Abstract
(1) Background: Our study aimed to assess the association between the neutrophil to lymphocyte ratio (NLR), platelet to leukocyte ratio (PLR), lymphocyte to monocyte ratio (LMR), red cell distribution width (RDW), and systemic immune inflammation index (SII) and periodontitis. (2) Methods: We searched PubMed, Embase, Scopus, Web of Science, and LILACS databases, identifying observational studies. The Newcastle Ottawa scale was used to evaluate the quality of the included studies. The principal summary outcome measure in our random effects meta-analysis was the mean difference (MD). (3) Results: After screening 682 search results, a total of 10 studies including 3164 subjects were selected for quantitative assessment. We found a higher mean NLR, PLR, and LMR in the periodontitis group compared to the control group (0.41 (95% CI 0.12–0.7), p = 0.006; 7.43 (95% CI 0.31–14.54), p = 0.04; 2.05 (95% CI 0.27–3.83), p = 0.024). No differences were observed for RDW. (4) Conclusions: We found an association between NLR, LMR, and PLR and periodontitis, which might be thought of as emerging blood cell count inflammatory biomarkers that could shed light on the link between periodontitis and systemic disbalances, as well as for periodontitis prognosis and grading.
1. Introduction
Periodontitis represents a group of chronic diseases that affect the supporting tissues of the teeth and are characterized by the destruction of periodontal tissues, the alveolar bone, and the supporting tissues of teeth. Inflammatory cells cause an immune response in the periodontal tissues [1]. The inflammatory mediators from the periodontal tissues can activate the immune system and initiate a systemic acute phase response [2]. In addition, many chronic diseases are linked to periodontitis, including cardiovascular disease, diabetes, cerebrovascular disease, neurodegenerative disease, and cancer [3]. Analyzing systemic circulatory markers, such as neutrophils [4,5], the neutrophil to lymphocyte ratio (NLR) [1], platelets [6], the platelet to leukocyte ratio (PLR) [7], and erythrocyte counts [8], could offer relevant data regarding systemic and periodontal infection.
The white blood cell count and absolute neutrophil count seem to be among the additional markers that could also help predict infection [9]. The amount of peripheral white blood cells has been reported to rise as the severity of periodontitis increases [10]. Despite the fact that these indicators are not specific to periodontitis, there may be a link between them.
In 2017, a new classification scheme for periodontitis was adopted [11]. The new periodontal disease categorization replaced the previous one [12], which uses a single term, “periodontitis”, for all earlier forms of the disease defined as “chronic” or “aggressive”.
To the best of our knowledge, there is no systematic review focusing on the relation between blood cell count inflammatory markers and periodontitis. Therefore, the objectives of this research were to carry out a systematic review and meta-analysis to investigate the association between the neutrophil to lymphocyte ratio (NLR), platelet to leukocyte ratio (PLR), lymphocyte to monocyte ratio (LMR), red cell distribution width (RDW), and systemic immune inflammation index (SII) and periodontitis.
2. Materials and Methods
This systematic review was performed in accordance with the recommendations of the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA) Statement” [13].
2.1. Eligibility Criteria
We included in our review all the studies on periodontitis subjects assessing inflammation status using blood cell count ratios or the red cell distribution width. We excluded case reports, mechanistic articles, animal studies, reviews, editorials, and conference abstracts.
2.2. Information Sources
A structured electronic search was conducted in March 2022 of the following databases: PubMed, Scopus, Embase, Web of Science, and LILACS. MeSH and Emtree terms were used, where applicable. The last electronic search was performed on all databases on 15 April 2022.
2.3. Search Strategy
The search strategy included the terms “neutrophils”, “platelets”, “lymphocytes”, “ratio”, “systemic immune inflammation index”, “red cell distribution width”, and “periodontitis” as free text words, along with MeSH or Emtree terms (where possible), synonyms, singular as well as plural forms, and abbreviations (NLR, PLR, LMR, SII, RDW). The complete strategies adapted for each database are presented in Supplementary Table S1.
2.4. Selection Process
The exported lists of results from all the databases were imported in the Clarivate EndNoteTM online version [14], where the duplicates were removed by the software. Next, the remaining results were exported to an Excel spreadsheet file (Microsoft Office 365, MS, Redmond, WA, USA), which served as a selection, extraction, and quality assessment electronic form. All references were managed with Zotero software version 6.0.6 (Roy Rosenzweig Center for History and New Media, Fairfax, Virginia, USA) [15]. Two authors (A.O., L.D.C.) independently screened the titles and abstracts of all the articles manually, and, when in doubt, debated whether the paper should be considered. The selected articles were retrieved in full-text and assessed for inclusion by the same authors independently, with differences in opinion resolved by discussion. For each excluded article, the exclusion motive was recorded. For one article for which we could not locate a full-text version, we contacted the corresponding author, and he provided us with the document we needed.
2.5. Data Collection Process
Two reviewers extracted data from the articles in the standardized Excel form file.
2.6. Data Items
Data were extracted using a standardized form, which included the following information: (1) author names and year of publication; (2) title; (3) abstract; (4) publication title; (5) keywords; (6) study selection; (7) screening; (8) inclusion criteria; (9) exclusion criteria; (10) population; (11) exposure; (12) age; (13) gender; (14) other characteristics; (15) outcomes (NLR, PLR, LMR, RDW), i.e., mean and standard deviations; and (16) studies’ quality assessment.
2.7. Study Risk of Bias Assessment
All the selected articles were independently assessed regarding their methodological quality by two reviewers, and differences in assessment were resolved by discussion. The Newcastle Ottawa Scale [16] for case-control studies was used to identify the sources of bias.
2.8. Effect Measures
For all the outcomes, the mean difference was used as an effect measure, along with its confidence interval.
2.9. Synthesis Methods
If we could not identify the mean and standard deviation for the outcomes we were interested in and only found medians, we used the formula supplied by Hozo SP et al. to convert the range and number of participants [17]. Although some papers lacked the needed numbers, we were able to identify them in their charts. We extracted the numerical values from the figures using WebPlotDigitizer [18].
