Management of Displaced Midshaft Clavicle Fractures with Figure-of-Eight Bandage: The Impact of Residual Shortening on Shoulder Function
Abstract
:1. Introduction
2. Materials and Methods
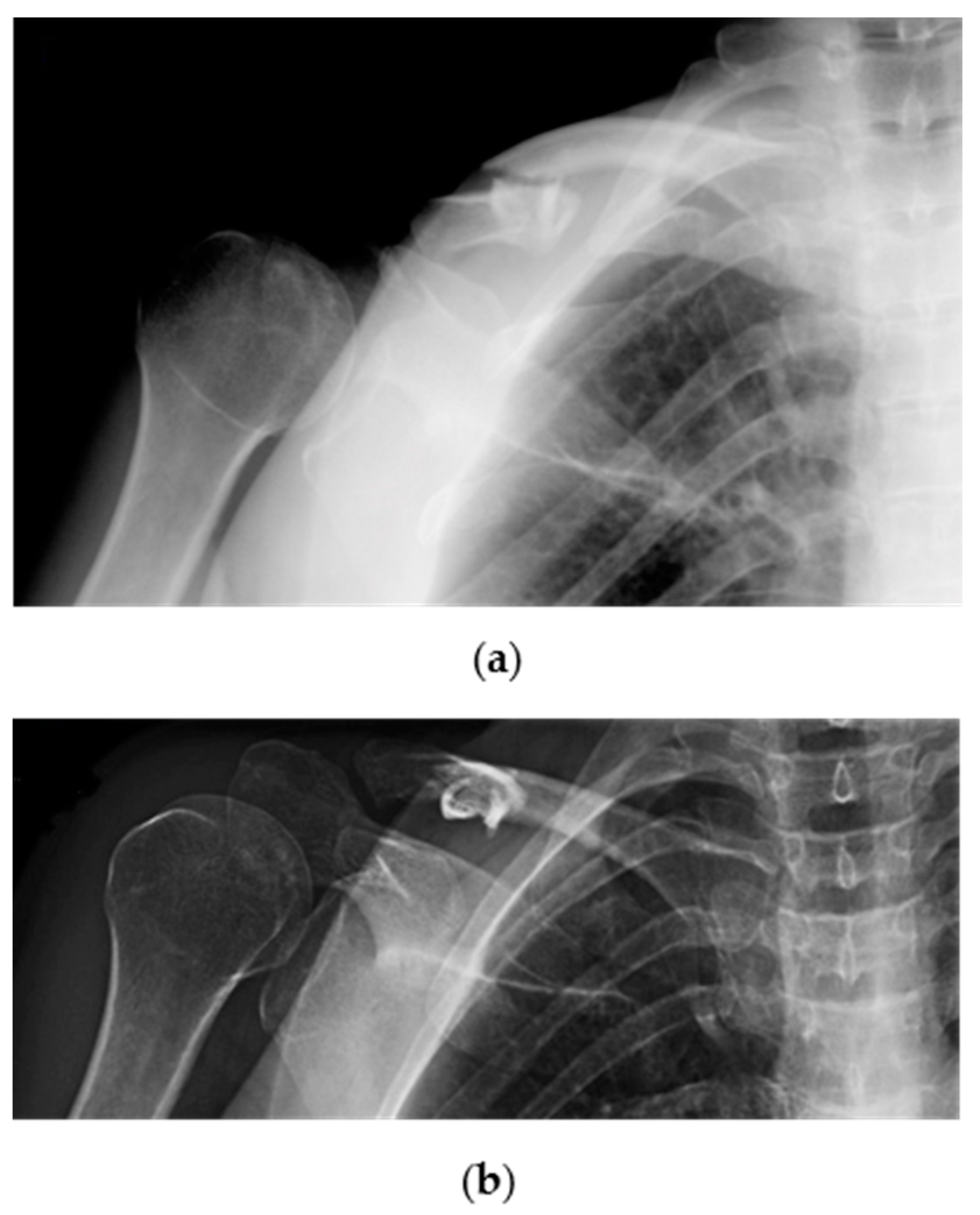
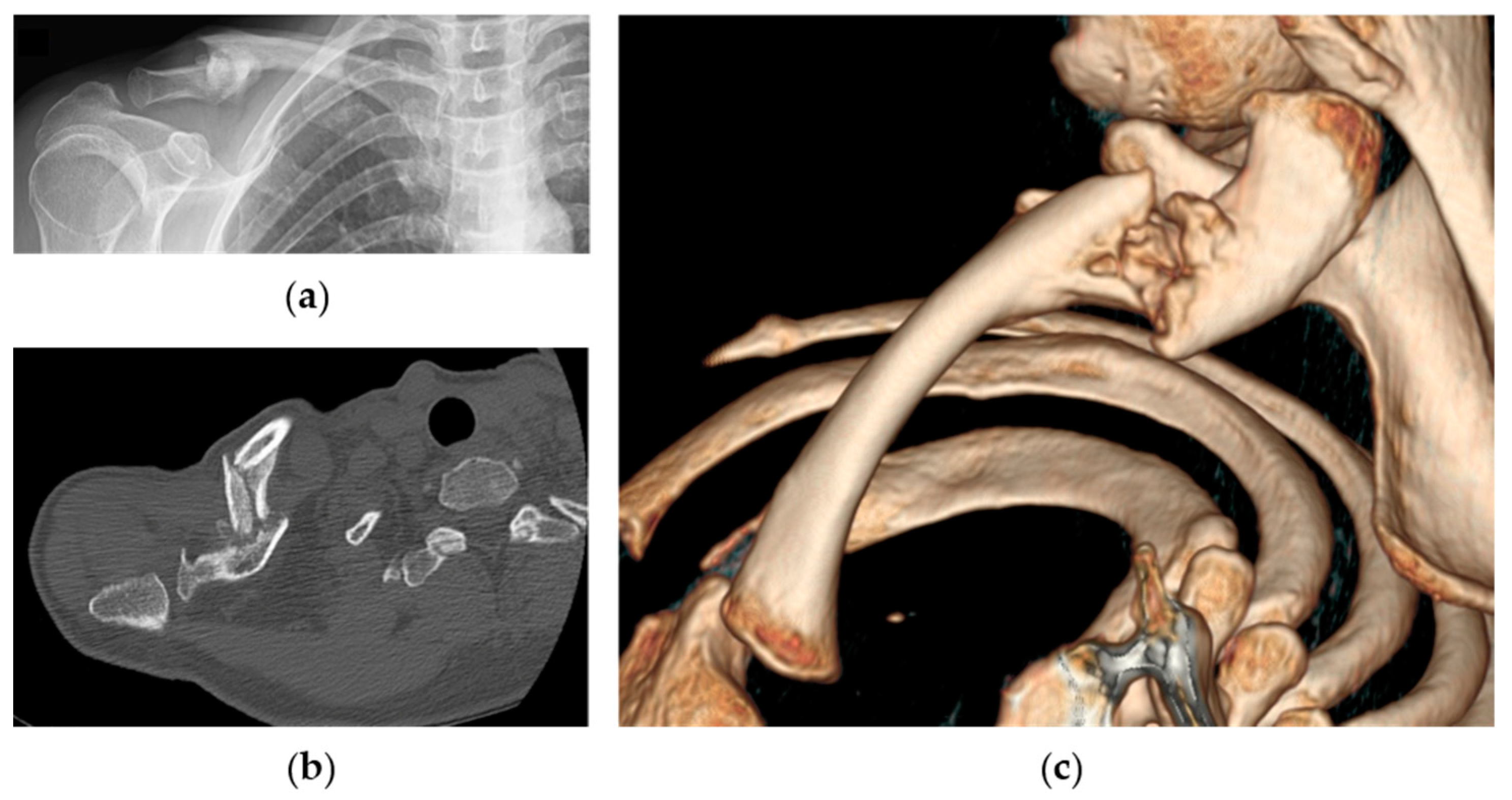
2.1. Patient Selection
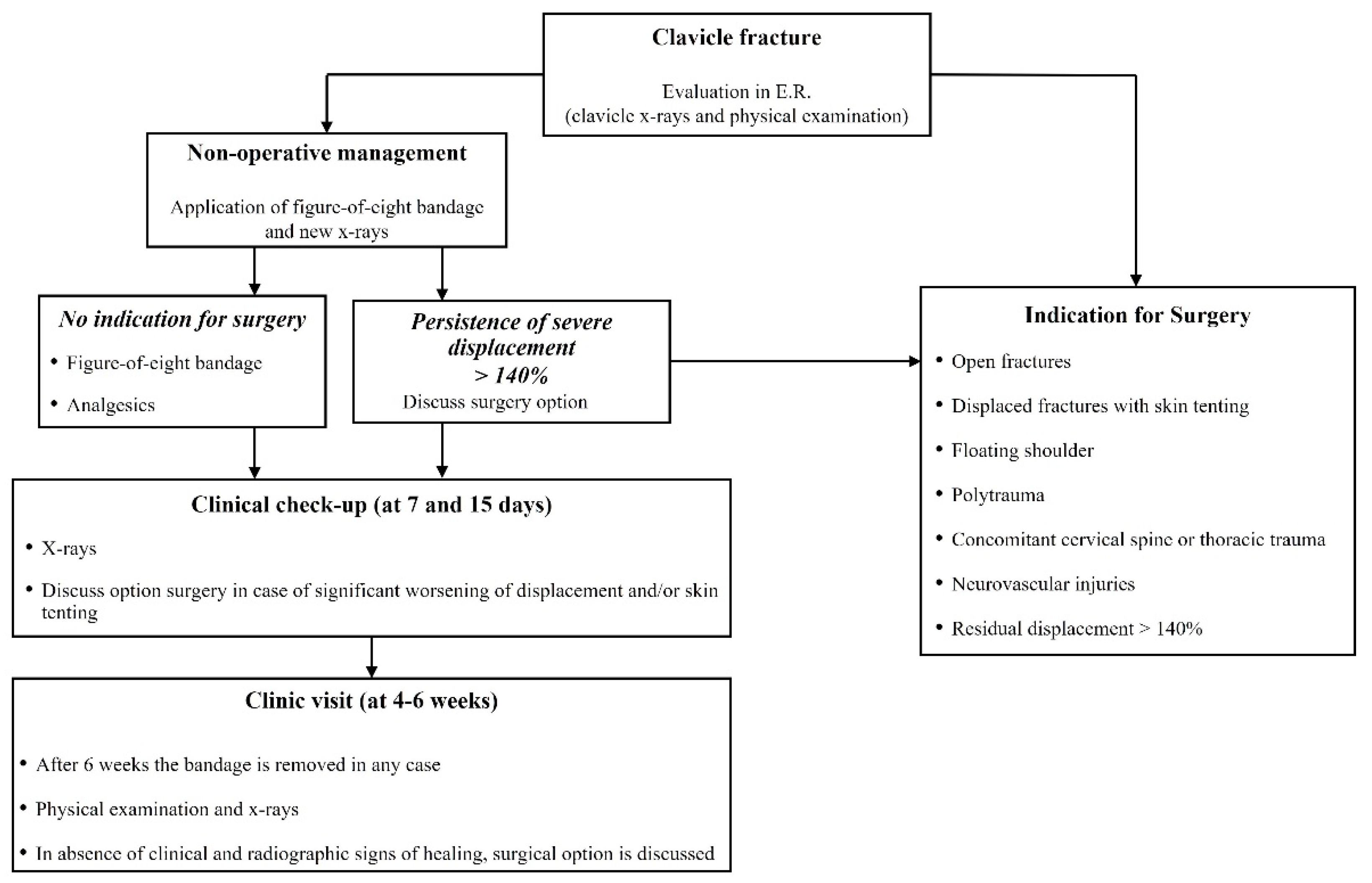
2.2. Treatment Protocol
2.3. Patient Assessment
2.4. Nonoperative Rehabilitation Protocol
2.5. Statistical Analysis
3. Results
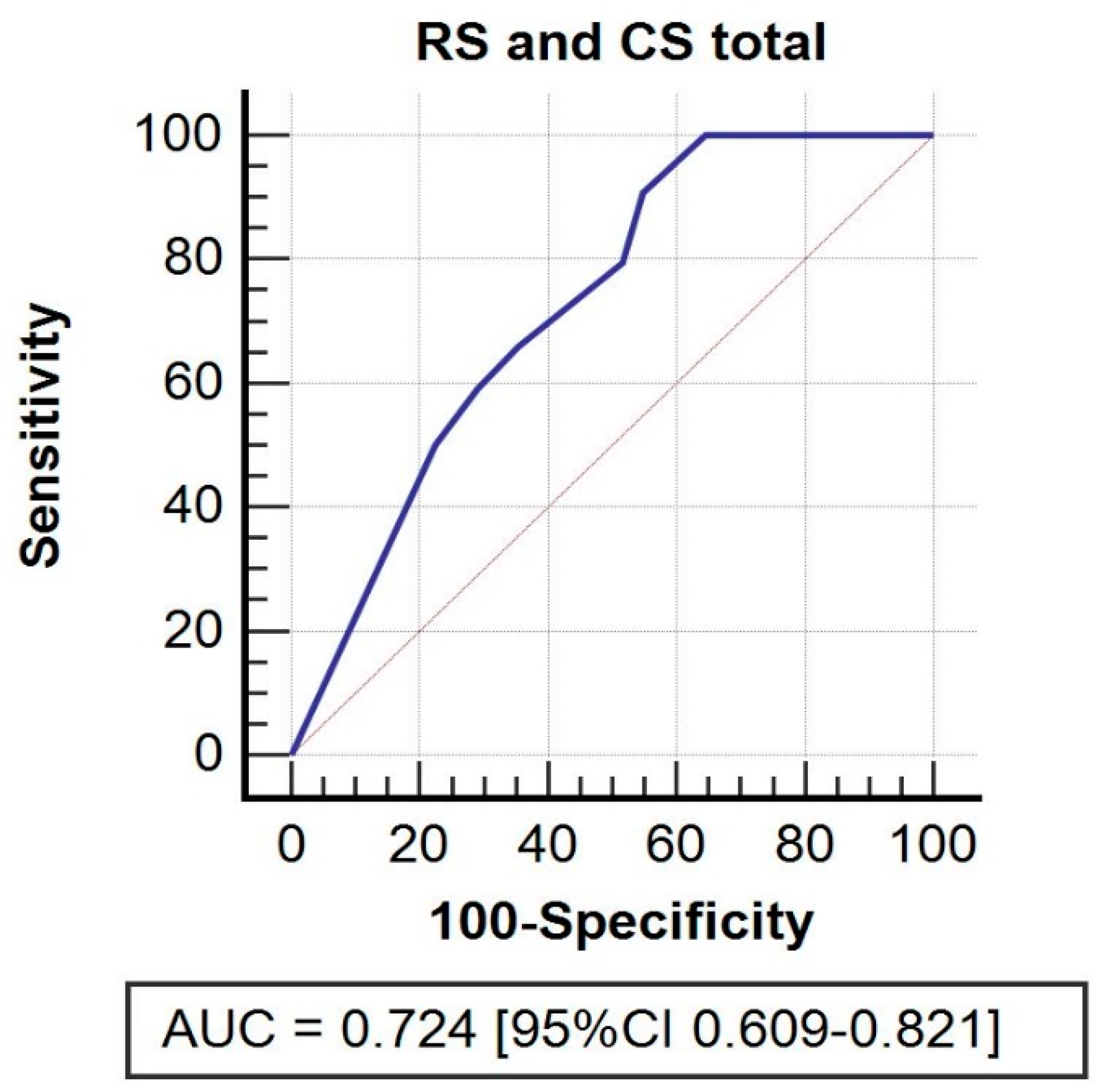
Potential Predictive Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Postacchini, F.; Gumina, S.; De Santis, P.; Albo, F. Epidemiology of clavicle fractures. J. Shoulder Elb. Surg. 2002, 11, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C.M. Fractures of the clavicle in the adult. Epidemiology and classification. J. Bone Joint Surg. Br. 1998, 80, 476–484. [Google Scholar] [CrossRef] [PubMed]
- Coppa, V.; Dei Giudici, L.; Cecconi, S.; Marinelli, M.; Gigante, A. Midshaft clavicle fractures treatment: Threaded Kirschner wire versus conservative approach. Strateg. Trauma Limb Reconstr. 2017, 12, 141–150. [Google Scholar]
- Faldini, C.; Nanni, M.; Leonetti, D.; Acri, F.; Galante, C.; Luciani, D.; Giannini, S. Nonoperative treatment of closed displaced midshaft clavicle fractures. J. Orthop. Traumatol. 2010, 11, 229–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeFroda, S.F.; Lemme, N.; Kleiner, J.; Gil, J.; Owens, B.D. Incidence and mechanism of injury of clavicle fractures in the NEISS database: Athletic and non athletic injuries. J. Clin. Orthop. Trauma 2019, 10, 954–958. [Google Scholar] [CrossRef]
- Guerra, E.; Previtali, D.; Tamborini, S.; Filardo, G.; Zaffagnini, S.; Candrian, C. Midshaft Clavicle Fractures: Surgery Provides Better Results as Compared With Nonoperative Treatment: A Meta-analysis. Am. J. Sports Med. 2019, 47, 3541–3551. [Google Scholar] [CrossRef]
- Van der Meijden, O.A.; Gaskill, T.R.; Millett, P.J. Treatment of clavicle fractures: Current concepts review. J. Shoulder Elb. Surg. 2012, 21, 423–429. [Google Scholar] [CrossRef]
- Lenza, M.; Belloti, J.C.; Andriolo, R.B.; Gomes Dos Santos, J.B.; Faloppa, F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst. Rev. 2009, 12, CD007121. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Xu, L.; Xu, W.; Gu, Y. Operative versus nonoperative treatment in the management of midshaft clavicular fractures: A meta-analysis of randomized controlled trials. J. Shoulder Elb. Surg. 2014, 23, 173–181. [Google Scholar] [CrossRef]
