Effect of Low or High Pressure Alveolar Recruitment Maneuver on Postoperative Pain and Quality of Recovery in Patients with Obesity Undergoing Laparoscopic Sleeve Gastrectomy
Abstract
1. Introduction
2. Materials and Methods
3. Results
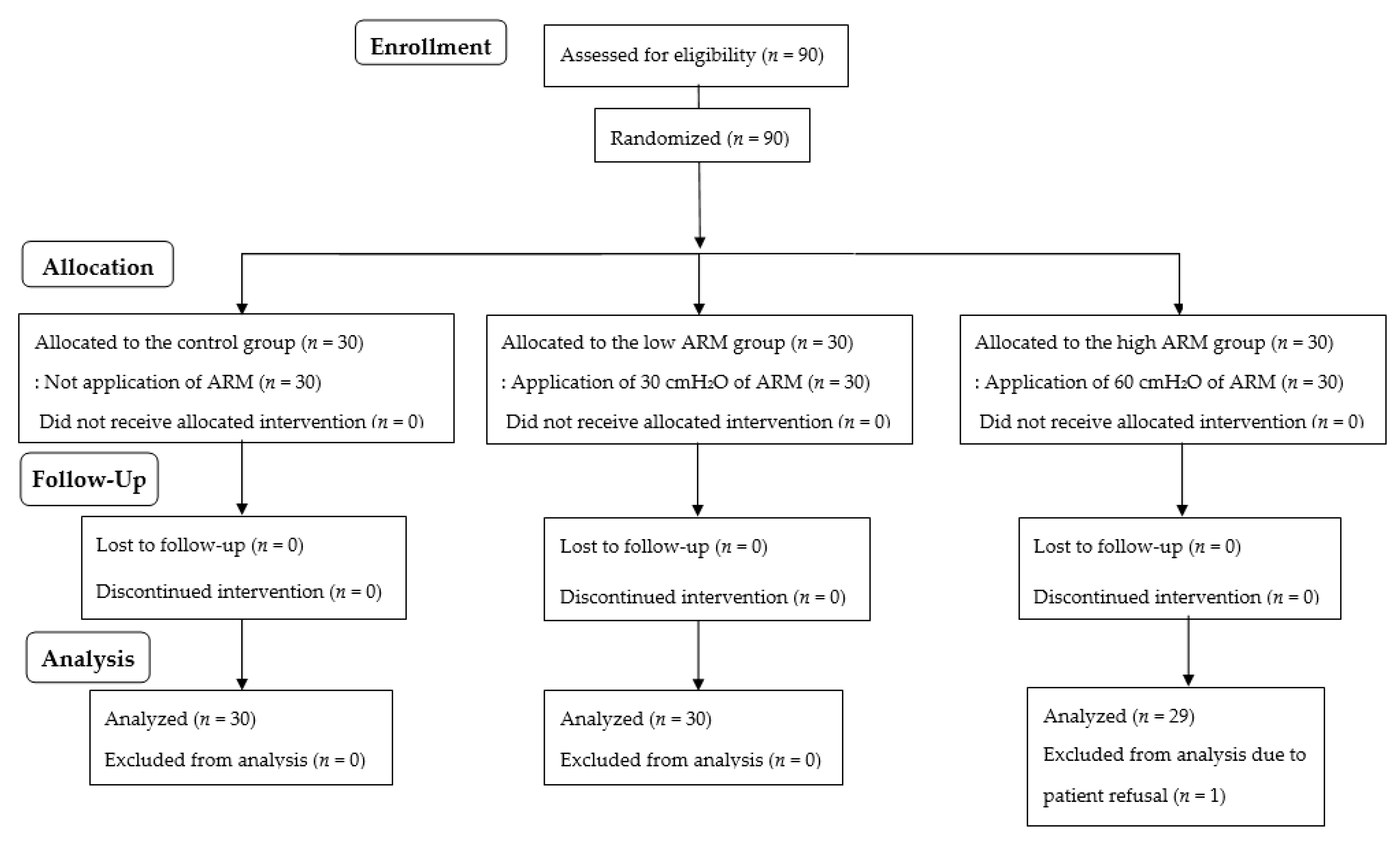
3.1. Participants
3.2. Intraoperative Hemodynamic Changes
3.3. PACU Data
3.4. Postoperative Pain and QoR40 Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, X.; Li, K. Time characteristics of shoulder pain after laparoscopic surgery. JSLS 2021, 25, e2021.00027. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Song, T.; Kim, K.H.; Lee, K.W. Incidence, natural course, and characteristics of postlaparoscopic shoulder pain. Surg. Endosc. 2018, 32, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, E.K.; Andersson, E. Pulmonary recruitment maneuver reduces shoulder pain and nausea after laparoscopic cholecystectomy: A randomized controlled trial. World J. Surg. 2021, 45, 3575–3583. [Google Scholar] [CrossRef] [PubMed]
- Li, X.Y.; Tian, M.; Li, A.Z.; Han, C.L.; Li, K.Z. The risk of shoulder pain after laparoscopic surgery for infertility is higher in thin patients. Sci. Rep. 2021, 11, 13421. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.B.; Kang, K.; Song, M.K.; Seok, S.; Kim, Y.H.; Kim, J.E. Pain characteristics after total laparoscopic hysterectomy. Int. J. Med. Sci. 2016, 13, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Sharami, S.H.; Sharami, M.B.; Abdollahzadeh, M.; Keyvan, A. Randomised clinical trial of the influence of pulmonary recruitment manoeuvre on reducing shoulder pain after laparoscopy. J. Obstet. Gynaecol. 2010, 30, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Ryu, K.; Choi, W.; Shim, J.; Song, T. The impact of a pulmonary recruitment maneuver to reduce post-laparoscopic shoulder pain: A randomized controlled trial. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 208, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Dixon, J.B.; Reuben, Y.; Halket, C.; O’Brien, P.E. Shoulder pain is a common problem following laparoscopic adjustable gastric band surgery. Obes. Surg. 2005, 15, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, D.; Seo, D.; Son, J.S.; Kim, D.C. Validity and reliability of the Korean version of the Quality of Recovery-40 questionnaire. Korean J. Anesthesiol. 