Association of Genetic Polymorphisms with Complications of Implanted LVAD Devices in Patients with Congestive Heart Failure: A Kazakhstani Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Selection of the SNPs
2.3. DNA Extraction and SNP Genotyping
2.4. Statistical Analysis
3. Results
3.1. Clinical Characteristics of HF Patients with and without Complications
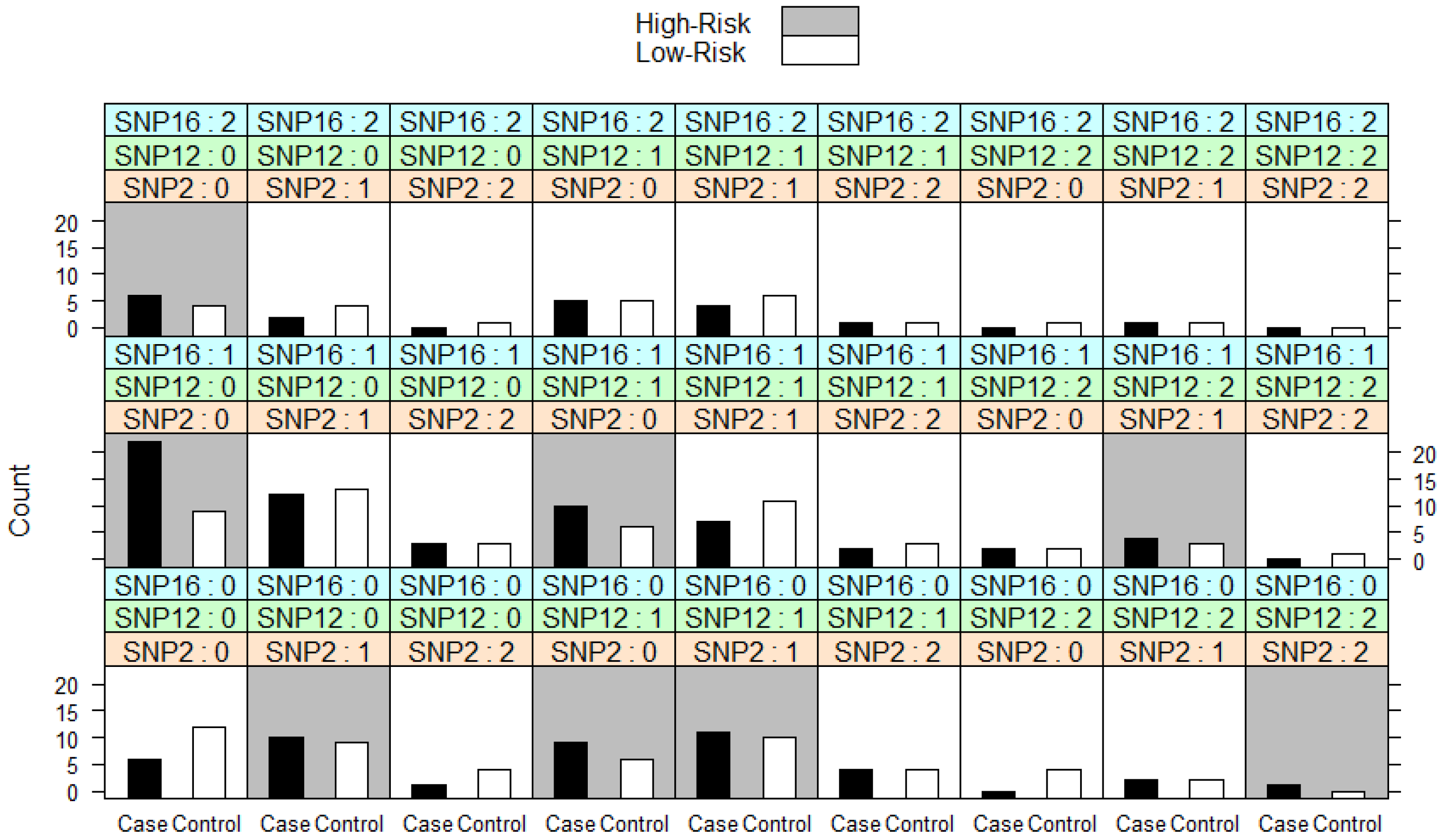
3.2. Analysis of Genotyping
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nakagita, K.; Wada, K.; Mukai, Y.; Uno, T.; Nishino, R.; Matsuda, S.; Takenaka, H.; Terakawa, N.; Oita, A.; Takada, M. Effects of vitamin K epoxide reductase complex 1 gene polymorphisms on warfarin control in Japanese patients with left ventricular assist devices (LVAD). Eur. J. Clin. Pharmacol. 2018, 74, 885–894. [Google Scholar] [CrossRef] [PubMed]
- Kadakia, S.; Moore, R.; Ambur, V.; Toyoda, Y. Current status of the implantable LVAD. Gen. Thorac. Cardiovasc. Surg. 2016, 64, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Nascimbene, A.; Neelamegham, S.; Frazier, O.H.; Moake, J.L.; Dong, J.F. Acquired von Willebrand syndrome associated with left ventricular assist device. Blood 2016, 127, 3133–3141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, A.; Williamitis, C.A.; Slaughter, M.S. Comparison of continuous-flow and pulsatile-flow left ventricular assist devices: Is there an advantage to pulsatility? Ann. Cardiothorac. Surg. 2014, 3, 573–581. [Google Scholar]
- Pya, Y.; Bekbossynova, M.; Jetybayeva, S.; Bekbossynov, S.; Andossova, S.; Salov, R.; Medressova, A.; Novikova, S.; Murzagaliyev, M. Initial 3-year outcomes with left ventricular assist devices in a country with a nascent heart transplantation program. ESC Heart Fail. 2016, 3, 26–34. [Google Scholar] [CrossRef] [Green Version]
- Zimpfer, D.; Netuka, I.; Schmitto, J.D.; Pya, Y.; Garbade, J.; Morshuis, M.; Beyersdorf, F.; Marasco, S.; Rao, V.; Damme, L.; et al. Multicentre clinical trial experience with the HeartMate 3 left ventricular assist device: 30-day outcomes. Eur. J. Cardiothorac. Surg. 2016, 50, 548–554. [Google Scholar] [CrossRef] [Green Version]
- Mondal, N.K.; Sorensen, E.N.; Hiivala, N.J.; Feller, E.D.; Pham, S.M.; Griffith, B.P.; Wu, Z.J. Intraplatelet reactive oxygen species, mitochondrial damage and platelet apoptosis augment non-surgical bleeding in heart failure patients supported by continuous-flow left ventricular assist device. Platelets 2015, 26, 536–544. [Google Scholar] [CrossRef]
- Susen, S.; Rauch, A.; van Belle, E.; Vincentelli, A.; Lenting, P.J. Circulatory support devices: Fundamental aspects and clinical management of bleeding and thrombosis. J. Thromb. Haemost. 2015, 13, 1757–1767. [Google Scholar] [CrossRef]
- Topkara, V.K.; Knotts, R.J.; Jennings, D.L.; Garan, A.R.; Levin, A.P.; Breskin, A.; Castagna, F.; Cagliostro, B.; Yuzefpolskaya, M.; Takeda, K.; et al. Effect of CYP2C9 and VKORC1 Gene Variants on Warfarin Response in Patients with Continuous-Flow Left Ventricular Assist Devices. ASAIO J. 2016, 62, 558–564. [Google Scholar] [CrossRef]
- Zimpfer, D.; Gustafsson, F.; Potapov, E.; Pya, Y.; Schmitto, J.; Berchtold-Herz, M.; Morshuis, M.; Shaw, S.M.; Saeed, D.; Lavee, J.; et al. Two-year outcome after implantation of a full magnetically levitated left ventricular assist device: Results from the ELEVATE Registry. Eur. Heart J. 2020, 41, 3801–3809. [Google Scholar] [CrossRef]
- Awad, M.; Czer, L.S.C.; Soliman, C.; Mirocha, J.; Ruzza, A.; Pinzas, J.; Rihbany, K.; Chang, D.; Moriguchi, J.; Ramzy, D.; et al. Prevalence of Warfarin Genotype Polymorphisms in Patients with Mechanical Circulatory Support. ASAIO J. 2015, 61, 391–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boehme, A.K.; Pamboukian, S.V.; George, J.F.; Beasley, T.M.; Kirklin, J.K.; Tallaj, J.; Dillon, C.; Levitan, E.B.; Griffin, R.; McGwin, G., Jr.; et al. Anticoagulation Control in Patients with Ventricular Assist Devices. ASAIO J. 2017, 63, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Perera, M.A.; Cavallari, L.H.; Limdi, N.A.; Gamazon, E.R.; Konkashbaev, A.; Daneshjou, R.; Pluzhnikov, A.; Crawford, D.C.; Wang, J.; Liu, N.; et al. Genetic variants associated with warfarin dose in African-American individuals: A genome-wide association study. Lancet 2013, 382, 790–796. [Google Scholar] [CrossRef] [Green Version]
