Efficacy of Endoscopic and Surgical Treatments for Gastroesophageal Reflux Disease: A Systematic Review and Network Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Study Selection
2.5. Data Extraction and Study Endpoint
2.6. Statistical Analysis
3. Results
3.1. Study Selection and Characteristics
3.2. Direct Meta-Analysis for the Efficacy of Endoscopic or Surgical Treatments
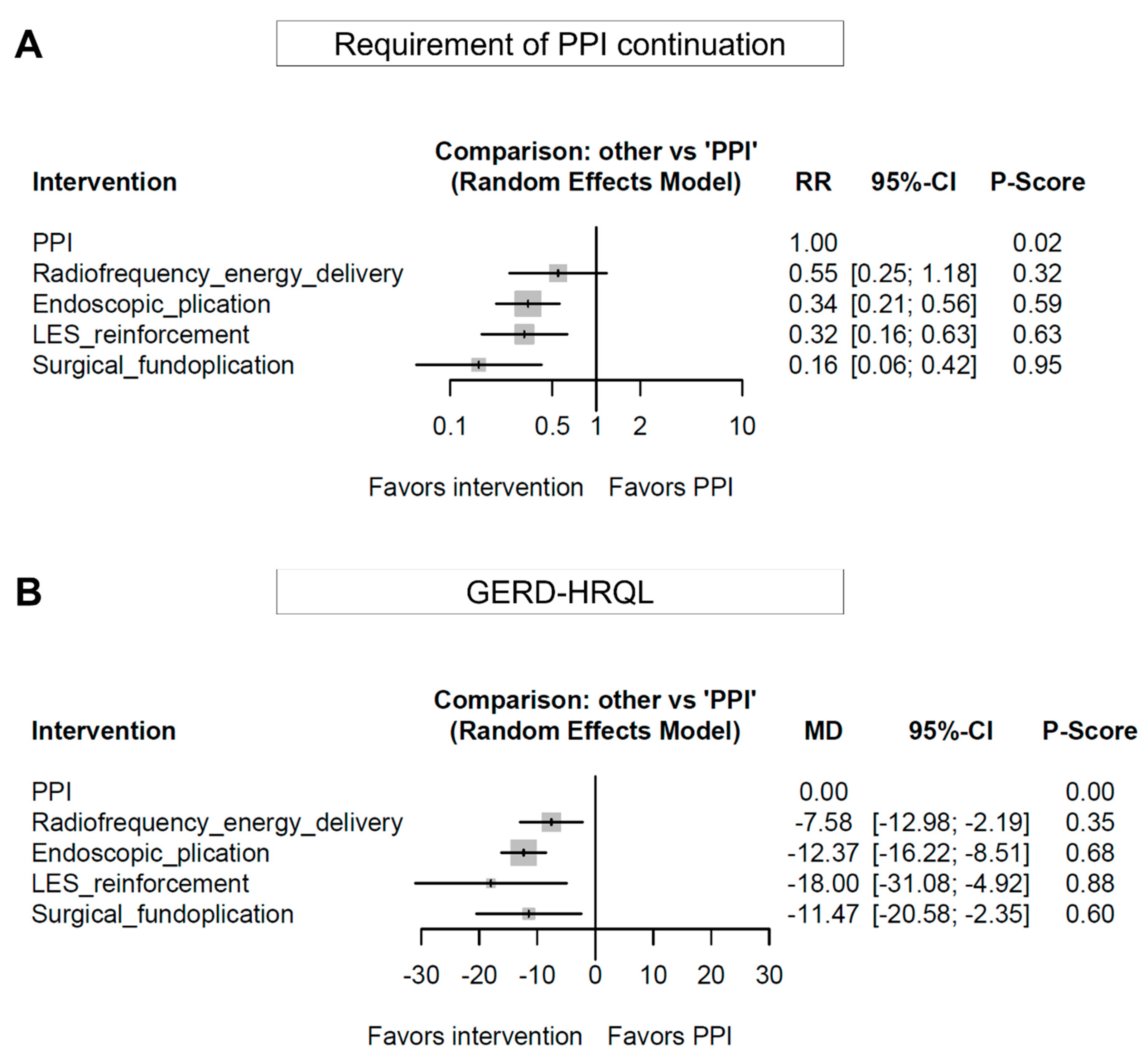
3.3. Network Meta-Analysis for the Efficacy of Endoscopic or Surgical Treatments
3.4. Sensitivity Analysis
3.5. Adverse Events
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Detailed Search Strategy
- MEDLINE (Search interface: PubMed)
- (reflux[tw] OR regurgitation[tw] OR GERD[tw] OR GORD[tw]) AND (radiofrequency[tw] OR stretta[tw] OR esophyX[tw] OR (transoral[tw] AND (plication[tw] OR fundoplication[tw])) OR (endoscopic plication[tw]) OR (endoscopic fundoplication[tw]) OR (endoscopic gastroplication[tw]) OR (endoscopic full-thickness plication[tw]) OR (endoscopic full-thickness fundoplication[tw]) OR plicator[tw] OR EndoCinch[tw] OR TIF[tw] OR (magnetic[tw] AND augmentation[tw]) OR MSA[tw] OR LINX[tw] OR (endoscopic polymer implantation[tw]) OR (nonresorbable copolymer implantation[tw]) OR (esophageal prosthesis[tw]) OR (oesophageal prosthesis[tw]) OR Enteryx[tw] OR Gatekeeper[tw] OR ((surgical[tw] OR laparoscopic[tw] OR Nissen[tw] OR Toupet[tw]) AND fundoplication[tw]) OR (total fundoplication[tw]) OR (partial fundoplication[tw]) OR (antireflux surgery[tw]) OR (anti-reflux surgery[tw])) AND random*[tw] AND (“1990/01/01”[Date - Publication] : “3000”[Date - Publication])
- EMBASE (Search interface: Ovid)
- 1: ((reflux or regurgitation or GERD or GORD) and (radiofrequency or stretta or esophyX or (transoral and (plication or fundoplication)) or endoscopic plication or endoscopic fundoplication or endoscopic gastroplication or endoscopic full-thickness plication or endoscopic full-thickness fundoplication or plicator or EndoCinch or TIF or (magnetic and augmentation) or MSA or LINX or endoscopic polymer implantation or nonresorbable copolymer implantation or esophageal prosthesis or oesophageal prosthesis or Enteryx or Gatekeeper or ((surgical or laparoscopic or Nissen or Toupet) and fundoplication) or total fundoplication or partial fundoplication or antireflux surgery or anti-reflux surgery) and random*).ab,ti.
- 2: Limit 1 to (english language and embase and yr=“1990 -Current”)
- Cochrane library
- #1: reflux or regurgitation or GERD or GORD
- #2: radiofrequency or stretta or esophyX
- #3: transoral and plication
- #4: transoral and fundoplication
- #5: #3 or #4
- #6: ‘endoscopic plication’ or ‘endoscopic fundoplication’ or ‘endoscopic gastroplication’ or ‘endoscopic full-thickness plication’ or ‘endoscopic full-thickness fundoplication’ or plicator or EndoCinch or TIF
- #7: magnetic and augmentation
- #8: MSA or LINX
- #9: ‘endoscopic polymer implantation’ or ‘nonresorbable copolymer implantation’ or ‘esophageal prosthesis’ or ‘oesophageal prosthesis’ or Enteryx or Gatekeeper