- McKnight, B.; Heckmann, N.; Hill, J.R.; Pannell, W.C.; Mostofi, A.; Omid, R.; Hatch, G.F., 3rd. Surgical management of midshaft clavicle nonunions is associated with a higher rate of short-term complications compared with acute fractures. J. Shoulder Elb. Surg. 2016, 25, 1412–1417. [Google Scholar] [CrossRef]
- Martetschläger, F.; Gaskill, T.R.; Millett, P.J. Management of clavicle nonunion and malunion. J. Shoulder Elb. Surg. 2013, 22, 862–868. [Google Scholar] [CrossRef] [PubMed]
- McKee, R.C.; Whelan, D.B.; Schemitsch, E.H.; McKee, M.D. Operative versus nonoperative care of displaced midshaft clavicular fractures: A meta-analysis of randomized clinical trials. J. Bone Joint Surg. Am. 2012, 94, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C.M.; Goudie, E.B.; Murray, I.R.; Jenkins, P.J.; Ahktar, M.A.; Read, E.O.; Foster, C.J.; Clark, K.; Brooksbank, A.J.; Arthur, A.; et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: A multicenter, randomized, controlled trial. J. Bone Joint Surg. Am. 2013, 95, 1576–1584. [Google Scholar] [CrossRef] [PubMed]
- Woltz, S.; Stegeman, S.A.; Krijnen, P.; van Dijkman, B.A.; van Thiel, T.P.; Schep, N.W.; de Rijcke, P.A.; Frölke, J.P.; Schipper, I.B. Plate Fixation Compared with Nonoperative Treatment for Displaced Midshaft Clavicular Fractures: A Multicenter Randomized Controlled Trial. J. Bone Joint Surg. Am. 2017, 99, 106–112. [Google Scholar] [CrossRef]
- Wolf, S.; Chitnis, A.S.; Manoranjith, A.; Vanderkarr, M.; Plaza, J.Q.; Gador, L.V.; Holy, C.E.; Sparks, C.; Lambert, S.M. Surgical treatment, complications, reoperations, and healthcare costs among patients with clavicle fracture in England. BMC Musculoskelet. Disord. 2022, 23, 135. [Google Scholar] [CrossRef]
- Biz, C.; Tagliapietra, J.; Angelini, A.; Belluzzi, E.; Pozzuoli, A.; Berizzi, A.; Ruggieri, P. The challenging management of a delayed union midshaft clavicle fracture complicated by an acute pseudoaneurysm of the subclavian artery in a superelderly diabetic patient. Aging Clin. Exp. Res. 2019, 31, 567–569. [Google Scholar] [CrossRef]
- Ahmed, A.F.; Salameh, M.; AlKhatib, N.; Elmhiregh, A.; Ahmed, G.O. Open Reduction and Internal Fixation Versus Nonsurgical Treatment in Displaced Midshaft Clavicle Fractures: A Meta-Analysis. J. Orthop. Trauma 2018, 32, e276–e283. [Google Scholar] [CrossRef]
- Subramanyam, K.N.; Mundargi, A.V.; Gopakumar, K.U.; Bharath, T.; Prabhu, M.V.; Khanchandani, P. Displaced midshaft clavicle fractures in adults—Is non-operative management enough? Injury 2021, 52, 493–500. [Google Scholar] [CrossRef]