- Scott, S.A.; Khasawneh, R.; Peter, I.; Kornreich, R.; Desnick, R.J. Combined CYP2C9, VKORC1 and CYP4F2 frequencies among racial and ethnic groups. Pharmacogenomics 2010, 11, 781–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Limdi, N.A.; Beasley, T.M.; Crowley, M.R.; Goldstein, J.A.; Rieder, M.J.; Flockhart, D.A.; Arnett, D.K.; Acton, R.T.; Liu, N. VKORC1 polymorphisms, haplotypes and haplotype groups on warfarin dose among African–Americans and European–Americans. Pharmacogenomics 2008, 9, 1445–1458. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Mondal, N.K.; Ding, J.; Koenig, S.C.; Slaughter, M.S.; Griffith, B.P.; Wu, Z.J. Activation and shedding of platelet glycoprotein IIb/IIIa under non-physiological shear stress. Mol. Cell Biochem. 2015, 409, 93–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Z.; Koenig, S.C.; Slaughter, M.S.; Griffith, B.P.; Wu, Z.J. Quantitative Characterization of Shear-Induced Platelet Receptor Shedding: Glycoprotein Ibalpha, Glycoprotein VI, and Glycoprotein IIb/IIIa. ASAIO J. 2018, 64, 773–778. [Google Scholar] [CrossRef]
- Knowles, J.W.; Wang, H.; Itakura, H.; Southwick, A.; Myers, R.M.; Iribarren, C.; Fortmann, S.P.; Go, A.S.; Quertermous, T.; Hlatky, M.A. Association of polymorphisms in platelet and hemostasis system genes with acute myocardial infarction. Am. Heart J. 2007, 154, 1052–1058. [Google Scholar] [CrossRef] [Green Version]
- Feher, G.; Feher, A.; Pusch, G.; Lupkovics, G.; Szapary, L.; Papp, E. The genetics of antiplatelet drug resistance. Clin. Genet. 2009, 75, 1–18. [Google Scholar] [CrossRef]
- Wurtz, M.; Kristensen, S.D.; Hvas, A.M.; Grove, E.L. Pharmacogenetics of the Antiplatelet Effect of Aspirin. Curr. Pharm. Des. 2012, 18, 5294–5308. [Google Scholar] [CrossRef]
- Alrashid, M.H.; Al-Serri, A.; Alshemmari, S.H.; Koshi, P.; Al-Bustan, S.A. Association of Genetic Polymorphisms in the VKORC1 and CYP2C9 Genes with Warfarin Dosage in a Group of Kuwaiti Individuals. Mol. Diagn Ther. 2016, 20, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Limdi, N.A.; Veenstra, D.L. Warfarin pharmacogenetics. Pharmacotherapy 2008, 28, 1084–1097. [Google Scholar] [CrossRef] [PubMed]
- Krishna Kumar, D.; Shewade, D.G.; Loriot, M.A.; Beaune, P.; Balachander, J.; Sai Chandran, B.V.; Adithan, C. Effect of CYP2C9, VKORC1, CYP4F2 and GGCX genetic variants on warfarin maintenance dose and explicating a new pharmacogenetic algorithm in South Indian population. Eur. J. Clin. Pharmacol. 2014, 70, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Agúndez, J.A.G.; Martínez, C.; Pérez-Sala, D.; Carballo, M.; Torres, M.J.; García-Martín, E. Pharmacogenomics in Aspirin Intolerance. Curr. Drug Metab. 2009, 10, 998–1008. [Google Scholar] [CrossRef] [Green Version]
- Wadelius, M.; Chen, L.Y.; Eriksson, N.; Bumpstead, S.; Ghori, J.; Wadelius, C.; Bentley, D.; McGinnis, R.; Deloukas, P. Association of warfarin dose with genes involved in its action and metabolism. Hum. Genet. 2007, 121, 23–34. [Google Scholar] [CrossRef] [Green Version]
- van Hylckama Vlieg, A.; Baglin, C.A.; Bare, L.A.; Rosendaal, F.R.; Baglin, T.P. Proof of principle of potential clinical utility of multiple SNP analysis for prediction of recurrent venous thrombosis. J. Thromb. Haemost. 2008, 6, 751–754. [Google Scholar] [CrossRef]
- Shi, H.; Yang, S.; Liu, Y.; Huang, P.; Lin, N.; Sun, X.; Yu, R.; Zhang, Y.; Qin, Y.; Wang, L. Study on Environmental Causes and SNPs of MTHFR, MS and CBS Genes Related to Congenital Heart Disease. PLoS ONE 2015, 10, e0128646. [Google Scholar] [CrossRef] [Green Version]
- Ritchie, M.D.; Hahn, L.W.; Roodi, N.; Bailey, L.R.; Dupont, W.D.; Parl, F.F.; Moore, J.H. Multifactor-dimensionality reduction reveals high-order interactions among estrogen-metabolism genes in sporadic breast cancer. Am. J. Hum. Genet. 2001, 69, 138–147. [Google Scholar] [CrossRef] [Green Version]
