Wearable Devices and Smartphone Inertial Sensors for Static Balance Assessment: A Concurrent Validity Study in Young Adult Population
Abstract
1. Introduction
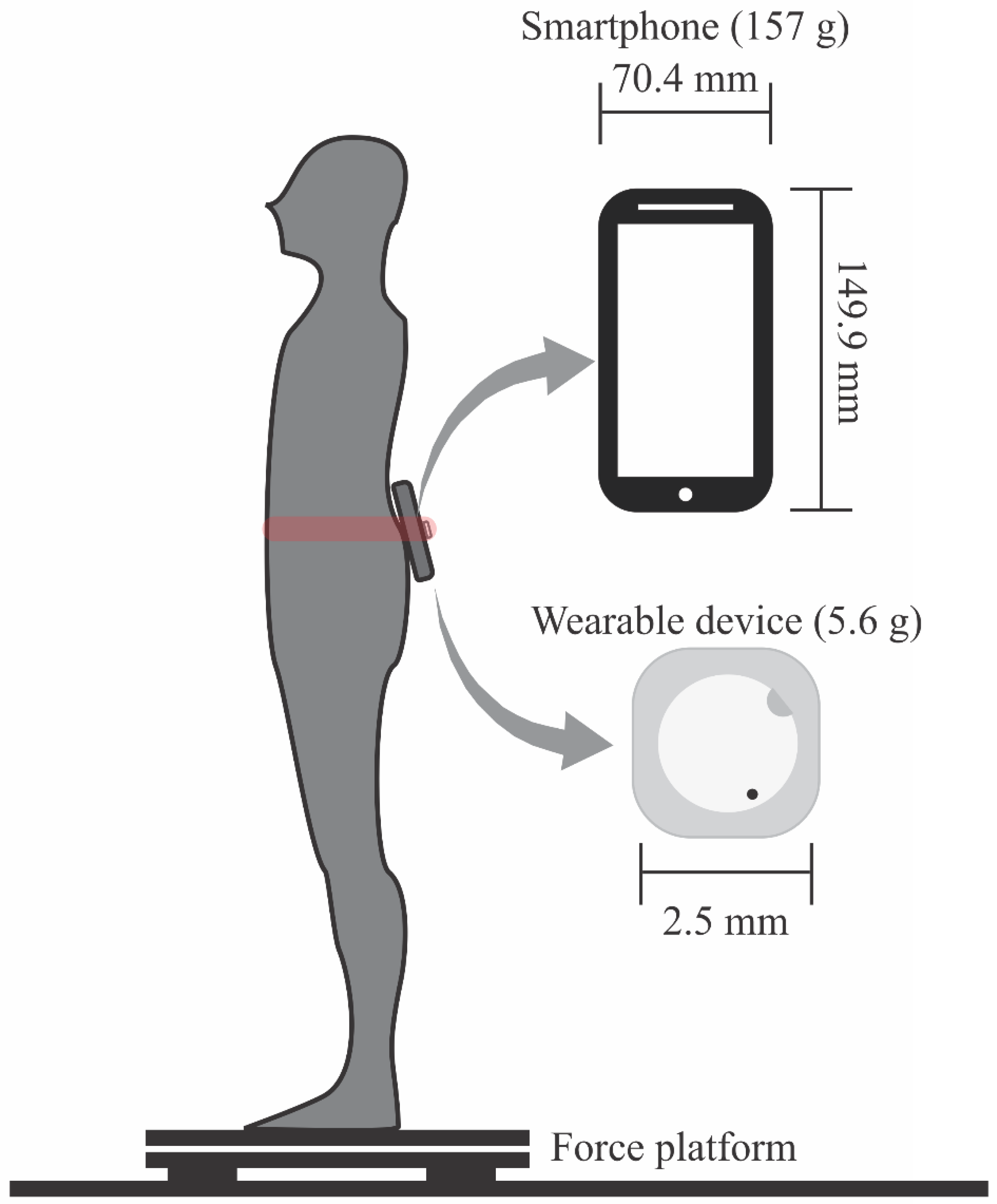
2. Materials and Methods
3. Results
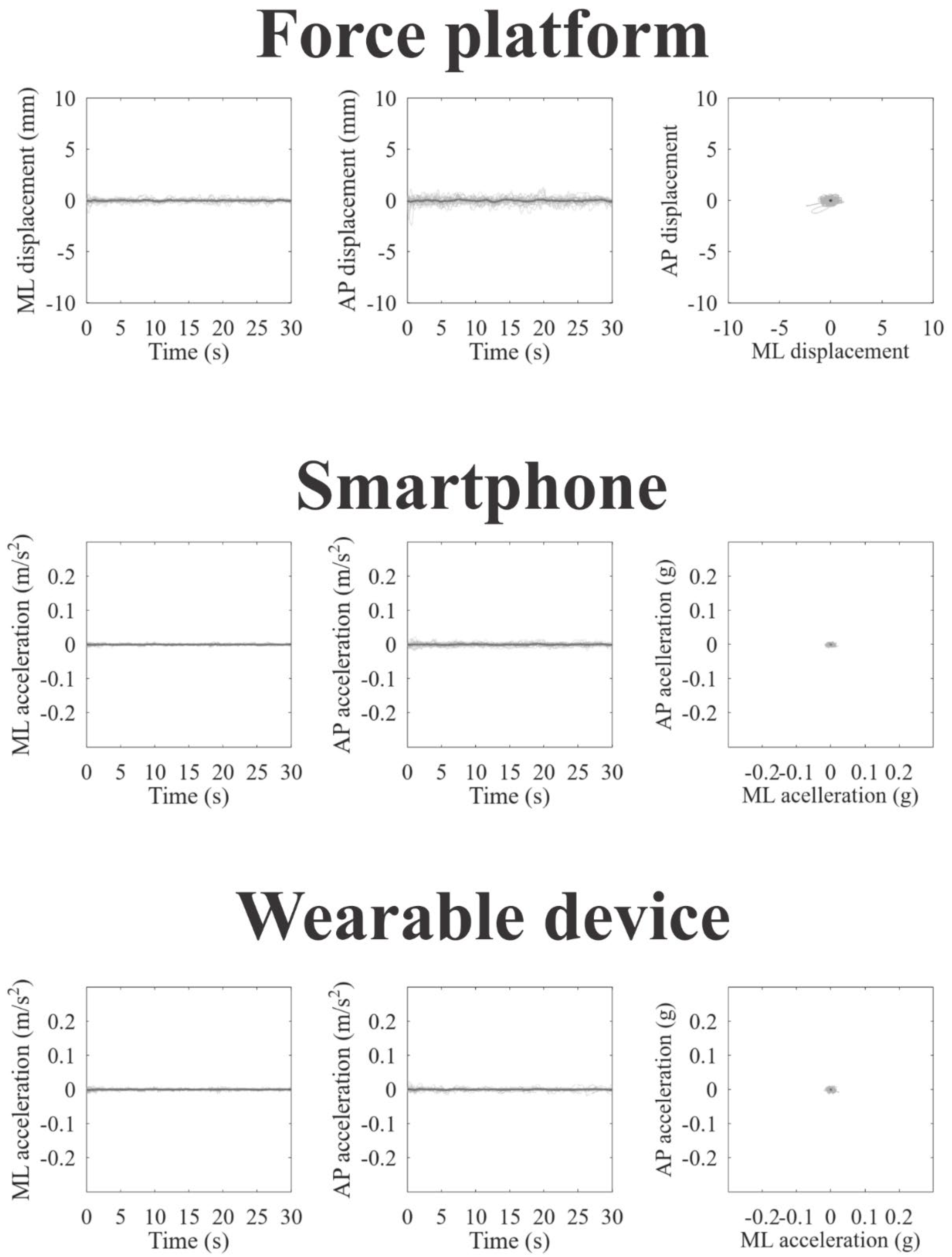
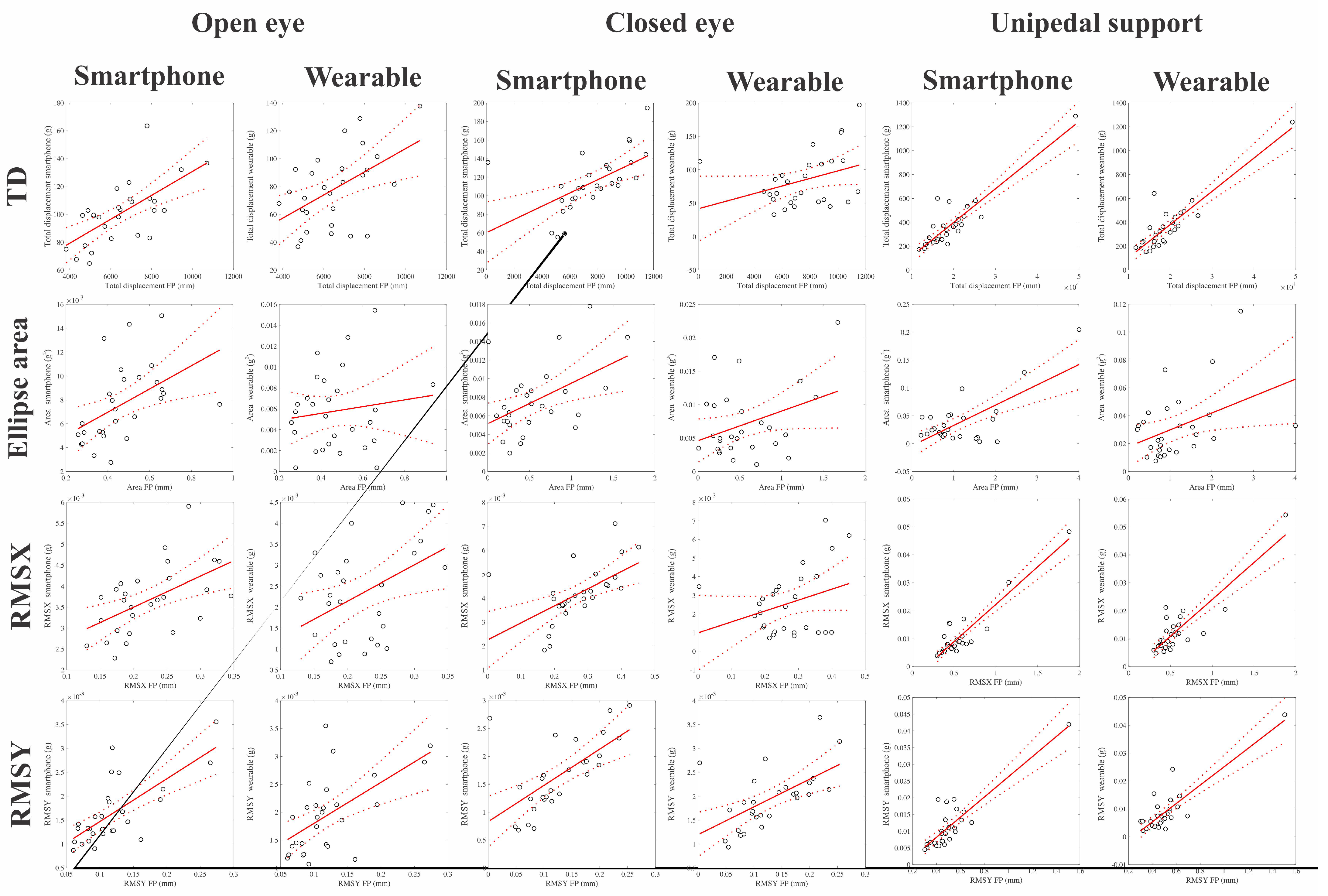
3.1. Validity Analysis
3.2. Reliability Analysis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hou, Y.R.; Chiu, Y.L.; Chiang, S.L.; Chen, H.Y.; Sung, W.H. Development of a smartphone-based balance assessment system for subjects with stroke. Sensors 2020, 20, 88. [Google Scholar] [CrossRef] [PubMed]
- Horak, F.B.; Macpherson, J.M. Postural Orientation and Equilibrium in Handbook of Physiology; New York Univ. Press: New York, NY, USA, 1995. [Google Scholar]
- Silveira, C.R.A.; Menuchi, M.R.P.; Simões, C.S.; Caetano, M.J.D.; Gobbi, L.T.B. Validade de construção em testes de equilíbrio: Ordenação cronológica na apresentação das tarefas. Rev. Bras. Cineantropometria Desempenho Hum. 2006, 8, 66–72. [Google Scholar]
- Patrício, N.A.; Rios, M.A.; Barbosa, P.C.; Ribeiro, J.R.; Vidal, D.G.; Sá, K.N.; Baptista, A.F. Balance assessment in HTLV-1 associated myelopathy or tropical spastic paraparesis. J. Braz. Soc. Trop. Med. 2020, 53, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pinho, A.S.; Salazar, A.P.; Hennig, E.M.; Spessato, B.C.; Domingo, A.; Pagnussat, A.S. Can We Rely on Mobile Devices and Other Gadgets to Assess the Postural Balance of Healthy Individuals? A Systematic Review. Sensors 2019, 19, 2972. [Google Scholar] [CrossRef] [PubMed]
- Ghislieri, M.; Gastaldi, L.; Pastorelli, S.; Tadano, S.; Agostini, V. Wearable Inertial Sensors to Assess Standing Balance: A Systematic Review. Sensors 2019, 19, 4075. [Google Scholar] [CrossRef]
- Whitney, S.L.; Roche, J.L.; Marchetti, G.F.; Lin, C.C.; Steed, D.P.; Furman, G.R.; Musolino, M.C.; Redfern, M.S. A comparison of accelerometry and center of pressure measures during computerized dynamic posturography: A measure of balance. Gait Posture 2011, 33, 594–599. [Google Scholar] [CrossRef]