- #10: surgical or laparoscopic or Nissen or Toupet
- #11: fundoplication
- #12: #10 and #11
- #13: ‘total fundoplication’ or ‘partial fundoplication’ or ‘antireflux surgery’ or ‘anti-reflux surgery’
- #14: #2 or #5 or #6 or #7 or #8 or #9 or #12 or #13
- #15: random*
- #16: #1 and #14 and #15 (with Publication Year from 1990 to 2021, in Trials)
References
- Richter, J.E.; Rubenstein, J.H. Presentation and Epidemiology of Gastroesophageal Reflux Disease. Gastroenterology 2018, 154, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.K.; Tae, C.H.; Song, K.H.; Kang, S.J.; Park, J.K.; Gong, E.J.; Shin, J.E.; Lim, H.C.; Lee, S.K.; Jung, D.H.; et al. 2020 Seoul Consensus on the Diagnosis and Management of Gastroesophageal Reflux Disease. J. Neurogastroenterol. Motil. 2021, 27, 453–481. [Google Scholar] [CrossRef] [PubMed]
- Chiba, N.; De Gara, C.J.; Wilkinson, J.M.; Hunt, R.H. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: A meta-analysis. Gastroenterology 1997, 112, 1798–1810. [Google Scholar] [CrossRef] [PubMed]
- Katz, P.O.; Gerson, L.B.; Vela, M.F. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am. J. Gastroenterol. 2013, 108, 308–328. [Google Scholar] [CrossRef]
- Lei, W.Y.; Chang, W.C.; Wen, S.H.; Yi, C.H.; Liu, T.T.; Hung, J.S.; Wong, M.W.; Chen, C.L. Predicting factors of recurrence in patients with gastroesophageal reflux disease: A prospective follow-up analysis. Ther. Adv. Gastroenterol. 2019, 12. [Google Scholar] [CrossRef] [Green Version]
- Gyawali, C.P.; Fass, R. Management of Gastroesophageal Reflux Disease. Gastroenterology 2018, 154, 302–318. [Google Scholar] [CrossRef]
- Park, S.; Park, S.; Park, J.M.; Ryu, S.; Hwang, J.; Kwon, J.W.; Seo, K.W. Anti-reflux Surgery Versus Proton Pump Inhibitors for Severe Gastroesophageal Reflux Disease: A Cost-Effectiveness Study in Korea. J. Neurogastroenterol. Motil. 2020, 26, 215–223. [Google Scholar] [CrossRef] [Green Version]
- Niu, X.P.; Yu, B.P.; Wang, Y.D.; Han, Z.; Liu, S.F.; He, C.Y.; Zhang, G.Z.; Wu, W.C. Risk factors for proton pump inhibitor refractoriness in Chinese patients with non-erosive reflux disease. World J. Gastroenterol. 2013, 19, 3124–3129. [Google Scholar] [CrossRef]
- Lee, E.S.; Kim, N.; Lee, S.H.; Park, Y.S.; Kim, J.W.; Jeong, S.H.; Lee, D.H.; Jung, H.C.; Song, I.S. Comparison of risk factors and clinical responses to proton pump inhibitors in patients with erosive oesophagitis and non-erosive reflux disease. Aliment. Pharm. 2009, 30, 154–164. [Google Scholar] [CrossRef]
- Wang, R.; Zou, D.; Ma, X.; Zhao, Y.; Yan, X.; Yan, H.; Fang, J.; Yin, P.; Kang, X.; Li, Q.; et al. Impact of gastroesophageal reflux disease on daily life: The Systematic Investigation of Gastrointestinal Diseases in China (SILC) epidemiological study. Health Qual. Life Outcomes 2010, 8, 128. [Google Scholar] [CrossRef] [Green Version]
