Evaluation of a Diagnostic and Management Algorithm for Adult Caustic Ingestion: New Concept of Severity Stratification and Patient Categorization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Algorithm Establishment and Study Population
2.2. Patient Categorization
2.3. EGD Survey
2.4. CT Survey
2.5. Post-Caustic Ingestion Patient Care
2.6. Complications
2.7. Statistical Analyses
3. Results
3.1. Patient Characteristics
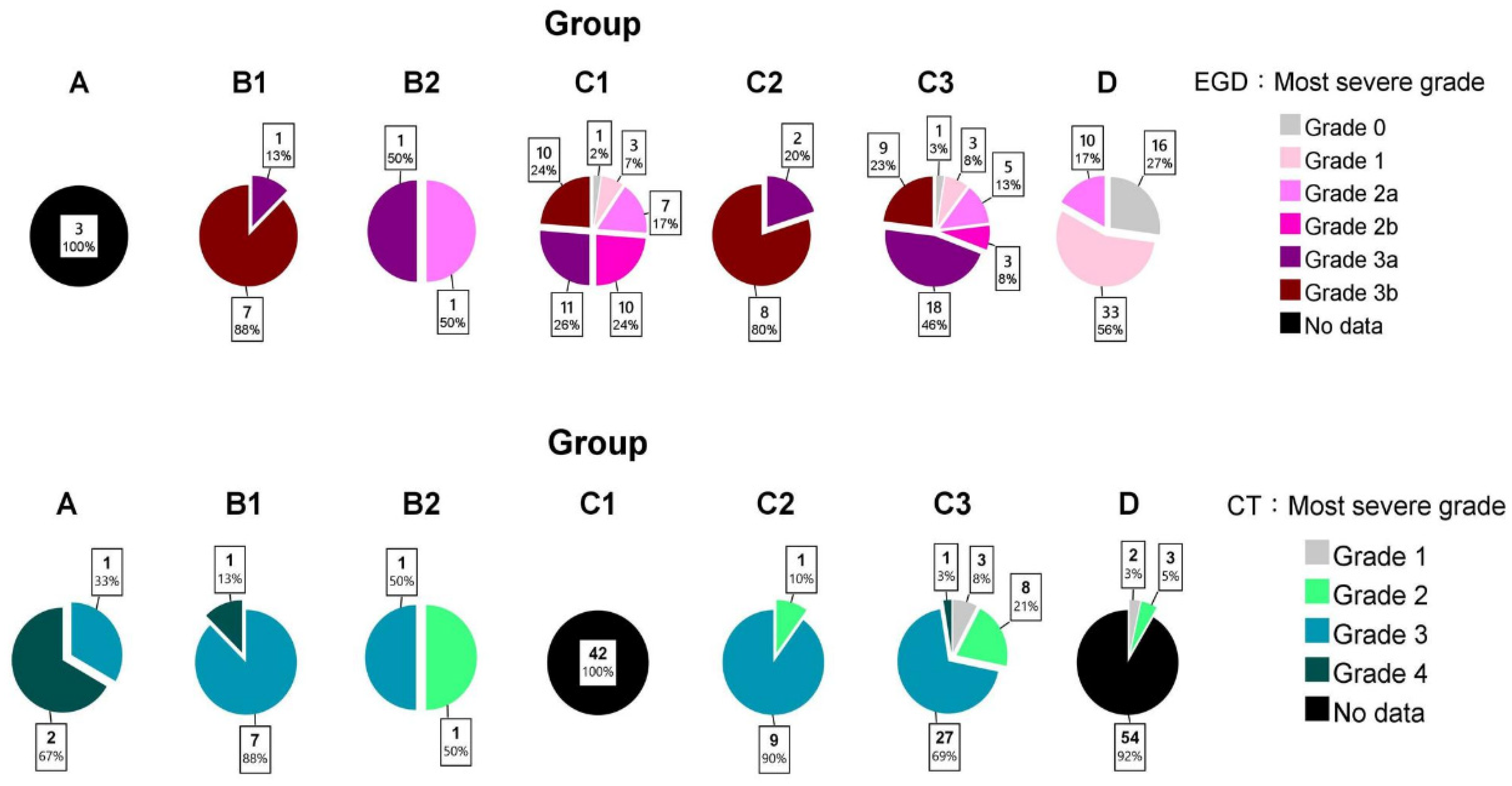
3.2. EGD Grading
3.3. CT Grading
3.4. Survival Outcomes
3.5. Roles of EGD/CT in Group C
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hoffman, R.S.; Burns, M.M.; Gosselin, S. Ingestion of Caustic Substances. N. Engl. J. Med. 2020, 382, 1739–1748. [Google Scholar] [CrossRef]
- Chirica, M.; Bonavina, L.; Kelly, M.D.; Sarfati, E.; Cattan, P. Caustic ingestion. Lancet 2017, 389, 2041–2052. [Google Scholar] [CrossRef]
- Hall, A.H.; Jacquemin, D.; Henny, D.; Mathieu, L.; Josset, P.; Meyer, B. Corrosive substances ingestion: A review. Crit. Rev. Toxicol. 2019, 49, 637–669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Contini, S.; Scarpignato, C. Caustic injury of the upper gastrointestinal tract: A comprehensive review. World J. Gastroenterol. 2013, 19, 3918–3930. [Google Scholar] [CrossRef]
- Hugh, T.B.; Kelly, M.D. Corrosive ingestion and the surgeon. J. Am. Coll. Surg. 1999, 189, 508–522. [Google Scholar] [CrossRef]
- Chen, Y.J.; Seak, C.J.; Kang, S.C.; Chen, T.H.; Chen, C.C.; Ng, C.J.; Lee, C.W.; Su, M.Y.; Huang, H.C.; Chen, P.C.; et al. A new perspective of the risk of caustic substance ingestion: The outcomes of 468 patients in one North Taiwan medical center within 20 years. Clin. Toxicol. 2021, 59, 409–417. [Google Scholar] [CrossRef]
- Chang, J.M.; Liu, N.J.; Pai, B.C.J.; Liu, Y.H.; Tsai, M.H.; Lee, C.S.; Chu, Y.Y.; Lin, C.C.; Chiu, C.T.; Cheng, H.T. The role of age in predicting the outcome of caustic ingestion in adults: A retrospective analysis. BMC Gastroenterol. 2011, 11, 72. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.J.; Seak, C.J.; Chen, C.C.; Chen, T.H.; Kang, S.C.; Ng, C.J.; Lee, C.W.; Su, M.Y.; Huang, H.C.; Ooyang, C.H.; et al. The Association Between Caustic Ingestion and Psychiatric Comorbidity Based on 396 Adults Within 20 Years. Risk Manag. Healthc. Policy 2020, 13, 1815–1824. [Google Scholar] [CrossRef]
- Chen, C.M.; Chung, Y.C.; Tsai, L.H.; Tung, Y.C.; Lee, H.M.; Lin, M.L.; Liu, H.L.; Tang, W.R. A Nationwide Population-Based Study of Corrosive Ingestion in Taiwan: Incidence, Gender Differences, and Mortality. Gastroenterol. Res. Pract. 2016, 2016, 7905425. [Google Scholar] [CrossRef]