- Mancini, M.; Salarian, A.; Carlson-Kuhta, P.; Zampieri, C.; King, L.; Chiari, L.; Horak, F.B. ISway: A sensitive, valid and reliable measure of postural control. J. Neuroeng. Rehabil. 2012, 9, 59. [Google Scholar] [CrossRef]
- Seimetz, C.; Tan, D.; Katayama, R.; Lockhart, T. A comparison between methods of measuring postural stability: Force plates versus accelerometers. Biomed. Sci. Instrum. 2012, 48, 386–392. [Google Scholar]
- Ozinga, S.J.; Alberts, J.L. Quantification of postural stability in older adults using mobile technology. Exp. Brain Res. 2014, 232, 3861–3872. [Google Scholar] [CrossRef]
- Patterson, J.A.; Amick, R.Z.; Pandya, P.D.; Hakansson, N.; Jorgensen, M.J. Comparison of a mobile technology application with the balance error scoring system. Int. J. Athl. Ther. Train. 2014, 19, 4–7. [Google Scholar] [CrossRef]
- Rouis, A.; Rezzoug, N.; Gorge, P. Validity of a low-cost wearable device for body sway parameter evaluation. Comp. Meth. Biomech. Biomed. Eng. 2014, 17, 182–183. [Google Scholar] [CrossRef] [PubMed]
- Alberts, J.L.; Thota, A.; Hirsch, J.; Ozinga, S.; Dey, T.; Schindler, D.D.; Koop, M.M.; Burke, D.; Linder, S.M. Quantification of the balance error scoring system with mobile technology. Med. Sci. Sports Exerc. 2015, 47, 2233–2240. [Google Scholar] [CrossRef] [PubMed]
- Abe, Y.; Sakamoto, M.; Nakazawa, R.; Shirakura, K. Relationship between joint motion and acceleration during single-leg standing in healthy male adults. J. Phys. Ther. Sci. 2015, 27, 1251–1256. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heebner, N.R.; Akins, J.S.; Lephart, S.M.; Sell, T.C. Reliability and validity of an accelerometry based measure of static and dynamic postural stability in healthy and active individuals. Gait Posture 2015, 41, 535–539. [Google Scholar] [CrossRef]
- Kosse, N.M.; Caljouw, S.; Vervoort, D.; Vuillerme, N.; Lamoth, C.J. Validity and reliability of gait and postural control analysis using the tri-axial accelerometer of the iPod touch. Ann. Biomed. Eng. 2015, 43, 1935–1946. [Google Scholar] [CrossRef]