- Gross, M.; Beckenbauer, U.; Burkowitz, J.; Walther, H.; Brueggenjuergen, B. Impact of gastro-oesophageal reflux disease on work productivity despite therapy with proton pump inhibitors in Germany. Eur. J. Med. Res. 2010, 15, 124–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nissen, R. [A simple operation for control of reflux esophagitis]. Schweiz. Med. Wochenschr. 1956, 86, 590–592. [Google Scholar] [PubMed]
- Dallemagne, B.; Weerts, J.M.; Jehaes, C.; Markiewicz, S.; Lombard, R. Laparoscopic Nissen fundoplication: Preliminary report. Surg. Laparosc. Endosc. 1991, 1, 138–143. [Google Scholar] [PubMed]
- Galmiche, J.P.; Hatlebakk, J.; Attwood, S.; Ell, C.; Fiocca, R.; Eklund, S.; Langstrom, G.; Lind, T.; Lundell, L.; Collaborators, L.T. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: The LOTUS randomized clinical trial. JAMA 2011, 305, 1969–1977. [Google Scholar] [CrossRef] [Green Version]
- Yadlapati, R.; DeLay, K. Proton Pump Inhibitor-Refractory Gastroesophageal Reflux Disease. Med. Clin. N. Am. 2019, 103, 15–27. [Google Scholar] [CrossRef]
- Pandolfino, J.E.; Krishnan, K. Do endoscopic antireflux procedures fit in the current treatment paradigm of gastroesophageal reflux disease? Clin. Gastroenterol. Hepatol. 2014, 12, 544–554. [Google Scholar] [CrossRef] [Green Version]
- Kushner, B.S.; Awad, M.M.; Mikami, D.J.; Chand, B.B.; Wai, C.J.; Murayama, K.M. Endoscopic treatments for GERD. Ann. N. Y. Acad. Sci. 2020, 1482, 121–129. [Google Scholar] [CrossRef]
- Testoni, P.A.; Testoni, S.; Distefano, G.; Mazzoleni, G.; Fanti, L.; Passaretti, S. Transoral incisionless fundoplication with EsophyX for gastroesophageal reflux disease: Clinical efficacy is maintained up to 10 years. Endosc. Int. Open 2019, 7, E647–E654. [Google Scholar] [CrossRef] [Green Version]
- Bell, R.; Lipham, J.; Louie, B.E.; Williams, V.; Luketich, J.; Hill, M.; Richards, W.; Dunst, C.; Lister, D.; McDowell-Jacobs, L.; et al. Magnetic Sphincter Augmentation Superior to Proton Pump Inhibitors for Regurgitation in a 1-Year Randomized Trial. Clin. Gastroenterol. Hepatol. 2020, 18, 1736–1743.e1732. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Jansen, J.P.; Fleurence, R.; Devine, B.; Itzler, R.; Barrett, A.; Hawkins, N.; Lee, K.; Boersma, C.; Annemans, L.; Cappelleri, J.C. Interpreting indirect treatment comparisons and network meta-analysis for health-care decision making: Report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: Part 1. Value Health 2011, 14, 417–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. Available online: https://handbook-5-1.cochrane.org/ (accessed on 23 November 2021).
- Rucker, G. Network meta-analysis, electrical networks and graph theory. Res. Synth. Methods 2012, 3, 312–324. [Google Scholar] [CrossRef] [PubMed]
- Rucker, G.; Schwarzer, G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 2015, 15, 58. [Google Scholar] [CrossRef] [Green Version]
