The Impact of Oxygen Pulse and Its Curve Patterns on Male Patients with Heart Failure, Chronic Obstructive Pulmonary Disease, and Healthy Controls—Ejection Fractions, Related Factors and Outcomes
Abstract
1. Introduction
2. Materials and Methods
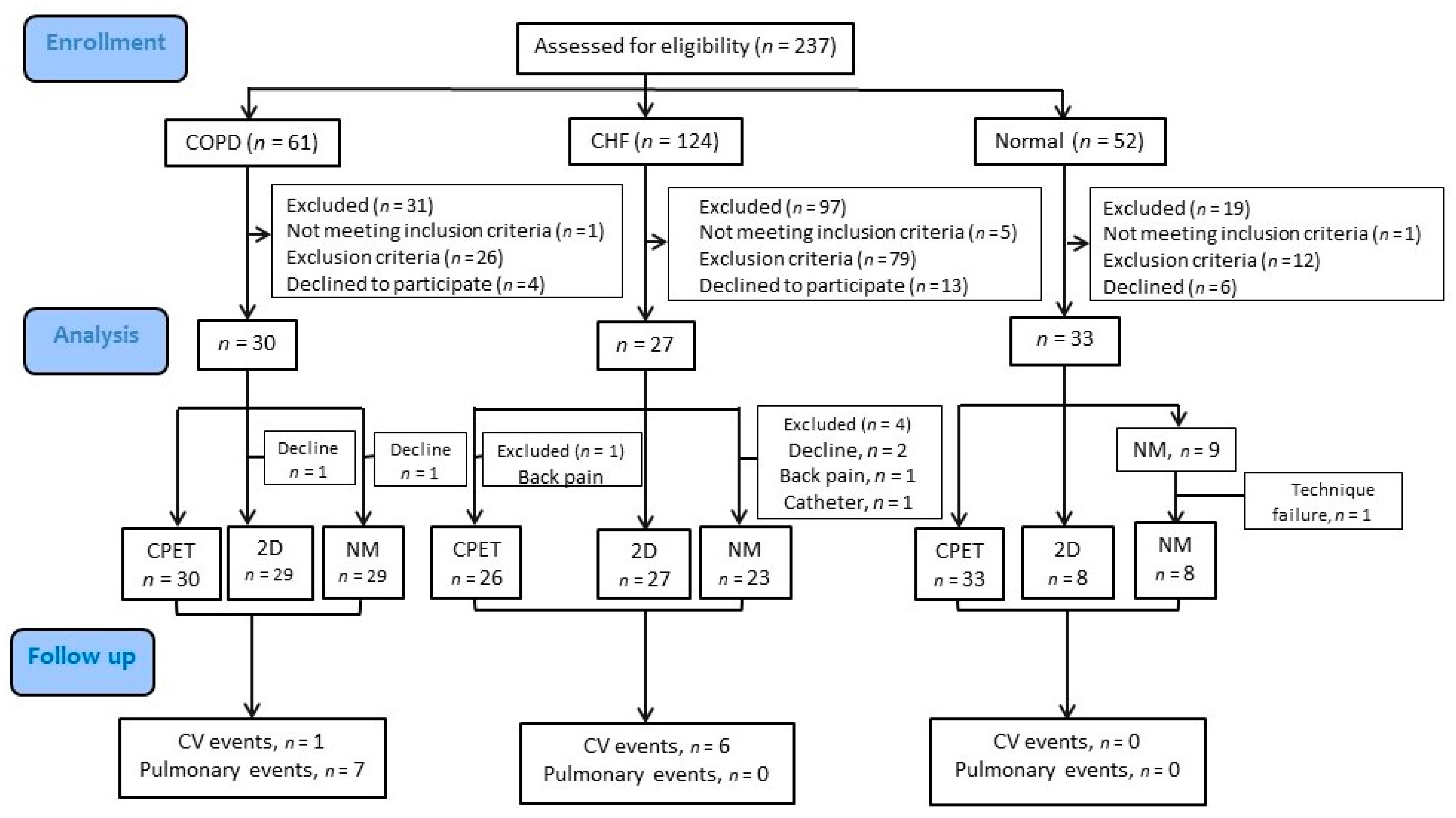
2.1. Study Design
2.2. Subjects
2.3. Measurements
2.4. Statistical Analysis
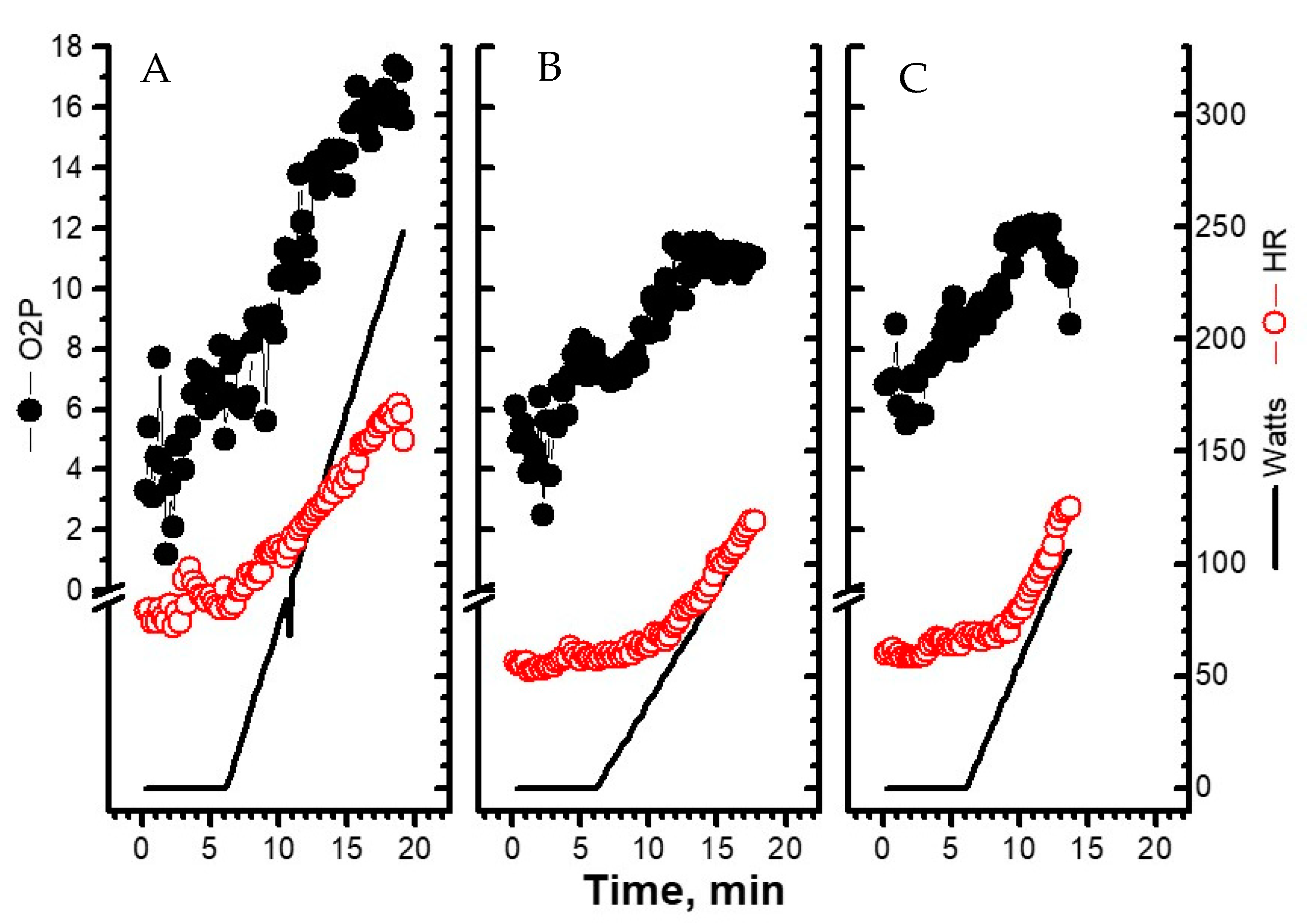
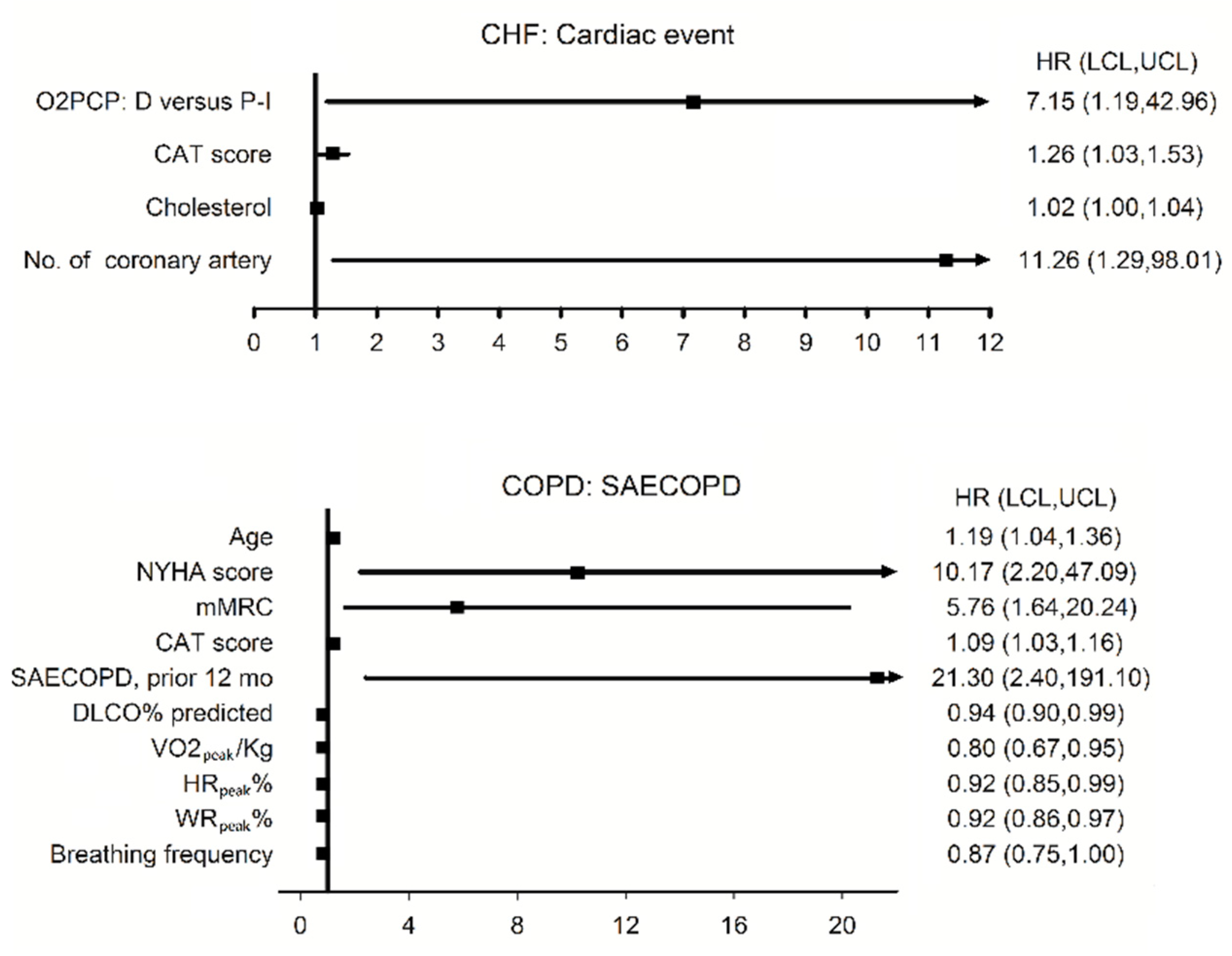
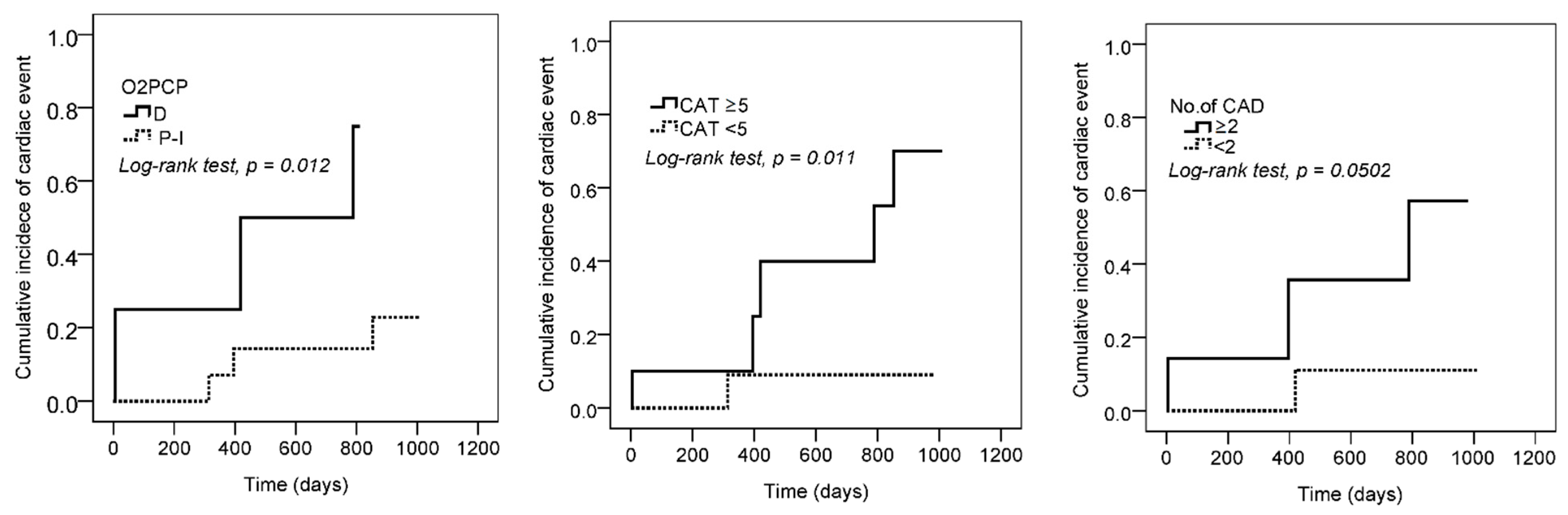
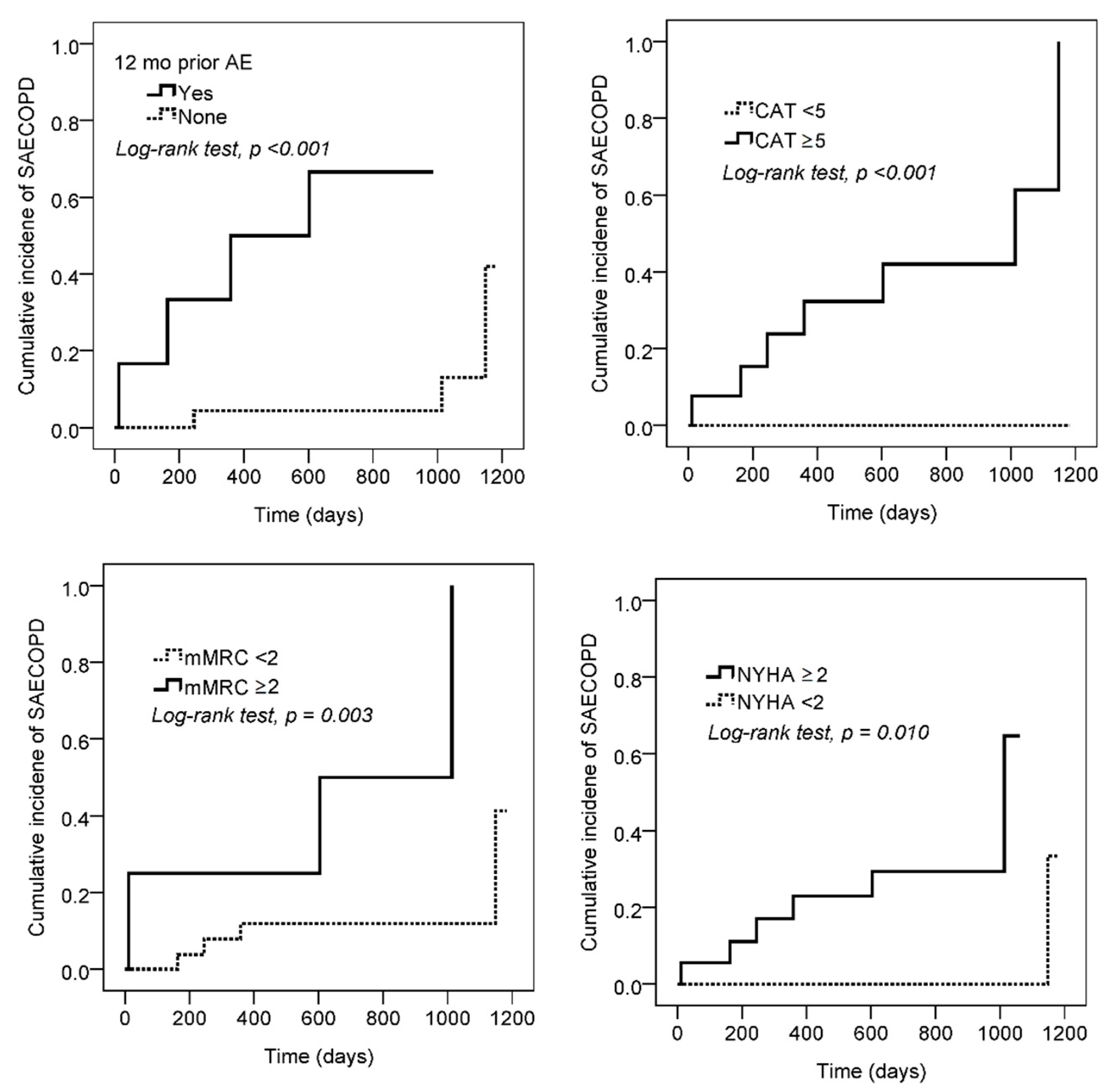
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 2-D echo | two-dimensional echocardiography |
| 2DLVEF | left ventricular ejection fraction using two-dimensional echocardiography |
| ANOVA | analysis of variance |
| AT | anaerobic threshold |
| CAD | coronary artery disease |
| CAT | COPD Assessment Test |
| CHF | chronic heart failure |
| COPD | chronic obstructive pulmonary disease |
| CPETs | cardiopulmonary exercise tests |
| CV | cardiovascular |
| D | decreasing |
| Δ | change |
| DLCO | diffusing capacity of lung for carbon monoxide |
| EKG | electrocardiograms |
| FPRV | first-pass radionuclide ventriculography |
| HFrEF/HFmrEF | heart failure with reduced or mildly reduced ejection fraction |
| HRs | hazard ratios |
| HR | heart rate |
| hs-CRP | high-sensitivity C-reactive protein |
| I | increasing |
| LABA/LAMA | long-acting beta bronchodilators/muscarinic antagonists |
| mMRC | modified Medical Research Council |
| LVEF | the ejection fraction of left ventricles |
| NM | nuclear medicine |
| NT pro-BNP | N terminal pro-brain natriuretic peptide |
| NYHAfc | New York Heart Association functional class |
| OB | oscillatory breathing |
| OCD | oxygen-cost diagram |
| O2P | oxygen pulse value |
| O2PCP | oxygen pulse curve pattern |
| P | plateau |
| PPPY | per person per year |
| RV | residual volume |
| RVEF | the ejection fraction of right ventricles |
| SAECOPD | severe acute exacerbation of COPD |
| SDS | summed difference score |
| SPECT | gated myocardial perfusion single-photon emission computed tomography |
| SPO2 | arterial oxyhemoglobin saturation measured by pulse oximetry |
| SRS | summed rest scores |
| SSS | summed stress score |
| V’CO2 | CO2 output |
| TLC | total lung capacity |
| V’E | minute ventilation |
| V’O2 | oxygen uptake |
| VT | tidal volume |
| WR | work rate |
References
- Wasserman, K.; Hansen, J.E.; Sue, D.Y.; Stringer, W.W.; Whipp, B.J. Normal values. In Principles of Exercise Testing and Interpretation, 4th ed.; Wasserman, K., Ed.; Lippicott Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 160–182. [Google Scholar]
