1362–1379. [Google Scholar] [CrossRef] [PubMed]
- Oh, R.C.; Malave, B.; Chaltry, J.D. Collapse in the heat—From overhydration to the emergency room—Three cases of exercise-associated hyponatremia associated with exertional heat illness. Mil. Med. 2018, 183, e225–e228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez, M.; Hernandez, M.; Cheungpasitporn, W.; Kashani, K.B.; Riaz, I.; Rangaswami, J.; Herzog, E.; Guglin, M.; Krittanawong, C. Hyponatremia in Heart Failure: Pathogenesis and Management. Curr. Cardiol. Rev. 2019, 15, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Rotondo, F.; Butz, H.; Syro, L.V.; Yousef, G.M.; Di Ieva, A.; Restrepo, L.M.; Quintanar-Stephano, A.; Berczi, I.; Kovacs, K. Arginine vasopressin (AVP): A review of its historical perspectives, current research and multifunctional role in the hypothalamo-hypophysial system. Pituitary 2016, 19, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Sparapani, S.; Millet-Boureima, C.; Oliver, J.; Mu, K.; Hadavi, P.; Kalostian, T.; Ali, N.; Avelar, C.M.; Bardies, M.; Barrow, B.; et al. The Biology of Vasopressin. Biomedicines 2021, 9, 89. [Google Scholar] [CrossRef]
- Tudor, R.M.; Thompson, C.J. Posterior pituitary dysfunction following traumatic brain injury: Review. Pituitary 2019, 22, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Brault, C.; Flahaut, G.; Maizel, J.; Choukroun, G. Hyponatremia in a Patient with Central Nervous System Lymphoma. Am. J. Kidney Dis. 2016, 68, A17–A19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misra, U.K.; Kalita, J.; Tuberculous Meningitis International Research Consortium. Mechanism, spectrum, consequences and management of hyponatremia in tuberculous meningitis. Wellcome Open Res. 2021, 4, 189. [Google Scholar] [CrossRef]
- Schwartz, W.B.; Bennett, W.; Curelop, S.; Bartter, F.C. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am. J. Med. 1957, 23, 529–542. [Google Scholar] [CrossRef]
- Mazhar, F.; Pozzi, M.; Gentili, M.; Scatigna, M.; Clementi, E.; Radice, S.; Carnovale, C. Association of Hyponatraemia and Antidepressant Drugs: A Pharmacovigilance-Pharmacodynamic Assessment Through an Analysis of the US Food and Drug Administration Adverse Event Reporting System (FAERS) Database. CNS Drugs 2019, 33, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Spinler, S.A. Hyponatremia associated with selective serotonin-reuptake inhibitors in older adults. Ann. Pharmacother. 2006, 40, 1618–1622. [Google Scholar] [CrossRef] [PubMed]
- Mazhar, F.; Battini, V.; Pozzi, M.; Invernizzi, E.; Mosini, G.; Gringeri, M.; Capuano, A.; Scavone, C.; Radice, S.; Clementi, E.; et al. Hyponatremia Following Antipsychotic Treatment: In Silico Pharmacodynamics Analysis of Spontaneous Reports from the US Food and Drug Administration Adverse Event Reporting System Database and an Updated Systematic Review. Int. J. Neuropsychopharmacol. 2021, 24, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Wilke, R.A.; Hsu, S.F.; Jackson, M.B. Dopamine D4 receptor mediated inhibition of potassium current in neurohypophysial nerve terminals. J. Pharmacol. Exp. Ther. 1998, 284, 542–548. [Google Scholar]
- Lupardus, P.J.; Wilke, R.A.; Aydar, E.; Palmer, C.P.; Chen, Y.; Ruoho, A.E.; Jackson, M.B. Membrane-delimited coupling between sigma receptors and K+ channels in rat neurohypophysial terminals requires neither G-protein nor ATP. J Physiol. 2000, 526, 527–539. [Google Scholar] [CrossRef] [PubMed]
