How the First Year of the COVID-19 Pandemic Impacted Patients’ Hospital Admission and Care in the Vascular Surgery Divisions of the Southern Regions of the Italian Peninsula
Abstract
:1. Introduction
2. Materials and Methods
- (1)
- open repair or endovascular aneurysm repair (EVAR) for asymptomatic abdominal aortic aneurysm (AAA);
- (2)
- open repair or EVAR for primary ruptured or symptomatic AAA;
- (3)
- duplex or computed-tomography scans performed for post-EVAR surveillance;
- (4)
- Previous EVAR treated again (in an open or endovascular fashion) for recurring symptomatic or ruptured AAA, or for endoleak at risk of AAA rupture (type 1, 3, or 2 with sac expansion);
- (5)
- open, or endovascular treatments for thrombotic, non-embolic, acute lower limb ischemia;
- (6)
- treatments for Rutherford category 3 peripheral arterial disease (R3-PAD) in socially active patients with very short distance intermittent claudication (less than 50 mt. on the flat), not responsive to best medical therapy, and asking for a resolutive treatment to improve their lifestyle;
- (7)
- open or endovascular revascularizations for chronic limb-threatening ischemia (CLTI);
- (8)
- CLTI patients who have had a thigh or leg amputated;
- (9)
- open or endovascular revascularizations for asymptomatic severe internal carotid artery (ICA) stenosis;
- (10)
- Asymptomatic severe ICA stenosis on surgical waiting list, complicated to total obstruction (with or without neurological symptoms);
- (11)
- symptomatic ICA stenosis operated in urgency;
- (12)
- conservative or surgical treatments for venous ulcers;
- (13)
- diagnosis of deep vein thrombosis (DVT), also from requests of consultation from the emergency room or any medical/surgical divisions.
3. Results
4. Discussion
- −
- Prophylactic ICA revascularization during each month of the pandemic compared to the prior year, as well as during the first two months of the pandemic compared to the prior two months;
- −
- Imaging for post-EVAR surveillance from April to June, 2020 compared to the corresponding time-period in 2019, as well as during the first two months of the pandemic (March–April, 2020) in comparison with the two months before it (January–February, 2020);
- −
- Treatment for R3-PAD during the first two months of the pandemic in comparison with the two prior months, and in April 2020 and January 2021 when compared with the corresponding month of the previous year.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gupta, R.; Mouawad, N.J.; Yi, J.A. The impact of the COVID-19 pandemic on vascular surgery: Health care systems, economic, and clinical implications. Semin. Vasc. Surg. 2021, 34, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Schuivens, P.M.; Buijs, M.; Winter, L.B.