- Cohen-Solal, A.; Tabet, J.Y.; Logeart, D.; Bourgoin, P.; Tokmakova, M.; Dahan, M. A non-invasively determined surrogate of cardiac power (‘circulatory power’) at peak exercise is a powerful prognostic factor in chronic heart failure. Eur. Heart J. 2002, 23, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.B.; Myers, J.; Araújo, C.G.S.; Abella, J.; Mandic, S.; Froelicher, V. Maximal exercise oxygen pulse as a predictor of mortality among male veterans referred for exercise testing. Eur. J. Cardiol. Prev. Rehab. 2009, 16, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.B.; Myers, J.; Araujo, C.G.S.; Arena, R.; Mandic, S.; Bensimhon, D.; Abella, J.; Chase, P.; Guazzi, M.; Brubaker, P.; et al. Does peak oxygen pulse complement peak oxygen uptake in risk stratifying patients with heart failure? Am. J. Cardiol. 2009, 104, 554–558. [Google Scholar] [CrossRef] [PubMed]
- Laukkanen, J.A.; Kurl, S.; Salonen, J.T.; Lakka, T.A.; Rauramaa, R. Peak oxygen pulse during exercise as a predictor for coronary heart disease and all cause death. Heart 2006, 92, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Groepenhoff, H.; Vonk-Noordegraaf, A.; Boonstra, A.; Spreeuwenberg, M.D.; Postmus, P.E.; Bogaard, H.J. Exercise testing to estimate survival in pulmonary hypertension. Med. Sci. Sports Exerc. 2008, 40, 1725–1732. [Google Scholar] [CrossRef]
- Wasserman, K.; Hansen, J.E.; Sue, D.Y.; Stringer, W.W.; Whipp, B.J. Measurements during integrative cardiopulmonary exercise testing. In Principles of Exercise Testing and Interpretation, 4th ed.; Wasserman, K., Ed.; Lippicott Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 76–110. [Google Scholar]
- Vassaux, C.; Torre-Bouscoulet, L.; Zeineldine, S.; Cortopassi, F.; Paz-Diaz, H.; Celli, B.R.; Pinto-Plata, V.M. Effects of hyperinflation on the oxygen pulse as a marker of cardiac performance in COPD. Eur. Respir. J. 2008, 32, 1275–1282. [Google Scholar] [CrossRef]
- Montes de Oca, M.; Rassulo, J.; Celli, B.R. Respiratory muscle and cardiopulmonary function during exercise in very severe COPD. Am. J. Respir. Crit. Care Med. 1996, 154, 1284–1289. [Google Scholar] [CrossRef]
- Stark-Leyva, K.N.; Beck, K.C.; Johnson, B.D. Influence of expiratory loading and hyperinflation on cardiac output during exercise. J. Appl. Physiol. 2004, 96, 1920–1927. [Google Scholar] [CrossRef]
- Miller, J.D.; Hemauer, S.J.; Smith, C.A.; Stickland, M.K.; Dempsey, J.A. Expiratory threshold loading impairs cardiovascular function in health and chronic heart failure during submaximal exercise. J. Appl. Physiol. 2006, 101, 213–227. [Google Scholar] [CrossRef][Green Version]
- Lammi, M.R.; Ciccolella, D.; Marchetti, N.; Kohler, M.; Criner, G.J. Increased oxygen pulse after lung volume reduction surgery is associated with reduced dynamic hyperinflation. Eur. Respir. J. 2012, 40, 837–843. [Google Scholar] [CrossRef]
