Evaluating Virtual and Inpatient Pulmonary Rehabilitation Programs for Patients with COPD
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Lung Volumes and Respiratory Strength
2.4. Physical Capacity, Disease Impact, and Dyspnea
2.5. Intervention
2.6. Statistical Analysis
3. Results
3.1. Comparison of Pre-Test and Post-Test Results in the Inpatient Setting
3.2. Comparison of Pre-Test and Post-Test Results in the Online Setting
3.3. Comparison of Pre-Test Results between Inpatients and Online Participants
3.4. Comparison in Post-Test Results between Inpatients and Online Participants
4. Discussion
4.1. Important Findings
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murray, C.; Kyu, H.; Abate, D.; Abate, K.; Abay, S.; Cristiana, A.; Abbasi, N.; Abbastabar, H.; Ebro, J.; Abdelalim, A.; et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Glob. Health Metr. 2018, 392, 1859–1922. [Google Scholar]
- Ramon, M.A.; Ter Riet, G.; Carsin, A.-E.; Gimeno-Santos, E.; Agustí, A.; Antó, J.M.; Donaire-Gonzalez, D.; Ferrer, J.; Rodríguez, E.; Rodriguez-Roisin, R.; et al. The dyspnoea-inactivity vicious circle in COPD: Development and external validation of a conceptual model. Eur. Respir. J. 2018, 52, 1800079. [Google Scholar] [CrossRef] [PubMed]
- Christenson, S.A.; Smith, B.M.; Bafadhel, M.; Putcha, N. Chronic obstructive pulmonary disease. Lancet 2022, 399, 2227–2242. [Google Scholar] [CrossRef]
- Chronic Obstructive Pulmonary Disease in over 16s: Diagnosis and Management; National Institute for Health and Care Excellence (NICE): London, UK, 2019; ISBN 978-1-4731-3468-3.
- Vogiatzis, I.; Rochester, C.L.; Spruit, M.A.; Troosters, T.; Clini, E.M. Increasing implementation and delivery of pulmonary rehabilitation: Key messages from the new ATS/ERS policy statement. Eur. Respir. J. 2016, 47, 1336–1341. [Google Scholar] [CrossRef] [PubMed]
- Méndez, A.; Labra, P.; Pizarro, R.; Baeza, N. Low rates of participation and completion of pulmonary rehabilitation in patients with chronic obstructive pulmonary disease in primary health care. Rev. Med. Chil. 2018, 146, 1304–1308. [Google Scholar] [CrossRef]
- Cox, N.S.; Oliveira, C.C.; Lahham, A.; Holland, A.E. Pulmonary rehabilitation referral and participation are commonly influenced by environment, knowledge, and beliefs about consequences: A systematic review using the Theoretical Domains Framework. J. Physiother. 2017, 63, 84–93. [Google Scholar] [CrossRef]
- Keating, A.; Lee, A.; Holland, A.E. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron. Respir. Dis. 2011, 8, 89–99. [Google Scholar] [CrossRef]