2018, 71, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Pergialiotis, V.; Vlachos, D.E.; Kontzoglou, K.; Perrea, D.; Vlachos, G.D. Pulmonary recruitment maneuver to reduce pain after laparoscopy: A meta-analysis of randomized controlled trials. Surg. Endosc. 2015, 29, 2101–2108. [Google Scholar] [CrossRef] [PubMed]
- Kaloo, P.; Armstrong, S.; Kaloo, C.; Jordan, V. Interventions to reduce shoulder pain following gynaecological laparoscopic procedures. Cochrane Database Syst. Rev. 2019, 1, CD011101. [Google Scholar] [CrossRef]
- Chung, J.W.; Kang, K.S.; Park, S.H.; Kim, C.S.; Chung, J.H.; Yoo, S.H.; Kim, N.S.; Seo, Y.H.; Jung, H.S.; Chun, H.R.; et al. Effect of intraperitoneal CO2 concentration on postoperative pain after laparoscopic cholecystectomy. Ann. Surg. Treat. Res. 2017, 93, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Woehlck, H.J.; Otterson, M.; Yun, H.; Connolly, L.A.; Eastwood, D.; Colpaert, K. Acetazolamide reduces referred postoperative pain after laparoscopic surgery with carbon dioxide insufflation. Anesthesiology 2003, 99, 924–928. [Google Scholar] [CrossRef]
- Bala, I.; Bhatia, N.; Mishra, P.; Verma, G.R.; Kaman, L. Comparison of preoperative oral acetazolamide and intraperitoneal normal saline irrigation for reduction of postoperative pain after laparoscopic cholecystectomy. J. Laparoendosc. Adv. Surg. Tech. A 2015, 25, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh, F.; Nasiri, E.; Behroozi, T. Investigating the effects of drainage by hemovac drain on shoulder pain after female laparoscopic surgery and comparison with deep breathing technique: A randomized clinical trial study. Surg. Endosc. 2020, 34, 5439–5446. [Google Scholar] [CrossRef] [PubMed]
- Rettenmaier, M.A.; Micha, J.P.; Lopez, K.L.; Wilcox, A.M.; Goldstein, B.H. A prospective, observational trial assessing the efficacy of abdominal compression in reducing laparoscopic-induced shoulder pain. Surg. Innov. 2017, 24, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Defresne, A.A.; Hans, G.A.; Goffin, P.J.; Bindelle, S.P.; Amabili, P.J.; DeRoover, A.M.; Poirrier, R.; Brichant, J.F.; Joris, J.L. Recruitment of lung volume during surgery neither affects the postoperative spirometry nor the risk of hypoxaemia after laparoscopic gastric bypass in morbidly obese patients: A randomized controlled study. Br. J. Anaesth. 2014, 113, 501–507. [Google Scholar] [CrossRef] [PubMed]