- Tzani, P.; Aiello, M.; Elia, D.; Boracchia, L.; Marangio, E.; Olivieri, D.; Clini, E.; Chetta, A. Dynamic hyperinflation is associated with a poor cardiovascular response to exercise in COPD patients. Respir. Res. 2011, 12, 150. [Google Scholar] [CrossRef] [PubMed]
- Teopompi, E.; Tzani, P.; Aiello, M.; Ramponi, S.; Andrani, F.; Marangio, E.; Clini, E.; Chetta, A. Fat-free mass depletion is associated with poor exercise capacity irrespective of dynamic hyperinflation in COPD patients. Respir. Care 2014, 59, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Dickstein, K.; Cohen-Solal, A.; Filippatos, G.; McMurray, J.J.; Ponikowski, P.; Poole-Wilson, P.A.; Stromberg, A.; van Veldhuisen, D.J.; Atar, D.; Hoes, A.W.; et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur. Heart. J. 2008, 29, 2388–2442. [Google Scholar] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar]
- Ahmad, M.N.; Yusuf, S.H.; Ullah, R.; Ahmad, M.M.; Ellis, M.K.; Yousaf, H.; Patrick, T.E.; Ammar, K.A. Multivariate Criteria Most Accurately Distinguish Cardiac from Noncardiac Causes of Dyspnea. Tex. Heart Inst. J. 2015, 42, 514–521. [Google Scholar] [CrossRef]
- Chuang, M.L.; Lin, I.F.; Huang, S.F.; Hsieh, M.J. Patterns of Oxygen Pulse Curve in Response to Incremental Exercise in Patients with Chronic Obstructive Pulmonary Disease-An Observational Study. Sci. Rep. 2017, 7, 10929. [Google Scholar] [CrossRef]
- Chaudhry, S.; Arena, R.; Wasserman, K.; Hansen, J.E.; Lewis, G.D.; Myers, J.; Chronos, N.; Boden, W.E. Exercise-induced myocardial ischemia detected by cardiopulmonary exercise testing. Am. J. Cardiol. 2009, 103, 615–619. [Google Scholar] [CrossRef]
- Degani-Costa, L.H.; Nery, L.E.; Rodrigues, M.T.; Gimenes, A.C.; Ferreira, E.V.; Ota-Arakaki, J.S.; Neder, J.A.; Ramos, R.P. Does oxygen pulse trajectory during incremental exercise discriminate impaired oxygen delivery from poor muscle oxygen utilisation? ERJ Open Res. 2019, 5, 00108–02018. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Bohm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 33, 1787–1847. [Google Scholar]
- Huang, T.H.; Hsiue, T.R.; Lin, S.H.; Liao, X.M.; Su, P.L.; Chen, C.Z. Comparison of different staging methods for COPD in predicting outcomes. Eur. Respir. J. 2018, 51, 1700577. [Google Scholar] [CrossRef]
- GOLD Committees. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2019. Available online: www.goldcopd.org (accessed on 1 July 2021).
