1. Introduction
Neurosurgeons have traditionally spent a great deal of time attempting to prevent injury in the so-called eloquent areas of the brain. Revolutionary advancements in neuroimaging technologies and intraoperative brain mapping technologies have expanded our ability to preserve motor and language functions in resective brain surgery while continuing to increase the extent of resection [
1,
2]. However, it is also clear that glioma patients still often present post-operatively with more subtle deficits in higher-order complex functions [
3,
4,
5,
6]. Complex neuro-behavioral functions, such as memory, attention, executive functioning, and emotion are commonly disrupted in brain tumor surgery, and can prevent patients from integrating back into society and the workforce [
7]. Therefore, there has been a growing interest by some to reduce the cognitive footprint of supratentorial, intra-axial brain tumor surgery [
8].
One reason we have previously been held back in the ability to optimize post-operative cognitive morbidity is because it has not been entirely clear exactly what we can and cannot do during surgery to avoid these problems. Although our study and subsequent understanding of brain anatomy responsible for language and motor functions has grown considerably in the last few decades, the neurosurgical community has generally maintained a less thorough familiarity with anatomy responsible for higher-order functions. One concept which has emerged from the field of neuroscience which may address this issue includes large-scale brain networks. These networks include reproducible areas that demonstrate highly synchronized activity based on specific functions or at rest, and are often measured with changes in blood oxygenation as a proxy for functional connectivity [
9,
10]. More recently, it has also been found that there are almost always large-scale white matter connections linking functionally connected regions within a structural network, illustrating:
regions that fire together are also wired together [
11,
12,
13,
14,
15]. Information on the structural and functional connectome has allowed for more precise maps and localization of complex patient symptomology that is not confined to isolated cortical regions [
16,
17].
Despite there being a large body of literature supporting this concept in the general field of neuroscience, the importance of the large-scale brain networks has still yet to deeply penetrate regular neurosurgical thinking. One reason for this stagnation may be because the clinical evidence and importance behind non-traditional, large-scale brain networks other than language and motor systems has yet to be systematically reviewed, and this may ultimately cause some to believe their presence may not be relevant for neurosurgery. Given that various neurological diseases and symptomology can often be better understood through consideration of their effects on networks [
16], failure to consider brain network architecture hinders our successful movement as a community toward personalized neurosurgical treatments. Thus, here we attempt to address these concerns through a comprehensive review which aims to examine and outline the large body of available literature on this topic. Further, we raise the strong possibility that the features seen in other papers also apply to patients with brain tumors and may require further consideration moving forward. Through a brief systematic review, we outline and discuss the relevance of non-traditional eloquent areas in neurosurgery, specifically as it relates to damage or dysfunction in the large-scale brain networks: default mode network (DMN), central executive network (CEN), salience network (SN), dorsal attention network (DAN), and ventral attention network (VAN).
2. Materials and Methods
2.1. Search Strategy
A systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. An exhaustive screening process was completed using the electronic database PubMed. A search string was utilized with the following terms: “tractography OR fMRI” AND “memory OR language OR speech OR motor function OR attention OR depression OR neurologic deficit” AND “default mode OR central executive OR salience network OR sensorimotor OR language”. This search was conducted on 1 August 2021, for the period 2011–2021.
2.2. Selection Criteria
Articles were included which demonstrated the importance of the non-traditional, large-scale brain networks in relation to clinical symptoms or general disease states. Articles were included if they (1) mentioned fMRI or DTI techniques, (2) discussed the DMN, CEN, SN, DAN, VAN or related connections and network names, and (3) mentioned damage to or dysfunction in a network or related network alterations in association with neurologic, cognitive, or emotional deficits. Articles which clearly defined a disease state based on specific network changes in comparison with healthy controls were also examined. All article types, including reviews and conference abstracts, were included if the above criteria were met. Articles including only healthy subjects or traditionally known networks, such as language or motor networks, were excluded. Studies unable to provide an English text or which were strictly methodology focused were also excluded.
2.3. Screening and Data Extraction
A rigorous screening process was completed using EndNote and Rayyan (
https://rayyan.qcri.org/, accessed on 29 September 2021). Title screening and abstract screening were completed by M.S. and the full-text review was completed by N.D. Included full-texts underwent a comprehensive qualitative review (N.D.) based on specific elements addressed, such as the network implicated, the type of network damage or dysfunction, the disease state, and the specific clinical symptoms implicated. Each article was also graded (M.D.) based on the class of evidence demonstrated.
3. Results
A total of 22,697 articles were screened and 1315 articles underwent full-text review (
Figure 1). Ultimately, 551 full-text articles were included in final analyses and these are summarized below as well as included in the
Supplementary Materials Content 1.
3.1. Study Types
Studies included were generally of moderate study quality and demonstrated class III evidence (n = 524, 95%). Networks were mostly examined with functional connectivity analyses, such as resting-state fMRI to examine network dysfunction (n = 436, 79%) rather than in the context of network damage or structural integrity with DTI (n = 52, 9%). Combined structural-functional analyses were utilized in n = 63 (11%) studies to examine the relationship between network dysfunction in relation to its underlying structural network damage. Depression was the most common diagnosis (n = 124) described in the included studies. This was followed by Schizophrenia (n = 81), Parkinson’s disease (n = 64), Alzheimer’s disease (n = 46), stroke (n = 40), epilepsy (n = 29), and tumor cases (n = 21). These data are presented further and according to individual networks in
Supplementary Materials Content 2, Figures S1 and S2.