-D.; Veen, E.J.; de Groot, H.G.; Buimer, T.G.; Ho, G.H.; van der Laan, L. Impact of the COVID-19 Lockdown Strategy on Vascular Surgery Practice: More Major Amputations than Usual. Ann. Vasc. Surg. 2020, 69, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Pini, R.; Faggioli, G.; Vacirca, A.; Gallitto, E.; Mascoli, C.; Attard, L.; Viale, P.; Gargiulo, M. Is it Possible to Safely Maintain a Regular Vascular Practice During the COVID-19 Pandemic? Eur. J. Vasc. Endovasc. Surg. 2020, 60, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Musajee, M.; Biasi, L.; Thulasidasan, N.; Green, M.; Francia, F.; Arissol, M.; Lakhani, A.; Thomas, S.; Patel, S.; Zayed, H. The Impact of the COVID-19 Pandemic on the Workload, Case Mix and hospital Resources at a Tertiary Vascular Unit. Ann. Vasc. Surg. 2022, 80, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Mouawad, N.J.; Woo, K.; Malgor, R.D.; Wohlauer, M.V.; Johnson, A.P.; Cuff, R.F.; Coleman, D.M.; Coogan, S.M.; Sheahan, M.G., 3rd; Shalhub, S. The impact of the COVID-19 pandemic on vascular surgery practice in the United States. J. Vasc. Surg. 2021, 73, 772–779.e4. [Google Scholar] [CrossRef] [PubMed]
- Leong Tan, G.W.; Chandrasekar, S.; Lo, Z.J.; Hong, Q.; Yong, E.; Lingam, P.; Zhang, L.; Quek, L.H.H.; Pua, U. Early experience in the COVID-19 pandemic from a vascular surgery unit in a Singapore tertiary hospital. J. Vasc. Surg. 2020, 72, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Sigvant, B.; Lundin, F.; Wahlberg, E. The Risk of Disease Progression in Peripheral Arterial Disease is Higher than Expected: A Meta-Analysis of Mortality and Disease Progression in Peripheral Arterial Disease. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 395–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mouawad, N.J.; Cuff, R.F.; Hultgren, R.; Chuen, J.; Galeazzi, E.; Wohlauer, M. The Vascular Surgery COVID-19 Collaborative (VASCC). J. Vasc. Surg. 2020, 72, 379–380. [Google Scholar] [CrossRef] [PubMed]
- D’Oria, M.; Sr Mills, J.L.; Cohnert, T.; Oderich, G.S.; Hultgren, R.; Lepidi, S. Vascular Surgery COVID-19 Collaborative (VASCC). The “Vascular Surgery COVID-19 Collaborative” (VASCC). Eur. J. Vasc. Endovasc. Surg. 2020, 60, 489–490. [Google Scholar] [PubMed]
- Etkin, Y.; Conway, A.M.; Silpe, J.; Qato, K.; Carroccio, A.; Manvar-Singh, P.; Giangola, G.; Deitch, J.S.; Davila-Santini, L.; Schor, J.A.; et al. Acute Arterial Thromboembolism in Patients with COVID-19 in the New York City Area. Ann. Vasc. Surg. 2021, 70, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Attisani, L.; Pucci, A.; Luoni, G.; Luzzani, L.; Pegorer, M.A.; Settembrini, A.M.; Bissacco, D.; Wohlauer, M.V.; Piffaretti, G.; Bellosta, R. COVID-19 and acute limb ischemia: A systematic review. J. Cardiovasc. Surg. 2021, 62, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Canale, M.P.; Menghini, R.; Martelli, E.; Federici, M. COVID-19-Associated Endothelial Dysfunction and Microvascular Injury: From Pathophysiology to Clinical Manifestations. Card Electrophysiol. Clin. 2022, 14, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Ho, V.T.; Eberhard, A.V.; Asch, S.M.; Leeper, N.J.; Fukaya, E.; Arya, S.; Ross, E.G. US National Trends in Vascular Surgical Practice during the COVID-19 Pandemic. JAMA Surg. 2021, 156, 681–683. [Google Scholar] [CrossRef] [PubMed]