- Chuang, M.L.; Lin, I.F.; Lee, C.Y. Clinical assessment tests in evaluating patients with chronic obstructive pulmonary disease-A cross-sectional study. Medicine 2016, 95, e5471. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Chuang, M.L.; Lin, I.F.; Wasserman, K. The body weight-walking distance product as related to lung function, anaerobic threshold and peak VO2 in COPD patients. Respir. Med. 2001, 95, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Chuang, M.L.; Chuang, D.C.; Lin, I.F.; Vintch, J.R.; Ker, J.J.; Tsao, T.C. Ventilation and exercise performance after phrenic nerve and multiple intercostal nerve transfers for avulsed brachial plexus injury. Chest 2005, 128, 3434–3439. [Google Scholar] [CrossRef] [PubMed]
- Leite, J.J.; Mansur, A.J.; de Freitas, H.F.G.; Chizola, P.R.; Bocchi, E.A.; Terra-Filho, M.; Neder, J.A.; Lorenzi-Filho, G. Periodic breathing during incremental exercise predicts mortality in patients with chronic heart failure evaluated for cardiac transplantation. J. Am. Coll. Cardiol. 2003, 41, 2175–2181. [Google Scholar] [CrossRef]
- Sharir, T.; Germano, G.; Kang, X.; Lewin, H.C.; Miranda, R.; Cohen, I.; Agafitei, R.D.; Friedman, J.D.; Berman, D.S. Prediction of myocardial infarction versus cardiac death by gated myocardial perfusion SPECT: Risk stratification by the amount of stressinduced ischemia and poststress ejection fraction. J. Nucl. Med. 2001, 42, 831–837. [Google Scholar]
- Chuang, M.L.; Lee, C.H.; Lin, I.F. Using the oxygen-cost diagram in ramp-slope selection for dyspneic patients. Intern. Med. 2010, 49, 1325–1332. [Google Scholar] [CrossRef][Green Version]
- Kjaer, A.; Lebech, A.; Hesse, B.; Petersen, C.L. Right-sided cardiac function in healthy volunteers measured by first-pass radionuclide ventriculography and gated blood-pool SPECT: Comparison with cine MRI. Clin. Physiol. Funct. Imaging 2005, 25, 344–349. [Google Scholar] [CrossRef]
- Matthay, R.A.; Berger, H.J.; Davies, R.A.; Loke, J.; Mahler, D.A.; Gottschalk, A.; Zaret, B.L. Right and left ventricular exercise performance in chronic obstructive pulmonary disease: Radionuclide assessment. Ann. Intern. Med. 1980, 93, 234–239. [Google Scholar] [CrossRef]
- Belardinelli, R.; Lacalaprice, F.; Carle, F.; Minnucci, A.; Cianci, G.; Perna, G.; D’Eusanio, G. Exercise-induced myocardial ischaemia detected by cardiopulmonary exercise testing. Eur. Heart J. 2003, 24, 1304–1313. [Google Scholar] [CrossRef]
- Hurst, J.R.; Vestbo, J.; Anzueto, A.; Locantore, N.; Müllerova, H.; Tal-Singer, R.; Miller, B.; Lomas, D.A.; Agusti, A.; Macnee, W.; et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N. Engl. J. Med. 2010, 363, 1128–1138. [Google Scholar] [CrossRef] [PubMed]