3.2. Networks Examined
The DMN (n = 213, 39%) represented the majority of articles identified in the current study. A number of works examined the effects of network disruptions in combination and therefore were further categorized into the most common combinations assessed. A triple network model of the DMN, CEN, and/or SN was the next most commonly studied network (n = 182, 33%). Similarly, the attention networks (VAN and DAN) were only examined in isolation in one study [
18], and instead were mostly studied in combination with the other brain networks or each other (n = 93, 17%). Few studies were identified on the CEN (n = 25, 5%) in the current study. However, a number of studies were excluded that discussed the superior longitudinal fasciculus, a major fiber bundle linking the CEN, but were not clearly discussed in reference to the CEN. Differences in the diagnosis frequency per network are further demonstrated in
Supplementary Materials Content 2, Figure S3.
3.3. Cognitive, Emotional, and Neurologic Deficits
Cognitive deficits (n = 226, 41%), such as in attentional processing, memory, and executive functioning, were the most commonly identified outcomes of network disturbances. This was followed by emotional processing deficits in 26% (n = 143) of studies, mostly in the context of affective traits in depression and/or anxiety. A number of studies were identified which demonstrated deficits in more than one outcome, such as emotion and cognition (6%), motor and cognition (5%), motor alone (4%), language or speech (4%), or many additional deficits together (7%).
Deficits were also analyzed based on their frequency in each network or network combination (
Figure 2). Cognitive deficits demonstrated the largest proportion of all network or network combination deficits in varying amounts (36–56%), except for the SN which mostly consisted of emotional processing deficits (35%) following network disturbance. The CEN and SN demonstrated the most diverse range of symptoms according to frequency, with a noted increase in motor symptoms with the CEN (12%) and language processing or speech deficits with the SN (24%). Disruption of the attention networks (VAN/DAN) in combination with each other or the other networks most commonly led to cognitive deficits (56%).
4. Discussion
In this paper, we have performed the first systematic review that examines and outlines the literature on major non-traditional, large-scale brain networks as it relates to neurosurgery. A large amount of plausible evidence was identified suggesting that disturbances in non-traditional networks can result in severe neurological, cognitive, or emotional deficits. Although it remains unclear if or what specific damage to a brain network causes a specific neurologic deficit, the available literature seems to suggest that at least some deficits will occur when key network regions or their interconnecting fibers are disrupted. However, to date, this information has only been briefly discussed and has yet to be systematically reviewed in a way which can demonstrate their clinical importance for regular neurosurgical thinking. Given these neuroanatomic substrates are commonly encountered during resective brain surgery, below we attempt to briefly characterize their relative importance based on the previous literature and current neurosurgical practices, and also elucidate how features seen in many different papers can be especially relevant to brain tumor patients. Importantly, as a first step, the current review provides a broad overview of the likely clinical importance of these networks and how incorporating their presence in regular neurosurgical thinking may provide us a more nuanced, personalized approach to connectome-based neurosurgery moving forward.
4.1. Who Are the Big Five Non-Traditional Brain Networks?
Brain networks have been found to be central to the organizing principle of the structural and functional brain connectome. Although some networks may be new to many in neurosurgery, it is important to note that the default mode, central executive, salience, dorsal attention, and ventral attention networks are far from fringe in the broader neuroscientific community and have been well-documented over the past 20 years. These networks are made up of highly synchronized cortical regions and the interconnecting white matter bundles between these regions. As it relates to resective brain surgery, the structural integrity of large-scale networks is paramount for patients to maintain a level of functional capacity and metabolic efficiency necessary to subserve complex human functions (
