The Accuracy of 3D Surgical Design and Simulation in Prefabricated Fibula Free Flaps for Jaw Reconstruction
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Patients
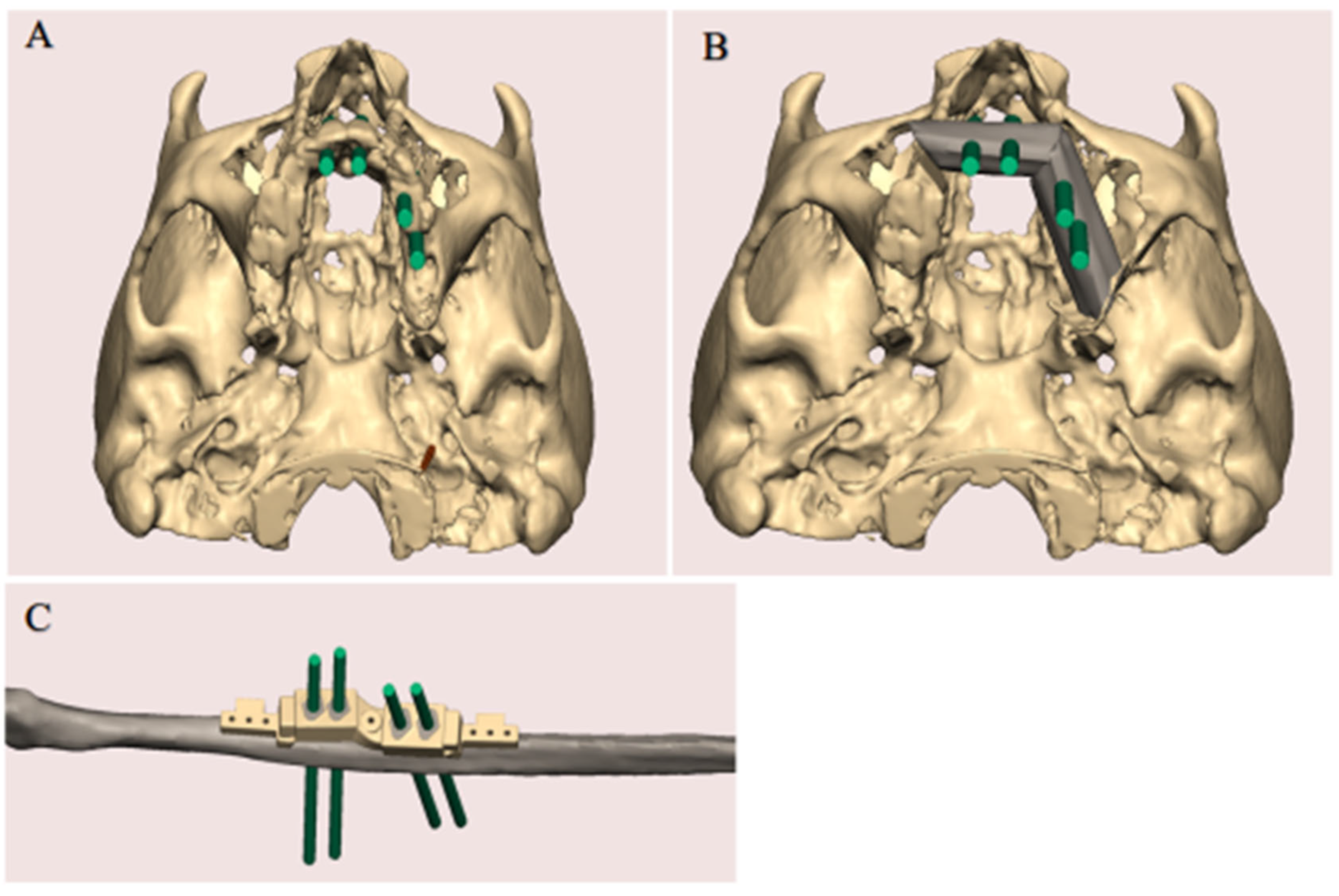
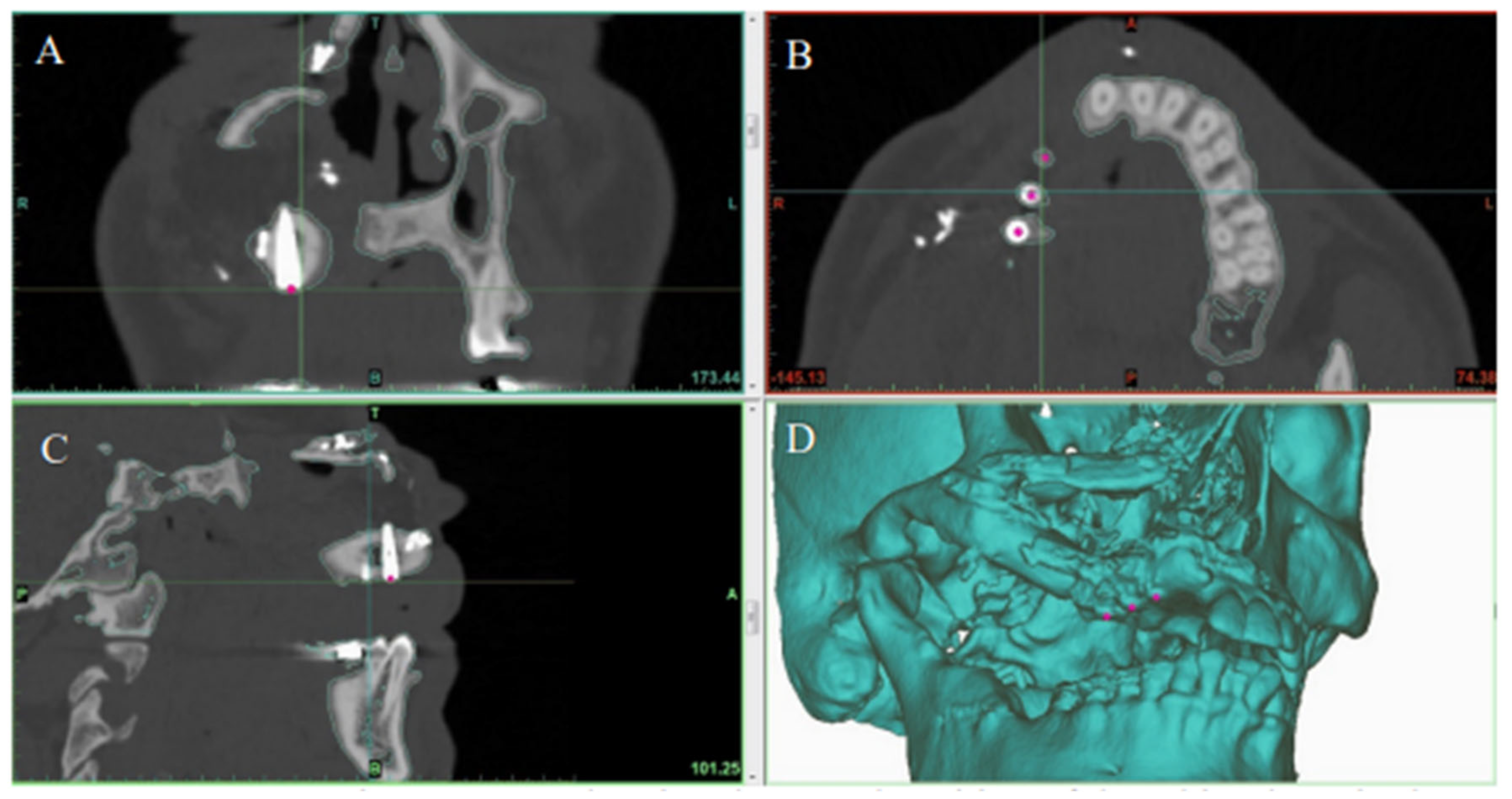
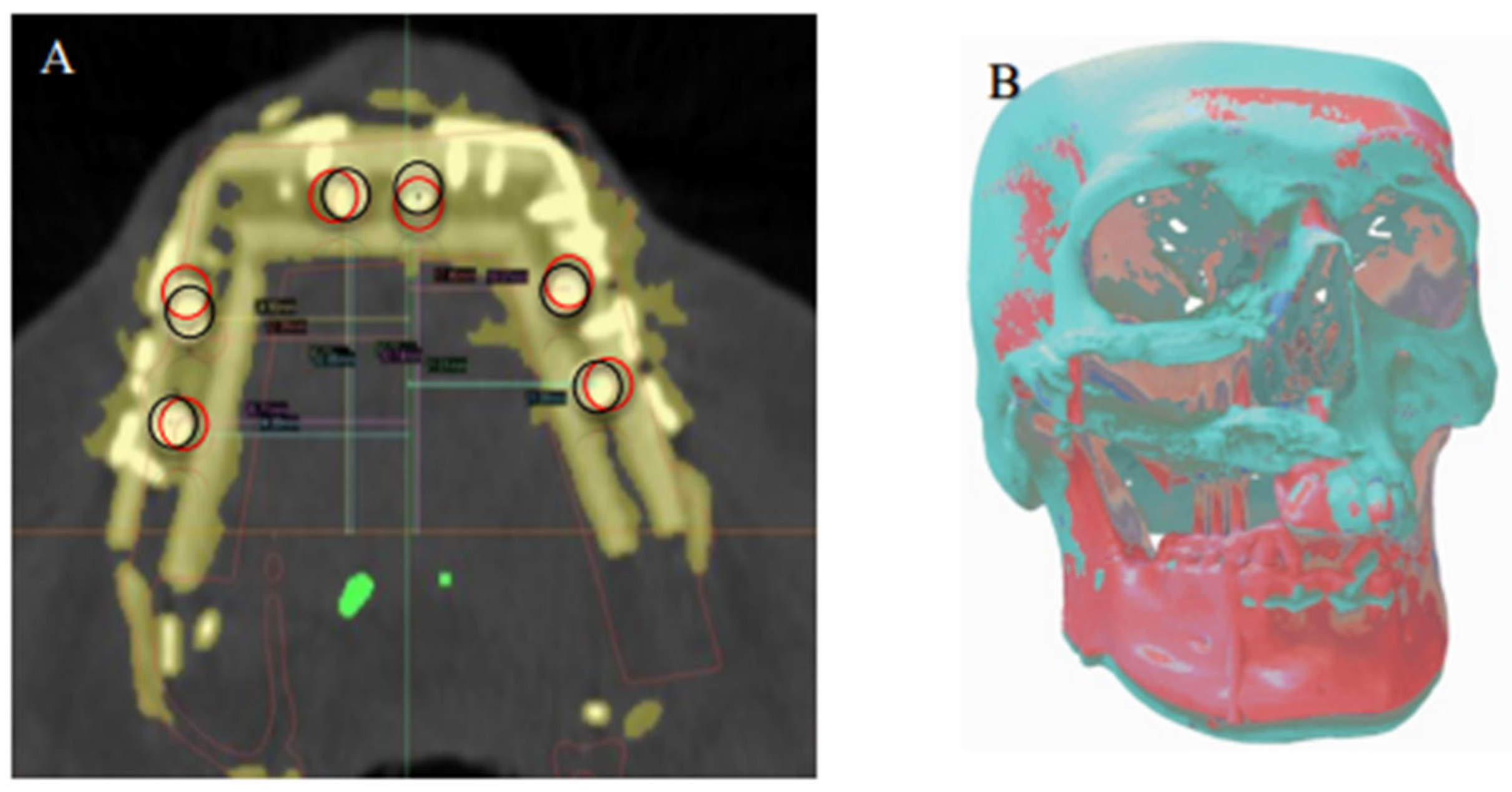
2.3. Virtual Surgical Planning
2.4. Surgical Procedure
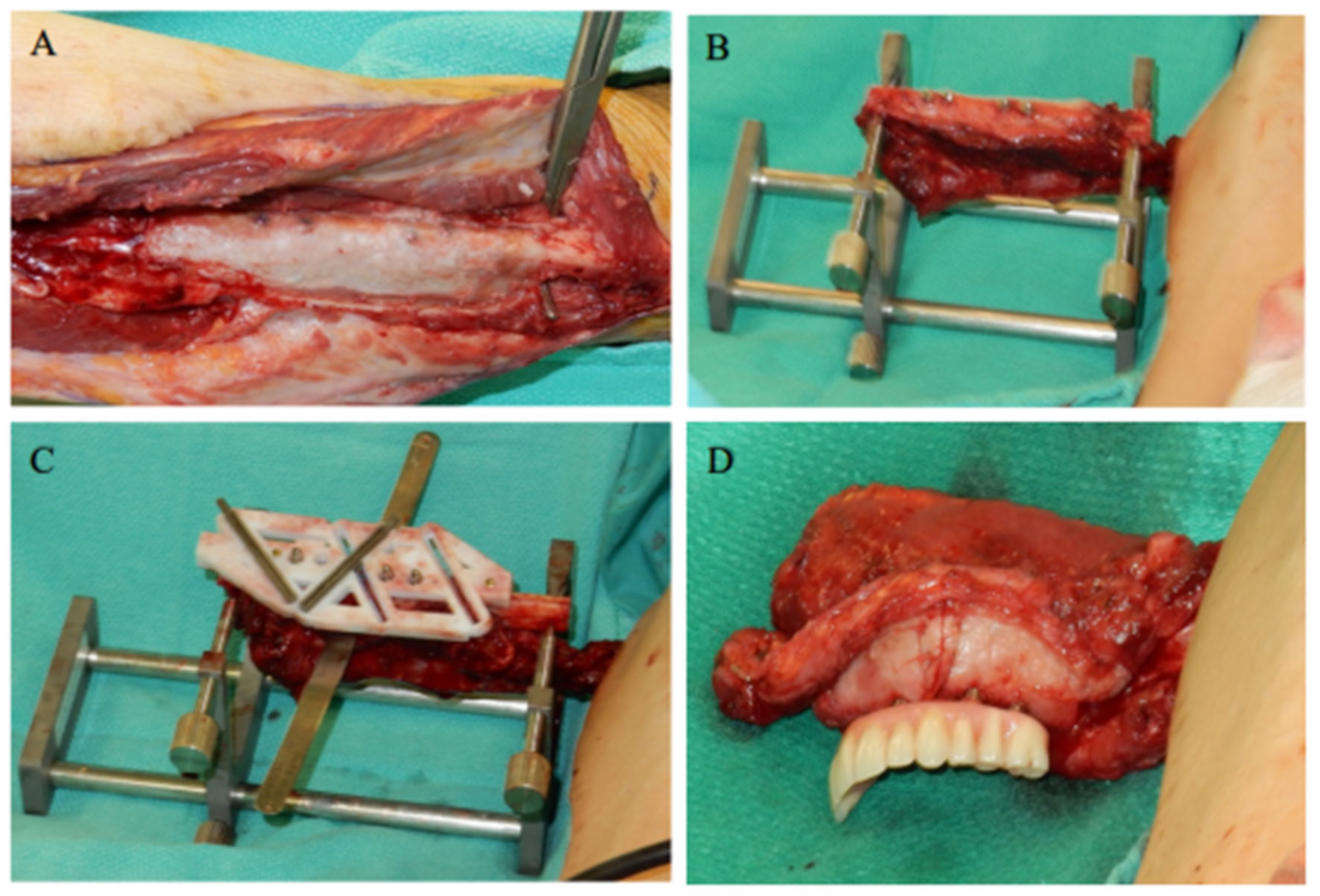
2.4.1. Stage I: Flap Prefabrication
2.4.2. Stage II: Jaw Reconstruction
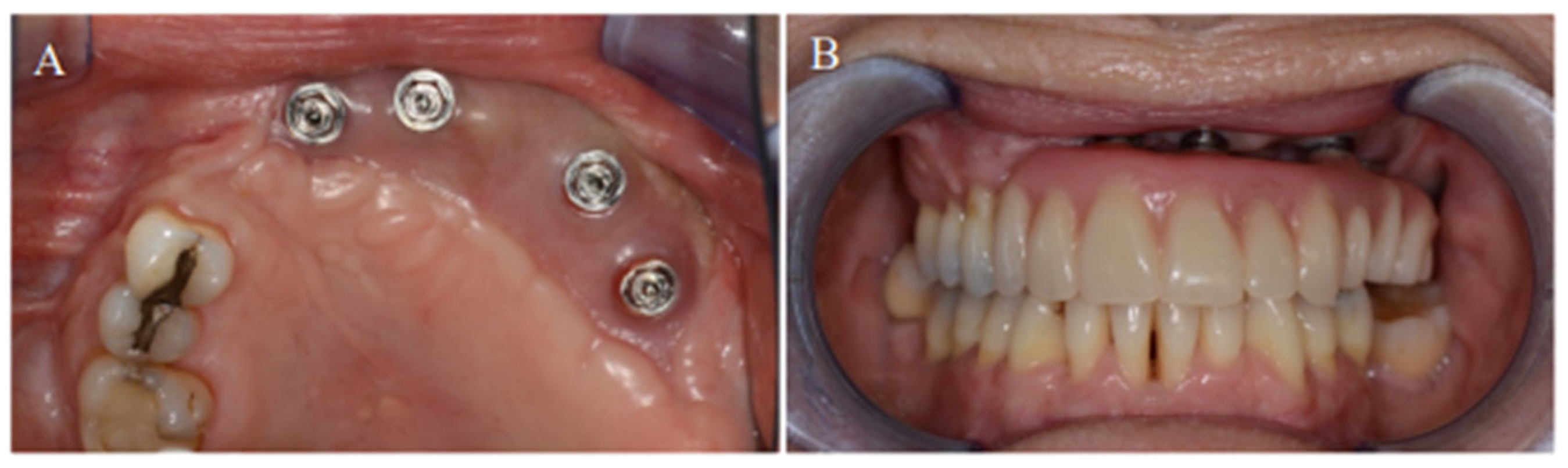
2.4.3. Stage III: Prosthodontic Treatment
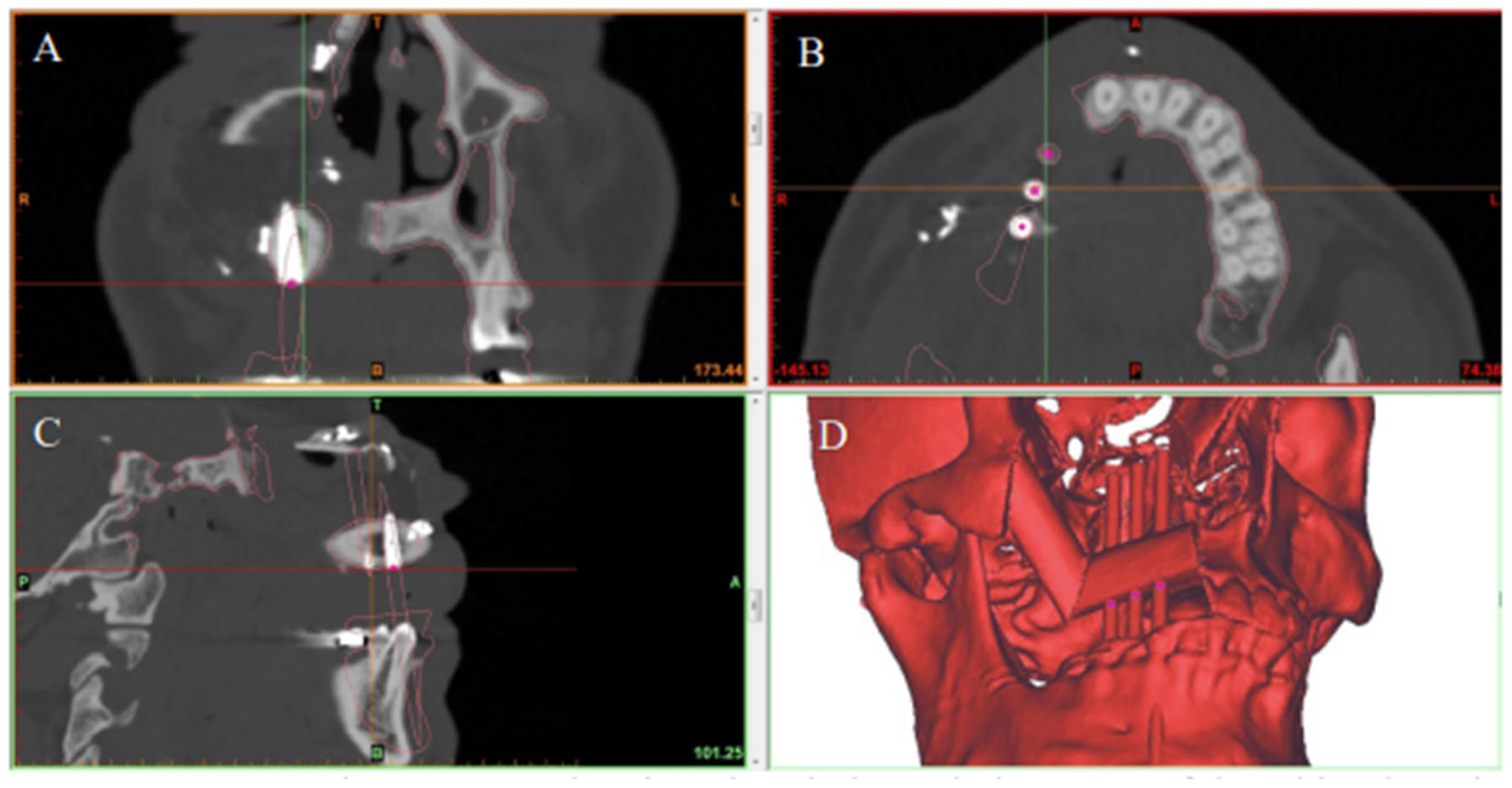
2.5. Primary Outcome
2.6. Data Analysis
3. Results
Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rohner, D.; Jaquiéry, C.; Kunz, C.; Bucher, P.; Maas, H.; Hammer, B. Maxillofacial reconstruction with prefabricated osseous free flaps: A 3-year experience with 24 patients. Plast. Reconstr. Surg. 2003, 112, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Weitz, J.; Bauer, F.J.M.; Hapfelmeier, A.; Rohleder, N.H.; Wolff, K.D.; Kesting, M.R. Accuracy of mandibular reconstruction by three-dimensional