- Fischer, M.J.; Scharloo, M.; Abbink, J.J.; van ’t Hul, A.J.; van Ranst, D.; Rudolphus, A.; Weinman, J.; Rabe, K.F.; Kaptein, A.A. Drop-out and attendance in pulmonary rehabilitation: The role of clinical and psychosocial variables. Respir. Med. 2009, 103, 1564–1571. [Google Scholar] [CrossRef]
- Rochester, C.L.; Vogiatzis, I.; Holland, A.E.; Lareau, S.C.; Marciniuk, D.D.; Puhan, M.A.; Spruit, M.A.; Masefield, S.; Casaburi, R.; Clini, E.M.; et al. An official American Thoracic Society/European Respiratory Society policy statement: Enhancing implementation, use, and delivery of pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2015, 192, 1373–1386. [Google Scholar] [CrossRef]
- Holland, A.E.; Mahal, A.; Hill, C.J.; Lee, A.L.; Burge, A.T.; Cox, N.S.; Moore, R.; Nicolson, C.; O’Halloran, P.; Lahham, A.; et al. Home-based rehabilitation for COPD using minimal resources: A randomised, controlled equivalence trial. Thorax 2017, 72, 57–65. [Google Scholar] [CrossRef]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef] [PubMed]
- Rabe, K.F.; Hurd, S.; Anzueto, A.; Barnes, P.J.; Buist, S.A.; Calverley, P.; Fukuchi, Y.; Jenkins, C.; Rodriguez-Roisin, R.; van Weel, C.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2007, 176, 532–555. [Google Scholar] [CrossRef] [PubMed]
- Laveneziana, P.; Albuquerque, A.; Aliverti, A.; Babb, T.; Barreiro, E.; Dres, M.; Dubé, B.-P.; Fauroux, B.; Gea, J.; Guenette, J.A.; et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur. Respir. J. 2019, 53, 1801214. [Google Scholar] [CrossRef] [PubMed]
- Issues, S.; Test, M.W.; Equipment, R.; Preparation, P. American Thoracic Society ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.-H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Munari, A.B.; Gulart, A.A.; Dos Santos, K.; Venâncio, R.S.; Karloh, M.; Mayer, A.F. Modified Medical Research Council Dyspnea Scale in GOLD Classification Better Reflects Physical Activities of Daily Living. Respir. Care 2018, 63, 77–85. [Google Scholar] [CrossRef]
- Munteanu, L.A.; Frandes, M.; Timar, B.; Tudorache, E.; Fildan, A.P.; Oancea, C.; Tofolean, D.E. The efficacy of a mobile phone application to improve adherence to treatment and self-management in people with chronic respiratory disease in Romanian population—A pilot study. BMC Health Serv. Res. 2020, 20, 475. [Google Scholar] [CrossRef]
- Irina, B.P.; Steluta, M.M.; Emanuela, T.; Diana, M.; Cristina, O.D.; Mirela, F.; Cristian, O. Respiratory muscle training program supplemented by a cell-phone application in COPD patients with severe airflow limitation. Respir. Med. 2021, 190, 106679. [Google Scholar] [CrossRef]