Table 1).
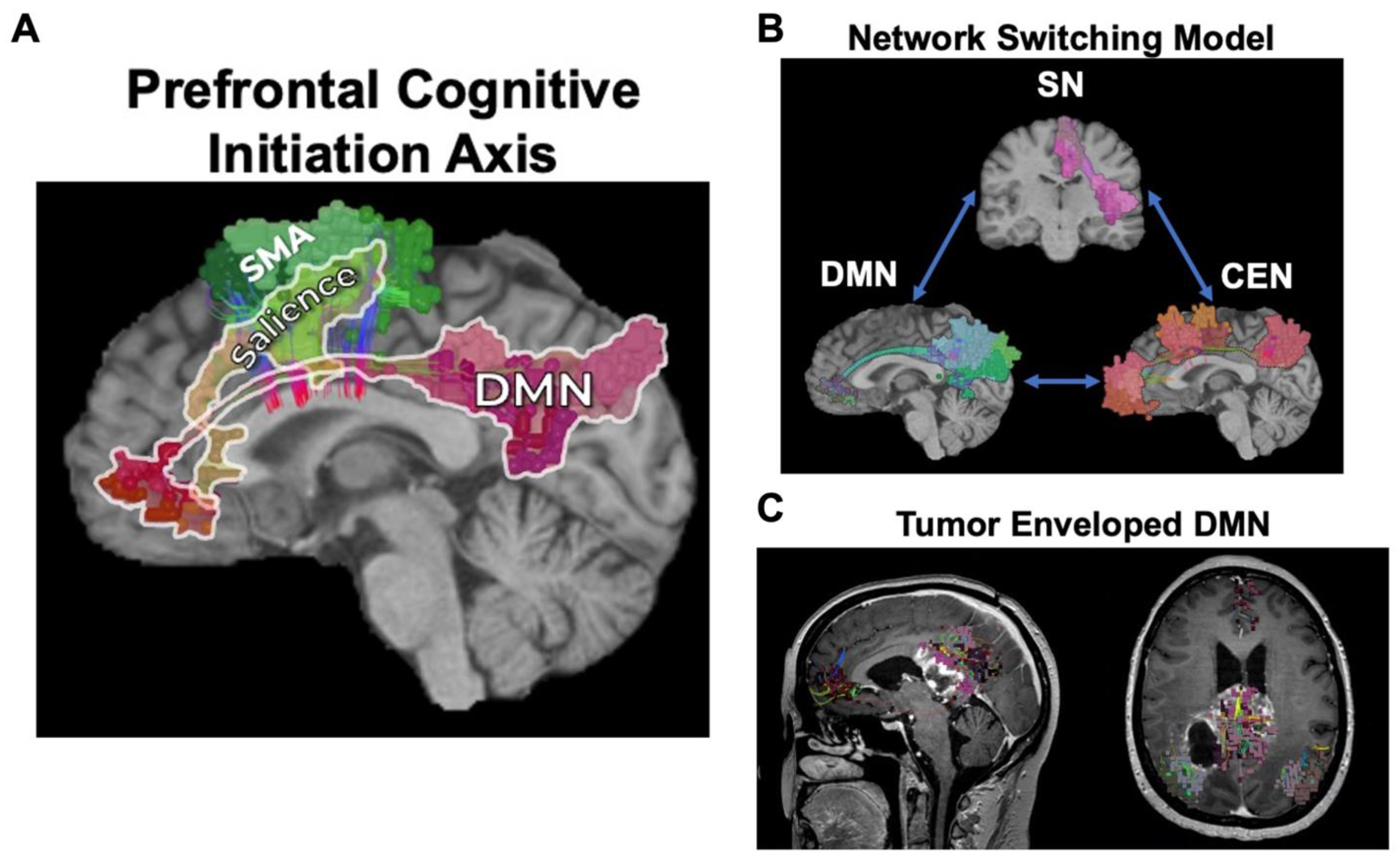
Three canonical resting-state networks which sit at the top of the network hierarchy and define an axis by which the other networks align for complex neuro-behavioral functions are the DMN, CEN, and SN (
Figure 3). Although only briefly discussed previously [
8], results from the current work strongly suggest that disruption of these networks can commonly lead to cognitive and emotional deficits, which are also thought to underlie a number of neuro-psychiatric illnesses such as depression [
19]. In contrast, the attention networks chiefly work in tangent with other large-scale networks for top-down and bottom-up processing of stimuli and to re-orient attention based on internal and external motivations (
Figure 4) [
11,
20,
21]. Unsurprisingly, disruption of the VAN or DAN when in combination with the other higher-order networks most commonly leads to impaired cognitive processes, such as in spatial neglect [
22] and impaired memory [
23]. Given that these five networks seem to be a common feature that explains much of the human functioning we understand in neuroscience and are commonly encountered during resective brain surgery, it is likely safe to say they are more important than previously considered, and that whether they need to be preserved is a question worth asking.
4.2. Evidence for Avoiding Damage to Brain Networks in Brain Tumor Patients
There is no randomized controlled trial showing that not destroying one of these five non-traditional, large-scale networks in a surgery leads to improved neurological outcomes. Despite this limitation, the evidence that damage or dysfunction in these networks causes a cognitive, neurological, or emotional disturbance is relatively vast and should be considered as such. Most of the previous literature has focused on network disturbances in the context of neuro-psychiatric illnesses, where a clear neuroanatomic substrate or lesion is not readily identifiable but the pathophysiology clearly involves widespread dysfunction across numerous spatially distant regions involved in interacting networks [
26,
27]. However, psychiatric symptoms can often be the primary and only symptoms of brain tumors as well due to similar network disturbances which alter neural connectivity [
28,
29] and this has only been recently acknowledged. Therefore, despite some differences between the mechanisms of network disruption, decisions during resective brain surgery may also benefit from consideration of these five non-traditional networks as there are clear deficits and widespread effects associated with their disruption when key network regions or fibers are cut [
30,
31].
Based on this review, a significant proportion of studies demonstrated cognitive and emotional deficits in the context of multiple, interacting brain networks. This is unsurprising given most higher-order functions are not localized to one specific region of brain tissue, but instead rely on numerous dynamic interactions amongst higher-order networks such as the DMN, CEN, and SN (
Figure 5). The importance of these cognitive control networks have been increasingly demonstrated through various lines of evidence [
19,
30,
31,
32], including brain tumor, stroke, and psychiatric patients. Together, these data have suggested that disruption in these networks, often following damage in the medial frontal lobe, may cause cognitive and psychomotor disturbances related to an abnormal allocation of cognitive resources between networks [
30,
31,
33]. An example of this can be seen with butterfly gliomas which often envelop non-traditional networks such as the DMN and/or SN, and when damaged in surgery can result in post-operative abulia and akinetic mutism (
Figure 5) [
33].
Ultimately, without consideration of the large-scale, non-traditional brain networks, we are left with the traditional localizationist view:
if we cut across any of these networks, then no deficit will occur. Alternatively, the available body of evidence found in the current review suggests that if you cut across networks such as the DMN, there may be at least some consequences in some patients, if not most. Simultaneously, it must be noted that these results do not suggest we cannot remove tumors involved in major brain networks. Instead, the current report suggests that considering their connectomic architecture and presence in our thinking during brain tumor surgery may provide additional information of prognostic value for the operating neurosurgeon [
34,
35].