guided vascularised fibular free flap after segmental mandibulectomy. J. Maxillofac. Oral Surg. 2016, 54, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Toto, J.M.; Chang, E.I.; Agag, R.; Devarajan, K.; Patel, S.A.; Topham, N.S. Improved operative efficiency of free fibula flap mandible reconstruction with patient-specific, computer-guided preoperative planning. Head Neck 2015, 37, 1660–1664. [Google Scholar] [CrossRef] [PubMed]
- Hanasono, M.M.; Weinstock, Y.E.; Yu, P. Reconstruction of extensive head and neck defects with multiple simultaneous free flaps. Plast. Reconstr. Surg. 2008, 122, 1739–1746. [Google Scholar] [CrossRef]
- Seruya, M.; Fisher, M.; Rodriguez, E.D. Computer-assisted versus conventional free fibula flap technique for craniofacial reconstruction. Plast. Reconstr. Surg. 2013, 132, 1219–1228. [Google Scholar] [CrossRef]
- Wu, J.; Sun, J.; Shen, S.G.; Xu, B.; Li, J.; Zhang, S. Computer-assisted navigation: Its role in intraoperatively accurate mandibular reconstruction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 134–142. [Google Scholar] [CrossRef]
- Ochi, M.; Kanazawa, M.; Sato, D.; Kasugai, S.; Hirano, S.; Minakuchi, S. Factors affecting accuracy of implant placement with mucosa-supported stereolithographic surgical guides in edentulous mandibles. Comput. Biol. Med. 2013, 43, 1653–1660. [Google Scholar] [CrossRef]
- Zhang, N.; Liu, S.; Hu, Z.; Hu, J.; Zhu, S.; Li, Y. Accuracy of virtual surgical planning in two-jaw orthognathic surgery: Comparison of planned and actual results. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 143–151. [Google Scholar] [CrossRef]
- Okay, D.J.; Buchbinder, D.; Urken, M.; Jacobson, A.; Lazarus, C.; Persky, M. Computer-assisted implant rehabilitation of maxillomandibular defects reconstructed with vascularized bone free flaps. JAMA Otolaryngol. Head Neck Surg. 2013, 139, 371–381. [Google Scholar] [CrossRef]
- Toro, C.; Robiony, M.; Costa, F.; Zerman, N.; Politi, M. Feasibility of preoperative planning using anatomical facsimile models for mandibular reconstruction. Head Face Med. 2007, 3, 1006–1011. [Google Scholar] [CrossRef]