- Neupane, B.; Richer, D.; Bonner, A.J.; Kibret, T.; Beyene, J. Network meta-analysis using R: A review of currently available automated packages. PLoS ONE 2014, 9, e115065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corley, D.A.; Katz, P.; Wo, J.M.; Stefan, A.; Patti, M.; Rothstein, R.; Edmundowicz, S.; Kline, M.; Mason, R.; Wolfe, M.M. Improvement of gastroesophageal reflux symptoms after radiofrequency energy: A randomized, sham-controlled trial. Gastroenterology 2003, 125, 668–676. [Google Scholar] [CrossRef]
- Coron, E.; Sebille, V.; Cadiot, G.; Zerbib, F.; Ducrotte, P.; Ducrot, F.; Pouderoux, P.; Arts, J.; Le Rhun, M.; Piche, T.; et al. Clinical trial: Radiofrequency energy delivery in proton pump inhibitor-dependent gastro-oesophageal reflux disease patients. Aliment. Pharm. 2008, 28, 1147–1158. [Google Scholar] [CrossRef]
- Aziz, A.M.; El-Khayat, H.R.; Sadek, A.; Mattar, S.G.; McNulty, G.; Kongkam, P.; Guda, M.F.; Lehman, G.A. A prospective randomized trial of sham, single-dose Stretta, and double-dose Stretta for the treatment of gastroesophageal reflux disease. Surg. Endosc. 2010, 24, 818–825. [Google Scholar] [CrossRef]
- Arts, J.; Bisschops, R.; Blondeau, K.; Farre, R.; Vos, R.; Holvoet, L.; Caenepeel, P.; Lerut, A.; Tack, J. A double-blind sham-controlled study of the effect of radiofrequency energy on symptoms and distensibility of the gastro-esophageal junction in GERD. Am. J. Gastroenterol. 2012, 107, 222–230. [Google Scholar] [CrossRef]
- Kalapala, R.; Shah, H.; Nabi, Z.; Darisetty, S.; Talukdar, R.; Nageshwar Reddy, D. Treatment of gastroesophageal reflux disease using radiofrequency ablation (Stretta procedure): An interim analysis of a randomized trial. Indian. J. Gastroenterol. 2017, 36, 337–342. [Google Scholar] [CrossRef]
- Montgomery, M.; Hakanson, B.; Ljungqvist, O.; Ahlman, B.; Thorell, A. Twelve months’ follow-up after treatment with the EndoCinch endoscopic technique for gastro-oesophageal reflux disease: A randomized, placebo-controlled study. Scand. J. Gastroenterol. 2006, 41, 1382–1389. [Google Scholar] [CrossRef] [PubMed]
- Rothstein, R.; Filipi, C.; Caca, K.; Pruitt, R.; Mergener, K.; Torquati, A.; Haber, G.; Chen, Y.; Chang, K.; Wong, D.; et al. Endoscopic full-thickness plication for the treatment of gastroesophageal reflux disease: A randomized, sham-controlled tri.al. Gastroenterology 2006, 131, 704–712. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M.P.; Wellink, H.; Gooszen, H.G.; Conchillo, J.M.; Samsom, M.; Smout, A.J. Endoscopic gastroplication for the treatment of gastro-oesophageal reflux disease: A randomised, sham-controlled trial. Gut 2007, 56, 20–28. [Google Scholar] [CrossRef] [Green Version]
- Hakansson, B.; Montgomery, M.; Cadiere, G.B.; Rajan, A.; Bruley des Varannes, S.; Lerhun, M.; Coron, E.; Tack, J.; Bischops, R.; Thorell, A.; et al. Randomised clinical trial: Transoral incisionless fundoplication vs. sham intervention to control chronic GERD. Aliment. Pharm. 2015, 42, 1261–1270. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.G.; Kahrilas, P.J.; Bell, R.C.; Wilson, E.B.; Trad, K.S.; Dolan, J.P.; Perry, K.A.; Oelschlager, B.K.; Soper, N.J.; Snyder, B.E.; et al. Efficacy of transoral fundoplication vs omeprazole for treatment of regurgitation in a randomized controlled trial. Gastroenterology 2015, 148, 324–333.e325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rinsma, N.F.; Farre, R.; Bouvy, N.D.; Masclee, A.A.; Conchillo, J.M. The effect of endoscopic fundoplication and proton pump inhibitors on baseline impedance and heartburn severity in GERD patients. Neurogastroenterol. Motil. 2015, 27, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Trad, K.S.; Barnes, W.E.; Simoni, G.; Shughoury, A.B.; Mavrelis, P.G.; Raza, M.; Heise, J.A.; Turgeon, D.G.; Fox, M.A. Transoral incisionless fundoplication effective in eliminating GERD symptoms in partial responders to proton pump inhibitor therapy at 6 months: The TEMPO Randomized Clinical Trial. Surg. Innov. 2015, 22, 26–40. [Google Scholar] [CrossRef]
- Witteman, B.P.; Conchillo, J.M.; Rinsma, N.F.; Betzel, B.; Peeters, A.; Koek, G.H.; Stassen, L.P.; Bouvy, N.D. Randomized controlled trial of transoral incisionless fundoplication vs. proton pump inhibitors for treatment of gastroesophageal reflux disease. Am. J. Gastroenterol. 2015, 110, 531–542. [Google Scholar] [CrossRef]
- Kalapala, R.; Karyampudi, A.; Nabi, Z.; Darisetty, S.; Jagtap, N.; Ramchandani, M.; Gupta, R.; Lakhtakia, S.; Goud, R.; Venkat Rao, G.; et al. Endoscopic full-thickness plication for the treatment of PPI-dependent GERD: Results from a randomised, sham controlled trial. Gut 2022, 71, 686–694. [Google Scholar] [CrossRef]
- Deviere, J.; Costamagna, G.; Neuhaus, H.; Voderholzer, W.; Louis, H.; Tringali, A.; Marchese, M.; Fiedler, T.; Darb-Esfahani, P.; Schumacher, B. Nonresorbable copolymer implantation for gastroesophageal reflux disease: A randomized sham-controlled multicenter trial. Gastroenterology 2005, 128, 532–540. [Google Scholar] [CrossRef]
- Fockens, P.; Cohen, L.; Edmundowicz, S.A.; Binmoeller, K.; Rothstein, R.I.; Smith, D.; Lin, E.; Nickl, N.; Overholt, B.; Kahrilas, P.J.; et al. Prospective randomized controlled trial of an injectable esophageal prosthesis versus a sham procedure for endoscopic treatment of gastroesophageal reflux disease. Surg. Endosc. 2010, 24, 1387–1397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bell, R.; Lipham, J.; Louie, B.; Williams, V.; Luketich, J.; Hill, M.; Richards, W.; Dunst, C.; Lister, D.; McDowell-Jacobs, L.; et al. Laparoscopic magnetic sphincter augmentation versus double-dose proton pump inhibitors for management of moderate-to-severe regurgitation in GERD: A randomized controlled trial. Gastrointest. Endosc. 2019, 89, 14–22.e11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lundell, L.; Miettinen, P.; Myrvold, H.E.; Pedersen, S.A.; Thor, K.; Lamm, M.; Blomqvist, A.; Hatlebakk, J.G.; Janatuinen, E.; Levander, K.; et al. Long-term management of gastro-oesophageal reflux disease with omeprazole or open antireflux surgery: Results of a prospective, randomized clinical trial. The Nordic GORD Study Group. Eur. J. Gastroenterol. Hepatol. 2000, 12, 879–887. [Google Scholar] [CrossRef]