4.3. Brain Network Maps vs. Other Surgical Adjuncts: Mutually Exclusive?
Decisions made during surgery to preserve higher-order functions have previously been made based on incomplete anatomic information that also ignores inter-individual differences in brain structural–functional relationships, often leading to significant consequences [
3,
4,
5,
6,
36]. Brain networks provide clear maps which can define specific onco-functional resection boundaries, or at least offer additional information to the operating neurosurgeon to make more informed decisions during surgery while causing fewer deficits [
8]. However, a common concern expressed by many neurosurgeons is that the consideration of brain networks may not be necessary if one already employs awake surgery techniques to identify eloquent cortices. Nevertheless, it is important to note that raising such concerns may be misleading, as awake surgery and brain network mapping are not mutually exclusive. In fact, these two surgical tools are complementary as awake surgery relies on a strong anatomical understanding of where specific regions are located before surgery [
33,
37,
38]. Network maps provide the best available tool to date to make this anatomy known, and likely provide additional benefits for awake surgeons regardless of previous experience due to there being more details about brain anatomy between individual patients that can be estimated before and during surgery.
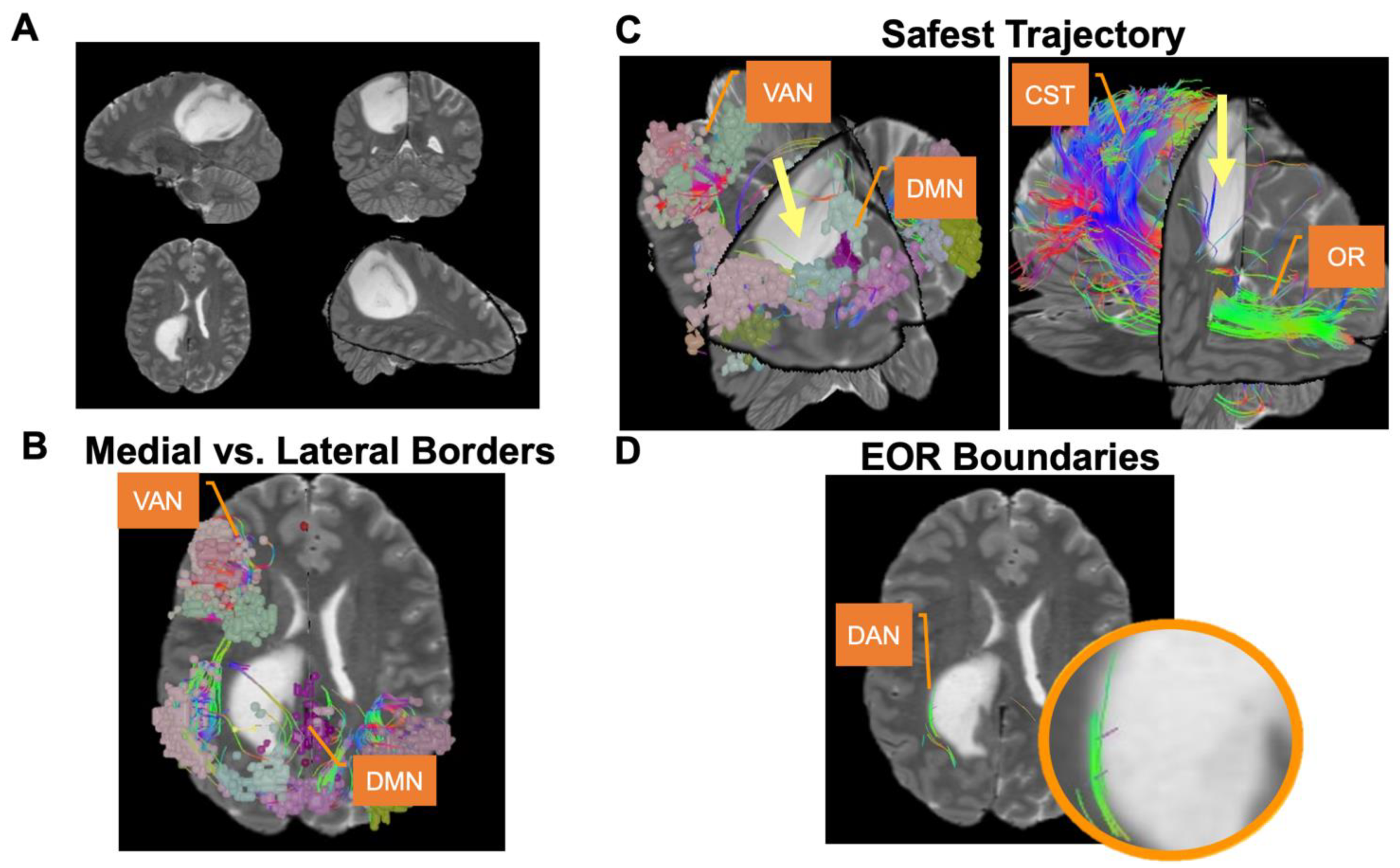
In the pre-operative period, brain network maps can identify the relative risks of specific tumors [
39,
40], outline the functional boundaries of resection [
31,
33], and clarify subtle differences in trajectory according to surrounding networks (
Figure 6) [
41,
42]. However, unlike brain network maps, awake surgery is not appropriate in many cases [
43]. Glioblastoma (GBM) patients often present with substantial pre-operative neurological deficits and therefore are often not suitable awake craniotomy candidates due to an increased risk of adverse events. Unfortunately, maintaining a binary view of “awake or nothing” may make these deficits a self-fulfilling prophesy, where we unknowingly destroy their network which otherwise may just be compressed or edematous.