- Neville, C.; Ludlow, C.; Rieger, B. Measuring postural stability with an inertial sensor: Validity and sensitivity. Med. Devices 2015, 8, 447–455. [Google Scholar] [CrossRef]
- Alessandrini, M.; Micarelli, A.; Viziano, A.; Pavone, I.; Costantini, G.; Casali, D.; Paolizzo, F.; Saggio, G. Body-worn triaxial accelerometer coherence and reliability related to static posturography in unilateral vestibular failure. Acta Otorhinolaryngol. Ital. 2017, 37, 231–236. [Google Scholar] [CrossRef]
- Burghart, M.; Craig, J.; Radel, J.; Huisinga, J. Reliability and validity of a mobile device application for use in sports-related concussion balance assessment. Curr. Res. Concussion 2017, 4, 1–6. [Google Scholar] [CrossRef]
- Dabbs, N.C.; Sauls, N.M.; Zayer, A.; Chander, H. Balance performance in collegiate athletes: A comparison of balance error scoring system measures. J. Funct. Morphol. Kinesiol. 2017, 2, 26. [Google Scholar] [CrossRef]
- Fiems, C.L.; Dugan, E.L.; Moore, E.S.; Combs-Miller, S.A. Reliability and validity of the Sway Balance mobile application for measurement of postural sway in people with Parkinson disease. Neurorehabilitation 2018, 43, 147–154. [Google Scholar] [CrossRef]
- Kim, K.J.; Agrawal, V.; Bennett, C.; Gaunaurd, I.; Feigenbaum, L.; Gailey, R. Measurement of lower limb segmental excursion using inertial sensors during single limb stance. J. Biomech. 2018, 71, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, K.L.; Roach, K.L.; Wajda, D.A.; Sosnoff, J.J. Smartphone technology can measure postural stability and discriminate fall risk in older adults. Gait Posture 2019, 67, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Scoppa, F.; Capra, R.; Gallamini, M.; Shiffer, R. Clinical stabilometry standardization. Gait Posture 2013, 37, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Goldie, P.A.; Bach, T.M.; Evans, O.M. Force platform measures for evaluating postural control: Reliability and validity. Arch. Phys. Med. Rehabil. 1989, 70, 510–517. [Google Scholar] [PubMed]