- Mullerova, H.; Maselli, D.J.; Locantore, N.; Vestbo, J.; Hurst, J.R.; Wedzicha, J.A.; Bakke, P.; Agusti, A.; Anzueto, A. Hospitalized exacerbations of COPD: Risk factors and outcomes in the ECLIPSE cohort. Chest 2015, 147, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Hulley, S.B.; Cummings, S.R.; Browner, W.S.; Grady, D.; Newman, T.B. Designing Clinical Research: An Epidemiologic Approach, 4th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Flaherty, K.R.; Wald, J.; Weisman, I.M.; Zeballos, R.J.; Schork, M.A.; Blaivas, M.; Rubenfire, M.; Martinez, F.J. Unexplained exertional limitation characterization of patients with a mitochondrial myopathy. Am. J. Respir. Crit. Care Med. 2001, 164, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Stringer, W.; Hansen, J.E.; Wasserman, K. Cardiac output estimated noninvasively from oxygen uptake during exercise. J. Appl. Physiol. 1997, 82, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Munhoz, E.C.; Hollanda, R.; Vargas, J.P.; Silveira, C.W.; Lemos, A.L.; Hollanda, R.M.; Ribeiro, J.P. Flattening of oxygen pulse during exercise may detect extensive myocardial ischemia. Med. Sci. Sports Exerc. 2007, 39, 1221–1226. [Google Scholar] [CrossRef]
- Taivassalo, T.; Jensen, T.D.; Kennaway, N.; DiMauro, S.; Vissing, J.; Haller, R.G. The spectrum of exercise tolerance in mitochondrial myopathies: A study of 40 patients. Brain 2003, 126, 413–423. [Google Scholar] [CrossRef]
- Adibi, A.; Sin, D.D.; Safari, A.; Johnson, K.M.; Aaron, S.D.; FitzGerald, J.M.; Sadatsafavi, M. The Acute COPD Exacerbation Prediction Tool (ACCEPT): A modelling study. Lancet Respir. Med. 2020, 8, 1013–1021. [Google Scholar] [CrossRef]
- Singh, M.; Gersh, B.J.; McClelland, R.L.; Ho, K.K.; Willerson, J.T.; Penny, W.F.; Holmes, D.R., Jr. Predictive factors for ischemic target vessel revascularization in the Prevention of Restenosis with Tranilast and its Outcomes (PRESTO) trial. J. Am. Coll. Cardiol. 2005, 45, 198–203. [Google Scholar] [CrossRef]
- Sun, X.; Hansen, J.E.; Beshai, J.F.; Wasserman, K. Oscillatory breathing and exercise gas exchange abnormalities prognosticate early mortality and morbidity in heart failure. J. Am. Coll. Cardiol. 2010, 55, 1814–1823. [Google Scholar] [CrossRef]
- Meyer, P.; Filippatos, G.S.; Ahmed, M.I.; Iskandrian, A.E.; Bittner, V.; Perry, G.J.; White, M.; Aban, I.B.; Mujib, M.; Dell’Italia, L.J. Effects of right ventricular ejection fraction on outcomes in chronic systolic heart failure. Circulation 2010, 121, 252–258. [Google Scholar] [CrossRef]
- Francis, D.P.; Shamim, W.; Davies, L.C.; Piepoli, M.F.; Ponikowski, P.; Anker, S.D.; Coats, A.J. Cardiopulmonary exercise testing for prognosis in chronic heart failure: Continuous and independent prognostic value from VE/VCO(2)slope and peak VO(2). Eur. Heart J. 2000, 21, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Paolillo, S.; Veglia, F.; Salvioni, E.; Corra, U.; Piepoli, M.; Lagioia, R.; Limongelli, G.; Sinagra, G.; Cattadori, G.; Scardovi, A.B.; et al. Heart failure prognosis over time: How the prognostic role of oxygen consumption and ventilatory efficiency during exercise has changed in the last 