- Zheng, G.-S.; Su, Y.-X.; Liao, G.-Q.; Liu, H.-C.; Zhang, S.-E.; Liang, L.-Z. Mandibular reconstruction assisted by preoperative simulation and accurate transferring templates: Preliminary report of clinical application. J. Oral Maxillofac. Surg. 2013, 71, 1613–1618. [Google Scholar] [CrossRef] [PubMed]
- Seikaly, H.; Idris, S.; Chuka, R.; Jeffrey, C.; Dzioba, A.; Makki, F.; Logan, H.; O’Connell, D.A.; Harris, J.; Ansari, K.; et al. The Alberta Reconstructive Technique: An occlusion-driven and digitally based jaw reconstruction. Laryngoscope 2019, 129, S1–S14. [Google Scholar] [CrossRef] [PubMed]
- Schepers, R.H.; Raghoebar, G.M.; Vissink, A.; Stenekes, M.W.; Kraeima, J.; Roodenburgm, J.L.; Reintsema, H.; Witjes, M.J. Accuracy of fibula reconstruction using patient-specific CAD/CAM reconstruction plates and dental implants: A new modality for functional reconstruction of mandibular defects. J. Craniomaxillofac. Surg. 2015, 43, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Avraham, T.; Franco, P.; Brecht, L.E.; Ceradini, D.J.; Saadeh, P.B.; Hirsch, D.L.; Levine, J.P. Functional outcomes of virtually planned free fibula flap reconstruction of the mandible. Plast. Reconstr. Surg. 2014, 134, 628e–6234e. [Google Scholar] [CrossRef] [PubMed]