- Scott, V.; Bishop, V.R.; Leng, G.; Brown, C.H. Dehydration-induced modulation of kappa-opioid inhibition of vasopressin neurone activity. J Physiol. 2009, 587, 5679–5689. [Google Scholar] [CrossRef] [PubMed]
- Na, E.S.; Morris, M.J.; Johnson, A.K. Opioid mechanisms that mediate the palatability of and appetite for salt in sodium replete and deficient states. Physiol. Behav. 2012, 106, 164–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falhammar, H.; Calissendorff, J.; Skov, J.; Nathanson, D.; Lindh, J.D.; Mannheimer, B. Tramadol- and codeine-induced severe hyponatremia: A Swedish population-based case-control study. Eur. J. Int. Med. 2019, 69, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Seifert, J.; Letmaier, M.; Greiner, T.; Schneider, M.; Deest, M.; Eberlein, C.K.; Bleich, S.; Grohmann, R.; Sermin Toto, S. Psychotropic drug-induced hyponatremia: Results from a drug surveillance program—An update. J. Neural Transm. 2021, 128, 1249–1264. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Wang, X. Hyponatremia induced by antiepileptic drugs in patients with epilepsy. Expert Opin. Drug Saf. 2017, 16, 77–87. [Google Scholar] [CrossRef]
- Berghuis, B.; van der Palen, J.; de Haan, G.J.; Lindhout, D.; Koeleman, B.P.C.; Sander, J.W.; EpiPGX Consortium. Carbamazepine- and oxcarbazepine-induced hyponatremia in people with epilepsy. Epilepsia 2017, 58, 1227–1233. [Google Scholar] [CrossRef]
- Fricke-Galindo, I.; LLerena, A.; Jung-Cook, H.; López-López, M. Carbamazepine adverse drug reactions. Expert Rev. Clin. Pharmacol. 2018, 11, 705–718. [Google Scholar] [CrossRef]
- Chiu, C.Y.; Sarwal, A.; Azhar Munir, R.; Widjaja, M.; Khalid, A.; Khanna, R. Syndrome of inappropriate antidiuretic hormone (SIADH) induced by long-term use of citalopram and short-term use of naproxen. Am. J. Case Rep. 2020, 21, e926561. [Google Scholar] [CrossRef] [PubMed]
- Verzicco, I.; Regolisti, G.; Quaini, F.; Bocchi, P.; Brusasco, I.; Ferrari, M.; Passeri, G.; Cannone, V.; Coghi, P.; Fiaccadori, E.; et al. Electrolyte Disorders Induced by Antineoplastic Drugs. Front. Oncol. 2020, 10, 779. [Google Scholar] [CrossRef]
- Krishnamurthy, A.; Bhattacharya, S.; Lathia, T.; Kantroo, V.; Kalra, S.; Dutta, D. Anticancer medications and sodium dysmetabolism. Eur. Endocrinol. 2020, 16, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.F.; Zhao, S.F.; Du, Z.Q. Small cell carcinoma of the cervix complicated by syndrome of inappropriate antidiuretic hormone secretion: A case report. J. Int. Med. Res. 2021, 49, 300060520985657. [Google Scholar] [CrossRef]
- Shepshelovich, D.; Schechter, A.; Calvarysky, B.; Diker-Cohen, T.; Rozen-Zvi, B.; Gafter-Gvili, A. Medication-induced SIADH: Distribution and characterization according to medication class. Br. J. Clin. Pharmacol. 2017, 83, 1801–1807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liamis, G.; Megapanou, E.; Elisaf, M.; Milionis, H. Hyponatremia-Inducing Drugs. Front. Horm. Res. 2019, 52, 167–177. [Google Scholar] [CrossRef]
- Faiver, L.; Hensler, D.; Rush, S.C.; Kashlan, O.; Williamson, C.A.; Rajajee, V. Safety and Efficacy of 23.4% Sodium Chloride Administered via Peripheral Venous Access for the Treatment of Cerebral Herniation and Intracranial Pressure Elevation. Neurocrit. Care 2021. [Google Scholar] [CrossRef] [PubMed]