20 years. Eur. J. Heart Fail. 2019, 21, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Sim, J.K.; Oh, J.Y.; Lee, Y.S.; Hur, G.Y.; Lee, S.Y.; Shim, J.J.; Rhee, C.K.; Min, K.H. Prognostic marker for severe acute exacerbation of chronic obstructive pulmonary disease: Analysis of diffusing capacity of the lung for carbon monoxide (DLCO) and forced expiratory volume in one second (FEV1). BMC Pulm. Med. 2021, 21, 152. [Google Scholar] [CrossRef] [PubMed]
- Oga, T.; Nishimura, K.; Tsukino, M.; Sato, S.; Hajiro, T. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: Role of exercise capacity and health status. Am. J. Respir. Crit. Care Med. 2003, 167, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Lindenauer, P.K.; Stefan, M.S.; Pekow, P.S.; Mazor, K.M.; Priya, A.; Spitzer, K.A.; Lagu, T.C.; Pack, Q.R.; Pinto-Plata, V.M.; ZuWallack, R. Association Between Initiation of Pulmonary Rehabilitation After Hospitalization for COPD and 1-Year Survival Among Medicare Beneficiaries. JAMA 2020, 323, 1813–1823. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Solal, A.; Barnier, P.; Pessione, F.; Seknadji, P.; Logeart, D.; Laperche, T.; Gourgon, R. Comparison of the long-term prognostic value of peak exercise oxygen pulse and peak oxygen uptake in patients with chronic heart failure. Heart 1997, 78, 572–576. [Google Scholar] [CrossRef] [PubMed]
| Group | CHF | COPD | Controls | ANOVA | |||
|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | mean | SD | p-value | |
| n | 27 | 30 | 33 | ||||
| Demographics and history | |||||||
| Age | 57.7 ‡ | 9.2 | 68.3 | 7.5 | 61.8 | 9.0 | ‡ |
| Height, cm | 167.4 | 4.2 | 166.0 | 4.9 | 166.7 | 5.2 | NS |
| Body mass index, kg/m2 | 26.6 ‡ | 3.2 | 23.1 | 3.2 | 24.8 | 2.7 | † |
| Smoke, pack-year | 28.9 ‡ | 28.1 | 67.9 | 38.8 | 2.9 | 9.7 | ‡ |
| SAECOPD 12 mo prior, count | NA | 6 | NA | NA | |||
| Cardiac event/SAECOPD on follow-up, count | 6 | 7 | NA | NA | |||
| SAECOPD on follow-up, rate, PPPY | NA | 0.21 | 0.65 | NA | NA | ||
| Functional capability and quality of life | |||||||
| NYHAfc I, II, III, IV, n | 14/12/1/0 | 12/13/5/0 | 32∨/0/0/0 | ‡ | |||
| Borg dyspnea score @ rest, 0/0.5/1/2, n | 13/8/6/0 | 18/9/1/2 | 32/0/1/0 | † | |||
| mMRC 0–4, n | 17/7/3/0/0 | 12/14/4/0/0 | 33/0/0/0/0 | ‡ | |||
| Oxygen-cost diagram, cm | 7.5 | 0.9 | 7.0 | 1.6 | 8.3 | 1.0 | † |
| CAT, summed score | 3.8 | 3.7 | 6.0 | 6.9 | 0.5 | 1.0 | ‡ |
| Blood test | |||||||
| hs-CRP, mg/dL | 0.2 * | 0.3 | 2.0 | 4.0 | 0.2 | 0.2 | ** |
| NT-proBNP, pg/mL | 358.3 ‡ | 295.8 | 46.0 | 36.0 | 45.3 | 36.2 | ‡ |
| Hemoglobin, gm/dL | 15.3 | 1.2 | 14.8 | 1.6 | 14.7 | 1.1 | NS |
| Cholesterol, mg/dL | 163.0 | 45.1 | NA | NA | NA | ||
| 2DLVEF | |||||||
| resting, % | 41.6 ‡ | 6.6 | 65.5 | 8.8 | 61.3 ^ | 5.9 | ‡ |