- Siddiq, M.A.B.; Rathore, F.A.; Clegg, D.; Rasker, J.J. Pulmonary Rehabilitation in COVID-19 patients: A scoping review of current practice and its application during the pandemic. Turk. J. Phys. Med. Rehabil. 2020, 66, 480–494. [Google Scholar] [CrossRef]
- Liu, W.; Wang, C.; Lin, H.; Lin, S.; Lee, K.; Lo, Y.; Hung, S. Efficacy of a cell phone-based exercise programme for COPD. Eur. Respir. J. 2008, 32, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Pezzuto, A.; Carico, E. Effectiveness of smoking cessation in smokers with COPD and nocturnal oxygen desaturation: Functional analysis. Clin. Respir. J. 2020, 14, 29–34, PMID: 31613417. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Milne, S.; Sin, D.D. Pulmonary rehabilitation in a postcoronavirus disease 2019 world: Feasibility, challenges, and solutions. Curr. Opin. Pulm. Med. 2022, 28, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Bourne, S.; DeVos, R.; North, M.; Chauhan, A.; Green, B.; Brown, T.; Cornelius, V.; Wilkinson, T. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: Randomised controlled trial. BMJ Open 2017, 7, e014580. [Google Scholar] [CrossRef] [PubMed]
- Chaplin, E.; Hewitt, S.; Apps, L.; Bankart, J.; Pulikottil-Jacob, R.; Boyce, S.; Morgan, M.; Williams, J.; Singh, S. Interactive web-based pulmonary rehabilitation programme: A randomised controlled feasibility trial. BMJ Open 2017, 7, e013682. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.; Bieler, T.; Beyer, N.; Kallemose, T.; Wilcke, J.T.; Østergaard, L.M.; Frost Andeassen, H.; Martinez, G.; Lavesen, M.; Frølich, A.; et al. Supervised pulmonary tele-rehabilitation versus pulmonary rehabilitation in severe COPD: A randomised multicentre trial. Thorax 2020, 75, 413–421. [Google Scholar] [CrossRef]
- Langer, D.; Ciavaglia, C.; Faisal, A.; Webb, K.A.; Neder, J.A.; Gosselink, R.; Dacha, S.; Topalovic, M.; Ivanova, A.; O’Donnell, D.E. Inspiratory muscle training reduces diaphragm activation and dyspnea during exercise in COPD. J. Appl. Physiol. 2018, 125, 381–392. [Google Scholar] [CrossRef]
- Holland, A.E.; Hill, C.J.; Rasekaba, T.; Lee, A.; Naughton, M.T.; McDonald, C.F. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch. Phys. Med. Rehabil. 2010, 91, 221–225. [Google Scholar] [CrossRef]
- Tsai, L.L.Y.; McNamara, R.J.; Moddel, C.; Alison, J.A.; McKenzie, D.K.; McKeough, Z.J. Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: The randomized controlled TeleR Study. Respirology 2017, 22, 699–707. [Google Scholar] [CrossRef]