Furthermore, it is important to note the relative difficulty in mapping higher cognitive functions during awake surgery. For instance, it hard to consider what test protects the default mode network function, or, if you find a positive site for verbal memory, what you should do to keep that area connected to the rest of the system. Although there have been some improvements in the ability to map higher cognitive functions using awake surgery, it remains difficult to save a brain function when the complete anatomy underlying that function is unknown [
37].
4.4. Do You Put Patient Survival at Risk to Preserve the Network?
An important point to address is that using brain network maps does not inherently require decisions to be made in specific patients between destroying a network core or decreasing patient survival by leaving substantially more tumor. Such a question is a drastic oversimplification, and is rarely presented when utilizing brain network maps according to our experience. Instead, a more appropriate question brain networks allow us to pose is: is it worth leaving the last 1–5% of tumor to prevent a specific patient from having serious cognitive problems after this surgery?
In glioma surgery, comparing a 98% resection with good neurologic function with a 100% “complete resection” with somewhat worse function, given that neither is generally curative for most gliomas, is a philosophical question. Although many would argue that an additional 2% extent of resection may only provide negligible additional benefits that do not justify a trade-off in neurologic function, brain network maps allow us to better consider the risks associated with these decisions [
44]. By defining the tumor and personalized surgical plan against clear network boundaries marked by white matter bundles with known functional significance, we may be able to make more informed decisions during surgery on when to and when not to extend the rate of resection according to pre-defined patient onco-functional goals on an individualized patient basis [
45,
46]. We may ultimately choose to ignore this network information due to the inability to preserve a network completely enveloped in tumor, or rather use it to achieve a supramaximal resection up to key network structures to preserve significant functions (
Figure 6) [
41]. Regardless, network information may allow us to better consider the risks and benefits of these surgical decisions, the risks of certain tumors, or even when to consider alternative radiotherapeutic strategies that have continued to advance in precision.
4.5. What We Still Do Not Know
Despite the clear benefits posed with improved knowledge of the brain connectome architecture in neurosurgical patients, there remain a number of areas requiring further research to better leverage this information.
Importantly, if a network is invaded by a tumor, it is still not completely clear how we are to understand if that network is salvageable or not. Leaving residual tumor in a network may not ultimately be worth it if the tumor is disrupting a core network region, and at other times attempting to save a network may be far from surgically feasible or practical. Furthermore, it is unclear if it possible to remove a tumor and save the underlying network, as we could do for an acoustic neuroma, for example [
47]. However, in many cases, brain tractography allows us to consider adjusting the surgical trajectory by just a few millimeters to avoid the network, and still completely remove the tumor and save the network (
Figure 6) [
48].
How do we know if the other side of a network or another region can compensate for losing part of the network? This is a great question for connectomics in the future as we understand a great portion of the human brain maintains a certain degree of redundancy [
49]. A large amount of this redundancy likely originates from the contralateral hemisphere, given most functions are processed bi-hemispherically. When operating in the SMA with a tumor invading the salience network, preservation of this network’s transcallosal fibers (“crossed FAT”) may allow patient recovery from SMA syndrome [
50]. However, in our experience, the other side of a network does not always compensate well for losses in core parts of a network, such as with the default mode network, and this should be considered prospectively. Improved statistical modeling techniques of the brain connectome are underway to develop clinically applicable metrics which can estimate these neurological features; however, further clinical study is necessary [
49].
Lastly, it remains unclear to what degree small distant parts of a network matter if they are not part of its core. For instance, the CEN is a three-part network with parcellation clusters in the frontopolar region, posterior DLPFC, and inferior parietal lobe (
Figure 3). Damaging the middle aspect of this network and key fibers linking all other frontal and parietal parcellations likely disrupts the entire network’s function. However, the ability to sacrifice a portion of the frontal cluster or parcellations in the periphery without disrupting overall network functioning remains unclear, and we have seen cases where disconnecting these regions from the network in surgery creates mild clinical deficits.
These are just some of the important questions that should be the subject of future research efforts. It is important to know, however, that the reason these answers remain unknown is because up until this point, we did not have a common nomenclature for studying these networks, nor sufficient tools for having meaningful discussions and developing technique refinements in this area. Moving forward, consideration of the non-traditional brain networks in regular neurosurgical thinking provides additional opportunities to optimize the patient onco-functional balance following resective brain surgery.
5. Conclusions
What we can conclude is that there is a substantial body of plausible evidence suggesting that damage or dysfunction in the non-traditional, large-scale brain networks may cause severe neurological, cognitive, or emotional deficits. The default mode, central executive, salience, dorsal attention, and ventral attention networks explain much of the complex human functioning currently understood in the neuroscientific community and therefore whether there is a need to preserve these non-traditional “eloquent” regions is an important question that should be incorporated into regular neurosurgical thinking moving forward. Increased use of rigorous pre- and post-operative neurocognitive assessments remains a priority moving forward, and these outcomes should be linked with data on network disturbances in larger trials in order to advance our understanding of and subsequent ability to optimize cognitive outcomes following brain surgery.
Supplementary Materials
The following supporting information can be downloaded at:
https://www.mdpi.com/article/10.3390/jpm12040587/s1, Supplementary Materials Content 1. Results, List of included studies. The 551 included articles detailed in the current study are provided. This file includes how each study was categorized based on the outcomes discussed above. Supplementary Materials Content 2. Results, 4 Figures. The Supplementary Materials Content expands on the Results provided. Figure S1: Frequency of diagnoses in all included studies. Figure S2: Frequency of diagnoses in all included studies according to network affiliation. Figure S3: Breakdown of Included Studies.