| Group | CHF | COPD | Controls | ANOVA | |||
|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | mean | SD | p-value | |
| n | 27 | 30 | 33 | ||||
| Lung function | |||||||
| FEV1 %predicted, % | 94.9 ‡ | 13.0 | 61.0 | 15.5 | 102.7 | 12.8 | ‡ |
| FEV1/FVC, % | 81.4 ‡ | 3.9 | 57.5 | 10.4 | 79.8 | 5.7 | ‡ |
| RV %predicted | 102.4 ‡ | 18.1 | 138.7 | 32.8 | 101.0 | 17.5 | ‡ |
| RV/TLC %predicted | 106.6 ‡ | 14.3 | 137.0 | 20.7 | 101.4 | 11.9 | ‡ |
| DLCO %predicted | 89.4 * | 12.9 | 76.5 | 20.4 | 106.2 | 15.4 | ‡ |
| CPET | |||||||
| V’E/VCO2 at anaerobic threshold | 33.1 ** | 5.7 | 38.2 | 6.7 | 31.7 | 3.6 | ‡ |
| at peak exercise | |||||||
| V’O2%pred | 72.9 | 17.7 | 72.8 | 18.4 | 91.6 | 19.3 | ‡ |
| Respiratory exchange ratio | 1.06 | 0.08 | 1.00 | 0.09 | 1.17 | 0.14 | ‡ |
| Heart rate (HR)%predicted | 83.0 | 11.4 | 82.9 | 11.6 | 95.2 | 9.6 | ‡ |
| ΔHR/ΔV’O2%, beat/min/L/min | 104.0 † | 35.2 | 94.3 | 21.9 | 104.1 | 29.1 | NS |
| O2P%predicted, % | 88.2 | 18.9 | 87.4 | 16.2 | 96.9 | 22.5 | NS |
| O2PCP, type I/P/D, n (%) | 9/13/4 ^ (35/50/15) | 14/12/4 (47/40/13) | 21/11/1 (64/33/3) | NS ^^ | |||
| ΔV’O2/ΔWR, slope 2 | 9.1 | 2.6 | 9.3 | 2.2 | 9.3 | 1.3 | NS |
| Blood pressure, systolic, mm Hg | 182.9 * | 22.4 | 203.3 | 35.2 | 207.1 | 25.9 | ** |
| Pulse pressure, mm Hg | 71.7 ‡ | 28.7 | 109.5 | 32.5 | 103.2 | 32.2 | ‡ |
| Breathing frequency, b/min | 31.6 | 7.3 | 32.8 | 6.5 | 36.4 | 10.3 | ¶ |
| ΔBorg dyspnea/ΔV’O2 | 10.5 | 5.1 | 12.7 | 7.0 | 8.8 | 3.5 | * |
| VT/TLC | 0.32 ‡ | 0.07 | 0.24 | 0.06 | 0.33 | 0.05 | ‡ |
| SpO2, % | 96.8 ‡ | 1.5 | 92.6 | 3.3 | 96.7 | 1.2 | ‡ |
| FPRV | |||||||
| FPRVEF,% | 52.3 † | 8.3 | 63.2 | 13.0 | 57.4 | 12.9 | ** |
| FPLVEF,% | 42.0 ‡ | 11.7 | 63.6 | 11.7 | 72.4 | 3.6 | ‡ |
| SPECT ^^^: SSS | 25.3 ‡ | 9.9 | 7.6 | 2.6 | NA | NA | |
| SDS | 0.7 | 1.6 | NA | NA | NA | ||
| LVEF post exercise,% | 44.8 ‡ | 17.2 | 70.3 | 1.7 | NA | NA | |
| Group, n | Normal, 33 | COPD, 30 | CHF, 27 | |||
|---|---|---|---|---|---|---|
| r | p-value | r | p-value | r | p-value | |
| Functional capability/Quality of life | ||||||
| Oxygen-cost diagram | 0.50 | 0.003 | ns | 0.37 | 0.07 | |
| Aerobic capability | ||||||
| V’O2peak% | 0.91 | <0.0001 | 0.85 | <0.0001 | 0.81 | <0.0001 |
| ΔV’O2/ΔWR | 0.42 | 0.02 | 0.60 | 0.001 | 0.69 | 0.0001 |
| Cardiac function | ||||||
| NT-proBNP | ns | ns | −0.40 | 0.06 | ||
| 2DLVEF, resting, % | ns | ns | ns | |||
| FPLVEF, peak, % | ns | ^ | ns | 0.49 | 0.02 | |
| FPRVEF, dynamic, % | 0.74 | 0.03 | ^ | ns | 0.40 | 0.06 |
| Peak dynamic hyperinflation | ||||||
| VT/TLC | ns | 0.53 | 0.003 | 0.44 | 0.03 | |
| Lung function | ||||||
| FEV1% | ns | 0.51 | 0.004 | ns | ||
| DLCO% | ns | 0.55 | 0.002 | ns | ||
| RV/TLC % predicted | −0.45 | 0.01 | −0.34 | 0.07 | ns | |