- Kon, S.S.C.; Canavan, J.L.; Jones, S.E.; Nolan, C.M.; Clark, A.L.; Dickson, M.J.; Haselden, B.M.; Polkey, M.I.; Man, W.D.-C. Minimum clinically important difference for the COPD Assessment Test: A prospective analysis. Lancet Respir. Med. 2014, 2, 195–203. [Google Scholar] [CrossRef]
- Loeckx, M.; Rabinovich, R.A.; Demeyer, H.; Louvaris, Z.; Tanner, R.; Rubio, N.; Frei, A.; De Jong, C.; Gimeno-Santos, E.; Rodrigues, F.M.; et al. Smartphone-Based Physical Activity Telecoaching in Chronic Obstructive Pulmonary Disease: Mixed-Methods Study on Patient Experiences and Lessons for Implementation. JMIR Mhealth Uhealth 2018, 6, e200. [Google Scholar] [CrossRef] [PubMed]

| Variables * | Pre-Test (n = 72) | Post-Test (n = 72) | p-Value |
|---|---|---|---|
| Age, years (mean ± SD) | 64.9 ± 5.7 | 64.9 ± 5.7 | - |
| Sex (men) ** | 54 (75.0%) | 54 (75.0%) | - |
| BMI, kg/m2 (mean ± SD) | 25.4 ± 3.3 | 25.4 ± 3.3 | - |
| FVC (L) pred | 4.1 ± 0.4 | 4.1 ± 0.4 | - |
| FVC (L) actual | 2.9 ± 0.4 | 3.0 ± 0.3 | 0.091 |
| FVC (%) | 70.8 ± 5.9 | 70.1 ± 5.9 | 0.477 |
| FEV1 (L) pred | 3.0 ± 0.3 | 3.0 ± 0.3 | - |
| FEV1 (L) actual | 1.4 ± 0.2 | 1.3 ± 0.3 | 0.200 |
| FEV1 (%) | 42.5 ± 4.6 | 43.1 ± 4.5 | 0.430 |
| FEV1/FVC (%) pred | 74.6 ± 1.1 | 74.6 ± 1.1 | - |
| FEV1/FVC (%) actual | 44.9 ± 5.7 | 45.2 ± 5.7 | 0.752 |
| MIP (cmH2O) pred | 103.3 ± 4.5 | 103.3 ± 4.5 | - |
| MIP (cmH2O) actual | 55.7 ± 15.8 | 62.5 ± 16.6 | 0.012 |
| MIP (%) | 53.8 ± 14.5 | 60.4 ± 15.1 | 0.008 |
| MEP (cmH2O) pred | 112.7 ± 4.6 | 112.7 ± 4.6 | - |
| MEP (cmH2O) actual | 82.2 ± 12.3 | 86.8 ± 12.5 | 0.027 |
| MEP (%) | 72.8 ± 9.9 | 76.9 ± 9.9 | 0.038 |
| 6MWT (m) pred | 467.6 ± 35.0 | 467.6 ± 35.0 | - |
| 6MWT (m) actual | 340.5 ± 85.0 | 371.5 ± 79.6 | 0.025 |
| 6MWT (%) | 72.5 ± 15.6 | 79.2 ± 14.4 | 0.008 |
| CAT | 19.5 ± 5.1 | 14.7 ± 4.1 | <0.001 |
| mMRC (mean rank) | 45.25 | 27.75 | <0.001 |
| Variables * | Pre-Test (n = 58) | Post-Test (n = 58) | p-Value |
|---|---|---|---|
| Age, years (mean ± SD) | 64.3 ± 4.3 | 64.3 ± 4.3 | - |
| Sex (men) ** | 42 (72.4%) | 42 (72.4%) | - |
| BMI, kg/m2 (mean ± SD) | 25.7 ± 2.5 | 25.7 ± 2.5 | - |
| FVC (L) pred | 4.3 ± 0.3 | 4.3 ± 0.3 | - |
| FVC (L) actual | 3.0 ± 0.4 | 3.1 ± 0.4 | 0.896 |
| FVC (%) | 71.0 ± 6.8 | 71.4 ± 6.6 | 0.830 |
| FEV1 (L) pred | 3.3 ± 0.3 | 3.3 ± 0.3 | - |
| FEV1 (L) actual | 1.3 ± 0.2 | 1.4 ± 0.2 | 0.800 |
| FEV1 (%) | 41.7 ± 4.6 | 42.2 ± 4.6 | 0.674 |
| FEV1/FVC (%) pred | 74.8 ± 0.9 | 74.8 ± 0.9 | - |