Author Contributions
Conceptualization, M.E.S.; methodology, N.B.D. and M.E.S.; software, N.B.D. and M.E.S.; validation, N.B.D. and M.E.S.; formal analysis, N.B.D. and M.E.S.; investigation, N.B.D. and M.E.S.; resources, N.B.D. and M.E.S.; data curation, N.B.D. and M.E.S.; writing—original draft preparation, N.B.D.; writing—review and editing, N.B.D. and M.E.S.; visualization, N.B.D.; supervision, M.E.S.; project administration, M.E.S.; funding acquisition, M.E.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Acknowledgments
The authors would like to thank Lewis Crawford and Omniscient Neurotechnology for helping with the creation of all network figures.
Conflicts of Interest
Nicholas B. Dadario has no conflicts of interest to disclose. Michael E. Sughrue is the Chief Medical Officer, co-founder, and shareholder for Omniscient Neurotechnology. However, no products or aspects of this relationship were discussed in the current manuscript.
References
- Young, J.S.; Lee, A.T.; Chang, E.F. A Review of Cortical and Subcortical Stimulation Mapping for Language. Neurosurgery 2021, 89, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Vigneswaran, K.; Sawaya, R. Role of Resection of Glioblastoma: Can Technology Overcome Biology? Neurosurgery 2020, 67, 4–14. [Google Scholar] [CrossRef]
- Drewes, C.; Sagberg, L.M.; Jakola, A.S.; Solheim, O. Perioperative and Postoperative Quality of Life in Patients with Glioma–A Longitudinal Cohort Study. World Neurosurg. 2018, 117, e465–e474. [Google Scholar] [CrossRef] [PubMed]
- Dhandapani, M.; Gupta, S.; Mohanty, M.; Gupta, S.K.; Dhandapani, S. Trends in cognitive dysfunction following surgery for intracranial tumors. Surg. Neurol. Int. 2016, 7, S190–S195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herbet, G.; Moritz-Gasser, S. Beyond Language: Mapping Cognition and Emotion. Neurosurg. Clin. N. Am. 2019, 30, 75–83. [Google Scholar] [CrossRef]
- Rijnen, S.J.M.; Kaya, G.; Gehring, K.; Verheul, J.B.; Wallis, O.C.; Sitskoorn, M.M.; Rutten, G.M. Cognitive functioning in patients with low-grade glioma: Effects of hemispheric tumor location and surgical procedure. J. Neurosurg. 2019, 133, 1671–1682. [Google Scholar] [CrossRef]
- Starnoni, D.; Berthiller, J.; Idriceanu, T.-M.; Meyronet, D.; d’Hombres, A.; Ducray, F.; Guyotat, J. Returning to work after multimodal treatment in glioblastoma patients. Neurosurg. Focus FOC 2018, 44, E17. [Google Scholar] [CrossRef]
- Dadario, N.B.; Brahimaj, B.; Yeung, J.; Sughrue, M.E. Reducing the Cognitive Footprint of Brain Tumor Surgery. Front. Neurol. 2021, 12, 711646. [Google Scholar] [CrossRef]
- Buckner, R.L.; Andrews-Hanna, J.R.; Schacter, D.L. The brain’s default network: Anatomy, function, and relevance to disease. Ann. N. Y. Acad. Sci. 2008, 1124, 1–38. [Google Scholar] [CrossRef] [Green Version]
- Seeley, W.W.; Menon, V.; Schatzberg, A.F.; Keller, J.; Glover, G.H.; Kenna, H.; Reiss, A.L.; Greicius, M.D. Dissociable intrinsic connectivity networks for salience processing and executive control. J. Neurosci. 2007, 27, 2349–2356. [Google Scholar] [CrossRef]
- Allan, P.G.; Briggs, R.G.; Conner, A.K.; O’Neal, C.M.; Bonney, P.A.; Maxwell, B.D.; Baker, C.M.; Burks, J.D.; Sali, G.; Glenn, C.A.; et al. Parcellation-based tractographic modeling of the ventral attention network. J. Neurol. Sci. 2020, 408, 116548. [Google Scholar] [CrossRef] [PubMed]
- Briggs, R.G.; Tanglay, O.; Dadario, N.B.; Young, I.M.; Fonseka, R.D.; Hormovas, J.; Dhanaraj, V.; Lin, Y.H.; Kim, S.J.; Bouvette, A.; et al. The Unique Fiber Anatomy of Middle Temporal Gyrus Default Mode Connectivity. Oper. Neurosurg. 2021, 21, E8–E14. [Google Scholar] [CrossRef] [PubMed]
- Briggs, R.G.; Lin, Y.H.; Dadario, N.B.; Kim, S.J.; Young, I.M.; Bai, M.Y.; Dhanaraj, V.; Fonseka, R.D.; Hormovas, J.; Tanglay, O.; et al. Anatomy and White Matter Connections of the Middle Frontal Gyrus. World Neurosurg. 2021, 150, e520–e529. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.H.; Dadario, N.B.; Hormovas, J.; Young, I.M.; Briggs, R.G.; MacKenzie, A.E.; Palejwala, A.H.; Fonseka, R.D.; Kim, S.J.; Tanglay, O.; et al. Anatomy and White Matter Connections of the Superior Parietal Lobule. Oper. Neurosurg. 2021, 21, E199–E214. [Google Scholar] [CrossRef]
- Tanglay, O.; Young, I.M.; Dadario, N.B.; Briggs, R.G.; Fonseka, R.D.; Dhanaraj, V.; Hormovas, J.; Lin, Y.H.; Sughrue, M.E. Anatomy and white-matter connections of the precuneus. Brain Imaging Behav. 2021, 1–13. [Google Scholar] [CrossRef]