| Type | I | P | D | ||||
|---|---|---|---|---|---|---|---|
| CHF | |||||||
| Mean | SD | Mean | SD | Mean | SD | ||
| n | 9 | 13 | 4 | ||||
| NT-proBNP | 184.7 | 170.7 | 346.3 | 261.2 | 629.8 * | 410.6 | |
| CAT score | 2.2 | 2.4 | 3.4 | 3.3 | 7.5 * | 4.8 | |
| @peak exercise | |||||||
| V’O2/kg, mL/min/kg | 23.8 | 5.6 | 19.4 | 4.6 | 16.8 * | 2.9 | |
| O2P%predicted max,% | 101.2 | 12.0 | 80.0 | 19.8 | 85.4 * | 14.7 | |
| O2P%pred max < 80%, n ^ | 1 | 7 | 1 | ||||
| V’E/V’O2 | 31.0 | 5.2 | 41.3 | 6.7 | 37.6 ** | 2.0 | |
| FPRVEF, % | 51.0 | 7.9 | 50.4 | 8.9 | 58.3 | 4.7 | |
| FPLVEF, % | 44.2 | 7.9 | 40.7 | 13.2 | 42.4 | 16.1 | |
| COPD | |||||||
| n | 14 | 12 | 4 | ||||
| OCD score | 6.3 | 1.7 | 7.4 | 0.8 | 8.9 ** | 1.4 | |
| mMRC score | 1.1 | 0.7 | 0.6 | 0.5 | 0.0 ** | 0.0 | |
| NYHAFc score | 2.1 | 0.8 | 1.7 | 0.5 | 1.0 * | 0.0 | |
| @peak exercise | |||||||
| FPRVEF, % | 62.1 | 5.6 | 69.3 | 17.5 | 54.7 | 11.4 | |
| FPLVEF, % | 63.5 | 9.4 | 63.5 | 13.3 | 67.8 | 10.5 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chuang, M.-L.; Tsai, C.-F.; Ueng, K.-C.; Weng, J.-H.; Tsai, M.-F.; Lo, C.-H.; Chen, G.-B.; Sia, S.-K.; Chuang, Y.-T.; Wu, T.-C.; et al. The Impact of Oxygen Pulse and Its Curve Patterns on Male Patients with Heart Failure, Chronic Obstructive Pulmonary Disease, and Healthy Controls—Ejection Fractions, Related Factors and Outcomes. J. Pers. Med. 2022, 12, 703. https://doi.org/10.3390/jpm12050703
Chuang M-L, Tsai C-F, Ueng K-C, Weng J-H, Tsai M-F, Lo C-H, Chen G-B, Sia S-K, Chuang Y-T, Wu T-C, et al. The Impact of Oxygen Pulse and Its Curve Patterns on Male Patients with Heart Failure, Chronic Obstructive Pulmonary Disease, and Healthy Controls—Ejection Fractions, Related Factors and Outcomes. Journal of Personalized Medicine. 2022; 12(5):703. https://doi.org/10.3390/jpm12050703
Chicago/Turabian StyleChuang, Ming-Lung, Chin-Feng Tsai, Kwo-Chang Ueng, Jui-Hung Weng, Ming-Fong Tsai, Chien-Hsien Lo, Gang-Bin Chen, Sung-Kien Sia, Yao-Tsung Chuang, Tzu-Chin Wu, and et al. 2022. "The Impact of Oxygen Pulse and Its Curve Patterns on Male Patients with Heart Failure, Chronic Obstructive Pulmonary Disease, and Healthy Controls—Ejection Fractions, Related Factors and Outcomes" Journal of Personalized Medicine 12, no. 5: 703. https://doi.org/10.3390/jpm12050703
APA StyleChuang, M.-L., Tsai, C.-F., Ueng, K.-C., Weng, J.-H., Tsai, M.-F., Lo, C.-H., Chen, G.-B., Sia, S.-K., Chuang, Y.-T., Wu, T.-C., Kao, P.-F., & Hsieh, M.-J. (2022). The Impact of Oxygen Pulse and Its Curve Patterns on Male Patients with Heart Failure, Chronic Obstructive Pulmonary Disease, and Healthy Controls—Ejection Fractions, Related Factors and Outcomes. Journal of Personalized Medicine, 12(5), 703. https://doi.org/10.3390/jpm12050703