All meta-analyses were performed with the random effects model using the method of restricted maximum likelihood to estimate the heterogeneity variance, as we anticipated a clinical heterogenicity between studies. The Χ2-based Q-test and I2 were used to assess between-study heterogeneity, according to the Cochrane Handbook’s recommendations [19]
Meta-analyses were carried out in the R environment for statistical computing and graphics, version 4.1.2 [20], using the meta R package [21]. The leave-one-out sensitivity analyses, performed in case of important heterogeneity meta-analyses, as well as meta-analysis diagnostics to identify influential studies were carried out with the dmetar package [22]. No subgroup analyses were performed.
2.10. Reporting Bias Assessment
Since the number of selected studies was low, publication bias assessment is underpowered. Nevertheless, we computed the Egger test and plotted funnel plots to assess the presence of publication bias.
3. Results
3.1. Study Selection
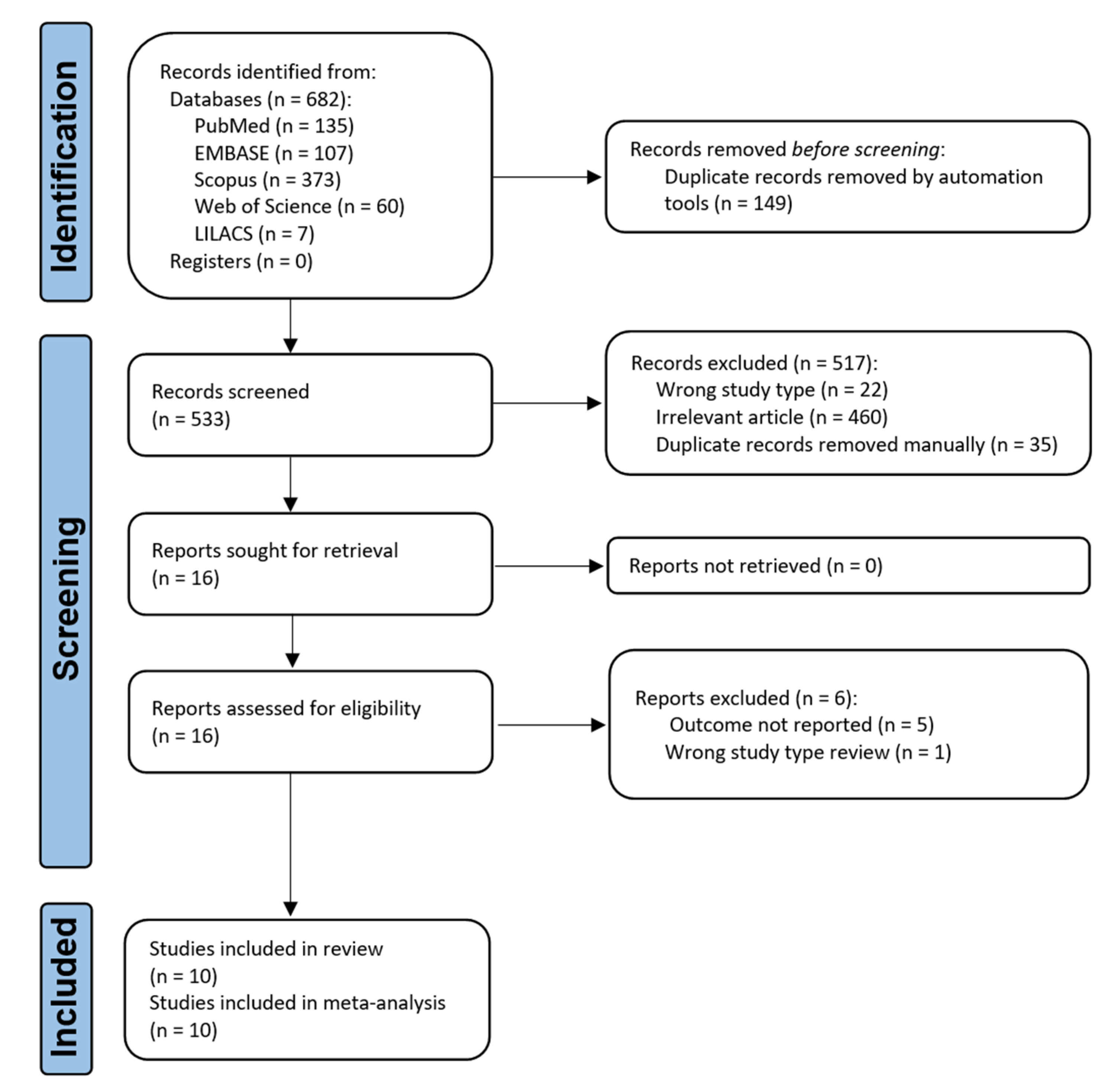
A description of the search process and selection is presented in a PRISMA flow diagram (Figure 1). A total of 682 publications were found in the initial search (PubMed n = 135, EMBASE n = 107, Scopus n = 373, Web of Science n = 60, LILACS n = 7). After being identified as duplicates, a total of 149 studies were deleted. Following the removal of duplicates, 533 articles were subjected to a preliminary screening that included a review of the title and abstract for compliance with the inclusion and exclusion criteria. Then, 110 articles were eliminated during the screening process. There were 460 irrelevant articles and 22 wrong study types, and 35 duplicate records. We looked for the complete text of 16 articles, and for one article, we contacted the authors through email, and finally, we managed to collect all the necessary files. We read and evaluated the whole text thoroughly in order to determine the remaining articles’ eligibility. Six of these articles were eliminated for the following reasons: outcome not reported (n = 5) or wrong study type, i.e., review (n = 1). As a result, the qualitative and quantitative synthesis included 10 articles.

Figure 1.
Flow diagram of the literature search and selection criteria adapted for PRISMA 2020.
3.2. Study Characteristics
Table 1 and Supplementary Table S2 summarizes the basic characteristics of the studies that were included. A total of 3164 subjects were included in this systematic review and meta-analysis.

Table 1.
Characteristics of the included studies.