- Kramer, F.J.; Dempf, R.; Bremer, B. Efficacy of dental implants placed into fibula-free flaps for orofacial reconstruction. Clin. Oral Implants Res. 2005, 16, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Seikaly, H.; Chau, J.; Li, F.; Driscoll, B.; Seikaly, D.; Calhoun, J.; Calhoun, K.H. Bone that best matches the properties of the mandible. J. Otolaryngol. 2003, 32, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Ide, Y.; Matsunaga, S.; Harris, J.; O’Connell, D.; Seikaly, H.; Wolfaardt, J. Anatomical examination of the fibula: Digital imaging study for osseointegrated implant installation. J. Otolaryngol. Head Neck Surg. 2015, 44, 1. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, D.A. Fibula free flap. Plast. Reconstr. Surg. 1989, 84, 71–79. [Google Scholar] [CrossRef]
- Hayden, R.E.; Mullin, D.P.; Patel, A.K. Reconstruction of the segmental mandibular defect. Curr. Opin. Otolaryngol. Head Neck Surg. 2012, 20, 231–236. [Google Scholar] [CrossRef]
- Matsuurra, M.; Ohno, K.; Michi, K.; Egawa, K.; Takiguchi, R. Clinicoanatomic examination of the fibula: Anatomic basis for dental implant placement. Int. J. Oral Maxillofac. Implants 1999, 14, 879–884. [Google Scholar]
- Niimil, A.; Ozekil, K.; Uedal, M.; Nakayama, B. A comparative study of removal torque of endosseous implants in the fibula, iliac crest and scapula of cadavers: Preliminary report. Clin. Oral Implants Res. 1997, 8, 286–289. [Google Scholar] [CrossRef] [PubMed]
- Ivanoff, C.J.; Sennerby, L.; Lekholm, U. Influence of mono- and bicortical anchorage on the integration of titanium implants. Int. J. Oral Maxillofac. Surg. 1996, 25, 229–235. [Google Scholar] [CrossRef]
- Seikaly, H.; Maharaj, M.; Rieger, J.; Harris, J. Functional outcomes after primary mandibular resection and reconstruction with the fibular free flap. J. Otolaryngol. 2005, 34, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Logan, H.; Wolfaardt, J.; Boulanger, P.; Hodgetts, B.; Seikaly, H. Exploratory benchtop study evaluating the use of surgical design and simulation in fibula free flap mandibular reconstruction. J. Otolaryngol. Head Neck Surg. 2013, 42, 42. [Google Scholar] [CrossRef]