- Chowdhury, A.; Kanetkar, M. Determination of Most Preferred Mobile Phone Size Based on Hand Anthropometry and Mobile Handiness. In Research into Design for Communities; Chakrabarti, A., Chakrabarti, D., Eds.; ICoRD 2017. Smart Innovation, Systems and Technologies, vol 65; Springer: Singapore, 2017; Volume 1. [Google Scholar] [CrossRef]
- Duarte, M.B.; da Costa Moraes, A.A.; Ferreira, E.V.; da Silva Almeida, G.C.; da Rocha Santos, E.G.; Pinto, G.H.L.; de Oliveira, P.R.; Amorim, C.F.; Dos Santos Cabral, A.; Saunier, G.; et al. Validity and reliability of a smartphone-based assessment for anticipatory and compensatory postural adjustments during predictable perturbations. Gait Posture 2022, 96, 9–17. [Google Scholar] [CrossRef] [PubMed]
- da Costa Moraes, A.A.; Duarte, M.B.; Ferreira, E.V.; da Silva Almeida, G.C.; da Rocha Santos, E.G.; Pinto, G.H.L.; de Oliveira, P.R.; Amorim, C.F.; Cabral, A.D.S.; de Athayde Costa E Silva, A.; et al. Validity and Reliability of Smartphone App for Evaluating Postural Adjustments during Step Initiation. Sensors 2022, 22, 2935. [Google Scholar] [CrossRef]
- Maki, B.E.; Holliday, P.J.; Topper, A.K. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J. Gerontol. 1994, 49, M72–M84. [Google Scholar] [CrossRef]
- Piirtola, M.; Era, P. Force platform measurements as predictors of falls among older people—A review. Gerontology 2006, 52, 1–16. [Google Scholar] [CrossRef]
- Merlo, A.; Zemp, D.; Zanda, E.; Rocchi, S.; Meroni, F.; Tettamanti, M.; Recchia, A.; Lucca, U.; Quadri, P. Postural stability and history of falls in cognitively able older adults: The Canton Ticino study. Gait Posture 2012, 36, 662–666. [Google Scholar] [CrossRef]
- Faber, L.M.; Moreira, L.A.; Scheicher, M.E. Comparison of static balance and mobility between nursing home residents and community-dwelling elderly. Man. Ther. Posturology Rehabil. J. 2019, 17, 749. [Google Scholar] [CrossRef]
- Duarte, M. Análise Estabilográfica da Postura Ereta Humana Quase Estática; Univ. São Paulo: São Paulo, Brazil, 2000. [Google Scholar]
- Cohen, L.; Holliday, M. Statistics for Social Sciences; Harper & How: London, UK, 1982. [Google Scholar]