- Mahon, D.; Rhodes, M.; Decadt, B.; Hindmarsh, A.; Lowndes, R.; Beckingham, I.; Koo, B.; Newcombe, R.G. Randomized clinical trial of laparoscopic Nissen fundoplication compared with proton-pump inhibitors for treatment of chronic gastro-oesophageal reflux. Br. J. Surg. 2005, 92, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Anvari, M.; Allen, C.; Marshall, J.; Armstrong, D.; Goeree, R.; Ungar, W.; Goldsmith, C. A randomized controlled trial of laparoscopic nissen fundoplication versus proton pump inhibitors for treatment of patients with chronic gastroesophageal reflux disease: One-year follow-up. Surg. Innov. 2006, 13, 238–249. [Google Scholar] [CrossRef]
- Grant, A.M.; Boachie, C.; Cotton, S.C.; Faria, R.; Bojke, L.; Epstein, D.M.; Ramsay, C.R.; Corbacho, B.; Sculpher, M.; Krukowski, Z.H.; et al. Clinical and economic evaluation of laparoscopic surgery compared with medical management for gastro-oesophageal reflux disease: 5-year follow-up of multicentre randomised trial (the REFLUX trial). Health Technol. Assess. 2013, 17, 1–167. [Google Scholar] [CrossRef] [PubMed]
- Hatlebakk, J.G.; Zerbib, F.; Bruley des Varannes, S.; Attwood, S.E.; Ell, C.; Fiocca, R.; Galmiche, J.P.; Eklund, S.; Langstrom, G.; Lind, T.; et al. Gastroesophageal Acid Reflux Control 5 Years After Antireflux Surgery, Compared With Long-term Esomeprazole Therapy. Clin. Gastroenterol. Hepatol. 2016, 14, 678–685.e673. [Google Scholar] [CrossRef] [Green Version]
- Domagk, D.; Menzel, J.; Seidel, M.; Ullerich, H.; Pohle, T.; Heinecke, A.; Domschke, W.; Kucharzik, T. Endoluminal gastroplasty (EndoCinch) versus endoscopic polymer implantation (Enteryx) for treatment of gastroesophageal reflux disease: 6-month results of a prospective, randomized trial. Am. J. Gastroenterol. 2006, 101, 422–430. [Google Scholar] [CrossRef]
- Svoboda, P.; Kantorova, I.; Kozumplik, L.; Scheer, P.; Radvan, M.; Radvanova, J.; Krass, V.; Horalek, F. Our experience with transoral incisionless plication of gastroesophageal reflux disease: NOTES procedure. Hepatogastroenterology 2011, 58, 1208–1213. [Google Scholar] [CrossRef]
- Antoniou, S.A.; Koch, O.O.; Kaindlstorfer, A.; Asche, K.U.; Berger, J.; Granderath, F.A.; Pointner, R. Endoscopic full-thickness plication versus laparoscopic fundoplication: A prospective study on quality of life and symptom control. Surg. Endosc. 2012, 26, 1063–1068. [Google Scholar] [CrossRef]
- Yanes, M.; Santoni, G.; Maret-Ouda, J.; Markar, S.; Ness-Jensen, E.; Kauppila, J.; Farkkila, M.; Lynge, E.; Pukkala, E.; Tryggvadottir, L.; et al. Mortality, Reoperation, and Hospital Stay Within 90 Days of Primary and Secondary Antireflux Surgery in a Population-Based Multinational Study. Gastroenterology 2021, 160, 2283–2290. [Google Scholar] [CrossRef] [PubMed]



| Publication Year, First Author [Reference Number] | Country | Study Period | Study Population | Number of Participants | Arm 1 | Arm 2 | Age, Year | Male, % |
