Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—The Amount of Posterior Crossbite Correction
Abstract
:1. Introduction
2. Materials and Methods
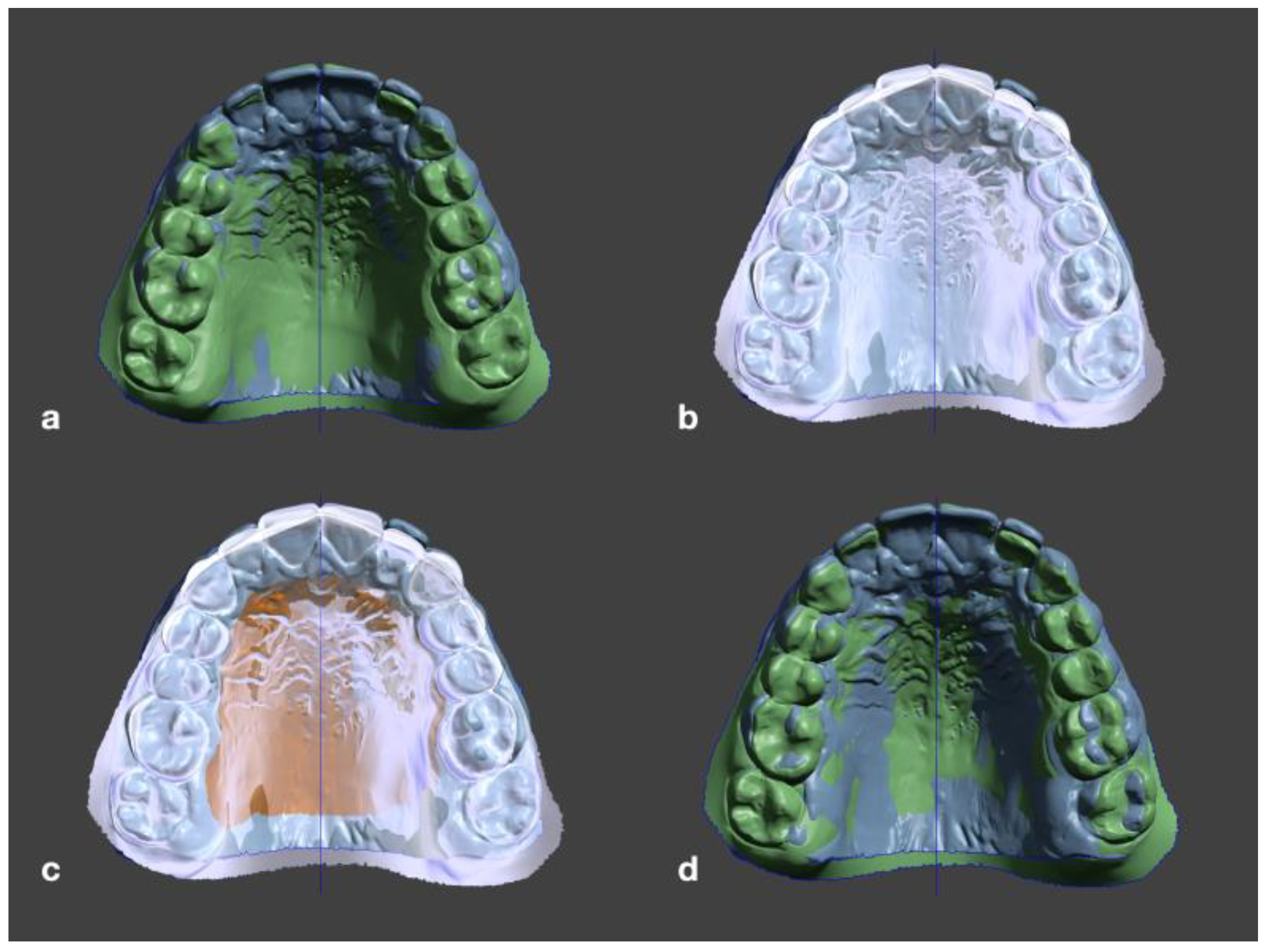
2.1. Measurement Process
2.2. Statistical Analysis
3. Results
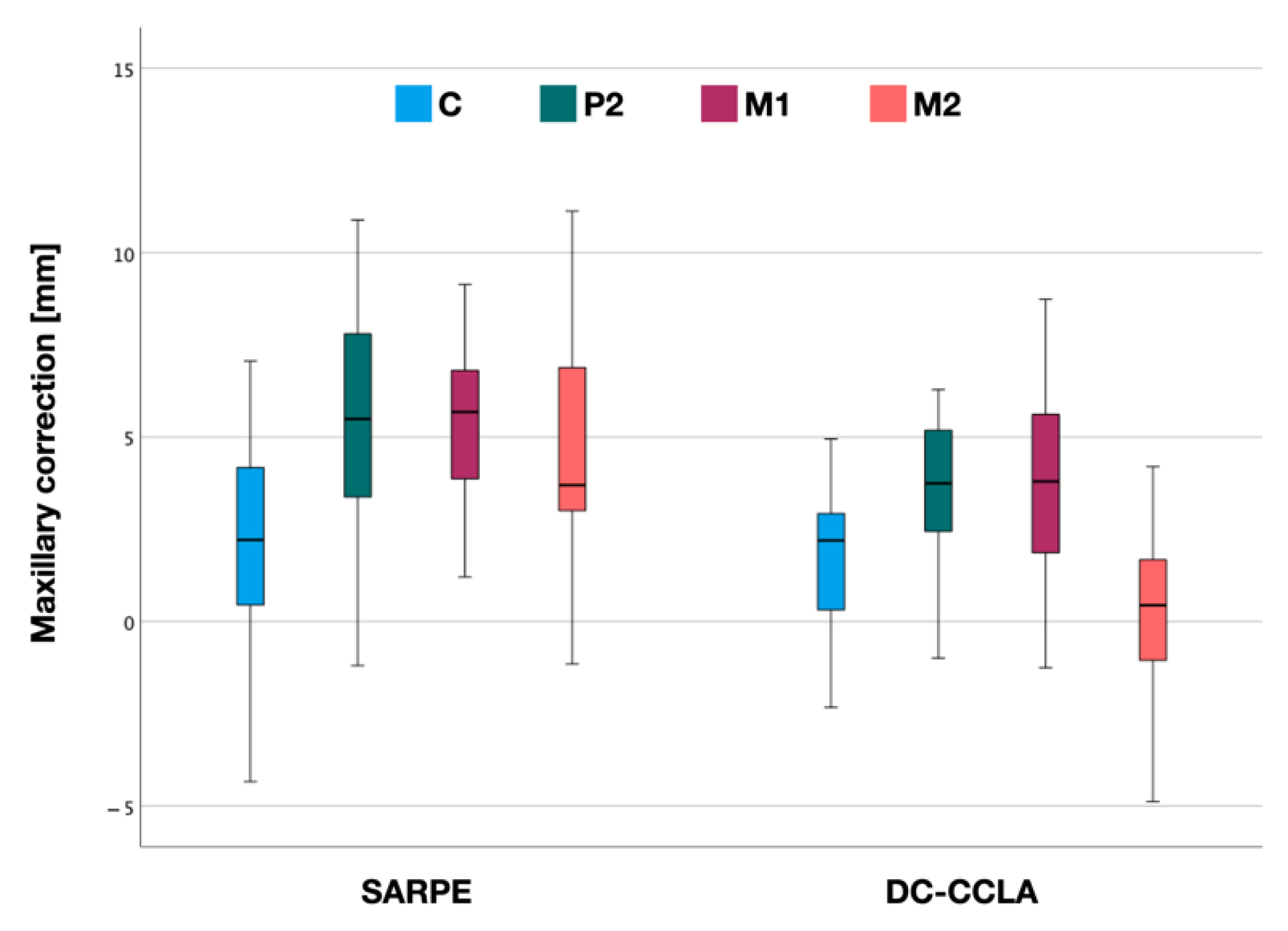
3.1. Maxillary Correction
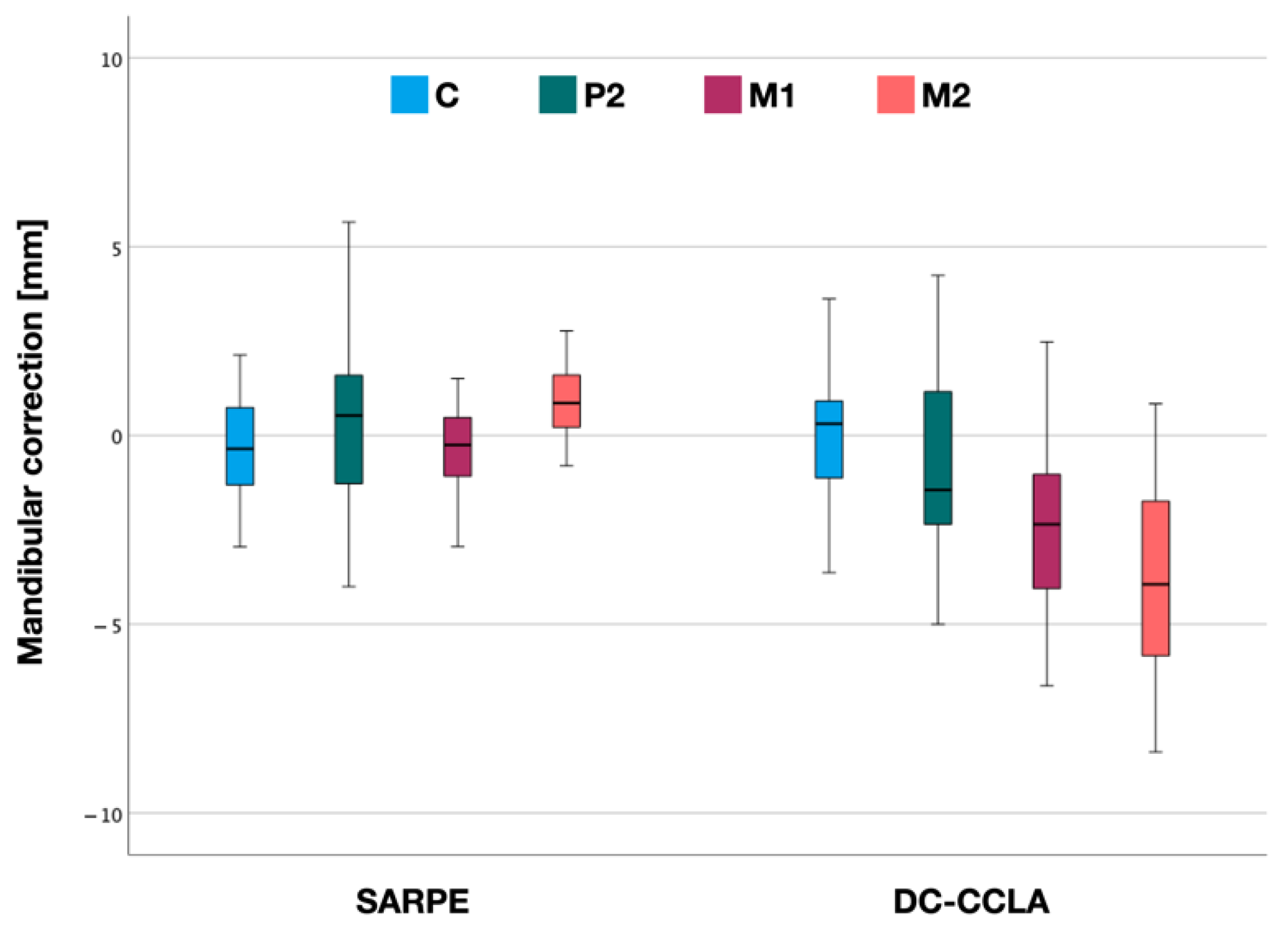
3.2. Mandibular Correction
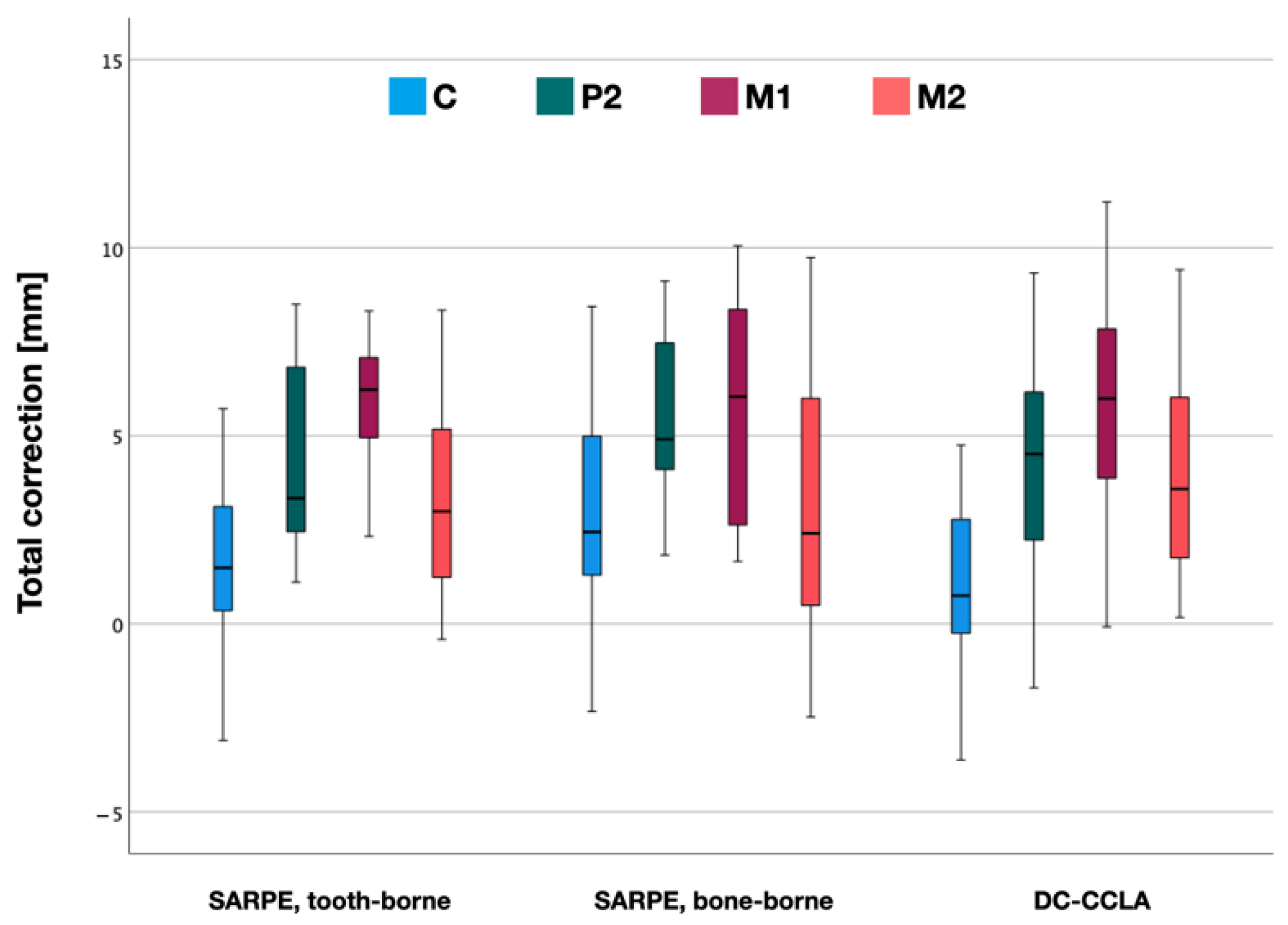
3.3. Total Crossbite Correction
4. Discussion
Strength and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global Distribution of Malocclusion Traits: A Systematic Review. Dental Press, J. Orthod. 2018, 23, e1–e10. [Google Scholar] [CrossRef] [PubMed]
- Hensel, E.; Born, G.; Körber, V.; Altvater, T.; Gesch, D. Prevalence of Defined Symptoms of Malocclusion among Probands Enrolled in the Study of Health in Pomerania (SHIP)* in the Age Group from 20 to 49 Years. J. Orofac. Orthop. 2003, 64, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Ugolini, A.; Agostino, P.; Silvestrini-Biavati, A.; Harrison, J.E.; Batista, K.B.S.L. Orthodontic Treatment for Posterior Crossbites. Cochrane Database Syst. Rev. 2021, 2021, 1–87. [Google Scholar] [CrossRef]
- Borrie, F.R.P.; Bearn, D.R.; Innes, N.P.T.; Iheozor-Ejiofor, Z. Interventions for the Cessation of Non-Nutritive Sucking Habits in Children. Cochrane Database Syst. Rev. 2015, 2015, CD008694. [Google Scholar] [CrossRef]
- Schmid, K.M.; Kugler, R.; Nalabothu, P.; Bosch, C.; Verna, C. The Effect of Pacifier Sucking on Orofacial Structures: A Systematic Literature Review. Prog. Orthod. 2018, 19, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boronat-Catalá, M.; Montiel-Company, J.M.; Bellot-Arcís, C.; Almerich-Silla, J.M.; Catalá-Pizarro, M. Association between Duration of Breastfeeding and Malocclusions in Primary and Mixed Dentition: A Systematic Review and Meta-Analysis. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Little, R.M. Stability and Relapse of Mandibular Anterior Alignment: University of Washington Studies. Semin. Orthod. 1999, 5, 191–204. [Google Scholar] [CrossRef]