- Fox, M.D. Mapping Symptoms to Brain Networks with the Human Connectome. N. Engl. J. Med. 2018, 379, 2237–2245. [Google Scholar] [CrossRef] [Green Version]
- O’Neal, C.M.; Ahsan, S.A.; Dadario, N.B.; Fonseka, R.D.; Young, I.M.; Parker, A.; Maxwell, B.D.; Yeung, J.T.; Briggs, R.G.; Teo, C.; et al. A connectivity model of the anatomic substrates underlying ideomotor apraxia: A meta-analysis of functional neuroimaging studies. Clin. Neurol. Neurosurg. 2021, 207, 106765. [Google Scholar] [CrossRef]
- Bezdicek, O.; Ballarini, T.; Růžička, F.; Roth, J.; Mueller, K.; Jech, R.; Schroeter, M.L. Mild cognitive impairment disrupts attention network connectivity in Parkinson’s disease: A combined multimodal MRI and meta-analytical study. Neuropsychologia 2018, 112, 105–115. [Google Scholar] [CrossRef]
- Kaiser, R.H.; Andrews-Hanna, J.R.; Wager, T.D.; Pizzagalli, D.A. Large-Scale Network Dysfunction in Major Depressive Disorder: A Meta-analysis of Resting-State Functional Connectivity. JAMA Psychiatry 2015, 72, 603–611. [Google Scholar] [CrossRef]
- Allan, P.G.; Briggs, R.G.; Conner, A.K.; O’Neal, C.M.; Bonney, P.A.; Maxwell, B.D.; Baker, C.M.; Burks, J.D.; Sali, G.; Glenn, C.A.; et al. Parcellation-based tractographic modeling of the dorsal attention network. Brain Behav. 2019, 9, e01365. [Google Scholar] [CrossRef]
- Corbetta, M.; Shulman, G.L. Control of goal-directed and stimulus-driven attention in the brain. Nat. Rev. Neurosci. 2002, 3, 201–215. [Google Scholar] [CrossRef] [PubMed]
- Corbetta, M.; Shulman, G.L. Spatial neglect and attention networks. Annu. Rev. Neurosci. 2011, 34, 569–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mallas, E.J.; De Simoni, S.; Scott, G.; Jolly, A.E.; Hampshire, A.; Li, L.M.; Bourke, N.J.; Roberts, S.A.G.; Gorgoraptis, N.; Sharp, D.J. Abnormal dorsal attention network activation in memory impairment after traumatic brain injury. Brain 2021, 144, 114–127. [Google Scholar] [CrossRef]
- Glasser, M.F.; Coalson, T.S.; Robinson, E.C.; Hacker, C.D.; Harwell, J.; Yacoub, E.; Ugurbil, K.; Andersson, J.; Beckmann, C.F.; Jenkinson, M.; et al. A multi-modal parcellation of human cerebral cortex. Nature 2016, 536, 171–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeo, B.T.; Krienen, F.M.; Sepulcre, J.; Sabuncu, M.R.; Lashkari, D.; Hollinshead, M.; Roffman, J.L.; Smoller, J.W.; Zollei, L.; Polimeni, J.R.; et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J. Neurophysiol. 2011, 106, 1125–1165. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Xu, X.; Zhu, C.; Luo, L.; Wang, Q.; Xiao, B.; Feng, B.; Hu, L.; Liu, L. Disrupted Structural Brain Network Organization Behind Depressive Symptoms in Major Depressive Disorder. Front. Psychiatry 2020, 11, 565890. [Google Scholar] [CrossRef]
- Menon, V. Large-scale brain networks and psychopathology: A unifying triple network model. Trends Cogn. Sci. 2011, 15, 483–506. [Google Scholar] [CrossRef]
- Bartolomei, F.; Bosma, I.; Klein, M.; Baayen, J.C.; Reijneveld, J.C.; Postma, T.J.; Heimans, J.J.; van Dijk, B.W.; de Munck, J.C.; de Jongh, A.; et al. How do brain tumors alter functional connectivity? A magnetoencephalography study. Ann. Neurol. 2006, 59, 128–138. [Google Scholar] [CrossRef]
- Madhusoodanan, S.; Ting, M.B.; Farah, T.; Ugur, U. Psychiatric aspects of brain tumors: A review. World J. Psychiatry 2015, 5, 273–285. [Google Scholar] [CrossRef]
- Briggs, R.G.; Allan, P.G.; Poologaindran, A.; Dadario, N.B.; Young, I.M.; Ahsan, S.A.; Teo, C.; Sughrue, M.E. The Frontal Aslant Tract and Supplementary Motor Area Syndrome: Moving towards a Connectomic Initiation Axis. Cancers 2021, 13, 1116. [Google Scholar] [CrossRef]
- Young, J.S.; Gogos, A.J.; Aabedi, A.A.; Morshed, R.A.; Pereira, M.P.; Lashof-Regas, S.; Mansoori, Z.; Luks, T.; Hervey-Jumper, S.L.; Villanueva-Meyer, J.E.; et al. Resection of supplementary motor area gliomas: Revisiting supplementary motor syndrome and the role of the frontal aslant tract. J. Neurosurg. 2021, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Darby, R.R.; Joutsa, J.; Burke, M.J.; Fox, M.D. Lesion network localization of free will. Proc. Natl. Acad. Sci. USA 2018, 115, 10792–10797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burks, J.D.; Bonney, P.A.; Conner, A.K.; Glenn, C.A.; Briggs, R.G.; Battiste, J.D.; McCoy, T.; O’Donoghue, D.L.; Wu, D.H.; Sughrue, M.E. A method for safely resecting anterior butterfly gliomas: The surgical anatomy of the default mode network and the relevance of its preservation. J. Neurosurg. 2017, 126, 1795–1811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darby, R.R.; Joutsa, J.; Fox, M.D. Network localization of heterogeneous neuroimaging findings. Brain 2018, 142, 70–79. [Google Scholar] [CrossRef]