|---|---|---|---|---|---|---|---|---|
| 2003, Corley [27] | USA | 2000–2001 | PPI-dependent patients with GERD | 64 | Radiofrequency energy delivery | Sham + PPI | Arm 1: mean 45 (SD 12) Arm 2: mean 52 (SD 15) | 51.6 |
| 2008, Coron [28] | France | 2003–2006 | PPI-dependent patients with GERD | 43 | Radiofrequency energy delivery | PPI | Arm 1: mean 50 (SD 10) Arm 2: mean 47 (SD 14) | 69.8 |
| 2010, Aziz [29] | USA | 2005–2006 | PPI-dependent patients with GERD | 24 | Radiofrequency energy delivery | Sham + PPI | Arm 1: mean 36.7 (SD 9.5) Arm 2: mean 32.0 (SD 8.3) | 66.7 |
| 2012, Arts [30] | Belgium | N/A | Patients with GERD | 22 | Radiofrequency energy delivery | Sham + PPI | Mean 46.5 (SD 2.4) | 22.7 |
| 2017, Kalapala [31] | India | 2015–2016 | Patients with refractory GERD | 20 | Radiofrequency energy delivery | Sham + PPI | Mean 36.5 (SD 13.0) | 100.0 |
| 2006, Montgomery [32] | Sweden | N/A | PPI-dependent patients with GERD | 46 | Endoscopic plication | Sham + PPI | Arm 1: median 42 (range 22–66) Arm 2: median 41 (range 19–66) | 32.6 |
| 2006, Rothstein [33] | USA and Europe | 2005 | PPI-dependent patients with GERD | 144 | Endoscopic plication | Sham + PPI | Arm 1: mean 48.1 (SD 13.1) Arm 2: mean 46.3 (SD 13.8) | 52.1 |
| 2007, Schwartz [34] | The Netherlands | 2003–2005 | PPI-dependent patients with GERD | 60 | Endoscopic plication | Sham + PPI | Arm 1: mean 45 (SD 12) Arm 2: mean 47 (SD 12) | 62.5 |
| 2015, Håkansson [35] | Sweden | 2011–2013 | PPI-dependent patients with GERD | 44 | Endoscopic plication | Sham + PPI | Arm 1: median 41 (range 21–67) Arm 2: median 62 (range 31–76) | 54.5 |
| 2015, Hunter [36] | USA | 2011–2013 | Patients with refractory GERD | 129 | Endoscopic plication | Sham + PPI | Arm 1: median 52 (range 22–74) Arm 2: median 55 (range 22–73) | 48.8 |
| 2015, Rinsma [37] | The Netherlands | 2008–2012 | PPI-dependent patients with GERD | 47 | Endoscopic plication | PPI | Mean 45 (range 19–68) | 63.8 |
| 2015, Trad [38] | USA | 2012 | Patients with refractory GERD | 60 | Endoscopic plication | PPI | Arm 1: median 54.8 (range 35.7–73.3) Arm 2: median 50.1 (range 32.5–63.3) | 45.0 |
| 2015, Witteman [39] | The Netherlands and USA | 2008–2011 | PPI-dependent patients with GERD | 60 | Endoscopic plication | PPI | Mean 44.7 (SD 12.9) | 63.3 |
| 2021, Kalapala [40] | India | 2017–2019 | PPI-dependent patients with GERD | 70 | Endoscopic plication | Sham + PPI | Median 36 (IQR 29–42) | 71.4 |
| 2005, Devière [41] | Germany, Beligum, and Italy | 2001–2004 | PPI-dependent patients with GERD | 64 | Reinforcement of the LES | Sham + PPI | Arm 1: mean 49.7 (SD 14.2) Arm 2: mean 48.6 (SD 10.2) | 67.2 |
| 2010, Fockens [42] | USA and the Netherlands | 2003–2005 | PPI-dependent patients with GERD | 118 | Reinforcement of the LES | Sham + PPI | Arm 1: mean 47.9 (SD 11.6) Arm 2: mean 52.6 (SD 11.8) | 63.6 |
| 2019, Bell [43] | USA | 2015–2017 | Patients with refractory GERD | 152 | Reinforcement of the LES | PPI | Median 46 (range 21–76) | 56.6 |