- Winham, S.J.; Motsinger-Reif, A.A. An R package implementation of multifactor dimensionality reduction. BioData Min. 2011, 4, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Patron, J.; Serra-Cayuela, A.; Han, B.; Li, C.; Wishart, D.S. Assessing the performance of genome-wide association studies for predicting disease risk. PLoS ONE 2019, 14, e0220215. [Google Scholar] [CrossRef] [Green Version]
- Al-Eitan, L.N.; Almasri, A.Y.; Khasawneh, R.H. Effects of CYP2C9 and VKORC1 polymorphisms on warfarin sensitivity and responsiveness during the stabilization phase of therapy. Saudi Pharm. J. 2019, 27, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Topkara, V.K.; Levin, A.; Mody, K.; Garan, A.; Ronquillo, K.O.; Tiburcio, M.; Murphy, J.S.; Parkis, G.; Takeda, K.; Takayama, H.; et al. Association of Warfarin Genotype with Thrombosis and Bleeding Events in Continuous-Flow Left Ventricular Assist Device (CF-LVAD) Patients. J. Heart Lung Transpl. 2015, 34, S13. [Google Scholar] [CrossRef]
- Hu, J.; Mondal, N.K.; Sorensen, E.N.; Cai, L.; Fang, H.B.; Griffith, B.P.; Wu, Z.J. Platelet glycoprotein Ibalpha ectodomain shedding and non-surgical bleeding in heart failure patients supported by continuous-flow left ventricular assist devices. J. Heart Lung Transpl. 2014, 33, 71–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Z.; Zhang, J.; Kareem, K.; Tran, D.; Conway, R.G.; Arias, K.; Griffith, B.P.; Wu, Z.J. Device-induced platelet dysfunction in mechanically assisted circulation increases the risks of thrombosis and bleeding. Artif. Organs 2019, 43, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Koliopoulou, A.; McKellar, S.H.; Rondina, M.; Selzman, C.H. Bleeding and thrombosis in chronic ventricular assist device therapy: Focus on platelets. Curr. Opin. Cardiol. 2016, 31, 299–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grinshtein, Y.I.; Kosinova, A.A.; Grinshtein, I.Y.; Subbotina, T.N.; Savchenko, A.A. The Prognostic Value of Combinations of Genetic Polymorphisms in the ITGB3, ITGA2, and CYP2C19*2 Genes in Predicting Cardiovascular Outcomes After Coronary Bypass Grafting. Genet. Test. Mol. Biomark. 2018, 22, 259–265. [Google Scholar] [CrossRef] [Green Version]
- Stankovic, S.; Majkic-Singh, N. Genetic aspects of ischemic stroke: Coagulation, homocysteine, and lipoprotein metabolism as potential risk factors. Crit. Rev. Clin. Lab. Sci. 2010, 47, 72–123. [Google Scholar] [CrossRef]
- Kucharska-Newton, A.M.; Monda, K.L.; Campbell, S.; Bradshaw, P.T.; Wagenknecht, L.E.; Boerwinkle, E.; Wasserman, B.A.; Heiss, G. Association of the platelet GPIIb/IIIa polymorphism with atherosclerotic plaque morphology: The Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis 2011, 216, 151–156. [Google Scholar] [CrossRef] [Green Version]
- Grove, E.L.; Orntoft, T.F.; Lassen, J.F.; Jensen, H.K.; Kristensen, S.D. The platelet polymorphism PlA2 is a genetic risk factor for myocardial infarction. J. Int. Med. 2004, 255, 637–644. [Google Scholar] [CrossRef]
- Nadasi, E.; Bene, J.; Havasi, V.; Komlosi, K.; Talian, G.; Melegh, G.; Papp, E.; Gasztonyi, B.; Szolnoki, Z.; Sandor, J.; et al. Detection of the Leu40Arg variant of the platelet glycoprotein IIb/IIIa receptor in subjects with thrombotic diseases. Thromb. Res. 2005, 116, 479–482. [Google Scholar] [CrossRef]
- Lanni, F.; Santulli, G.; Izzo, R.; Rubattu, S.; Zanda, B.; Volpe, M.; Iaccarino, G.; Trimarco, B. The PlA1/A2 polymorphism of glycoprotein IIIa and cerebrovascular events in hypertension: Increased risk of ischemic stroke in high-risk patients. J. Hypertens. 2007, 25, 551–556. [Google Scholar] [CrossRef] [PubMed]