Eight studies used a cross-sectional study design, and two used a case-control study design. All investigations were conducted in Asia (Turkey n = 4, India n = 4, Thailand n = 1, China n = 1). Two articles assessed gingival aggressive periodontitis and eight articles observed chronic periodontitis as a case group; all articles compared them to healthy controls. The periodontitis classification differed between articles, with seven using World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions (1999 or 2017 versions); one used the Centers for Disease Control and Prevention, American Academy of Periodontology classification; and two did not stipulate any classification system. Six studies had a mean age of subjects between 26 and 40, three studies had a mean age of around 50, and one study did not report the age range. Most studies reported a similar distribution of gender between the groups. Concerning outcomes, seven studies reported NLR, four reported PLR and RDW, one reported LMR, and no article was identified to report SII.
3.3. Results of Syntheses
3.3.1. Neutrophil to Lymphocyte Ratio
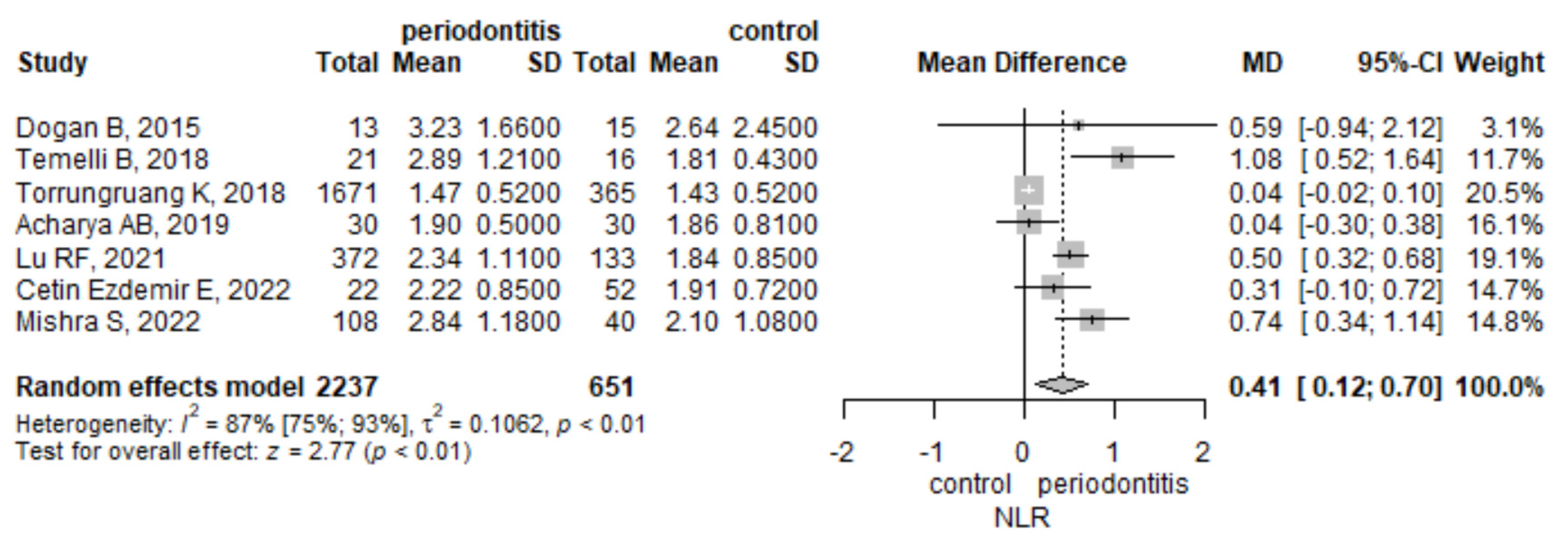
The meta-analysis of seven studies found that the mean NLR was higher by 0.41 (95% CI 0.12–0.7), p = 0.006, in the periodontitis group compared to the control group (Figure 2). There was a statistically significant heterogeneity, measured with I2 = 86.8% (95% CI 74.9–93%), p = < 0.001. To assess the robustness of the result, we performed a leave-one-out sensitivity analysis (Supplementary Figure S1). The result remained statistically significant after excluding each of the articles included in the meta-analysis. The influence analysis indicated the Torrungruang [29] study to be influential. When removing the Torrungruang study [29], the heterogeneity was the lowest, dropping to 62%, as assessed by I2, while with the removal of any other study, the heterogeneity was greater than or equal to 81%.

Figure 2.
Neutrophile to lymphocyte ratio-mean difference between periodontitis and control subjects.
3.3.2. Platelet to Leucocyte Ratio
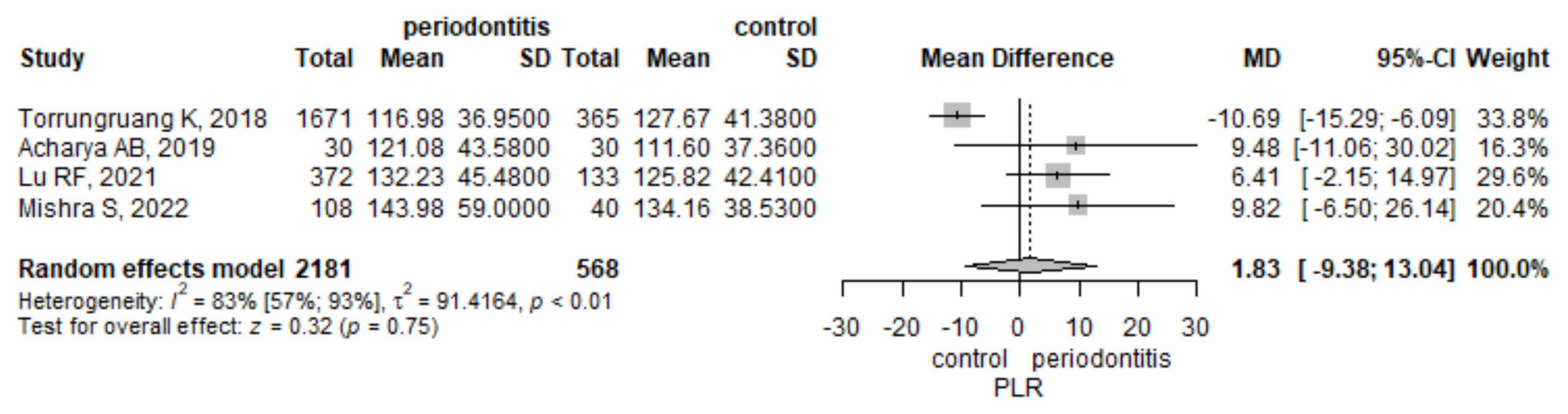
Four studies analyzed the values of PLR. The meta-analysis found a mean PLR higher by 1.83 (95% CI −9.38–13.04) in the periodontitis group compared to the control group, but the result was not statistically significant, p = 0.749 (Figure 3). There was a statistically significant heterogeneity, measured with I2 = 83.1% (95% CI 56.9–93.4%), p = < 0.001. To assess the robustness of the result, we performed a leave-one-out sensitivity analysis (Supplementary Figure S2). The influence analysis indicated the Torrungruang study [29] to be influential. When removing the Torrungruang study [29], the result became statistically significant, and the heterogeneity dropped to 0%, as assessed by I2. When removing any other study, the pooled estimate did not reach statistical significance.