| Control (n = 30) | Low ARM (n = 30) | High ARM (n = 29) | p Value | |
|---|---|---|---|---|
| Age (years) | 36 [33–39] | 35 [32–39] | 33 [30–36] | 0.530 |
| Gender (M/F) | 3/27 | 5/25 | 4/25 | 0.750 |
| Body mass index (kg/m2) | 38 [36–41] | 38 [36–40] | 37 [36–39] | 0.826 |
| Diabetes mellitus (n) | 12 | 8 | 10 | 0.547 |
| Hypertension (n) | 16 | 8 | 13 | 0.101 |
| Anesthesia time (min) | 143 [125–161] | 153 [128–178] | 140 [124–156] | 0.615 |
| Operation time (min) | 115 [97–132] | 122 [99–146] | 109 [94–125] | 0.617 |
| Pneumoperitoneum time (min) | 89 [73–105] | 97 [74–121] | 89 [68–93] | 0.432 |
| Variables | Group | Baseline | Before ARM | ARM 1 min | ARM 3 min | ARM 5 min |
|---|---|---|---|---|---|---|
| Mean BP (mmHg) | Control | 101 [94–107] | 85 [81–89] | 87 [84–91] | 86 [83–90] | 87 [82–91] |
| Low ARM | 97 [91–102] | 91 [84–98] | 90 [83–96] | 88 [83–94] | 89 [83–95] | |
| High ARM | 100 [93–107] | 88 [82–94] | 87 [80–94] | 87 [81–93] | 87 [81–92] | |
| Heart rate (beats/min) | Control | 80 [76–85] | 84 [79–89] | 82 [77–87] | 82 [77–87] | 83 [78–88] |
| Low ARM | 77 [73–81] | 83 [78–88] | 81 [75–86] | 79 [75–84] | 80 [75–85] | |
| High ARM | 82 [78–87] | 78 [74–83] | 81 [76–85] | 80 [76–85] | 81 [77–85] | |
| SpO2 (%) | Control | 99 [99–100] | 99 [98–99] | 99 [99–99] | 99 [98–99] | 99 [98–99] |
| Low ARM | 99 [99–100] | 99 [99–100] | 100 [99–100] | 100 [99–100] | 100 [99–100] | |
| High ARM | 99 [98–99] | 99 [98–99] | 99 [99–100] | 99 [99–100] | 99 [99–100] | |
| Vasopressor use (n) | Control | 1 | 1 | 0 | 0 | 0 |
| Low ARM | 1 | 1 | 0 | 0 | 0 | |
| High ARM | 1 | 0 | 0 | 0 | 0 |
| Control (n = 30) | Low ARM (n = 30) | High ARM (n = 29) | p Value | |
|---|---|---|---|---|
| Pain score (NRS) | 5 [4–6] | 5 [4–7] | 6 [3–7] | 0.318 |
| Rescue fentanyl (µg) | 50 [0–100] | 50 [0–100] | 50 [0–88] | 0.993 |
| Nausea (n) | 16 | 11 | 9 | 0.191 |
| Nausea (NRS) | 3 [0–5] | 1 [0–5] | 1 [0–4] | 0.245 |
| Vomiting (n) | 2 | 2 | 3 | 0.833 |
| Rescue antiemetics use (n) | 8 | 6 | 4 | 0.469 |
| Control (n = 30) | Low ARM (n = 30) | High ARM (n = 29) | p Value | |