| FEV1/FVC (%) actual | 44.2 ± 6.5 | 44.5 ± 6.2 | 0.894 |
| MIP (cmH2O) pred | 103.8 ± 3.4 | 103.8 ± 3.4 | - |
| MIP (cmH2O) actual | 55.7 ± 12.1 | 59.9 ± 12.3 | 0.194 |
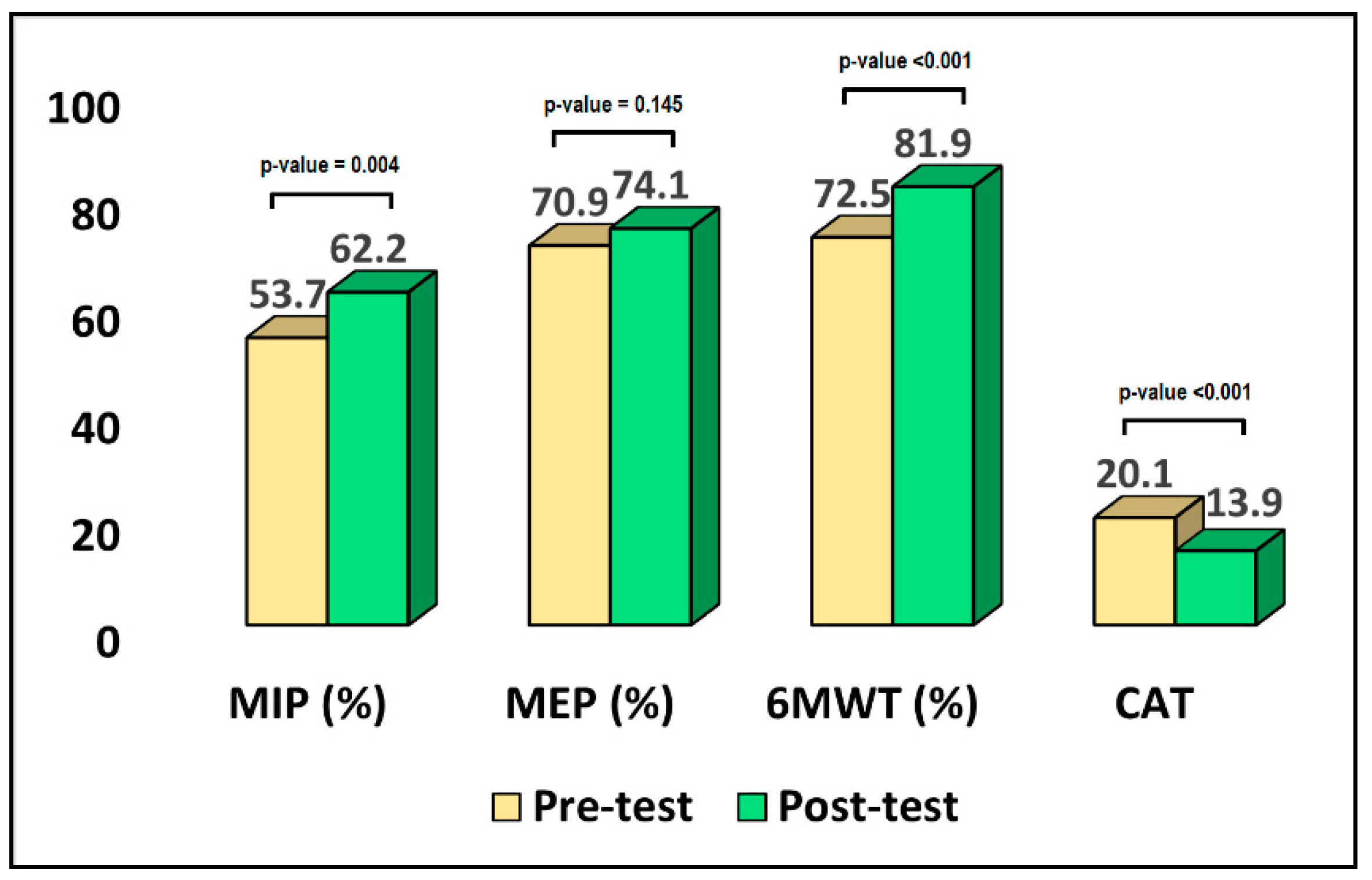
| MIP (%) | 53.7 ± 11.6 | 62.2 ± 13.3 | 0.004 |
| MEP (cmH2O) pred | 113.2 ± 3.5 | 113.2 ± 3.5 | - |
| MEP (cmH2O) actual | 80.2 ± 13.6 | 83.3 ± 13.1 | 0.307 |
| MEP (%) | 70.9 ± 12.0 | 74.1 ± 11.5 | 0.145 |
| 6MWT (m) pred | 473.0 ± 35.0 | 467.6 ± 35.0 | - |
| 6MWT (m) actual | 342.9 ± 61.9 | 387.3 ± 56.3 | 0.006 |
| 6MWT (%) | 72.5 ± 12.5 | 81.9 ± 11.3 | <0.001 |
| CAT | 20.1 ± 5.3 | 13.9 ± 4.5 | <0.001 |
| mMRC (mean rank) | 39.4 | 19.5 | 0.004 |
| Variables * | Inpatient (n = 72) | Online (n = 58) | p-Value |
|---|---|---|---|
| Age, years (mean ± SD) | 64.9 ± 5.7 | 64.3 ± 4.3 | 0.659 |
| Sex (men) ** | 54 (75.0%) | 42 (72.4%) | 0.727 |
| BMI, kg/m2 (mean ± SD) | 25.4 ± 3.3 | 25.7 ± 2.5 | 0.689 |
| FVC (L) pred | 4.1 ± 0.4 | 4.3 ± 0.3 | 0.133 |
| FVC (L) actual | 2.9 ± 0.4 | 3.0 ± 0.4 | 0.105 |
| FVC (%) | 70.8 ± 5.9 | 71.0 ± 6.8 | 0.930 |
| FEV1 (L) pred | 3.0 ± 0.3 | 3.3 ± 0.3 | 0.299 |
| FEV1 (L) actual | 1.4 ± 0.2 | 1.3 ± 0.2 | 0.066 |
| FEV1 (%) | 42.5 ± 4.6 | 41.7 ± 4.6 | 0.479 |
| FEV1/FVC (%) pred | 74.6 ± 1.1 | 74.8 ± 0.9 | 0.639 |
| FEV1/FVC (%) actual | 44.9 ± 5.7 | 44.2 ± 6.5 | 0.654 |
| MIP (cmH2O) pred | 103.3 ± 4.5 | 103.8 ± 3.4 | 0.659 |
| MIP (cmH2O) actual | 55.7 ± 15.8 | 55.7 ± 12.1 | 0.978 |
| MIP (%) | 53.8 ± 14.5 | 53.7 ± 11.6 | 0.959 |
| MEP (cmH2O) pred | 112.7 ± 4.6 | 113.2 ± 3.5 | 0.662 |
| MEP (cmH2O) actual | 82.2 ± 12.3 | 80.2 ± 13.6 | 0.536 |
| MEP (%) | 72.8 ± 9.9 | 70.9 ± 12.0 | 0.482 |
| 6MWT (m) pred | 467.6 ± 35.0 | 473.0 ± 35.0 | 0.496 |
| 6MWT (m) actual | 340.5 ± 85.0 | 342.9 ± 61.9 | 0.899 |
| 6MWT (%) | 72.5 ± 15.6 | 72.5 ± 12.5 | 0.967 |
| CAT | 19.5 ± 5.1 | 20.1 ± 5.3 | 0.608 |
| mMRC (mean rank) | 45.25 | 39.4 | 0.696 |
| Variables * | Inpatient (n = 72) | Online (n = 58) | p-Value |
|---|---|---|---|
| Age, years (mean ± SD) | 64.9 ± 5.7 | 64.3 ± 4.3 | 0.508 |
| Sex (men) ** | 54 (75.0%) | 42 (72.4%) | 0.727 |
| BMI, kg/m2 (mean ± SD) | 25.4 ± 3.3 | 25.7 ± 2.5 | 0.568 |
| FVC (L) pred | 4.1 ± 0.4 | 4.3 ± 0.4 | 0.502 |
| FVC (L) actual | 2.9 ± 0.4 | 3.1 ± 0.4 | 0.004 |
| FVC (%) | 71.3 ± 5.9 | 71.4 ± 6.6 | 0.927 |
| FEV1 (L) pred | 3.0 ± 0.3 | 3.2 ± 0.3 | 0.140 |
| FEV1 (L) actual | 1.2 ± 0.2 | 1.4 ± 0.2 | 0.010 |
| FEV1 (%) | 43.1 ± 4.5 | 42.2 ± 4.6 | 0.263 |
| FEV1/FVC (%) pred | 74.6 ± 1.2 | 74.8 ± 0.9 | 0.426 |
| FEV1/FVC (%) actual | 45.2 ± 5.7 | 44.5 ± 6.2 | 0.461 |