- Van de Velde, A.-S.; De Boodt, L.; Cadenas de Llano-Pérula, M.; Laenen, A.; Willems, G. Short Term Effects of Interceptive Expansion Treatment: A Prospective Study. Eur. J. Orthod. 2021, 43, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Melsen, B. Palatal Growth Studied on Human Autopsy Material. A Histologic Microradiographic Study. Am. J. Orthod. 1975, 68, 42–54. [Google Scholar] [CrossRef]
- Suri, L.; Taneja, P. Surgically Assisted Rapid Palatal Expansion: A Literature Review. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Ghoneima, A.; Abdel-Fattah, E.; Hartsfield, J.; El-Bedwehi, A.; Kamel, A.; Kula, K. Effects of Rapid Maxillary Expansion on the Cranial and Circummaxillary Sutures. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 510–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angelieri, F.; Cevidanes, L.H.S.; Franchi, L.; Gonçalves, J.R.; Benavides, E.; McNamara, J.A. Midpalatal Suture Maturation: Classification Method for Individual Assessment before Rapid Maxillary Expansion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 759–769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonello, D.L.; Ladewig, V.D.M.; Guedes, F.P.; Conti, A.C.D.C.F.; Almeida-Pedrin, R.R.; Capelozza-Filho, L. Midpalatal Suture Maturation in 11- to 15-Year-Olds: A Cone-Beam Computed Tomographic Study. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Isfeld, D.; Lagravere, M.; Leon-Salazar, V.; Flores-Mir, C. Novel Methodologies and Technologies to Assess Mid-Palatal Suture Maturation: A Systematic Review. Head Face Med. 2017, 13, 1–15. [Google Scholar] [CrossRef]
- Hamedi Sangsari, A.; Sadr-Eshkevari, P.; Al-Dam, A.; Friedrich, R.E.; Freymiller, E.; Rashad, A. Surgically Assisted Rapid Palatomaxillary Expansion with or Without Pterygomaxillary Disjunction: A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2016, 74, 338–348. [Google Scholar] [CrossRef]