- van Oijen, M.G.; Huybers, S.; Peters, W.H.; Drenth, J.P.; Laheij, R.J.; Verheugt, F.W.; Jansen, J.B. Polymorphisms in genes encoding acetylsalicylic acid metabolizing enzymes are unrelated to upper gastrointestinal health in cardiovascular patients on acetylsalicylic acid. Br. J. Clin. Pharmacol. 2005, 60, 623–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maruo, Y.; Iwai, M.; Mori, A.; Sato, H.; Takeuchi, Y. Polymorphism of UDP-Glucuronosyltransferase and Drug Metabolism. Curr. Drug Metab. 2005, 6, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Kuehl, G.E.; Bigler, J.; Rimorin, C.F.; Schwarz, Y.; Shen, D.D.; Lampe, J.W. UGT1A6 polymorphism and salicylic acid glucuronidation following aspirin. Pharmacogen. Genom. 2007, 17, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Sheth, H.; Northwood, E.; Ulrich, C.M.; Scherer, D.; Elliott, F.; Barrett, J.H.; Forman, D.; Wolf, C.R.; Smith, G.; Jackson, M.S.; et al. Interaction between polymorphisms in aspirin metabolic pathways, regular aspirin use and colorectal cancer risk: A case-control study in unselected white European populations. PLoS ONE 2018, 13, e0192223. [Google Scholar] [CrossRef] [Green Version]
- Zhang, C.; He, Y.; Shan, K.R.; Tan, K.; Zhang, T.; Wang, C.J.; Guan, Z.Z. Correlations between polymorphisms in the uridine diphosphate-glucuronosyltransferase 1A and C-C motif chemokine receptor 5 genes and infection with the hepatitis B virus in three ethnic groups in China. J. Int. Med. Res. 2018, 46, 739–751. [Google Scholar] [CrossRef]
- Scherer, D.; Koepl, L.M.; Poole, E.M.; Balavarca, Y.; Xiao, L.; Baron, J.A.; Hsu, L.; Coghill, A.E.; Campbell, P.T.; Kleinstein, S.E.; et al. Genetic variation in UGT genes modify the associations of NSAIDs with risk of colorectal cancer: Colon cancer family registry. Genes Chromosomes Cancer 2014, 53, 568–578. [Google Scholar] [CrossRef] [Green Version]
- Thompson, C.L.; Plummer, S.J.; Merkulova, A.; Cheng, I.; Tucker, T.C.; Casey, G.; Li, L. No association between cyclooxygenase-2 and uridine diphosphate glucuronosyltransferase 1A6 genetic polymorphisms and colon cancer risk. World J. Gastroenterol. 2009, 15, 2240–2244. [Google Scholar] [CrossRef]
- Iskakova, A.N.; Romanova, A.A.; Aitkulova, A.M.; Sikhayeva, N.S.; Zholdybayeva, E.V.; Ramanculov, E.M. Polymorphisms in genes involved in the absorption, distribution, metabolism, and excretion of drugs in the Kazakhs of Kazakhstan. BMC Genet. 2016, 17, 23. [Google Scholar] [CrossRef] [Green Version]
- Boyle, A.J.; Jorde, U.P.; Sun, B.; Park, S.J.; Milano, C.A.; Frazier, O.H.; Sundareswaran, K.S.; Farrar, D.J.; Russell, S.D. Pre-operative risk factors of bleeding and stroke during left ventricular assist device support: An analysis of more than 900 HeartMate II outpatients. J. Am. Coll. Cardiol. 2014, 63, 880–888. [Google Scholar] [CrossRef] [Green Version]
- Xiang, Q.; Ji, S.D.; Zhang, Z.; Zhao, X.; Cui, Y.M. Identification of ITGA2B and ITGB3 Single-Nucleotide Polymorphisms and Their Influences on the Platelet Function. BioMed. Res. Int. 2016, 2016, 5675084. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sciaccaluga, C.; Ghionzoli, N.; Mandoli, G.E.; D’Ascenzi, F.; Focardi, M.; Valente, S.; Cameli, M. Biomarkers in Patients with Left Ventricular Assist Device: An Insight on Current Evidence. Biomolecules 2022, 12, 334. [Google Scholar] [CrossRef] [PubMed]
- Oussalah, A.; Bosco, P.; Anello, G.; Spada, R.; Gueant-Rodriguez, R.M.; Chery, C.; Rouyer, P.; Josse, T.; Romano, A.; Elia, M.; et al. Exome-Wide Association Study Identifies New Low-Frequency and Rare UGT1A1 Coding Variants and UGT1A6 Coding Variants Influencing Serum Bilirubin in Elderly Subjects: A Strobe Compliant Article. Medicine 2015, 94, e925. [Google Scholar] [CrossRef] [PubMed]
- Mazur-Kominek, K.; Romanowski, T.; Bielawski, K.; Kielbratowska, B.; Preis, K.; Domzalska-Popadiuk, I.; Slominska-Fraczek, M.; Sznurkowska, K.; Renke, J.; Plata-Nazar, K.; et al. Association between uridin diphosphate glucuronosylotransferase 1A1 (UGT1A1) gene polymorphism and neonatal hyperbilirubinemia. Acta Biochim. Pol. 2017, 64, 351–356. [Google Scholar] [CrossRef]
- Justyna Gil, J.; Sąsiadek, M.M. Gilbert syndrome: The UGT1A1*28 promoter polymorphism as a biomarker of multifactorial diseases and drug metabolism. Biomark. Med. 2012, 6, 223–230. [Google Scholar]