- Miell, J.; Dhanjal, P.; Jamookeeah, C. Evidence for the use of demeclocycline in the treatment of hyponatraemia secondary to SIADH: A systematic review. Int. J. Clin. Pract. 2015, 69, 1396–1417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarafidis, P.; Loutradis, C.; Ferro, C.J.; Ortiz, A. SGLT-2 Inhibitors to Treat Hyponatremia Associated with SIADH: A Novel Indication? Am. J. Nephrol. 2020, 51, 553–555. [Google Scholar] [CrossRef] [PubMed]
- Verbalis, J.G.; Goldsmith, S.R.; Greenberg, A.; Korzelius, C.; Schrier, R.W.; Sterns, R.H.; Thompson, C.J. Diagnosis, evaluation, and treatment of hyponatremia: Expert panel recommendations. Am. J. Med. 2013, 126, S1–S42. [Google Scholar] [CrossRef] [PubMed]
- Denny, J.C.; Rutter, J.L.; Goldstein, D.B.; Philippakis, A.; Smoller, J.W.; Jenkins, G.; Dishman, E.; All of Us Research Program Investigators. The “All of Us” Research Program. N. Engl. J. Med. 2019, 381, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Duong, B.Q.; Arwood, M.J.; Hicks, J.K.; Beitelshees, A.L.; Franchi, F.; Houder, J.T.; Limdi, N.A.; Cook, K.J.; Owusu Obeng, A.; Petry, N.; et al. Development of Customizable Implementation Guides to Support Clinical Adoption of Pharmacogenomics: Experiences of the Implementing GeNomics In pracTicE (IGNITE) Network. Pharm. Pers. Med. 2020, 13, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Timmons, A.K.; Korpak, A.M.; Tan, J.; Moore, K.P.; Liu, C.H.; Forsberg, C.W.; Goldberg, J.; Smith, N.L.; Cohen, D.M. Heritability and individuality of the plasma sodium concentration: A twin study in the United States veteran population. Am. J. Physiol. Renal. Physiol. 2019, 316, F1114–F1123. [Google Scholar] [CrossRef] [PubMed]
- Böger, C.A.; Gorski, M.; McMahon, G.M.; Xu, H.; Chang, Y.C.; van der Most, P.J.; Navis, G.; Nolte, I.M.; de Borst, M.H.; Zhang, W.; et al. NFAT5 and SLC4A10 loci associate with plasma osmolality. J. Am. Soc. Nephrol. 2017, 28, 2311–2321. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.S.; Wain, L.V.; Channavajjhala, S.K.; Jackson, V.E.; Edwards, E.; Lu, R.; Siew, K.; Jia, W.; Shrine, N.; Kinnear, S.; et al. Phenotypic and pharmacogenetic evaluation of patients with thiazide-induced hyponatremia. J. Clin. Investig. 2017, 127, 3367–3374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilke, R.A.; Reif, D.M.; Moore, J.H. Combinatorial pharmacogenetics. Nat. Rev. Drug Discov. 2005, 4, 911–918. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.P.H.; Christopoulos, A.; Davenport, A.P.; Kelly, E.; Mathie, A.; Peters, J.A.; Veale, E.L.; Armstrong, J.F.; Faccenda, E.; Harding, S.D.; et al. The concise guide to pharmacology 2019/20: G protein-coupled receptors. Br. J. Pharmacol. 2019, 176 (Suppl. 1), S21–S141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wentworth, K.; Hsing, A.; Urrutia, A.; Zhu, Y.; Horvai, A.E.; Bastepe, M.; Hsiao, E.C. A Novel T55A Variant of Gs alpha Associated with Impaired cAMP Production, Bone Fragility, and Osteolysis. Case Rep. Endocrinol. 