- Bonavina, L.; Chirica, M.; Skrobic, O.; Kluger, Y.; Andreollo, N.A.; Contini, S.; Simic, A.; Ansaloni, L.; Catena, F.; Fraga, G.P.; et al. Foregut caustic injuries: Results of the world society of emergency surgery consensus conference. World J. Emerg. Surg. 2015, 10, 44. [Google Scholar] [CrossRef] [Green Version]
- Bruzzi, M.; Chirica, M.; Resche-Rigon, M.; Corte, H.; Voron, T.; Sarfati, E.; Zagdanski, A.M.; Cattan, P. Emergency Computed Tomography Predicts Caustic Esophageal Stricture Formation. Ann. Surg. 2019, 270, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Zargar, S.A.; Kochhar, R.; Mehta, S.; Mehta, S.K. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest. Endosc. 1991, 37, 165–169. [Google Scholar] [CrossRef]
- Cheng, H.T.; Cheng, C.L.; Lin, C.H.; Tang, J.H.; Chu, Y.Y.; Liu, N.J.; Chen, P.C. Caustic ingestion in adults: The role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008, 8, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryu, H.H.; Jeung, K.W.; Lee, B.K.; Uhm, J.H.; Park, Y.H.; Shin, M.H.; Kim, H.L.; Heo, T.; Min, Y.I. Caustic injury: Can CT grading system enable prediction of esophageal stricture? Clin. Toxicol. 2010, 48, 137–142. [Google Scholar] [CrossRef]
- Methasate, A.; Lohsiriwat, V. Role of endoscopy in caustic injury of the esophagus. World J. Gastrointest. Endosc. 2018, 10, 274–282. [Google Scholar] [CrossRef]
- Bahrami-Motlagh, H.; Hadizadeh-Neisanghalb, M.; Peyvandi, H. Diagnostic Accuracy of Computed Tomography Scan in Detection of Upper Gastrointestinal Tract Injuries Following Caustic Ingestion. Emergency 2017, 5, e61. [Google Scholar]
- Chirica, M.; Resche-Rigon, M.; Zagdanski, A.M.; Bruzzi, M.; Bouda, D.; Roland, E.; Sabatier, F.; Bouhidel, F.; Bonnet, F.; Munoz-Bongrand, N.; et al. Computed Tomography Evaluation of Esophagogastric Necrosis After Caustic Ingestion. Ann. Surg. 2016, 264, 107–113. [Google Scholar] [CrossRef]
- Chirica, M.; Resche-Rigon, M.; Pariente, B.; Fieux, F.; Sabatier, F.; Loiseaux, F.; Munoz-Bongrand, N.; Gornet, J.M.; Brette, M.D.; Sarfati, E.; et al. Computed tomography evaluation of high-grade esophageal necrosis after corrosive ingestion to avoid unnecessary esophagectomy. Surg. Endosc. 2015, 29, 1452–1461. [Google Scholar] [CrossRef]
- Havanond, C.; Havanond, P. Initial signs and symptoms as prognostic indicators of severe gastrointestinal tract injury due to corrosive ingestion. J. Emerg. Med. 2007, 33, 349–353. [Google Scholar] [CrossRef]