Figure 3.
Platelet to leucocyte ratio-mean difference between periodontitis and control subjects.
3.3.3. Lymphocyte to Monocyte Ratio
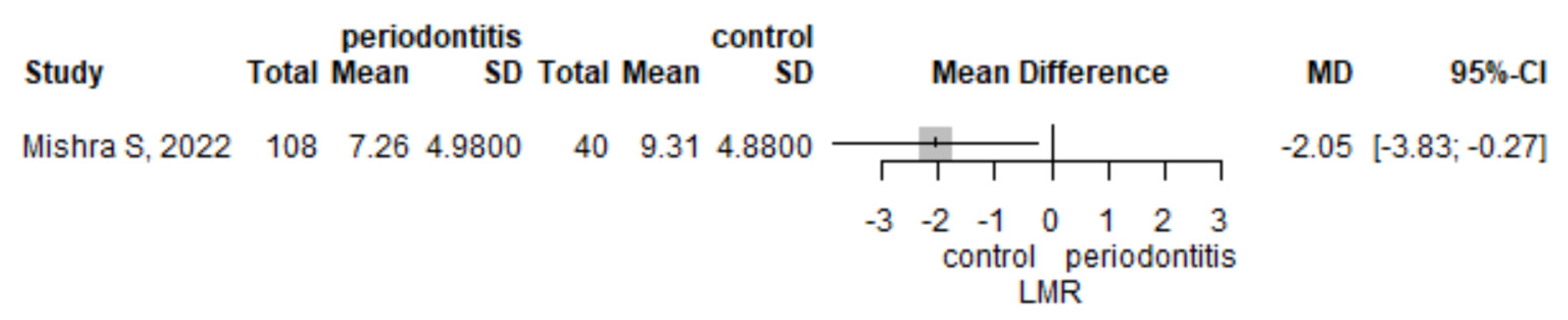
The mean LMR was lower in the periodontitis group compared to the control group (mean difference of 2.05 (95% CI 0.27–3.83), p = 0.024, as observed in one study, Mishra et al. [26]) (Figure 4).

Figure 4.
Lymphocyte to monocyte ratio -mean difference between periodontitis and control subjects.
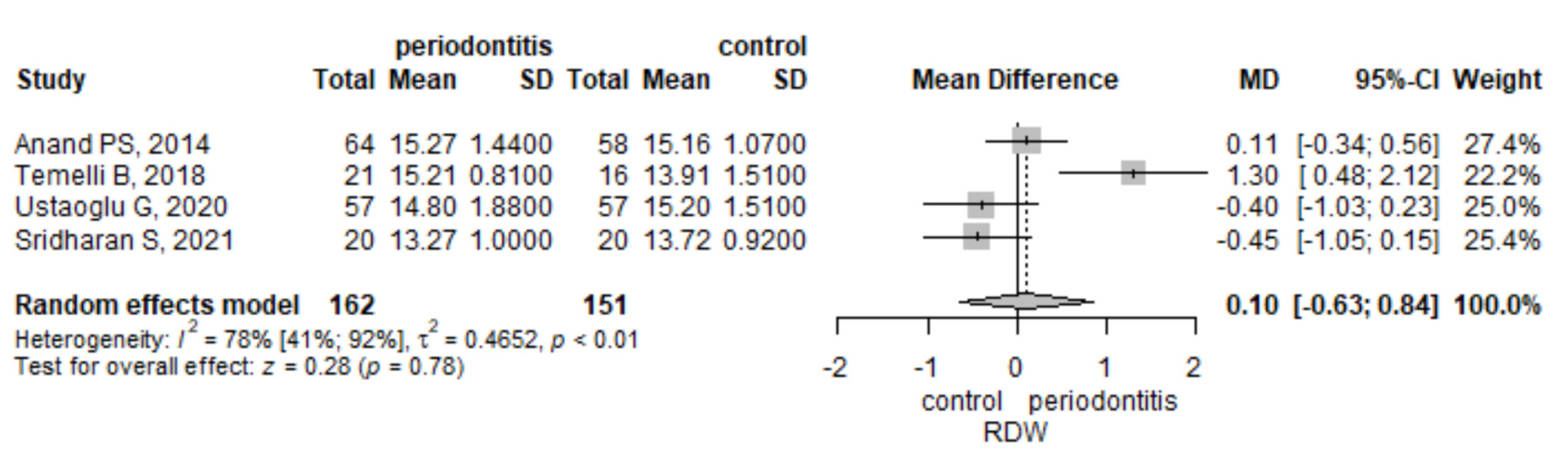
3.3.4. Red Cell Distribution Width
The meta-analysis of four studies that assessed RDW observed that its mean values were higher by 0.1 (95% CI −0.63–0.84) in the periodontitis group compared to the control group, but the result was not significant, p = 0.782 (Figure 5). There was a statistically significant heterogeneity, measured with I2 = 78.1% (95% CI 40.9–91.9%), p = 0.003. To assess the robustness of the result, we performed a leave-one-out sensitivity analysis (Supplementary Figure S3). The influence analysis indicated the Temelli B et al. study [28] to be influential. When removing the Temelli study [28], the result did not reach the significance level, although the heterogeneity dropped to 30%. In the case of any other study removal, the heterogeneity was greater than or equal to 81%.