- Amer, K.; Smith, B.; Thomson, J.E.; Congiusta, D.; Reilly, M.C.; Sirkin, M.S.; Adams, M.R. Operative Versus Nonoperative Outcomes of Middle-Third Clavicle Fractures: A Systematic Review and Meta-Analysis. J. Orthop. Trauma 2020, 34, e6–e13. [Google Scholar] [CrossRef]
- Axelrod, D.E.; Ekhtiari, S.; Bozzo, A.; Bhandari, M.; Johal, H. What Is the Best Evidence for Management of Displaced Midshaft Clavicle Fractures? A Systematic Review and Network Meta-analysis of 22 Randomized Controlled Trials. Clin. Orthop. Relat. Res. 2020, 478, 392–402. [Google Scholar] [CrossRef]
- Schneider, P.; Bransford, R.; Harvey, E.; Agel, J. Operative treatment of displaced midshaft clavicle fractures: Has randomised control trial evidence changed practice patterns? BMJ Open 2019, 9, e031118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kluijfhout, W.P.; Tutuhatunewa, E.D.; van Olden, G.D.J. Plate fixation of clavicle fractures: Comparison between early and delayed surgery. J. Shoulder Elb. Surg. 2020, 29, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Potter, J.M.; Jones, C.; Wild, L.M.; Schemitsch, E.H.; McKee, M.D. Does delay matter? The restoration of objectively measured shoulder strength and patient-oriented outcome after immediate fixation versus delayed reconstruction of displaced midshaft fractures of the clavicle. J. Shoulder Elb. Surg. 2007, 16, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Sawalha, S.; Guisasola, I. Complications associated with plate fixation of acute midshaft clavicle fractures versus non-unions. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, K.J.; Remes, V.; Pajarinen, J.; Savolainen, V.; Björkenheim, J.M.; Paavola, M. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: A randomized clinical trial. J. Bone Joint Surg. Am. 2012, 94, 1546–1553. [Google Scholar] [CrossRef] [Green Version]
- Tamaoki, M.J.S.; Matsunaga, F.T.; Costa, A.; Netto, N.A.; Matsumoto, M.H.; Belloti, J.C. Treatment of Displaced Midshaft Clavicle Fractures: Figure-of-Eight Harness Versus Anterior Plate Osteosynthesis: A Randomized Controlled Trial. J. Bone Joint Surg. Am. 2017, 99, 1159–1165. [Google Scholar] [CrossRef]
- Van der Ven Denise, J.C.; Timmers, T.K.; Flikweert, P.E.; Van Ijseldijk, A.L.; van Olden, G.D. Plate fixation versus conservative treatment of displaced midshaft clavicle fractures: Functional outcome and patients’ satisfaction during a mean follow-up of 5 years. Injury 2015, 46, 2223–2229. [Google Scholar] [CrossRef]
- Jørgensen, A.; Troelsen, A.; Ban, I. Predictors associated with nonunion and symptomatic malunion following non-operative treatment of displaced midshaft clavicle fractures—A systematic review of the literature. Int. Orthop. 2014, 38, 2543–2549. [Google Scholar] [CrossRef]