- Koudstaal, M.J.; Wolvius, E.B.; Schulten, A.J.M.; Hop, W.C.J.; van der Wal, K.G.H. Stability, Tipping and Relapse of Bone-Borne versus Tooth-Borne Surgically Assisted Rapid Maxillary Expansion; a Prospective Randomized Patient Trial. Int. J. Oral Maxillofac. Surg. 2009, 38, 308–315. [Google Scholar] [CrossRef]
- Blæhr, T.L.; Mommaerts, M.Y.; Kjellerup, A.D.; Starch-Jensen, T. Surgically Assisted Rapid Maxillary Expansion with Bone-Borne versus Tooth-Borne Distraction Appliances—A Systematic Review. Int. J. Oral Maxillofac. Surg. 2019, 48, 492–501. [Google Scholar] [CrossRef]
- Jia, H.; Zhuang, L.; Zhang, N.; Bian, Y.; Li, S. Comparison of Skeletal Maxillary Transverse Deficiency Treated by Microimplant-Assisted Rapid Palatal Expansion and Tooth-Borne Expansion during the Post-Pubertal Growth Spurt Stage: A Prospective Cone Beam Computed Tomography Study. Angle Orthod. 2021, 91, 36–45. [Google Scholar] [CrossRef]
- Celenk-Koca, T.; Erdinc, A.E.; Hazar, S.; Harris, L.; English, J.D.; Akyalcin, S. Evaluation of Miniscrew-Supported Rapid Maxillary Expansion in Adolescents: A Prospective Randomized Clinical Trial. Angle Orthod. 2018, 88, 702–709. [Google Scholar] [CrossRef] [Green Version]
- Colak, O.; Paredes, N.A.; Elkenawy, I.; Torres, M.; Bui, J.; Jahangiri, S.; Moon, W. Tomographic Assessment of Palatal Suture Opening Pattern and Pterygopalatine Suture Disarticulation in the Axial Plane after Midfacial Skeletal Expansion. Prog. Orthod. 2020, 21, 1–9. [Google Scholar] [CrossRef]
- de Oliveira, C.B.; Ayub, P.; Ledra, I.M.; Murata, W.H.; Suzuki, S.S.; Ravelli, D.B.; Santos-Pinto, A. Microimplant Assisted Rapid Palatal Expansion vs. Surgically Assisted Rapid Palatal Expansion for Maxillary Transverse Discrepancy Treatment. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, P.H.A.; Moura, L.B.; Trento, G.S.; Holzinger, D.; Gabrielli, M.A.C.; Gabrielli, M.F.R.; Pereira Filho, V.A. Surgically Assisted Rapid Maxillary Expansion: A Systematic Review of Complications. Int. J. Oral Maxillofac. Surg. 2020, 49, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Asscherickx, K.; Govaerts, E.; Aerts, J.; Vande Vannet, B. Maxillary Changes with Bone-Borne Surgically Assisted Rapid Palatal Expansion: A Prospective Study. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, F.; Solidoro, L.; Bartolucci, M.L.; Incerti Parenti, S.; Paganelli, C.; Alessandri-Bonetti, G. Skeletal and Dental Effects of Surgically Assisted Rapid Palatal Expansion: A Systematic Review of Randomized Controlled Trials. Eur. J. Orthod. 2020, 42, 434–440. [Google Scholar] [CrossRef]
- Brandtner, C.; Hachleitner, J.; Rippel, C.; Krenkel, C.; Gaggl, A. Long-Term Skeletal and Dental Stability after Orthognathic Surgery of the Maxillo-Mandibular Complex in Class II Patients with Transverse Discrepancies. J. Cranio-Maxillofac. Surg. 2015, 43, 1516–1521. [Google Scholar] [CrossRef]
- Silverstein, K.; Quinn, P.D. Surgically-Assisted Rapid Palatal Expansion for Management of Transverse Maxillary Deficiency. J. Oral Maxillofac. Surg. 1997, 55, 725–727. [Google Scholar] [CrossRef]
- Pauls, A.H. Therapeutic Accuracy of Individualized Brackets in Lingual Orthodontics. J. Orofac. Orthop. 2010, 71, 348–361. [Google Scholar] [CrossRef]
- Pauls, A.; Nienkemper, M.; Schwestka-Polly, R.; Wiechmann, D. Therapeutic Accuracy of the Completely Customized Lingual Appliance WIN: A Retrospective Cohort Study. J. Orofac. Orthop. 2017, 78, 52–61. [Google Scholar] [CrossRef] [Green Version]
- Grauer, D.; Proffit, W.R. Accuracy in Tooth Positioning with a Fully Customized Lingual Orthodontic Appliance. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 433–443. [Google Scholar] [CrossRef]