- Lurie, Y.; Slotky, M.; Fischer, D.; Shreter, R.; Bentur, Y. The role of chest and abdominal computed tomography in assessing the severity of acute corrosive ingestion. Clin. Toxicol. 2013, 51, 834–837. [Google Scholar] [CrossRef]
- Fil, L.J.; Verma, G.; Hoffman, R.S. Clarifying a study: Computed tomography and assessing the severity of acute corrosive ingestion. Clin. Toxicol. 2014, 52, 82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonnici, K.S.; Wood, D.M.; Dargan, P.I. Should computerised tomography replace endoscopy in the evaluation of symptomatic ingestion of corrosive substances? Clin. Toxicol. 2014, 52, 911–925. [Google Scholar] [CrossRef] [PubMed]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron. Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Hotchkiss, R.S.; Moldawer, L.L.; Opal, S.M.; Reinhart, K.; Turnbull, I.R.; Vincent, J.L. Sepsis and septic shock. Nat. Rev. Dis. Primers 2016, 2, 16045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keh, S.M.; Onyekwelu, N.; McManus, K.; McGuigan, J. Corrosive injury to upper gastrointestinal tract: Still a major surgical dilemma. World J. Gastroenterol. 2006, 12, 5223–5228. [Google Scholar] [PubMed]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; p. 177. [Google Scholar]
- Li, Y.; Langworthy, J.; Xu, L.; Cai, H.; Yang, Y.; Lu, Y.; Wallach, S.L.; Friedenberg, F.K. Nationwide estimate of emergency department visits in the United States related to caustic ingestion. Dis. Esophagus 2020, 33, doaa012. [Google Scholar] [CrossRef]




| Variable | Group A | Group B1 | Group B2 | Group C1 | Group C2 | Group C3 | Group D | Total |
|---|---|---|---|---|---|---|---|---|
| (n = 3, 1.8%) | (n = 8, 4.9%) | (n = 2, 1.2%) | (n = 42, 25.8%) | (n = 10, 6.1%) | (n = 39, 23.9%) | (n = 59, 36.2%) | (n = 163, 100%) | |
| Female | 2 (66.7) | 5 (62.5) | 1 (50.0) | 22 (52.4) | 7 (70.0) | 25 (64.1) | 25 (42.4) | 87 (53.4) |
| Age, year | 64 (nil) | 51 (37) | 55 (nil) | 48 (22) | 45 (13) | 55 (26) | 43 (28) | 50 (28) |
| Old (age ≥ 65) | 1 (33.3) | 3 (37.5) | 1 (50.0) | 8 (19.0) | 1 (10.0) | 15 (38.5) | 14 (23.7) | 43 (26.4) |
| Caustics substances | ||||||||
| Acid | 3 (100) | 4 (50.0) | 1 (50.0) | 19 (45.2) | 6 (60.0) | 23 (59.0) | 25 (42.4) | 81 (49.7) |
| Alkaline | 0 (0) | 4 (50.0) | 1 (50.0) | 19 (45.2) | 4 (40.0) | 13 (33.3) | 25 (42.4) | 66 (40.5) |
| Uncertain 1 | 0 (0) | 0 (0) | 0 (0) | 4 (9.5) | 0 (0) | 3 (7.7) | 9 (15.3) | 16 (9.8) |
| Strong caustics (pH < 2 or >12) | 3 (100) | 6 (75.0) | 1 (50.0) | 20 (57.1) | 5 (50.0) | 21 (63.6) | 14 (26.4) | 70 (42.9) |