- Tagliapietra, J.; Belluzzi, E.; Biz, C.; Angelini, A.; Fantoni, I.; Scioni, M.; Bolzan, M.; Berizzi, A.; Ruggieri, P. Midshaft Clavicle Fractures Treated Nonoperatively Using Figure-of-Eight Bandage: Are Fracture Type, Shortening, and Displacement Radiographic Predictors of Failure? Diagnostics 2020, 10, 788. [Google Scholar] [CrossRef]
- Padulo, J.; Oliva, F.; Frizziero, A.; Maffulli, N. Basic principles and recommendations in clinical and field science research: 2018 update. Muscles Ligaments Tendons J. 2018, 8, 305–307. [Google Scholar] [CrossRef] [Green Version]
- Delaune, L.A.; Wehrli, L.; Maeder, Y.; Vauclair, F.; Moerenhout, K. Acute brachial plexus deficit due to clavicle fractures. JSES Int. 2021, 5, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Della Santa, D.; Narakas, A.; Bonnard, C. Late lesions of the brachial plexus after fracture of the clavicle. Ann. Chir. Main Memb. Super. 1991, 10, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Feriani, N.; Ben Ghezala, H.; Snouda, S. Pneumothorax Caused by an Isolated Midshaft Clavicle Fracture. Case Rep. Emerg Med. 2016, 2016, 2409894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amer, K.M.; Congiusta, D.V.; Suri, P.; Choudhry, A.; Otero, K.; Adams, M. Clavicle fractures: Associated trauma and morbidity. J. Clin. Orthop. Trauma 2021, 13, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Hani, R.; Ennaciri, B.; Jeddi, I.; El Bardouni, A.; Mahfoud, M.; Berrada, M.S. Pneumothorax complicating isolated clavicle fracture. Pan Afr. Med. J. 2015, 21, 202. [Google Scholar] [CrossRef]
- Mouzopoulos, G.; Stamatakos, M.; Arabatzi, H.; Tzurbakis, M. Complications of clavicle fracture and acromioclavicular joint rupture. What the general surgeon should know. Chirurgia 2008, 103, 509–512. [Google Scholar]
- Fletcher, C.; Fletcher, K.L. A delayed and recurrent pneumothorax complicating a fractured clavicle—A novel presentation. Trauma Case Rep. 2020, 26, 100294. [Google Scholar] [CrossRef]
- Gandham, S.; Nagar, A. Delayed pneumothorax following an isolated clavicle injury. BMJ Case Rep. 2013, 2013, bcr1120115168. [Google Scholar] [CrossRef] [Green Version]
- Society, C.O.T. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J. Bone Joint Surg. Am. 2007, 89, 1–10. [Google Scholar]
- Ateş, C.; Kaymaz, Ö.; Kale, H.E.; Tekindal, M.A. Comparison of Test Statistics of Nonnormal and Unbalanced Samples for Multivariate Analysis of Variance in terms of Type-I Error Rates. Comput. Math. Methods Med. 2019, 2019, 2173638. [Google Scholar] [CrossRef]