- Lossdörfer, S.; Bieber, C.; Schwestka-Polly, R.; Wiechmann, D. Analysis of the Torque Capacity of a Completely Customized Lingual Appliance of the next Generation. Head Face Med. 2014, 10, 1–9. [Google Scholar] [CrossRef]
- Alouini, O.; Knösel, M.; Blanck-Lubarsch, M.; Helms, H.J.; Wiechmann, D. Controlling Incisor Torque with Completely Customized Lingual Appliances. J. Orofac. Orthop. 2020, 81, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Owen, B.; Tran, B.; Guan, R.; Luo, J.; Granley, A.; Carey, J.P.; Major, P.W.; Romanyk, D.L. The Biomechanics of Posterior Maxillary Arch Expansion Using Fixed Labial and Lingual Appliances. Angle Orthod. 2020, 90, 688–694. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beyling, F.; Klang, E.; Niehoff, E.; Schwestka-Polly, R.; Helms, H.J.; Wiechmann, D. Class II Correction by Maxillary En Masse Distalization Using a Completely Customized Lingual Appliance and a Novel Mini-Screw Anchorage Concept–Preliminary Results. Head Face Med. 2021, 17, 1–10. [Google Scholar] [CrossRef]
- Stamm, T.; Böttcher, D.; Kleinheinz, J. The University Münster Model Surgery System for Orthognathic Surgery-The Digital Update. Head Face Med. 2021, 17, 1–10. [Google Scholar] [CrossRef]
- Dahlberg, G. Statistical Methods for the Medical and Biological Students; Alien and Unwin: Sydney, Australia, 1940. [Google Scholar]
- Chamberland, S.; Proffit, W.R. Short-Term and Long-Term Stability of Surgically Assisted Rapid Palatal Expansion Revisited. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 815–823. [Google Scholar] [CrossRef] [Green Version]
- De Luca Canto, G.; Pachêco-Pereira, C.; Lagravere, M.O.; Flores-Mir, C.; Major, P.W. Intra-Arch Dimensional Measurement Validity of Laser-Scanned Digital Dental Models Compared with the Original Plaster Models: A Systematic Review. Orthod. Craniofacial Res. 2015, 18, 65–76. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Diagnostic Accuracy and Measurement Sensitivity of Digital Models for Orthodontic Purposes: A Systematic Review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 161–170. [Google Scholar] [CrossRef]