| Strong acids (pH < 2) | 3 (100) | 4 (50.0) | 1 (50.0) | 11 (26.8) | 4 (40.0) | 15 (44.1) | 9 (15.8) | 47 (28.8) |
| Strong alkalis (pH > 12) | 0 (0) | 2 (25.0) | 0 (0) | 9 (22.0) | 1 (10.0) | 6 (15.4) | 5 (8.8) | 23 (14.1) |
| Ingested amount, mL | 150 (nil) | 250 (200) | 505 (nil) | 100 (175) | 50 (125) | 100 (200) | 50 (120) | 100 (183) |
| Amount ≥ 100 mL | 2 (66.7) | 5 (83.3) | 1 (50.0) | 17 (58.6) | 3 (42.9) | 17 (63.0) | 15 (34.1) | 60 (50.8) |
| Suicidal ingestion | 3 (100) | 8 (100) | 2 (100) | 32 (76.2) | 9 (90.0) | 34 (87.2) | 38 (64.4) | 126 (77.3) |
| EGD grades | ||||||||
| Esophagus ≥ 2b | nil | 7 (87.5) | 1 (50) | 21 (50.0) | 9 (90.0) | 17 (43.6) | 0 (0) | 55 (34.4) |
| Stomach ≥ 2b | nil | 8 (100) | 1 (50) | 23 (54.8) | 10 (100) | 29 (76.3) | 0 (0) | 71 (44.4) |
| Duodenum ≥ 2b | nil | 5 (62.5) | 1 (50) | 3 (7.7) | 5 (50.0) | 6 (16.7) | 0 (0) | 20 (12.5) |
| Incomplete EGD study | nil | 0 (0) | 0 (0) | 3 (7.1) | 0 (0) | 3 (7.7) | 0 (0) | 6 (3.8) |
| ETT + MV during EGD | nil | 5 (62.5) | 0 (0) | 8 (19.0) | 3 (30.0) | 8 (20.5) | 0 (0) | 24 (15.0) |
| CT grades | ||||||||
| Esophagus ≥ 3 | 3 (100) | 5 (62.5) | 0 (0) | nil | 8 (80.0) | 20 (51.3) | 0 (0) | 36 (53.7) |
| Stomach ≥ 3 | 3 (100) | 8 (100) | 1 (50.0) | nil | 9 (90.0) | 25 (64.1) | 0 (0) | 46 (68.7) |
| Duodenum ≥ 3 | 0 (0) | 3 (37.5) | 0 (0) | nil | 0 (0) | 2 (5.1) | 0 (0) | 5 (7.5) |
| Admission | 3 (100) | 8 (100) | 2 (100) | 42 (100) | 10 (100) | 39 (100) | 0 (100) | 104 (63.8) |
| Inpatient days | 16 (nil) | 31 (29) | 8 (nil) | 10 (10) | 16 (13) | 13 (18) | 0 (0) | 8 (16) |
| ICU admission | 3 (100) | 7 (87.5) | 0 (0) | 5 (11.9) | 7 (70) | 9 (23.1) | 0 (0) | 31 (19.0) |
| In-hospital mortality | 1 (33.3) | 1 (12.5) | 0 (0) | 1 (2.4) | 0 (0) | 0 (0) | 0 (0) | 3 (2.9) |
| Operation | 3 (100) | 8 (100) | 0 (0) | 0 (0) | 10 (100) | 0 (0) | 0 (0) | 21 (12.9) |
| Systemic complications | 3 (100) | 4 (50.0) | 0 (0) | 18 (42.9) | 6 (60.0) | 9 (23.1) | 0 (0) | 43 (26.4) |
| Aspiration injury | 2 (66.7) | 2 (25.0) | 0 (0) | 11 (26.2) | 2 (20.0) | 6 (15.4) | 0 (0) | 22 (13.5) |
| Respiratory failure | 2 (66.7) | 2 (25.0) | 0 (0) | 8 (19.0) | 1 (10.0) | 6 (15.4) | 0 (0) | 19 (11.7) |
| Hepatic injury | 1 (33.3) | 2 (25.0) | 0 (0) | 6 (14.3) | 3 (30.0) | 2 (5.1) | 0 (0) | 14 (8.6) |
| Renal injury | 0 (0) | 1 (12.5) | 0 (0) | 7 (16.7) | 2 (20.0) | 2 (5.1) | 0 (0) | 12 (7.4) |
| Septic shock | 1 (33.3) | 1 (12.5) | 0 (0) | 1 (2.4) | 0 (0) | 0 (0) | 0 (0) | 3 (1.8) |