- Wu, C.L.; Chang, H.C.; Lu, K.H. Risk factors for nonunion in 337 displaced midshaft clavicular fractures treated with Knowles pin fixation. Arch. Orthop. Trauma Surg. 2013, 133, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Xiao, J.; Ji, F.; Xie, Y.; Hao, Y. Intrinsic and extrinsic risk factors for nonunion after nonoperative treatment of midshaft clavicle fractures. Orthop. Traumatol. Surg. Res. 2015, 101, 197–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clement, N.D.; Goudie, E.B.; Brooksbank, A.J.; Chesser, T.J.; Robinson, C.M. Smoking status and the Disabilities of the Arm Shoulder and Hand score are early predictors of symptomatic nonunion of displaced midshaft fractures of the clavicle. Bone Joint J. 2016, 98-B, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, P.; Kühle, L.; Stöckle, U.; Wintermeyer, E.; Stollhof, L.E.; Ihle, C.; Bahrs, C. Evaluation of the Constant score: Which is the method to assess the objective strength? BMC Musculoskelet. Disord. 2019, 20, 403. [Google Scholar] [CrossRef] [Green Version]
- Robertson, G.A.; Wood, A.M. Return to sport following clavicle fractures: A systematic review. Br. Med. Bull. 2016, 119, 111–128. [Google Scholar] [CrossRef]
- Woltz, S.; Krijnen, P.; Schipper, I.B. Mid-Term Patient Satisfaction and Residual Symptoms After Plate Fixation or Nonoperative Treatment for Displaced Midshaft Clavicular Fractures. J. Orthop. Trauma 2018, 32, e435–e439. [Google Scholar] [CrossRef]
- Tutuhatunewa, E.D.; Stevens, M.; Diercks, R.L. Clinical outcomes and predictors of patient satisfaction in displaced midshaft clavicle fractures in adults: Results from a retrospective multicentre study. Injury 2017, 48, 2788–2792. [Google Scholar] [CrossRef]
- Postacchini, R.; Gumina, S.; Farsetti, P.; Postacchini, F. Long-term results of conservative management of midshaft clavicle fracture. Int. Orthop. 2010, 34, 731–736. [Google Scholar] [CrossRef] [Green Version]
- Malik, S.S.; Tahir, M.; Jordan, R.W.; Malik, S.S.; Saithna, A. Is shortening of displaced midshaft clavicle fractures associated with inferior clinical outcomes following nonoperative management? A systematic review. J. Shoulder Elb. Surg. 2019, 28, 1626–1638. [Google Scholar] [CrossRef] [Green Version]
- Moverley, R.; Little, N.; Gulihar, A.; Singh, B. Current concepts in the management of clavicle fractures. J. Clin. Orthop. Trauma 2020, 11, S25–S30. [Google Scholar] [CrossRef]