|---|---|---|---|---|
| Shoulder pain (NRS) | 3 [1–3] | 2 [0–3] | 2 [0–2] | 0.141 |
| Abdominal pain (NRS) | 3 [2–5] | 3 [3–5] | 3 [2–3] | 0.101 |
| Shoulder pain > abdominal pain (n) | 8 | 3 | 4 | 0.196 |
| Rescue meperidine (mg) | 50 [25–50] | 50 [25–50] | 50 [25–50] | 0.820 |
| Infused PCA (mL) | 55 [40–75] | 64 [51–76] | 60 [42–80] | 0.591 |
| Total QoR score | 149 [138–160] | 152 [143–160] | 155 [142–167] | 0.755 |
| Physical comfort | 46 [43–49] | 46 [43–48] | 46 [43–50] | 0.935 |
| Emotional state | 36 [34–39] | 36 [34–38] | 37 [34–39] | 0.904 |
| Psychological support | 27 [25–30] | 28 [26–30] | 28 [26–31] | 0.818 |
| Physical independence | 14 [12–16] | 14 [12–16] | 16 [14–18] | 0.374 |
| Pain | 27 [25–29] | 28 [27–30] | 28 [25–30] | 0.589 |
| Postoperative complications (n) | 4 | 1 | 0 | 0.124 |
| Hospital stay (day) | 5 [5–6] | 5 [5–7] | 5 [5–7] | 0.339 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, Y.-Y.; Kim, S.-M.; Lee, D.; Kim, Y.-B.; Cha, J.; Kwak, H.-J. Effect of Low or High Pressure Alveolar Recruitment Maneuver on Postoperative Pain and Quality of Recovery in Patients with Obesity Undergoing Laparoscopic Sleeve Gastrectomy. J. Pers. Med. 2022, 12, 1550. https://doi.org/10.3390/jpm12101550
Jo Y-Y, Kim S-M, Lee D, Kim Y-B, Cha J, Kwak H-J. Effect of Low or High Pressure Alveolar Recruitment Maneuver on Postoperative Pain and Quality of Recovery in Patients with Obesity Undergoing Laparoscopic Sleeve Gastrectomy. Journal of Personalized Medicine. 2022; 12(10):1550. https://doi.org/10.3390/jpm12101550
Chicago/Turabian StyleJo, Youn-Yi, Seong-Min Kim, Dongchul Lee, Yong-Beom Kim, Jeongho Cha, and Hyun-Jeong Kwak. 2022. "Effect of Low or High Pressure Alveolar Recruitment Maneuver on Postoperative Pain and Quality of Recovery in Patients with Obesity Undergoing Laparoscopic Sleeve Gastrectomy" Journal of Personalized Medicine 12, no. 10: 1550. https://doi.org/10.3390/jpm12101550
APA StyleJo, Y.-Y., Kim, S.-M., Lee, D., Kim, Y.-B., Cha, J., & Kwak, H.-J. (2022). Effect of Low or High Pressure Alveolar Recruitment Maneuver on Postoperative Pain and Quality of Recovery in Patients with Obesity Undergoing Laparoscopic Sleeve Gastrectomy. Journal of Personalized Medicine, 12(10), 1550. https://doi.org/10.3390/jpm12101550