- Kunz, F.; Linz, C.; Baunach, G.; Böhm, H.; Meyer-Marcotty, P. Expansion Patterns in Surgically Assisted Rapid Maxillary Expansion: Transpalatal Distractor versus Hyrax Appliance. J. Orofac. Orthop. 2016, 77, 357–365. [Google Scholar] [CrossRef]
- Jafari, A.; Shetty, K.S.; Kumar, M. Study of Stress Distribution and Displacement of Various Craniofacial Structures Following Application of Transverse Orthopedic Forces-A Three-Dimensional FEM Study. Angle Orthod. 2003, 73, 12–20. [Google Scholar] [CrossRef]
- Holberg, C.; Steinhäuser, S.; Rudzki, I. Surgically Assisted Rapid Maxillary Expansion: Midfacial and Cranial Stress Distribution. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Habersack, K.; Becker, J.; Ristow, O.; Paulus, G.W. Dental and Skeletal Effects of Two-Piece and Three-Piece Surgically Assisted Rapid Maxillary Expansion with Complete Mobilization: A Retrospective Cohort Study. J. Oral Maxillofac. Surg. 2014, 72, 2278–2288. [Google Scholar] [CrossRef] [PubMed]
- Holberg, C. Effects of Rapid Maxillary Expansion on the Cranial Base–An FEM-Analysis. J. Orofac. Orthop. 2005, 66, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Gogna, N.; Johal, A.S.; Sharma, P.k. The Stability of Surgically Assisted Rapid Maxillary Expansion (SARME): A Systematic Review. J. Cranio-Maxillofac. Surg. 2020, 48, 845–852. [Google Scholar] [CrossRef]
- Bishara, S.E.; Jakobsen, J.R.; Treder, J.; Nowak, A. Arch Width Changes from 6 Weeks to 45 Years of Age. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 401–409. [Google Scholar] [CrossRef]
- Dager, M.M.; McNamara, J.A.; Baccetti, T.; Franchi, L. Aging in the Craniofacial Complex. Angle Orthod. 2008, 78, 440–444. [Google Scholar] [CrossRef] [Green Version]