- Sarajlic, P.; Simonsson, M.; Jernberg, T.; Back, M.; Hofmann, R. Incidence, associated outcomes, and predictors of upper gastrointestinal bleeding following acute myocardial infarction: A SWEDEHEART-based nationwide cohort study. Eur. Heart J. Cardiovasc. Pharmacother. 2021, 1–9. [Google Scholar] [CrossRef]

| Characteristic | Control Group, N = 95 | HF Patients, N = 98 | p Value |
|---|---|---|---|
| Age (years) | 44.01 ± 13.8 | 52.7 ± 11.0 | 0.001 ** |
| Gender | |||
| Male | 63 (66.3) | 92 (93.9) | 0.001 |
| Female | 32 (33.7) | 6 (6.1) | |
| Ethnicity | |||
| Asian | 60 (63.2) | 77 (78.6) | 0.03 |
| Caucasian | 35 (36.8) | 21 (21.4) | |
| Body weight (kg) | 69.5 ± 14.0 | 79.8 ± 13.9 | 0.001 ** |
| Height (cm) | 168.3 ± 7.46 | 169.8 ± 6.36 | 0.15 * |
| BMI (kg/m) | 24.6 ± 4.9 | 27.7 ± 4.5 | 0.001 ** |
| SBP | 114.4 ± 9.9 | 104.8 ± 15.5 | 0.001 ** |
| DBP | 75.7 ± 5.7 | 71.2 ± 10.3 | 0.001 ** |
| History of smoking | |||
| Smokers | 38 (40.0) | 58 (59.2) | 0.01 |
| Non-smokers | 57 (60.0) | 40 (40.8) | |
| Diagnosis | - | ||
| ICM | - | 44 (44.9) | |
| DCM | - | 40 (40.8) | |
| HCM | - | 11 (11.2) | |
| VHD | - | 3 (3.1) | |
| NYHA | - | ||
| I | - | 1 (1.0) | |
| II | - | 1 (1.0) | |
| III | - | 2 (2.0) | |
| IV | - | 26 (26.5) | |
| IIIA | - | 34 (34.7) | |
| IIIB | - | 34 (34.7) | |
| HF type | - | ||
| HFrEF | - | 97 (99.0) | |
| HFmrEF | - | 1 (1.0) | |
| INR | - | ||
| Basic INR | - | 1.21 ± 0.36 | |
| Target INR | - | 2.39 ± 0.26 | |
| Device strategy | - | ||
| BTT | - | 10 (10.2) | |
| DT | - | 88 (89.8) | |
| Device type | - | ||
| HW | - | 18 (18.4) | |
| HM2 | - | 34 (34.7) | |
| HM3 | - | 46 (46.9) | |
| Warfarin dose (mg/day) | - | 2.99 ± 1.15 | |
| Duration of LVAD support till outcome, from 2011 untill 2016, n = 36 (in months) | - | 29.6 ± 17.3 | |
| Patients’ achieved outcome till 2017 | - | ||
| Survived | - | 71 (72.4) | |
| Not-survived | - | 27 (27.6) | |
| Thrombosis | - | ||
| Yes | - | 13 (13.3) | |
| No | - | 85 (86.7) | |
| Bleeding | - | ||
| Yes | - | 14 (14.3) | |
| No | - | 84 (85.7) | |
| Infections | - | ||
| Yes | - | 39 (39.8) | |
| No | - | 59 (60.2) | |
| Stroke | - | ||
| No Stroke | - | 78 (79.6) | |
| Hemorrhagic stroke | - | 8 (8.2) | |
| Ischemic stroke | - | 12 (12.2) | |
| Myocardial infarction | - | ||
| Yes | - | 44 (44.9) | |
| No | - | 54 (55.1) | |
| Characteristic | Comparison between HF Patients | ||
|---|---|---|---|
| Group 1, N = 74 | Group 2, N = 24 | p Value | |
| Age (years) | 52.5 ± 11.3 | 53.4 ± 10.1 | 0.92 ** |
| Gender | |||
| Male | 71 (95.9) | 21 (87.5) | 0.16 |
| Female | 3 (4.1) | 3 (12.5) | |
| Ethnicity | |||
| Asian | 56 (75.7) | 21 (87.5) | 0.27 |
| Caucasian | 18 (24.3) | 3 (12.5) | |
| Body weight (kg) | 80.0 ± 12.2 | 79.3 ± 18.5 | 0.86 * |
| Height (cm) | 170.0 ± 6.08 | 168.9 ± 7.24 | 0.46 * |
| BMI (kg/m) | 27.7 ± 4.10 | 27.6 ± 5.66 | 0.97 * |
| SBP | 105.0 ± 15.7 | 104.0 ± 15.0 | 0.99 ** |
| DBP | 70.9 ± 10.7 | 72.1 ± 9.35 | 0.33 ** |
| History of smoking | |||
| Smokers | 46 (62.2) | 12 (50.0) | 0.34 |
| Non-smokers | 28 (37.8) | 12 (50.0) | |
| Diagnosis | |||
| ICM | 36 (48.6) | 8 (33.3) | 0.10 |
| DCM | 25 (33.8) | 15 (62.5) | |
| HCM | 10 (13.5) | 1 (4.2) | |
| VHD | 3 (4.1) | 0 | |
| NYHA | |||
| I | 1 (1.4) | 0 | 0.58 |
| II | 1 (1.4) | 0 | |
| III | 1 (1.4) | 1 (4.2) | |
| IV | 17 (23.0) | 9 (37.5) | |
| IIIA | 27 (36.5) | 7 (29.2) | |
| IIIB | 27 (36.5) | 7 (29.2) | |
| HF type | |||
| HFrEF | 74 (100) | 23 (95.8) | 0.25 |
| HFmrEF | 0 | 1 (4.2) | |
| INR | |||
| Basic INR | 1.19 ± 0.37 | 1.26 ± 0.33 | 0.11 ** |
| Target INR | 2.36 ± 0.24 | 2.46 ± 0.32 | 0.06 ** |
| Device strategy | |||
| BTT | 6 (8.1) | 4 (16.7) | 0.25 |
| DT | 68 (91.9) | 20 (83.3) | |
| Device type | |||
| HW | 11 (14.9) | 7 (29.2) | 0.01 |
| HM2 | 22 (29.7) | 12 (50.0) | |
| HM3 | 41 (55.4) | 5 (20.8) | |
| Warfarin dose (mg/day) | 3.01 ± 1.04 | 2.92 ± 1.46 | 0.29 ** |
| Duration of LVAD support till outcome, from 2011 untill 2016, n = 36 (in months) | 29.1 ± 17.6 (n = 21) | 30.3 ± 17.5 (n = 15) | 0.84 * |
| Patients’ achieved outcome till 2017 | |||
| Survived | 58 (78.4) | 13 (54.2) | 0.03 |