| 2000, Lundell [44] | Europe | 1991–1999 | Patients with GERD | 298 | Surgical fundoplication | PPI | N/A | 75.5 |
| 2005, Mahon [45] | UK | 1997–2001 | PPI-dependent patients with GERD | 217 | Surgical fundoplication | PPI | Arm 1: median 48 (IQR 39–56) Arm 2: median 47 (IQR 35–57) | 69 |
| 2006, Anvari [46] | Canada | 2000–2004 | PPI-dependent patients with GERD | 104 | Surgical fundoplication | PPI | Arm 1: mean 42.9 Arm 2: mean 42.1 | 52.9 |
| 2013, Grant [47] | UK | 2001–2004 | PPI-dependent patients with GERD | 357 | Surgical fundoplication | PPI | Arm 1: mean 46.7 (SD 10.3) Arm 2: mean 45.9 (SD 11.9) | 66.1 |
| 2016, Hatlebakk [48] | Europe | 2001–2009 | Patients with GERD | 554 | Surgical fundoplication | PPI | Mean 45.1 (SD 11.2) | 71.8 |
| 2006, Domagk [49] | Germany | 2002–2005 | PPI-dependent patients with GERD | 49 | Endoscopic plication | Reinforcement of the LES | Mean 48 (SD 15) | 53.1 |
| 2011, Svoboda [50] | Czech | 2007–2009 | Patients with GERD | 52 | Endoscopic plication | Surgical fundoplication | Arm 1: median 49 (range 25–69) Arm 2: median 55 (range 39–70) | 48.1 |
| 2012, Antoniou [51] | Austria | 2006–2010 | Patients with GERD | 56 | Endoscopic plication | Surgical fundoplication | Arm 1: mean 46.5 Arm 2: mean 46.3 | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gong, E.J.; Park, C.H.; Jung, D.H.; Kang, S.H.; Lee, J.Y.; Lim, H.; Kim, D.H.; Endoscopic Therapy and Instrument Research Group under the Korean Society of Neurogastroenterology and Motility. Efficacy of Endoscopic and Surgical Treatments for Gastroesophageal Reflux Disease: A Systematic Review and Network Meta-Analysis. J. Pers. Med. 2022, 12, 621. https://doi.org/10.3390/jpm12040621
Gong EJ, Park CH, Jung DH, Kang SH, Lee JY, Lim H, Kim DH, Endoscopic Therapy and Instrument Research Group under the Korean Society of Neurogastroenterology and Motility. Efficacy of Endoscopic and Surgical Treatments for Gastroesophageal Reflux Disease: A Systematic Review and Network Meta-Analysis. Journal of Personalized Medicine. 2022; 12(4):621. https://doi.org/10.3390/jpm12040621
Chicago/Turabian StyleGong, Eun Jeong, Chan Hyuk Park, Da Hyun Jung, Sun Hyung Kang, Ju Yup Lee, Hyun Lim, Do Hoon Kim, and Endoscopic Therapy and Instrument Research Group under the Korean Society of Neurogastroenterology and Motility. 2022. "Efficacy of Endoscopic and Surgical Treatments for Gastroesophageal Reflux Disease: A Systematic Review and Network Meta-Analysis" Journal of Personalized Medicine 12, no. 4: 621. https://doi.org/10.3390/jpm12040621
APA StyleGong, E. J., Park, C. H., Jung, D. H., Kang, S. H., Lee, J. Y., Lim, H., Kim, D. H., & Endoscopic Therapy and Instrument Research Group under the Korean Society of Neurogastroenterology and Motility. (2022). Efficacy of Endoscopic and Surgical Treatments for Gastroesophageal Reflux Disease: A Systematic Review and Network Meta-Analysis. Journal of Personalized Medicine, 12(4), 621. https://doi.org/10.3390/jpm12040621