- Brignardello-Petersen, R. Uncertainty about the Average Rate of Complications after Surgically Assisted Rapid Maxillary Expansion Owing to Limitations in a Systematic Review, but the Rate Seems to Vary Importantly across Studies. J. Am. Dent. Assoc. 2020, 151, e25. [Google Scholar] [CrossRef]
- Magnusson, A.; Bjerklin, K.; Kim, H.; Nilsson, P.; Marcusson, A. Three-Dimensional Assessment of Transverse Skeletal Changes after Surgically Assisted Rapid Maxillary Expansion and Orthodontic Treatment: A Prospective Computerized Tomography Study. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 825–833. [Google Scholar] [CrossRef]
- Gül, A.; Pieter de Gijt, J.; Wolvius, E.B.; Koudstaal, M.J. Patient Experience and Satisfaction of Surgically Assisted Rapid Maxillary Expansion and Mandibular Midline Distraction. J. Cranio-Maxillofac. Surg. 2021, 49, 649–654. [Google Scholar] [CrossRef]
- Habersack, K.; Karoglan, A.; Sommer, B.; Benner, K.U. High-Resolution Multislice Computerized Tomography with Multiplanar and 3-Dimensional Reformation Imaging in Rapid Palatal Expansion. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 776–781. [Google Scholar] [CrossRef]




| SARPE | DC-CCLA | p | |
|---|---|---|---|
| Female | 19 (44%) | 25 (66%) | |
| age (years) at T0 | 26.7 ± 9.7 | 32.1 ± 12.3 | 0.086 |
| age (years) at T1 | 30.1 ± 9.6 | 34.4 ± 12.4 | 0.255 |
| Male | 24 (56%) | 13 (34%) | |
| age (years) at T0 | 27.8 ± 9.8 | 27.0 ± 14.2 | 0.404 |
| age (years) at T1 | 30.9 ± 9.5 | 30.0 ± 14.4 | 0.276 |
| Angle class I | 1 | 20 | |
| Angle class II | 14 | 13 | |
| Angle class III | 28 | 5 |
| Group | Jaw | Tooth | Mean | SD | 95% CI | Min | Max |
|---|---|---|---|---|---|---|---|
| SARPE | Mx | C | 2.28 | 3.02 | 1.26–3.30 | −4.34 | 11.11 |
| P2 | 5.40 | 2.98 | 4.39–6.41 | −1.19 | 10.89 | ||
| M1 | 5.69 | 2.60 | 4.80–6.57 | 1.21 | 14.79 | ||
| M2 | 4.71 | 2.76 | 3.78–5.64 | −1.15 | 11.13 | ||
| Md | C | −0.44 | 1.66 | −1.05–0.17 | −5.35 | 2.13 | |
| P2 | 0.36 | 2.31 | −0.49–1.21 | −4.00 | 5.65 | ||