| DIC | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (10.0) | 0 (0) | 0 (0) | 1 (0.6) |
| GI complications | 3 (100) | 5 (62.5) | 1 (50.0) | 16 (38.1) | 5 (50.0) | 16 (41.0) | 0 (0) | 49 (30.1) |
| Bleeding | 3 (100) | 4 (50.0) | 1 (50.0) | 8 (19.0) | 2 (20.0) | 7 (17.9) | 0 (0) | 25 (15.3) |
| Perforation | 3 (100) | 3 (37.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6 (3.7) |
| Stricture formation | 1 (33.3) | 1 (12.5) | 0 (0) | 9 (21.4) | 2 (20.0) | 13 (33.3) | 0 (0) | 0 (0) |
| Delayed fistula formation | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (10.0) | 0 (0) | 0 (0) | 1 (0.6) |
| Follow-up duration, months | 50.9 (nil) | 32.5 (69.8) | 31.2 (nil) | 13.0 (50.2) | 33.8 (34.0) | 15.4 (32.4) | 6.1 (26.3) | 12.8 (39.3) |
| All-cause mortality | 2 (66.7) | 1 (12.5) | 0 (0) | 4 (9.5) | 0 (0) | 3 (7.7) | 1 (1.7) | 11 (6.7) |
| Endoscopic dilation for stricture or obstruction | 1 (33.3) | 0 (0) | 0 (0) | 7 (16.7) | 1 (10.0) | 6 (15.4) | 0 (0) | 15 (9.2) |
| Operation for stricture or obstruction | 0 (0) | 1 (12.5) | 0 (0) | 3 (7.1) | 0 (0) | 6 (15.4) | 0 (0) | 10 (6.1) |
| Psychiatric comorbidities | 3 (100) | 7 (87.5) | 2 (100) | 35 (83.3) | 9 (90.0) | 33 (84.6) | 37 (62.7) | 126 (77.3) |
| Systemic comorbidities | ||||||||
| Hypertension | 1 (33.3) | 3 (37.5) | 0 (0) | 13 (31.0) | 0 (0) | 13 (33.3) | 11 (18.6) | 41 (25.2) |
| Diabetes mellitus | 0 (0) | 0 (0) | 0 (0) | 7 (16.7) | 2 (20.0) | 10 (25.6) | 2 (3.4) | 21 (12.9) |
| Cancer | 0 (0) | 1 (12.5) | 0 (0) | 2 (4.8) | 1 (10.0) | 5 (12.8) | 1 (1.7) | 10 (6.1) |
| Coronary artery disease | 0 (0) | 0 (0) | 0 (0) | 1 (2.4) | 1 (10.0) | 2 (5.1) | 2 (3.4) | 6 (3.7) |
| Variable | Group C1 (n = 42) | Group C2/C3 (n = 49) | p-Value |
|---|---|---|---|
| Female | 22 (52.4) | 32 (65.3) | 0.285 |
| Age, year | 48 (22) | 54 (26) | 0.188 |
| Strong caustics (pH < 2 or > 12) | 20 (57.1) | 26 (60.5) | 0.82 |
| Acid/Alkaline/Uncertain | 19 (45.2)/19 (45.2)/4 (9.5) | 29 (59.2)/17 (34.7)/3 (6.1) | 0.405 |
| Ingested amount ≥ 100 mL | 17 (58.6) | 20 (58.8) | >0.999 |
| Suicidal ingestion | 32 (76.2) | 43 (87.8) | 0.175 |
| Psychiatric comorbidity | 35 (83.3) | 42 (85.7) | 0.827 |
| EGD grades | 0.122 | ||
| 0/1 | 1 (2.4)/3 (7.1) | 1 (2.0)/3 (6.1) | |
| 2a/2b | 7 (16.7)/10 (23.8) | 5 (10.2)/3 (6.1) | |
| 3a/3b | 11 (26.2)/10 (23.8) | 20 (40.8)/17 (34.7) | |
| ETT + MV during EGD | 8 (19.0) | 11 (22.4) | 0.798 |
| Inpatient days | 10 (10) | 14 (16) | 0.297 |
| In-hospital mortality | 1 (2.4) | 0 (0) | 0.466 |
| Overall survival 1 | 38 (90.5) | 46 (93.9) | 0.545 |