Figure 5.
Red cell distribution width-mean difference between periodontitis and control subjects.
3.4. Risk of Bias in Studies
We used the Newcastle Ottawa scale (NOS) [16] to assess the methodological quality of the included studies (Table 2). For the objective of our review, we used the case-control subsection of the NOS.

Table 2.
Newcastle Ottawa Scale quality assessment of the selected articles.
Regarding the selection section of the NOS scale, all the studies used pre-defined, transparent criteria to identify the presence of the disease (chronic periodontitis or aggressive periodontitis) and controls; thus, the case and control definitions were adequate. Nevertheless, the authors of the studies used different criteria to identify the disease according to official classifications (Periodontal Disease Classification, American Association of Periodontology 1999-three studies [23,25,28]; Classification of Periodontal and Peri-Implant Diseases and Conditions 2017-four studies [1,2,26,27]; Center of Disease Control and Prevention, American Academy of Periodontology Periodontal Disease Classification CDC/AAP-one study [29]), or no specified classification [7,24]. Only two studies (20%) out of ten had clear representativeness of the cases [23,28]. Two studies had a poor selection of controls [7,27], and two studies had a correct selection of controls. For the other six, it might be difficult to assess if the selection of controls was correct. Half of the studies enrolled subjects from the department of periodontology [1,2,7,23,26]; the other studies enrolled subjects from the internal medicine [28] or cardiology departments [24], or from an electrical company [29], and in two studies, the population was not stated [25,27].
Concerning comparability, only one study used matching for age and gender [27], and all the other studies performed a simple comparison between cases and controls. Nevertheless, all the studies used extensive exclusion criteria for systemic diseases, which help in group comparability. A problem in comparability might be the smoking status, as four studies had a percentage under 25% of smokers or occasional smokers [25,27,28].
All research can be regarded as bias-free when it comes to assessing blood parameters since the laboratory methods used were reliable, the same methods for cases and controls were used, and there was no non-response rate.
The biggest issue in the methodology of these studies is the representativeness of the cases. The possible problem with control selection, as well as the comparability of the groups, appears to be less affected.
3.5. Reporting Biases
Since the number of studies in each meta-analysis was below ten, publication bias could not be reliably assessed. Nevertheless, the p-values for the Egger test for assessing publication bias were greater than the level of significance.
4. Discussion
This is the first systematic review and meta-analysis, to our knowledge, investigating the association between blood cell count inflammatory biomarkers and periodontitis. Periodontitis was found to have a statistically significant relationship with NLR and LMR, a debatable association with PLR, and RDW did not approach the significance level.
The neutrophil to lymphocyte ratio and platelet to lymphocyte ratio are two biomarkers of systemic inflammation that have increasingly gained interest in the diagnosis of a variety of cardiovascular diseases [30,31,32], diabetes [33,34,35], inflammatory diseases [36,37], and malignancies [38,39]. In our review, we found higher mean values of NLR in periodontitis patients compared to healthy controls. Although there was an important heterogeneity, the result was robust even when performing the leave-one-out sensitivity analyses. Furthermore, a prospective study by Acharya et al. [7] objectivated the reduction of NLR and PLR levels after scaling and root planing.
Concerning PLR, the initial analysis did not reach statistical significance, but after the removal of the statistically influential study of Torrungruang et al. [29], the result became statistically significant and without heterogeneity. Twenty-five percent of the subjects in this study were with impaired glucose tolerance or diabetes, while all the other studies that reported PLR were free of systemic diseases; thus, this exclusion is likely to be warranted.
Little is known-and remains unknown-about the association between LMR and periodontitis, which could serve as a possible marker of systemic inflammation as well as aid in diagnosing and predicting the prognosis of periodontitis. Only one study reported the association between periodontitis and LMR, and it proved to be statistically significant, with higher values being observed in the periodontitis group.
Several studies found a link between periodontal disorders and low erythrocyte count, implying that periodontal diseases could be linked to chronic anemia [40,41]. RDW has also been linked to inflammatory markers, including erythrocyte sedimentation rate and high-sensitivity C-reactive protein, which have both been linked to periodontitis [42]. In our meta-analysis, we could not objectivate a statistically significant association between RDW and periodontitis, the results being heterogeneous, with studies showing conflicting results concerning the direction of the association.
Leite et al., in a systematic review and meta-regression, studied the effect of smoking on periodontitis and showed that periodontitis is aggravated by smoking [43]. Larvin et al. used a unique artificial intelligence-based network analysis to identify systemic multimorbidity clusters in subjects with periodontitis and analyzed factors that may influence the severity of those clusters. The authors stated that hypertension, arthritis, and obesity had the largest impact on multimorbidity clusters in subjects with periodontitis, and diabetes was more prevalent in those who had experienced a greater degree of clinical attachment loss. they also showed that in adults with severe periodontitis, smoking status influenced the clustering pattern of diabetes and cancer [44]. The authors of the chosen studies from our systematic review and meta-analysis evaluated the smoking status in different ways: the authors Acharya AB et al. [7] and Lu RF et al. [25] did not discuss smoking. Çetin Özdemir E et al. [1], Mishra S et al. [26], and Ustaoglu G et al. [2] studied non-smoking subjects; thus smoking was excluded as a confounder. In the study of Dogan B et al. [24], almost the entire population consisted of non-smokers, and therefore, the results were interpreted as independent of the effects of smoking. The authors Anand PS et al. [23] discussed smoking, and they performed a logistic regression model adjusted for age, gender, smoking, and body mass index. Sridharan S et al. [27] and Temelli B at al. [28] discussed smoking and found no significant differences between smokers and non-smokers. Torrungruang K et al. [29] discussed the smoking status and did not show the relation between periodontitis and the biomarkers of interest.
Michaud et al., in a review, showed that periodontitis is common in adults, and it worsens with age [45]. Ciesielska et al., in a narrative review, showed that menopausal women have a higher risk of periodontal disease [46]. In the publications selected in our review and meta-analysis, the authors Çetin Özdemir et al. [1] showed that the mean age of the individuals in the periodontitis group was higher than the other groups, and gender was significantly different. Dogan B et al. revealed a higher proportion of females in the risk factor groups and a higher age [24]. Sridharan S et al. showed that age was significantly related to red cell distribution width, but not gender [27]. Temelli B et al. found only age differences among groups [28]. No significant differences in age and gender distribution between the groups were found by Lu RF et al. [25], Mishra S et al. [26], Torrungruang K et al. [29], or Ustaoglu G et al. [2].