| M1 | −0.36 | 1.52 | −0.92–0.20 | −3.51 | 3.19 | ||
| M2 | 0.86 | 1.20 | 0.42–1.30 | −3.36 | 2.77 | ||
| total | C | 2.21 | 2.62 | 1.23–3.18 | −3.10 | 8.44 | |
| P2 | 4.82 | 2.68 | 3.82–5.82 | −1.68 | 9.11 | ||
| M1 | 5.82 | 2.35 | 4.94–6.70 | 1.66 | 10.05 | ||
| M2 | 3.26 | 3.05 | 2.12–4.40 | −2.47 | 9.74 | ||
| DC-CCLA | Mx | C | 1.78 | 1.91 | 1.08–2.48 | −2.33 | 4.95 |
| P2 | 4.07 | 2.85 | 3.02–5.11 | −0.99 | 10.23 | ||
| M1 | 3.66 | 2.45 | 2.77–4.56 | −1.25 | 8.74 | ||
| M2 | 0.36 | 2.64 | −0.61–1.33 | −6.59 | 6.43 | ||
| Md | C | 0.20 | 1.67 | −0.49–0.89 | −3.63 | 3.62 | |
| P2 | −0.69 | 2.53 | −1.73–0.36 | −5.00 | 4.24 | ||
| M1 | −2.70 | 2.26 | −3.63–−1.77 | −6.63 | 2.48 | ||
| M2 | −3.54 | 2.64 | −4.63–−2.45 | −8.38 | 0.84 | ||
| total | C | 1.29 | 2.10 | 0.36–2.22 | −3.62 | 4.75 | |
| P2 | 4.38 | 2.71 | 3.17–5.58 | −1.70 | 9.33 | ||
| M1 | 6.00 | 2.78 | 4.77–7.23 | −0.08 | 11.22 | ||
| M2 | 4.11 | 2.86 | 2.85–5.38 | 0.17 | 9.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmid, J.Q.; Gerberding, E.; Hohoff, A.; Kleinheinz, J.; Stamm, T.; Middelberg, C. Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—The Amount of Posterior Crossbite Correction. J. Pers. Med. 2022, 12, 1893. https://doi.org/10.3390/jpm12111893
Schmid JQ, Gerberding E, Hohoff A, Kleinheinz J, Stamm T, Middelberg C. Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—The Amount of Posterior Crossbite Correction. Journal of Personalized Medicine. 2022; 12(11):1893. https://doi.org/10.3390/jpm12111893
Chicago/Turabian StyleSchmid, Jonas Q., Elena Gerberding, Ariane Hohoff, Johannes Kleinheinz, Thomas Stamm, and Claudius Middelberg. 2022. "Non-Surgical Transversal Dentoalveolar Compensation with Completely Customized Lingual Appliances versus Surgically Assisted Rapid Palatal Expansion in Adults—The Amount of Posterior Crossbite Correction" Journal of Personalized Medicine 12, no. 11: 1893. https://doi.org/10.3390/jpm12111893