- Figueiredo, G.S.; Tamaoki, M.J.; Dragone, B.; Utino, A.Y.; Netto, N.A.; Matsumoto, M.H.; Matsunaga, F.T. Correlation of the degree of clavicle shortening after non-surgical treatment of midshaft fractures with upper limb function. BMC Musculoskelet. Disord. 2015, 16, 151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasmussen, J.V.; Jensen, S.L.; Petersen, J.B.; Falstie-Jensen, T.; Lausten, G.; Olsen, B.S. A retrospective study of the association between shortening of the clavicle after fracture and the clinical outcome in 136 patients. Injury 2011, 42, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Fuglesang, H.F.; Flugsrud, G.B.; Randsborg, P.H.; Stavem, K.; Utvåg, S.E. Radiological and functional outcomes 2.7 years following conservatively treated completely displaced midshaft clavicle fractures. Arch. Orthop. Trauma Surg. 2016, 136, 17–25. [Google Scholar] [CrossRef]
- Jones, G.L.; Bishop, J.Y.; Lewis, B.; Pedroza, A.D. Intraobserver and interobserver agreement in the classification and treatment of midshaft clavicle fractures. Am. J. Sports Med. 2014, 42, 1176–1181. [Google Scholar] [CrossRef] [PubMed]
- Goudie, E.B.; Clement, N.D.; Murray, I.R.; Lawrence, C.R.; Wilson, M.; Brooksbank, A.J.; Robinson, C.M. The Influence of Shortening on Clinical Outcome in Healed Displaced Midshaft Clavicular Fractures After Nonoperative Treatment. J. Bone Joint Surg. Am. 2017, 99, 1166–1172. [Google Scholar] [CrossRef] [PubMed]
- Bajuri, M.Y.; Maidin, S.; Rauf, A.; Baharuddin, M.; Harjeet, S. Functional outcomes of conservatively treated clavicle fractures. Clinics 2011, 66, 635–639. [Google Scholar] [CrossRef] [Green Version]
- Woltz, S.; Sengab, A.; Krijnen, P.; Schipper, I.B. Does clavicular shortening after nonoperative treatment of midshaft fractures affect shoulder function? A systematic review. Arch. Orthop. Trauma Surg. 2017, 137, 1047–1053. [Google Scholar] [CrossRef] [Green Version]
| Variable | Patients Enrolled n = 75 |
|---|---|
| Age, mean (SD) | 42.8 (13.7) |
| Gender, number (%) | |
| male | 62 (82.7) |
| female | 13 (17.3) |
| BMI, mean (SD) | 24.1 (2.3) |
| Smoking status, number (%) | |
| active | 33 (44.0) |
| inactive | 42 (56.0) |
| Hypercholesterolemia, number (%) | |
| LDL ≥ 240 mg/dL | 7 (9.3) |
| LDL < 240 md/dL | 68 (90.7) |
| Hypertension, number (%) | |
| Systolic ≥ 130, Diastolic ≥ 80 | 17 (22.7) |
| Systolic < 130, Diastolic < 80 | 58 (77.3) |
| Type of trauma, number (%) | |
| Bike Fall | 29 (38.7) |
| Motorcycle trauma | 21 (28.0) |
| Sport injury | 16 (21.3) |
| Simple fall | 9 (12.0) |
| Dominant side involved, | |
| number (%) | 31 (41.3) |
| Variable | Patients Enrolled n = 75 |
|---|---|