- Dadario, N.B.; Zaman, A.; Pandya, M.; Dlouhy, B.J.; Gunawardena, M.P.; Sughrue, M.E.; Teo, C. Endoscopic-assisted surgical approach for butterfly glioma surgery. J. Neurooncol. 2022, 156, 635–644. [Google Scholar] [CrossRef]
- Jenkins, L.M.; Drummond, K.J.; Andrewes, D.G. Emotional and personality changes following brain tumour resection. J. Clin. Neurosci. 2016, 29, 128–132. [Google Scholar] [CrossRef]
- Duffau, H. Mapping the connectome in awake surgery for gliomas: An update. J. Neurosurg. Sci. 2017, 61, 612–630. [Google Scholar] [CrossRef]
- Greisman, J.D.; Dadario, N.B.; Park, J.; Silverstein, J.W.; D’Amico, R.S. Subcortical Stimulation in Brain Tumor Surgery: A closer look beneath the surface. World Neurosurg. 2022, 161, 55–63. [Google Scholar] [CrossRef]
- Nenning, K.-H.; Furtner, J.; Kiesel, B.; Schwartz, E.; Roetzer, T.; Fortelny, N.; Bock, C.; Grisold, A.; Marko, M.; Leutmezer, F.; et al. Distributed changes of the functional connectome in patients with glioblastoma. Sci. Rep. 2020, 10, 18312. [Google Scholar] [CrossRef]
- Jütten, K.; Weninger, L.; Mainz, V.; Gauggel, S.; Binkofski, F.; Wiesmann, M.; Merhof, D.; Clusmann, H.; Na, C.-H. Dissociation of structural and functional connectomic coherence in glioma patients. Sci. Rep. 2021, 11, 16790. [Google Scholar] [CrossRef]
- Glenn, C.; Conner, A.K.; Rahimi, M.; Briggs, R.G.; Baker, C.; Sughrue, M. Common Disconnections in Glioma Surgery: An Anatomic Description. Cureus 2017, 9, e1778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sughrue, M.E. Chapter 5—Surgical techniques and operative nuances of complex glioma surgery. In New Techniques for Management of ‘Inoperable’ Gliomas; Sughrue, M.E., Yang, I., Eds.; Academic Press: Cambridge, MA, USA, 2019; pp. 39–46. [Google Scholar] [CrossRef]
- Takami, H.; Khoshnood, N.; Bernstein, M. Preoperative factors associated with adverse events during awake craniotomy: Analysis of 609 consecutive cases. J. Neurosurg. JNS 2021, 134, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Castellano, A.; Bello, L.; Michelozzi, C.; Gallucci, M.; Fava, E.; Iadanza, A.; Riva, M.; Casaceli, G.; Falini, A. Role of diffusion tensor magnetic resonance tractography in predicting the extent of resection in glioma surgery. Neuro Oncol. 2012, 14, 192–202. [Google Scholar] [CrossRef]
- Duffau, H. New Philosophy, Clinical Pearls, and Methods for Intraoperative Cognition Mapping and Monitoring “a la carte” in Brain Tumor Patients. Neurosurgery 2021, 88, 919–930. [Google Scholar] [CrossRef] [PubMed]
- Ius, T.; Isola, M.; Budai, R.; Pauletto, G.; Tomasino, B.; Fadiga, L.; Skrap, M. Low-grade glioma surgery in eloquent areas: Volumetric analysis of extent of resection and its impact on overall survival. A single-institution experience in 190 patients: Clinical article. J. Neurosurg. 2012, 117, 1039–1052. [Google Scholar] [CrossRef] [PubMed]
- Ung, N.; Mathur, M.; Chung, L.K.; Cremer, N.; Pelargos, P.; Frew, A.; Thill, K.; Mathur, I.; Voth, B.; Lim, M.; et al. A Systematic Analysis of the Reliability of Diffusion Tensor Imaging Tractography for Facial Nerve Imaging in Patients with Vestibular Schwannoma. J. Neurol. Surg. B Skull Base 2016, 77, 314–318. [Google Scholar] [CrossRef] [Green Version]
- Conner, A.K.; Burks, J.D.; Baker, C.M.; Smitherman, A.D.; Pryor, D.P.; Glenn, C.A.; Briggs, R.G.; Bonney, P.A.; Sughrue, M.E. Method for temporal keyhole lobectomies in resection of low- and high-grade gliomas. J. Neurosurg. JNS 2018, 128, 1388–1395. [Google Scholar] [CrossRef] [Green Version]
- Tanglay, O.; Young, I.M.; Dadario, N.B.; Taylor, H.M.; Nicholas, P.J.; Doyen, S.; Sughrue, M.E. Eigenvector PageRank difference as a measure to reveal topological characteristics of the brain connectome for neurosurgery. J. Neurooncol. 2022, 157, 49–61. [Google Scholar] [CrossRef]
- Baker, C.M.; Burks, J.D.; Briggs, R.G.; Smitherman, A.D.; Glenn, C.A.; Conner, A.K.; Wu, D.H.; Sughrue, M.E. The crossed frontal aslant tract: A possible pathway involved in the recovery of supplementary motor area syndrome. Brain Behav. 2018, 8, e00926. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).