- Telles, G.F.; Ferreira, A.S.; Junior, P.; Lemos, T.; Bittencourt, J.V.; Nogueira, L. Concurrent validity of the inertial sensors for assessment of balance control during quiet standing in patients with chronic low back pain and asymptomatic individuals. J. Med. Eng. Technol. 2022, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Roeing, K.L.; Hsieh, K.L.; Sosnoff, J.J. A systematic review of balance and fall risk assessments with mobile phone technology. Arch. Gerontol. Geriatr. 2017, 73, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Al-Amri, M.; Nicholas, K.; Button, K.; Sparkes, V.; Sheeran, L.; Davies, J.L. Inertial measurement units for clinical movement analysis: Reliability and Concurrent Validity. Sensors 2018, 18, 719. [Google Scholar] [CrossRef] [PubMed]


| Reference | Inertial Sensor (AR Hz) | Recording Duration | Gold-Standard Instrument |
|---|---|---|---|
| Whitney et al. (2011) [7] | Wearable (100 Hz) | 90 s | Force platform |
| Mancini et al. (2012) [8] | Wearable (50 Hz) | 30 min | Force Platform |
| Seimetz et al. (2012) [9] | Wearable (n.i.) | 90 s | Force platform |
| Ozinga et al. (2014) [10] | iPad 3 (100 Hz) | 60 s | Motion capture |
| Patterson et al. (2014) [11] | iPod touch (60 Hz) | 20 s | Balance Error Scoring System |
| Rouis et al. (2014) [12] | Wearable (50 Hz) | 30 s | Force platform |
| Alberts et al. (2015) [13] | iPad (100 Hz) | 20 s | Motion capture |
| Abe et al. (2015) [14] | Wearable (50 Hz) | 30 s | Motion capture |
| Heebner et al. (2015) [15] | Wearable (1000 Hz) | 30 min | Force platform |
| Kosse et al. (2015) [16] | iPod touch (88–92 Hz) | 60 s | Wearable |
| Neville et al. (2015) [17] | Wearable (250 Hz) | 30 s | Motion capture, force platform |
| Alessandrini et al. (2017) [18] | Wearable (25 Hz) | 60 s | Force Platform |
| Burghart et al. (2017) [19] | iPod Touch (10 Hz) | 60 s | Force platform |
| Dabbs et al. (2017) [20] | Iphone (n.i.) | 10 s | Force platform |
| Fiems et al. (2018) [21] | iPod Touch (60 Hz) | 1 h | Fall protocol and Modified Clinical, Test of Sensory Integration and Balance Protocol |
| Kim et al. (2018) [22] | Wearable (50 Hz) | 30 s | Motion capture |
| Hsieh et al. (2019) [23] | Smartphone (200 Hz) | 30 s | Force Platform |