| Type of fracture, number (%) | |
| A1 | 5 (6.7) |
| A2 | 20 (26.7) |
| A3 | 6 (8.0) |
| B1 | 3 (4.0) |
| B2 | 13 (17.3) |
| B3 | 28 (37.3) |
| Initial shortening (%), mean (SD) | 5.4 (4.6) |
| Residual shortening (%), mean (SD) | 3.4 (3.6) |
| Initial displacement (%), mean (SD) | 113 (43.4) |
| Residual displacement (%), mean (SD) | 91.8 (30.8) |
| Outcomes | Patients Enrolled n = 75 |
|---|---|
| Constant score, mean (SD) | |
| Total | 96.8 (5.6) |
| Pain subscale | 14.6 (1.2) |
| Activity Daily Living subscale | 19.6 (1.2) |
| Range of movement subscale | 39.3 (1.5) |
| Strength subscale | 23.3 (3.1) |
| qDASH score, mean (SD) | |
| Total | 4.2 (6.3) |
| Work | 3.5 (9.1) |
| Sport | 5.2 (11.8) |
| Return to work (months), mean (SD) | 2.5 (1.1) |
| Return to sport (months), mean (SD) | 4.1 (1.8) |
| VAS satisfaction, mean (SD) | 7.6 (1.0) |
| Cosmetic problem, number (%) | 30 (40) |
| Shortening ratio (%), mean (SD) | 3.5 (3.5) |
| Dependent Variable | Parameter | B | Std. Error | t | p-Value | 95% Confidence Interval | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | Partial Eta Squared | Noncent. Parameter | Observed Power | ||||||
| CS total | Intercept | 99.129 | 7.412 | 13.374 | <.001 | 84.241 | 114.017 | 0.782 | 13.374 | 1.000 |
| ID | −0.020 | 0.017 | −1.180 | 0.244 | −0.054 | 0.014 | 0.027 | 1.180 | 0.212 | |
| RD | 0.016 | 0.025 | 0.637 | 0.527 | −0.034 | 0.066 | 0.008 | 0.637 | 0.096 | |
| IS | 0.510 | 0.265 | 1.922 | 0.060 | −0.023 | 1.042 | 0.069 | 1.922 | 0.470 | |
| RS | −1.554 | 0.335 | −4.637 | <0.001 | −2.228 | −0.881 | 0.301 | 4.637 | 0.995 | |
| Shortening ratio | −0.069 | 0.047 | −1.461 | 0.150 | −0.164 | 0.026 | 0.041 | 1.461 | 0.300 | |
| Pain | Intercept | 10.282 | 2.068 | 4.972 | <0.001 | 6.128 | 14.435 | 0.331 | 4.972 | 0.998 |
| ID | 0.001 | 0.005 | 0.276 | 0.784 | −0.008 | 0.011 | 0.002 | 0.276 | 0.058 | |
| RD | 0.008 | 0.007 | 1.079 | 0.286 | −0.006 | 0.022 | 0.023 | 1.079 | 0.185 | |
| IS | 0.024 | 0.074 | 0.318 | 0.751 | −0.125 | 0.172 | 0.002 | 0.318 | 0.061 | |
| RS | −0.209 | 0.094 | −2.235 | 0.030 | −0.397 | −0.021 | 0.091 | 2.235 | 0.592 | |
| Shortening ratio | −0.004 | 0.013 | −0.328 | 0.745 | −0.031 | 0.022 | 0.002 | 0.328 | 0.062 | |
| ADL | Intercept | 17.816 | 2.081 | 8.559 | <0.001 | 13.635 | 21.997 | 0.594 | 8.559 | 1.000 |
| ID | −0.001 | 0.005 | −0.315 | 0.754 | −0.011 | 0.008 | 0.002 | 0.315 | 0.061 | |
| RD | 0.005 | 0.007 | 0.665 | 0.509 | −0.009 | 0.019 | 0.009 | 0.665 | 0.100 | |
| IS | 0.048 | 0.074 | 0.647 | 0.521 | −0.101 | 0.198 | 0.008 | 0.647 | 0.097 | |