| Not-survived | 16 (21.6) | 11 (45.8) | |
| Thrombosis | |||
| Yes | 0 | 13 (54.2) | 0.0001 |
| No | 74 (100) | 11 (45.8) | |
| Bleeding | |||
| Yes | 0 | 14 (58.3) | 0.0001 |
| No | 74 (100) | 10 (41.7) | |
| Infections | |||
| Yes | 24 (32.4) | 15 (62.5) | 0.015 |
| No | 50 (67.6) | 9 (37.5) | |
| Stroke | |||
| No Stroke | 60 (81.1) | 18 (75.0) | 0.57 |
| Hemorrhagic stroke | 5 (6.8) | 3 (12.5) | |
| Ischemic stroke | 9 (12.2) | 3 (12.5) | |
| Myocardial infarction | |||
| Yes | 36 (48.6) | 8 (33.3) | 0.24 |
| No | 38 (51.4) | 16 (66.7) | |
| Study Groups | Parameters | Before 14 Days | p-Value | After 3–6 Months | p-Value | After 12–18 Month | p-Value |
|---|---|---|---|---|---|---|---|
| Group 1 | Hemoglobin, g/L | 139.6 ± 18.2 | 129.5 ± 16.2 | 125.7 ± 20.0 | |||
| Group 2-1 | 145.8 ± 21.7 | 0.32 * | 129.0 ± 15.3 | 0.93 * | 125.1 ± 18.4 | 0.95 * | |
| Group 2-2 | 128.5 ± 21.2 | 0.052 * | 111.1 ± 29.2 | 0.04 ** | 117.6 ± 35.0 | 0.55 * | |
| Group 1 | Hematocrit, % | 41.1 ± 6.72 | 38.2 ± 4.92 | 37.5 ± 5.46 | |||
| Group 2-1 | 43.1 ± 6.95 | 0.39 * | 37.0 ± 3.67 | 0.51 * | 36.3 ± 6.14 | 0.58 * | |
| Group 2-2 | 39.0 ± 6.61 | 0.30 * | 32.8 ± 8.70 | 0.016 * | 35.6 ± 10.3 | 0.63 * | |
| Group 1 | Lymphocytes, % | 27.5 ± 9.25 | 26.2 ± 8.79 | 22.0 ± 6.44 | |||
| Group 2-1 | 31.0 ± 8.78 | 0.19 ** | 18.4 ± 6.34 | 0.015 * | 29.8 ± 11.3 | 0.03 ** | |
| Group 2-2 | 21.8 ± 6.28 | 0.02 ** | 24.8 ± 9.35 | 0.68 * | 19.9 ± 11.3 | 0.27 ** | |
| Group 1 | LDH, U/L | 271.5 ± 137.0 | 273.5 ± 93.7 | 306.0 ± 156.1 | |||
| Group 2-1 | N/A | 335.4 ± 133.3 | 0.24 ** | 194.6 ± 42.7 | 0.02 ** | ||
| Group 2-2 | 254.0 ± 171.9 | 0.38 ** | 260.2 ± 139.0 | 0.78 * | 377.4 ± 174.2 | 0.19 ** | |
| Group 1 | AST, U/L | 27.9 ± 21.4 | 19.6 ± 5.50 | 21.2 ± 8.08 | |||
| Group 2-1 | 29.5 ± 10.6 | 0.11 ** | 26.9 ± 19.0 | 0.42 ** | 22.2 ± 8.44 | 0.77 * | |
| Group 2-2 | 33.3 ± 27.0 | 0.43 ** | 36.9 ± 37.5 | 0.02 ** | 43.0 ± 70.3 | 0.63 ** | |
| Group 1 | Total bilirubin, mg/dL | 1.33 ± 1.56 | 0.70 ± 0.51 | 1.03 ± 1.51 | |||
| Group 2-1 | 1.03 ± 0.73 | 0.74 ** | 1.26 ± 0.58 | 0.01 ** | 0.76 ± 0.80 | 0.55 ** | |
| Group 2-2 | 3.00 ± 5.09 | 0.40 ** | 1.59 ± 2.76 | 0.77 ** | 0.96 ± 0.71 | 0.42 ** |
| Gene | SNP rs Number | Genotype | Control Group, No. (%) | Allele Frequency in Population Control Group | HF Patients, No. (%) | Allele Frequency in HF Patients | p Value |
|---|---|---|---|---|---|---|---|
| VKORC1*1 | rs8050894 | CC | 17 (17.9) | C:G = 0.39:0.61 | 55 (56.1) | C:G = 0.68:0.32 | 0.0001 * |
| CG | 41 (43.2) | 24 (24.5) | |||||
| GG | 37 (38.9) | 19 (19.4) | |||||
| C | 75 | 134 | |||||
| G | 115 | 62 | |||||
| ITGB3 | rs5918 | TT | 71 (74.7) | T:C = 0.87:0.13 | 48 (49.0) | T:C = 0.66:0.34 | 0.0001 * |
| TC | 23 (24.2) | 34 (34.7) | |||||
| CC | 1 (1.1) | 16 (16.3) | |||||
| T | 165 | 130 | |||||
| C | 25 | 66 |
| Gene | SNP rs Number | Genotype | Group 1, No. (%) | Allele Frequency in Group 1 | Group 2, No. (%) | Allele Frequency in Group 2 | p-Value |
|---|---|---|---|---|---|---|---|
| VKORC1*1 | rs8050894 | CC | 41 (55.4) | C:G = 0.68:0.32 | 14 (58.3) | C:G = 0.71:0.29 | 1 |
| CG | 18 (24.3) | 6 (25.0) | |||||
| GG | 15 (20.3) | 4 (16.7) | |||||
| C | 100 | 34 | |||||
| G | 48 | 14 | |||||
| VKORC1*2 | rs9934438 | GG | 14 (18.9) | G:A = 0.39:0.61 | 0 | G:A = 0.35:0.65 | 0.008 * |
| GA | 29 (39.2) | 17 (70.8) | |||||
| AA | 31 (41.9) | 7 (29.2) | |||||
| G | 57 | 17 | |||||
| A | 91 | 31 | |||||
| VKORC1*3 | rs9923231 | CC | 14 (18.9) | C:T = 0.40:0.60 | 0 | C:T = 0.35:0.65 | 0.012 * |
| CT | 31 (41.9) | 17 (70.8) | |||||
| TT | 29 (39.2) | 7 (29.2) | |||||
| C | 59 | 17 | |||||
| T | 89 | 31 | |||||
| CYP2C9*2 | rs1799853 | CC | 70 (94.6) | C:T = 0.97:0.03 | 21 (87.5) | C:T = 0.94:0.06 | 0.357 |
| CT | 4 (5.4) | 3 (12.5) | |||||
| TT | 0 | 0 | |||||
| C | 144 | 45 | |||||
| T | 4 | 3 | |||||
| CYP2C9*3 | rs1057910 | AA | 68 (91.9) | A:C = 0.96:0.04 | 23 (95.8) | A:C = 0.98:0.02 | 1 |
| AC | 6 (8.1) | 1 (4.2) | |||||
| CC | 0 | 0 | |||||
| A | 142 | 47 | |||||
| C | 6 | 1 | |||||