| MIP (cmH2O) pred | 103.3 ± 4.5 | 103.8 ± 3.4 | 0.639 |
| MIP (cmH2O) actual | 62.6 ± 16.6 | 59.9 ± 12.3 | 0.602 |
| MIP (%) | 60.4 ± 15.1 | 62.2 ± 13.2 | 0.659 |
| MEP (cmH2O) pred | 112.7 ± 4.6 | 113.2 ± 3.5 | 0.477 |
| MEP (cmH2O) actual | 86.9 ± 12.5 | 83.8 ± 13.1 | 0.614 |
| MEP (%) | 76.9 ± 9.9 | 74.1 ± 11.5 | 0.662 |
| 6MWT (m) pred | 467.6 ± 35.0 | 473.0 ± 25.7 | 0.346 |
| 6MWT (m) actual | 371.5 ± 79.6 | 387.3 ± 56.3 | 0.293 |
| 6MWT (%) | 79.2 ± 14.4 | 81.9 ± 11.3 | 0.245 |
| CAT | 14.7 ± 4.1 | 13.9 ± 4.5 | 0.291 |
| mMRC (mean rank) | 35.33 | 30.10 | 0.222 |
| Variables * | Inpatient (n = 72) | Online (n = 58) | p-Value |
|---|---|---|---|
| FVC (L) actual | 0.1 ± 0.1 | 0.1 ± 0.1 | 1 |
| FVC (%) | 0.7 ± 0.1 | 0.4 ± 0.2 | <0.001 |
| FEV1 (L) actual | 0.1 ± 0.1 | 0.1 ± 0.1 | 1 |
| FEV1 (%) | 0.6 ± 0.1 | 0.5 ± 0.1 | <0.001 |
| FEV1/FVC (%) actual | 0.3 ± 0.1 | 0.3 ± 0.1 | 1 |
| MIP (cmH2O) actual | 6.8 ± 0.1 | 4.2 ± 0.3 | <0.001 |
| MIP (%) | 6.6 ± 0.6 | 8.5 ± 1.3 | <0.001 |
| MEP (cmH2O) actual | 4.6 ± 0.2 | 3.1 ± 0.5 | <0.001 |
| MEP (%) | 4.1 ± 0.1 | 3.2 ± 0.1 | <0.001 |
| 6MWT (m) actual | 31.0 ± 5.4 | 44.4 ± 5.6 | <0.001 |
| 6MWT (%) | 6.7 ± 1.2 | 9.4 ± 1.2 | <0.001 |
| CAT | 4.8 ± 1.0 | 6.2 ± 0.8 | <0.001 |
| mMRC (mean rank) | 17.5 | 19.9 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barata, P.I.; Crisan, A.F.; Maritescu, A.; Negrean, R.A.; Rosca, O.; Bratosin, F.; Citu, C.; Oancea, C. Evaluating Virtual and Inpatient Pulmonary Rehabilitation Programs for Patients with COPD. J. Pers. Med. 2022, 12, 1764. https://doi.org/10.3390/jpm12111764
Barata PI, Crisan AF, Maritescu A, Negrean RA, Rosca O, Bratosin F, Citu C, Oancea C. Evaluating Virtual and Inpatient Pulmonary Rehabilitation Programs for Patients with COPD. Journal of Personalized Medicine. 2022; 12(11):1764. https://doi.org/10.3390/jpm12111764
Chicago/Turabian StyleBarata, Paula Irina, Alexandru Florian Crisan, Adelina Maritescu, Rodica Anamaria Negrean, Ovidiu Rosca, Felix Bratosin, Cosmin Citu, and Cristian Oancea. 2022. "Evaluating Virtual and Inpatient Pulmonary Rehabilitation Programs for Patients with COPD" Journal of Personalized Medicine 12, no. 11: 1764. https://doi.org/10.3390/jpm12111764
APA StyleBarata, P. I., Crisan, A. F., Maritescu, A., Negrean, R. A., Rosca, O., Bratosin, F., Citu, C., & Oancea, C. (2022). Evaluating Virtual and Inpatient Pulmonary Rehabilitation Programs for Patients with COPD. Journal of Personalized Medicine, 12(11), 1764. https://doi.org/10.3390/jpm12111764