| RS | −0.193 | 0.094 | −2.054 | 0.045 | −0.382 | −0.004 | 0.078 | 2.054 | 0.522 | |
| Shortening ratio | −.032 | 0.013 | −2.375 | 0.021 | −0.058 | −0.005 | 0.101 | 2.375 | 0.644 | |
| ROM | Intercept | 45.954 | 2.442 | 18.816 | <0.001 | 41.049 | 50.860 | 0.876 | 18.816 | 1.000 |
| ID | −0.006 | 0.006 | −1.079 | 0.286 | −0.017 | 0.005 | 0.023 | 1.079 | 0.185 | |
| RD | −0.001 | 0.008 | −.146 | 0.885 | −0.018 | 0.015 | 0.000 | 0.146 | 0.052 | |
| IS | 0.095 | 0.087 | 1.090 | 0.281 | −0.080 | 0.271 | 0.023 | 1.090 | 0.188 | |
| RS | −0.272 | 0.110 | −2.466 | 0.017 | −0.494 | −0.051 | 0.108 | 2.466 | 0.677 | |
| Shortening ratio | −0.030 | 0.016 | −1.905 | 0.063 | −0.061 | 0.002 | 0.068 | 1.905 | 0.464 | |
| Strength | Intercept | 25.679 | 4.299 | 5.974 | <0.001 | 17.045 | 34.313 | 0.416 | 5.974 | 1.000 |
| ID | −0.015 | 0.010 | −1.551 | 0.127 | −0.035 | 0.004 | 0.046 | 1.551 | 0.331 | |
| RD | 0.006 | 0.015 | 0.397 | 0.693 | −0.023 | 0.035 | 0.003 | 0.397 | 0.068 | |
| IS | 0.340 | 0.154 | 2.209 | 0.032 | 0.031 | 0.648 | 0.089 | 2.209 | 0.582 | |
| RS | −0.799 | 0.194 | −4.110 | <0.001 | −1.190 | −0.409 | 0.253 | 4.110 | 0.981 | |
| Shortening ratio | −.030 | 0.027 | −1.082 | 0.284 | −0.085 | 0.025 | 0.023 | 1.082 | 0.186 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biz, C.; Scucchiari, D.; Pozzuoli, A.; Belluzzi, E.; Bragazzi, N.L.; Berizzi, A.; Ruggieri, P. Management of Displaced Midshaft Clavicle Fractures with Figure-of-Eight Bandage: The Impact of Residual Shortening on Shoulder Function. J. Pers. Med. 2022, 12, 759. https://doi.org/10.3390/jpm12050759
Biz C, Scucchiari D, Pozzuoli A, Belluzzi E, Bragazzi NL, Berizzi A, Ruggieri P. Management of Displaced Midshaft Clavicle Fractures with Figure-of-Eight Bandage: The Impact of Residual Shortening on Shoulder Function. Journal of Personalized Medicine. 2022; 12(5):759. https://doi.org/10.3390/jpm12050759
Chicago/Turabian StyleBiz, Carlo, Davide Scucchiari, Assunta Pozzuoli, Elisa Belluzzi, Nicola Luigi Bragazzi, Antonio Berizzi, and Pietro Ruggieri. 2022. "Management of Displaced Midshaft Clavicle Fractures with Figure-of-Eight Bandage: The Impact of Residual Shortening on Shoulder Function" Journal of Personalized Medicine 12, no. 5: 759. https://doi.org/10.3390/jpm12050759
APA StyleBiz, C., Scucchiari, D., Pozzuoli, A., Belluzzi, E., Bragazzi, N. L., Berizzi, A., & Ruggieri, P. (2022). Management of Displaced Midshaft Clavicle Fractures with Figure-of-Eight Bandage: The Impact of Residual Shortening on Shoulder Function. Journal of Personalized Medicine, 12(5), 759. https://doi.org/10.3390/jpm12050759