| CYP2C9*5 | rs28371686 | CC | 74 (100) | C:G = 1.000:0.000 | 24 (100) | C:G = 1.000:0.000 | N/A |
| CG | 0 | 0 | |||||
| GG | 0 | 0 | |||||
| C | 148 | 48 | |||||
| G | 0 | 0 | |||||
| CYP2C19*2 | rs4244285 | GG | 52 (70.3) | G:A = 0.84:0.16 | 19 (79.2) | G:A = 0.90:0.10 | 0.772 |
| GA | 20 (27.0) | 5 (20.8) | |||||
| AA | 2 (2.7) | 0 | |||||
| G | 124 | 43 | |||||
| A | 24 | 5 | |||||
| CYP2C19*3 | rs4986893 | GG | 70 (94.6) | G:A = 0.97:0.03 | 23 (95.8) | G:A = 0.98:0.02 | 1 |
| GA | 4 (5.4) | 1 (4.2) | |||||
| AA | 0 | 0 | |||||
| G | 144 | 47 | |||||
| A | 4 | 1 | |||||
| ITGB3 | rs5918 | TT | 42 (56.8) | T:C = 0.70:0.30 | 6 (25.0) | T:C = 0.56:0.44 | 0.005 * |
| TC | 19 (25.7) | 15 (62.5) | |||||
| CC | 13 (17.6) | 3 (12.5) | |||||
| T | 103 | 27 | |||||
| C | 45 | 21 | |||||
| GGCX | rs11676382 | CC | 70 (94.6) | C:G = 0.97:0.03 | 24 (100) | C:G = 1.000:0.000 | 0.677 |
| CG | 3 (4.0) | 0 | |||||
| GG | 1 (1.4) | 0 | |||||
| C | 143 | 48 | |||||
| G | 5 | 0 | |||||
| CYP4F2 | rs2108622 | CC | 47 (63.5) | C:T = 0.78:0.22 | 13 (54.2) | C:T = 0.71:0.29 | 0.501 |
| CT | 22 (29.7) | 8 (33.3) | |||||
| TT | 5 (6.8) | 3 (12.5) | |||||
| C | 116 | 34 | |||||
| T | 32 | 14 | |||||
| UGT1A6 | rs2070959 | AA | 28 (37.8) | A:G = 0.66:0.34 | 12 (50.0) | A:G = 0.65: 0.35 | 0.03 * |
| AG | 41 (55.4) | 7 (29.2) | |||||
| GG | 5 (6.8) | 5 (20.8) | |||||
| A | 97 | 31 | |||||
| G | 51 | 17 | |||||
| ACSM2A | rs1133607 | CC | 44 (59.5) | C:T = 0.78:0.22 | 15 (62.5) | C:T = 0.79:0.21 | 1 |
| CT | 27 (36.5) | 8 (33.3) | |||||
| TT | 3 (4.0) | 1 (4.2) | |||||
| C | 115 | 38 | |||||
| T | 33 | 10 | |||||
| PTGS1 | rs3842787 | CC | 72 (97.3) | C:T = 0.99:0.01 | 23 (95.8) | C:T = 0.98:0.02 | 1 |
| CT | 2 (2.7) | 1 (4.2) | |||||
| TT | 0 | 0 | |||||
| C | 146 | 47 | |||||
| T | 2 | 1 | |||||
| F5 | rs6025 | CC | 73 (98.6) | C:T = 0.99:0.01 | 24 (100) | C:T = 1.000:0.000 | 1 |
| CT | 1 (1.4) | 0 | |||||
| TT | 0 | 0 | |||||
| C | 147 | 48 | |||||
| T | 1 | 0 | |||||
| F13A1 | rs5985 | CC | 53 (71.6) | C:A = 0.84:0.16 | 19 (79.2) | C:A = 0.90:0.10 | 0.879 |
| CA | 19 (25.7) | 5 (20.8) | |||||
| AA | 2 (2.7) | 0% | |||||
| C | 125 | 43 | |||||
| A | 23 | 5 | |||||
| F2 | rs1799963 | GG | 74 (100) | G:A = 1.000:0.000 | 24 (100) | G:A = 1.000:0.000 | N/A |
| GA | 0 | 0 | |||||
| AA | 0 | 0 | |||||
| G | 148 | 48 | |||||
| A | 0 | 0 | |||||
| F7 | rs6046 | GG | 57 (77.0) | G:A = 0.87:0.13 | 18 (75.0) | G:A = 0.85:0.15 | 1 |
| GA | 15 (20.3) | 5 (20.8) | |||||
| AA | 2 (2.7) | 1 (4.2) | |||||
| G | 129 | 41 | |||||
| A | 19 | 7 | |||||
| FGB | rs1800790 | GG | 49 (66.2) | G:A = 0.82:0.18 | 16 (66.7) | G:A = 0.81:0.19 | 1 |
| GA | 23 (31.1) | 7 (29.2) | |||||
| AA | 2 (2.7) | 1 (4.2) | |||||
| G | 121 | 39 | |||||
| A | 27 | 9 | |||||
| MTHFR*1 | rs1801133 | GG | 37 (50.0) | G:A = 0.70:0.30 | 10 (41.7) | G:A = 0.65:0.35 | 0.742 |
| GA | 30 (40.5) | 11 (45.8) | |||||
| AA | 7 (9.5) | 3 (12.5) | |||||
| G | 104 | 31 | |||||
| A | 44 | 17 | |||||
| MTHFR*2 | rs1801131 | TT | 43 (58.1) | T:G = 0.76:0.24 | 11 (45.8) | T:G = 0.69:0.31 | 0.589 |
| TG | 27 (36.5) | 11 (45.8) | |||||
| GG | 4 (5.4) | 2 (8.3) | |||||
| T | 113 | 33 | |||||
| G | 35 | 15 |
| Gene, SNP | Model | Genotype | Group 1, No. (%) | Group 2, No. (%) | OR (95% CI) | p-Value | AIC | BIC |
|---|---|---|---|---|---|---|---|---|
| VKORC1 rs9934438 | Codominant | A/A | 31 (41.9) | 7 (29.2) | 1.00 | 0.0015 * | 106.1 | 121.6 |
| G/A | 29 (39.2) | 17 (70.8) | 2.69 (0.95–7.63) | |||||
| G/G | 14 (18.9) | 0 (0) | 0.00 (0.00–NA) | |||||
| Dominant | A/A | 31 (41.9) | 7 (29.2) | 1.00 | 0.27 | 115.9 | 128.8 | |
| G/A-G/G | 43 (58.1) | 17 (70.8) | 1.73 (0.64–4.74) | |||||
| Recessive | A/A-G/A | 60 (81.1) | 24 (100) | 1.00 | 0.0023 | 107.8 | 120.7 | |
| G/G | 14 (18.9) | 0 (0) | 0.00 (0.00–NA) | |||||
| Overdominant | A/A-G/G | 45 (60.8) | 7 (29.2) | 1.00 | 0.0057 * | 109.4 | 122.4 | |
| G/A | 29 (39.2) | 17 (70.8) | 3.96 (1.42–11.02) | |||||
| Log-additive | --- | --- | --- | 0.85 (0.43–1.70) | 0.65 | 116.9 | 129.8 | |
| VKORC1 rs9923231 | Codominant | T/T | 29 (39.2) | 7 (29.2) | 1.00 | 0.0024 | 107 | 122.5 |