| a. The pre-COVID period. | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time Period→ | April 2019 | May 2019 | June 2019 | July 2019 | August 2019 | September 2019 | October 2019 | November 2019 | December 2019 | January 2020 | February 2020 |
| Questions ↓ | |||||||||||
| #1 | 99 | 108 | 93 | 94 | 45 | 102 | 125 | 120 | 105 | 102 | 90 |
| #2 | 184 | 182 | 192 | 159 | 77 | 173 | 197 | 175 | 145 | 162 | 155 |
| #3 | 16 | 12 | 14 | 10 | 6 | 16 | 11 | 10 | 11 | 11 | 10 |
| #4 | 171 | 180 | 152 | 153 | 88 | 162 | 166 | 179 | 150 | 175 | 128 |
| #5 | 47 | 45 | 53 | 51 | 40 | 53 | 53 | 58 | 55 | 59 | 49 |
| #6 | 57 | 71 | 67 | 68 | 53 | 58 | 85 | 75 | 54 | 67 | 52 |
| #7 | 87 | 90 | 82 | 77 | 76 | 79 | 97 | 86 | 79 | 96 | 77 |
| #8 | 162 | 180 | 188 | 183 | 99 | 189 | 190 | 207 | 160 | 164 | 158 |
| #9 | 16 | 21 | 12 | 12 | 15 | 19 | 18 | 30 | 32 | 18 | 17 |
| #10 | 46 | 169 | 165 | 145 | 108 | 151 | 159 | 166 | 136 | 141 | 136 |
| #11 | 44 | 48 | 45 | 41 | 40 | 36 | 38 | 32 | 34 | 34 | 37 |
| #12 | 0 | 1 | 2 | 0 | 0 | 2 | 1 | 0 | 1 | 0 | 1 |
| #13 | 18 | 9 | 14 | 15 | 8 | 20 | 20 | 22 | 14 | 16 | 13 |
| b. The COVID-19 period. | |||||||||||
| Time Period→ | March 2020 | April 2020 | May 2020 | June 2020 | July 2020 | August 2020 | September 2020 | October 2020 | November 2020 | December 2020 | January 2021 |
| Questions ↓ | |||||||||||
| #1 | 69 | 53 | 58 | 73 | 81 | 52 | 97 | 109 | 87 | 81 | 85 |
| #2 | 67 | 50 | 69 | 115 | 131 | 76 | 149 | 149 | 142 | 133 | 144 |
| #3 | 5 | 5 | 8 | 11 | 10 | 8 | 14 | 9 | 8 | 7 | 6 |
| #4 | 79 | 47 | 78 | 125 | 118 | 80 | 153 | 147 | 113 | 98 | 92 |
| #5 | 41 | 44 | 37 | 45 | 37 | 42 | 47 | 42 | 38 | 38 | 44 |
| #6 | 32 | 25 | 47 | 61 | 68 | 41 | 67 | 48 | 61 | 43 | 61 |
| #7 | 63 | 67 | 71 | 91 | 86 | 71 | 86 | 85 | 68 | 70 | 76 |
| #8 | 66 | 52 | 90 | 124 | 124 | 66 | 126 | 144 | 115 | 93 | 87 |
| #9 | 14 | 14 | 22 | 21 | 18 | 16 | 24 | 23 | 15 | 18 | 15 |
| #10 | 90 | 89 | 121 | 138 | 152 | 92 | 160 | 171 | 142 | 139 | 142 |
| #11 | 31 | 43 | 36 | 41 | 44 | 36 | 44 | 38 | 42 | 31 | 44 |
| #12 | 4 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 2 | 0 | 0 |
| #13 | 12 | 12 | 19 | 11 | 21 | 15 | 16 | 18 | 23 | 18 | 13 |
| Activities | April/ December 2019 (no COVID) (n = 9161) n (%) | April/ December 2020 (COVID) (n = 7092) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 891 (9.73) | 691 (9.74) | 1.00 | −22.45 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 175 (1.91) | 171 (2.41) | 0.03 | −2.29 |
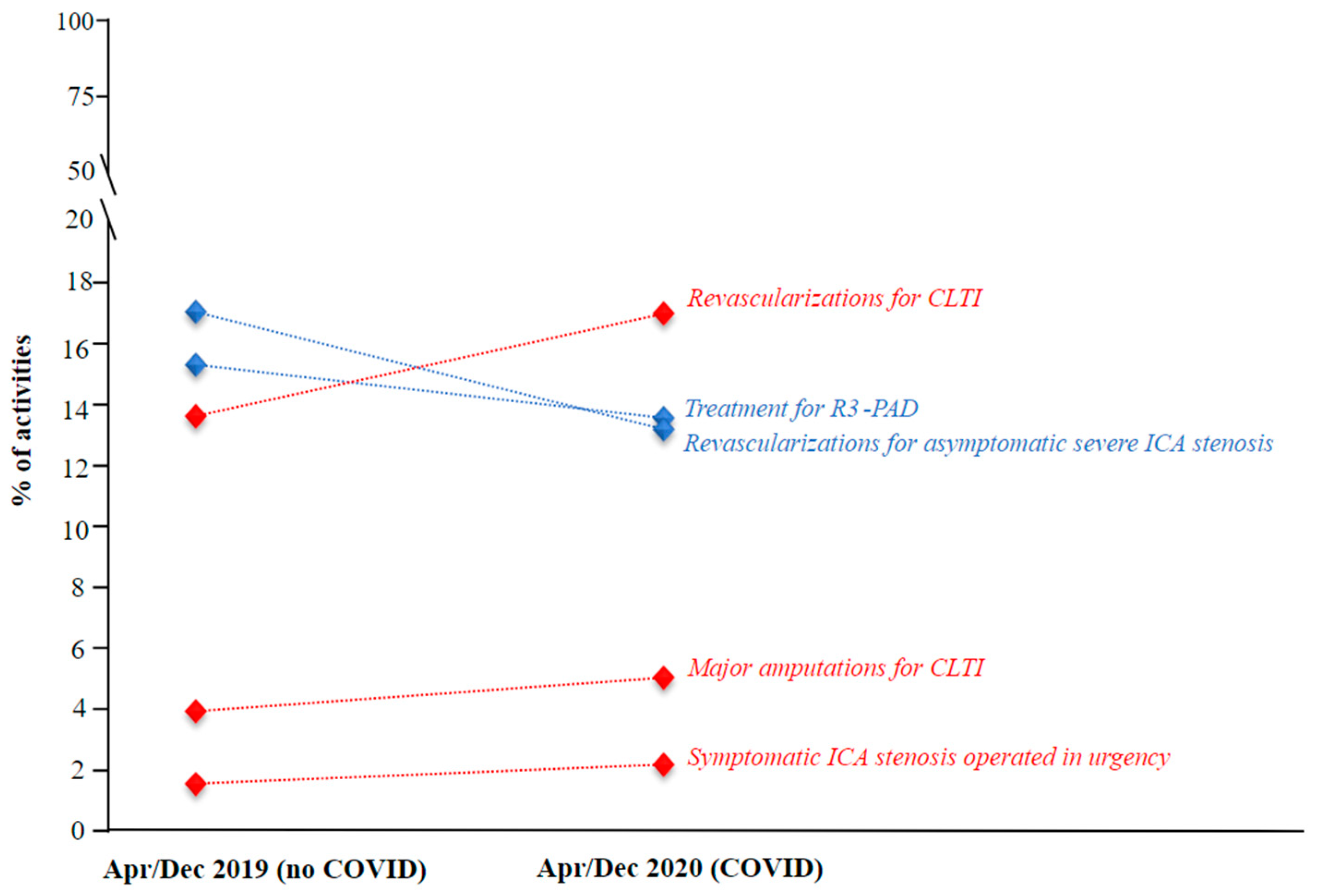