2016, 2016, 2691385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hicks, J.K.; Bishop, J.R.; Sangkuhl, K.; Müller, D.J.; Ji, Y.; Leckband, S.G.; Leeder, J.S.; Graham, R.L.; Chiulli, D.L.; LLerena, A.; et al. Clinical Pharmacogenetics Implementation Consortium guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin. Pharmacol. Ther. 2015, 98, 127–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petry, N.; Lupu, R.A.; Gohar, A.; Larson, E.A.; Peterson, C.; Williams, V.; Zhao, J.; Wilke, R.A.; Hines, L. CYP2C19 genotype, physician prescribing pattern, and risk for long QT on SSRIs. Pharmacogenomics 2019, 20, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Hicks, J.K.; Bishop, J.R.; Gammal, R.S.; Sangkuhl, K.; Bousman, C.A.; Leeder, J.S.; Llerena, A.; Mueller, D.J.; Ramsey, L.B.; Scott, S.A.; et al. A Call for Clear and Consistent Communications Regarding the Role of Pharmacogenetics in Antidepressant Pharmacotherapy. Clin. Pharmacol. Ther. 2020, 107, 50–52. [Google Scholar] [CrossRef]
- Crews, K.R.; Gaedigk, A.; Dunnenberger, H.M.; Leeder, J.S.; Klein, T.E.; Caudle, K.E.; Haidar, C.E.; Shen, D.D.; Callaghan, J.T.; Sadhasivam, S.; et al. Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update. Clin. Pharmacol. Ther. 2014, 95, 376–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crews, K.R.; Monte, A.A.; Huddart, R.; Caudle, K.E.; Kharasch, E.D.; Gaedigk, A.; Dunnenberger, H.M.; Leeder, J.S.; Callaghan, J.T.; Samer, C.F.; et al. Clinical Pharmacogenetics Implementation Consortium Guideline for CYP2D6, OPRM1, and COMT Genotypes and Select Opioid Therapy. Clin. Pharmacol. Ther. 2021. [Google Scholar] [CrossRef] [PubMed]
- Caudle, K.E.; Rettie, A.E.; Whirl-Carrillo, M.; Smith, L.H.; Mintzer, S.; Lee, M.T.; Klein, T.E.; Callaghan, J.T.; Clinical Pharmacogenetics Implementation Consortium. Clinical pharmacogenetics implementation consortium guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing. Clin. Pharmacol. Ther. 2014, 96, 542–548. [Google Scholar] [CrossRef] [Green Version]
- Karnes, J.H.; Rettie, A.E.; Somogyi, A.A.; Huddart, R.; Fohner, A.E.; Formea, C.M.; Ta Michael Lee, M.; Llerena, A.; Whirl-Carrillo, M.; Klein, T.E.; et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2C9 and HLA-B Genotypes and Phenytoin Dosing: 2020 Update. Clin. Pharmacol. Ther. 2021, 109, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Cavallari, L.H.; Weitzel, K.W.; Elsey, A.R.; Liu, X.; Mosley, S.A.; Smith, D.M.; Staley, B.J.; Winterstein, A.G.; Mathews, C.A.; Franchi, F.; et al. University of Florida Health Personalized Medicine Program. Pharmacogenomics 2017, 18, 421–426. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilke, R.A. Potential Use of Pharmacogenetics to Reduce Drug-Induced Syndrome of Inappropriate Antidiuretic Hormone (SIADH). J. Pers. Med. 2021, 11, 853. https://doi.org/10.3390/jpm11090853
Wilke RA. Potential Use of Pharmacogenetics to Reduce Drug-Induced Syndrome of Inappropriate Antidiuretic Hormone (SIADH). Journal of Personalized Medicine. 2021; 11(9):853. https://doi.org/10.3390/jpm11090853
Chicago/Turabian StyleWilke, Russell A. 2021. "Potential Use of Pharmacogenetics to Reduce Drug-Induced Syndrome of Inappropriate Antidiuretic Hormone (SIADH)" Journal of Personalized Medicine 11, no. 9: 853. https://doi.org/10.3390/jpm11090853
APA StyleWilke, R. A. (2021). Potential Use of Pharmacogenetics to Reduce Drug-Induced Syndrome of Inappropriate Antidiuretic Hormone (SIADH). Journal of Personalized Medicine, 11(9), 853. https://doi.org/10.3390/jpm11090853