| Systemic complications | 18 (42.9) | 15 (30.6) | 0.276 |
| Aspiration injury | 11 (26.2) | 8 (16.3) | 0.305 |
| Respiratory failure | 8 (19.0) | 7 (14.3) | 0.582 |
| Hepatic injury | 6 (14.3) | 5 (10.2) | 0.749 |
| Renal injury | 7 (16.7) | 4 (8.2) | 0.334 |
| Septic shock | 1 (2.4) | 0 (0) | 0.462 |
| DIC | 0 (0) | 1 (2.0) | >0.999 |
| GI complications | 16 (38.1) | 21 (42.9) | 0.674 |
| Bleeding | 8 (19.0) | 9 (18.4) | >0.999 |
| Perforation | 0 (0) | 0 (0) | – |
| Stricture formation | 9 (21.4) | 15 (30.6) | 0.35 |
| Endoscopic dilation for stricture | 7 (16.7) | 7 (14.3) | 0.779 |
| Covariate | Univariate | Multivariate | ||
|---|---|---|---|---|
| Unadjusted OR (95% CI) for Requiring Operation | p-Value | Adjusted OR (95% CI) for Requiring Operation | p-Value | |
| Age (year) | 0.960 (0.919–1.003) | 0.069 | 0.970 (0.923–1.020) | 0.236 |
| EGD grade 1 | 8.556 (1.622–45.136) | 0.011 | 8.555 (1.559–46.942) | 0.013 |
| CT grade 1 | 2.250 (0.497–10.178) | 0.292 | 0.350 (0.028–4.360) | 0.415 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-J.; Seak, C.-J.; Cheng, H.-T.; Chen, C.-C.; Chen, T.-H.; Sung, C.-M.; Ng, C.-J.; Kang, S.-C.; Su, M.-Y.; Hsieh, S.-Y. Evaluation of a Diagnostic and Management Algorithm for Adult Caustic Ingestion: New Concept of Severity Stratification and Patient Categorization. J. Pers. Med. 2022, 12, 989. https://doi.org/10.3390/jpm12060989
Chen Y-J, Seak C-J, Cheng H-T, Chen C-C, Chen T-H, Sung C-M, Ng C-J, Kang S-C, Su M-Y, Hsieh S-Y. Evaluation of a Diagnostic and Management Algorithm for Adult Caustic Ingestion: New Concept of Severity Stratification and Patient Categorization. Journal of Personalized Medicine. 2022; 12(6):989. https://doi.org/10.3390/jpm12060989
Chicago/Turabian StyleChen, Yu-Jhou, Chen-June Seak, Hao-Tsai Cheng, Chien-Cheng Chen, Tsung-Hsing Chen, Chang-Mu Sung, Chip-Jin Ng, Shih-Ching Kang, Ming-Yao Su, and Sen-Yung Hsieh. 2022. "Evaluation of a Diagnostic and Management Algorithm for Adult Caustic Ingestion: New Concept of Severity Stratification and Patient Categorization" Journal of Personalized Medicine 12, no. 6: 989. https://doi.org/10.3390/jpm12060989
APA StyleChen, Y.-J., Seak, C.-J., Cheng, H.-T., Chen, C.-C., Chen, T.-H., Sung, C.-M., Ng, C.-J., Kang, S.-C., Su, M.-Y., & Hsieh, S.-Y. (2022). Evaluation of a Diagnostic and Management Algorithm for Adult Caustic Ingestion: New Concept of Severity Stratification and Patient Categorization. Journal of Personalized Medicine, 12(6), 989. https://doi.org/10.3390/jpm12060989