Our pooled results ring a bell, paving the way for future studies that could identify viable strategies for evaluating blood cell count inflammatory biomarkers for diagnostic, prognostic, and therapeutic management. Moreover, this study emphasizes that periodontitis has a repercussive potential upon systemic inflammation, being a response to bacterial infection.
4.1. Limitations and Strengths
There are several limitations of our study as well as of the included studies. The observational nature of the studies precludes any cause and effect relationship affirmations. This is further limited by the fact many of the studies were cross-sectional, a design that cannot assess the directional relation between the inflammatory biomarkers and periodontitis. Only one study assessed the effects of periodontal treatment on NLR and PLR that significantly lowered their values. There was a high heterogeneity between the results of the studies. To check the robustness of our results, we performed leave-one-out sensitivity analyses, and NLR results resisted. Furthermore, PLR became statistically significant after the removal of one study that had other comorbidities, and the heterogeneity dropped to 0. Nevertheless, for RDW, the heterogeneity remained important. For several of the outcomes, we found only a few studies to support our meta-analyses since the literature is still emerging on this topic. Concerning the methodological quality, the selected studies had two more relevant drawbacks: the representativeness of the cases was problematic since many studies did not report if all the cases in the accessible population were included in their research, and the reporting of the selection of controls, whether derived from the same population as the cases, was lacking in several studies. Nevertheless, the other quality criteria were fulfilled. Although the majority of the studies reported the classification system used to diagnose periodontitis, there was some heterogeneity between them regarding the type or the year of classification. Nevertheless, the systems used are from trusted authorities on the subject.
4.2. Study Strengths
The study’s key strength is that it primarily assessed four commonly viable non-invasive biomarkers that may be easily used in a clinical context. To the best of our knowledge, this is the first systematic review and meta-analysis on this emerging topic. Our search technique was thorough and included many medical databases, allowing us to explore the link in a systematic manner across a wide range of populations, resulting in more generalizable findings. Furthermore, the review has a robust methodology and uses a solid approach that includes sensitivity analyses and quality assessments of the selected publications.
4.3. Implications for Practice and Future Research
These inflammatory markers could be included as potential parameters to assess the impact of periodontitis on systemic health, adding to the burden of other inflammation-generating diseases. Furthermore, they could be used as prognostic markers for the evolution of the disease and the treatment efficiency assessment on a systemic level. Moreover, it would be possible to employ the inflammatory markers in a way that uses standardized values to allow for consistent periodontal disease diagnosis and severity grading. Through the creation and utilization of biological instruments to make a diagnosis and evaluate treatment outcomes, this method will serve as a key step toward the medicalization of periodontics and dentistry [47].
To gain evidence in these directions, future prospective designed studies should be endeavored.
If their role is confirmed, clinicians could better classify and monitor the disease progression and treatment efficiency with these inflammatory markers.
5. Conclusions
Our systematic review and meta-analysis found an association between NLR, LMR, and PLR and periodontitis, but not for RDW. Thus, these ratios might be thought of as emerging blood cell count inflammatory biomarkers that could shed light on the link between periodontitis and systemic disbalances, as well as for periodontitis prognosis and grading. However, because the methodological quality of the evaluated research is imperfect, the results should be used with care. Further prospective design studies are warranted.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm12060992/s1, Figure S1: Leave-one-out sensitivity analysis for neutrophils to lymphocyte ratio; Figure S2: Leave-one-out sensitivity analysis for platelet to leucocyte ratio; Figure S3: Leave-one-out sensitivity analysis for red cell distribution width; Table S1: Search strategies for each database; Table S2: Inclusion and exclusion criteria of the subjects within the original articles.
Author Contributions
Conceptualization, O.A. and D.-C.L.; methodology, D.-C.L.; software, D.-C.L.; validation, O.A. and D.-C.L.; formal analysis, D.-C.L.; investigation, O.A. and D.-C.L.; data curation, O.A. and D.-C.L.; writing-original draft preparation, O.A. and D.-C.L.; writing-review and editing, O.A., D.-C.L. and M.H.; visualization, O.A., D.-C.L. and M.H.; supervision, M.H.; project administration, O.A.; All authors have read and agreed to the published version of the manuscript.