| C/T | 31 (41.9) | 17 (70.8) | 2.36 (0.83–6.70) | |||||
| C/C | 14 (18.9) | 0 (0) | 0.00 (0.00–NA) | |||||
| Dominant | T/T | 29 (39.2) | 7 (29.2) | 1.00 | 0.38 | 116.3 | 129.2 | |
| C/T-C/C | 45 (60.8) | 17 (70.8) | 1.56 (0.57–4.27) | |||||
| Recessive | T/T-C/T | 60 (81.1) | 24 (100) | 1.00 | 0.0023 | 107.8 | 120.7 | |
| C/C | 14 (18.9) | 0 (0) | 0.00 (0.00–NA) | |||||
| Overdominant | T/T-C/C | 43 (58.1) | 7 (29.2) | 1.00 | 0.011 * | 110.6 | 123.5 | |
| C/T | 31 (41.9) | 17 (70.8) | 3.55 (1.28–9.86) | |||||
| Log-additive | --- | --- | --- | 0.80 (0.40–1.62) | 0.54 | 116.7 | 129.6 | |
| ITGB3 rs5918 | Codominant | T/T | 42 (56.8) | 6 (25.0) | 1.00 | 0.0056 * | 108.7 | 124.2 |
| T/C | 19 (25.7) | 15 (62.5) | 5.37 (1.79–16.16) | |||||
| C/C | 13 (17.6) | 3 (12.5) | 1.47 (0.31–7.05) | |||||
| Dominant | T/T | 42 (56.8) | 6 (25.0) | 1.00 | 0.0079 * | 110 | 123 | |
| T/C-C/C | 32 (43.2) | 18 (75.0) | 3.83 (1.35–10.89) | |||||
| Recessive | T/T-T/C | 61 (82.4) | 21 (87.5) | 1.00 | 0.49 | 116.6 | 129.5 | |
| C/C | 13 (17.6) | 3 (12.5) | 0.62 (0.15–2.53) | |||||
| Overdominant | T/T-C/C | 55 (74.3) | 9 (37.5) | 1.00 | 0.0014 * | 106.9 | 119.9 | |
| T/C | 19 (25.7) | 15 (62.5) | 4.83 (1.79–13.06) | |||||
| Log-additive | --- | --- | --- | 1.59 (0.84–2.99) | 0.15 | 115 | 128 | |
| UGT1A6 rs2070959 | Codominant | A/A | 28 (37.8) | 12 (50) | 1.00 | 0.03 | 112.1 | 127.6 |
| A/G | 41 (55.4) | 7 (29.2) | 0.40 (0.13–1.17) | |||||
| G/G | 5 (6.8) | 5 (20.8) | 2.67 (0.59–12.07) | |||||
| Dominant | A/A | 28 (37.8) | 12 (50) | 1.00 | 0.29 | 116 | 128.9 | |
| A/G-G/G | 46 (62.2) | 12 (50) | 0.60 (0.23–1.56) | |||||
| Recessive | A/A-A/G | 69 (93.2) | 19 (79.2) | 1.00 | 0.044 * | 113 | 125.9 | |
| G/G | 5 (6.8) | 5 (20.8) | 4.40 (1.06–18.20) | |||||
| Overdominant | A/A-G/G | 33 (44.6) | 17 (70.8) | 1.00 | 0.02 * | 111.7 | 124.6 | |
| A/G | 41 (55.4) | 7 (29.2) | 0.32 (0.11–0.87) | |||||
| Log-additive | --- | --- | --- | 1.08 (0.51–2.29) | 0.84 | 117 | 130 |
| Level | Best Models | SNP rs Number | Training Accuracy | Classification Accuracy | Prediction Accuracy |
|---|---|---|---|---|---|
| 1 | MTHFR*1 | rs1801133 | 69.70 | 68.23 | 50.00 |
| 2 | VKORC1*2, MTHFR*2 | rs9934438, rs1801131 | 73.79 | 76.04 | 54.17 |
| *3 | VKORC1*2, UGT1A6, MTHFR*1 | rs9934438, rs2070959, rs1801133 | 88.33 | 82.29 | 95.83 |
| Level | Best Models | SNP rs Number | Training Accuracy | Classification Accuracy | Prediction Accuracy |
|---|---|---|---|---|---|
| 1 | ITGB3 | rs5918 | 66.82 | 83.18 | 83.18 |
| 2 | VKORC1*2 ITGB3 | rs9934438 rs5918 | 74.24 | 86.41 | 86.41 |
| 3 | ITGB3 MTHFR*1 FGB | rs5918 rs1801133 rs1800790 | 83.79 | 95.16 | 95.16 |
| *4 | ITGB3 CYP4F2 MTHFR*1 FGB | rs5918 rs2108622 rs1801133 rs1800790 | 92.12 | 96.77 | 96.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhalbinova, M.R.; Rakhimova, S.E.; Kozhamkulov, U.A.; Akilzhanova, G.A.; Kaussova, G.K.; Akilzhanov, K.R.; Pya, Y.V.; Lee, J.H.; Bekbossynova, M.S.; Akilzhanova, A.R. Association of Genetic Polymorphisms with Complications of Implanted LVAD Devices in Patients with Congestive Heart Failure: A Kazakhstani Study. J. Pers. Med. 2022, 12, 744. https://doi.org/10.3390/jpm12050744
Zhalbinova MR, Rakhimova SE, Kozhamkulov UA, Akilzhanova GA, Kaussova GK, Akilzhanov KR, Pya YV, Lee JH, Bekbossynova MS, Akilzhanova AR. Association of Genetic Polymorphisms with Complications of Implanted LVAD Devices in Patients with Congestive Heart Failure: A Kazakhstani Study. Journal of Personalized Medicine. 2022; 12(5):744. https://doi.org/10.3390/jpm12050744
Chicago/Turabian StyleZhalbinova, Madina R., Saule E. Rakhimova, Ulan A. Kozhamkulov, Gulbanu A. Akilzhanova, Galina K. Kaussova, Kenes R. Akilzhanov, Yuriy V. Pya, Joseph H. Lee, Makhabbat S. Bekbossynova, and Ainur R. Akilzhanova. 2022. "Association of Genetic Polymorphisms with Complications of Implanted LVAD Devices in Patients with Congestive Heart Failure: A Kazakhstani Study" Journal of Personalized Medicine 12, no. 5: 744. https://doi.org/10.3390/jpm12050744