| #3 | Post-EVAR surveillance | 1484 (16.2) | 1014 (14.3) | 0.0009 | −31.67 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 106 (1.16) | 80 (1.13) | 0.55 | −24.53 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 455 (4.97) | 370 (5.22) | 0.57 | −18.68 |
| #6 | Treatment for R3-PAD | 1401 (15.29) | 959 (13.52) | 0.0006 | −31.55 |
| #7 | Revascularizations for CLTI | 1245 (13.59) | 1204 (16.98) | <0.0001 | −3.29 |
| #8 | Major amputations for CLTI | 358 (3.91) | 355 (5.01) | 0.0007 | −0.84 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 1558 (17.01) | 934 (13.17) | <0.0001 | −40.05 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 7 (0.08) | 5 (0.07) | 0.91 | −28.57 |
| #11 | Symptomatic ICA stenosis operated in urgency | 140 (1.53) | 153 (2.16) | 0.0009 | 9.29 |
| #12 | Treatment for venous ulcers | 588 (6.42) | 461 (6.5) | 0.80 | −21.60 |
| #13 | Diagnosis of deep vein thrombosis | 753 (8.22) | 695 (9.8) | 0.0004 | −7.70 |
| Activities | April 2019 (no COVID) (n = 947) n (%) | April 2020 (COVID) (n = 501) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 99 (10.45) | 53 (10.58) | 0.91 | −46.46 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 16 (1.69) | 14 (2.79) | 0.16 | −12.50 |
| #3 | Post-EVAR surveillance | 184 (19.43) | 50 (9.98) | <0.0001 | −72.83 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 16 (1.69) | 5 (1) | 0.006 | −68.75 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 47 (4.96) | 44 (8.78) | 0.005 | −6.38 |
| #6 | Treatment for R3-PAD | 171 (18.06) | 47 (9.38) | <0.0001 | −72.51 |
| #7 | Revascularizations for CLTI | 46 (4.86) | 89 (17.76) | <0.0001 | 93.48 |
| #8 | Major amputations for CLTI | 44 (4.65) | 43 (8.58) | 0.002 | −2.27 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 162 (17.11) | 52 (10.38) | 0.0006 | −67.90 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 0 (0) | 0 (0) | - | - |
| #11 | Symptomatic ICA stenosis operated in urgency | 18 (1.9) | 12 (2.4) | 0.52 | −33.33 |
| #12 | Treatment for venous ulcers | 57 (6.02) | 25 (4.99) | 0.43 | −56.14 |
| #13 | Diagnosis of deep vein thrombosis | 87 (9.19) | 67 (13.37) | 0.01 | −22.99 |
| Activities | May–June 2019 (no COVID) (n = 2195) n (%) | May–June 2020 (COVID) (n = 1513) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 201 (9.16) | 131 (8.66) | 0.60 | −34.83 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 33 (1.5) | 43 (2.84) | 0.006 | 30.30 |
| #3 | Post-EVAR surveillance | 374 (17.04) | 184 (12.16) | 0.0001 | −50.80 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 26 (1.18) | 19 (1.26) | 0.79 | −26.92 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 98 (4.46) | 82 (5.42) | 0.21 | −16.33 |
| #6 | Treatment for R3-PAD | 332 (15.13) | 203 (13.42) | 0.15 | −38.86 |
| #7 | Revascularizations for CLTI | 334 (15.22) | 259 (17.12) | 0.12 | −22.46 |