Funding
This work was granted by project PDI-PFE-CDI 2021, entitled “Increasing the Performance of Scientific Research, Supporting Excellence in Medical Research and Innovation, PROGRES”, no. 40PFE/30.12.2021 of Iuliu Hațieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Acknowledgments
This work was granted by project PDI-PFE-CDI 2021, entitled “Increasing the Performance of Scientific Research, Supporting Excellence in Medical Research and Innovation, PROGRES”, no. 40PFE/30.12.2021.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Çetin Özdemir, E.; Bilen, E.; Yazar, F.M. Can the Delta Neutrophil Index Be Used as a Preliminary Biomarker In the Evaluation of Periodontal Disease: A Pilot Study. J. Appl. Oral Sci. 2022, 30, e20210555. [Google Scholar] [CrossRef] [PubMed]
- Ustaoglu, G.; Erdal, E.; İnanır, M. Does Periodontitis Affect Mean Platelet Volume(MPV) and Plateletcrit (PCT) Levels in Healthy Adults? Rev. Assoc. Med. Bras. 2020, 66, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Cecoro, G.; Annunziata, M.; Iuorio, M.T.; Nastri, L.; Guida, L. Periodontitis, Low-Grade Inflammation and Systemic Health: A Scoping Review. Medicina 2020, 56, 272. [Google Scholar] [CrossRef] [PubMed]
- Brum, R.S.; Duarte, P.M.; Canto, G.D.L.; Flores-Mir, C.; Benfatti, C.A.M.; Porporatti, A.L.; Zimmermann, G.S. Biomarkers in Biological Fluids in Adults with Periodontitis and/or Obesity: A Meta-Analysis. J. Indian Soc. Periodontol. 2020, 24, 191–215. [Google Scholar] [CrossRef]
- Shi, D.; Meng, H.; Xu, L.; Zhang, L.; Chen, Z.; Feng, X.; Lu, R.; Sun, X.; Ren, X. Systemic Inflammation Markers in Patients With Aggressive Periodontitis: A Pilot Study. J. Periodontol. 2008, 79, 2340–2346. [Google Scholar] [CrossRef]
- Papapanagiotou, D.; Nicu, E.A.; Bizzarro, S.; Gerdes, V.E.A.; Meijers, J.C.; Nieuwland, R.; van der Velden, U.; Loos, B.G. Periodontitis Is Associated with Platelet Activation. Atherosclerosis 2009, 202, 605–611. [Google Scholar] [CrossRef]
- Acharya, A.B.; Shetty, I.P.; Jain, S.; Padakannaya, I.; Acharya, S.; Shettar, L.; Thakur, S. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Chronic Periodontitis before and after Nonsurgical Therapy. J. Indian Soc. Periodontol. 2019, 23, 419–423. [Google Scholar] [CrossRef]
- Yamamoto, T.; Tsuneishi, M.; Furuta, M.; Ekuni, D.; Morita, M.; Hirata, Y. Relationship between Decrease of Erythrocyte Count and Progression of Periodontal Disease in a Rural Japanese Population. J. Periodontol. 2011, 82, 106–113. [Google Scholar] [CrossRef]
- Park, S.; Lee, S.J.; Shin, B.; Lee, S.J.; Kim, S.-H.; Kwon, W.C.; Kim, J.; Lee, M.K. The Association of Delta Neutrophil Index with the Prognosis of Acute Exacerbation of Chronic Obstructive Pulmonary Disease. BMC Pulm Med. 2020, 20, 47. [Google Scholar] [CrossRef]
- Loos, B.G.; Craandijk, J.; Hoek, F.J.; Wertheim-van Dillen, P.M.; van der Velden, U. Elevation of Systemic Markers Related to Cardiovascular Diseases in the Peripheral Blood of Periodontitis Patients. J. Periodontol. 2000, 71, 1528–1534. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus Report of Workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. 1), S173–S182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armitage, G.C. Development of a Classification System for Periodontal Diseases and Conditions. Ann. Periodontol. 1999, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- EndNote. Available online: https://access.clarivate.com/login?app=endnote (accessed on 29 April 2022).
- Zotero; Corporation for Digital Scholarship. Available online: https://www.zotero.org/ (accessed on 5 May 2022).
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. Ottawa Hospital Research Institute. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 29 April 2022).
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the Mean and Variance from the Median, Range, and the Size of a Sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rohatgi, A. WebPlotDigitizer. Available online: https://apps.automeris.io/wpd/ (accessed on 29 April 2022).
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- R Core Team. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to Perform a Meta-Analysis with R: A Practical Tutorial. Evid.-Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrer, M.; Pim, C.; Toshi, F.; David Daniel, E. Companion R Package for the Guide ’Doing Meta-Analysis in R; Taylor & Francis Group: Boca Ranton, FL, USA, 2019. [Google Scholar]
- Anand, P.S.; Sagar, D.K.; Ashok, S.; Kamath, K.P. Association of Aggressive Periodontitis with Reduced Erythrocyte Counts and Reduced Hemoglobin Levels. J. Periodont. Res. 2014, 49, 719–728. [Google Scholar] [CrossRef]
- Doğan, B.; Fentoğlu, Ö.; Kırzıoğlu, F.Y.; Kemer, E.S.; Köroğlu, B.K.; Aksu, O.; Çarsancaklı, S.A.; Orhan, H. Lipoxin A4 and Neutrophil/Lymphocyte Ratio: A Possible Indicator in Achieved Systemic Risk Factors for Periodontitis. Med. Sci. Monit. 2015, 21, 2485–2493. [Google Scholar] [CrossRef] [Green Version]
- Lu, R.; Li, W.; Wang, X.; Shi, D.; Meng, H. Elevated Neutrophil-to-Lymphocyte Ratio but Not Platelet-to-Lymphocyte Ratio Is Associated with Generalized Aggressive Periodontitis in a Chinese Population. J. Periodontol. 2021, 92, 507–513. [Google Scholar] [CrossRef]
- Mishra, S.; Gazala, M.P.; Rahman, W. Clinical and Diagnostic Significance of Blood Leukocyte Ratios in Young Patients with Stage III Grade C Periodontitis. Acta Odontol. Scand. 2022, 80, 161–168. [Google Scholar] [CrossRef]
- Sridharan, S.; Sravani, P.; Rao, R.J. Coefficient of Variation of Red Cell Distribution Width Has Correlations to Periodontal Inflamed Surface Area in Non-Obese Hypertensive Patients. J. Int. Acad. Periodontol. 2021, 23, 106–114. [Google Scholar]