- Barber, B.R.; Dziegelewski, P.T.; Chuka, R.; O’Connell, D.; Harris, J.R.; Seikaly, H. Bone-impacted fibular free flap: Long-term dental implant success and complications compared to traditional fibular free tissue transfer. Head Neck 2015, 38 (Suppl. S1), E1783–E1787. [Google Scholar] [CrossRef]
- Dziegielewski, P.T.; Mlynarek, A.M.; Harris, J.R.; Hrdlicka, A.; Barber, B.; Al-Qahtani, K.; Wolfaardt, J.; Raboud, D.; Seikaly, H. Bone impacted fibular free flap: A novel technique to increase bone density for dental implantation in osseous reconstruction. Head Neck 2013, 36, 1648–1653. [Google Scholar] [CrossRef]

| Patient | Age (Years) | Sex | Diagnosis | Jaw Defect |
|---|---|---|---|---|
| 1 | 46 | F | Ameloblastoma | Maxilla |
| 2 | 27 | M | Hemangioma | Maxilla |
| 3 | 61 | M | SCC | Maxilla |
| 4 | 23 | M | Ameloblastoma | Mandible |
| 5 | 49 | M | Keratocyst | Maxilla |
| 6 | 56 | F | ORN | Maxilla |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Idris, S.; Logan, H.; Tabet, P.; Osswald, M.; Nayar, S.; Seikaly, H. The Accuracy of 3D Surgical Design and Simulation in Prefabricated Fibula Free Flaps for Jaw Reconstruction. J. Pers. Med. 2022, 12, 1766. https://doi.org/10.3390/jpm12111766
Idris S, Logan H, Tabet P, Osswald M, Nayar S, Seikaly H. The Accuracy of 3D Surgical Design and Simulation in Prefabricated Fibula Free Flaps for Jaw Reconstruction. Journal of Personalized Medicine. 2022; 12(11):1766. https://doi.org/10.3390/jpm12111766
Chicago/Turabian StyleIdris, Sherif, Heather Logan, Paul Tabet, Martin Osswald, Suresh Nayar, and Hadi Seikaly. 2022. "The Accuracy of 3D Surgical Design and Simulation in Prefabricated Fibula Free Flaps for Jaw Reconstruction" Journal of Personalized Medicine 12, no. 11: 1766. https://doi.org/10.3390/jpm12111766
APA StyleIdris, S., Logan, H., Tabet, P., Osswald, M., Nayar, S., & Seikaly, H. (2022). The Accuracy of 3D Surgical Design and Simulation in Prefabricated Fibula Free Flaps for Jaw Reconstruction. Journal of Personalized Medicine, 12(11), 1766. https://doi.org/10.3390/jpm12111766