| Parameter | Force Platform | Smartphone | MetaMotionC® | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Open eyes | ||||||
| TD | 6443.88 | 1701.04 | 98.12 | 18.6 | 74.54 | 24.53 |
| AREA | 0.47 | 0.16 | 0.0076 | 0.0032 | 0.0054 | 0.0036 |
| RMSX | 0.22 | 0.06 | 0.0036 | 0.0006 | 0.0022 | 0.0011 |
| RMSY | 0.12 | 0.05 | 0.0016 | 0.0006 | 0.0019 | 0.0006 |
| Closed eyes | ||||||
| TD | 7324.83 | 2420.43 | 109.41 | 26.39 | 77.49 | 32.21 |
| AREA | 0.54 | 0.37 | 0.0073 | 0.0037 | 0.0061 | 0.0038 |
| RMSX | 0.26 | 0.09 | 0.004 | 0.001 | 0.0023 | 0.0014 |
| RMSY | 0.12 | 0.06 | 0.0016 | 0.0006 | 0.0019 | 0.0006 |
| Unipedal support | ||||||
| TD | 19575.9 | 7073.5 | 383.08 | 222.02 | 365.69 | 221.91 |
| AREA | 1.17 | 0.8519 | 0.0384 | 0.0444 | 0.0317 | 0.0246 |
| RMSX | 0.59 | 0.316 | 0.0111 | 0.0093 | 0.0131 | 0.01 |
| RMSY | 0.52 | 0.2239 | 0.0118 | 0.0077 | 0.0091 | 0.0086 |
| Correlation | Smartphone | p-Value | MetaMotionC | p-Value |
|---|---|---|---|---|
| Open eyes | ||||
| TD | 0.65 (0.99) | 0.0001 * | 0.51 (0.75) | 0.0087 * |
| AREA | 0.49 (0.75) | 0.0105 * | 0.14 | 0.5631 |
| RMSX | 0.54 (0.82) | 0.0041 * | 0.44 (0.62) | 0.0238 * |
| RMSY | 0.72 (0.99) | 0.0001 * | 0.58 (0.88) | 0.0024 * |
| Closed eyes | ||||
| TD | 0.57 (0.68) | 0.0161 * | 0.35 | 0.478 |
| AREA | 0.49 | 0.0565 | 0.36 | 0.3234 |
| RMSX | 0.57 (0.7) | 0.0124 * | 0.32 | 0.5053 |
| RMSY | 0.63 (0.9) | 0.0015 * | 0.58 (0.82) | 0.0045 * |
| Unipedal support | ||||
| TD | 0.91 (0.99) | 0.0001 * | 0.90 (0.99) | 0.0001 * |
| AREA | 0.70 (0.99) | 0.0001 * | 0.42 (0.57) | 0.0339 * |
| RMSX | 0.93 (0.99) | 0.0001 * | 0.87 (0.99) | 0.0001 * |
| RMSY | 0.87 (0.99) | 0.0001 * | 0.86 (0.99) | 0.0001 * |
| Parameter | Open Eyes | Closed Eyes | Unipedal Support |
|---|---|---|---|
| Force platform | |||
| TD | 0.46 (0.14) | −0.15 (0.6) | 0.54 (0.06) |
| AREA | 0.54 (0.08) | 0.12 (0.38) | 0.32 (0.26) |
| RMSX | 0.59 (0.07) | 0.16 (0.37) | 0.31 (0.23) |
| RMSY | 0.2 (0.34) | 0.2 (0.36) | 0.47 (0.08) |
| Smartphone | |||
| TD | 0.22 (0.34) | 0.81 (0.003) | 0.3 (0.25) |