- Temelli, B.; Yetkin Ay, Z.; Aksoy, F.; Büyükbayram, H.İ.; Kumbul Doğuç, D.; Uskun, E.; Varol, E. Platelet Indices (Mean Platelet Volume and Platelet Distribution Width) Have Correlations with Periodontal Inflamed Surface Area in Coronary Artery Disease Patients: A Pilot Study. J. Periodontol. 2018, 89, 1203–1212. [Google Scholar] [CrossRef]
- Torrungruang, K.; Ongphiphadhanakul, B.; Jitpakdeebordin, S.; Sarujikumjornwatana, S. Mediation Analysis of Systemic Inflammation on the Association between Periodontitis and Glycaemic Status. J. Clin. Periodontol. 2018, 45, 548–556. [Google Scholar] [CrossRef]
- Larmann, J.; Handke, J.; Scholz, A.S.; Dehne, S.; Arens, C.; Gillmann, H.-J.; Uhle, F.; Motsch, J.; Weigand, M.A.; Janssen, H. Preoperative Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio Are Associated with Major Adverse Cardiovascular and Cerebrovascular Events in Coronary Heart Disease Patients Undergoing Non-Cardiac Surgery. BMC Cardiovasc. Disord. 2020, 20, 230. [Google Scholar] [CrossRef]
- Lee, C.D.; Folsom, A.R.; Nieto, F.J.; Chambless, L.E.; Shahar, E.; Wolfe, D.A. White Blood Cell Count and Incidence of Coronary Heart Disease and Ischemic Stroke and Mortality from Cardiovascular Disease in African-American and White Men and Women: Atherosclerosis Risk in Communities Study. Am. J. Epidemiol. 2001, 154, 758–764. [Google Scholar] [CrossRef]
- Zhang, S.; Diao, J.; Qi, C.; Jin, J.; Li, L.; Gao, X.; Gong, L.; Wu, W. Predictive Value of Neutrophil to Lymphocyte Ratio in Patients with Acute ST Segment Elevation Myocardial Infarction after Percutaneous Coronary Intervention: A Meta-Analysis. BMC Cardiovasc. Disord. 2018, 18, 75. [Google Scholar] [CrossRef] [Green Version]
- Gkrania-Klotsas, E.; Ye, Z.; Cooper, A.J.; Sharp, S.J.; Luben, R.; Biggs, M.L.; Chen, L.-K.; Gokulakrishnan, K.; Hanefeld, M.; Ingelsson, E.; et al. Differential White Blood Cell Count and Type 2 Diabetes: Systematic Review and Meta-Analysis of Cross-Sectional and Prospective Studies. PLoS ONE 2010, 5, e13405. [Google Scholar] [CrossRef] [Green Version]
- Wan, H.; Wang, Y.; Fang, S.; Chen, Y.; Zhang, W.; Xia, F.; Wang, N.; Lu, Y. Associations between the Neutrophil-to-Lymphocyte Ratio and Diabetic Complications in Adults with Diabetes: A Cross-Sectional Study. J. Diabetes Res. 2020, 2020, 6219545. [Google Scholar] [CrossRef]
- Wang, S.-Y.; Shen, T.-T.; Xi, B.-L.; Shen, Z.; Zhang, X. Vitamin D Affects the Neutrophil-to-Lymphocyte Ratio in Patients with Type 2 Diabetes Mellitus. J. Diabetes Investig. 2021, 12, 254–265. [Google Scholar] [CrossRef]
- Kuplay, H.; Erdoğan, S.B.; Bastopcu, M.; Arslanhan, G.; Baykan, D.B.; Orhan, G. The Neutrophil-Lymphocyte Ratio and the Platelet-Lymphocyte Ratio Correlate with Thrombus Burden in Deep Venous Thrombosis. J. Vasc. Surg. Venous. Lymphat. Disord. 2020, 8, 360–364. [Google Scholar] [CrossRef]
- Isaac, V.; Wu, C.-Y.; Huang, C.-T.; Baune, B.T.; Tseng, C.-L.; McLachlan, C.S. Elevated Neutrophil to Lymphocyte Ratio Predicts Mortality in Medical Inpatients with Multiple Chronic Conditions. Medicine 2016, 95, e3832. [Google Scholar] [CrossRef]
- Stefaniuk, P.; Szymczyk, A.; Podhorecka, M. The Neutrophil to Lymphocyte and Lymphocyte to Monocyte Ratios as New Prognostic Factors in Hematological Malignancies - A Narrative Review. Cancer Manag. Res. 2020, 12, 2961–2977. [Google Scholar] [CrossRef] [PubMed]
- Mleko, M.; Pitynski, K.; Pluta, E.; Czerw, A.; Sygit, K.; Karakiewicz, B.; Banas, T. Role of Systemic Inflammatory Reaction in Female Genital Organ Malignancies - State of the Art. Cancer Manag. Res. 2021, 13, 5491–5508. [Google Scholar] [CrossRef] [PubMed]
- Musalaiah, S.V.V.S.; Anupama, M.; Nagasree, M.; Krishna, C.M.; Kumar, A.; Kumar, P.M. Evaluation of Nonsurgical Periodontal Therapy in Chronic Periodontitis Patients with Anemia by Estimating Hematological Parameters and High-Sensitivity C-Reactive Protein Levels. J. Pharm. Bioallied Sci. 2014, 6, S64–S69. [Google Scholar] [CrossRef] [PubMed]
- Naik, V.; Acharya, A.; Deshmukh, V.L.; Shetty, S.; Shirhatti, R. Generalized, Severe, Chronic Periodontitis Is Associated with Anemia of Chronic Disease: A Pilot Study in Urban, Indian Males. J. Investig. Clin. Dent. 2010, 1, 139–143. [Google Scholar] [CrossRef]
- Lappé, J.M.; Horne, B.D.; Shah, S.H.; May, H.T.; Muhlestein, J.B.; Lappé, D.L.; Kfoury, A.G.; Carlquist, J.F.; Budge, D.; Alharethi, R.; et al. Red Cell Distribution Width, C-Reactive Protein, the Complete Blood Count, and Mortality in Patients with Coronary Disease and a Normal Comparison Population. Clin. Chim. Acta 2011, 412, 2094–2099. [Google Scholar] [CrossRef]
- Leite, F.R.M.; Nascimento, G.G.; Scheutz, F.; López, R. Effect of Smoking on Periodontitis: A Systematic Review and Meta-Regression. Am. J. Prev. Med. 2018, 54, 831–841. [Google Scholar] [CrossRef]
- Larvin, H.; Kang, J.; Aggarwal, V.R.; Pavitt, S.; Wu, J. Systemic Multimorbidity Clusters in People with Periodontitis. J. Dent. Res. 2022, 220345221098910. [Google Scholar] [CrossRef]
- Michaud, D.S.; Fu, Z.; Shi, J.; Chung, M. Periodontal Disease, Tooth Loss, and Cancer Risk. Epidemiol. Rev. 2017, 39, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Ciesielska, A.; Kusiak, A.; Ossowska, A.; Grzybowska, M.E. Changes in the Oral Cavity in Menopausal Women—A Narrative Review. IJERPH 2021, 19, 253. [Google Scholar] [CrossRef]
- Khoury, W.; Glogauer, J.; Tenenbaum, H.C.; Glogauer, M. Oral Inflammatory Load: Neutrophils as Oral Health Biomarkers. J Periodontal Res. 2020, 55, 594–601. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).