| #8 | Major amputations for CLTI | 93 (4.24) | 77 (5.09) | 0.20 | −17.20 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 368 (16.77) | 214 (14.14) | 0.03 | −41.85 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 3 (0.14) | 1 (0.07) | 1.00 | −66.67 |
| #11 | Symptomatic ICA stenosis operated in urgency | 23 (1.05) | 30 (1.98) | 0.01 | 30.43 |
| #12 | Treatment for venous ulcers | 138 (6.29) | 108 (7.14) | 0.34 | −21.74 |
| #13 | Diagnosis of deep vein thrombosis | 172 (7.84) | 162 (10.71) | 0.002 | −5.81 |
| Activities | July–August 2019 (no COVID) (n = 1663) n (%) | July–August 2020 (COVID) (n = 1485) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 139 (8.36) | 133 (8.96) | 0.55 | −4.32 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 27 (1.62) | 34 (2.29) | 0.15 | 25.93 |
| #3 | Post-EVAR surveillance | 236 (14.19) | 207 (13.94) | 0.81 | −12.29 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 16 (0.96) | 18 (1.21) | 0.59 | 12.50 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 91 (5.47) | 79 (5.32) | 0.80 | −13.19 |
| #6 | Treatment for R3-PAD | 241 (14.49) | 198 (13.33) | 0.33 | −17.84 |
| #7 | Revascularizations for CLTI | 253 (15.21) | 244 (16.43) | 0.36 | −3.56 |
| #8 | Major amputations for CLTI | 81 (4.87) | 80 (5.39) | 0.53 | −1.23 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 282 (16.96) | 190 (12.79) | 0.001 | −32.62 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 0 (0) | 0 (0) | - | - |
| #11 | Symptomatic ICA stenosis operated in urgency | 23 (1.38) | 36 (2.42) | 0.04 | 56.52 |
| #12 | Treatment for venous ulcers | 121 (7.28) | 109 (7.34) | 1.00 | −9.92 |
| #13 | Diagnosis of deep vein thrombosis | 153 (9.2) | 157 (10.57) | 0.19 | 2.61 |
| Activities | September/ October 2019 (no COVID) (n = 2220) n (%) | September/ October 2020 (COVID) (n = 1968) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 227 (10.23) | 206 (10.47) | 0.75 | −9.25 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 37 (1.67) | 47 (2.39) | 0.11 | 27.03 |
| #3 | Post-EVAR surveillance | 370 (16.67) | 298 (15.14) | 0.16 | −19.46 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 27 (1.22) | 23 (1.17) | 1.00 | −14.81 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 106 (4.77) | 89 (4.52) | 0.65 | −16.04 |
| #6 | Treatment for R3-PAD | 328 (14.77) | 300 (15.24) | 0.72 | −8.54 |
| #7 | Revascularizations for CLTI | 310 (13.96) | 331 (16.82) | 0.01 | 6.77 |
| #8 | Major amputations for CLTI | 74 (3.33) | 82 (4.17) | 0.12 | 10.81 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 379 (17.07) | 270 (13.72) | 0.002 | −28.76 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 3 (0.14) | 2 (0.1) | 1.00 | −33.33 |
| #11 | Symptomatic ICA stenosis operated in urgency | 40 (1.8) | 34 (1.73) | 0.81 | −15.00 |
| #12 | Treatment for venous ulcers | 143 (6.44) | 115 (5.84) | 0.42 | −19.58 |
| #13 | Diagnosis of deep vein thrombosis | 176 (7.93) | 171 (8.69) | 0.35 | −2.84 |