| AREA | −0.15 (0.6) | 0.32 (0.22) | −0.01 (0.51) |
| RMSX | 0.36 (0.21) | 0.91 (0.001) | 0.1 (0.42) |
| RMSY | 0.18 (0.37) | 0.47 (0.14) | 0.34 (0.21) |
| Wearable device | |||
| TD | −0.1 (0.59) | 0.47 (0.03) | 0.43 (0.17) |
| AREA | −0.23 (0.64) | 0.13 (0.4) | 0.17 (0.38) |
| RMSX | 0.005 (0.49) | 0.2 (0.2) | 0.18 (0.32) |
| RMSY | 0.59 (0.07) | 0.58 (0.07) | 0.25 (0.32) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, L.A.; Santos, E.G.R.; Santos, P.S.A.; Igarashi, Y.; Oliveira, L.K.R.; Pinto, G.H.L.; Santos Lobato, B.L.; Cabral, A.S.; Belgamo, A.; Costa e Silva, A.A.; et al. Wearable Devices and Smartphone Inertial Sensors for Static Balance Assessment: A Concurrent Validity Study in Young Adult Population. J. Pers. Med. 2022, 12, 1019. https://doi.org/10.3390/jpm12071019
Rodrigues LA, Santos EGR, Santos PSA, Igarashi Y, Oliveira LKR, Pinto GHL, Santos Lobato BL, Cabral AS, Belgamo A, Costa e Silva AA, et al. Wearable Devices and Smartphone Inertial Sensors for Static Balance Assessment: A Concurrent Validity Study in Young Adult Population. Journal of Personalized Medicine. 2022; 12(7):1019. https://doi.org/10.3390/jpm12071019
Chicago/Turabian StyleRodrigues, Luciana Abrantes, Enzo Gabriel Rocha Santos, Patrícia Seixas Alves Santos, Yuzo Igarashi, Luana Karine Resende Oliveira, Gustavo Henrique Lima Pinto, Bruno Lopes Santos Lobato, André Santos Cabral, Anderson Belgamo, Anselmo Athayde Costa e Silva, and et al. 2022. "Wearable Devices and Smartphone Inertial Sensors for Static Balance Assessment: A Concurrent Validity Study in Young Adult Population" Journal of Personalized Medicine 12, no. 7: 1019. https://doi.org/10.3390/jpm12071019
APA StyleRodrigues, L. A., Santos, E. G. R., Santos, P. S. A., Igarashi, Y., Oliveira, L. K. R., Pinto, G. H. L., Santos Lobato, B. L., Cabral, A. S., Belgamo, A., Costa e Silva, A. A., Callegari, B., & Souza, G. S. (2022). Wearable Devices and Smartphone Inertial Sensors for Static Balance Assessment: A Concurrent Validity Study in Young Adult Population. Journal of Personalized Medicine, 12(7), 1019. https://doi.org/10.3390/jpm12071019