| Activities | November/ December 2019 (no COVID) (n = 2136) n (%) | November/ December 2020 (COVID) (n = 1625) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 225 (10.53) | 168 (10.34) | 0.84 | −25.33 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 62 (2.9) | 33 (2.03) | 0.08 | −46.77 |
| #3 | Post-EVAR surveillance | 320 (14.98) | 275 (16.92) | 0.11 | −14.06 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 21 (0.98) | 15 (0.92) | 0.75 | −28.57 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 113 (5.29) | 76 (4.68) | 0.4 | −32.74 |
| #6 | Treatment for R3-PAD | 329 (15.4) | 211 (12.98) | 0.04 | −35.87 |
| #7 | Revascularizations for CLTI | 302 (14.14) | 281 (17.29) | 0.007 | −6.95 |
| #8 | Major amputations for CLTI | 66 (3.09) | 73 (4.49) | 0.02 | 10.61 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 367 (17.18) | 208 (12.8) | 0.0002 | −43.32 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 1 (0.05) | 2 (0.12) | 0.14 | 100.00 |
| #11 | Symptomatic ICA stenosis operated in urgency | 36 (1.69) | 41 (2.52) | 0.09 | 13.89 |
| #12 | Treatment for venous ulcers | 129 (6.04) | 104 (6.4) | 0.61 | −19.38 |
| #13 | Diagnosis of deep vein thrombosis | 165 (7.72) | 138 (8.49) | 0.37 | −16.36 |
| Activities | January/ February 2020 (no COVID) (n = 1968) n (%) | March/ April 2020 (COVID) (n = 1074) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 192 (9.76) | 122 (11.36) | 0.17 | −36.46 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 35 (1.78) | 28 (2.61) | 0.14 | −20.00 |
| #3 | Post-EVAR surveillance | 317 (16.11) | 117 (10.89) | 0.0001 | −63.09 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 21 (1.07) | 10 (0.93) | 0.60 | −52.38 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 108 (5.49) | 85 (7.91) | 0.01 | −21.30 |
| #6 | Treatment for R3-PAD | 303 (15.4) | 126 (11.73) | 0.005 | −58.42 |
| #7 | Revascularizations for CLTI | 277 (14.08) | 179 (16.67) | 0.06 | −35.38 |
| #8 | Major amputations for CLTI | 71 (3.61) | 74 (6.89) | <0.0001 | 4.23 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 322 (16.36) | 118 (10.99) | 0.0001 | −63.35 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 1 (0.05) | 4 (0.37) | 0.08 | 300.00 |
| #11 | Symptomatic ICA stenosis operated in urgency | 29 (1.47) | 24 (2.23) | 0.16 | −17.24 |
| #12 | Treatment for venous ulcers | 119 (6.05) | 57 (5.31) | 0.43 | −52.10 |
| #13 | Diagnosis of deep vein thrombosis | 173 (8.79) | 130 (12.1) | 0.004 | −24.86 |
| Activities | January 2020 (no COVID) (n = 1045) n (%) | January 2021 (COVID) (n = 809) n (%) | p-Value | Delta % | |
|---|---|---|---|---|---|
| #1 | Open repair/EVAR for asymptomatic AAA | 102 (9.76) | 85 (10.51) | 0.62 | −16.67 |
| #2 | Open repair/EVAR for primary ruptured or symptomatic AAA | 18 (1.72) | 15 (1.85) | 0.87 | −16.67 |
| #3 | Post-EVAR surveillance | 162 (15.5) | 144 (17.8) | 0.19 | −11.11 |
| #4 | Previous EVAR treated again for recurring symptomatic or ruptured AAA, or endoleak type 1, 3, or 2 with sac expansion | 11 (1.05) | 6 (0.74) | 0.49 | −45.45 |
| #5 | Treatment for thrombotic acute lower limb ischemia | 59 (5.65) | 44 (5.44) | 0.85 | −25.42 |
| #6 | Treatment for R3-PAD | 175 (16.75) | 92 (11.37) | 0.001 | −47.43 |
| #7 | Revascularizations for CLTI | 141 (13.49) | 142 (17.55) | 0.02 | 0.71 |
| #8 | Major amputations for CLTI | 34 (3.25) | 44 (5.44) | 0.02 | 29.41 |
| #9 | Revascularizations for asymptomatic severe ICA stenosis | 164 (15.69) | 87 (10.75) | 0.002 | −46.95 |
| #10 | Asymptomatic severe ICA stenosis on surgical waiting list complicated to total obstruction | 0 (0) | 0 (0) | - | |
| #11 | Symptomatic ICA stenosis operated in urgency | 16 (1.53) | 13 (1.61) | 0.86 | −18.75 |
| #12 | Treatment for venous ulcers | 67 (6.41) | 61 (7.54) | 0.35 | −8.96 |
| #13 | Diagnosis of deep vein thrombosis | 96 (9.19) | 76 (9.39) | 0.88 | −20.83 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martelli, E.; Sotgiu, G.; Saderi, L.; Federici, M.; Sangiorgi, G.; Zamboni, M.; Martelli, A.R.; Accarino, G.; Bianco, G.; Bonanno, F.; et al. How the First Year of the COVID-19 Pandemic Impacted Patients’ Hospital Admission and Care in the Vascular Surgery Divisions of the Southern Regions of the Italian Peninsula. J. Pers. Med. 2022, 12, 1170. https://doi.org/10.3390/jpm12071170
Martelli E, Sotgiu G, Saderi L, Federici M, Sangiorgi G, Zamboni M, Martelli AR, Accarino G, Bianco G, Bonanno F, et al. How the First Year of the COVID-19 Pandemic Impacted Patients’ Hospital Admission and Care in the Vascular Surgery Divisions of the Southern Regions of the Italian Peninsula. Journal of Personalized Medicine. 2022; 12(7):1170. https://doi.org/10.3390/jpm12071170
Chicago/Turabian StyleMartelli, Eugenio, Giovanni Sotgiu, Laura Saderi, Massimo Federici, Giuseppe Sangiorgi, Matilde Zamboni, Allegra R. Martelli, Giancarlo Accarino, Giuseppe Bianco, Francesco Bonanno, and et al. 2022. "How the First Year of the COVID-19 Pandemic Impacted Patients’ Hospital Admission and Care in the Vascular Surgery Divisions of the Southern Regions of the Italian Peninsula" Journal of Personalized Medicine 12, no. 7: 1170. https://doi.org/10.3390/jpm12071170
APA StyleMartelli, E., Sotgiu, G., Saderi, L., Federici, M., Sangiorgi, G., Zamboni, M., Martelli, A. R., Accarino, G., Bianco, G., Bonanno, F., Bracale, U. M., Cappello, E., Cioffi, G., Colacchio, G., Crinisio, A., De Vivo, S., Dionisi, C. P., Flora, L., Impedovo, G., ... Settembrini, A. M. (2022). How the First Year of the COVID-19 Pandemic Impacted Patients’ Hospital Admission and Care in the Vascular Surgery Divisions of the Southern Regions of the Italian Peninsula. Journal of Personalized Medicine, 12(7), 1170. https://doi.org/10.3390/jpm12071170










